Abstract
Objective
To identify post-operative risk factors for the development of chronic pain after knee replacement.
Design
Primary knee replacements in persons aged ≥18 years between April 2008 and December 2016 from the National Joint Registry, linked with English Hospital Episode Statistics data, and Patient Reported Outcome Measures. The outcome was chronic pain 6-months after surgery (Oxford Knee pain score). Logistic regression modelling identified risk factors for chronic pain outcome.
Results
258,386 patients; 56.7% women; average age 70.1 years (SD ± 8.8 years). 43,702 (16.9%) were identified as having chronic pain 6-months post-surgery. Within 3 months of surgery complications were uncommon: intra-operative complications 1224 (0.5%); ≥1 medical complication 6073 (2.4%)); 32,930 (12.7%) hospital readmissions; 3848 (1.5%) re-operation; 835 (0.3%) revision. Post-surgical risk factors of chronic pain were: mechanical complication of prosthesis odds ratio (OR) 1.56 (95% Confidence Interval 1.35, 1.80); surgical site infection OR 1.13 (0.99, 1.29); readmission OR 1.47 (1.42, 1.52); re-operation OR 1.39 (1.27, 1.51); revision OR 1.92 (1.64, 2.25); length of stay e.g. 6+ vs. <2 days OR 1.48 (1.35, 1.63), blood transfusion OR 0.47 (0.26, 0.86) and myocardial infarction OR 0.69 (0.49, 0.97). Discriminatory ability of the model was only fair (c-statistic 0.71) indicating that post-surgical predictors explain a limited amount of variability in chronic pain.
Conclusions
We identified a number of post-operative factors relating to the operation and early recovery that are associated with chronic pain following primary knee replacement. The model had weak discriminatory ability indicating that there remains considerable unexplained variability in chronic pain outcome.
Keywords: Knee replacement, Osteoarthritis, Epidemiology, Patient outcomes, Pain
1. Introduction
Osteoarthritis is a leading cause of pain and disability worldwide. For patients who have osteoarthritis and severe knee pain that has not responded adequately to conservative treatments, primary knee replacement is performed, with over 100,000 operations in the United Kingdom (UK) [1] and 1,000,000 in the United States (US) [2] each year. These numbers are projected to increase given an increasingly ageing and obese population [3].
After a knee replacement, improvements in pain usually stabilise at approximately three months after surgery, while physical function continues to improve to 12 months post-operatively with most benefit observed in the initial six month period [4]. Although many patients report good outcomes after knee replacement, best quality studies indicate that around 20% of patients experience chronic post-surgical pain [5], defined as pain persisting three months or longer after surgery. Based on current figures for knee replacement, around 20,000 new patients in the UK (200,000 in the US) per year will experience chronic pain afterwards. The yearly costs of knee replacement has been estimated at over £1 million in the UK [6] and exceeds $10 billion in the US [7]. Although the costs of knee replacement are significant, this is a very cost-effective procedure compared to no joint surgery in individuals with osteoarthritis [7,8]. Furthermore, it has been shown to be cost-effective even in patients with mild symptoms of pre-operative pain [9]. More generally, it is known that chronic pain has individual and societal impacts, including reduced function, increased psychological distress, reduced quality of life, and reduced participation in social life and employment [10].
There is a wide body of research exploring risk factors of patient outcomes following knee replacement surgery [11]. Pre-operative factors age [12], gender [13], obesity [14], social deprivation [15] and co-morbidity [16] (including multi-joint osteoarthritis [17]) are known to influence the surgical outcome, as does having an uni-compartmental knee replacement [18]. Most studies have focused on total scores encompassing several outcome domains, and there is limited research focusing solely on pain status [15]. The majority of studies have focused on pre-operative risk factors, but much less is known about risk factors that occur post-operatively [19]. The current extent of research into post-operative risk factors is limited and further research is needed [20].
The causes of chronic pain after knee replacement are currently poorly understood although they are believed to be multifactorial in origin with biological, psychological and surgical aspects [21]. Knowledge of determinants of poor outcomes is crucial to help guide intervention development to help target these cohorts of patients. Post-operative risk factors are important because the time after surgery may present an ideal opportunity for targeted intervention to prevent the persistence or worsening of pain.
Our study investigates intra-operative and post-surgical risk factors in the development of chronic pain in 258,386 patients with knee replacements using data from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man (NJR).
2. Methods
2.1. Study design
We conducted a retrospective observational study using anonymised depersonalised data from the NJR.
2.2. Population and data source
The NJR contains data on over 1 million knee replacement surgeries since 2003, covering 96% of primary knee replacements [1]. Primary operations were linked with English Hospital Episode Statistics (HES) data, which contains records of all inpatient episodes undertaken in NHS Trusts in England (125 million each year). In turn, primary knee replacements were linked to Patient Reported Outcome Measures (PROMs). Patients funded by the NHS in England are requested to complete questionnaires before and 6 months after surgery to evaluate improvement in health as perceived by the patients themselves. A cohort of patients undergoing elective total or unicompartmental knee replacement (TKR/UKR) in England, UK, was retrieved for the period April 2008 to December 2016. Patients are included in the study if they have linked data from the NJR-HES-PROMs databases and have completed the 6-month post-operative Oxford Knee scores.
2.3. Main outcome measure
The International Association for the Study of Pain (IASP) defines chronic post-surgical pain as pain that persists beyond the healing process, i.e. at least three months after surgery [22]. For this study, using routinely collected data, information on post-operative pain was assessed using the 6-month post-operative Oxford Knee score (OKS). Pain and function-related subscales within the OKS have been identified and validated [23]. An OKS pain subscale (OKS-PS) summary score can be calculated, ranging from 0 (most pain) to 28 (least pain), by summing the responses of the 7 OKS items related to the pain subscale. We have previously shown that patients with OKS-PS scores of 14 or less at six months after knee replacement can be considered to be in chronic pain that is likely to affect their quality of life negatively [24]. We used chronic pain at six months after surgery as the main outcome.
2.4. Exposure variables
Our interest is in surgical complications and post-operative risk factors of outcome that occur from the time of primary operation up to 3-months after surgery.
Length of hospital stay (LOS) was calculated as the number of days between the hospital admission and discharge date. Intra-operative surgical complications are recorded at the time of primary surgery within the NJR and include fracture, ligament avulsion and tendon damage. We identified medical complications within 3-months of surgery from the HES database. We defined complications as one or more events happening after the operation from the following list: stroke (excluding mini stroke), respiratory infection, acute myocardial infarction, pulmonary embolism/deep vein thrombosis, urinary tract infection, wound disruption, surgical site infection, fracture after surgery, complication of prosthesis, neurovascular injury, acute renal failure and blood transfusion. We identified these complications in HES data using diagnosis codes of the “International Statistical Classification of Diseases and Related Health Problems 10th Revision” (ICD-10) except for blood transfusion for which we used the “Classification of Interventions and Procedures version 4” (OPCS-4) codes since this is a procedure.
