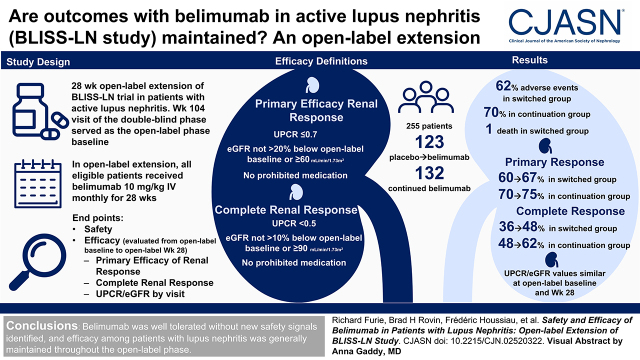
Visual Abstract
Keywords: clinical trial, glomerular disease, glomerulonephritis, kidney disease, lupus nephritis, proteinuria, belimumab
Abstract
Background and objectives
In the BLISS-LN study, belimumab improved kidney outcomes in adult patients with active lupus nephritis. This 28-week open-label extension of BLISS-LN assessed belimumab’s safety and efficacy.
Design, setting, participants, & measurements
Eligible patients completing BLISS-LN received monthly intravenous belimumab 10 mg/kg plus standard therapy. End points included safety, open-label week 28 primary efficacy renal response (urine protein-creatinine ratio [UPCR] ≤0.7, eGFR no more than 20% below open-label baseline value or ≥60 ml/min per 1.73 m2, no prohibited medications) and complete renal response (UPCR <0.5, eGFR no more than 10% below open-label baseline value or ≥90 ml/min per 1.73 m2, no prohibited medications), and UPCR and eGFR by visit. Responses were also analyzed post hoc using the double-blind phase criteria.
Results
Of 257 enrolled patients, 255 were treated (safety population: n=123 switched from placebo-to-belimumab; n=132 remained on belimumab); 245 (97%) patients completed the study. Adverse events and serious adverse events were experienced by 62% and 4% of placebo-to-belimumab patients, respectively, and by 70% and 8% of belimumab-to-belimumab patients, respectively. One death occurred in the placebo-to-belimumab group. From open-label baseline to week 28, increases occurred in the proportions of patients achieving primary efficacy renal response (placebo-to-belimumab: from 60% to 67%; belimumab-to-belimumab: from 70% to 75%) and complete renal response (placebo-to-belimumab: from 36% to 48%; belimumab-to-belimumab: from 48% to 62%). Based on double-blind phase criteria, changes also occurred in the proportions achieving primary efficacy renal response (placebo-to-belimumab: from 54% to 53%; belimumab-to-belimumab: from 66% to 52%) and complete renal response (placebo-to-belimumab: from 34% to 35%; belimumab-to-belimumab: from 46% to 41%). The seeming decrease in response rates in the belimumab-to-belimumab groups was attributed to discontinuations/administration of glucocorticoids for non-SLE reasons as opposed to nephritis. Median UPCR and eGFR values were similar at open-label baseline and week 28.
Conclusions
No new safety signals were identified, and efficacy was generally maintained throughout the open-label phase.
Clinical Trial registry name and registration number:
BLISS-LN, NCT01639339
Introduction
Lupus nephritis, the most common serious manifestation of SLE, occurs in approximately 40% of patients, and despite therapeutic advances, up to 30% of patients with lupus nephritis are at risk of progressing to kidney failure (1–3). Thus, there remains a need for efficacious lupus nephritis treatments that preserve long-term kidney function with a favorable safety profile.
Belimumab, a recombinant, human IgG1λ mAb that targets soluble B-lymphocyte stimulator (4), is approved for the treatment of patients aged ≥5 years with active autoantibody-positive SLE receiving standard therapy (5,6). The previously published phase 3 BLISS-LN (GSK Study BEL114054) study demonstrated that intravenous belimumab plus standard therapy had a favorable safety profile and significantly improved kidney outcomes in adult patients with active lupus nephritis (7). The results of BLISS-LN led to approvals of belimumab in the United States and Europe as the first biologic agent for the treatment of adult patients with active lupus nephritis (8,9).
Here, we present the results of a 28-week, open-label extension phase of the BLISS-LN study, the objectives of which were to assess safety, tolerability, and efficacy of belimumab in combination with standard therapy in patients with lupus nephritis who completed treatment in the 104-week, double-blind phase of BLISS-LN, and to assess whether the responses achieved in the double-blind phase were maintained for the additional 6-month open-label phase.
Materials and Methods
Study Design
This was a 28-week, open-label extension of the phase 3 multicenter, randomized, placebo-controlled, 104-week BLISS-LN study (GSK Study BEL114054) conducted between February 2015 and March 2020. The double-blind phase study design has been previously published (7).
All eligible patients received intravenous belimumab 10 mg/kg plus standard therapy every 28 days until week 24, with a final evaluation at week 28 (4 weeks after the last dose). The first open-label dose was administered at the double-blind phase week 104 visit (open-label phase day 0) following completion of all week 104 assessments. Patients who switched from placebo-to-belimumab were included in the placebo-to-belimumab group, and patients who remained on belimumab were included in the belimumab-to-belimumab group. Double-blind phase restrictions on concomitant medications, including glucocorticoids and immunosuppressants, no longer applied in the open-label phase, except for live vaccines, biologics, and other investigational drugs.
Patients continued to receive belimumab unless specific withdrawal criteria occurred (Supplemental Material). Patients were free to withdraw from treatment/study at any time.
This study was conducted in accordance with the principles of the Declaration of Helsinki, and all study sites received approval from ethics committees or institutional review boards. Written informed consent was obtained from all patients.
Patients
Patients who received belimumab or placebo through week 100 and completed the double-blind phase week 104 assessments were eligible to participate in the open-label phase. Full double-blind phase inclusion and exclusion criteria have been previously published (7). At the double-blind phase baseline, patients were aged ≥18 years and had autoantibody-positive SLE (antinuclear antibody ≥1:80 and/or antidouble-stranded DNA [anti-dsDNA] ≥30 IU/ml) as per the American College of Rheumatology SLE classification criteria (10,11) and biopsy-proven (within 6 months) proliferative lupus nephritis class 3 or 4 with or without coexisting class 5 or pure class 5 membranous lupus nephritis as per the 2003 International Society of Nephrology and Renal Pathology Society criteria (12).
End Points and Assessments
The primary objective was to evaluate the safety of belimumab from open-label baseline to open-label week 28. Safety assessments included monitoring of adverse events (AEs), serious AEs, AEs of special interest (malignancies, postinfusion systemic reactions, opportunistic infections, sepsis, and depression/suicide/self-injury), deaths, and immunogenicity.
Treatment-emergent AEs were defined as any AE that occurred after receipt of the first dose of open-label treatment. AEs were assessed at each infusion visit. Other safety end points were monitored at regular intervals until the 8-week follow-up visit (postfinal belimumab dose).
Key secondary efficacy end points were the proportions of patients with primary efficacy renal response and the proportions of patients with complete renal response at open-label week 28. During the open-label phase, primary efficacy renal response was defined as a urine protein-creatinine ratio (UPCR) ≤0.7, eGFR of no more than 20% below the open-label baseline eGFR or ≥60 ml/min per 1.73 m2, and no prohibited medications. Complete renal response was defined as a UPCR <0.5, eGFR no more than 10% below open-label baseline eGFR or ≥90 ml/min per 1.73 m2, and no prohibited medications. Although there were no restrictions on concurrent medications during the open-label phase, for primary efficacy renal response and complete renal response end points, the definition of prohibited medications in the double-blind phase was used to capture the use of medication that would have been classified as prohibited during the double-blind phase (7). In addition, primary efficacy renal response and complete renal response criteria were assessed based on observed data at open-label weeks 12, 24, and 28, and criteria were required to be met at a single time point only (i.e., criteria did not have to be met on consecutive visits as was required for the double-blind phase).
