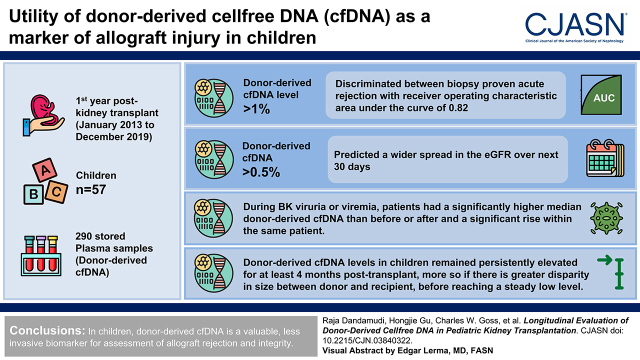
Visual Abstract
Keywords: pediatric kidney transplantation, rejection, BK, donor-derived cell free DNA
Abstract
Background and objectives
Donor-derived cellfree DNA (cfDNA) is a less-invasive marker of allograft injury compared with kidney biopsy. However, donor-derived cfDNA has not yet been extensively tested in children, where the test may have different characteristics.
Design, setting, participants, & measurements
We assayed donor-derived cfDNA (AlloSure; CareDx) from 290 stored plasma samples from a prospective biobank at our center, collected from 57 children monthly in the first year postkidney transplant between January 2013 and December 2019. We assessed the kinetic changes in donor-derived cfDNA levels within the first year post-transplant. We analyzed donor-derived cfDNA levels for associations with biopsy-proven acute rejection using area under the receiver operating characteristic curve to longitudinal plasma and urine BK viral loads using linear mixed models. We analyzed the prognostic effect of an elevated donor-derived cfDNA level on the eGFR 30 days after the assay via Kolmogorov–Smirnov two-sample tests or on measured GFR or interstitial fibrosis at 12 months post-transplant.
Results
The donor-derived cfDNA levels in children remained persistently elevated for at least 4 months post-transplant, more so if there is greater disparity in size between the donor and the recipient, before reaching a steady low level. A donor-derived cfDNA level of >1% discriminated between biopsy-proven acute rejection with a receiver operating characteristic area under the curve of 0.82 (95% confidence interval, 0.71 to 0.93). During BK viruria or viremia, patients had a significantly higher median donor-derived cfDNA than before or after and a significant rise within the same patient. A donor-derived cfDNA of >0.5% predicted a wider spread in the eGFR over the next 30 days but not the 12-month outcomes.
Conclusions
In children, donor-derived cfDNA is a valuable, less invasive biomarker for assessment of allograft rejection and injury.
Podcast
This article contains a podcast at https://www.asn-online.org/media/podcast/CJASN/2022_10_27_CJN03840322.mp3.
Introduction
The principal aims of pediatric kidney transplantation are to avoid dialysis and improve the growth and quality of life of children (1,2). Continuous monitoring of allografts is a part of post-transplant management to ensure that allograft function remains stable.
Serum creatinine, the most common endogenous marker for kidney allograft function, is affected by multiple characteristics, such as age, sex, muscle mass, and nutritional status (3–5). Post-transplant kidney allografts are susceptible to multiple types of injuries, including acute rejection, opportunistic infection, disease recurrence, and immunosuppression-induced toxicity. Serum creatinine is a lagging indicator of kidney injury (6), such that by the time serum creatinine levels increase, the allograft may have undergone severe and irreversible damage (7,8). A less-invasive and sensitive diagnostic marker that precedes a rise in serum creatinine may provide an opportunity for better-informed therapeutic decision making.
Circulating cellfree DNA (cfDNA) originates from cellular secretion or apoptosis (9,10). Donor-derived cfDNA arises from apoptosis or necrosis of foreign allograft tissue. Both are measurable in the body fluids of patients after organ transplantation (e.g., in blood and urine) (11). Differentiating donor-derived cfDNA from recipient cfDNA is an emerging tool for the early and sensitive detection of allograft injury. Most commonly, donor-derived cfDNA is expressed as a percentage of the total cfDNA fragments. Previous adult studies demonstrated that levels above 1% associate with allograft injury from biopsy-proven acute rejection (12–16) or from BK virus nephropathy (17). Serially monitoring donor-derived cfDNA as a dynamic marker allows for the assessment of trends and early injury identification. More than one value of donor-derived cfDNA >0.5% in year 1 associated with a >25% decrease in a patient’s eGFR over 3 years (14).
In children, however, the size disparity between the allograft and recipient, a lower background DNA due to the smaller body mass in children, or the higher frequency of primary viral infection after transplantation all can alter the percentage of donor-derived cfDNA. For these reasons, applying adult standards may be misleading in pediatric patients. To date, there are very limited data defining the usefulness of donor-derived cfDNA in pediatric patients with kidney transplants (18).
The aim of our study was to comprehensively determine longitudinally assayed donor-derived cfDNA levels in pediatric recipients at the time of different allograft injuries (BK virus infection and rejection), to understand the kinetics postkidney transplant in stable children, and to assess the prognostic relationship between the donor-derived cfDNA and later kidney function.
Materials and Methods
Patients and Samples
At our center, we initiated from January 2013 onward a prospective biobank of monthly plasma, serum, and urine sample collection for the first 12 months post-transplant. Participants provided informed consent under a protocol approved by the Washington University Institutional Review Board (201210079). The clinical and research activities being reported are consistent with the Principles of the Declaration of Istanbul as outlined in the Declaration of Istanbul on Organ Trafficking and Transplant Tourism.
In addition to regular clinic visits and standard laboratory testing, our pediatric kidney transplant program also performs the following monitoring as standard of care: (1) surveillance biopsies at 3, 6, and 12 months post-transplant; (2) quantitative monthly nucleic acid testing by PCR assay for Epstein–Barr virus, cytomegalovirus (plasma), and BK virus (urine monthly; plasma added if urine turns positive) in months 1–12 post-transplant; and (3) measured iothalamate clearance GFR at 12 months post-transplant.
Methods for biobanking samples; measuring creatinine, eGFR, measured GFR, and tissue interstitial fibrosis; and statistical analytic methods are provided in Supplemental Material. GFR was estimated using the creatinine-based CKD in children GFR equation using participant height (centimeters) and serum creatinine (19). The percentage change in eGFR was calculated as (last eGFR − prior eGFR)/(prior eGFR) ×100%.
BK virus viral loads in urine and plasma samples were determined by quantitative PCR. Assays were performed at Mayo Clinic Laboratories (Rochester, MN) using a Cobas 6800 system (Roche Molecular Systems Inc., USA), and the quantification range for this assay was 200–100,000,000 IU/ml. Probes were designed to specifically detect the BK virus and did not crossreact with sequences present in the related JC or SV-40 polyomavirus.