Revisions were identified from the NJR and HES records as any procedure involving the removal, addition or exchange of knee replacement components from the primary knee replacement procedure. Reoperations were identified from HES data and included any additional procedures after the primary knee replacement operation not meeting the revision definition specified. These included manipulation under anaesthetic (MUA), arthroscopic surgery, ligament repairs and surgical debridement.
2.5. Pre-operative demographic variables
Demographic information included age, sex, body mass index (BMI), American Society of Anaesthesiologists (ASA) grade, Index of Multiple Deprivation (IMD).
2.6. Statistical analysis
Descriptive statistics were used to describe the data with mean (standard deviation) for continuous variables, and number (percentage) for categorical variables. To assess for potential responder bias, the demographic characteristics of patients included in the analysis with a complete 6-month post-operative OKS-PS, are compared to all patients with baseline data (Table 1).
Table 1.
Descriptive demographic characteristics, comparing patients included in the analysis with a 6-month post-operative OKS, with all patients with baseline data.
| All patients |
Included in analysis (Post op OKS-PS) |
Excluded from analysis |
|
|---|---|---|---|
| N = 531,790 | N = 258,386 | N = 273,404 | |
| Year of primary | |||
| 2007 & 2008 | 34,151 (6.4%) | 3764 (1.5%) | 30,387 (11.1%) |
| 2009 | 46,857 (8.8%) | 19,048 (7.4%) | 27,809 (10.2%) |
| 2010 | 53,145 (10.0%) | 30,240 (11.7%) | 22,905 (8.4%) |
| 2011 | 57,256 (10.8%) | 33,775 (13.1%) | 23,481 (8.6%) |
| 2012 | 60,696 (11.4%) | 35,703 (13.8%) | 24,993 (9.1%) |
| 2013 | 62,168 (11.7%) | 37,807 (14.6%) | 24,361 (8.9%) |
| 2014 | 69,697 (13.1%) | 41,780 (16.2%) | 27,917 (10.2%) |
| 2015 | 70,908 (13.3%) | 40,563 (15.7%) | 30,345 (11.1%) |
| 2016 | 72,304 (13.6%) | 15,264 (5.9%) | 57,040 (20.9%) |
| 2017 | 4608 (0.9%) | 442 (0.2%) | 4166 (1.5%) |
| Age at primary knee replacement | 69.7 (SD 9.4) | 70.1 (SD 8.8) | 69.4 (SD 9.9) |
| Sex | |||
| Female | 301,224 (56.6%) | 146,510 (56.7%) | 154,714 (56.6%) |
| Male | 230,566 (43.4%) | 43.36 (100.0%) | 118,690 (43.4%) |
| Body mass index | 31.0 (SD 5.5) | 31.0 (SD 5.4) | 30.9 (SD 5.5) |
| Index of Multiple Deprivation (IMD) quintiles | |||
| Most deprived | 77,215 (14.5%) | 34,653 (13.4%) | 42,562 (15.6%) |
| 2 | 96,500 (18.2%) | 45,298 (17.5%) | 51,202 (18.7%) |
| 3 | 116,429 (21.9%) | 57,301 (22.2%) | 59,128 (21.6%) |
| 4 | 121,791 (22.9%) | 61,262 (23.7%) | 60,529 (22.1%) |
| Least deprived | 114,664 (21.6%) | 57,251 (22.2%) | 57,413 (21.0%) |
| ASA grade | |||
| P1 - Fit and healthy | 51,437 (9.7%) | 23,717 (9.2%) | 27,720 (10.1%) |
| P2 - Mild disease not incapacitating | 392,501 (73.8%) | 194,989 (75.5%) | 197,512 (72.2%) |
| P3 - Incapacitating systemic disease | 86,314 (16.2%) | 39,061 (15.1%) | 47,253 (17.3%) |
| P4 – P5 - Life threatening disease/Expected to die within 24 h s | 1538 (0.3%) | 619 (0.2%) | 919 (0.3%) |
The primary outcome is a binary variable of whether or not a patient had chronic pain at 6-months after surgery. The main exposures of interest are the surgical complications, length of hospital stay, and post-operative risk factors that occurred within 3-months of surgery (complications, readmission, reoperation, revision surgery). Confounding factors included the pre-operative OKS-PS, age, sex, body mass index (BMI), American Society of Anaesthesiologists (ASA) grade, Index of Multiple Deprivation (IMD). Missing data for the variables included in the analysis is described in Table 2, where all variables had <1% missing data with the exception of BMI with 26.6% missing data. Logistic regression modelling was used to identify predictors of the binary outcome of chronic pain at 6-months after surgery, adjusting for pre-operative OKS. Univariable analyses compare the association of each exposure with the outcome of interest. Multivariable models are then fitted, adjusting for: a) all post-operative risk factors, b) pre-operative demographic confounding variables. Fractional polynomial regression modelling was used to test the assumption of linearity of continuous variables with outcome. Where there was evidence of a non-linear association, variables were categorised. The area under the Receiver Operating Characteristic (ROC) curve was used as a measure of the predictive ability of the model (discrimination).
Table 2.
Summary of pre-operative OKS, post-operative factors, and demographic confounding factors, in the pain free and chronic pain groups from the NJR-HES dataset.