To assess the maintenance of response over time, post hoc analyses of primary efficacy renal response and complete renal response at open-label week 28 were also performed according to the double-blind phase criteria (i.e., the eGFR component was relative to the preflare value, and primary efficacy renal response and complete renal response criteria were required to be met on two consecutive visits [weeks 100 and 104 in the double-blind phase; weeks 24 and 28 in the open-label phase]). However, open-label week 28 was the only time point during the open-label phase where the double-blind criteria of primary efficacy renal response and complete renal response end points were applied.
Additional efficacy end points included the time to a sustained primary efficacy renal response and complete renal response from double-blind baseline through to open-label week 28 (using double-blind phase criteria; post hoc analyses); proportions of UPCR responders (<0.5) from double-blind week 4 through open-label week 28 by visit; mean eGFR levels from double-blind baseline to open-label week 28 by visit; proportions of patients with an SLE Disease Activity Index-2000 (SLEDAI-S2K) score less than four at open-label week 28; proportion of patients with a doubling of serum creatinine (compared with the open-label baseline) and/or progression to kidney failure (defined as the need for long-term dialysis or kidney transplantation); proportions of patients with average daily prednisone-equivalent dose ≤5, ≤7.5, or ≤10 mg/day at open-label week 28; and percentage changes from open-label baseline in anti-dsDNA and complement 3 (C3)/C4 biomarker levels to open-label week 28 among patients who were anti-dsDNA positive and had low C3/C4 at open-label baseline, respectively.
Statistical Analyses
Open-label baseline was defined as the last available value prior to the first dose of open-label treatment (day 0). All patients received belimumab in the open-label phase; thus, no statistically meaningful treatment comparisons can be made. All analyses were considered exploratory in nature using descriptive statistics. Safety and efficacy end points were assessed for the duration of the open-label phase only, unless otherwise indicated.
Safety end points were assessed in the open-label safety population, defined as all enrolled patients who received one or more doses of open-label belimumab treatment. AEs were summarized at any time postfirst dose of open-label treatment. Efficacy end points were assessed in the open-label safety population, excluding one patient due to Good Clinical Practice nonadherence issues (modified intention-to-treat population).
Predefined analyses were based on observed data, with no imputation for missing data. In the analyses of the primary efficacy renal response and complete renal response, patients who received medication in the open-label phase that met the definition of prohibited medications in the double-blind phase were counted as treatment failure and imputed as a nonresponse. For the post hoc analyses using the double-blind criteria for primary efficacy renal response and complete renal response, withdrawal from the trial, treatment failure, and discontinuation of study treatment were imputed as a nonresponse.
Results
Baseline Characteristics
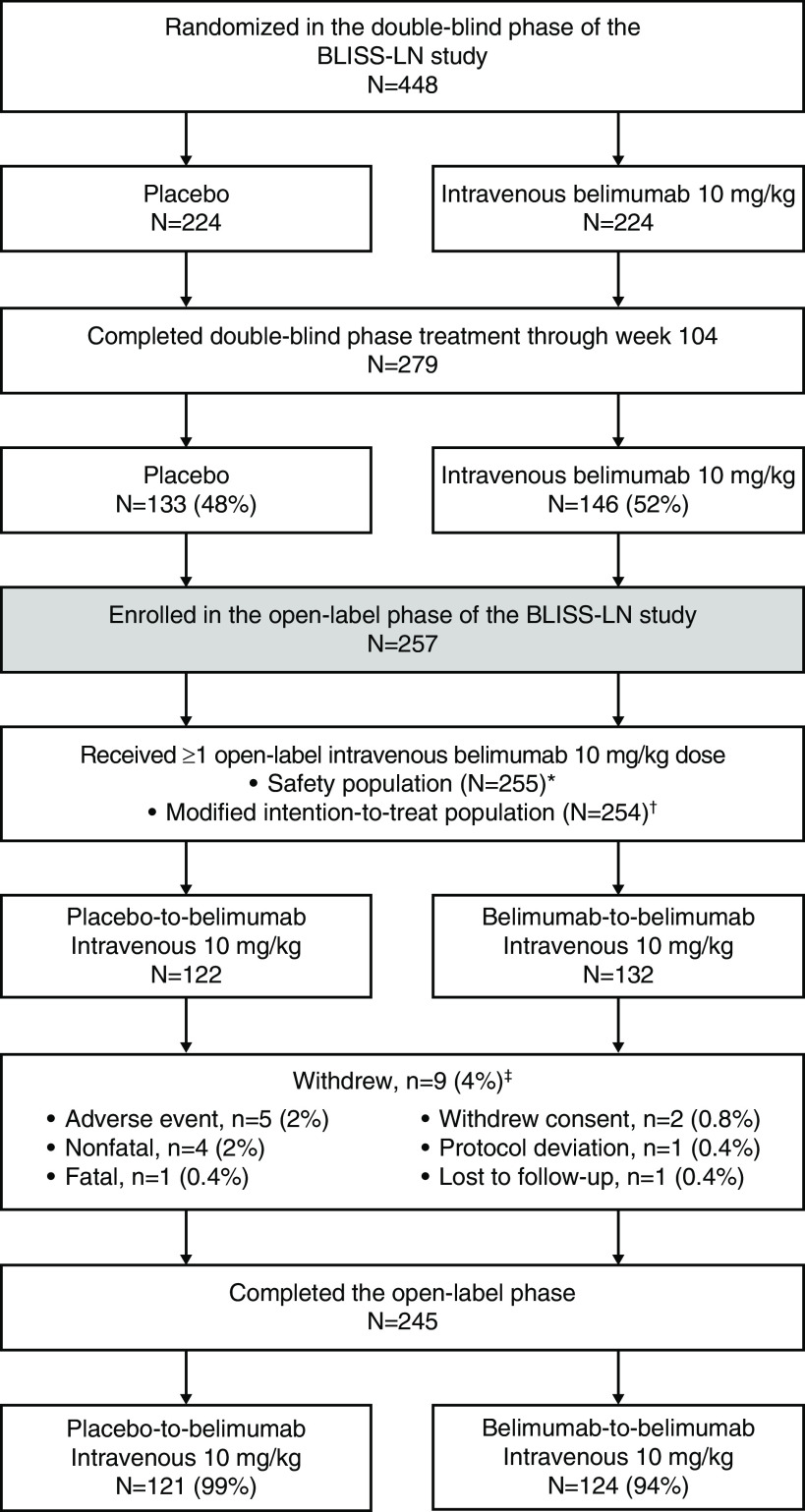
Of 448 patients randomized in the BLISS-LN study, 279 patients completed the double-blind phase; of these patients, 257 enrolled in the open-label phase, and 255 (n=123, placebo-to-belimumab; n=132, belimumab-to-belimumab) received one or more doses of intravenous belimumab 10 mg/kg and were included in the open-label safety population (Figure 1). Of 254 patients included in the open-label modified intention-to-treat population, most patients (245 [97%]) completed the open-label phase through week 28. The most common reason for withdrawal was AEs (five of 254 [2%]).
