Abstract
Objective
Evaluate the implementation of Good Life with osteoArthritis from Denmark (GLA:D®) for knee osteoarthritis in Australia using the RE-AIM QuEST (Reach, Effectiveness, Adoption, Implementation, Maintenance Qualitative Evaluation for Systematic Translation) framework.
Design
Physiotherapists completed surveys before and after GLA:D® training (2017–2020) to assess practices, and barriers and enablers to implementation. Patients completed online baseline, 3-month (post-treatment) and 12-month patient reported outcomes. Effective implementation was defined as within-participant moderate effect size (ES, ≥0.50) for average pain (100 mm VAS) and Knee Injury and Osteoarthritis Outcome Score quality of life scores (KOOS-QoL), and small effect size (≥0.20) for health-related quality of life (EQ-5D-5L).
Results
Reach: 1064 physiotherapists and 1945 patients from all states and territories participated. Key barriers included out-of-pocket cost to patients, and program suitability for culturally and linguistically diverse communities. Effectiveness: Following training, more physiotherapists reported discussing treatment goals and weight management, and prescribing supervised, neuromuscular exercise. Patient outcomes at 3- and 12-months (n = 1044 [54%] and 927 [48%]) reflected effective implementation, including reduced pain (ES, 95%CI = 0.72, 0.62–0.84; and 0.65, 0.54–0.77) and improved KOOS-QoL (0.79, 0.69–0.90; and 0.93, 0.81–1.04) and EQ-5D-5L (0.43, 0.31–0.54; and 0.46, 0.35–0.58) scores. Adoption: 297 sites (264 private, 33 public) implemented GLA:D®. Implementation: Most patients completed at least one education (90%), and 10 exercise-therapy (78%) sessions. Adequate staffing to support program delivery was a key enabler. Maintenance: 99% of sites (293/297) continued offering the program in July 2020.
Conclusion
Training changed practice and was associated with effective widespread implementation of GLA:D® in Australia.
Keywords: Osteoarthritis, Exercise, Education, Physiotherapy, Implementation, Program evaluation
1. Background
Osteoarthritis affects more than 500 million people worldwide [1], with knee osteoarthritis contributing most to global disability [1]. Associated pain and symptoms create substantial individual burden, including poorer health-related quality of life (QoL) [2,3] and greater risk of chronic disease (heart disease, diabetes) [4] compared to population norms. Disease trajectory for most involves stable or slow worsening of pain and symptoms [[5], [6], [7]]. Guidelines [[8], [9], [10]] recommend patient education, exercise-therapy and weight management where indicated as first-line care for knee osteoarthritis. Patient education and exercise-therapy are cost-effective [11,12], can avert surgery [13,14] and have compelling evidence of effectiveness including moderate pain and function improvements compared to control interventions, regardless of radiographic or pain severity [[15], [16], [17]].
More than half (57%) of the 2.2 million (9%) Australians with osteoarthritis do not access guideline-based care [18,19]. Referral rates from general practitioners (GPs) to exercise-therapy are less than 4% [20], despite definitive evidence supporting the implementation of exercise-therapy existing since 2002 [17]. In Australia, GPs are more likely to provide medications including opioids (10%) and refer for surgical opinion (12%) than exercise-therapy [20]. These practices are considered inappropriate if exercise-therapy has not been adequately trialled [[8], [9], [10]]. Most people in Australia with knee osteoarthritis referred for surgery have not received adequate education about osteoarthritis and treatment options [21,22]. Inadequate resourcing and workforce capacity are key drivers of this guideline-practice gap [23]. For example, physiotherapists should provide patient education and exercise-therapy to people with knee osteoarthritis [24]. Yet, they do not always provide this care [[24], [25], [26]], and Australian doctors report frustration about this lack of standardised care [22,27].
In 2016, we adopted the Good Life with osteoArthritis from Denmark (GLA:D®) program [28,29] to provide education, training courses and implementation support for Australian physiotherapists to deliver guideline-based patient education and exercise-therapy to people with hip and knee osteoarthritis. GLA:D® requires physiotherapists to (i) deliver group-based patient education (2–3 x 60–90 min) and supervised exercise-therapy (12 × 60 min) as a ‘minimal intervention’; and (ii) facilitate collection of patient outcomes at baseline, post program (3-months) and 12-months following registration [[29], [30], [31]]. Physiotherapists can provide additional interventions based on evidence and clinical reasoning. GLA:D® has been delivered to more than 48,000 patients in Denmark [32], and is associated with clinically meaningful pain and joint-related quality of life improvements 12-months following participation [29]. Early evaluation of GLA:D® in Australia indicates the program is feasible [33], and associated with similar outcome to Denmark [34].
Implementation science and frameworks can optimise the success of initiatives like GLA:D® by guiding evaluation of, and strategies to improve reach, effectiveness, adoption, implementation, and maintenance [35,36]. In this paper, we evaluate the implementation of GLA:D® within an Australian context. Guided by the RE-AIM QuEST (Reach Effectiveness Adoption Implementation Maintenance Qualitative Evaluation for Systematic Translation) framework [35], this program evaluation investigated (i) changes in physiotherapists' practices, and confidence and beliefs about capabilities to provide patient education and exercise-therapy to people with knee osteoarthritis; (ii) outcomes of people with knee osteoarthritis participating in the program, including primary (pain, knee- and health-related quality of life), and secondary (surgical desire, functional performance) measures; and (iii) barriers and enablers to reach, implementation, adoption and maintenance of the program in Australian public and private settings.
2. Methods
2.1. Study design
A cohort study of the implementation of the GLA:D® Australia physiotherapy training program was conducted between 2017 and 2020. Reporting was guided by the Standards for Reporting Implementation Studies (StaRI) checklist [37,38]. A detailed logic model for the GLA:D® Australia program is in Additional file 1. This program evaluation, guided by the RE-AIM QuEST framework [35,39], included consideration at system, health services, health professional, patient and program levels. Data were provided by three sources:(i) physiotherapist surveys; (ii) the patient data registry; and (iii) a health service implementation registry managed by GLA:D® Australia.
Twenty-three physiotherapist training courses (2-days) delivered between March 2017 and December 2019 (Melbourne = 12, Brisbane = 5 Perth = 2, Adelaide = 2, Sydney = 1, Darwin = 1) involved (i) pre- and post-workshop surveys evaluating knowledge and learning needs, (ii) lectures regarding osteoarthritis management, (iii) patient education and exercise-therapy skills training sessions, (iv) training to contribute patient outcomes to the national registry, and (v) discussions about overcoming barriers to implementation. Each trained physiotherapist received an implementation manual, ready-to-use patient education materials (PowerPoint presentations and printable booklets), and access to online implementation resources (e.g. flyers, letter templates for referring doctors).
