Abstract
The first aim of this investigation was to quantify the distribution of trapezius muscle activity with different scapular postures while seated. The second aim of this investigation was to examine the association between changes in cervical and scapular posture when attempting to recruit different subdivisions of the trapezius muscle. Cervical posture, scapular posture, and trapezius muscle activity were recorded from 20 healthy participants during three directed shoulder postures. Planar angles formed by reflective markers placed on the acromion process, C7, and tragus were used to quantify cervical and scapular posture. Distribution of trapezius muscle activity was recorded using two high-density surface electromyography (HDsEMG) electrodes positioned over the upper, middle, and lower trapezius. Results validated the assumption that directed scapular postures preferentially activate different subdivisions of the trapezius muscle. In particular, scapular depression was associated with a more inferior location of trapezius muscle activity (r = 0.53). Scapular elevation was coupled with scapular abduction (r = 0.52). Scapular adduction was coupled with cervical extension (r = 0.35); all other changes in cervical posture were independent of changes in scapular posture. This investigation provides empirical support for reductions in static loading of the upper trapezius and improvements in neck posture through verbal cueing of scapular posture.
Keywords: High-density EMG, Trapezius muscle, Cervical posture, Scapular posture
1. Introduction
Poor neck and shoulder postures may contribute to the high incidence of chronic neck pain in visual display unit (VDU) users (Falla et al., 2007; Gerr et al., 2004; Kimura et al., 2007; McLean, 2005; Szeto et al., 2002). Poor neck posture is defined as a forward head posture, which is a combination of lower cervical flexion and upper cervical extension (Yip et al., 2008). Poor shoulder posture is defined as a combination of scapular abduction and elevation. Coupling of these two poor postures results in a “hunched” posture, which abnormally loads surrounding muscles (Chiu et al., 2002; Szeto et al., 2002; Falla et al., 2004; McLean, 2005; Yoo and Kim, 2010). Clinical signs of trapezius myalgia, characterized by tightness and palpable tender points in the trapezius muscle, have been documented in approximately one third of workers with chronic neck or shoulder pain (Sjøgaard et al., 2006). In addition, poor postures in the cervical spine and scapulae during prolonged static sitting postures have been linked to pain development (Falla et al., 2004; Szeto et al., 2005).
Postural correction is aimed toward reducing the static load on surrounding muscles, and correction of cervical posture is often recommended for treatment and prevention of chronic neck pain (Enwemeka et al., 1986; Falla et al., 2007). An advantage of postural correction compared to other therapies, such as analgesics, is that retraining of motor control strategies may have longer lasting effects and may prevent the recurrence of pain caused by cumulative overuse. Despite the primary function of the trapezius in scapular stabilization and evidence of scapular muscle weakness in patients with chronic neck pain compared to healthy controls (Petersen and Wyatt, 2011; Shahidi et al., 2012), correction of scapular posture has received less attention than correction of cervical posture in studies of neck pain (Wegner et al., 2010).
The primary anatomic connections of the trapezius are to both the scapulae and the cervicothoracic spine; however, potential coupling of cervical and scapular motions with trapezius activation has not been examined during postural tasks. The muscle architecture in the trapezius is complex and varies across three functional subdivisions (upper, middle, and lower). Primary functions of the trapezius are: 1) scapular adduction and depression; and 2) cervical extension and rotation (Johnson et al., 1994). In static seated postures, such as during VDU use, the upper trapezius activates to stabilize the cervical spine and scapulae. Although the subdivisions of the trapezius can be recruited independently with biofeedback training (Holtermann et al., 2009), the widespread assumption that trapezius activation can be redistributed with verbal cueing of scapular postures to activate individual subdivisions of the muscle has not been validated.
The primary aim of this study was to compare the distribution of trapezius muscle activity across a broad range of scapular motion. We hypothesized that inferior–superior shifts in the distribution of trapezius muscle activity would occur with movements of the scapulae in the frontal plane, and that these shifts would be more strongly associated with changes in scapular posture than with changes in cervical posture. The second aim was to examine the association between changes in cervical and scapular posture across the scapular postures. We hypothesized that changes in cervical and scapular posture would be correlated due to coupling of neck and scapular motions with trapezius activation.
2. Methods
2.1. Participants
Twenty participants (10 males, age: 30.4 ± 9.9 years, height: 183.8 ± 8.0 cm, mass: 84.1 ± 12.8 kg and 10 females, age: 36.5 ± 13.9 years, height: 171.1 ± 5.9 cm, mass: 77.5 ± 9.5 kg) without a history of chronic neck or shoulder pain participated in this single cohort investigation. Each participant provided a written, informed consent in accordance with the University of Denver Institutional Review Board and the Colorado Multiple Institutional Review Board prior to the start of the experimental session. Each participant visited the laboratory for one data collection in which cervical posture, scapular posture, and trapezius muscle activity were collected during three test positions.
