“Tradition, Tradition, Tradition.” This declaration is the main theme of Fiddler on The Roof, the iconic musical that questions traditions; traditions that become integral parts of our daily lives and behaviors; traditions so ingrained that we don’t even question their value, practicality, or usefulness. Traditions give us comfort but do not promote inquiry, and as Tevye from the musical learns, some traditions do not fit into the modern world. Shortly after the percutaneous renal biopsy (PRB) was adopted as a critical diagnostic tool for nephrologists, it became tradition to train nephrology fellows in this procedure. Competence in this procedure eventually became a requirement (for both native and transplanted kidneys) by both the Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Internal Medicine (ABIM) (1,2). Nephrology fellowship program Training Program Directors (TPD) are required to “sign-off” on this procedure to certify that graduating nephrology fellows are “board eligible,” allowing them to take the nephrology subspecialty board exam. Given the changing landscape of nephrology, should renal biopsy training remain a requirement, or has tradition clashed with the modern world’s changing views on its value, practicality, and usefulness? I have been charged with arguing that the kidney biopsy should not remain a required procedure for training programs (the “CON” argument).
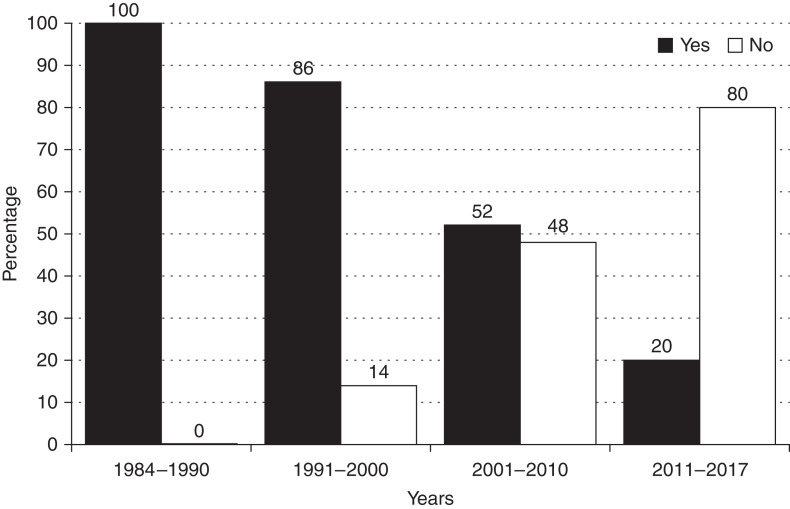
The procedure of obtaining tissue for diagnosis through percutaneous sampling of the kidney was developed in the early 1950s by Iverson, Brun, Kark, and Muehrcke, all nephrologists (3). As a result, the PRB has been a procedure “traditionally” performed by nephrologists. In 1990, a survey of 516 nephrologists who were trained from 1964 to 1974 reported that 95% of practicing nephrologists performed PRB. By 1995, 35% of PRB were performed by radiologists. By 2011, only 55% of nephrologists were performing PRB. And a report in 2012 found that over the 22-year time span of 1988–2010, only 35% of PRB were performed by nephrologists, with the majority of the others being done by the evolving subspecialty of interventional radiology (IR) (3). These findings were similar to a 2018 report that reported the practice habits of 55 nephrologists who had trained at Walter Reed Military Medical Center in which 83% considered themselves adequately trained to do the procedure; yet, only 35% of them were performing PRB (4). At Rush University Medical Center (RUMC) where I am the TPD, we have always made a point to train our fellows in PRB. In 2018, we surveyed 78 fellows who trained at RUMC between 1984 and 2017. We found that 100% considered themselves adequately trained in the procedure; yet, only 58% performed a PRB after graduation and entering practice. To emphasize these changing practices over time further, we broke down the group into four time periods on the basis of when fellowship training was completed: 1984–1990, 1991–2000, 2001–2010, and 2011–2017. As shown in Figure 1, the percentage of graduating fellows who did a single PRB post fellowship dropped from 100% in the early 1984–1990 training years to only 20% in the most recent period of 2011–2017. Of the 71 former RUMC trainees still in practice at the time of the survey, only 12 (17%) continued to perform their own renal biopsies! Of those fellows not performing PRBs, they all sent their patients to IR. The main reason they reported for this practice was that performing the biopsy themselves was too time-consuming and that the IR alternative was so readily available. Procedure liability was also a moderate factor in this decision for 52% of our past trainees not doing biopsies, but reimbursement was a consideration in only 30% (5). In fact, in the Walter Reed report, it was found that orders for a kidney biopsy increased as the PRB transitioned from nephrologists to interventional radiologists, suggesting that these considerations became barriers to nephrologists doing the procedure themselves (6).
