Visual Abstract
Keywords: nephrology, program director, fellowship program, protected time, program administration, didactic teaching
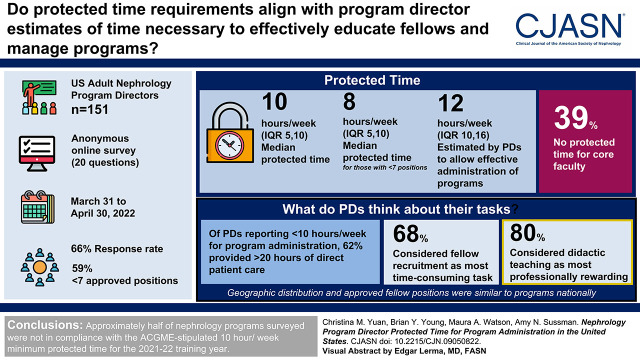
Abstract
Background and objectives
The Accreditation Council for Graduate Medical Education (ACGME) required that program directors receive 10–20 h/wk of protected time for program administration (including didactic teaching). In July 2022, this was reduced for all internal medicine subspecialties on the basis of program size, with 8 h/wk required for programs with fewer than seven fellows, the majority of nephrology programs.
Design, setting, participants, & measurements
We surveyed all 151 US adult nephrology program directors (ACGME Public List of Programs 2021–2022) to determine how much protected time they receive, how much they think is necessary, and the division of their professional time. The anonymous 20-question online survey was administered from March 31 to April 30, 2022. The analysis was descriptive.
Results
Response rate was 66% (99 of 151). Geographic distribution and approved fellow positions were similar to programs nationally; 59% had fewer than seven approved positions. Median protected time was 10 h/wk (interquartile range, 5–10), with 8 h/wk (interquartile range, 5–10) for those with fewer than seven positions. Program directors estimated needing 12 h/wk (interquartile range, 10–16) to effectively administer programs, including those with fewer than seven positions, a median 5 h/wk (interquartile range, 0–7) more than received. Of program directors reporting <10 h/wk for program administration, 62% provided >20 hours of direct patient care. Thirty-nine percent had no protected time for core faculty. Fellow recruitment (68%) was the most time-consuming task, and didactic teaching (80%) was the most professionally rewarding.
Conclusions
Approximately half of the nephrology programs surveyed were not in compliance with the ACGME-stipulated 10-h/wk minimum protected time for the 2021–2022 training year. Program directors estimated a median of 12 h/wk are needed to effectively manage programs.
Introduction
On July 1, 2022, the Accreditation Council for Graduate Medical Education (ACGME), citing a desire for standardization, adjusted protected time for program administration for all internal medicine subspecialty program directors (1). ACGME defines “program administration” as “nonclinical teaching and administration” (2). “Protected time” is defined as “salary support, supplemental compensation, educational value units, or relief of time from other professional duties” (2). Changes in ACGME-stipulated protected time for nephrology program leadership (program directors, associate program directors, and core clinical faculty) from 2019 to 2022 are summarized in Table 1.
Table 1.
Minimum dedicated/protected time for nephrology program leadership specified by the Accreditation Council for Graduate Medical Education
| Program Leadership | Before July 1, 2019 (5) | July 1, 2019 to June 30, 2022 (5) | July 1, 2022 (3) |
|---|---|---|---|
| Program director | 20 h/wk | 10–20 h/wka | 8 h/wk for <7 clinical fellows; 10 h/wk for 7–9 clinical fellows; 12 h/wk or more for ≥10 clinical fellowsb |
| Associate program director(s) (also count as core clinical faculty) | None stipulated | None stipulated | Required. As core faculty, 4 h/wk plus additional time on the basis of program size: 0 h/wk for <7 fellows; 1.2 h/wk for 7–9 fellows; 1.6 h/wk or more for ≥10 fellows |
| Key/core clinical faculty | 10 h/wk | None stipulated | 4 h/wkc |
| Minimum total hours for 6 fellow programs (program leadership: 1 program director; 4 core faculty, including the associate program director) | 60 h/wk (program director: 20 h; 4 core faculty: 40 h) | 10 h/wk (program director: 10 h) | 24 h/wk (program director: 8 h; associate program director: 4 h; 3 additional core faculty: 12 h) |
Defined as 25%–50% of salary. A 25% full-time equivalent was defined as “one and one quarter days per week” in the Accreditation Council for Graduate Medical Education Nephrology Program Requirements 2021 (2). On the basis of a standard 40-hour week, this would be 10–20 h/wk or 0.25–0.5 full-time equivalent.