| Parameter | Whole cohort |
No chronic pain |
Chronic pain |
|---|---|---|---|
| (n = 258,386) | (n = 214,684) | (n = 43,702) | |
| Preoperative OKS | 9.22 points (SD 4.64) | 9.76 points (SD 4.58) | 6.59 points (SD 4.02) |
| 0 to 4 | 42,331 (16.51%) | 27,411 (12.87%) | 14,920 (34.40%) |
| 5 to 7 | 56,918 (22.21%) | 44,483 (20.89%) | 12,435 (28.67%) |
| 8 to 9 | 40,513 (15.81%) | 34,197 (16.06%) | 6316 (14.56%) |
| 10 to 12 | 54,570 (21.29%) | 48,667 (22.85%) | 5903 (13.61%) |
| 13 to 28 | 61,990 (24.18%) | 58,198 (27.33%) | 3792 (8.74%) |
| Missing | 2064 (0.80%) | ||
|
Demographics | |||
| Age | |||
| <50 | 3398 (1.32%) | 2214 (1.03%) | 1184 (2.71%) |
| 50–59 | 26,977 (10.44%) | 19,792 (9.22%) | 7185 (16.44%) |
| 60–69 | 88,496 (34.25%) | 72,782 (33.90%) | 15,714 (35.96%) |
| 70–79 | 101,536 (39.30%) | 86,926 (40.49%) | 14,610 (33.43%) |
| 80–84 | 27,099 (10.49%) | 23,549 (10.97%) | 3550 (8.12%) |
| 85+ | 10,880 (4.21%) | 9421 (4.39%) | 1459 (3.34%) |
| Missing | 0 (0.00%) | ||
| Sex | |||
| Female | 146,510 (56.70%) | 120,758 (56.25%) | 25,752 (58.93%) |
| Male | 111,876 (43.30%) | 93,926 (43.75%) | 17,950 (41.07%) |
| Missing | 0 (0.00%) | ||
| BMI | |||
| Underweight | 231 (0.12%) | 194 (0.12%) | 37 (0.12%) |
| Normal | 17,000 (8.96%) | 14,948 (9.42%) | 2052 (6.58%) |
| Overweight | 64,509 (33.99%) | 56,098 (35.37%) | 8411 (26.99%) |
| Obese class 1 (30–34.9) | 62,736 (33.06%) | 52,243 (32.94%) | 10,493 (33.67%) |
| Obese class II (35–39.9) | 32,018 (16.87%) | 25,279 (15.94%) | 6739 (21.62%) |
| Obese class 3 (40+) | 13,289 (7.00%) | 9856 (6.21%) | 3433 (11.02%) |
| Missing | 68,603 (26.55%) | ||
| ASA grade | |||
| P1 - Fit and healthy | 23,717 (9.18%) | 20,534 (9.56%) | 3183 (7.28%) |
| P2 - Mild disease not incapacitating | 194,989 (75.46%) | 163,452 (76.14%) | 31,537 (72.16%) |
| P3 - Incapacitating systemic disease | 39,061 (15.12%) | 30,238 (14.08%) | 8823 (20.19%) |
| P4 – P5 - Life threatening disease/Expected to die within 24 h s | 619 (0.24%) | 460 (0.21%) | 159 (0.36%) |
| Missing | 0 (0.00%) | ||
| Index of Multiple Deprivation (IMD) quintiles | |||
| Most deprived | 34,653 (13.55%) | 25,171 (11.85%) | 9482 (21.89%) |
| 2 | 45,298 (17.71%) | 36,011 (16.95%) | 9287 (21.44%) |
| 3 | 57,301 (22.40%) | 48,094 (22.64%) | 9207 (21.26%) |
| 4 | 61,262 (23.95%) | 52,813 (24.86%) | 8449 (19.51%) |
| Least deprived | 57,251 (22.38%) | 50,360 (23.70%) | 6891 (15.91%) |
| Missing | 2621 (1.01%) | ||
| 3 month complications | |||
| Blood transfusion | 90 (0.03%) | 77 (0.04%) | 13 (0.03%) |
| Acute renal failure | 632 (0.24%) | 477 (0.22%) | 155 (0.35%) |
| Neurovascular injury | 22 (0.01%) | 17 (0.01%) | 5 (0.01%) |
| Mechanical complication of prosthesis | 1050 (0.41%) | 658 (0.31%) | 392 (0.90%) |
| Fracture | 37 (0.01%) | 27 (0.01%) | 10 (0.02%) |
| Surgical site infection | 1268 (0.49%) | 901 (0.42%) | 367 (0.84%) |
| Wound disruption | 646 (0.25%) | 475 (0.22%) | 171 (0.39%) |
| Urinary tract infection | 873 (0.34%) | 639 (0.30%) | 234 (0.54%) |
| DVT/PE | 786 (0.30%) | 602 (0.28%) | 184 (0.42%) |
| Acute MI | 271 (0.10%) | 229 (0.11%) | 42 (0.10%) |
| Respiratory tract infection | 1003 (0.39%) | 763 (0.36%) | 240 (0.55%) |
| Stroke | 180 (0.07%) | 144 (0.07%) | 36 (0.08%) |
| 3 month readmissions | 32,930 (12.74%) | 24,877 (11.59%) | 8053 (18.43%) |
| 3 month reoperations | 3848 (1.49%) | 2718 (1.27%) | 1130 (2.59%) |
| 3 month revision | 835 (0.32%) | 528 (100.00%) | 307 (0.70%) |
| Surgical complication 1 or greater | 1224 (0.47%) | 972 (0.45%) | 252 (0.58%) |
| Length of stay (continuous) | 4.58 days (SD 3.27) | 4.45 days (SD 3.19) | 5.19 days (SD 3.57) |
| <2 days | 3831 (1.48%) | 3226 (1.50%) | 605 (1.38%) |
| 2–4 days | 97,795 (37.85%) | 84,510 (39.37%) | 13,285 (30.40%) |
| 4–6 days | 99,385 (38.47%) | 82,978 (38.65%) | 16,407 (37.54%) |
| 6 plus days | 57,362 (22.20%) | 43,958 (20.48%) | 13,404 (30.67%) |
| Missing | 13 (0.01%) | ||
Analyses were conducted using Stata version 15.1 statistical software (StataCorp, College Station, Texas). We followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guideline to report our study.