Figure 1.
Patient disposition in the open-label phase. *Two patients enrolled in the open-label phase did not receive open-label belimumab. They were inadvertently enrolled in the open-label phase while permanently discontinued from the double-blind investigational product and were thus excluded from analysis populations. †Of the 255 patients who received one or more open-label intravenous belimumab 10-mg/kg doses, one patient was not included in the modified intention-to-treat population due to Good Clinical Practice nonadherence issues in the double-blind phases of the study. Open-label data from this patient were excluded from all efficacy analyses, but they were included in the safety analyses for consistency with the double-blind phase reporting. Data are reported for the modified intention-to-treat population from “Received ≥1 open-label intravenous belimumab 10 mg/kg” downward. ‡Includes all withdrawals for both treatment groups (belimumab-to-belimumab, n=8; placebo-to-belimumab, n=1).
At open-label baseline, patients in the belimumab-to-belimumab group exhibited trends suggesting overall better disease control compared with the placebo-to-belimumab group, as evidenced by lower baseline UPCR values, a higher proportion of patients with SLEDAI-S2K scores of less than eight, lower average prednisone-equivalent doses, and lower proportions of autoantibody-positive patients and patients with low C3/C4 levels (Table 1). Those entering the open-label phase had similar characteristics at the double-blind baseline compared with the overall population of the double-blind phase (Supplemental Table 1).
Table 1.
Patient characteristics at the start of the open-label phase of BLISS-LN (open-label modified intention-to-treat population, N=254)
| Placebo-to- Belimumab Intravenous 10 mg/kg, N=122 | Belimumab-to- Belimumab Intravenous 10 mg/kg, N=132 | |
|---|---|---|
| Race,a n (%) | ||
| Asian | 67 (55) | 71 (54) |
| Black African/American ancestry | 13 (11) | 12 (9) |
| White | 38 (31) | 47 (36) |
| Otherb | 4 (3) | 2 (2) |
| Age, yr, mean (SD) | 36 (10) | 36 (10) |
| Women, n (%) | 110 (90) | 118 (89) |
| Lupus nephritis class, n (%) | ||
| Class 3 or 4 | 70 (57) | 78 (59) |
| Class 3 + 5 or class 4 + 5 | 31 (25) | 36 (27) |
| Class 5 | 21 (17) | 18 (14) |
| UPCR, g/g, median (IQR) | 0.4 (0.1–1.0) | 0.3 (0.1–0.7) |
| UPCR category, g/g, n (%) | ||
| <0.5 | 71 (58) | 89 (67) |
| ≤0.7 | 79 (65) | 98 (74) |
| ≥3 | 6 (5) | 7 (5) |
| eGFR, ml/min per 1.73 m2, median (IQR) | 105 (84–123) | 108 (88–130) |
| SLEDAI-S2K score, median (IQR) | 4 (2–8) | 4 (1–6)c |
| SLEDAI-S2K score <8, n (%) | 84 (69) | 103 (78) |
| Medications at baseline | ||
| Steroids, n (%) | 103 (84) | 110 (83) |
| Average daily prednisone- equivalent dose, mg/day, median (IQR) | 7.5 (5.0–10.0) | 5.0 (2.5–10.0) |
| Antimalarials, n (%) | 86 (71) | 100 (76) |
| Immunosuppressants, n (%) | 120 (98) | 129 (98) |
| ACE/ARBs, n (%) | 83 (68) | 86 (65) |
| Biomarkers | ||
| Anti-dsDNA | ||
| Positive, ≥30 IU/ml, n (%) | 85 (70) | 64 (49) |
| Anti-C1q | ||
| Positive, ≥22.2 U/ml, n (%) | 64 (68)d | 60 (55)e |
| C3 | ||
| Low, <90 mg/dl, n (%) | 45 (37) | 37 (28) |
| C4 | ||
| Low, <10 mg/dl, n (%) | 18 (15) | 12 (9) |
UPCR, urine protein-creatinine ratio; IQR, interquartile range; SLEDAI-S2K, SLE Disease Activity Index-2000; ACE, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor antagonist/blocker; anti-dsDNA, antidouble-stranded DNA; C3, complement 3; C4, complement 4.
Patients were only counted in one category.
Composed of the categories: mixed race and American Indian or Alaska Native.
n=131.
n=94.
n=109.
The median (minimum, maximum) duration of exposure to intravenous belimumab 10 mg/kg during the open-label phase was 196 (85, 207) days in the placebo-to-belimumab group and 196 (56, 214) days in the belimumab-to-belimumab group (following approximately 104 weeks of blinded exposure to belimumab).
Safety
Overall, 76 of 123 (62%) placebo-to-belimumab patients and 92 of 132 (70%) belimumab-to-belimumab patients experienced AEs (Table 2). The most frequently reported AEs by system organ class occurring in ≥5% of patients in either open-label treatment group included infections and infestations, musculoskeletal and connective tissue disorders, and skin and subcutaneous tissue disorders.
Table 2.
Summary of treatment-emergent adverse events and adverse events of special interest (open-label safety population, N=255)
| n (%) | ||
|---|---|---|
| Placebo-to-Belimumab Intravenous 10 mg/kg, N=123 | Belimumab-to-Belimumab Intravenous 10 mg/kg, N=132 | |
| ≥1 AE | 76 (62) | 92 (70) |
| AE by SOC occurring in ≥5% of patients in either treatment group a | ||
| Infections and infestations | 52 (42) | 64 (49) |
| Musculoskeletal and connective tissue disorders | 16 (13) | 16 (12) |
| Skin and subcutaneous tissue disorders | 10 (8) | 17 (13) |
| Gastrointestinal disorders | 11 (9) | 13 (10) |
| Respiratory, thoracic, and mediastinal disorders | 5 (4) | 15 (11) |
| Nervous system disorders | 7 (6) | 10 (8) |
| General disorders and administration site conditions | 8 (7) | 8 (6) |
| Eye disorders | 0 (0) | 8 (6) |
| ≥1 treatment-related AE | 25 (20) | 24 (18) |
| Treatment-related AE by SOC occurring in ≥5% of patients in either treatment group | ||
| Infections and infestations | 17 (14) | 17 (13) |
| ≥1 serious AE | 5 (4) | 10 (8) |
| Serious AE by SOC occurring in ≥5% of patients in either treatment group | ||
| Infections and infestations | 4 (3) | 7 (5) |
| ≥1 AE resulting in study treatment discontinuation | 1 (0.8) | 4 (3) |
| AEs of special interest | ||
| Malignancies | 0 (0) | 0 (0) |
| Postinfusion systemic reactionsb | 4 (3) | 5 (4) |
| Infections of special interest (opportunistic infections, herpes zoster, tuberculosis, sepsis)c | 2 (2) | 6 (5) |
| Serious | 0 (0) | 2 (2) |
| Depression (including mood disorders and anxiety)/suicide/ self-injuryc | 2 (2) | 4 (3)d |
| Death e | 1 (0.8) | 0 (0) |
AE, adverse event; SOC, system organ class.
Patients are counted only once per SOC.
No serious postinfusion systemic reactions were reported.
Per customized Medical Dictionary for Regulatory Activities query (version 22.0).
There was one serious AE of suicidal behavior in a patient diagnosed with an adjustment disorder that occurred 12 days after the first open-label infusion. This patient recovered and completed belimumab treatment throughout the open-label phase.