Defined by the Accreditation Council for Graduate Medical Education as 0.2 full-time equivalent (fewer than seven fellows), 0.25 full-time equivalent (seven to nine fellows), and 0.3–0.5 full-time equivalent (ten or more fellows). One full-time equivalent is assumed to be a standard 40-hour work week.
Defined by the Accreditation Council for Graduate Medical Education as 0.1 full-time equivalent. One full-time equivalent is assumed to be a standard 40-hour work week.
These changes may have profound effects within nephrology training programs, reducing the minimum required program director protected time from 10 to 8 h/wk for programs with fewer than seven approved fellow positions (2,3). Although adjustments are made for larger programs, approximately two thirds of nephrology programs have fewer than seven positions, and the majority will be negatively affected (4). Core clinical faculty (one for every 1.5 fellows) will be required to have 4 h/wk of protected time, having had no specific requirement for the past 3 training years. Associate program directors will be required for all programs, but those in programs of fewer than seven fellows will receive no additional protected time other than for core faculty.
The 2022 requirements appear to represent an increase in overall protected time for training program leadership but only if the last 3 training years are considered (Table 1). Before July 2019 (since 2007), nephrology program directors were to dedicate 20 h/wk to the program (regardless of size), and key clinical faculty (now designated core faculty) were to dedicate at least 10 hours (5). In July 2019, ACGME required that program directors “must be provided with support adequate for administration of the program,” stipulated as 25%–50% of salary (10–20 h/wk) (2). No specific protected time was required for core faculty other than that they “devote a significant portion of their entire effort to … education and/or administration” (2). The 2022 requirements increase protected time for program leadership in a six-fellow program from a minimum of 10 h/wk up to 24 h/wk, but this is a decrement from the 60 h/wk required before July 2019 (Table 1). Program directors with seven or more fellows are given more protected time on the basis of fellow number, but none would receive 20 h/wk.
ACGME has provided no rationale for these requirements, and the literature regarding protected time in any specialty or subspecialty is sparse. A 2013 survey of pediatric specialty/subspecialty program directors found that those with fewer than seven fellows received on average 0.2 full-time equivalent (FTE; 8 hours) of protected time but that they required 0.25 FTE (10 hours) to adequately perform necessary program administration (6). A 2021 survey of urology program directors found that the majority felt that 0.2 FTE (8 hours) protected time “helped with administrative work,” but 31% felt that more time was required for larger programs (7). The Society of Teachers of Family Medicine recently published guidelines on the basis of family practice program faculty surveys recommending that program directors receive a minimum 0.5 FTE (20 hours) protected nonclinical time for program administration and that core faculty members have 0.3 FTE (12 hours) (8).
Over the past 10 years, the ACGME administrative requirements have increased due to the New Accreditation System, the Milestones Project, and expanded Common Fellowship Program Requirements (9). The time and cost of meeting these requirements have increased; the greatest cost is associated with faculty and program director time for evaluation and education (10).
There is no published information as to how much actual protected time for program administration is made available to nephrology program leadership by their sponsoring institutions, whether ACGME stipulations are being met, and how program director time is distributed. Most importantly, there is no information as to how much protected time program directors believe is needed for effective program administration. Therefore, we surveyed all nephrology program directors in the United States to define the amount of protected time their institutions allow for program administration, how much time they think is necessary, and how they distribute their professional time overall. We hypothesized that some were not receiving the 25%–50% protected time (10–20 h/wk) of salary support stipulated in the 2019 program requirements and that their estimates of time required to effectively administer their programs are greater than stipulated in the 2022 program requirements on the basis of program size.