3. Results
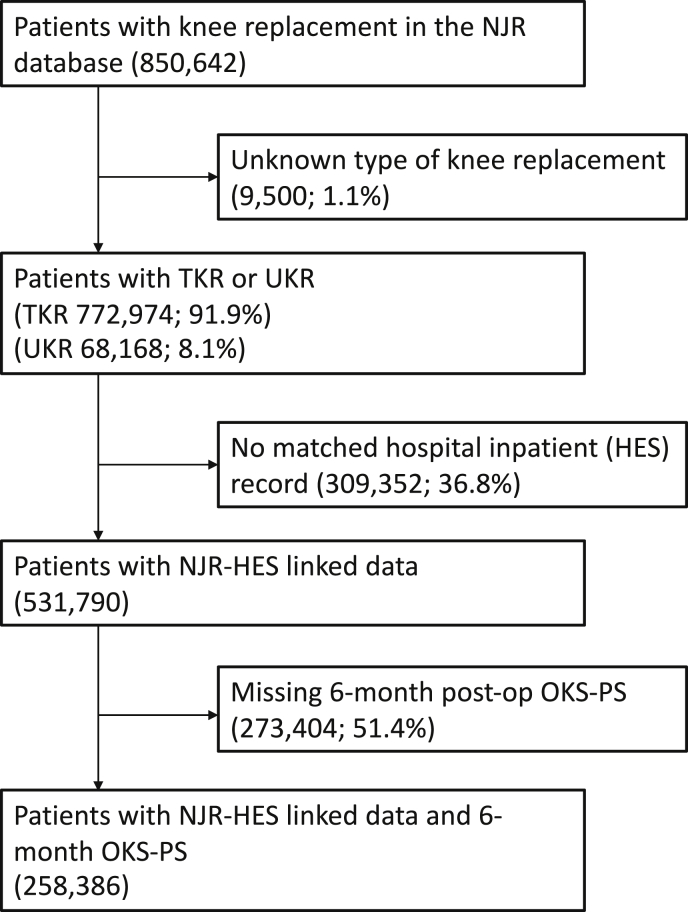
Fig. 1 describes the flow diagram of patients included within the study. Patients were included in analysis if they had a knee replacement (total or uni-compartmental), with linkage to English (HES) data, and linked PROMS data with a complete 6-month OKS-PS. Within the NJR-HES-PROMs linked dataset there were 258,386 patients with a 6-month OKS-PS. Table 1 describes descriptive demographic characteristics of patients with a complete 6-month follow up OKS, to those with baseline data. Characteristics of patients were similar comparing those included versus excluded from analysis. 56.7% of patients were women; the average age was 70.1 years (SD ± 8.8 years). 43,702 (16.9%) patients were identified as having chronic pain at 6-months post-surgery with the remaining 214,684 (83.1%) not having pain. The pre-operative OKS pain score, number of complications within three months of surgery, LOS, and demographic confounding factors in each group are summarised in Table 2.
Fig. 1.
Patient flow diagram.
221,354 (85.7%) met the definition of chronic knee pain pre-operatively. Of these patients, 179,699 (81.2%) no longer had chronic pain 6-months after surgery, but 41,655 (18.8%) still had chronic knee pain. 37,032 (14.3%) did not have pre-operative chronic knee pain, and of these patients although 34,985 (94.5%) still had no chronic pain at 6-months, importantly 2047 (5.5%) went on to develop chronic knee pain following surgery.
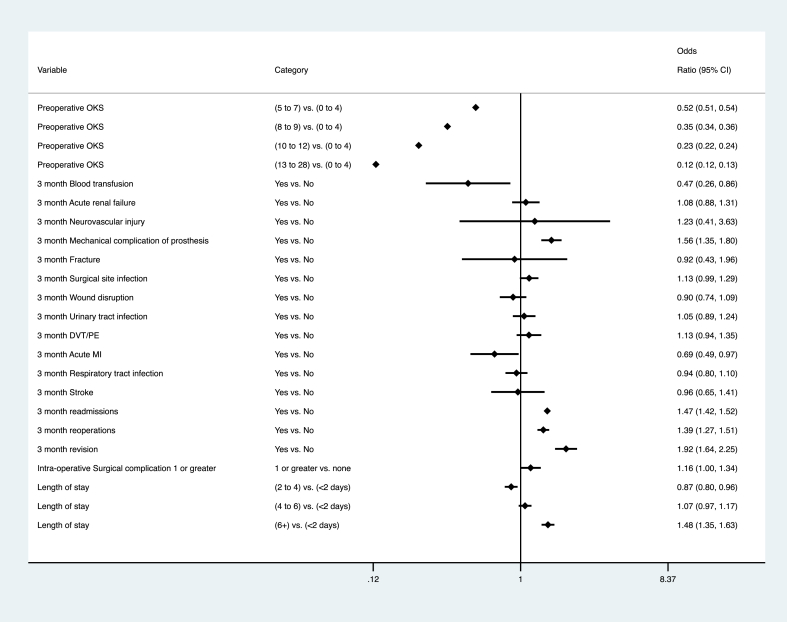
Fig. 2 describes the results of the multivariable logistic regression including all post-operative risk factors and adjusting for the pre-operative OKS-PS. Patients having a better pre-operative OKS were less likely to report chronic pain e.g. (13–28) vs. (0–4) odds ratio (OR) 0.12 (95% Confidence Interval 0.12, 0.13). Complications within three months of surgery that were predictors of chronic pain were: mechanical complication of prosthesis OR 1.56 (1.35, 1.80); surgical site infection OR 1.13 (0.99, 1.29); readmission OR 1.47 (1.42, 1.52); re-operation OR 1.39 (1.27, 1.51); revision OR 1.92 (1.64, 2.25); length of stay, e.g. 6+ vs. <2 days OR 1.48 (1.35, 1.63).
Fig. 2.
Forest plot describing logistic regression model results controlling for pre-operative OKS and post-operative risk factors.
Complications within three months of surgery that did not predispose to chronic pain included: acute renal failure, neurovascular injury, fracture, surgical site infections, wound disruption, urinary tract infections, DVTs/PEs, respiratory tract infections, stroke and NJR reported complications. Blood transfusions OR 0.47 (0.26, 0.86) and myocardial infarction OR 0.69 (0.49, 0.97) were less common in the chronic pain group than the rest of the cohort.
Models were further adjusted to control for demographic confounding factors (Table 3). All demographic confounding factors were significantly association with chronic pain, where those of younger age, males, obese patients, higher morbidity ASA grade, and those living in the most deprived areas, were more likely to have chronic knee pain. Adjusting for confounding factors did not change the effect of re-operations, revisions, readmissions and LOS, but some associations changed for the following complications: fracture OR 0.22 (0.05, 0.98); urinary tract infection OR 1.26 (1.04, 1.53); myocardial infarction OR 0.81 (0.56, 1.19).
Table 3.