Clinical data related to peritransplant characteristics and outcomes were collected in a secure Redcap database housed at Washington University.
Donor-Derived Cellfree DNA Assay
Plasma samples from our biobank were analyzed by CareDx, Inc. for donor-derived cfDNA levels at a Central Clinical Laboratories Improvements Act–certified laboratory. The donor-derived cfDNA assay of CareDx utilizes targeted next-generation sequencing amplification of DNA regions harboring 405 single nucleotide polymorphisms and the measurement by next-generation sequencing of each allele frequency at each single nucleotide polymorphism position as previously described (20,21). This method does not need separate genotyping of the recipient or the donor. The percentage of donor-derived cfDNA was determined by multiplying the mean donor allele frequency with a multiplier on the basis of the level of family-reported relatedness between a donor and recipient (20,21).
Results
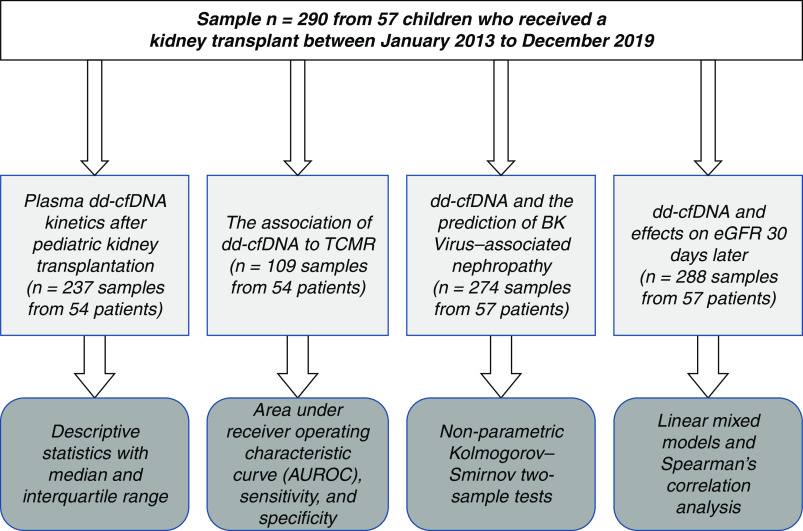
For the studies detailed below, a total of 290 plasma samples were available from an overall population of 57 unique children who received a kidney transplant between January 2013 and December 2019. The median age at the time of transplant was 14 years (interquartile range [IQR], 7.4–16 years), with a boy-girl ratio of 32:25. The median samples per participant were five (range, 1–11). Demographics of the overall cohort and the subgroup analyses are shown in Table 1. For each analysis, the demographic characteristics of the participants involved and the statistical tests used are summarized in Figure 1.
Table 1.
Demographics of overall cohort and for each subgroup analysis
| Variables | Overall Cohort Patient, n=57 | Kinetics Study, n=54 | T Cell–Mediated Rejection Study, n=54 | BK Virus Study, n=57 | 30-d Later eGFR Study, n=57 |
|---|---|---|---|---|---|
| Recipient sex, n (%) | |||||
| Boys | 32 (56) | 29 (54) | 29 (54) | 32 (56) | 32 (56) |
| Girls | 25 (44) | 25 (46) | 25 (46) | 25 (44) | 25 (44) |
| Recipient age, yr | |||||
| Median (25–75 percentile) | 14 (7.5–16) | 14 (7.5–16) | 14 (7.5–16) | 14 (7.5–16) | 14 (7.5–16) |
| Recipient BSA | |||||
| Median (25–75 percentile) | 0.86 (0.5–1.4) | 0.86 (0.5–1.4) | 0.86 (0.5–1.4) | 0.86 (0.5–1.4) | 0.86 (0.5–1.4) |
| Race, n (%) | |||||
| White | 45 (79) | 43 (80) | 43 (80) | 45 (79) | 45 (79) |
| Black | 9 (16) | 8 (15) | 8 (15) | 9 (16) | 9 (16) |
| Other | 3 (5) | 3 (5) | 3 (5) | 3 (5) | 3 (5) |
| Donor source, n (%) | |||||
| Deceased | 42 (74) | 39 (72) | 39 (72) | 42 (74) | 42 (74) |
| Living | 15 (26) | 15 (28) | 15 (28) | 15 (26) | 15 (26) |
| Prior transplant, n (%) | |||||
| Yes | 1 (2) | 1 (2) | 1 (2) | 1 (2) | 1 (2) |
| Primary kidney disease, n (%) | |||||
| Glomerular disease | 23 (40) | 22 (41) | 22 (41) | 23 (40) | 23 (40) |
| Nonglomerular disease | 30 (53) | 28 (52) | 28 (52) | 30 (53) | 30 (53) |
| Unknown | 4 (7) | 4 (7) | 4 (7) | 4 (7) | 4 (7) |
| Donor age, yr | |||||
| Median (25–75 percentile) | 27 (20–34) | 27 (20–34) | 27 (20–34) | 27 (20–34) | 27 (20–34) |
| Donor sex, n (%) | |||||
| Boys | 33 (58) | 30 (56) | 30 (56) | 33 (58) | 33 (58) |
| Girl | 24 (42) | 24 (44) | 24 (44) | 24 (42) | 24 (42) |
| Donor BSA | |||||
| Median (25–75 percentile) | 1.1 (0.78–1.6) | 1.1 (0.78–1.6) | 1.1 (0.78–1.6) | 1.1 (0.78–1.6) | 1.1 (0.78–1.6) |
BSA, body surface area.
Figure 1.
Flow diagram showing the total dataset and the datasets used to perform each of the separate analyses in the study, with the statistical tests used. dd-cfDNA, donor-derived cellfree DNA; TCMR; T cell–mediated rejection.
Plasma Donor-Derived Cellfree DNA Longitudinal Kinetics in the First Year in Stable Pediatric Kidney Transplant Recipients
To study the donor-derived cfDNA kinetics over time in children, we identified a subgroup of 237 samples from 54 unique children that were not associated with any major infectious events, biopsy-proven acute rejection, or delayed graft function. In this cohort, the median (IQR) plasma percentage of donor-derived cfDNA at 30 days postkidney transplant was 0.65% (IQR, 0.32%–0.91%), decreasing to 0.35% (IQR, 0.22%–0.57%) by month 2 to a median of 0.17% (IQR, 0.08%–0.46%) by month 6 and to a median of 0.16% (IQR, 0.12%–1.28%) by month 12 post-transplant (Figure 2).
Figure 2.