Materials and Methods
The 20-question anonymous online survey was developed by the authors and reviewed and edited by R.N. (core faculty) and R.R. (a former program director) for format and clarity. After uploading to the survey platform (11), it was tested by three program directors (A.N.S., M.A.W., and B.Y.Y.).
Program directors (n=151) were identified from the ACGME Public List of Nephrology Specialty Programs (12). The survey (Supplemental Material) was administered between March 31 and April 30, 2022. Respondent IP addresses were blocked. Survey links were delivered by email with delivery receipt. Reminders were sent at 1-week intervals. The first question, which was required, asked respondents to confirm program director status. If “no,” they were directed to the end of survey and asked to forward the link to the program director.
All surveys were preceded by explanatory text, allowing potential respondents to exit if they did not wish to participate. Demographic information collected included years in the position (<5, 5–10, >10–20, or >20 years), whether they had been in the position before the 2019–2020 training year, and the geographic location of the program (Northeast, Southern, Midwest, or West census areas). Program site identification was not requested. Although 1 FTE is commonly defined as 40 h/wk, we recognized that institutions may variably define FTE, and program director work hours differ. Therefore, we asked that surveyed program directors report and estimate time in hours per week.
Objectives were as follows:
-
(1)
to determine median hours per week of protected time for nephrology program directors on the basis of program size;
-
(2)
to determine the percentage of program directors not receiving 10 h/wk of protected time and if those with <5 years versus those with ≥5 years of experience are less likely to receive 10 h/wk;
-
(3)
to determine median hours per week of protected time program directors estimate are required to effectively administer their programs (on the basis of program size);
-
(4)
to determine how program directors distribute professional time in addition to program administration;
-
(5)
to identify the three most time-consuming program administration tasks, the three giving the most professional satisfaction, and the three giving the least professional satisfaction;
-
(6)
to determine whether there is a program administrative coordinator (an ACGME requirement) and how many hours per week that person dedicates to the program;
-
(7)
to determine whether there is an associate program director and their median hours per week of protected time; and
-
(8)
to determine median hours per week of protected time for core faculty.
Statistical analyses were descriptive, with percentages, means, SDs, medians, and interquartile ranges (IQRs) used as appropriate. The Fisher exact test was used to compare the percentages of programs meeting the ACGME requirements on the basis of time as program director (<5 versus 5 or more years). Geographic distribution and clinical fellow complement of respondent programs versus programs nationally were compared using the chi-squared test. P<0.05 was considered statistically significant.
The protocol (EDO-2022–0896) was approved by the Walter Reed National Military Medical Center Department of Research Protections as exempt from institutional review board review per 32 CFR 219.104(d)(4)(ii). There was no funding source.
Results
Ninety-nine of 151 nephrology program directors responded to the survey (66% response rate) either partially or completely. The number responding to each question is shown in Supplemental Material. Average question completion rate was 84%. Geographic distribution and approved fellow complement of respondent programs were similar to those of US nephrology programs overall (Table 2).
Table 2.