2.2. Instrumentation
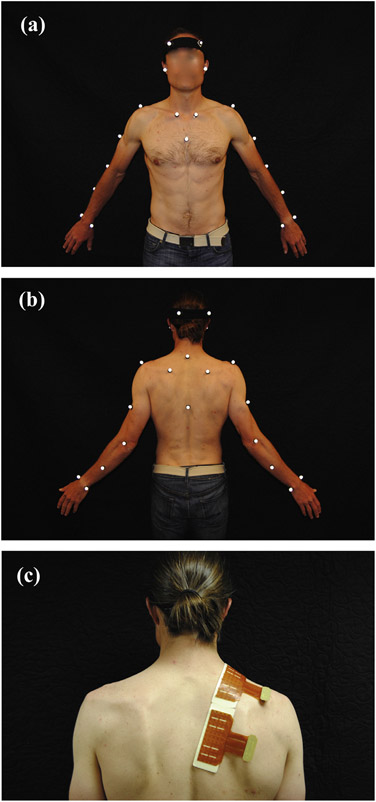
Each participant was instrumented with 25 reflective markers (Fig. 1a) used to record motion (100 Hz sampling frequency) with eight cameras surrounding the motion capture area (Vicon, Centennial, CO). High-density surface electromyography (HDsEMG) signals were recorded from two semi-disposable adhesive electrode arrays (ELSCH064NM2 Pin Out, OT Bioelettronica, Torino, Italy). The superior electrode array was placed overlying the upper and middle trapezius, and the inferior electrode array was placed overlying the middle and lower trapezius (Fig. 1b). Each electrode array was composed of 64 electrodes in a 13 × 5 orientation, with an 8-mm inter electrode distance (IED) and a 3-mm electrode diameter. A missing electrode in the inferior-lateral corner of each array was designated as the origin for assigning relative electrode positions (Fig. 2a). EMG signals were amplified (EMG-USB2 amplifier, OT Bioelettronica, Torino, Italy; bandwidth 10–500 Hz) by 5000, sampled at 2048 Hz, and converted to a digital signal by a 12-bit A/D converter. Visual inspection of the raw EMG signals was performed in post-processing to identify any channels with poor contact or short circuits, and low quality signals were linearly interpolated using adjacent channels (Gallina et al., 2013).
Fig. 1.
Reflective marker placement used to track cervical and scapular postures during three anatomically directed test positions: (a) anterior view, (b) posterior view, and (c) high-density surface EMG (HDsEMG) electrode array placement to record changes in the distribution of trapezius muscle activity across three test positions.
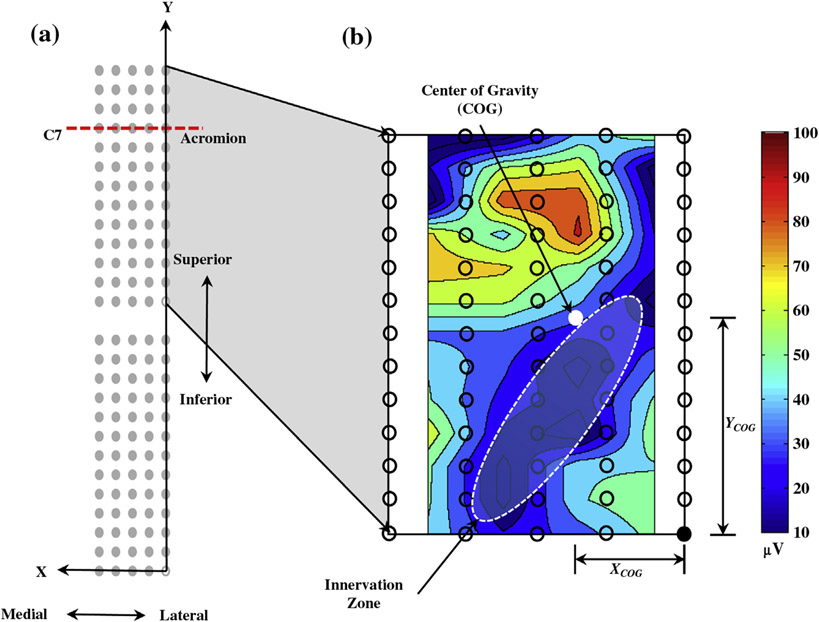
Fig. 2.
(a) Schematic of HDsEMG electrode array with position on trapezius. Array placement was normalized across all participants using a superior array with the 4th row placed along the C7-acromion line. (b) Example of topographical map (interpolation by a factor of 8) of 51 bipolar average rectified values of superior array, showing the center of gravity (white dot) and innervation zone (oval).
The innervation zone of the upper trapezius was used to standardize electrode array placement across participants (Farina et al., 2002). The main innervation zone of the upper trapezius was identified using a dry linear array (SA 16/5, OT Bioelettronica, Torino, Italy) with 16 silver bar electrodes (5-mm IED, 1 mm width). The superior electrode array was placed parallel to muscle fiber direction, with the 4th electrode row along the C7-acromion line and the most medial electrode column 10-mm distal from the innervation zone (Fig. 2a) (Farina et al., 2008). The skin beneath the electrode arrays was lightly abraded before placement. A reference electrode was placed on the ulnar styloid process of the dominant side of the participant.
2.3. Experimental protocol
Each participant was instructed to sit in a chair without trunk or arm support in an upright position, with the hips and knees at approximately 90° and the feet resting on the floor. The participant was instructed by a researcher to maintain a “neutral” posture in which their trunk was upright, chin was tucked, and scapulae were slightly depressed and adducted. After coaching and practice the participant maintained the neutral posture for 1 minute while marker position and EMG signals were recorded.
Starting from the neutral posture, the participant adopted three test positions that were intended to activate different anatomic subdivisions of the trapezius muscle: (1) scapular elevation (upper trapezius), (2) scapular adduction (middle trapezius), and (3) scapular adduction and depression (lower trapezius). These three postures were chosen because they create a broad range of motion of the scapulae, and are thought to activate distinct subdivisions of the muscle. No instructions were given to the participant with regard to head posture. The order of test positions was randomized. Each posture was performed to the end range of movement and held for 30 s. The participant rested for approximately 60 s between each posture. The duration of the directed scapular postures is less than the coached neutral posture to avoid potential effects of fatigue when holding the posture at the maximum range of motion. We chose a longer duration for the coached neutral posture to obtain robust data used for standardizing all dependent variables (see Section 2.5).