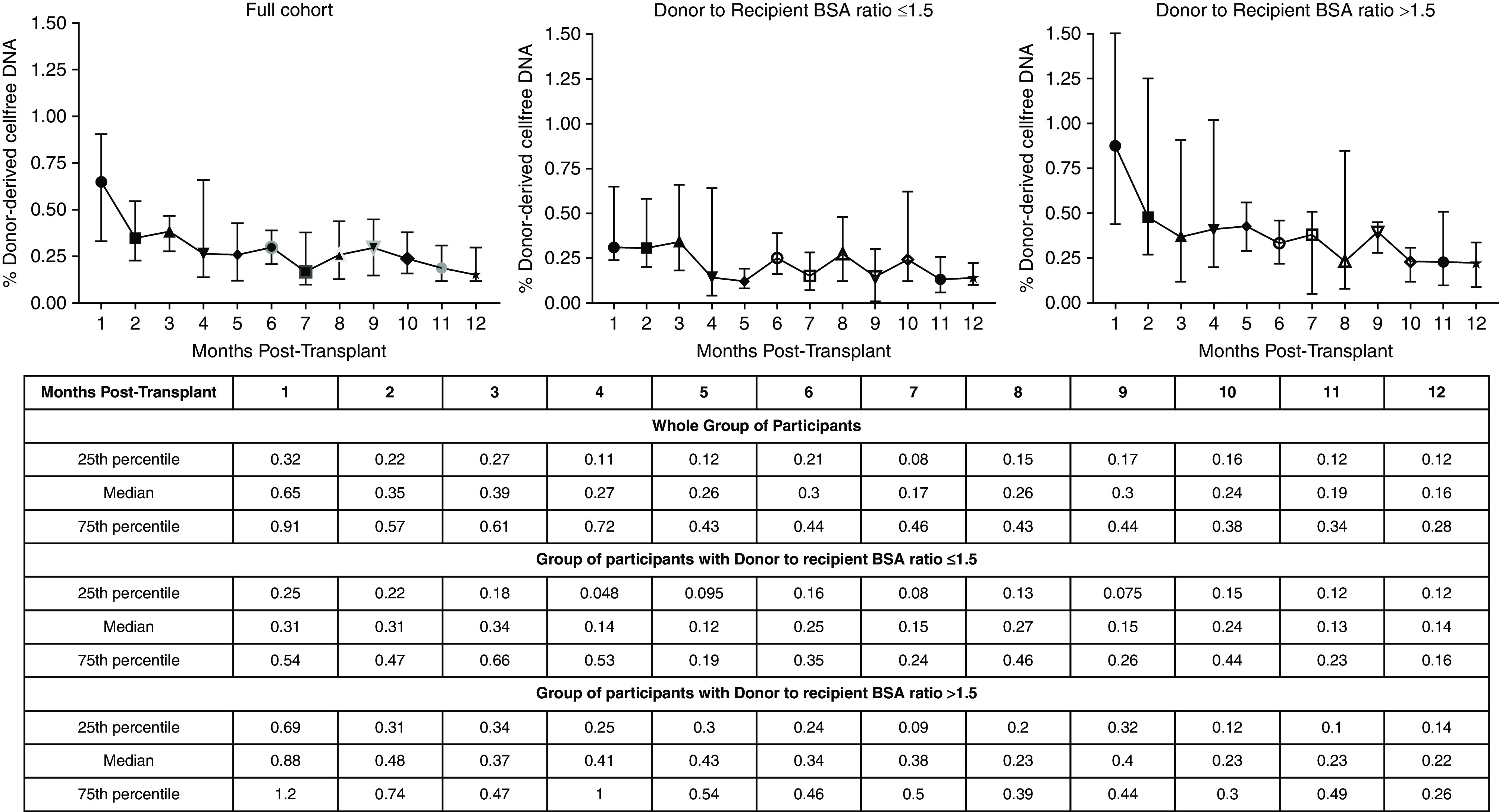
Donor-derived cfDNA kinetics during the first year after kidney transplant demostrating persistent elevation at least until 4 months post-transplant. The lines represent medians with interquartile ranges. BSA, body surface area.
Using the donor-recipient body surface area ratio as an indicator for size mismatch between the donor and the recipient, we stratified the participants into two groups (donor-recipient body surface area ratio <1.5 versus donor-recipient body surface area ratio >1.5). In comparison with the donor-recipient body surface area ratio <1.5 group (120 samples), the donor-recipient body surface area ratio >1.5 group (117 samples) had a higher mean percentage of donor-derived cfDNA through the entire first year post-transplant. In the donor-recipient body surface area ratio >1.5 group, the median percentage of donor-derived cfDNA did not reach <0.3% until 8 months post-transplant, whereas in the donor-recipient body surface area ratio <1.5 group, the mean percentage of donor-derived cfDNA reached <0.3% by 4 months post-transplant. We noted that the donor-derived cfDNA level fluctuated even after reaching a low level.