Summary of program director survey results
| Characteristics of Program and Program Leadership | Survey Result | Reference Information References: 2021–22 and 2022–23 Accreditation Council for Graduate Medical Education Nephrology Program Data and Program Requirements (2,3); National Resident Matching Program 2021 Appointment Year Match Data (4) |
|---|---|---|
| Years as program director, n (%) | n=89 | NA |
| <5 | 40 (45) | NA |
| 5–10 | 28 (31) | NA |
| >10–20 | 17 (19) | NA |
| >20 | 4 (4) | NA |
| Program geographical area (P=0.84; chi-squared test), n (%) | n=89 | 151 US nephrology programsa |
| Northeast | 33 (37) | 52 (34) |
| South | 30 (34) | 52 (34) |
| Midwest | 14 (16) | 28 (19) |
| West | 12 (13) | 19 (13) |
| Approved clinical fellow positions (P=0.07; chi-squared test), n (%) | Median=6 (IQR, 4–8; n=92) | National median=6 (IQR, 4–8; n=151) (4 [NRMP]) |
| 6 or fewer clinical fellows | 54 (59) | 99 (65); 3 positions or fewer offered in 2021 NRMPb |
| 7–9 clinical fellows | 22 (24) | 22 (15); 4 positions offered in 2021 NRMPb |
| 10 or more clinical fellows | 16 (17) | 30 (20); ≥5 positions offered in 2021 NRMPb |
| Program director estimated average hours worked per week | Median=56 (IQR, 50–60; n=88) | NA |
| Program director h/wk protected time for program administration | Median=10 (IQR, 5–10; n=83) | 2021–2022: 10 h/wk required |
| 6 or fewer clinical fellows | 8 (IQR, 5–10) | 2022–2023: 8 h/wk required |
| 7–9 clinical fellows | 9 (IQR, 6–10) | 2022–2023: 10 h/wk required |
| 10 or more clinical fellows | 10 (IQR, 10–15) | 2022–2023: ≥12 h/wk required |
| Estimated h/wk required for effective program administration | Median: 12 (IQR, 10–16; n=88) | NA |
| 6 or fewer clinical fellows | 12 (IQR, 10–15) | NA |
| 7–9 clinical fellows | 10 (IQR, 10–15) | NA |
| 10 or more clinical fellows | 20 (IQR, 16–20) | NA |
| Program coordinator? | 100% yes (n=81) | 2021–2022: Required |
| Hours per week dedicated to the nephrology program | 20 (IQR, 10–20) | 2022–2023: Minimum 20 h/wk for 4- to 6-fellow program |
| Associate program director? | 72% yes (58/81) | 2022–2023: Required |
| Hours per week protected time for program administration for associate program director | 4 (IQR, 1–5) | 2022–2023: Minimum 4 h/wk for 6 or fewer clinical fellows |
| No. of core clinical faculty (not including the associate program director) | 6 (IQR, 4–10, =79) | Minimum: 1 core faculty per 1.5 approved clinical fellows, not including the program director |
| Hours per week per faculty protected time for program administration for core faculty | 2 (IQR, 0–5); 39%=0 h | 2021–2022: No stipulation; 2022–2023: 4 h/wk |
IQR, interquartile range; NRMP, National Resident Matching Program.
The Accreditation Council for Graduate Medical Education Public List of Nephrology Specialty Programs (12).
Total positions estimated by multiplying the number offered in the 2021 National Resident Matching Program by two (2 years of clinical fellowship). This likely underestimates the number of programs having seven (three alternating with four positions offered yearly) or nine positions (four alternating with five positions offered yearly). Numbers are on the basis of the number of nephrology clinical fellowship positions offered for the 2021–2022 training year published in NRMP 2021 Appointment Year Match Data (4).
Overall, program directors received a median of 10 h/wk (IQR, 5–10) of protected time for program administration. Programs of fewer than seven fellows received a median of 8 h/wk (IQR, 5–10). Forty-eight percent received <10 h/wk, not meeting the 2021 ACGME protected time requirement, with 7% reporting 0 hours of protected time.
For those <5 years in their positions (n=36), 61% received ≥10 h/wk of protected time (median, 10; IQR, 7–12). For those with ≥5 years (n=46), 44% had ≥10 hours of protected time (median, 8; IQR, 4–10; P=0.13).
Seventy percent (n=62) had been a program director before July 2019, and of these, 52 (84%) reported that they had not received 20 h/wk of protected time as required. There were 149 nephrology programs in 2018–2019; this represents, at minimum, 37% of programs not in compliance at that time (13).
Program directors estimated requiring a median of 12 h/wk (IQR, 10–16) of protected time to effectively administer their programs (Table 2). Those with fewer than seven fellows estimated needing 12 h/wk (IQR, 10–15), whereas those with ten or more fellows needed 20 h/wk (IQR, 16–20). Overall, program directors (n=82) estimated they needed a median of 5 h/wk (IQR, 0–7) more than received to effectively administer their programs. Seventy-three percent (60 of 82) estimated that they needed more time than provided, 23% (19 of 82) estimated that the time was sufficient, and 4% (three of 82) estimated they could do with less time. Those <5 years in their positions (n=36) estimated needing a median of 4.5 h/wk (IQR, 2–7.25) more than received, whereas those ≥5 years (n=46) in their positions reported needing 4 h/wk (IQR, 0–5).