To help clinicians and patients identify where GLA:D® Australia is available and determine program reach and context, geographical locations of health services who implemented GLA:D® Australia were recorded and published on the study website (www.gladaustralia.com.au). Type of service (hospital, community health centre, private clinic) was also recorded.
2.2. Participant recruitment and data collection
1068 Australian Health Practioner Regulation Agency registered physiotherapists (average group size = 46) were trained during this evaluation period. Following informed consent [Ethics approval provided by La Trobe University, S16-51], and prior to training, an investigator-developed survey was administered (Additional file 2). The survey, developed by the research team (CJB, JLK, JW, NL and KMC), was informed by clinical practice guidelines [[8], [9], [10]] and the theoretical domains framework (TDF) [40,41]. Questions explored (i) current practices when treating knee osteoarthritis; and (ii) confidence and beliefs about capabilities to provide patient education and exercise-therapy to people with knee osteoarthritis. This survey was repeated 1-2-weeks post-training completion. A further repeat of the survey at 12-months post-training, sent to 775 physiotherapists and completed by 147 (19%), also explored implementation barriers and enablers via open-ended questions.
Trained physiotherapists provided GLA:D® to people presenting with knee and/or hip joint problems. Imaging was not required for diagnosis. People with other reasons for joint problems than osteoarthritis were excluded, including recent trauma, tumor, inflammatory joint disease, other symptoms that are more pronounced than osteoarthritis, or issues with understanding written or spoken English. All program participants were registered on a secure online patient data registry facilitated by the Research Electronic Data Capture (REDCap) system hosted at La Trobe University, with an ‘opt out’ consent process.
Participants who completed baseline questionnaires were automatically emailed 3- and 12-month follow up questionnaires. The online patient registry was launched in January 2018, with ethical approval granted by La Trobe University's Human Ethics Research Committee (S17 – 193). The focus on this evaluation was on participants registered with the knee as their most symptomatic joint. Data collection for this program evaluation captured all patient participants commencing the program between January 1, 2018 and June 30, 2019, allowing 12-month data follow ups by July 31, 2020. Primary and secondary patient reported outcome measures used for this program evaluation are shown in Table 1.
Table 1.
Primary and secondary patient reported outcome measures.
| DOMAIN | OUTCOME | DESCRIPTION |
|---|---|---|
| Primary patient reported outcomes | ||
| Pain intensity | 100 mm VAS: average paina | Using anchors of ‘no pain’ and ‘worst pain imaginable’, a valid, reliable and responsive measure [42]. |
| Knee-related quality of life | KOOS-QoL | 4-item scale providing scores ranging from 0 (worst) to 100 (best) points, which is reliable and responsive [43]. |
| Health-related quality of life | EQ-5D-5L | Five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Five severity levels: “no problems”, “slight problems”, “moderate problems”, “severe problems”, and “extreme problems” describing 3125 distinct health states. Most widely used generic patient reported outcome, and is valid and reliable [44]. The EQ-5D-5L index was calculated using an England-based value set [44] as it closely resembled the Australian population [45]. |
| Secondary patient outcomes | ||
| Surgery | Surgery desire | Determined through a custom developed question “Do you have so much pain and trouble from your knee that you want to have surgery?“, with answers categorised as ‘yes’ or ‘no’. |
| Functional performance | 30 s chair-stand test | Recommended by the OARSI [46], and administered by physiotherapists providing GLA:D® at baseline (prior to program commencement) and 3-month follow up. |
| Walking speed | 40 m fast-paced walk test | Recommended by the OARSI [46], and administered by physiotherapists providing GLA:D® at baseline (prior to program commencement) and 3-month follow up. |
EQ-5D-5L = European quality of life-5 dimensions-5 level quality of life scale; KOOS-QoL = Knee Injury and Osteoarthritis Outcomes Score Quality of Life subscale; VAS = visual analogue scale.
In previous month.
2.3. Data analysis
Physiotherapist data were dichotomised for statistical analysis; agreement (strongly agree and agree) and other responses (neither agree nor disagree, disagree and strongly disagree); confident (very confident or confident) and other responses (average, below average and not confident at all); or frequently providing (all of the time and most of the time) and other responses (some of the time, rarely and never). Chi-squared statistics with Yates correction determined significance of changes between pre- and post-training survey results. Effect sizes (ES) were calculated using Phi for 2 × 2 contingency table and Cramer's V for tables larger than 2 × 2 contingency table, and categorised as negligible (<0.10), small (≥0.10), moderate (≥0.30) or large (≥0.50) [47].
12-month quantitative physiotherapist survey data were not used in statistical analysis. Perceived implementation barriers and enablers among physiotherapists from 12-month surveys (n = 147) were coded using an inductive thematic analysis [48], with initial coding structure developed by KD, MFP and CJB. Coding was refined and mapped to system, health services, health professional, patient, and program factors by KD and CJB.
A linear mixed model with age and sex as covariates, patient participants as a random effect and time (baseline, 3-month and 12-month) as fixed effect was applied to patient participant outcomes where appropriate. Bonferroni's post-hoc test was applied for multiple pairwise comparisons when appropriate. A responder analysis was facilitated by calculating the proportion of patients achieving a minimal clinically important change (MIC) for each primary patient reported outcome – pain reduction (15 mm) [49,50], Knee Injury and Osteoarthritis Outcome Score quality of life subscale (KOOS-QoL, 15 points) [51], and European Quality of Life-5 dimensions-5 levels utility score (EQ-5D-5L, 0.07 for non-surgical patients) [52]; and for any of the primary patient reported outcomes. Paired t-tests compared functional performance outcomes (chair stand and 40 m timed fast walk) between baseline and 3-months. Effect sizes (ES) and 95% confidence intervals for pre/post comparisons were calculated with a correction for dependence among means applied by accounting for correlations between pre and post assessments [53], and interpreted as small (≥0.20), moderate (≥0.50) or large (≥0.80) [47]. Effective implementation for patient outcomes was determined if moderate or greater ES occurred for pain and knee-related quality of life, and if small or greater ES occurred for health-related quality of life [[15], [16], [17],54]. Comparison of surgical desire between baseline and 3-months, and baseline and 12-months were made descriptively as proportions (percentage of respondents).