Occurred 85 days after the first open-label infusion at open-label day 0 and 8 days after the last infusion at open-label week 12. Death was associated with fatal serious AEs of multiple organ dysfunction syndrome, sepsis secondary to nosocomial pneumonia, and CKD. The adjudicated category of death was “SLE related.”
The incidence of serious AEs during the open-label phase was low, reported in five of 123 (4%) placebo-to-belimumab patients and ten of 132 (8%) belimumab-to-belimumab patients (Table 2). Overall, the incidence of AEs resulting in study treatment discontinuation during the open-label study was ≤3% in both groups (Table 2), with infections and infestations being the most common (one of 123 [0.8%] in the placebo-to-belimumab group; four of 132 [3%] in the belimumab-to-belimumab group).
The overall incidence of AEs of special interest was low during the open-label phase (Table 2). Two serious infections of special interest (one event of serious tuberculosis and one event of serious disseminated herpes zoster) were reported in the belimumab-to-belimumab group. There was one case of suicidal behavior in the belimumab-to-belimumab group in a patient diagnosed with an adjustment disorder who took an overdose of lorazepam. This patient recovered and completed belimumab treatment throughout the open-label phase.
One death was reported in the placebo-to-belimumab group, which was associated with fatal serious AEs of multiple organ dysfunction syndrome, sepsis secondary to nosocomial pneumonia, and CKD.
Of 247 patients assessed for positive antidrug antibodies at any time post open-label baseline, one patient in the belimumab-to-belimumab group tested positive for antibelimumab antibodies at a follow-up visit 8 weeks after the last dose.
Efficacy
The proportions of patients who achieved primary efficacy renal response increased from open-label baseline to open-label week 28 in both groups: from 60% to 67% in the placebo-to-belimumab group and from 70% to 75% in the belimumab-to-belimumab group (Table 3). The proportions of patients with complete renal response also increased: from 36% at open-label baseline to 48% at open-label week 28 in the placebo-to-belimumab group and from 48% to 62% in the belimumab-to-belimumab group (Table 3).
Table 3.
Primary efficacy renal response and complete renal response at open-label baseline and open-label week 28 (open-label modified intention-to-treat population, N=254)
| Placebo-to-Belimumab Intravenous 10 mg/kg, N=122 | Belimumab-to-Belimumab Intravenous 10 mg/kg, N=132 | |||
|---|---|---|---|---|
| Open-Label Baselinea | Open-Label Week 28 | Open-Label Baselinea | Open-Label Week 28 | |
| Key secondary efficacy end points primary efficacy renal response and complete renal response using open-label phase criteria (observed cases) | ||||
| Primary efficacy renal responseb | ||||
| N | 122 | 118c | 132 | 122c |
| Responders, n (%) | 73 (60)d | 79 (67) | 93 (70)d | 91 (75) |
| Complete renal responseb | ||||
| N | 122 | 118c | 132 | 122c |
| Responders, n (%) | 44 (36)d | 57 (48) | 63 (48)d | 76 (62) |
| Post hoc analyses primary efficacy renal response and complete renal response using double-blind phase criteria | ||||
| Primary efficacy renal responsee | ||||
| N | 122 | 122 | 132 | 132 |
| Responders, n (%) | 66 (54) | 64 (53) | 87 (66) | 69 (52) |
| Complete renal responsee | ||||
| N | 122 | 122 | 132 | 132 |
| Responders, n (%) | 41 (34) | 43 (35) | 60 (46) | 54 (41) |
The double-blind week 104 visit and the open-label baseline visit were the same visit.
To have a primary efficacy renal response and a complete renal response, the results did not have to be replicated across two consecutive visits.
Among patients who had data on kidney outcomes at open-label week 28, including any patients who continued to provide data in the study after stopping the study treatment.
Post hoc analyses.
To have a primary efficacy renal response and a complete renal responses, the results had to be replicated across two consecutive visits. All patients were included in the analysis. Withdrawal from the trial, treatment failure, and discontinuation of study treatment were counted as nonresponses.
Post hoc analyses performed using the more stringent double-blind phase criteria for primary efficacy renal response and complete renal response showed that in the placebo-to-belimumab group, the proportions of patients with primary efficacy renal response and complete renal response at open-label baseline were 54% and 34%, respectively, with the response rates maintained at open-label week 28 (Table 3). In the belimumab-to-belimumab group, the proportions of patients who met double-blind criteria for primary efficacy renal response and complete renal response were 66% and 46%, respectively, at open-label baseline and 52% and 41%, respectively, at open-label week 28 (Table 3). Reductions in primary efficacy renal response and complete renal response rates at open-label week 28 in the belimumab-to-belimumab group were mainly due to discontinuations (n=8) or intake of concomitant medications (n=9) allowed during the open-label phase but counted as treatment failures for the statistical analysis. All but one of the treatment failures were for nonkidney reasons, indicating that reductions in rates of primary efficacy renal response and complete renal response were not due to kidney worsening, but due to medications taken for non-SLE reasons (Supplemental Material). At open-label week 28, in the placebo-to-belimumab group, one patient discontinued, and one patient took concomitant medications classified as treatment failures (Supplemental Material).
The post hoc analysis of durability of response to open-label week 28 suggested that the primary efficacy renal response and complete renal response achieved in the double-blind phase were maintained for another 6 months in the open-label phase in both treatment groups (Figure 2).
Figure 2.