Figure 1 shows the division of professional time. Although 48% reported <10 h/wk of protected time, 65% reported devoting <10 h/wk to program administration, which includes didactic, nonclinical teaching. One commented that “salary support is there for the program director, however, clinical activity is not changed” (redacted comments) (Supplemental Material). This is suggested by the finding that the majority spend most of their time delivering direct and indirect clinical care. Sixty-nine percent spent at least 10 h/wk directly/indirectly supervising fellow-delivered patient care (clinical teaching). Fifty-two percent spent >20 h/wk personally providing direct and indirect patient care. Program directors devoting <10 h/wk to training program administration reported a median of 8 h/wk (IQR, 4–10) of protected time, and 62% reported providing >20 h/wk of patient care personally. On the other hand, those devoting 10 h/wk or more to program administration had a median of 10 hours (IQR, 10–15) of protected time, and only 32% provided >20 h/wk of patient care personally.
Figure 1.
Division of professional tasks by average hours per week among program directors (PDs; n=82). Time spent on hospital-required administration and training tasks was <8 h/wk for 77% of PDs (63 of 82). Time dedicated to teaching and other program administration (e.g., medical students or medical residents) was <8 h/wk for 78% of PDs. These tasks are not shown. Notably, five PDs (6%) were simultaneously medical directors of dialysis.
Table 3 summarizes the three most time-consuming, the three most professionally rewarding, and the three least professionally rewarding tasks associated with program administration. The most time-consuming tasks were fellow recruitment, didactic teaching, and routine required administrative work. Didactic teaching, despite being time consuming, was considered the most professionally rewarding task, followed by curriculum development and mentorship of fellow projects and research. The least professionally rewarding tasks were routine required administrative work, also considered one of the most time consuming, followed by fellow remediation and Program Evaluation Committee Improvement Plan implementation.
Table 3.
Program administration tasks
| Program Administration Task | Most Time Consuming | Most Professionally Rewarding | Least Professionally Rewarding |
|---|---|---|---|
| Curriculum development | 26 (32)a | 45 (56)a | 2 (2) |
| Didactic teaching | 44 (54)a | 65 (80)a | 0 (0) |
| Attendance at didactic conferences | 16 (20) | 40 (49)a | 6 (7) |
| Developing and scheduling fellow rotations | 21 (26)a | 7 (9) | 22 (27)a |
| Fellow and faculty evaluation/milestone assessment | 10 (12) | 2 (2) | 12 (15) |
| Mentorship of fellow projects and research | 15 (19) | 41 (50)a | 3 (4) |
| Fellow remediation | 8 (10) | 1 (1) | 30 (37)a |
| Fellow recruitment | 55 (68)a | 14 (17) | 23 (28)a |
| Annual fellow orientation and graduation administration | 8 (10) | 16 (20) | 7 (9) |
| Clinical competency committee administration | 10 (12) | 2 (2) | 16 (20) |
| Program evaluation committee and program improvement action plan administration and implementation | 20 (25)a | 4 (5) | 27 (33)a |
| Routine ACGME/GME administrative work, response to data calls, and documentation | 41 (51)a | 0 (0) | 66 (81)a |
Data are presented as n (percentage). ACGME, Accreditation Council for Graduate Medical Education; GME, Graduate Medical Education.
Those chosen by 25% or more of program directors as the three most time consuming, most professionally rewarding, and least professionally rewarding (n=81).