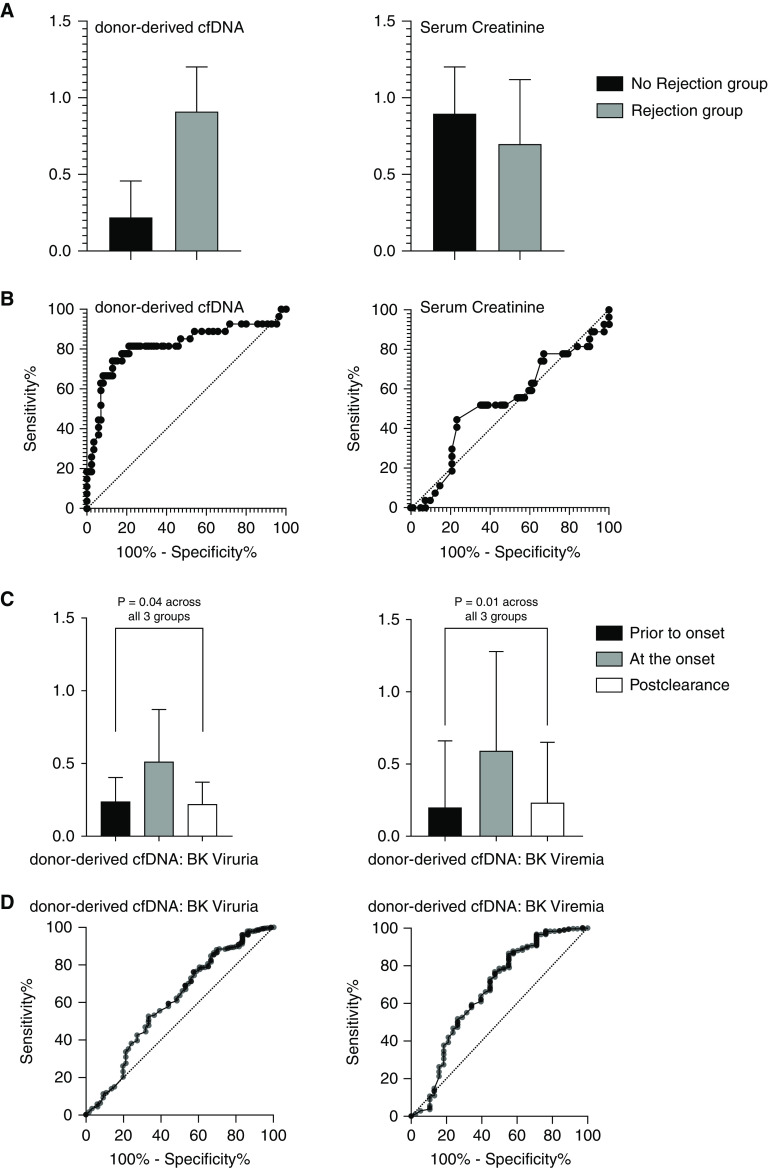
The Association of Donor-Derived Cellfree DNA with Acute T Cell–Mediated Rejection
For these analyses, we studied 109 samples of plasma donor-derived cfDNA levels drawn on the same morning prior to kidney biopsies within the first year post-transplant from 54 unique patients. Of 109 biopsies, 92 (84%) were surveillance biopsies, whereas 17 (16%) were performed for clinical suspicion of rejection. All other pathologies were excluded, and we had no antibody-mediated rejection events in our cohort before month 12. Treating each sample as independent, we analyzed the 109 plasma samples with concurrent biopsies and donor-derived cfDNA levels as two groups (no evidence of T cell–mediated rejection versus any T cell–mediated rejection, including subclinical rejection). We defined subclinical rejection as the presence of histologic features of acute rejection on kidney biopsy in the absence of a decline in kidney function (defined as a <10% rise in serum creatinine within the 2 weeks before the protocol biopsy) as used by other investigators (22–24). We had 27 biopsy specimens from 22 patients with biopsy-proven acute rejection and 82 biopsy specimens from 45 patients without biopsy-proven acute rejection. At biopsy-proven acute rejection, the donor-derived cfDNA median (IQR) level was significantly higher at 0.91% (IQR, 0.54%–1.2%) than the nonbiopsy-proven acute rejection group (median, 0.22%; IQR, 0.14%–0.45%; P<0.001 by the Mann–Whitney U test). The area under the receiver operating characteristic curve (AUROC) value was 0.82 (95% confidence interval [95% CI], 0.71 to 0.93).
At a 1% cutoff, donor-derived cfDNA had a high 96% specificity (95% CI, 90% to 99%) but low 33% sensitivity (95% CI, 19% to 52%) to discriminate biopsy-proven acute rejection from no rejection. At the lower cutoff of 0.5%, donor-derived cfDNA had a lower 79% specificity (95% CI, 69% to 87%) but higher 78% sensitivity (95% CI, 59% to 89%) to discriminate biopsy-proven acute rejection from no rejection (Figure 3, A and B, Table 2).
Figure 3.
High performance of donor-derived cfDNA in T cell mediated–rejection and BK viremia and viruria. The bar graphs in (A) show the median (interquartile range) of the percentage fraction of dd-cfDNA or serum creatinine in T cell–mediated rejection versus no T cell–mediated rejection. (B) The area under the receiver operating characteristic curve for dd-cfDNA and creatinine to discriminate acute T cell–mediated rejection. (C) The bar graphs depict the percentage of dd-cfDNA levels prior to onset, during, and postresolution of BK viruria and BK viremia. Lines represent medians with interquartile ranges. (D) The area under the receiver operating characteristic curve for dd-cfDNA for the detection of BK viruria and BK viremia.
Table 2.
Diagnostic accuracy of donor-derived cellfree DNA levels for detecting biopsy-proven acute rejection
| Cutoff of Donor-Derived Cellfree DNA, % | Specificity | Sensitivity |
|---|---|---|
| 1.0 | 96.5 (95% CI, 90.1 to 99.04) | 33.3 (95% CI, 18.6 to 52.2) |
| 0.5 | 78.8 (95% CI, 69 to 86.2) | 77.8 (95% CI, 59.2 to 89.4) |
Plotted sensitivity versus (1 − specificity) over the range of possible cut points, and the area under this receiver operating curve is C=0.82. 95% CI, 95% confidence interval.
Serum creatinine at the time of the biopsy did not discriminate biopsy-proven acute rejection from no rejection. At biopsy-proven acute rejection, the median (IQR) level of creatinine was 0.70 mg/dl (IQR, 0.53–1.1), not statistically different from the nonbiopsy-proven acute rejection group (median, 0.90 mg/dl; IQR, 0.70–1.20; P=0.63). The AUROC value was 0.53 (95% CI, 0.40 to 0.66).
Donor-Derived Cellfree DNA and the Prediction of BK Virus–Associated Nephropathy
For these analyses, we studied 274 simultaneously drawn plasma donor-derived cfDNA levels, plasma BK virus levels, and urinary BK virus levels within the first year post-transplant drawn from 57 independent patients. Of the 274 samples, 71 (26%) urinary samples and 42 (15%) plasma samples were positive for BK virus DNA, representing 11 unique patients. Patients with any BK viruria (median, 1,505,000 copies per milliliter) had a higher median donor-derived cfDNA of 0.34% (IQR, 0.15%–0.75%) when compared with patients with no BK viruria (0.27; IQR, 0.14%–0.48%). Patients with any BK viremia (median, 10,000 copies per milliliter) had a higher median donor-derived cfDNA of 0.49% (IQR, 0.20%–1.28%) when compared with patients with no BK viremia (0.28; IQR, 0.14%–0.48%). Figure 3C depicts the donor-derived cfDNA results prior to onset, at onset, and after clearance of the viremia and viruria. A clear rise in donor-derived cfDNA is noted at the onset of viruria and viremia, with a drop in donor-derived cfDNA levels after the resolution of viruria or viremia (the P value for viruria was 0.04 and the P value for viremia was 0.01 by the Kruskal–Wallis test). We found a significant positive correlation coefficient of 0.21 (P≤0.001) between the percentage of donor-derived cfDNA and BK plasma viral load. Also, we observed a significant positive correlation coefficient of 0.17 (P=0.004) between the percentage of donor-derived cfDNA and BK urine viral load.