Results of the logistic regression describing crude univariable model and models adjusting for pre-operative OKS, post-operative factors, and pre-operative demographic characteristics.
| Parameter | Crude Models |
Adjusted model 1 (N = 256,309) |
Adjusted model 2 (N = 187,054) |
|||
|---|---|---|---|---|---|---|
| Odds Ratio (OR) 95% Confidence Interval (CI) | P-value | Odds Ratio (OR) 95% Confidence Interval (CI) | P-value | Odds Ratio (OR) 95% Confidence Interval (CI) | P-value | |
| Preoperative OKS | ||||||
| 0 to 4 | REF | REF | REF | |||
| 5 to 7 | 0.51 (0.50, 0.53) | <0.001 | 0.52 (0.51, 0.54) | <0.001 | 0.56 (0.54, 0.57) | <0.001 |
| 8 to 9 | 0.34 (0.33, 0.35) | <0.001 | 0.35 (0.34, 0.36) | <0.001 | 0.39 (0.38, 0.41) | <0.001 |
| 10 to 12 | 0.22 (0.22, 0.23) | <0.001 | 0.23 (0.22, 0.24) | <0.001 | 0.27 (0.26, 0.28) | <0.001 |
| 13 to 28 | 0.12 (0.12, 0.12) | <0.001 | 0.12 (0.12, 0.13) | <0.001 | 0.16 (0.15, 0.16) | <0.001 |
|
Demographics | ||||||
| Age | ||||||
| <50 | 3.18 (2.96, 3.42) | <0.001 | 2.37 (2.16, 2.61) | <0.001 | ||
| 50–59 | 2.16 (2.09, 2.23) | <0.001 | 1.78 (1.71, 1.86) | <0.001 | ||
| 60–69 | 1.28 (1.25, 1.32) | <0.001 | 1.22 (1.19, 1.26) | <0.001 | ||
| 70–79 | REF | REF | ||||
| 80–84 | 0.90 (0.86, 0.93) | <0.001 | 0.85 (0.80, 0.89) | <0.001 | ||
| 85+ | 0.92 (0.87, 0.98) | 0.006 | 0.75 (0.70, 0.81) | <0.001 | ||
| Sex | ||||||
| Female | REF | REF | ||||
| Male | 0.90 (0.88, 0.92) | <0.001 | 1.14 (1.11, 1.17) | <0.001 | ||
| BMI | ||||||
| Underweight | 1.39 (0.97, 1.98) | 0.069 | 0.98 (0.67, 1.43) | 0.918 | ||
| Normal | REF | REF | ||||
| Overweight | 1.09 (1.04, 1.15) | 0.001 | 1.04 (0.99, 1.10) | 0.154 | ||
| Obese class 1 (30–34.9) | 1.46 (1.39, 1.54) | <0.001 | 1.17 (1.11, 1.24) | <0.001 | ||
| Obese class II (35–39.9) | 1.94 (1.84, 2.05) | <0.001 | 1.28 (1.21, 1.35) | <0.001 | ||
| Obese class 3 (40+) | 2.54 (2.39, 2.70) | <0.001 | 1.27 (1.19, 1.36) | <0.001 | ||
| ASA grade | ||||||
| P1 - Fit and healthy | 0.80 (0.77, 0.84) | <0.001 | 0.82 (0.78, 0.87) | <0.001 | ||
| P2 - Mild disease not incapacitating | REF | REF | ||||
| P3 - Incapacitating systemic disease | 1.51 (1.47, 1.55) | <0.001 | 1.21 (1.17, 1.25) | <0.001 | ||
| P4 – P5 - Life threatening disease/Expected to die within 24 h s | 1.79 (1.50, 2.15) | <0.001 | 1.16 (0.92, 1.46) | 0.215 | ||
| Index of Multiple Deprivation (IMD) quintiles | ||||||
| Most deprived |
REF |
REF |
||||
| 2 | 0.68 (0.66, 0.71) | <0.001 | 0.76 (0.73, 0.80) | <0.001 | ||
| 3 | 0.51 (0.49, 0.52) | <0.001 | 0.62 (0.60, 0.65) | <0.001 | ||
| 4 | 0.42 (0.41, 0.44) | <0.001 | 0.56 (0.54, 0.58) | <0.001 | ||
| Least deprived | 0.36 (0.35, 0.38) | <0.001 | 0.53 (0.50, 0.55) | <0.001 | ||
| 3 month complications | ||||||
| Blood transfusion | 0.83 (0.46, 1.49) | 0.533 | 0.47 (0.26, 0.86) | 0.015 | 0.42 (0.20, 0.86) | 0.018 |
| Acute renal failure | 1.60 (1.33, 1.92) | <0.001 | 1.08 (0.88, 1.31) | 0.455 | 1.11 (0.88, 1.40) | 0.373 |
| Neurovascular injury | 1.45 (0.53, 3.92) | 0.469 | 1.23 (0.41, 3.63) | 0.712 | 1.27 (0.36, 4.43) | 0.709 |
| Mechanical complication of prosthesis | 2.94 (2.60, 3.34) | <0.001 | 1.56 (1.35, 1.80) | <0.001 | 1.51 (1.27, 1.80) | <0.001 |
| Fracture | 1.82 (0.88, 3.76) | 0.106 | 0.92 (0.43, 1.96) | 0.822 | 0.22 (0.05, 0.98) | 0.047 |
| Surgical site infection | 2.01 (1.78, 2.27) | <0.001 | 1.13 (0.99, 1.29) | 0.072 | 1.25 (1.07, 1.47) | 0.004 |
| Wound disruption | 1.77 (1.49, 2.11) | <0.001 | 0.90 (0.74, 1.09) | 0.265 | 0.85 (0.68, 1.06) | 0.141 |
| Urinary tract infection | 1.80 (1.55, 2.10) | <0.001 | 1.05 (0.89, 1.24) | 0.541 | 1.26 (1.04, 1.53) | 0.016 |
| DVT/PE | 1.50 (1.27, 1.77) | <0.001 | 1.13 (0.94, 1.35) | 0.186 | 1.10 (0.89, 1.36) | 0.372 |
| Acute MI | 0.90 (0.65, 1.25) | 0.534 | 0.69 (0.49, 0.97) | 0.034 | 0.81 (0.56, 1.19) | 0.292 |
| Respiratory tract infection | 1.55 (1.34, 1.79) | <0.001 | 0.94 (0.80, 1.10) | 0.461 | 0.97 (0.81, 1.18) | 0.784 |
| Stroke | 1.23 (0.85, 1.77) | 0.27 | 0.96 (0.65, 1.41) | 0.841 | 1.09 (0.68, 1.72) | 0.728 |
| 3 month readmissions | 1.72 (1.68, 1.77) | <0.001 | 1.47 (1.42, 1.52) | <0.001 | 1.49 (1.44, 1.55) | <0.001 |
| 3 month reoperations | 2.07 (1.93, 2.22) | <0.001 | 1.39 (1.27, 1.51) | <0.001 | 1.29 (1.17, 1.43) | <0.001 |
| 3 month revision | 2.87 (2.49, 3.30) | <0.001 | 1.92 (1.64, 2.25) | <0.001 | 1.93 (1.59, 2.33) | <0.001 |
| Surgical complication 1 or greater | 1.28 (1.11, 1.47) | 0.001 | 1.16 (1.00, 1.34) | 0.054 | 1.09 (0.91, 1.30) | 0.366 |
| Length of stay | ||||||
| <2 days | REF | REF | REF | |||
| 2–4 days | 0.84 (0.77, 0.92) | <0.001 | 0.87 (0.80, 0.96) | 0.004 | 0.91 (0.81, 1.01) | 0.087 |
| 4–6 days | 1.05 (0.97, 1.15) | 0.241 | 1.07 (0.97, 1.17) | 0.173 | 1.16 (1.04, 1.29) | 0.009 |
| 6 plus days | 1.63 (1.49, 1.78) | <0.001 | 1.48 (1.35, 1.63) | <0.001 | 1.68 (1.50, 1.87) | <0.001 |
Predictive ability of the model to explain variation in pain outcome was moderate. For the model including only the pre-operative OKS-PS and post-operative risk factors the area under the ROC curve was 0.71. Further including pre-operative demographic factors, the area under the curve increased to 0.73, indicating that in respect of discriminatory ability, the included surgical complications, post-surgical predictors and pre-operative demographic factors explain a limited amount of variability in chronic pain outcome at six months after surgery.