3. Results
3.4. Participants
Physiotherapists: 1064 out of 1068 trained physiotherapists consented to use their survey data. Years of experience varied (<5 = 34%, n = 362; 5–10 = 20%, n = 208; 11–15 = 11%, n = 113; >15 = 36%, n = 381), and 37% (397/1064) reported having completed post-graduate training (Masters or PhD). Survey completion rate post-training (typically within 2-weeks) was 35% (371/1064). Characteristics of physiotherapists who completed the post-training survey are provided in Additional file 3.
Patients: 2611 people with knee osteoarthritis entered the GLA:D® Australia registry between January 2018 and June 2019, with 1945 (75%) completing baseline data collection. Average (SD) age, height, body mass and body mass index (BMI) of respondents was 65 (9) years, 1.67 (0.1) metres, 84 (18.7) kg, and 30.1 (6.4) kg/m2. Of the 1945 who provided baseline data, 1044 (54%) and 927 (48%) completed 3- and 12-month follow up questionnaires, respectively. Baseline characteristics of people with knee osteoarthritis lost to follow up were similar to the overall cohort (Additional file 4). Knee surgery was reported by 2% at 3-months (n = 23; 19 joint replacements [13 most affected side at baseline]; 3 arthroscopies [1 most affected side at baseline]; and 1 tibial osteotomy) and 9% at 12-months (n = 86; 71 unilateral joint replacements [47 most affected side at baseline]; 7 bilateral joint replacements; 6 arthroscopies [2 most affected side at baseline]).
3.5. Quantitative evaluation outcomes
3.5.1. Reach
Health professional: Approximately 7% of all Australian physiotherapists practising in the musculoskeletal field (1068/14,462 [55]) were trained between March 2017 and December 2019.
Patient: Approximately 0.1% of Australians with osteoarthritis (2611/2.2 million [18]) participated in GLA:D® between January 2018 and June 2019. Of the 2611 patients registered, 1945 (74%) provided baseline data. Proportions of those not providing baseline data were similar to those providing baseline data in private (82% v 79%), public (13% v 15%) and unknown (5% v 6%) settings.
Table 2 provides the break down of public/private and geographical location for reach to health professionals and patients.
Table 2.
Reach related to geography (state/territory) and setting (public/private) at a physiotherapist and patient level.
| Physiotherapist | Patient | |
|---|---|---|
| State/territory | n = 1068 | n = 1945 |
| Victoria | 526 (49%) | 1109 (57%) |
| NSW | 91 (9%) | 128 (7%) |
| ACT | 19 (2%) | 43 (2%) |
| Queensland | 151 (14%) | 108 (6%) |
| Tasmania | 23 (2%) | 91 (5%) |
| South Australia | 124 (12%) | 249 (13%) |
| Northern Territory | 20 (2%) | 26 (1%) |
| Western Australia | 108 (10%) | 72 (4%) |
| Unknown | 6 (<1%) | 119 (6%) |
| Setting | n = 1028 | n = 1945 |
| Private | 746 (73%) | 1546 (79%) |
| Public | 205 (20%) | 290 (15%) |
| Public and private | 77 (7%) | – |
| Unknown | – | 109 (6%) |
ACT = Australian Capital Territory; NSW = New South Wales.
3.5.2. Effectiveness
Health professional: Training had a small effect on the number of physiotherapists discussing treatment goals, prescribing neuromuscular exercise, using supervised exercise, and discussing the importance of weight management (ES = 0.10–0.26) all or most of the time (Table 3). Training had a moderate effect on the proportion of physiotherapists believing they had been trained to deliver guideline-recommended education and exercise-therapy (ES = 0.46), and small effect on perceived knowledge and skills (ES = 0.27) to do so (Table 4). Training had a large effect on the proportion of physiotherapists confident to prescribe neuromuscular exercise (ES = 0.51); and moderate effect on the proportion of physiotherapists confident to provide education and exercise-therapy following guidelines when a patient is not motivated, provide education related to self-management and physical activity, and discuss weight management (ES = 0.30–0.43) (Table 4). Detailed data related to physiotherapy survey outcomes, including 12-month follow-up in a sub-set of trained physiotherapists (n = 147), are presented in Additional file 5.
Table 3.
Practice behaviours (‘all of the time’ or ‘most of the time’) related to treatment goals, neuromuscular exercise, supervised exercise, and weight management discussion.
| Survey item | Baseline | Post-course | Baseline vs post-course effect size (p value) |
|---|---|---|---|
| Discuss treatment goals | 87% | 94% | 0.14 (<0.001) |
| Prescribe neuromuscular exercise | 54% | 81% | 0.26 (<0.001) |
| Refer to, or provide supervised exercise programs | 53% | 72% | 0.19 (<0.001) |
| Discuss the importance of weight management | 55% | 65% | 0.10 (<0.001) |
Table 4.
Beliefs about capabilities related to delivering education and exercise-therapy including elements of the GLA:D® Australia program to people with knee osteoarthritis.