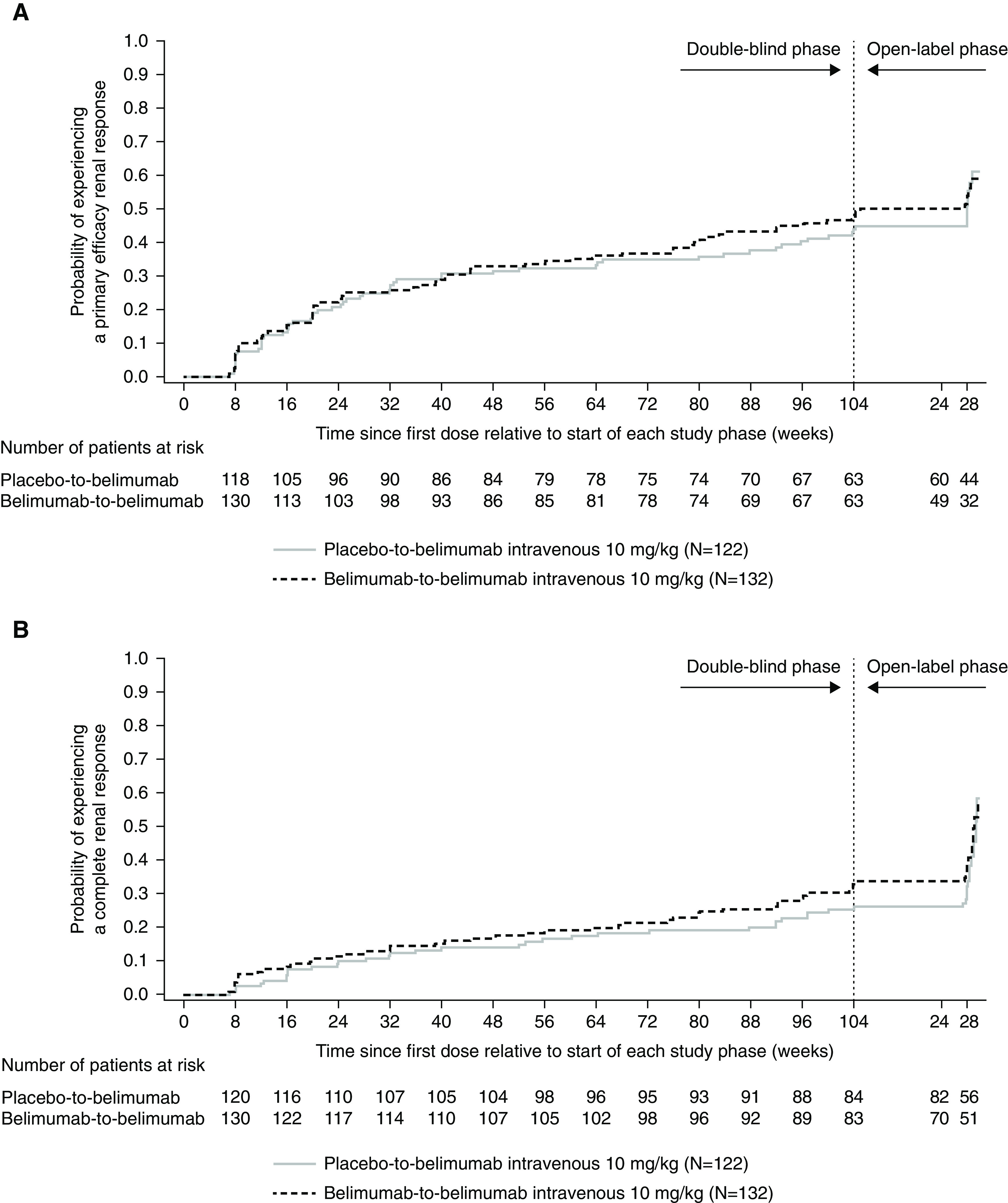
Probability of (A) primary efficacy renal response and (B) complete renal response maintained through open-label week 28 (using double-blind criteria) in patients enrolled in the open-label phase (open-label modified intention-to-treat population; post hoc analyses). This figure shows the cumulative probability of primary efficacy renal response and complete renal response that were sustained through open-label week 28 estimated using the Kaplan–Meier method. Patients randomized to placebo in the double-blind phase started belimumab in the open-label phase. Week 104 denotes the end of the double-blind phase and the start of the open-label phase. Primary efficacy renal response and complete renal response were defined using double-blind phase criteria. To have a primary efficacy renal response and a complete renal response, the results had to be replicated across two consecutive visits. Patients who discontinued open-label treatment, had treatment failure, or withdrew from the trial were not considered to have had a sustained response. Data on patients who did not have a primary efficacy renal response and a complete renal response at open-label week 28 were censored at the last available visit to open-label week 28. Data from patients who had treatment failure and discontinued open-label treatment, were lost to follow-up, or died were censored. The time to event in days was calculated as the event date minus the treatment start date plus one.
Median (interquartile range [IQR]) UPCR values were 0.4 (0.1–1.0) g/g in the placebo-to-belimumab group and 0.3 (0.1–0.7) g/g in the belimumab-to-belimumab group at open-label baseline; these values remained low at open-label week 28 for both groups (Table 4). The UPCR (<0.5 g/g) responder rates improved from double-blind week 4 through to open-label week 28 in both groups (Figure 3A). Median (IQR) eGFR values were 105 (84–123) ml/min per 1.73 m2 in the placebo-to-belimumab group and 108 (88–130) ml/min per 1.73 m2 in the belimumab-to-belimumab group at open-label baseline, and these values remained high at open-label week 28 in both groups (Table 4). The eGFR levels generally remained stable through open-label week 28 (Figure 3B).
Table 4.
Summary of other efficacy end points at open-label baseline and open-label week 28 (open-label modified intention-to-treat population, N=254; observed cases)
| Placebo-to-Belimumab Intravenous 10 mg/kg, N=122 | Belimumab-to-Belimumab Intravenous 10 mg/kg, N=132 | |||
|---|---|---|---|---|
| Open-Label Baselinea | Open-Label Week 28 | Open-Label Baselinea | Open-Label Week 28 | |
| UPCR, g/g | ||||
| N | 122b | 118 | 132b | 122 |
| Median (IQR) | 0.4 (0.1–1.0) | 0.4 (0.1–0.9) | 0.3 (0.1–0.7) | 0.2 (0.1–0.5) |
| UPCR <0.5, g/g | ||||
| N | 121b | 118 | 127b | 122 |
| n (%) | 69 (57) | 68 (58) | 87 (69) | 91 (75) |
| eGFR, ml/min per 1.73 m2 | ||||
| N | 122b | 119 | 132b | 123 |
| Median (IQR) | 105 (84–123) | 104 (81–124) | 108 (88–130) | 106 (88–127) |
| SLEDAI-S2K score <4 | ||||
| N | 122 | 120 | 132 | 122 |
| Responders, n (%) | 44 (36)c | 40 (33) | 64 (49)c | 64 (53) |
| Average daily prednisone-equivalent dose, mg/day | ||||
| N | 122 | 121 | 132 | 128 |
| ≤10, n (%) | 122 (100) | 120 (99) | 132 (100) | 126 (98) |
| ≤7.5, n (%) | 62 (51) | 66 (55) | 85 (64) | 83 (65) |
| ≤5, n (%) | 59 (48) | 60 (50) | 78 (59) | 75 (59) |
| Biomarkers | ||||
| Anti-dsDNA among anti-dsDNA–positive patients at baseline, IU/ml | ||||
| N | 85 | 81 | 64 | 61 |
| Median (IQR) % change from baseline d | — | −30.2 (−46.3 to −6.8) | — | −10.7 (−27.2 to 9.1) |
| C3 among patients with low C3 levels at baseline, mg/dl | ||||
| N | 45 | 44 | 37 | 35 |
| Median (IQR) % change from baseline e | — | 6.2 (−4.2 to 14.6) | — | 4.7 (−4.8 to 16.9) |
| C4 among patients with low C4 levels at baseline, mg/dl | ||||
| N | 18 | 18 | 12 | 11 |
| Median (IQR) % change from baseline e | 23.6 (11.1–37.5) | — | 11.1 (0.0–57.1) | |
UPCR, urine protein-creatinine ratio; IQR, interquartile range; SLEDAI-S2K, SLE Disease Activity Index-2000; anti-dsDNA, antidouble-stranded DNA; C3, complement 3; C4, complement 4.
The double-blind week 104 visit and the open-label baseline visit were the same visit.
The open-label baseline has been derived where data were missing at week 104 of the double-blind phase (i.e., using double-blind phase data from week 96 onward).
Post hoc analyses.
Among anti-dsDNA–positive patients at open-label baseline (≥30 IU/ml). Normal range: <30 IU/ml. Median (IQR) baseline anti-dsDNA values: 107.0 (49.0–212.0) IU/ml in the placebo-to-belimumab group and 65.5 (42.5–126.5) IU/ml in the belimumab-to-belimumab group.
Among patients with low C3 (<90 mg/dl)/C4 (<10 mg/dl) levels at open-label baseline. Normal range: C3, 90−180 mg/dl; C4, 10−40 mg/dl. Median (IQR) baseline value: C3, 78.0 (72.0–83.0) mg/dl in the placebo-to-belimumab group and 80.0 (71.0–84.0) mg/dl in the belimumab-to-belimumab group; C4, 7.5 (6.0–8.0) mg/dl in the placebo-to-belimumab group and 7.0 (7.0–8.5) mg/dl in the belimumab-to-belimumab group.
Figure 3.