By longitudinal analysis that accounted for within-individual variability, a significant rise of 0.88% in donor-derived cfDNA levels was seen during the duration of BK viremia (P≤0.001). A lower but also significant rise of 0.49% in donor-derived cfDNA levels was seen during the duration of BK viruria (P=0.003). Notably, we did not see any significant rise in donor-derived cfDNA levels at the time of systemic viremia, which typically does not infect the allograft (Epstein–Barr or cytomegalovirus). The AUROC to detect BK viruria was 0.60 (95% CI, 0.52 to 0.69), and the AUROC to detect BK viremia was 0.67 (95% CI, 0.56 to 0.77).
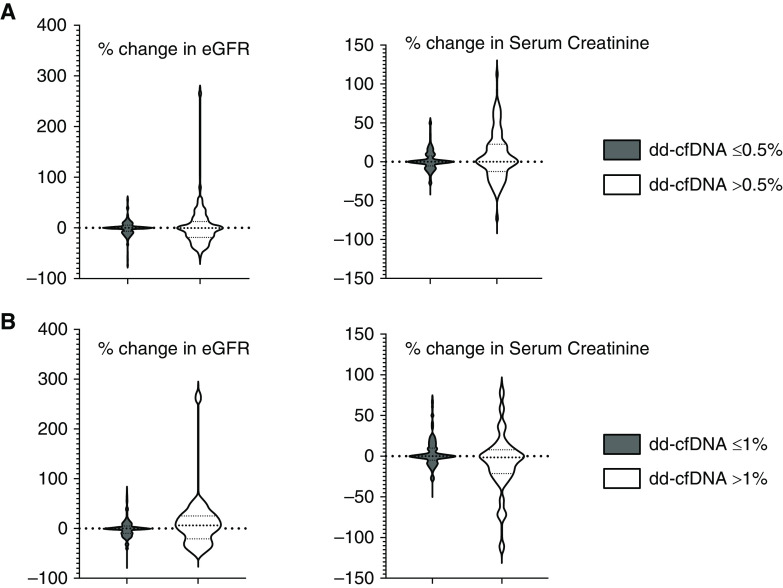
Donor Cellfree DNA and Effects on Estimated Glomerular Filtration Rate 30 Days Later
For these analyses, at a cutoff of 0.5% donor-derived cfDNA, we included 197 eGFR data points with >0.5% donor-derived cfDNA and 91 with ≤0.5% donor-derived cfDNA drawn from 57 unique patients. The ≤0.5% donor-derived cfDNA group showed a low spread of change in eGFR (median, 0%; IQR, −8% to 5%). In contrast, the >0.5% donor-derived cfDNA group showed a significantly greater spread of change in eGFR (median, 0%; IQR, −19% to 13%), even with nearly identical measures of central tendency (Figure 4) (the Kolmogorov–Smirnov two‐sample test; P=0.002). Similar changes in serum creatinine and eGFR spread were also observed when the donor-derived cfDNA cutoff level was 1% (Figure 4, Tables 3 and 4).
Figure 4.
An elevated donor-derived cfDNA level predicts a wider spread in the estimated glomerular filtration rate (eGFR) over the next 30 days, implying that a greater proportion had a bigger eGFR decline. (A) Cumulative distribution functions of the percentage change in eGFR and serum creatinine 30 days after the percentage of dd-cfDNA test when the level is >0.5%. (B) Cumulative distribution functions of the percentage change in eGFR and serum creatinine 30 days after the percentage of dd-cfDNA test when the level is 1%.
Table 3.
Median (interquartile range) spread of allograft kidney function parameters stratified by the low donor-derived cellfree DNA group using a cutoff of 0.5%
| Characteristics | Low Donor-Derived Cellfree DNA (<0.5%), n=197 | High Donor-Derived Cellfree DNA (>0.5%), n=91 |
|---|---|---|
| Donor-derived cfDNA | 0.21 (0.12–0.32) | 0.89 (0.62–1.2) |
| Serum creatinine, mg/dl | 0.9 (0.68–1.2) | 0.8 (0.52–1.2) |
| Percentage change in serum creatinine | 0.0 (−5.0 to 7.7) | 0.0 (−13 to 22) |
| eGFR, ml/min per 1.73 m2 | 68 (57–87) | 68 (54–85) |
| Percentage change in eGFR | 0.0 (−7.6 to 5.1) | 0.0 (−19 to 13) |
cfDNA, cellfree DNA.
Table 4.
Median (interquartile range) spread of allograft kidney function parameters stratified by the high donor-derived cellfree DNA group using a cutoff of 1%
| Characteristics | Low Donor-Derived Cellfree DNA (<1%), n=249 | High Donor-Derived Cellfree DNA (>1%), n=39 |
|---|---|---|
| Donor-derived cfDNA | 0.28 (0.15–0.47) | 1.6 (1.2–2.5) |
| Serum creatinine, mg/dl | 0.9 (0.6–1.2) | 0.9 (0.7–1.6) |
| Percentage change in serum creatinine | 0.0 (−4.5 to 10) | −1.3 (−2.1 to 7.7) |
| eGFR, ml/min per 1.73 m2 | 68 (57–87) | 62 (44–76) |
| Percentage change in eGFR | 0.0 (−9.1 to 5.3) | 6.7 (−20 to 25) |
cfDNA, cellfree DNA.
Lack of Association of Donor-Derived Cellfree DNA with Post-Transplant Month 12 Measured Glomerular Filtration Rate and Surveillance Biopsy Interstitial Fibrosis Amount in Pediatric Kidney Transplantation
For these analyses, 49 patients had available surveillance biopsies and 46 had measured iothalamate clearance GFR results at 12 months. We did not observe any significant difference in measured GFR values between the participants who had an elevated donor-derived cfDNA (>1%) level at any one time (mean ± SD: 80.9±37.3 versus 84.2±28 in those whose donor-derived cfDNA always remained <1%; P=0.76). Similarly, we did not see a significant difference in donor-derived cfDNA levels (mean ± SD) between those with mild interstitial fibrosis on the 12-month surveillance biopsy (n=36; donor-derived cfDNA 0.41%±0.33%) versus those with moderate or severe fibrosis (n=7; donor-derived cfDNA 0.21%±0.10%; P=0.18).
Discussion
We used our biobanked samples over several years and the associated clinical follow-up outcomes to comprehensively analyze for the first time in children several relationships between the allograft integrity and donor-derived cfDNA: (1) longitudinally kinetics; (2) specific donor-derived cfDNA levels with different allograft injuries; and (3) prognostic associations.