| Baseline | Post-course | Baseline vs post-course effect size (p value) | |
|---|---|---|---|
| Knowledge, training and skills | |||
| I know how to deliver exercise and education to people with knee osteoarthritis following current guidelines | 76% | 100% | 0.27 (<0.001) |
| I have been trained in delivering exercise and education to people with knee osteoarthritis following current guidelines | 48% | 100% | 0.46 (<0.001) |
| I have the skills to deliver exercise and education to people with knee osteoarthritis following current guidelines | 77% | 99% | 0.27 (<0.001) |
| Confidence | |||
| I am confident I can deliver exercise and education to people with knee osteoarthritis following current guidelines | 76% | 100% | 0.27 (<0.001) |
| I am confident I can deliver exercise and education to people with knee osteoarthritis following guidelines, even when the patient is not motivated | 47% | 94% | 0.43 (<0.001) |
| I am confident in prescribing neuromuscular exercise | 39% | 96% | 0.51 (<0.001) |
| I am confident in providing education related to-self management | 69% | 95% | 0.30 (<0.001) |
| I am confident in providing education related to physical activity participation | 60% | 94% | 0.35 (<0.001) |
| I am confident in discussing the importance of weight management | 51% | 85% | 0.34 (<0.001) |
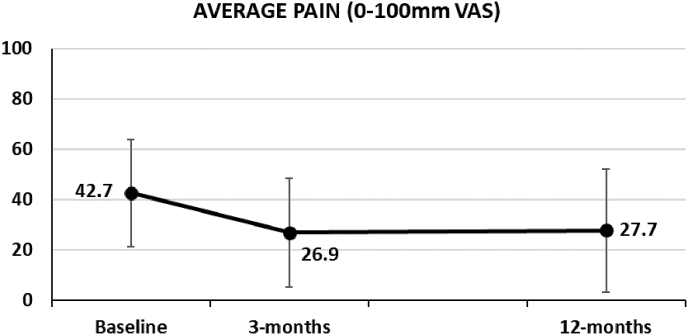
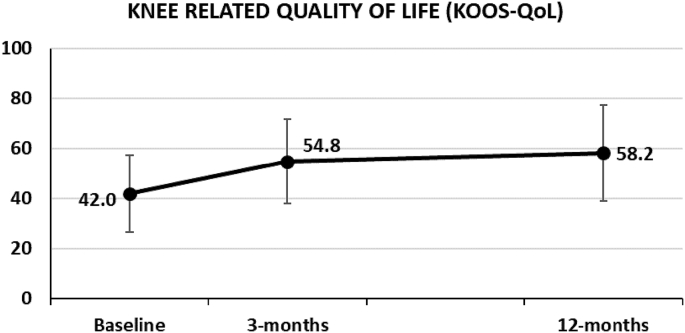
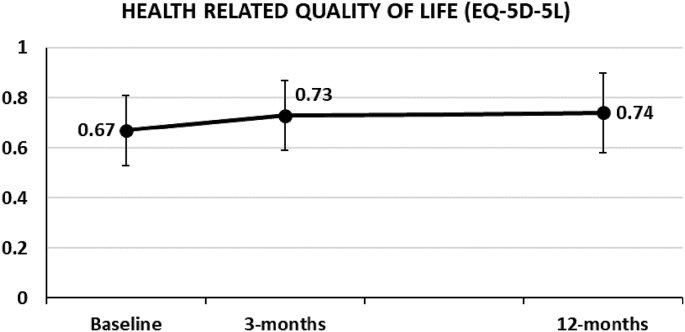
Patient: Group-level improvements at 3- and 12-months were moderate for average pain in the previous month (ES = 0.73 and 0.65; Fig. 1a), moderate-large for knee-related quality of life (0.79 and 0.93; Fig. 1b), and small for health-related quality of life (0.43 and 0.46; Fig. 1c) (Table 5). Minimal important changes were achieved for primary patient reported outcome measures by 49–56% at 3-months, and 52–55% at 12-months (Table 5). Seventy-three percent achieved MIC for at least one primary outcome at both 3-months (544/741), and 12-months (498/679).
Fig. 1a.
Average pain in the previous month (measured on 100 mm visual analogue scale) at baseline, 3-months and 12-months.
Fig. 1b.
Knee-related quality of life (measured by the Knee Injury and Osteoarthritis Outcome Score quality of life [KOOS-QoL] subscale) at baseline, 3-months and 12-months.
Fig. 1c.
Health-related quality of life (measured by European Quality of Life-5 dimensions-5 levels [EQ-5D-5L]) utility score at baseline, 3-months and 12-months.
Table 5.
Pain, knee-related quality of life, and health related quality of life comparisons between baseline and 3-months, and baseline and 12-months.
| Baseline v 3-months |
Baseline v 12-months |
|||||
|---|---|---|---|---|---|---|
| Mean difference (95% CI) | Effect size (95% CI) | Responders (n = ) | Mean difference (95% CI) | Effect size (95% CI) | Responders (n = )a | |
| Average pain in previous month (mm) | 14 (11–18) | 0.73 (62–0.84) | 56% (398/716) | 15 (11–18) | 0.65 (0.54–0.77) | 55% (357/653) |
| KOOS-QoL subscale | 14 (11–17) | 0.79 (0.69–0.90) | 50% (363/731) | 17 (14–20) | 0.93 (0.81–1.04) | 53% (356/668) |
| EQ-5D-5L utility score | 0.06 (0.04–0.08) | 0.43 (0.31–0.54) | 49% (337/682) | 0.07 (0.04–0.10) | 0.46 (0.35–0.58) | 52% (326/624) |
KOOS-QoL = Knee Injury and Osteoarthritis Outcome Score quality of life; EQ-5D-5L = European Quality of Life-5 dimensions-5 levels.
Number of responders/number of participants with adequate data at baseline and follow up to determine responsiveness.
Of 1044 participants for whom 3-month follow up data were available, 198 (19%) desired surgery before commencing GLA:D®, with 100 (51%) not receiving surgery and no longer desiring surgery at 3 months. Of the 927 participants for whom 12-month follow up data were available, 157 (17%) desired surgery before commencing GLA:D®, with 117 (74%) not receiving surgery and no longer desiring surgery at 12 months. Significant changes in functional performance occurred between baseline and 3-months including the 30-s chair stand (3.2; 2.8 to 3.6 repetitions, ES = 0.91 [0.78 to 1.04], p-value < 0.001) and walking speed during the 40 m walk test (0.21; 0.16–0.26 m/s, ES = 0.48 [0.36 to 0.60], p-value < 0.001) (Additional file 6).
3.5.3. Adoption
Health services: 297 sites (Victoria = 155, NSW = 34, Western Australia = 31, Queensland = 29, South Australia = 30, ACT = 9, Tasmania = 5, Northern Territory = 4) implemented GLA:D® Australia by December 2019 (settings: private = 264, 89%; and public = 33, 11%).
Health professional: 91% (337/371) of physiotherapist post-training survey respondents had implemented GLA:D® or intended to implement in the next 6-months. 79% (116/147) of physiotherapists who responded to the 12-month survey had implemented GLA:D®.
3.5.4. Implementation
Patient: 90% completed at least one patient education session, and 78% completed at least 10 exercise-therapy sessions (Additional file 7).
3.5.5. Maintenance
Health services: Of the 297 sites who implemented GLA:D® from 2017 to 19, 99% (n = 293) continued to offer the program in July 2020 (i.e. 6-39 months following implementation).
3.6. Qualitative evaluation outcomes
Key barrier and enabler findings from this GLA:D® Australia program evaluation, guided by the RE-AIM QuEST framework [35,39], are provided in Table 6, with detailed findings including illustrative quotes available in Additional file 8.
Table 6.