Figure 1.
Performance of percutaneous renal biopsy post fellowship on the basis of the year of fellowship completion. Used with permission from Korbet et al. (5).
What are the pros and cons of this transition from nephrologist to interventional radiologist? Some potential concerns of interventional radiologists doing the “lion’s share” of the PRBs are sample adequacy and complication rate. Regarding the later, prospective comparisons are not available; however, in a retrospective analysis, there was no difference on the complication rate (hematoma or need for transfusion, gross hematuria or pain) between PRBs done by nephrologists or radiologists using real-time ultrasound (7). The issue of tissue adequacy is a bit more complicated. While Sousanieh et al. were not able to find a difference in the complication rates of PRB when using the smaller 18-gauge needle, they did find that that using it led to clinically significantly fewer glomeruli compared with 14- and 16-gauge PRB needles. A sample size of 20 glomeruli is generally considered an “adequate” sample to minimize the risk of missing a focal glomerular lesion. This magic number of 20 was obtained in 85% of PRB using a 14-gauge (average 2.3 cores obtained), 82% using a 16-gauge (average 2.3 cores), but only 46% using an 18-gauge biopsy needle (average 2.2 cores) (8). Of course, the glomerular yield using an 18-gauge needle can be increased by obtaining more cores. As interventional radiologists often use 18-gauge needles as a default for tissue sampling, communication by the nephrologist to the interventional radiologist on the number of desired cores or needle gauge size may be prudent.
An obvious advantage of interventional radiologists doing the PRB is that they are likely able to do the procedure using either real-time ultrasound (the means by which the majority of nephrologists are trained), in addition to computed tomography, which may be preferred for obese patients, cystic kidneys, or for those in whom kidney visualization by renal ultrasound is inadequate (7). Additionally, many IR programs are able to obtain tissue through the transvenous approach (TVRB)—a major advantage in patients with bleeding disorders. Despite the transvenous approach being typically limited to higher-risk patients, one study found no difference in diagnostic yield or complication rate for PRB (n=400) and TVRB (n=400 of whom 303 had a bleeding disorder) (7). And finally, an obvious advantage to IR-performed PRBs is that if a bleeding complication were to occur, it would be diagnosed and treated by the team that did the procedure.
I shall now address the elephant in the room: What even determines PRB competence? How many percutaneous renal biopsies should be performed before a nephrology fellow is considered competent? Do they all need to be supervised? Should a determination be on the basis of numbers alone (objective), or should there be some observer subjectivity to this determination? Neither the ABIM nor ACGME provides any specific guidance on this critical issue. In a 2008 poll in which 93 of 136 nephrology fellowship training programs responded, 28% of reporting programs had no minimum required number of biopsies, and of those programs that did have a minimum number, 25% required that only between zero and two procedures be done, and 20% required between three and six procedures (9). These numbers were consistent whether considering a biopsy of the native or transplanted kidney. Granted, competence probably is a function of both procedure number and innate skill, but can you really expect someone to be at a safe and proficient level when they have performed but a handful of procedures?
Additionally, it is not obvious if competence (however that is defined) in PRB is even an absolute requirement for graduation (ACGME) or board eligibility (ABIM). ACGME data suggest that 25% of fellows completing training in 2017 were not considered ready to perform temporary dialysis catheter placement or kidney biopsy without supervision (specific numbers for each procedure are not available) (10). Yet, I doubt any of these were not allowed to take the subspecialty boards. TPDs have admitted to “vouching” for PRB competence in their graduating trainees, despite lacking confidence in their ability (11).
Given the abysmal rate of nephrology graduates doing a single PRB after graduation, and the alternative of the procedure being done by interventional radiologists, where do we go from here? I would hardly recommend any program that feels they have the numbers and skills to train a fellow adequately to be competent in PRB to stop training altogether. Still, they should have the option not to attempt to “certify” every one of their fellows. Additionally, the many programs that struggle with this requirement for all their fellows and yet feel compelled to sign off on these trainees, despite not being convinced of their competence, should not be required to do so. The ACGME and ABIM should make competence in PRB an elective designation and not a mandated requirement (12).