As shown in Table 2, 100% (81 of 81) reported having a program coordinator, as required by the ACGME. Seventy-one percent (57 of 80) had an associate program director (required as of July 2022). Thirty percent of these had two or more associate program directors; the median number of approved fellow positions for these programs was eight (IQR, 6–12). Median protected time for associate program directors was 4 h/wk (IQR, 1–5). Some arranged protected time for their associate program director by donating some of their own. Core clinical faculty (required to have 4 h/wk of protected time beginning in July 2022) had a median of 1.5 h/wk (IQR, 0–5). Thirty-nine percent of responding programs had no protected time available to core clinical faculty. One program director commented, “We ask a lot of them, but they get no time to do it” (Supplemental Material). Another said, “For the last several years, recruitment has been challenging. This has required faculty to pick up the tasks usually assigned to fellows” (Supplemental Material).
Discussion
Our survey indicates that a substantial number of US nephrology program directors were not receiving ACGME-required institutional support for protected time for program administration in training year 2021–2022. This situation was present before the coronavirus disease 2019 pandemic. Before July 2019, when required protected time was reduced from 20 to 10–20 h/wk, at least one third of program directors did not receive 20 h/wk. At the time of the survey (April 2022), approximately half were not receiving 10 h/wk, and about half of programs with fewer than seven fellows would not be in compliance with the 8 h/wk requirement that went into effect in July 2022. Some reported they were given 10 h/wk officially, but scheduled direct patient care and other administrative duties (e.g., dialysis unit directorships and supervision of advanced practice providers) made time for program administration aspirational, unless done on one’s own time and despite working a median of 56 h/wk.
The respondents estimated that minimum protected time should increase to a median of 12 h/wk in order to effectively meet program administration time needs, even in smaller programs of fewer than seven fellows, rather than decrease to 8 h/wk. Program directors with ten or more fellows estimated needing a median of 20 h/wk. No contradictory data are available in the literature indicating that a median of 12 h/wk of protected time (with 20 h/wk for larger programs) is an overestimate of program director needs. As ACGME defines them, the duties are considerable: “The program director must have responsibility, authority, and accountability for: administration and operations; teaching and scholarly activity; fellow recruitment and selection, evaluation, and promotion of fellows, and disciplinary action; supervision of fellows; and fellow education in the context of patient care” (2).
Decreasing time allotted for program administration may make the position vulnerable to being viewed as an ancillary duty, and at some institutions may already be (comments in Supplemental Material). Some institutions may not factor program directorship into academic promotion decisions. For some, time for program administration (which includes curriculum development and didactic teaching) is undertaken in addition to a demanding personal and supervisory clinical load, further extending the work week and affecting work-life balance. Sponsoring institutions and division chiefs may have conflicts in ensuring that clinical work hours are maximized and that ACGME stipulations are met.
As the majority of nephrology program directors experience a reduction in protected time, another difficulty will be securing protected time for core faculty to help shoulder the burden of program administration and education. Almost 40% of core faculty members now receive no protected time. Some programs may struggle to secure the mandated 4 h/wk from their sponsoring institutions, and ACGME has recently paused implementation of this requirement (14,15). It is unclear how core faculty given no protected time are able to “devote a significant portion of their entire effort to fellow education and/or administration, and must, as a component of their activities, teach, evaluate, and provide formative feedback to fellows” (2).
For nephrology, the erosion of protected time has occurred in a setting of declining board pass rates (74%–80% over the last 3 years) (16). This has been attributed to poor fellow preparation and associated with international medical school graduate status, smaller program size, and lower Internal Medicine-certifying examination scores among fellows entering training (17). ACGME and the nephrology training community should consider the possibility that another contributor to poor board performance may be a lack of sufficient time for curriculum development and didactic teaching by program directors and core faculty. This might be the focus of future research. Although program directors have expressed the highest satisfaction in developing curriculum, participating in and delivering didactic teaching, and mentoring fellows in scholarly work, they may have little time for these pursuits. Despite what ACGME has championed, as protected time for didactics and curriculum innovation declines and routine administration and data submission burdens increase, the majority of time with fellows may be spent in bedside clinical teaching.