Key findings from the GLA:D® Australia program evaluation guided by the RE-AIM QuEST framework (35, 38).
| Dimension | Barriers and Enablers (detailed findings in Additional file 5) |
|---|---|
| Reach |
Barriers System: personal cost to patient. Patient: patient motivation and commitment. Program: suitability for CALD communities; suitability for patients with complex needs; COVID-19 (preventing face-to-face care). Barriers/Enablers System: public/private funding to support participation. Health professional: referrer (e.g. GP) buy in. Patient: patient demand; patient beliefs and understanding. Program: program promotion and awareness; data and evidence. |
| Effectiveness |
Barriers Patient: patient motivation and commitment. |
| Adoption |
Barriers Health services: Conflicting managerial and organisational priorities; inadequate time to support program administration; rural/regional location. Barriers/Enablers Health services: Fit of program to current services; Equipment and physical space; scheduling. |
| Implementation |
Barriers Program: program ethics and legal requirements. Barriers/Enablers Health services: staff resourcing and capacity to meet demand. Enablers Program: Developing materials for CALD groups; central program support; further professional development opportunity. |
| Maintenance |
Barriers/Enablers Program: Access to staff training. |
4. Discussion
GLA:D® Australia training reached 7% of all Australian musculoskeletal physiotherapists [55] over a three year period. Training was associated with increased proportions of physiotherapists reporting they were confident to, and actually did, prescribe neuromuscular exercise, educate about self-management and physical activity, and discuss the importance of weight management all or most of the time. The majority adopted the GLA:D® program in their practice, leading to widespread implementation (297 public and private sites) across all Australian states and territories. Patient adherence to education and exercise-therapy, combined with moderate-to-large improvements in pain and knee-related quality of life, and small improvements in health-related quality of life following GLA:D® in Australia indicates effective implementation.
Pain and knee-related quality of life outcomes are consistent with clinical trials evaluating education and exercise-therapy [[15], [16], [17],54], implementation of GLA:D® in Denmark [29,34] and Canada [34,56], and other similar nationwide implementation initiatives [57,58]. Considering stable or slow worsening of symptoms typically occurs in the longer term for people with knee osteoarthritis [[5], [6], [7]], including in those receiving usual care in clinical trials [11], these improvements are important. Notably, 73% of participants reported a MIC in at least one of pain severity, knee-related quality of life, or health-related quality of life 12-months following GLA:D® participation.
Although small, health-related quality of life improvements at 3- and 12-months indicate the broader health and well-being benefits to Australians with knee osteoarthritis participating in GLA:D®. Effective implementation of education and exercise-therapy through GLA:D® is further indicated by functional performance and walking speed improvements at 3-months. Further evaluation will determine if effective implementation of GLA:D® in Australia is sustained as the program is further scaled up.
Seventy-four percent of those who desired surgery prior to GLA:D®, had not undergone surgery and no longer desired surgery at 12-months. This real-world outcome is consistent with clinical trial findings reported by Skou et al. where 74% of people with moderate to severe knee osteoarthritis who received patient education, exercise-therapy and other non-surgical treatment prior to joint replacement surgery chose to forgo surgery at 12-months [13]. Approximately 10% of our registry participants with knee osteoarthritis did report having knee surgery at 12-months, which is higher than the 5% reported following GLA:D® in Denmark [29]. Baseline demographics and pain severity, along with pain and quality of life outcomes are comparable between the two countries. Therefore, the reason for higher surgery rates in Australia requires further investigation with consideration to potential health system funding, cultural differences, and treatment expectations.
Effective implementation of education and exercise-therapy through GLA:D® is likely the result of multiple factors. At a health professional level, GLA:D® has a strong focus on skills-based training, which meets preferred professional development needs of physiotherapists [26,59] and is an effective means to change practice [[60], [61], [62]]. Standardisation of education and exercise-therapy through GLA:D® addresses variation in physiotherapy practice for osteoarthritis [25,26], which is desired by many surgeons, general practitioners and rheumatologists in Australia [22,27]. Supporting evidence for the program is also considered a key enabler to improving program reach and trust from referrers. At a patient level, education and supervision of exercise-therapy to develop exercise skills, guide appropriate progression and manage pain may be important to address key exercise participation barriers in people with osteoarthritis [15,[63], [64], [65]].
Despite evidence of effective implementation of education and exercise-therapy through GLA:D®, not all people with knee osteoarthritis improved. Approximately one in two participants reported changes above the MIC threshold for pain severity, knee-related quality of life, and health-related quality of life at 3- and 12-months. Among other factors, these variable outcomes may reflect the heterogeneity of osteoarthritis, with individual patient factors associated with pain and disability [64]. It also highlights the need to consider alternate or additional interventions beyond education and exercise-therapy delivered during GLA:D®. Previous detailed evaluation of the Danish GLA:D® registry could not predict outcomes with greater precision than group average changes for pain, joint-related quality of life and function [66], and co-morbidities do not appear to influence potential to respond [67]. Further work is encouraged to identify responders and non-responders for GLA:D®, and to test the effectiveness of alternate exercise-therapy approaches (e.g. greater aerobic exercise focus) or additional care (e.g. psychology, diet, etc.) in these people.
GLA:D® Australia's reach to people with knee osteoarthritis in the 18-month period was small (0.1%: 2611/~2.2 million). This is not surprising, considering the program is in its initial stage of implementation. There is a lag between physiotherapist training, program implementation, and patient participant follow up, including 12-month outcomes used for this evaluation. Improved funding to support implementation and delivery is needed to enhance the accessibility and reach of guideline-based programs like GLA:D®. Consistent with qualitative findings among patients and referrers [27], changing reimbursement models to improve access was a key suggested enabler. Further work is urgently needed to better understand barriers to changing reimbursement models for effective chronic disease programs in Australia. A recent budget impact analysis indicates nationwide implementation of GLA:D® could translate to savings of more than $300 million to the Australian healthcare system annually [68].
Reach and adoption was more limited in public settings, with few trained physiotherapists (15%) and implementation sites (11%), and publicly-funded participants making up just 15% of those entering the registry. Comparatively, 27% of Australian physiotherapists work in the public setting [55]. Addressing barriers to people with osteoarthritis accessing GLA:D® in public settings is a priority. Our findings indicate that key initiatives to help should include developing culturally and linguistically diverse (CALD) patient education resources, and supporting legal and ethics requirements related to data collection. Additional barriers specific to public health implementation and adoption in Australia were also identified, including conflicting managerial and organization priorities, fit of the program to current services, inadequate time to support administration, and capacity to provide staffing to support program delivery. Once adopted, maintenance was strong, with 99% of the 297 public and private health services continuing to offer the program 6–39 months following implementation. This highlights the importance of adequately supporting health services to overcome initial implementation barriers.