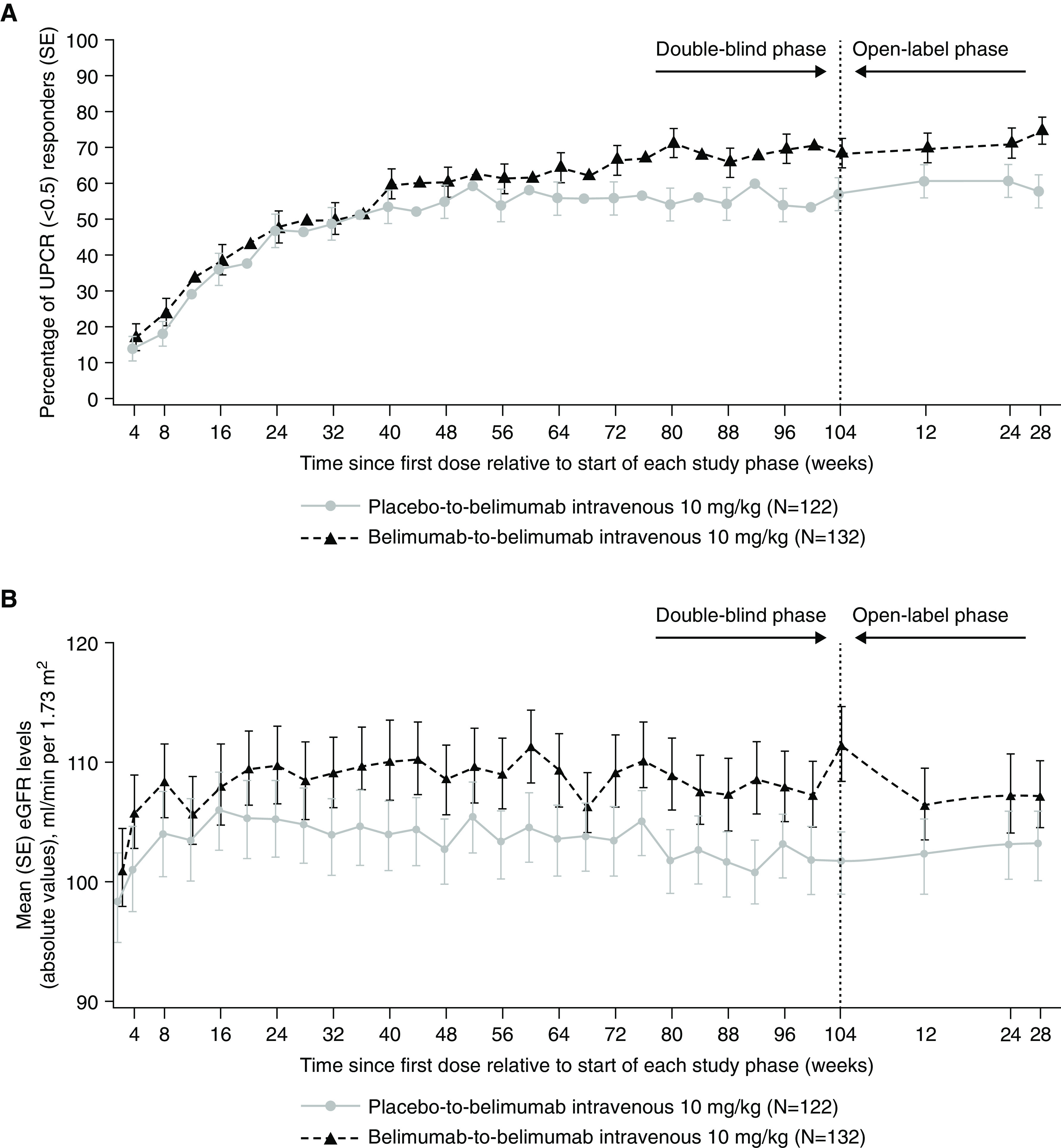
(A) UPCR (<0.5) and (B) eGFR by visit over double-blind and open-label phases in patients enrolled in the open-label phase (open-label modified intention-to-treat population; observed cases). Patients randomized to placebo in the double-blind phase started belimumab in the open-label phase; double-blind week 104 visit and the open-label baseline visit were the same visit. The UPCR graph denotes the proportion of responders over time. SE, standard error, UPCR, urine protein-creatinine ratio.
No marked changes were observed in the proportions of patients with SLEDAI-S2K scores less than four during the open-label phase in either group (Table 4).
One patient in each treatment group had a doubling of serum creatinine. In the placebo-to-belimumab group, the doubling of serum creatinine was followed by progression to kidney failure.
Among patients receiving prednisone, doses were unchanged from open-label baseline to open-label week 28, and almost all patients received an average dose of ≤10 mg/day (Table 4), despite no restrictions on doses of concomitant glucocorticoids.
Among anti-dsDNA–positive patients at open-label baseline, the median (IQR) percentage changes from open-label baseline to open-label week 28 in anti-dsDNA levels were −30.2 (−46.3 to −6.8) in the placebo-to-belimumab group and −10.7 (−27.2 to 9.1) in the belimumab-to-belimumab group (Table 4).
At open-label week 28, in patients with low C3/C4 levels at open-label baseline, the median (IQR) percentage changes from open-label baseline in C3/C4 levels were 6.2 (−4.2 to 14.6) for C3 and 23.6 (11.1–37.5) for C4 in the placebo-to-belimumab group and 4.7 (−4.8 to 16.9) for C3 and 11.1 (0.0–57.1) for C4 in the belimumab-to-belimumab group (Table 4).
Discussion
Despite the short duration of this open-label extension, adding or continuing belimumab treatment beyond 2 years was associated with enduring safety and efficacy consistent with that observed in the double-blind phase of the BLISS-LN study (7).
Patient demographics and disease characteristics at open-label baseline were generally balanced between the placebo-to-belimumab and belimumab-to-belimumab groups. Between-group differences in UPCR, proportions of patients with SLEDAI-S2K scores of less than eight, average prednisone-equivalent doses, and proportions of autoantibody-positive patients and patients with low C3/C4 levels were observed, favoring the belimumab-to-belimumab group. These data suggest that, as expected, patients in belimumab-to-belimumab group had better disease control than patients in the placebo-to-belimumab group at open-label baseline. Improvements in UPCR and eGFR values as well as serological activity from double-blind baseline to open-label baseline were observed in patients enrolled in the open-label phase, regardless of prior treatment assignment (7).
No new safety signals were observed with regard to continuing or initiating belimumab treatment. Overall, five of 123 (4%) patients in the placebo-to-belimumab group and ten of 132 (8%) patients in the belimumab-to-belimumab group experienced serious AEs, driven mainly by infections and infestations. Infections of special interest were reported in two of 123 (2%) patients in the placebo-to-belimumab group and six of 132 (5%) patients in the belimumab-to-belimumab group. However, this open-label extension phase was not controlled, so differences in safety profile between treatment groups should be interpreted with caution. Overall, the safety findings of this study were consistent with those observed during the BLISS-LN study double-blind phase and other open-label belimumab studies (7,13–15).