2.4. Data processing
The HDsEMG signals were filtered using a 2nd order Butterworth filter (10–400 Hz). Fifty-one bipolar signals were calculated from each electrode array. The average rectified value was computed from each bipolar recording from adjacent, non-overlapping signal epochs of 0.5 s. To characterize the spatial distribution of trapezius muscle activity, the center of gravity (COG) was calculated from the 51 bipolar average rectified values recordings (Farina et al., 2008) in the medial–lateral direction (XCOG) and the inferior–superior direction (YCOG) (Fig. 2b).
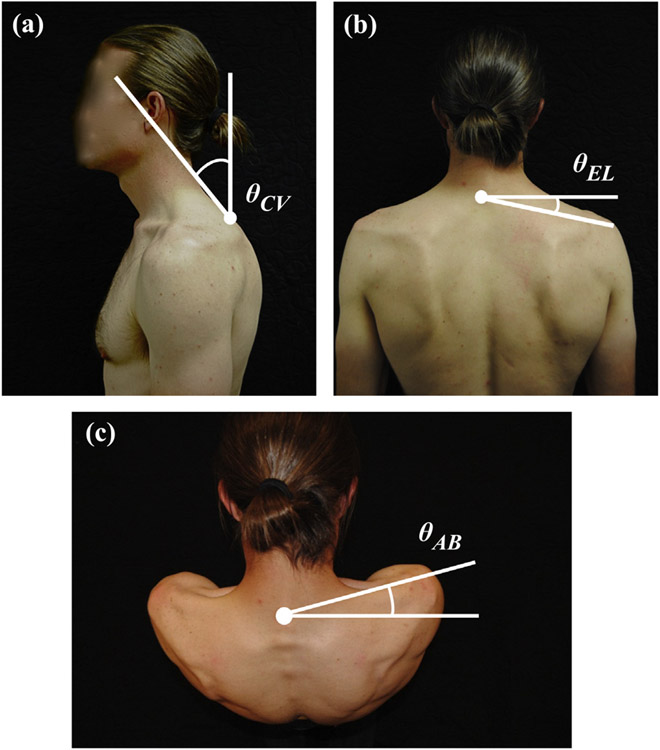
Cervical and scapular postures were quantified during each test position by three angle measures. Marker data were filtered with a 4th order, zero phase lag, Butterworth filter (5 Hz lowpass cutoff frequency). The cranial–vertebral angle (θCV) was calculated as the angle of a line from C7 to the tragus with respect to the frontal plane defined in a torso-fixed reference frame (Fig. 3a). Because overlying soft tissue and an irregular bone shape preclude accurate measurement of the position of the scapulae with motion capture, scapular posture was quantified by the angle of a line from C7 to the acromion process. This line was projected onto frontal and transverse planes defined in a torso reference frame. The angle between C7 and the acromion in the frontal plane (θEL) represented scapular elevation and depression (Fig. 3b). The angle between C7 and the acromion in the transverse plane (θAB) represented scapular adduction and abduction (Fig. 3c).
Fig. 3.
Three postures were measured during the experiment: (a) cervical posture (θCV) where positive angle indicates cervical flexion and negative angle indicates cervical extension; (b) scapular elevation/depression (θEL) where positive angle indicates scapular elevation and negative angle indicates scapular depression; (c) scapular abduction/adduction (θAB) where positive angle indicates scapular abduction and negative angle indicates scapular adduction. A local coordinate system origin was defined by a marker placed on the C7 vertebrae.
Trapezius muscle activity, cervical posture, and scapular posture were averaged across a 15-s window, that began 10 s after assuming the test position to ensure the measurements reflected a stable end range posture (Fig. 4).
Fig. 4.
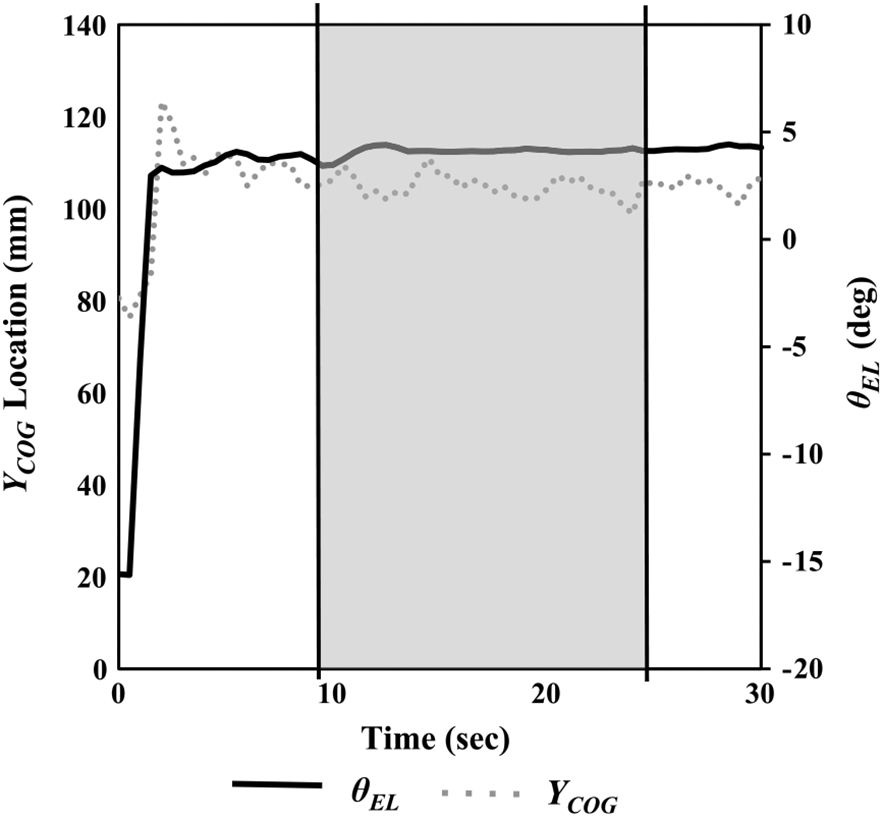
Example of data window used to obtain every dependent variable (averaged across 10–25 s). Scapular elevation (θEL) and the distribution of trapezius muscle activity in the superior–inferior direction (YCOG) during scapular elevation for a representative subject.