Addressing patient beliefs and understanding about osteoarthritis and treatment options, and facilitating referrer buy-in to improve program reach were key themes from physiotherapist surveys. Future education initiatives targeting health professionals and the community to address misinformation about osteoarthritis [27] and promote the value of education and exercise-therapy for knee osteoarthritis may improve the reach and effectiveness of GLA:D® in Australia [27]. Initiatives to support osteoarthritis education from research and healthcare communities may also help address limited patient motivation and commitment to participate, which were viewed by physiotherapists as key barriers to program participation and effectiveness.
4.1. Limitations and future directions
The survey response rate of physiotherapists post-training was 35%, which may impact on our effectiveness evaluation at a health professional level. Reasons for non-response are unclear, and may include not wishing to continue participation, incorrect email addresses being provided at baseline, or emails going to junk mail. However, characteristics of those who did and did not complete the post-training survey were similar regarding work settings, levels of experience, and perceived capabilities to follow guidelines prior to training (Additional file 3). The response rate for the physiotherapists 12-month survey, where we only used qualitative data related to barriers and enablers, was even lower at 19%. We encourage others completing similar program evaluations to consider if mandatory post-training testing of health professionals is appropriate, to improve response rates.
Being a pragmatic implementation study, not all patients entered into the data registry provided baseline data. Possible reasons for this could be the email to enter data was not received (e.g. it went to ‘junk’ mail), or they did not want to participate. Follow-up response rates were low for people with knee osteoarthritis (48% at 12-months), which is common in real-world implementation evaluations. As a comparison, patient-level evaluations for GLA:D® in Denmark, and the Better Management of osteoaAthritis (BOA) program in Sweden reported 12-month response rates of 68% [29] and 42% [57], respectively. The influence of dropouts on our effectiveness outcomes is difficult to determine. However, baseline characteristics of patients lost to follow up were similar to the overall cohort. Fidelity of treatment provided by trained physiotherapists was not evaluated, but underway following a published protocol [56]. It is unclear what level of maintenance occurs at a health professional level. A recurrent accreditation process was implemented for GLA:D® Australia in 2020, which will provide greater insight into this.
We chose conservative values recommended for non-surgical treatments when determining MIC values for our primary outcomes [[49], [50], [51], [52]]. However, we acknowledge the lack of consensus regarding definition and use of cut offs for MIC scores [43,69], and other methods for determining responders such as the OMERACT-OARSI criteria [70] exist. Our responder analysis could be subject to change depending on methods applied. Future work involving patients to determine consensus on MIC scores and responder criteria following programs like GLA:D® is encouraged.
This program evaluation focussed on knee osteoarthritis, but GLA:D® is also provided to people with hip osteoarthritis, and further evaluation is planned to determine reach and effectiveness in this population. Our barriers and enablers evaluation were limited to physiotherapists attending training courses. Further evaluation with patients, other medical professionals (general practitioners, surgeons, etc.), organisational administrative staff, health insurance companies, and government policy makers is needed. Further mixed-methods work is underway with these various stakeholders across public and private settings, and in varying geographical locations. This will provide more comprehensive insight into barriers and enablers to program implementation and maintenance. The generalisability of findings from this study to provide insight into implementation at individual health services within Australia requires consideration, due to the large diversity in resources, staffing, funding for services, and surrounding community demographics.
4.2. Conclusion
Our evaluation of GLA:D® in Australia using the mixed-methods RE-AIM QuEST framework [35,39] provides valuable insight to health professionals and health services considering the program in their setting. Targeted physiotherapist training provides physiotherapists with enhanced confidence and belief about capabilities to deliver guideline-based education and exercise-therapy. Effective implementation of GLA:D® in Australia is demonstrated by moderate effect for improvements in pain and knee-related quality of life, small effect for health-related quality of life, and reduced desire for surgery. Further work is warranted to address barriers, and to leverage enablers, in order to scale up GLA:D® Australia, particularly in public settings.
Authors contributions
CJB, KMC, JLK and NAL conceived the program evaluation design. ER and STS are the founders of GLA:D® and trained and supported CJB, JLK and JW to train Australian physiotherapists to implement GLA:D® in Australia. CJB, JLK and JW facilitated all physiotherapists training. CJB, MF and KD facilitated survey data collection from physiotherapists. KMC, JLK, CJB, MF, and KD established and managed the patient data registry. CJB and MP completed quantitative data analysis. CJB, KD and MP completed qualitative data analysis. All authors contributed to, read and approved the final manuscript.
Funding
CJB is supported by an MRFF TRIP Fellowship (APP1150439). JLK is supported by an NHMRC Early Career Fellowship (APP1119971). STS is currently funded by a program grant from Region Zealand (Exercise First) and a grant from the European Research Council (ERC) under the European Union's Horizon 2020 research and innovation program (grant agreement No 801790). NAL is supported by a National Heart Foundation of Australia Future Leader Fellowship (GNT 102055). The funders did not have any role in this study other than to provide funding.
Ethics approval and consent to participate
Ethics approval for physiotherapists data collection was provided by La Trobe University's Human Ethics Research Committee (S16-51), with consent provided via a tick box on the first page of the online survey. Ethics approval for patient data collection was provided by La Trobe University's Human Ethics Research Committee (S17 – 193), with an online ‘opt out’ consent process. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Declaration of competing interest
CJB, JLK and KMC are program leads of GLA:D® Australia, which is a not for profit implementation initiative. Their institution has received payment for training GLA:D® practitioners. ER and STS are the co-founders of Good Life with Osteoarthritis in Denmark (GLA:D®), a not for profit initiative hosted at University of Southern Denmark aimed at implementing clinical guidelines for osteoarthritis in clinical practice. STS has received grants from The Lundbeck Foundation, personal fees from Munksgaard and TrustMe-ED, all of which are outside the submitted work. The authors affirm that they have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript, except as disclosed in an attachment and cited in the manuscript.