4. Discussion
Most research investigating factors related to chronic knee pain after knee replacement surgery has focused on pre-operative factors, with limited research into the effect of post-operative factors. This is important given current multivariable models of pre-operative factors have poor predictive power in explaining chronic knee pain development [15]. If at-risk patients could be identified in the early post-operative period, timely interventions such as physiotherapy [25] or chronic pain care pathways [26] could prevent the development of chronic pain.
A recent systematic review looked at evidence from clinical trials on interventions after hospital discharge to reduce the severity of chronic pain after TKR [25]. The majority of these trials were comparisons of physiotherapy interventions (e.g. walking skills programme, group-based exercise classes, cycling, home-based rehabilitation, clinic-based rehabilitation, home-based exercises, aquatic therapy), although there was no evidence favouring one format of physiotherapy over another.
This study analysed post-operative predictive factors in 258,386 knee replacements performed in England. We found the following post-operative predictors of chronic pain: (1) mechanical complication of prosthesis; (2) surgical site infection; (3) readmission; (4) reoperation; (5) revision and (6) prolonged length of stay over six days. All post-operative factors with the exception of readmissions and prolonged length of stay had low incidences, meaning these would only be detected in large datasets, but would understandably not be a clinically useful chronic pain marker at a local level. This suggests that the post-operative factors explored in this analysis cannot be reliably used to identify subgroups of patients at risk of chronic pain after knee replacement.
Although many of the post-operative factors we identified, particularly medical complications, are uncommon, the aim of our study was to see whether we could use information obtained from national routinely collected data, to identify patients in the early post-operative period that may be at increased risk of chronic pain. Although these risk factors are uncommon, they are available and captured in standard routine data, making it possible to identify such patients from their medical records. Whilst these are not necessarily modifiable risk factors, they allow us to identify high risk patients early, so that we can intervene early, such as chronic pain management strategies or alternative interventions to treat chronic pain. Further, such patients who have these rare complications would not necessarily be seeking help for further pain management, particularly as they have just had surgery that was meant to treat their pain. Such patients would be brought to the attention of medical services, rather than continue in pain.
These are nevertheless important findings, given they clearly point towards a need to identify other variables not analysed in this study of surgical and post-operative factors for chronic pain development. Of the studies identified in Wylde et al.‘s [20] systematic review, the post-operative risk factors explored included acute post-operative pain, post-operative knee function and psychosocial factors (catastrophising, depression, social support, coping skills, fear of movement and anxiety). However, they found insufficient evidence for them to predict chronic post-operative pain development. Further work might consider the role of pain coping behaviours or other aspects of psychology, genetics, social or environmental factors. Pre-operative pain catastrophizing might be an important predictor for chronic postoperative pain following TKR. Although coping strategies can reduce preoperative pain catastrophizing, recent clinical trials have shown that this does not affect chronic postoperative pain outcome after surgery [27,28]. There is a need for more research into intra-operative factors including the actual surgical procedure itself and the implant positioning achieved at the primary operation. Indeed there has been a shift towards robotic knee replacement surgery in recent years with evidence of both improved implant positioning and functional outcomes post-operatively [29]. However, for robotic operations to be potentially cost-effective they would have to combine both important improvements in patients’ outcomes and reduction of revision rates, all at only moderate additional costs, making them unlikely to be made widely available [30].
Another explanation is that chronic pain is highly multifactorial and therefore only through a combination of pre-, intra- and post-operative factors can a model accurately identify patients at risk at a local level. There is already evidence that prediction of at-risk patients is strongest when analysing both pre-operative and post-operative factors together [31].
In this study the OKS was used to define chronic pain given that it is widely available and used commonly in routine clinical practice. Although the OKS is a validated patient reported outcome measure that provides a robust assessment of pain, it does not provide a detailed understanding of pain. Patterns of pain are often complex varying with time, activity levels, time of the day, seasons and analgesic usage. Additionally, using a threshold for chronic pain from the OKS is likely an oversimplification, given it is a complex multifactorial disorder.
The strengths of this study are that we used linked NJR-HES-PROMs data for 258,386 knee replacements to investigate the effect of various intra-operative and post-operative factors on chronic pain development. Additionally, the results are not from a single centre with knee replacements from across the country increasing the study findings generalisability. However, as discussed other factors not collected from the HES and NJR datasets such as more detailed intra-operative factors (including implant positioning and surgical technique) and patient factors (including factors that cover pain management, pain medication use, psychology, genetics and environmental factors) may play an important role. A limitation of our study was that by using routinely collected data we only had a single measure of post-operative knee pain, as defined by a national programme of patient reported outcome measures that made the decision to collect data on outcomes at a 6-month time point. A single measure of pain at the 6 month follow-up does not necessarily provide sufficient data to determine whether “chronic pain” has been established. Furthermore, studies have shown that patients continue to receive improvement in pain beyond the 6-month time point [32].
In conclusion, currently there is no algorithm with a high sensitivity and specificity for identifying which patients are likely to develop chronic post-surgical pain after knee replacement. The surgical and post-operative factors included in our analysis do not appear to predict the presence of chronic pain at six months after knee replacement. Even though there are some individual post-operative risk factors, they do not explain much of the variation in the outcome, even in combination. Further work is needed to investigate other potential predictors, which may include a wider range of intra-operative factors such as implant positioning and surgical technique, and more patient-based factors including psychological, genetic, social and environmental variables.