In adults, Gielis et al. (25) evaluated donor-derived cfDNA early kinetics in 42 kidney transplant recipients and showed that median donor-derived cfDNA fractions on the first day after kidney transplant were elevated at 10% (range, 3%–42%). Thereafter, fractions of donor-derived cfDNA decreased to a mean (SD) value of 0.46% (0.21%) that was reached on average 9.85±5.6 days after transplantation. In months 1–12, Bromberg et al. (8) established a median plasma donor-derived cfDNA of 0.21% (IQR, 0.12–0.39) or mean of 0.34% (SD ± 0.58%) in stable post-transplant adults.
In our pediatric cohort, the time required for initial stabilization post-transplant was significantly longer. Our results are consistent with the only other published pediatric study. Nie et al. (26) showed that median donor-derived cfDNA at day 30 post-transplant was 0.90%; at day 60, it was 0.64% (0.47%–0.87%), and at day 90, it was 0.63%. However, this study did not evaluate the donor-derived cfDNA levels out to 1-year post-transplant as we did, nor did they stratify out the younger recipients. In our study, patients did not reach the low levels seen by 1 month in the Bromberg et al. (8) study until at least 4 months, longer if there was greater size disparity between donor and recipient (measured by the donor-recipient body surface area ratio ratio). We believe that the size disparity between the allograft and recipient and the lower levels of circulating recipient cfDNA in younger children might be contributing to this disparity. To support this concept, when there was greater disparity between the donor and recipient in our cohort (donor-recipient body surface area ratio >1.5), there was greater mean percentage of donor-derived cfDNA in the entire first year post-transplant when compared with the donor-recipient body surface area ratio <1.5 group.
In our study, using 109 plasma samples coupled with simultaneous histologic examination, donor-derived cfDNA levels >1% discriminated biopsy-proven acute rejection with an AUROC of 0.82 and provided a high 96% specificity but low 33% sensitivity (95% CI, 19% to 52%). In comparison, in the prospective adult multicenter Diagnosing Acute Rejection in Kidney Transplant Recipients (DART) study utilizing 107 biopsy specimens, the investigators obtained an AUROC of 0.74 for donor-derived cfDNA to discriminate biopsy-proven acute rejection. In the DART study, at a cutoff of 1%, donor-derived cfDNA had an 85% specificity (95% CI, 79% to 91%) and 59% sensitivity (95% CI, 44% to 74%) to discriminate acute rejection from no rejection (27). Sigdel et al. (16) using a different donor-derived cfDNA assay (28) demonstrated an AUROC of 0.87, 89% sensitivity (95% CI, 78% to 100%), and 73% specificity (95% CI, 65% to 80%) using a similar cutoff level of 1% to differentiate between rejection and control samples (16). The differences in our donor-derived cfDNA sensitivity and specificity versus the prior adult studies may be related to the size disparity between the graft and body size and may be due to the inclusion of subclinical rejections in our analysis.
The only previous pediatric study by Puliyanda et al. (18) found that donor-derived cfDNA >1% had a sensitivity of 86% and specificity of 100% for biopsy-proven acute rejection (AUROC: 0.996; 0.98–1.00; P=0.002). Their study included both antibody-mediated rejection and T cell–mediated rejections from for-cause biopsies, primarily the former, as 11 of 21 had only antibody-mediated rejection; however, an additional eight had mixed antibody-mediated rejection and T cell–mediated rejection, and only two had T cell–mediated rejection alone. In contrast, although we had no antibody-mediated rejection events in the early 12-month post-transplant time period in our cohort, we have a T cell–mediated rejection–rich dataset, with many surveillance biopsies and subclinical rejections. Previous studies in adult kidney transplants noted that donor-derived cfDNA values were higher in antibody-mediated rejection than with T cell–mediated rejection (16,29,30). These reasons may explain the differences in the AUROC and sensitivity/specificity between the prior pediatric study and our study.
Like the DART study, serum creatinine did not show any discriminatory benefit to identify biopsy-proven acute rejection in our study. In children specifically, serum creatinine may remain within a normal range due to the large kidney reserve offered by an adult-sized graft.
Our study is the first pediatric study looking at whether donor-derived cfDNA levels associated with the progression of BK virus infection in kidney transplant recipients. BK viral replication postkidney transplant first manifests as viruria, typically preceding viremia by a median of 4 weeks (31). In our study, levels of donor-derived cfDNA showed a significant correlation with BK viral loads in both urine and plasma. Taken together, the higher median donor-derived cfDNA levels in the BK viremia/viruria groups and the rise within the same individual suggest that kidney allograft parenchymal injury can occur at high levels of viruria, before the onset of viremia. The further increase in donor-derived cfDNA levels with BK viremia suggests increasing kidney parenchymal injury. The drop in donor-derived cfDNA levels we saw after resolution of viruria/viremia, not previously reported, suggests the end of acute injury. In adults, Kant et al. (17) reported higher plasma donor-derived cfDNA levels in biopsy-diagnosed BK virus nephropathy compared with BK viremia. Chen et al. (32) demonstrated that elevated urinary donor-derived cfDNA (measured by a different assay) could discriminate BK nephropathy in recipients with BK viruria. Our novel sets of longitudinal data provide a range of percentage increases at the onset of BK viruria or viremia and drop with viremia resolution, allowing for donor-derived cfDNA to be used to detect early allograft injury and track improvement.
We also tested the utility of donor-derived cfDNA as a surveillance tool for prognostication. In our study, an elevation in donor-derived cfDNA beyond 0.5% associated with a much higher spread in the eGFR 30 days later, with many more values showing a decline. A similar decline in eGFR was previously shown by Stites et al. (13) after a rejection event. Elevation in donor-derived cfDNA is agnostic of the cause of injury. Our belief is that the wider spread in the later eGFR implies that a bigger subsequent decline in eGFR occurred in a significant proportion of the population. This subgroup might have suffered injury that has become chronic, needing greater attention. Further, Bu et al. (14) in the Assessing AlloSure Donor-Derived cfDNA, Monitoring Insights of Kidney Allografts with Longitudinal Surveillance study demonstrated that more than one elevation in donor-derived cfDNA (>0.5%) was associated with significant eGFR decline at 3 years post-transplant. At this time, we hypothesize that donor-derived cfDNA may help to stratify the risk groups at the risk of declining allograft function and optimize the management in terms of surveillance.
Our study has some limitations. Although the plasma and urine samples were banked prospectively by protocol, the donor-derived cfDNA assay was performed much later. Even though the small patient size was a limitation for the study, we had an advantage of serial longitudinal sampling, resulting in a large sample size. Our patient cohort consists of mostly White recipients and Black recipients with first kidney transplants who were deceased donor recipients and had no antibody-mediated rejection events in the first 12 months.