Proportions of patients achieving the key secondary efficacy end points of primary efficacy renal response or complete renal response increased from open-label baseline to open-label week 28 in both groups. Primary efficacy renal response and complete renal response criteria for the open-label phase were relaxed as compared with those used in the double-blind phase: criteria were not required to be reproduced on consecutive visits, and the eGFR criterion was relative to open-label baseline and not to preflare values. Furthermore, the treatment failure criterion with respect to prohibited medications, including immunosuppressants and glucocorticoids, was less restrictive than during the double-blind phase. These differences made it difficult to evaluate the rates of maintenance of primary efficacy renal response and complete renal response across the two phases of the study. Thus, post hoc analyses of primary efficacy renal response and complete renal response using the double-blind criteria were performed. These analyses showed that the seeming decrease in primary efficacy renal response and complete renal response rates from open-label baseline to open-label week 28 observed in the belimumab-to-belimumab group when using the double-blind criteria was driven by discontinuations (eight patients) and administration of glucocorticoids (nine patients) for non-SLE reasons and not by worsening or flaring nephritis. UPCR and eGFR values were maintained over the 28-week open-label phase in both the placebo-to-belimumab and belimumab-to-belimumab groups, with the data suggesting, as expected, that UPCR was better controlled in patients starting belimumab treatment at double-blind baseline. Importantly, despite the absence of any protocol mandates, the daily dose of glucocorticoids did not increase during the open-label phase of the study in either treatment group.
The biologic impact of belimumab was also evident from the observed serological improvements. At open-label baseline, the belimumab-to-belimumab group comprised lower proportions of autoantibody-positive patients and patients with low C3/C4 levels than the placebo-to-belimumab group. During the open-label phase, additional reductions in anti-dsDNA and increases in C3 and C4 levels were observed in both the placebo-to-belimumab and belimumab-to-belimumab groups.
There are limitations to the interpretation of these data. There was no placebo control during the open-label phase, and all patients received belimumab; thus, no statistically meaningful treatment comparisons can be made. Furthermore, the total duration of belimumab exposure was different between patients who received belimumab or placebo during the double-blind phase. During the double-blind phase, patients who, due to disease activity, required treatment with prohibited medications were withdrawn from treatment and did not enroll into the open-label phase. Therefore, there may have been selection bias as patients who completed the double-blind phase were those who tolerated belimumab or placebo with background immunosuppressants, were willing to participate in the open-label phase, and were potentially more likely to respond well to belimumab over time.
The derivation of the primary efficacy renal response/complete renal response criteria in the open-label phase was modified from the double-blind phase as patients in the belimumab-to-belimumab group received their first dose of belimumab during a period of high disease activity/flare, whereas patients in the placebo-to-belimumab group received their first dose of belimumab 104 weeks after double-blind baseline while receiving maintenance of remission therapy and had different disease activity status. The double-blind baseline was confounded by these differences, and therefore, the open-label baseline was used in the analysis of primary efficacy renal response and complete renal response for patients in the belimumab-to-belimumab and placebo-to-belimumab groups. The comparison with the open-label baseline level minimizes the difficulty to interpret data from patients who switched over from placebo-to-belimumab with a different exposure duration than those in the belimumab-to-belimumab group. Additionally, the treatment failure criterion was only applicable to the double-blind phase and was not adjudicated in the open-label phase.
The apparent improvement in primary efficacy renal response and complete renal response in placebo-to-belimumab patients suggests that the addition of belimumab may benefit patients treated with standard therapy who did not respond completely. The relatively short duration of the open-label phase may not have allowed adequate time for appreciable benefit to be derived among those who transitioned from placebo. We speculate that longer duration on belimumab would have allowed the placebo-to-belimumab patients to “catch up” with those who were given belimumab from the beginning of the double-blind phase. The small change in belimumab-to-belimumab patients may also be expected, but importantly, responders in the belimumab-to-belimumab group did not lose renal responses.
In conclusion, treatment with belimumab was well tolerated, with no new safety findings identified during this 28-week open-label phase of the BLISS-LN study. These data suggest that continuation or initiation of belimumab in addition to standard therapy at 104 weeks can be beneficial in patients with lupus nephritis.
Disclosures
G. Contreras reports consultancy agreements with Aurinia, GSK, and Roche; research funding from GSK USA, the Immunotolerance Network of the National Institutes of Health (NIH), and NIH SPRINT as an investigator; honoraria from Aurinia, GSK, and Roche; grant/research and consulting fees support from Genentech and Merck; and advisory or leadership roles with Aurinia, GSK, and Roche. P. Curtis is an employee of GSK and hold stocks and shares in the company. R. Furie reports employment with Northwell Health, consultancy agreements with GSK, research funding from GSK, and speakers bureau for AstraZeneca. Y. Green is an employee of GSK and hold stocks and shares in the company. F. Houssiau reports consultancy agreements with GSK and IDORSIA, research funding from GSK and UCB, and honoraria from GSK (ad board) and OTSUKA (ad board). A. Madan was an employee of GSK at the time of this study and reports employment with Danik Innovations and GSK and ownership interest in GSK. M. Okily is an employee of GSK and hold stocks and shares in the company. D.A. Roth is an employee of GSK and hold stocks and shares in the company. B.H. Rovin reports consultancy agreements with Alexion, AstraZeneca, Aurinia, Biocryst, Biogen, BMS, Calliditas, Chemocentryx, Corrona EMD-Serono/Merck, Exagen, Galapagos, Genentech, Horizon, Human Genome Sciences (GSK), Idorsia, Janssen, MedImmune, Morphosys, Novartis, Omeros, Otsuka, Resonance, Retrophin, RILITE Foundation, Roche, and Vistera; research funding from Biogen; honoraria from Alexion, AstraZeneca, Aurinia, Biocryst, Biogen, BMS, Calliditas, Chemocentryx, Corrona EMD-Serono/Merck, Exagen, Galapagos, Genentech, Horizon, Human Genome Sciences (GSK), Idorsia, Janssen, MedImmune, Morphosys, Novartis, Omeros, Otsuka, Resonance, Retrophin, RILITE Foundation, Roche, and Vistera; advisory or leadership roles for the American Society of Nephrology (ASN) Kidney Week, CureGN, Kidney Disease Improving Global Outcomes, Kidney International, Kidney International Reports, the Lupus Foundation of America, Nephrology Dialysis and Transplantation, and UpToDate; and work with ASN (mostly educational courses), International Society of Nephrology, Lupus Foundation of America, and the National Kidney Foundation. Y.K.O. Teng reports consultancy agreements with AstraZeneca, Aurinia Pharmaceuticals, GSK, KezarBio, Novartis, Otsuka Pharmaceuticals, and Vifor Pharma; research funding from Aurinia Pharmaceuticals, GSK, and ViforPharma; and serving on the editorial board of Rheumatology.
Funding
This study was funded by GSK (GSK study BEL114054).
Supplementary Material
Acknowledgments
The authors thank the participating patients and their families, clinicians, and study investigators. Medical writing support was provided by Olga Conn of Fishawack Indicia Ltd., United Kingdom (part of Fishawack Health) and was funded by GSK.
Elements of these data were presented at the following congresses: the European Renal Association 58th Congress with the European Dialysis and Transplant Association (16) and the European Alliance of Associations for Rheumatology 2021 E-Congress (17).
GSK was involved in the study design; collection, analysis, and interpretation of data; and publication development.
The views expressed in this paper are those of the authors and not necessarily of the authors’ organizations. The paper is intended to help inform and stimulate discussion.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “The Role of Anti-B Cell Activating Factor Therapy for Treating Lupus Nephritis,” on pages 1583–1585.