2.5. Statistical analysis
To standardize the dependent variables across participants, all measurements were referenced to the coached neutral posture where a value of zero represents no change in the dependent variable with respect to the coached neutral posture. Changes in trapezius muscle activity were defined as ΔXCOG and ΔYCOG. Positive ΔXCOG and ΔYCOG values indicated a more medial and superior location of trapezius muscle activity with respect to the coached neutral posture, respectively. Changes in cervical and scapular posture were defined as ΔθCV, ΔθEL, and ΔθAB. Positive ΔθCV indicated cervical flexion, and negative ΔθCV indicated cervical extension. Positive ΔθEL indicated scapular elevation, and negative ΔθEL indicated scapular depression. Positive ΔθAB indicated scapular abduction, and negative ΔθAB indicated scapular adduction.
Two ensure that each participant achieved three separate postures, two-tailed one sample t-tests were used to determine if trapezius activation (ΔXCOG, ΔYCOG) and cervical and scapular posture (ΔθCV, ΔθEL, ΔθAB) were different from the neutral posture in each of the three test positions (scapular elevation, scapular adduction, scapular adduction and depression). Differences in trapezius activation (ΔXCOG, ΔYCOG) and cervical and scapular posture (ΔθCV, ΔθEL, ΔθAB) between test positions were compared using separate one-factor analysis of variance (ANOVA) tests with repeated measures, in which scapular posture (3 levels) was treated as a fixed effect and subjects were treated as a random factor. Significant main effects were followed by pairwise comparisons with a Bonferroni correction (α = 0.017). The level of significance was set at 0.05 for all inferential tests.
The associations between trapezius activation (ΔXCOG, ΔYCOG) and cervical and scapular posture (ΔθCV, ΔθEL, ΔθAB) were quantified with Pearson product-moment correlations. The associations between cervical posture (ΔθCV) and scapular postures (ΔθEL and ΔθAB) were quantified with Pearson product-moment correlations. Latin hypercube sampling (Laz and Browne, 2010) followed by a bootstrap was used to ensure that repeatability would not affect the correlations (Efron and Tibshirani, 1993; Curran-Everett, 2009). Sixty Pearson product-moment correlations were calculated with one randomly selected data point per participant using orthogonal Latin hypercube random sampling. Bias-corrected accelerated bootstrap 99% confidence intervals were estimated from 10,000 bootstrap replications of the 60 Pearson product-moment correlations. Correlations were considered significantly different from zero if the 99% confidence interval did not cross zero (α = 0.01). The strength of the association was qualitatively interpreted as uncorrelated (r < 0.25), fairly correlated (0.25 ⩽ r < 0.50), moderately correlated (0.5 ⩽ r < 0.75), or highly correlated (0.75 ⩽ r < 1.0) (Portney and Watkins, 2000).
3. Results
3.1. Effect of test position on trapezius muscle activity, cervical posture, and scapular posture
There was a significant difference in YCOG between postures (F = 12.111, P < 0.001). YCOG was 22.98 ± 34.86 mm lower during scapular adduction than compared to scapular elevation (t = −2.948, P = 0.008). YCOG was 36.29 ± 36.11 mm lower during scapular adduction and depression than compared to scapular elevation (t = −4.494, P < 0.001) (Fig. 5b).
Fig. 5.
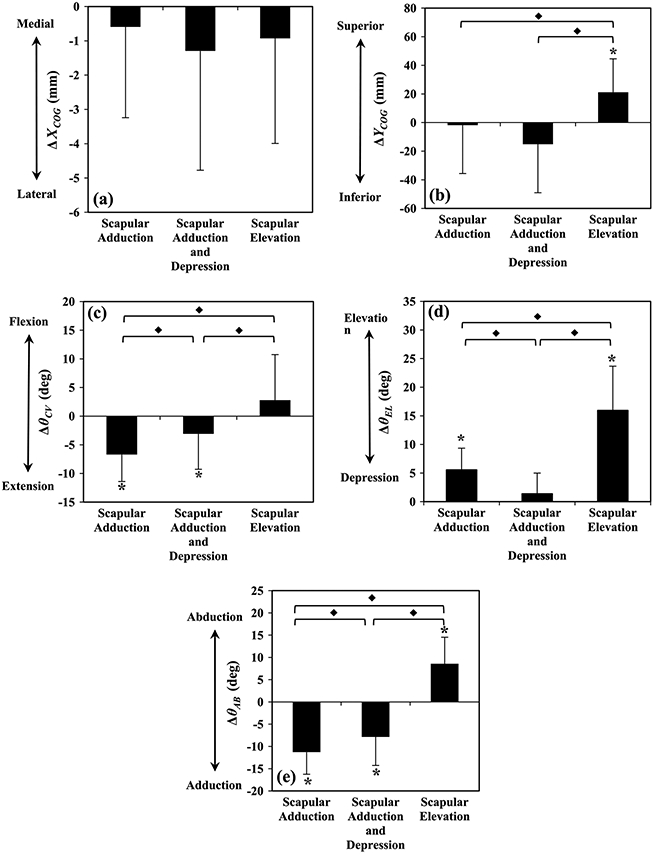
Mean (SD) change in trapezius muscle activity in the (a) medial–lateral direction (ΔXCOG), (b) inferior–superior direction (ΔYCOG), (c) cervical flexion/extension (ΔθCV), (d) scapular elevation/depression (ΔθEL), and (e) scapular abduction/adduction (ΔθAB) with respect to the coached neutral posture during three anatomically directed test positions. A value of zero indicates a variables value during coached neutral posture. * Indicates a statistically significant difference from neutral posture (P < 0.05). φ Indicates a statistically significant difference between postures (P < 0.05).