In conclusion, donor-derived cfDNA levels positively correlated with BK viral loads in urine and serum and with T cell–mediated rejection. Our results indicate that donor-derived cfDNA postkidney transplantation is a reasonable, noninvasive marker for allograft integrity. Multicenter prospective studies in children are recommended to generalize and validate the findings and to investigate the role of the percentage of donor-derived cfDNA as a standard of care surveillance tool.
Disclosures
R. Dandamudi reports research funding from an American Society of Transplantation Research Network/CareDx–directed research grant. V.R. Dharnidharka reports consultancy agreements with Atara Biotherapeutics and Medincell, research funding from CareDx, honoraria from CareDx, an advisory or leadership role for North American Pediatric Renal Trials and Collaborative Studies, and other interests or relationships with the independent data safety monitoring committee of Akebia/MedPace. All remaining authors have nothing to disclose.
Funding
The donor-derived cfDNA AlloSure assay was supported by CareDx.
Supplementary Material
Acknowledgments
The authors thank the team at CareDx for performing the donor-derived cfDNA assays.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
Author Contributions
R. Dandamudi and V.R. Dharnidharka conceptualized the study; R. Dandamudi, C.W. Goss, and L. Walther were responsible for data curation; R. Dandamudi was responsible for investigation; C.W. Goss, and H. Gu were responsible for formal analysis; R. Dandamudi, V.R. Dharnidharka, and L. Walther were responsible for methodology; V.R. Dharnidharka was responsible for project administration; C.W. Goss and H. Gu were responsible for software; V.R. Dharnidharka was responsible for funding acquisition; V.R. Dharnidharka provided supervision; R. Dandamudi and V.R. Dharnidharka wrote the original draft; and R. Dandamudi, V.R. Dharnidharka, C.W. Goss, H. Gu and L. Walther reviewed and edited the manuscript.
Data Sharing Statement
Deidentified individual participant data will be made available upon request.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.03840322/-/DCSupplemental.
Supplemental Material. Methods.
References
- 1.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, Port FK: Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 341: 1725–1730, 1999. 10.1056/NEJM199912023412303 [DOI] [PubMed] [Google Scholar]
- 2.Dharnidharka VR, Fiorina P, Harmon WE: Kidney transplantation in children. N Engl J Med 371: 549–558, 2014. 10.1056/NEJMra1314376 [DOI] [PubMed] [Google Scholar]
- 3.Waikar SS, Bonventre JV: Creatinine kinetics and the definition of acute kidney injury. J Am Soc Nephrol 20: 672–679, 2009. 10.1681/ASN.2008070669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halawa A: The early diagnosis of acute renal graft dysfunction: A challenge we face. The role of novel biomarkers. Ann Transplant 16: 90–98, 2011 [PubMed] [Google Scholar]
- 5.Dandamudi R, Vyas N, Hmiel SP, Dharnidharka VR: Performance of the various serum creatinine-based GFR estimating equations in pediatric kidney transplant recipients, stratified by age and CKD staging. Pediatr Nephrol 36: 3221–3228, 2021. 10.1007/s00467-021-05024-9 [DOI] [PubMed] [Google Scholar]
- 6.Slocum JL, Heung M, Pennathur S: Marking renal injury: Can we move beyond serum creatinine? Transl Res 159: 277–289, 2012. 10.1016/j.trsl.2012.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serón D, Arns W, Chapman JR: Chronic allograft nephropathy--clinical guidance for early detection and early intervention strategies. Nephrol Dial Transplant 23: 2467–2473, 2008. 10.1093/ndt/gfn130 [DOI] [PubMed] [Google Scholar]
- 8.Bromberg JS, Brennan DC, Poggio E, Bunnapradist S, Langone A, Sood P, Matas AJ, Mannon RB, Mehta S, Sharfuddin A, Fischbach B, Narayanan M, Jordan SC, Cohen DJ, Zaky ZS, Hiller D, Woodward RN, Grskovic M, Sninsky JJ, Yee JP, Bloom RD: Biological variation of donor-derived cell-free DNA in renal transplant recipients: Clinical implications. J Appl Lab Med 2: 309–321, 2017. 10.1373/jalm.2016.022731 [DOI] [PubMed] [Google Scholar]
- 9.Stroun M, Lyautey J, Lederrey C, Olson-Sand A, Anker P: About the possible origin and mechanism of circulating DNA apoptosis and active DNA release. Clin Chim Acta 313: 139–142, 2001. 10.1016/s0009-8981(01)00665-9 [DOI] [PubMed] [Google Scholar]
- 10.Stroun M, Lyautey J, Lederrey C, Mulcahy HE, Anker P: Alu repeat sequences are present in increased proportions compared to a unique gene in plasma/serum DNA: Evidence for a preferential release from viable cells? Ann N Y Acad Sci 945: 258–264, 2001. 10.1111/j.1749-6632.2001.tb03894.x [DOI] [PubMed] [Google Scholar]
- 11.Martuszewski A, Paluszkiewicz P, Król M, Banasik M, Kepinska M: Donor-derived cell-free DNA in kidney transplantation as a potential rejection biomarker: A systematic literature review. J Clin Med 10: 193, 2021. 10.3390/jcm10020193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gielis EM, Ledeganck KJ, Dendooven A, Meysman P, Beirnaert C, Laukens K, De Schrijver J, Van Laecke S, Van Biesen W, Emonds MP, De Winter BY, Bosmans JL, Del Favero J, Abramowicz D: The use of plasma donor-derived, cell-free DNA to monitor acute rejection after kidney transplantation. Nephrol Dial Transplant 35: 714–721, 2020. 10.1093/ndt/gfz091 [DOI] [PubMed] [Google Scholar]
- 13.Stites E, Kumar D, Olaitan O, John Swanson S, Leca N, Weir M, Bromberg J, Melancon J, Agha I, Fattah H, Alhamad T, Qazi Y, Wiseman A, Gupta G: High levels of dd-cfDNA identify patients with TCMR 1A and borderline allograft rejection at elevated risk of graft injury. Am J Transplant 20: 2491–2498, 2020. 10.1111/ajt.15822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bu L, Gupta G, Pai A, Anand S, Stites E, Moinuddin I, Bowers V, Jain P, Axelrod DA, Weir MR, Wolf-Doty TK, Zeng J, Tian W, Qu K, Woodward R, Dholakia S, De Golovine A, Bromberg JS, Murad H, Alhamad T: Clinical outcomes from the Assessing Donor-derived cell-free DNA Monitoring Insights of kidney Allografts with Longitudinal surveillance (ADMIRAL) study. Kidney Int 101: 793–803, 2022. 10.1016/j.kint.2021.11.034 [DOI] [PubMed] [Google Scholar]