Our survey had an excellent response rate (66%) and was verified as delivered to all US nephrology program directors. Respondents were not significantly different in terms of geographic distribution and program size to national nephrology programs. To internally validate responses, we asked program directors to indicate the amount of protected time they received and later estimate how many hours per week they dedicated to program administration. The survey was conducted in April when program leadership begins work on graduation tasks and planning for the new training year but not during the intense work of the recruitment/matching period and during the turnover of the training year. Limitations include that respondents had to estimate the time spent in multiple tasks, and average to weekly effort. Many tasks associated with program administration take up blocks of time depending on training cycle stage (e.g., preparing for the academic year, recruiting and interviewing, and didactic curriculum development) or cannot be routinely anticipated (e.g., remediation and new curriculum or evaluation requirements from ACGME). We did not inquire about the number of filled versus approved fellow positions, which would have provided information regarding protected time needs in underfilled programs. There was no external validation of time estimates, which would require an external or personal timekeeping process over the course of a training year and might be a focus for future research.
In conclusion, our survey demonstrated that one third to one half of US nephrology programs were not in compliance with the ACGME-stipulated 10-h/wk minimum protected time for program directors. Although no public data are available, this may also be the situation for other internal medicine subspecialties. It is unclear what the effect of the new standardized protected time requirements will be nationally or if there will be unintended consequences. Many training institutions will likely provide no more than the minimum protected time required. As we demonstrate, many do not provide the minimum. The majority of nephrology program directors estimate that at least 12 h/wk are needed to effectively educate fellows and manage their programs, and it is not unreasonable to suppose that this is also true for other subspecialties. In view of this survey, ACGME should prospectively track compliance with the requirements and effects on fellow education and board performance. Consideration should be given to collecting objective data on the time necessary to effectively complete the tasks associated with program administration followed by reassessment of the 2019 and 2022 decreases in protected time, as they do not align with program director–reported needs for education and administration. ACGME should undertake similar efforts for all medicine subspecialties.
Disclosures
M.A. Watson reports employment with the US Army. B.Y. Young reports other interests or relationships as the Medical Director of Satellite Wellbound University Home Dialysis Clinic. C.M. Yuan reports employment with Walter Reed National Military Medical Center and other interests or relationships as an administrator and member of the Nephrology Education Research and Development Consortium (https://nerdc.org). The remaining author has nothing to disclose.
Funding
None.
Supplementary Material
Acknowledgments
We thank Drs. Rajeev Raghavan and Robert Nee for their assistance in development of the survey.
The views expressed are those of the authors and do not necessarily reflect the official policy of the Department of Defense or the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
Author Contributions
C.M. Yuan conceptualized the study; C.M. Yuan was responsible for data curation; A.N. Sussman, M.A. Watson, B.Y. Young, and C.M. Yuan were responsible for investigation; C.M. Yuan was responsible for formal analysis; A.N. Sussman, M.A. Watson, B.Y. Young, and C.M. Yuan were responsible for methodology; C.M. Yuan was responsible for project administration; C.M. Yuan was responsible for resources; A.N. Sussman, M.A. Watson, and B.Y. Young were responsible for validation; C.M. Yuan wrote the original draft; and A.N. Sussman, M.A. Watson, and B.Y. Young reviewed and edited the manuscript.
Data Sharing Statement
All data used in this study are available in this article.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.09050822/-/DCSupplemental.
Supplemental Material. Program director survey, the number of survey respondents answering each survey question, and survey comments.
References
- 1.Accreditation Council for Graduate Medical Education : Internal Medicine Program Requirements and FAQs, 2022. Available at: https://www.acgme.org/specialties/internal-medicine/program-requirements-and-faqs-and-applications/. Accessed May 25, 2022
- 2.Accreditation Council for Graduate Medical Education : ACGME Program Requirements for Graduate Medical Education in Nephrology. Focused Revision Approved June 13, 2021, Effective July 1, 2021, 2021. Available at: https://www.acgme.org/globalassets/pfassets/programrequirements/148_nephrology_2021.pdf. Accessed September 22, 2022
- 3.Accreditation Council for Graduate Medical Education : ACGME Program Requirements for Graduate Medical Education in Nephrology (Approved February 7, 2022, Effective July 1, 2022), 2022. Available at: https://www.acgme.org/specialties/internal-medicine/program-requirements-and-faqs-and-applications/. Accessed March 6, 2022
- 4.National Resident Matching Program : Results and Data: 2021 Main Residency Match, Washington, DC, National Resident Matching Program, 2021 [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education : ACGME Program Requirements for Graduate Medical Education in Nephrology (Editorial Revision: Effective July 1, 2019, Copyright, 2019 Accreditation Council for Graduate Medical Education (ACGME).