There was a significant difference in θCV between postures (F = 16.052, P < 0.001). θCV was 3.6 ± 4.8° smaller during scapular adduction than compared to scapular adduction and depression (t = −3.29, P = 0.004). θCV was 9.5 ± 9.0° smaller during scapular adduction than compared to scapular elevation (t = −4.60, P <0.001). θCV was 5.9 ± 7.7° smaller during scapular adduction and depression than compared to scapular elevation (t = −3.331, P = 0.004) (Fig. 5c).
There was a significant difference in θEL between postures (F = 64.692, P < 0.001). θEL was 4.2 ± 3.3° larger during scapular adduction than compared to scapular adduction and depression (t = 5.655, P < 0.001). θEL was 10.4 ± 6.6° smaller during scapular adduction than compared to scapular elevation (t = −6.996, P < 0.001). θEL was 14.6 ± 6.7° smaller during scapular adduction and depression than compared to scapular elevation (t = −9.795, P < 0.001) (Fig. 5d).
There was a significant difference in in θAB between postures (F = 14.178, P = 0.001). θAB was 3.4 ± 4.9° smaller during scapular adduction than compared to scapular adduction and depression (t = −3.131, P = 0.006). θAB was 19.8 ± 7.3° smaller during scapular adduction than compared to scapular elevation (t = −12.122, P < 0.001). θAB was 16.4 ± 8.4° smaller during scapular adduction and depression than compared to scapular elevation (t = −8.797, P < 0.001) (Fig. 5e).
3.2. Associations between cervical posture, scapular posture, and trapezius muscle activity
All correlation coefficients were statistically different from zero except for the association between ΔXCOG and ΔθCV. ΔθEL was moderately correlated with ΔYCOG (r = 0.53 [0.49, 0.56]) (Table 1, Fig. 6). ΔθEL was moderately correlated with ΔθAB (r = 0.52 [0.48, 0.56]) (Table 2, Fig. 6). ΔθAB was fairly correlated with ΔYCOG (r = 0.27 [0.22, 0.32]) (Table 1). ΔθCV was fairly correlated with ΔθAB and ΔθEL (r = 0.35 [0.29, 0.35], r = 0.28 [0.19, 0.34], respectively) (Table 2). All other combinations were uncorrelated (r < 0.25).
Table 1.
Latin-hypercube random sampling was used to generate 60 Pearson-product moment correlation coefficients associating changes in scapular posture (ΔβAB, ΔθEL), cervical posture (ΔθCV), and changes in the distribution of trapezius muscle activity (ΔXCOG, ΔYCOG) across all three distinct shoulder postures. Bias-corrected accelerated bootstrap confidence intervals were estimated from 10,000 bootstrap replications of 60 Pearson product-moment correlations coefficients (99% confidence interval). Bold indicates correlation coefficient (r) was significantly different from zero.
| ΔXCOG | ΔYCOG | |
|---|---|---|
| ΔθCV |
r = −0.01 (−0.07, 0.04) |
r = 0.17
(0.10, 0.24) |
| ΔθEL |
r = −0.19 (−0.25, −0.13) |
r = 0.53
(0.49, 0.56) |
| ΔθAB |
r = 0.09
(0.03, 0.14) |
r = 0.27
(0.22, 0.32) |
Fig. 6.
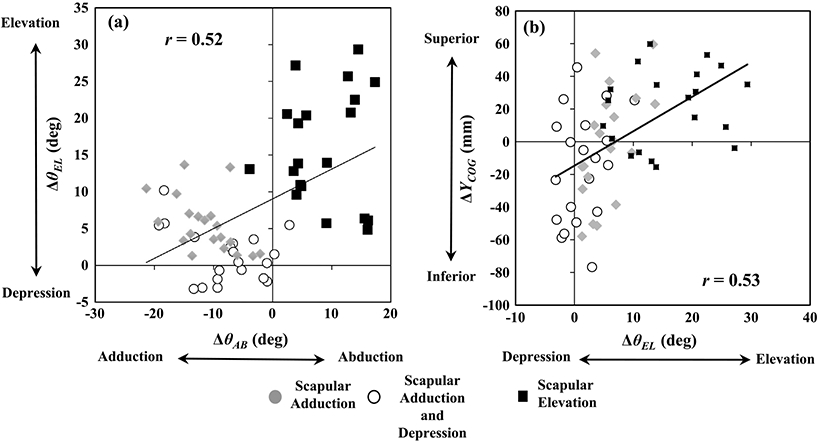
Correlation between (a) cervical posture (ΔθCV) and scapular abduction/adduction (ΔθAB) and (b) distribution of trapezius muscle activity in the inferior–superior direction (ΔYCOG) and scapular elevation/depression (ΔθEL). All data were referenced to the coached neutral posture and are grouped according to the three anatomically directed test positions (scapular elevation, scapular adduction, and scapular adduction and depression).