Acknowledgements
We thank the GLA:D® Australia tutors, and physiotherapists and sites who facilitated data collection which allowed evaluation of effectiveness of the program.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ocarto.2021.100175.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Vos T., Lim S.S., Abbafati C., Abbas K.M., Abbasi M., Abbasifard M., et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Filbay S.R., Ackerman I.N., Russell T.G., Macri E.M., Crossley K.M. Health-related quality of life after anterior cruciate ligament reconstruction: a systematic review. Am. J. Sports Med. 2014;42(5):1247–1255. doi: 10.1177/0363546513512774. [DOI] [PubMed] [Google Scholar]
- 3.Coburn S.L., Barton C.J., Filbay S.R., Hart H.F., Rathleff M.S., Crossley K.M. Quality of life in individuals with patellofemoral pain: a systematic review including meta-analysis. Phys. Ther. Sport. 2018;33:96–108. doi: 10.1016/j.ptsp.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Williams A., Kamper S.J., Wiggers J.H., O'Brien K.M., Lee H., Wolfenden L., et al. Musculoskeletal conditions may increase the risk of chronic disease: a systematic review and meta-analysis of cohort studies. BMC Med. 2018;16(1):167. doi: 10.1186/s12916-018-1151-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nicholls E., Thomas E., van der Windt D.A., Croft P.R., Peat G. Pain trajectory groups in persons with, or at high risk of, knee osteoarthritis: findings from the Knee Clinical Assessment Study and the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2014;22(12):2041–2050. doi: 10.1016/j.joca.2014.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bastick A.N., Wesseling J., Damen J., Verkleij S.P., Emans P.J., Bindels P.J., et al. Defining knee pain trajectories in early symptomatic knee osteoarthritis in primary care: 5-year results from a nationwide prospective cohort study (CHECK) Br. J. Gen. Pract. 2016;66(642):e32–e39. doi: 10.3399/bjgp15X688129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Øiestad B.E., White D.K., Booton R., Niu J., Zhang Y., Torner J., et al. Longitudinal course of physical function in people with symptomatic knee osteoarthritis: data from the multicenter osteoarthritis study and the osteoarthritis initiative. Arthritis Care Res. 2016;68(3):325–331. doi: 10.1002/acr.22674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.RACGP . 2018. Guideline for the Management of Hip and Knee Osteoarthritis. (Melbourne) [Google Scholar]
- 9.McAlindon T.E., Bannuru R.R., Sullivan M.C., Arden N.K., Berenbaum F., Bierma-Zeinstra S.M., et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(3):363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Nelson A.E., Allen K.D., Golightly Y.M., Goode A.P., Jordan J.M. A systematic review of recommendations and guidelines for the management of osteoarthritis: the chronic osteoarthritis management initiative of the U.S. bone and joint initiative. Semin. Arthritis Rheum. 2014;43(6):701–712. doi: 10.1016/j.semarthrit.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Abbott J.H., Wilson R., Pinto D., Chapple C.M., Wright A.A., team M.T. Incremental clinical effectiveness and cost effectiveness of providing supervised physiotherapy in addition to usual medical care in patients with osteoarthritis of the hip or knee: 2-year results of the MOA randomised controlled trial. Osteoarthritis Cartilage. 2018 doi: 10.1016/j.joca.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Skou S.T., Roos E.M., Laursen M., Arendt-Nielsen L., Rasmussen S., Simonsen O., et al. Cost-effectiveness of 12 weeks of supervised treatment compared to written advice in patients with knee osteoarthritis: a secondary analysis of the 2-year outcome from a randomized trial. Osteoarthritis Cartilage. 2020 doi: 10.1016/j.joca.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Skou S.T., Roos E.M., Laursen M.B., Rathleff M.S., Arendt-Nielsen L., Simonsen O., et al. A randomized, controlled trial of total knee replacement. N. Engl. J. Med. 2015;373(17):1597–1606. doi: 10.1056/NEJMoa1505467. [DOI] [PubMed] [Google Scholar]
- 14.Skou S.T., Roos E.M., Laursen M.B., Rathleff M.S., Arendt-Nielsen L., Rasmussen S., et al. Total knee replacement and non-surgical treatment of knee osteoarthritis: 2-year outcome from two parallel randomized controlled trials. Osteoarthritis Cartilage. 2018 doi: 10.1016/j.joca.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 15.Skou S.T., Pedersen B.K., Abbott J.H., Patterson B., Barton C. Physical activity and exercise therapy benefit more than just symptoms and impairments in people with hip and knee osteoarthritis. J. Orthop. Sports Phys. Ther. 2018;48(6):439–447. doi: 10.2519/jospt.2018.7877. [DOI] [PubMed] [Google Scholar]
- 16.Juhl C., Christensen R., Roos E.M., Zhang W., Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheum. 2014;66(3):622–636. doi: 10.1002/art.38290. [DOI] [PubMed] [Google Scholar]
- 17.Uthman O.A., van der Windt D.A., Jordan J.L., Dziedzic K.S., Healey E.L., Peat G.M., et al. Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. BMJ. 2013;347:f5555. doi: 10.1136/bmj.f5555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ackerman I., Bohensky M., Pratt C., Gorelik A., Liew D. 2016. Counting the Cost. Part 1. Healthcare Costs: the Current and Future Burden of Arthritis. [Google Scholar]
- 19.Runciman W.B., Hunt T.D., Hannaford N.A., Hibbert P.D., Westbrook J.I., Coiera E.W., et al. CareTrack: assessing the appropriateness of health care delivery in Australia. Med. J. Aust. 2012;197(2):100–105. doi: 10.5694/mja12.10510. [DOI] [PubMed] [Google Scholar]
- 20.Brand C.A., Harrison C., Tropea J., Hinman R.S., Britt H., Bennell K. Management of osteoarthritis in general practice in Australia. Arthritis Care Res. 2014;66(4):551–558. doi: 10.1002/acr.22197. [DOI] [PubMed] [Google Scholar]
- 21.Haskins R., Henderson J.M., Bogduk N. Health professional consultation and use of conservative management strategies in patients with knee or hip osteoarthritis awaiting orthopaedic consultation. Aust. J. Prim. Health. 2014;20(3):305–310. doi: 10.1071/PY13064. [DOI] [PubMed] [Google Scholar]
- 22.Bunzli S., Nelson E., Scott A., French S., Choong P., Dowsey M. Barriers and facilitators to orthopaedic surgeons' uptake of decision aids for total knee arthroplasty: a qualitative study. BMJ Open. 2017;7(11) doi: 10.1136/bmjopen-2017-018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Briggs A.M., Houlding E., Hinman R.S., Desmond L.A., Bennell K.L., Darlow B., et al. Health professionals and students encounter multi-level barriers to implementing high-value osteoarthritis care: a multi-national study. Osteoarthritis Cartilage. 2019;27(5):788–804. doi: 10.1016/j.joca.2018.12.024. [DOI] [PubMed] [Google Scholar]