- 15.Huang E, Sethi S, Peng A, Najjar R, Mirocha J, Haas M, Vo A, Jordan SC: Early clinical experience using donor-derived cell-free DNA to detect rejection in kidney transplant recipients. Am J Transplant 19: 1663–1670, 2019. 10.1111/ajt.15289 [DOI] [PubMed] [Google Scholar]
- 16.Sigdel TK, Archila FA, Constantin T, Prins SA, Liberto J, Damm I, Towfighi P, Navarro S, Kirkizlar E, Demko ZP, Ryan A, Sigurjonsson S, Sarwal RD, Hseish SC, Chan-On C, Zimmermann B, Billings PR, Moshkevich S, Sarwal MM: Optimizing detection of kidney transplant injury by assessment of donor-derived cell-free DNA via massively multiplex PCR. J Clin Med 8: 19, 2018. 10.3390/jcm8010019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kant S, Bromberg J, Haas M, Brennan D: Donor-derived cell-free DNA and the prediction of BK virus-associated nephropathy. Transplant Direct 6: 622, 2020. 10.1097/TXD.0000000000001061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Puliyanda DP, Swinford R, Pizzo H, Garrison J, De Golovine AM, Jordan SC: Donor-derived cell-free DNA (dd-cfDNA) for detection of allograft rejection in pediatric kidney transplants. Pediatr Transplant 25: e13850, 2021. 10.1111/petr.13850 [DOI] [PubMed] [Google Scholar]
- 19.Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL: New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20: 629–637, 2009. 10.1681/ASN.2008030287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grskovic M, Hiller DJ, Eubank LA, Sninsky JJ, Christopherson C, Collins JP, Thompson K, Song M, Wang YS, Ross D, Nelles MJ, Yee JP, Wilber JC, Crespo-Leiro MG, Scott SL, Woodward RN: Validation of a clinical-grade assay to measure donor-derived cell-free DNA in solid organ transplant recipients. J Mol Diagn 18: 890–902, 2016. 10.1016/j.jmoldx.2016.07.003 [DOI] [PubMed] [Google Scholar]
- 21.Wong L, Robert W, Dholakia S: Medical diagnostic methods the evolution and innovation of donor-derived cell-free DNA testing in transplantation, 2021. 10.35248/2168-9784.2020.9.302 [DOI]
- 22.Grimm PC, McKenna R, Nickerson P, Russell ME, Gough J, Gospodarek E, Liu B, Jeffery J, Rush DN: Clinical rejection is distinguished from subclinical rejection by increased infiltration by a population of activated macrophages. J Am Soc Nephrol 10: 1582–1589, 1999. 10.1681/ASN.V1071582 [DOI] [PubMed] [Google Scholar]
- 23.Colvin RB, Cohen AH, Saiontz C, Bonsib S, Buick M, Burke B, Carter S, Cavallo T, Haas M, Lindblad A, Manivel JC, Nast CC, Salomon D, Weaver C, Weiss M: Evaluation of pathologic criteria for acute renal allograft rejection: Reproducibility, sensitivity, and clinical correlation. J Am Soc Nephrol 8: 1930–1941, 1997. 10.1681/ASN.V8121930 [DOI] [PubMed] [Google Scholar]
- 24.Mehta R, Sood P, Hariharan S: Subclinical rejection in renal transplantation: Reappraised. Transplantation 100: 1610–1618, 2016. 10.1097/TP.0000000000001163 [DOI] [PubMed] [Google Scholar]
- 25.Gielis EM, Beirnaert C, Dendooven A, Meysman P, Laukens K, De Schrijver J, Van Laecke S, Van Biesen W, Emonds MP, De Winter BY, Bosmans JL, Del Favero J, Abramowicz D, Ledeganck KJ: Plasma donor-derived cell-free DNA kinetics after kidney transplantation using a single tube multiplex PCR assay. PLoS One 13: e0208207, 2018. 10.1371/journal.pone.0208207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nie W, Su X, Liu L, Li J, Fu Q, Li X, Wu C, Wang J, Deng R, Chen E, Yang S, Li S, Zhang H, Wang C: Dynamics of donor-derived cell-free DNA at the early phase after pediatric kidney transplantation: A prospective cohort study. Front Med (Lausanne) 8: 814517, 2022. 10.3389/fmed.2021.814517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bloom RD, Bromberg JS, Poggio ED, Bunnapradist S, Langone AJ, Sood P, Matas AJ, Mehta S, Mannon RB, Sharfuddin A, Fischbach B, Narayanan M, Jordan SC, Cohen D, Weir MR, Hiller D, Prasad P, Woodward RN, Grskovic M, Sninsky JJ, Yee JP, Brennan DC; Circulating Donor-Derived Cell-Free DNA in Blood for Diagnosing Active Rejection in Kidney Transplant Recipients (DART) Study Investigators : Cell-free DNA and active rejection in kidney allografts. J Am Soc Nephrol 28: 2221–2232, 2017. 10.1681/ASN.2016091034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Melancon JK, Khalil A, Lerman MJ: Donor-derived cell free DNA: Is it all the same? Kidney360 1: 1118–1123, 2020. 10.34067/kid.0003512020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bloom RD: Using (cell-free) DNA to incriminate rejection as the cause of kidney allograft dysfunction: Do we have a verdict? Am J Transplant 19: 1609–1610, 2019. 10.1111/ajt.15338 [DOI] [PubMed] [Google Scholar]
- 30.Whitlam JB, Ling L, Skene A, Kanellis J, Ierino FL, Slater HR, Bruno DL, Power DA: Diagnostic application of kidney allograft-derived absolute cell-free DNA levels during transplant dysfunction. Am J Transplant 19: 1037–1049, 2019. 10.1111/ajt.15142 [DOI] [PubMed] [Google Scholar]
- 31.Hirsch HH, Knowles W, Dickenmann M, Passweg J, Klimkait T, Mihatsch MJ, Steiger J: Prospective study of polyomavirus type BK replication and nephropathy in renal-transplant recipients. N Engl J Med 347: 488–496, 2002. 10.1056/NEJMoa020439 [DOI] [PubMed] [Google Scholar]
- 32.Chen XT, Chen WF, Li J, Deng RH, Huang Y, Yang SC, Chen PS, Jiang TY, Liu HT, Wang CX, Chen LZ, Qiu J, Huang G: Urine donor-derived cell-free DNA helps discriminate BK Polyomavirus-associated nephropathy in kidney transplant recipients with BK polyomavirus infection. Front Immunol 11: 1763, 2020. 10.3389/fimmu.2020.01763 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.