Author Contributions
R. Furie, Y. Green, and D.A. Roth conceptualized the study; G. Contreras, R. Furie, F. Houssiau, B.H. Rovin, and Y.K.O. Teng were responsible for data curation; G. Contreras, R. Furie, F. Houssiau, B.H. Rovin, and Y.K.O. Teng were responsible for investigation; P. Curtis, Y. Green, A. Madan, M. Okily, and D.A. Roth were responsible for formal analysis; B.H. Rovin was responsible for resources; and G. Contreras, P. Curtis, R. Furie, Y. Green, F. Houssiau, A. Madan, M. Okily, D.A. Roth, B.H. Rovin, and Y.K.O. Teng reviewed and edited the manuscript.
Data Sharing Statement
Anonymized patient data from this study, study protocol, and study report are available at the GSK study register (https://www.gsk-studyregister.com/en/trial-details/?id=114054). GSK is committed to publicly disclosing the results of GSK-sponsored clinical research that evaluates GSK medicines and, as such, was involved in the decision to submit the results of this study. Anonymized individual patient data and study documents can be requested for further research from www.clinicalstudydatarequest.com.
Supplemental Material
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.02520322/-/DCSupplemental.
Supplemental Material. Withdrawal criteria.
Supplemental Table 1. Double-blind phase baseline characteristics for patients enrolled in the open-label phase and the overall population of the double-blind phase (modified intention-to-treat population).
Supplemental Material. Treatment failures and discontinuations among non-responders for Primary Efficacy Renal Response and Complete Renal Response (based on the double-blind phase criteria; post hoc analyses).
References
- 1.Hanly JG, O’Keeffe AG, Su L, Urowitz MB, Romero-Diaz J, Gordon C, Bae SC, Bernatsky S, Clarke AE, Wallace DJ, Merrill JT, Isenberg DA, Rahman A, Ginzler EM, Fortin P, Gladman DD, Sanchez-Guerrero J, Petri M, Bruce IN, Dooley MA, Ramsey-Goldman R, Aranow C, Alarcón GS, Fessler BJ, Steinsson K, Nived O, Sturfelt GK, Manzi S, Khamashta MA, van Vollenhoven RF, Zoma AA, Ramos-Casals M, Ruiz-Irastorza G, Lim SS, Stoll T, Inanc M, Kalunian KC, Kamen DL, Maddison P, Peschken CA, Jacobsen S, Askanase A, Theriault C, Thompson K, Farewell V: The frequency and outcome of lupus nephritis: Results from an international inception cohort study. Rheumatology (Oxford) 55: 252–262, 2016. 10.1093/rheumatology/kev311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahajan A, Amelio J, Gairy K, Kaur G, Levy RA, Roth D, Bass D: Systemic lupus erythematosus, lupus nephritis and end-stage renal disease: A pragmatic review mapping disease severity and progression. Lupus 29: 1011–1020, 2020. 10.1177/0961203320932219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tektonidou MG, Dasgupta A, Ward MM: Risk of end-stage renal disease in patients with lupus nephritis, 1971–2015: A systematic review and Bayesian meta-analysis. Arthritis Rheumatol 68: 1432–1441, 2016. 10.1002/art.39594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baker KP, Edwards BM, Main SH, Choi GH, Wager RE, Halpern WG, Lappin PB, Riccobene T, Abramian D, Sekut L, Sturm B, Poortman C, Minter RR, Dobson CL, Williams E, Carmen S, Smith R, Roschke V, Hilbert DM, Vaughan TJ, Albert VR: Generation and characterization of LymphoStat-B, a human monoclonal antibody that antagonizes the bioactivities of B lymphocyte stimulator. Arthritis Rheum 48: 3253–3265, 2003. 10.1002/art.11299 [DOI] [PubMed] [Google Scholar]
- 5.European Medicines Agency : Belimumab Summary of Product Characteristics. Available at: https://www.ema.europa.eu/en/documents/product-information/benlysta-epar-product-information_en.pdf. Accessed January 10 2022
- 6.US Food and Drug Administration : Belimumab 2021. Prescribing Information, 2019. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/125370s064,761043s007lbl.pdf. Accessed January 10 2022
- 7.Furie R, Rovin BH, Houssiau F, Malvar A, Teng YKO, Contreras G, Amoura Z, Yu X, Mok CC, Santiago MB, Saxena A, Green Y, Ji B, Kleoudis C, Burriss SW, Barnett C, Roth DA: Two-year, randomized, controlled trial of belimumab in lupus nephritis. N Engl J Med 383: 1117–1128, 2020. 10.1056/NEJMoa2001180 [DOI] [PubMed] [Google Scholar]
- 8.GSK : FDA approves GSK’s belimumab as the first medicine for adult patients with active lupus nephritis in the US, 2020. Available at: https://www.gsk.com/en-gb/media/press-releases/fda-approves-gsk-s-benlysta-as-the-first-medicine-for-adult-patients-with-active-lupus-nephritis-in-the-us/#. Accessed October 21 2021
- 9.GSK : European Commission approves Benlysta for adult patients with active lupus nephritis, 2021. Available at: https://www.gsk.com/en-gb/media/press-releases/european-commission-approves-benlysta-for-adult-patients-with-active-lupus-nephritis/. Accessed October 22 2021
- 10.Hochberg MC: Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40: 1725, 1997. 10.1002/art.1780400928 [DOI] [PubMed] [Google Scholar]
- 11.Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ: The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25: 1271–1277, 1982. 10.1002/art.1780251101 [DOI] [PubMed] [Google Scholar]
- 12.Markowitz GS, D’Agati VD: The ISN/RPS 2003 classification of lupus nephritis: An assessment at 3 years. Kidney Int 71: 491–495, 2007. 10.1038/sj.ki.5002118 [DOI] [PubMed] [Google Scholar]
- 13.Doria A, Bass D, Schwarting A, Hammer A, Gordon D, Scheinberg M, Fox NL, Groark J, Stohl W, Kleoudis C, Roth D: A 6-month open-label extension study of the safety and efficacy of subcutaneous belimumab in patients with systemic lupus erythematosus. Lupus 27: 1489–1498, 2018. 10.1177/0961203318777634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Vollenhoven RF, Navarra SV, Levy RA, Thomas M, Heath A, Lustine T, Adamkovic A, Fettiplace J, Wang ML, Ji B, Roth D: Long-term safety and limited organ damage in patients with systemic lupus erythematosus treated with belimumab: A phase III study extension. Rheumatology (Oxford) 59: 281–291, 2020. 10.1093/rheumatology/kez279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wallace DJ, Ginzler EM, Merrill JT, Furie RA, Stohl W, Chatham WW, Weinstein A, McKay JD, McCune WJ, Petri M, Fettiplace J, Roth DA, Ji B, Heath A: Safety and efficacy of belimumab plus standard therapy for up to thirteen years in patients with systemic lupus erythematosus. Arthritis Rheumatol 71: 1125–1134, 2019. 10.1002/art.40861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rovin B, Furie R, Houssiau FA, Contreras G, Teng YKO, Curtis P, Madan A, Jones-Leone A, Gonzalez-Rivera T, Okily M, Roth D: Safety and efficacy of intravenous belimumab in patients with lupus nephritis: A 6-month open-label extension. Nephrol Dial Transplant 36[Suppl 1]: gfab121.003, 2021 [Google Scholar]
- 17.Furie R, Rovin BH, Houssiau F, Contreras G, Curtis P, Madan A, Jones-Leone A, Okily M, Roth D: A 6-month open-label extension study of the safety and efficacy of intravenous belimumab in patients with lupus nephritis. Ann Rheum Dis 80[Suppl 1]: 591–592, 2021. 33243781 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.