Table 2.
Latin-hypercube random sampling was used to generate 60 Pearson-product moment correlation coefficients associating changes in scapular posture (ΔθAB, ΔθEL) and cervical posture (ΔθCV) across all three distinct shoulder postures. Bias-corrected accelerated bootstrap confidence intervals were estimated from 10,000 bootstrap replications of 60 Pearson product-moment correlation coefficients (99% confidence interval). Bold indicates correlation coefficient (r) was significantly different from zero.
| ΔθCV | ΔθEL | ΔθAB | |
|---|---|---|---|
| ΔθCV |
r = 0.28
(0.19, 0.34) |
r = 0.35
(0.29, 0.42) |
|
| ΔθEL |
r = 0.52
(0.48, 0.56) |
||
| ΔθAB |
4. Discussion
We investigated the association between cervical posture, scapular posture, and the distribution of trapezius muscle activity during anatomically directed test positions that aimed to activate the three functional subdivisions of the trapezius muscle. The assumption that trapezius muscle activity can be redistributed between different functional subdivisions with verbal cueing was validated by directional shifts in the distribution of trapezius muscle activity between test positions. Scapular position in the frontal plane was moderately correlated with inferior–superior shifts in the distribution of trapezius muscle activity and scapular elevation was moderately correlated with scapular abduction. These findings indicate that an inferior shift in the distribution of trapezius muscle activity can be achieved by altering the position of the scapulae.
Each of the three test postures was intended to activate a different subdivision of the trapezius, and resulted in the expected changes in scapular posture and redistribution of trapezius muscle activity in the inferior–superior direction. This finding validates the use of verbal cueing, which is commonly used in clinical settings, to selectively activate functional subdivisions of the trapezius muscle by altering the position of the scapula. Interestingly, we observed no change in the distribution of trapezius muscle activity in the medial–lateral direction across test positions. This result may reflect a uniform propagation of action potentials along muscle fibers running in a medial–lateral direction from the spine to the scapula, present in all subdivisions of the trapezius muscle.
Correlation analyses demonstrate that scapular elevation was coupled to scapular abduction, indicating motion in both frontal and sagittal planes, which is consistent with previous findings (Ebaugh et al., 2005). In addition, fair correlations existed between cervical flexion and scapular abduction as well as between cervical flexion and scapular elevation. Although correlations between cervical and scapular posture were fair among healthy individuals, we anticipate that patients with neck or shoulder pathology may demonstrate stronger associations due to regional interdependence of the cervicoscapular region. Consistent with clinical theory (Behrsin and Macguire, 1986; Griegel-Morris et al., 1992; Szeto et al., 2002; Ha et al., 2011; Desai et al., 2013), these findings provide the first empirical evidence that cervical posture may be coupled to scapular posture such that a reduction in forward head posture can be achieved through verbal cues to adduct and depress the scapulae.
A shift in activation to the upper portion of the trapezius muscle was associated with scapular elevation, but not cervical extension. The lack of association between changes in trapezius muscle activity and changes in cervical posture is consistent with previous findings (Shahidi et al., 2013), and may suggest that efforts to reduce loading of the upper trapezius should emphasize retraining of scapular posture. The upper trapezius appears to play a primary role in scapular stabilization, whereas the intrinsic cervical muscles may play a more prominent role in neck posture during static sitting postures. We are aware of only one observational study of scapulae postural correction for the treatment of chronic neck pain (Wegner et al., 2010); therefore, additional research is needed to investigate the efficacy of postural training of the scapular muscles.
Scapular elevation was associated with activation of the upper trapezius, which supports the recommendation to avoid scapular elevation to help reduce static loading of the upper trapezius during tasks that require prolonged sitting. This shift in activation in the inferior–superior direction is consistent with previous investigations (Kleine et al., 2000; Madeleine et al., 2006; Farina et al., 2008). The lack of change in scapular depression and inferior activation during the test position intended to activate the lower trapezius (scapular adduction and depression) was an exception to the expected pattern of change based on the anatomic function of this muscle. This may have occurred because all variables were referenced to a neutral posture in which the lower trapezius was already active to position the scapula in a slightly adducted and depressed position.
Currently, the most accurate method to measure cervicoscapular posture is through radiographic techniques. The cranial–vertebral flexion angle is a poor surrogate for quantifying forward head postures because this position is achieved through a combination of lower cervical flexion (C7–C4) and upper cervical extension (C3–C1) (Szeto et al., 2002). To represent scapular adduction/abduction and elevation/depression, we related the acromion to C7 in the frontal and transverse planes of the torso, respectively. This method has been used as a reliable surrogate of scapular position (Meskers et al., 2007; van Andel et al., 2009); however, these investigations relied on marker clusters placed on rigid frames on the acromion, which may interfere with upper-extremity motion. The current method used two-dimensional planar angles, which could be implemented in clinical or occupational settings with two photographic cameras positioned behind and above the patient to measure scapular elevation/depression and abduction/adduction, respectively, during simulated or actual job tasks (illustrated in Fig. 3). This may provide a feasible and objective method of assessing impaired scapular posture during ergonomic evaluations, as well as monitoring the response to postural interventions designed to reduce loading of scapular muscles throughout the workday.