Funding
This study is funded by the National Institute for Health Research (NIHR) [Programme Grant for Applied Research (Grant Reference Number RP-PG-0613-20,001)]. This study was also supported by the NIHR Biomedical Research Centre at the University Hospitals Bristol NHS Foundation Trust and the University of Bristol. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Data sharing
Access to data is available from the National Joint Registry for England and Wales, Northern Ireland and the Isle of Man, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data access applications can be made to the National Joint Registry Research Committee. Access to linked HES and PROMs data is available through data applications to NHS Digital.
Disclaimer
The views expressed represent those of the authors and do not necessarily reflect those of the NHS, the National Institute for Health Research, the Programme Grants for Applied Research (PGfAR) Programme, the Department of Health and Social Care, the National Joint Registry Steering Committee or the Healthcare Quality Improvement Partnership (HQIP) who do not vouch for how the information is presented. HES data copyright © 2016, re-used with the permission of the Health & Social Care Information Centre. All rights reserved.
Patient consent
Before Personal Data and Sensitive Personal Data is recorded, express written patient consent is provided. The NJR records patient consent as either ‘Yes’, ‘No’, or ‘Not Recorded’.
Ethics approval
With support under Section 251 of the NHS Act 2006, the Ethics and Confidentiality Committee (ECC), (now the Health Research Authority Confidentiality Advisory Group) allows the NJR to collect patient data where consent is indicated as ‘Not Recorded’.
Contributor and guarantor information
All authors contributed to study design, data analysis, interpretation of results and writing the manuscript. All authors had full access to all statistical reports and tables in the study. SK and CG had full access to all of the study data and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the interpretation of results and critical revision of the manuscript and approved the final manuscript. AJ is the guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Declaration of competing interest
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf and declare: AJ has received consultancy fees from Freshfields Bruckhaus Deringer, and has held advisory board positions (which involved receipt of fees) from Anthera Pharmaceuticals, INC, outside the submitted work. AP reports personal fees from Zimmer Biomet, outside the submitted work. NKA received grants and personal fees outside the submitted work from: Bioberica; Merck; Flexion; Regeneron; Freshfields Bruckhaus Deringer. AWB is principal investigator, and VW a co-applicant, on a grant to investigate the outcome of a design of primary total knee replacement (Stryker, Triathlon), outside the submitted work. RPV reports consultancy fees from Kyowa Kirin, UCB, and Mereo, all outside the submitted work. All other authors declare no conflicts of interest.
Acknowledgements
We thank the patients and staff of all the hospitals in England, Wales and Northern Ireland who have contributed data to the National Joint Registry. We are grateful to the Healthcare Quality Improvement Partnership (HQIP), the NJR Research Committee and staff at the NJR Centre for facilitating this work. The authors have conformed to the NJR’s standard protocol for data access and publication. The views expressed represent those of the authors and do not necessarily reflect those of the National Joint Registry Steering Committee or the Healthcare Quality Improvement Partnership (HQIP) who do not vouch for how the information is presented.
Contributor Information
Sara Khalid, Email: sara.khalid@ndorms.ox.ac.uk.
Hasan Raza Mohammad, Email: hasan.mohammad@ndorms.ox.ac.uk.
Rachael Gooberman-Hill, Email: R.Gooberman-Hill@bristol.ac.uk.
Cesar Garriga, Email: cesar.garriga@phc.ox.ac.uk.
Rafael Pinedo-Villanueva, Email: rafael.pinedo@ndorms.ox.ac.uk.
Nigel Arden, Email: nigel.arden@ndorms.ox.ac.uk.
Andrew Price, Email: andrew.price@ndorms.ox.ac.uk.
Vikki Wylde, Email: V.Wylde@bristol.ac.uk.
Tim J. Peters, Email: Tim.Peters@bristol.ac.uk.
Ashley Blom, Email: Ashley.Blom@bristol.ac.uk.
Andrew Judge, Email: Andrew.judge@bristol.ac.uk.
References
- 1.National Joint Registry. report15th Annual Report. National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. http://www.njrreports.org.uk/Portals/0/PDFdownloads/NJR%2015th%20Annual%20Report%202018.pdf 2018.
- 2.Singh J.A., Yu S., Chen L., Cleveland J.D. Rates of total joint replacement in the United States: future projections to 2020–2040 using the national inpatient sample. J. Rheumatol. 2019:170990. doi: 10.3899/jrheum.170990. jrheum. [DOI] [PubMed] [Google Scholar]
- 3.Culliford D., Maskell J., Judge A., Cooper C., Prieto-Alhambra D., Arden N., et al. Future projections of total hip and knee arthroplasty in the UK: results from the UK clinical practice research datalink. Osteoarthritis Cartilage. 2015;23:594–600. doi: 10.1016/j.joca.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 4.Ethgen O., Bruyere O., Richy F., Dardennes C., Reginster J.-Y. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. JBJS. 2004;86:963–974. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Beswick A.D., Wylde V., Gooberman-Hill R., Blom A., Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leal J., Murphy J., Garriga C., Delmestri A., Rangan A., Price A., et al. Costs of joint replacement in osteoarthritis: a study using the national joint Registry and clinical practice research datalink datasets. Arthritis Care Res. 2020 doi: 10.1002/acr.24470. (n/a) [DOI] [PubMed] [Google Scholar]
- 7.Ferket B.S., Feldman Z., Zhou J., Oei E.H., Bierma-Zeinstra S.M., Mazumdar M. Impact of total knee replacement practice: cost effectiveness analysis of data from the Osteoarthritis Initiative. BMJ. 2017;356:j1131. doi: 10.1136/bmj.j1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jenkins P.J., Clement N.D., Hamilton D.F., Gaston P., Patton J.T., Howie C.R. Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Joint Lett. J. 2013;95-b:115–121. doi: 10.1302/0301-620X.95B1.29835. [DOI] [PubMed] [Google Scholar]