All nephrology training programs should have the indications, contraindications, risks, and benefits of the PRB in their curriculum. Fellows not planning on PRB certification should observe several of the procedures, whether performed by a nephrologist or an interventional radiologist. Programs that decide to certify a fellow for PRB should establish a minimum number of procedures (I will go out on a limb and suggest a minimum of six for each for native and transplant PRB), with one of these being a successfully performed PRB observed by a nephrology or IR faculty member who regularly does the procedure. This should result in a program-specific standardized document that states competence in a given fellow performing a PRB and should specify if this certification includes PRB of both native and transplanted kidneys. This document should go into the fellow’s academic file and serve as a guide to hospital privileges upon graduation.
In conclusion, the time has come for sensibility and practicality to supersede tradition. The days of PRB as a procedure in which training and competence certification should be mandated have passed. It is time for the ACGME and the ABIM to accept this new paradigm and adjust their training and certification requirements accordingly.
Disclosures
The author has nothing to disclose.
Funding
None.
Acknowledgments
The content of this article reflects the personal experience and views of the author and should not be considered medical advice or recommendation. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the author.
Footnotes
Author Contributions
R.A. Rodby wrote the original draft and reviewed and edited the manuscript.
References
- 1.Accreditation Council for Graduate Medical Education : ACGME Program Requirements for Graduate Medical Education in Nephrology (Internal Medicine), revised 2017. Available at: https://www.acgme.org/globalassets/PFAssets/ProgramRequirements/148_Nephrology_2021_TCC.pdf?ver=2021-06-21-145258-737&ver=2021-06-21-145258-737. Accessed December 1, 2021
- 2.American Board of Internal Medicine : Nephrology Policies, 2018. Available at: https://www.abim.org/certification/policies/internal-medicine-subspecialty-policies/nephrology/. Accessed December 1, 2021
- 3.Korbet SM: Nephrology and the percutaneous renal biopsy: A procedure in jeopardy of being lost along the way. Clin J Am Soc Nephrol 7: 1545–1547, 2012. 10.2215/CJN.08290812 [DOI] [PubMed] [Google Scholar]
- 4.Yuan CM, Nee R, Little DJ, Narayan R, Childs JM, Prince LK, Raghavan R, Oliver JD 3rd; Nephrology Education Research and Development Consortium (NERDC) : Survey of kidney biopsy clinical practice and training in the United States. Clin J Am Soc Nephrol 13: 718–725, 2018. 10.2215/CJN.13471217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Korbet SM, Whittier WL, Rodby RA: Changing trends in the performance of percutaneous renal biopsy from nephrologist to interventional radiologist: A single-center experience. Am J Nephrol 48: 326–329, 2018. 10.1159/000493925 [DOI] [PubMed] [Google Scholar]
- 6.Gilbert SJ: Does the kidney biopsy portend the future of nephrology? Clin J Am Soc Nephrol 13: 681–682, 2018. 10.2215/CJN.03380318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hogan JJ, Mocanu M, Berns JS: The native kidney biopsy: Update and evidence for best practice. Clin J Am Soc Nephrol 11: 354–362, 2016. 10.2215/CJN.05750515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sousanieh G, Whittier WL, Rodby RA, Peev V, Korbet SM: Percutaneous renal biopsy using an 18-gauge automated needle is not optimal. Am J Nephrol 51: 982–987, 2020 [DOI] [PubMed] [Google Scholar]
- 9.Berns JS, O’Neill WC: Performance of procedures by nephrologists and nephrology fellows at U.S. nephrology training programs. Clin J Am Soc Nephrol 3: 941–947, 2008. 10.2215/CJN.00490108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norby SM: Requirements for procedural skills in nephrology training programs: Framing the conversation. Clin J Am Soc Nephrol 13: 1096–1098, 2018. 10.2215/CJN.02210218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pivert K: ASN Data Brief: Nephrology Procedures in GME, 2017. Available at: https://www.researchgate.net/publication/315065568. Accessed December 1, 2021
- 12.Brown RS: Kidney biopsy training and the future of nephrology: What about the patient? Clin J Am Soc Nephrol 13: 1105–1106, 2018. 10.2215/CJN.05870518 [DOI] [PMC free article] [PubMed] [Google Scholar]