Several limitations to this investigation should be considered. First, the postures were performed to the end range of scapular motion. Large excursions in scapular posture increased the power of correlation analyses, but may overestimate the effects of more subtle postural changes on muscle activation patterns. Second, we did not consider the potential effects of fatigue on measures of muscle activation. A previous investigation on the effects of fatigue on the spatial distribution of trapezius muscle activity demonstrated a superior shift in COG throughout contraction duration (Farina et al., 2008). Because the order of test postures was randomized, the contractions were submaximal and short in duration (30 s) and participants were healthy, we do not consider fatigue to be a major confounding factor. Last, although the present findings may inform efforts to prevent the development of chronic neck pain in healthy individuals, the results cannot be generalized to patients who are currently experiencing pain because motor control strategies may differ in these individuals (Szeto et al., 2005; Goudy and McLean, 2006).
5. Conclusion
This study demonstrates that selective activation of individual subdivisions of the trapezius muscle may improve cervicoscapular posture and reduce the risk of injury caused by over activation of the upper trapezius. In addition, this is the first investigation to demonstrate coupling between cervical and scapular motions during three distinct shoulder postures. These findings indicate that scapular posture is more correlated with the distribution of trapezius muscle activity in comparison to cervical posture.
Acknowledgements
We thank Brett Donnermeyer and Oscar Reyes for their invaluable assistance with data collections.
Biographies

Brecca M. Gaffney is currently a PhD student at the University of Denver in the Human Dynamics Laboratory. She received a BS degree in mechanical engineering from the Colorado School of Mines and an MS degree in mechanical engineering from the University of Denver. Her current research in experimental biomechanics focuses on implementing EMG signals as rehabilitation therapies to musculoskeletal pain in the upper extremities.

Katrina S. Maluf received an MS degree in Physical Therapy (1999) and a PhD degree in Movement Science (2002) from Washington University in St. Louis, followed by a post-doctoral fellowship in neuromuscular physiology (2005) at the University of Colorado Boulder. She is currently an Associate Professor of Physical Therapy and founding Director of the Rehabilitation Science PhD Program at the University of Colorado Anschutz Medical Campus. Her research combines neurophysiologic and clinical techniques to investigate the mechanisms and management of stress-related musculoskeletal pain.

Douglas Curran-Everett graduated from Cornell University (BA), Duke University (MS in physical therapy), and the State University of New York at Buffalo (PhD in physiology). He is no Professor and Head of the Division of Biostatistics and Bioinformatics at National Jewish Health with an affiliate appointment as Professor in the Department of Biostatistics and Informatics in the Colorado School of Public Health at the University of Colorado Denver. He is accredited as a Professional Statistician by the American Statistical Association.

Bradley S. Davidson is an Assistant Professor in Mechanical Engineering and director of the Human Dynamics Laboratory at the University of Denver. He holds a BS in civil engineering from Tennessee Tech, an MS in engineering mechanics from Virginia Tech, and a PhD in biomedical engineering from the Virginia Tech–Wake Forest School of Biomedical Engineering and Sciences. His research in musculoskeletal biomechanics emphasizes measurement of human movement and motor control, with applications in spine stability, total knee arthroplasty, and Parkinson’s Disease.
Footnotes
Conflict of interest
None.
References
- Behrsin JK, Macguire K. Levator scapulae action during shoulder movement – a possible mechanism for shoulder pain of cervical origin. Aust J Physiother 1986;32(2):101–6. [DOI] [PubMed] [Google Scholar]
- Chiu TTW, Ku WY, Lee MH, Sum WK, Wan MP, Wong CY, et al. A study on the prevalence of and risk factors for neck pain among university academic staff in Hong Kong. J Occup Rehabil 2002;12(2):77–91. [DOI] [PubMed] [Google Scholar]
- Curran-everett D. Explorations in statistics: The bootstrap. Adv Physiol Educ 2009;2:286–92. [DOI] [PubMed] [Google Scholar]
- Desai NA, Khatri SM, Agarwal AB. Immediate effect of scapular repositioning with active cervical rotation in acute spasmodic torticollis. J Manipulative Physiol Ther Natl Univ Health Sci 2013: 10; 12–4. [DOI] [PubMed] [Google Scholar]
- Ebaugh DD, McClure PW, Karduna AR. Three-dimensional scapulothoracic motion during active and passive arm elevation. Clin Biomech 2005;20(7):700–9. [DOI] [PubMed] [Google Scholar]
- Efron B, Tibshirani RJ. An Introduction to the Bootstrap. Boca Raton, FL: Chapman & Hall/CRC; 1993. [Google Scholar]
- Enwemeka CS, Bonet IM, Ingle JA, Prudhithumrong S, Ogbahon FE, Gbenedio NA. Postural correction in persons with neck pain (II. Integrated electromyography of the upper trapezius in three simulated neck positions). J Orthop Sports Phys Ther 1986; 8(5): 240–2. [DOI] [PubMed] [Google Scholar]
- Falla D, Bilenkij G, Jull G. Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine (Phila. Pa. 1976). 2004. 1; 29(13): 1436–40. [DOI] [PubMed] [Google Scholar]
- Falla D, Jull G, Russell T, Vicenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther 2007;87(4):408–17. [DOI] [PubMed] [Google Scholar]