- 9.Dakin H., Eibich P., Beard D., Gray A., Price A. The use of patient-reported outcome measures to guide referral for hip and knee arthroplasty. Bone Joint J. 2020;102-B:950–958. doi: 10.1302/0301-620X.102B7.BJJ-2019-0105.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Woolf A., Zeidler H., Haglund U., Carr A., Chaussade S., De Cucinotta, et al. Musculoskeletal pain in Europe: its impact and a comparison of population and medical perceptions of treatment in eight European countries. Ann. Rheum. Dis. 2004;63:342–347. doi: 10.1136/ard.2003.010223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santaguida P.L., Hawker G.A., Hudak P.L., Glazier R., Mahomed N.N., Kreder H.J., et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can. J. Surg. 2008;51:428–436. [PMC free article] [PubMed] [Google Scholar]
- 12.Williams D.P., Price A.J., Beard D.J., Hadfield S.G., Arden N.K., Murray D.W., et al. The effects of age on patient-reported outcome measures in total knee replacements. Bone Joint J. 2013;95-B:38–44. doi: 10.1302/0301-620X.95B1.28061. [DOI] [PubMed] [Google Scholar]
- 13.Mehta S.P., Perruccio A.V., Palaganas M., Davis A.M. Do women have poorer outcomes following total knee replacement? Osteoarthritis Cartilage. 2015;23:1476–1482. doi: 10.1016/j.joca.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 14.Collins J.E., Donnell-Fink L.A., Yang H.Y., Usiskin I.M., Lape E.C., Wright J., et al. Effect of obesity on pain and functional recovery following total knee arthroplasty. J Bone Joint Surg Am. 2017;99:1812–1818. doi: 10.2106/JBJS.17.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Judge A., Arden N.K., Cooper C., Kassim Javaid M., Carr A.J., Field R.E., et al. Predictors of outcomes of total knee replacement surgery. Rheumatology. 2012;51:1804–1813. doi: 10.1093/rheumatology/kes075. [DOI] [PubMed] [Google Scholar]
- 16.Singh J.A., Lewallen D.G. Medical and psychological comorbidity predicts poor pain outcomes after total knee arthroplasty. Rheumatology. 2013;52:916–923. doi: 10.1093/rheumatology/kes402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huber J., Dieppe P., Dreinhoefer K., Günther K.P., Judge A. The influence of arthritis in other major joints and the spine on the one-year outcome of total hip replacement: a prospective, multicenter cohort study (EUROHIP) measuring the influence of musculoskeletal morbidity. J Bone Joint Surg Am. 2017;99:1428–1437. doi: 10.2106/JBJS.16.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liddle A.D., Pandit H., Judge A., Murray D.W. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint Lett. J. 2015;97-b:793–801. doi: 10.1302/0301-620X.97B6.35155. [DOI] [PubMed] [Google Scholar]
- 19.Baker P.N., Rushton S., Jameson S.S., Reed M., Gregg P., Deehan D.J. Patient satisfaction with total knee replacement cannot be predicted from pre-operative variables alone: a cohort study from the National Joint Registry for England and Wales. Bone Joint Lett. J. 2013;95-b:1359–1365. doi: 10.1302/0301-620X.95B10.32281. [DOI] [PubMed] [Google Scholar]
- 20.Wylde V., Beswick A.D., Dennis J., Gooberman-Hill R. Post-operative patient-related risk factors for chronic pain after total knee replacement: a systematic review. BMJ open. 2017;7 doi: 10.1136/bmjopen-2017-018105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peters T.J., Sanders C., Dieppe P., Donovan J. Factors associated with change in pain and disability over time: a community-based prospective observational study of hip and knee osteoarthritis. Br. J. Gen. Pract. 2005;55:205–211. [PMC free article] [PubMed] [Google Scholar]
- 22.Schug S.A., Lavand’homme P., Barke A., Korwisi B., Rief W., Treede R.D. The IASP classification of chronic pain for ICD-11: chronic postsurgical or posttraumatic pain. Pain. 2019;160:45–52. doi: 10.1097/j.pain.0000000000001413. [DOI] [PubMed] [Google Scholar]
- 23.Harris K., Dawson J., Doll H., Field R.E., Murray D.W., Fitzpatrick R., et al. Can pain and function be distinguished in the Oxford Knee Score in a meaningful way? An exploratory and confirmatory factor analysis. Qual. Life Res. 2013;22:2561–2568. doi: 10.1007/s11136-013-0393-x. [DOI] [PubMed] [Google Scholar]
- 24.Pinedo-Villanueva R., Khalid S., Wylde V., Gooberman-Hill R., Soni A., Judge A. Identifying individuals with chronic pain after knee replacement: a population-cohort, cluster-analysis of Oxford knee scores in 128,145 patients from the English National Health Service. BMC Muscoskel. Disord. 2018;19:354. doi: 10.1186/s12891-018-2270-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wylde V., Dennis J., Gooberman-Hill R., Beswick A.D. Effectiveness of postdischarge interventions for reducing the severity of chronic pain after total knee replacement: systematic review of randomised controlled trials. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-020368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wylde V., Bertram W., Beswick A.D., Blom A.W., Bruce J., Burston A., et al. Clinical- and cost-effectiveness of the STAR care pathway compared to usual care for patients with chronic pain after total knee replacement: study protocol for a UK randomised controlled trial. Trials. 2018;19:132. doi: 10.1186/s13063-018-2516-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Riddle D.L., Keefe F.J., Ang D.C., Slover J., Jensen M.P., Bair M.J., et al. Pain coping skills training for patients who catastrophize about pain prior to knee arthroplasty: a multisite randomized clinical trial. J Bone Joint Surg Am. 2019;101:218–227. doi: 10.2106/JBJS.18.00621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Birch S., Stilling M., Mechlenburg I., Hansen T.B. No effect of cognitive behavioral patient education for patients with pain catastrophizing before total knee arthroplasty: a randomized controlled trial. Acta Orthop. 2020;91:98–103. doi: 10.1080/17453674.2019.1694312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kayani B., Konan S., Tahmassebi J., Pietrzak J., Haddad F. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint Lett. J. 2018;100:930–937. doi: 10.1302/0301-620X.100B7.BJJ-2017-1449.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burn E., Prieto-Alhambra D., Hamilton T.W., Kennedy J.A., Murray D.W., Pinedo-Villanueva R. Threshold for computer- and robot-assisted knee and hip replacements in the English national health service. Value Health. 2020;23:719–726. doi: 10.1016/j.jval.2019.11.011. [DOI] [PubMed] [Google Scholar]
- 31.Althaus A., Hinrichs-Rocker A., Chapman R., Becker O.A., Lefering R., Simanski C., et al. Development of a risk index for the prediction of chronic post-surgical pain. Eur. J. Pain. 2012;16:901–910. doi: 10.1002/j.1532-2149.2011.00090.x. [DOI] [PubMed] [Google Scholar]
- 32.Jiang Y., Sanchez-Santos M.T., Judge A.D., Murray D.W., Arden N.K. Predictors of patient-reported pain and functional outcomes over 10 Years after primary total knee arthroplasty: a prospective cohort study. J. Arthroplasty. 2017;32:92–100. doi: 10.1016/j.arth.2016.06.009. e102. [DOI] [PMC free article] [PubMed] [Google Scholar]