- 6.Fleming GM, Brook MM, Herman BE, Kennedy C, McGann KA, Mason KE, Weiss P, Myers AL: Recommended protected time for pediatric fellowship program directors: A needs assessment survey. Acad Pediatr 16: 415–418, 2016 [DOI] [PubMed] [Google Scholar]
- 7.Cannon S, Sorensen MD, Joyner B: Program directors’ perspective s of ACGME requirements and effectiveness for training urology residents: A national survey in the era of the next accreditation system. Urology 149: 46–51, 2021 [DOI] [PubMed] [Google Scholar]
- 8.Griesbach S, Theobald M, Kolman K, Stutzman K, Holder S, Roett MA, Friend L, Dregansky GV, Frazier W, Lewis GR: Joint guidelines for protected nonclinical time for faculty in family medicine residency programs. Fam Med 53: 443–452, 2021 [DOI] [PubMed] [Google Scholar]
- 9.Edgar L, McLean S, Hogan SO, Hamstra S, Holmboe ES: The Milestones Guidebook (Version 2020), 2020. Available at: https://www.acgme.org/globalassets/MilestonesGuidebook.pdf. Accessed March 5, 2022
- 10.Kempenich JW, Willis RE, Campi HD, Schenarts PJ: The cost of compliance: The financial burden of fulfilling Accreditation Council for Graduate Medical Education and American Board of Surgery requirements. J Surg Educ 75: 47–53, 2018 [DOI] [PubMed] [Google Scholar]
- 11.SurveyMonkey : SurveyMonkey, Momentive, 2022. Available at: https://www.surveymonkey.com/. Accessed 3 November 2022
- 12.Accreditation Council for Graduate Medical Education : Accreditation Council for Graduate Medical Education Public List of Nephrology Specialty Programs. Available at: https://apps.acgme.org/ads/Public/Reports/Report/1. Accessed November 3,2022
- 13.Accreditation Council for Graduate Medical Education : Accreditation Council for Graduate Medical Education Public List of Nephrology Specialty Programs, Academic Year 2018–2019, Copyright, 2019 Accreditation Council for Graduate Medical Education
- 14.Accreditation Council for Graduate Medical Education : Letter from Alliance for Academic Internal Medicine (AAIM) President to Chief Accreditation Officer, September 8, 2022. Available at: https://higherlogicdownload.s3.amazonaws.com/IM/fecab58a-0e31-416b-8e56-46fc9eda5c37/UploadedImages/Documents/advocacy/09-08-2022_AAIM_Letter_to_ACGME_on_Concerns_about_Core_Faculty_Reqs.pdf. Accessed September 25, 2022
- 15.Accreditation Council for Graduate Medical Education : Specialty-specific program requirements: Core faculty dedicated time. Core Faculty Dedicated Time by Specialty Updated 06/2022, 2022. Available at: https://www.acgme.org/globalassets/pdfs/specialty-specific-requirement-topics/dio-dedicated_time_core_faculty_2022.pdf. Accessed September 29, 2022
- 16.American Board of Internal Medicine : Initial Certification Pass Rates: Internal Medicine and Subspecialty Certification Examinations: 2017–2021. Available at: https://www.abim.org/Media/yeqiumdc/certification-pass-rates.pdf. Accessed May 22, 2022
- 17.Berns JS, Weng W, Jaar BG, Lipner RS, Brossman BG, McDonald FS: Analysis of performance trends from 2010–2019 on the American Board of Internal Medicine nephrology certifying exam. J Am Soc Nephrol 32: 2714–2723, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.