- Farina D, Madeleine P, Graven-Nielsen T, Merletti R, Arendt-Nielsen L. Standardising surface electromyogram recordings for assessment of activity and fatigue in the human upper trapezius muscle. Eur J Appl Physiol 2002;86(6):469–78. [DOI] [PubMed] [Google Scholar]
- Farina D, Leclerc F, Arendt-Nielsen L, Buttelli O, Madeleine P. The change in spatial distribution of upper trapezius muscle activity is correlated to contraction duration. J Electromyogr Kinesiol 2008;18(1):16–25. [DOI] [PubMed] [Google Scholar]
- Gallina A, Merletti R, Gazzoni M. Uneven spatial distribution of surface EMG: what does it mean? Eur J Appl Physiol 2013;113(4):887–94. [DOI] [PubMed] [Google Scholar]
- Gerr F, Marcus M, Monteilh C. Epidemiology of musculoskeletal disorders among computer users: lesson learned from the role of posture and keyboard use. J Electromyogr Kinesiol 2004;14(1):25–31. [DOI] [PubMed] [Google Scholar]
- Goudy N, McLean L. Using myoelectric signal parameters to distinguish between computer workers with and without trapezius myalgia. Eur J Appl Physiol 2006;97(2):196–209. [DOI] [PubMed] [Google Scholar]
- Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther 1992;72(6):425–31. [DOI] [PubMed] [Google Scholar]
- Ha S, Kwon O, Yi C, Jeon H, Lee W. Effects of passive correction of scapular position on pain, proprioception, and range of motion in neck-pain patients with bilateral scapular downward-rotation syndrome. Man Ther. Elsevier Ltd. 2011;16(6): 585–9. [DOI] [PubMed] [Google Scholar]
- Holtermann A, Roeleveld K, Mork PJ, Grönlund C, Karlsson JS, Andersen LL, et al. Selective activation of neuromuscular compartments within the human trapezius muscle. J Electromyogr Kinesiol 2009;19(5):896–902. [DOI] [PubMed] [Google Scholar]
- Johnson G, Bogduk N, Nowitzke A, House D. Anatomy and actions of the trapezius muscle. Clin Biomech 1994;9:44–50. [DOI] [PubMed] [Google Scholar]
- Kimura M, Sato H, Ochi M, Hosoya S, Sadoyama T. Electromyogram and perceived fatigue changes in the trapezius muscle during typewriting and recovery. Eur J Appl Physiol 2007;100(1):89–96. [DOI] [PubMed] [Google Scholar]
- Kleine BU, Schumann NP, Stegeman DF, Scholle HC. Surface EMG mapping of the human trapezius muscle: the topography of monopolar and bipolar surface EMG amplitude and spectrum parameters at varied forces and in fatigue. Clin Neurophysiol 2000;111(4):686–93. [DOI] [PubMed] [Google Scholar]
- Laz PJ, Browne M. A review of probabilistic analysis in orthopaedic biomechanics. Proc Inst Mech Eng Part H J Eng Med 2010;224(8):927–43. [DOI] [PubMed] [Google Scholar]
- Madeleine P, Leclerc F, Arendt-Nielsen L, Ravier P, Farina D. Experimental muscle pain changes the spatial distribution of upper trapezius muscle activity during sustained contraction. Clin Neurophysiol 2006;117(11):2436–45. [DOI] [PubMed] [Google Scholar]
- McLean L. The effect of postural correction on muscle activation amplitudes recorded from the cervicobrachial region. J Electromyogr Kinesiol 2005;15(6):527–35. [DOI] [PubMed] [Google Scholar]
- Meskers CGM, van de Sande MAJ, de Groot JH. Comparison between tripod and skin-fixed recording of scapular motion. J. Biomech. 2007; 40(4): 941–6. [DOI] [PubMed] [Google Scholar]
- Petersen SM, Wyatt SN. Lower trapezius muscle strength in individuals with unilateral neck pain. J Orthop Sports Phys Ther 2011;41(4):260–5. [DOI] [PubMed] [Google Scholar]
- Portney LG, Watkins MP. Foundations of clinical research: applications to practice. Upper Saddle River, NJ: Prentice-Hall Inc.; 2000. [Google Scholar]
- Shahidi B, Johnson CL, Curran-Everett D, Maluf KS. Reliability and group differences in quantitative cervicothoracic measures among individuals with and without chronic neck pain. BMC Musculoskelet. Disord. BMC Musculoskeletal Disorders 2012;13(1):215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahidi B, Haight A, Maluf K. Differential effects of mental concentration and acute psychosocial stress on cervical muscle activity and posture. J Electromyogr Kinesiol. Elsevier Ltd. 2013; 23(5): 1082–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjøgaard G, Søgaard K, Hermens HJ, Sandsjö L, Läubli T, Thorn S, et al. Neuromuscular assessment in elderly workers with and without work related shoulder/neck trouble: the NEW-study design and physiological findings. Eur J Appl Physiol 2006;96(2):110–21. [DOI] [PubMed] [Google Scholar]
- Szeto GPY, Straker L, Raine S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl Ergon 2002;33(1):75–84. [DOI] [PubMed] [Google Scholar]
- Szeto GPY, Straker LM, O’Sullivan PB. A comparison of symptomatic and asymptomatic office workers performing monotonous keyboard work–2: neck and shoulder kinematics. Man Ther 2005;10(4):281–91. [DOI] [PubMed] [Google Scholar]
- Van Andel C, van Hutten K, Eversdijk M, Veeger D, Harlaar J. Recording scapular motion using an acromion marker cluster. Gait Posture 2009;29(1):123–8. [DOI] [PubMed] [Google Scholar]
- Wegner S, Jull G, O’Leary S, Johnston V. The effect of a scapular postural correction strategy on trapezius activity in patients with neck pain. Man Ther. Elsevier Ltd. 2010; 15(6): 562–6. [DOI] [PubMed] [Google Scholar]
- Yip CHT, Chiu TTW, Poon ATK. The relationship between head posture and severity and disability of patients with neck pain. Man Ther 2008;13(2): 148–54. [DOI] [PubMed] [Google Scholar]
- Yoo W-G, Kim M-H. Effect of different seat support characteristics on the neck and trunk muscles and forward head posture of visual display terminal workers. Work 2010;36(1):3–8. [DOI] [PubMed] [Google Scholar]