- 24.Briggs A., Hinman R., Darlow B., Bennell K., Leech M., Pizzari T., et al. Confidence and attitudes toward osteoarthritis care among the current and emerging health workforce: a multinational interprofessional study. American College of Rheumatology. 2019;1(4):219–235. doi: 10.1002/acr2.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zadro J., O'Keeffe M., Maher C. Do physical therapists follow evidence-based guidelines when managing musculoskeletal conditions? Systematic review. BMJ Open. 2019;9(10) doi: 10.1136/bmjopen-2019-032329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barton C.J., Ezzat A.M., Bell E.C., Rathleff M.S., Kemp J.L., Crossley K.M. Knowledge, confidence and learning needs of physiotherapists treating persistent knee pain in Australia and Canada: a mixed-methods study. Physiother. Theory Pract. 2021 doi: 10.1080/09593985.2021.1906805. [DOI] [PubMed] [Google Scholar]
- 27.Wallis J., Ackerman I., Brusco N., Kemp J., Sherwood J., Young K., et al. Barriers and enablers to uptake of a contemporary guideline-based management program for hip and knee osteoarthritis: a qualitative study. Osteoarthritis and Cartilage Open. 2020;2(4):100095. doi: 10.1016/j.ocarto.2020.100095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roos E.M., Barton C.J., Davis A.M., McGlasson R., Kemp J.L., Crossley K.M., et al. GLA:D to have a high-value option for patients with knee and hip arthritis across four continents: Good Life with osteoArthritis from Denmark. Br. J. Sports Med. 2018 doi: 10.1136/bjsports-2017-098904. [DOI] [PubMed] [Google Scholar]
- 29.Skou S.T., Roos E.M. Good Life with osteoArthritis in Denmark (GLA:D™): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Muscoskel. Disord. 2017;18(1):72. doi: 10.1186/s12891-017-1439-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ageberg E., Link A., Roos E.M. Feasibility of neuromuscular training in patients with severe hip or knee OA: the individualized goal-based NEMEX-TJR training program. BMC Muscoskel. Disord. 2010;11:126. doi: 10.1186/1471-2474-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ageberg E., Nilsdotter A., Kosek E., Roos E.M. Effects of neuromuscular training (NEMEX-TJR) on patient-reported outcomes and physical function in severe primary hip or knee osteoarthritis: a controlled before-and-after study. BMC Muscoskel. Disord. 2013;14 doi: 10.1186/1471-2474-14-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.GLA D. D Denmark; 2020. Annual Report 2019 GLA. [Google Scholar]
- 33.Francis M., Kemp J., Dundules K., Wallis J., Roos E., Skou S., et al. Victorian Allied Health Research Conference. 2019. Implementing evidence based education and exercise for knee osteoarthritis. (Melbourne, Australia) [Google Scholar]
- 34.M Roos E., Grønne D.T., Skou S.T., Zywiel M., McGlasson R., Barton C., et al. Immediate outcomes following the GLA:D(R) program in Denmark, Canada and Australia. A longitudinal analysis including 28,370 patients with symptomatic knee and hip osteoarthritis. Osteoarthritis Cartilage. 2021;29(4):502. doi: 10.1016/j.joca.2020.12.024. [DOI] [PubMed] [Google Scholar]
- 35.Forman J., Heisler M., Damschroder L.J., Kaselitz E., Kerr E.A. Development and application of the RE-AIM QuEST mixed methods framework for program evaluation. Prev Med Rep. 2017;6:322–328. doi: 10.1016/j.pmedr.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nilsen P. Making sense of implementation theories, models and frameworks. Implement. Sci. 2015;10:53. doi: 10.1186/s13012-015-0242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pinnock H., Epiphaniou E., Sheikh A., Griffiths C., Eldridge S., Craig P., et al. Developing standards for reporting implementation studies of complex interventions (StaRI): a systematic review and e-Delphi. Implement. Sci. 2015;10:42. doi: 10.1186/s13012-015-0235-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pinnock H., Barwick M., Carpenter C.R., Eldridge S., Grandes G., Griffiths C.J., et al. Standards for reporting implementation studies (StaRI) statement. BMJ. 2017;356:i6795. doi: 10.1136/bmj.i6795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Glasgow R.E., Vogt T.M., Boles S.M. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am. J. Publ. Health. 1999;89(9):1322–1327. doi: 10.2105/AJPH.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huijg J.M., Gebhardt W.A., Dusseldorp E., Verheijden M.W., van der Zouwe N., Middelkoop B.J., et al. Measuring determinants of implementation behavior: psychometric properties of a questionnaire based on the theoretical domains framework. Implement. Sci. 2014;9:33. doi: 10.1186/1748-5908-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Michie S., van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hawker G.A., Mian S., Kendzerska T., French M. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP) Arthritis Care Res. 2011;63(Suppl 11):S240–S252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 43.Collins N.J., Prinsen C.A., Christensen R., Bartels E.M., Terwee C.B., Roos E.M. Knee Injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage. 2016;24(8):1317–1329. doi: 10.1016/j.joca.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 44.Devlin N.J., Shah K.K., Feng Y., Mulhern B., van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ. 2018;27(1):7–22. doi: 10.1002/hec.3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Busija L., Ackerman I.N., Haas R., Wallis J., Nolte S., Bentley S., et al. Adult measures of general health and health-related quality of life. Arthritis Care Res. 2020;72(Suppl 10):522–564. doi: 10.1002/acr.24216. [DOI] [PubMed] [Google Scholar]
- 46.Dobson F., Hinman R.S., Roos E.M., Abbott J.H., Stratford P., Davis A.M., et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage. 2013;21(8):1042–1052. doi: 10.1016/j.joca.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 47.Cohen J. A power primer. Psychol. Bull. 1992;112(1):155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 48.Braun V., Clarke V. What can "thematic analysis" offer health and wellbeing researchers? Int. J. Qual. Stud. Health Well-Being. 2014;9:26152. doi: 10.3402/qhw.v9.26152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Salaffi F., Stancati A., Silvestri C.A., Ciapetti A., Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain. 2004;8(4):283–291. doi: 10.1016/j.ejpain.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 50.Farrar J.T., Young J.P., LaMoreaux L., Werth J.L., Poole R.M. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/s0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 51.Monticone M., Ferrante S., Salvaderi S., Motta L., Cerri C. Responsiveness and minimal important changes for the Knee Injury and Osteoarthritis Outcome Score in subjects undergoing rehabilitation after total knee arthroplasty. Am. J. Phys. Med. Rehabil. 2013;92(10):864–870. doi: 10.1097/PHM.0b013e31829f19d8. [DOI] [PubMed] [Google Scholar]
- 52.Bilbao A., García-Pérez L., Arenaza J.C., García I., Ariza-Cardiel G., Trujillo-Martín E., et al. Psychometric properties of the EQ-5D-5L in patients with hip or knee osteoarthritis: reliability, validity and responsiveness. Qual. Life Res. 2018;27(11):2897–2908. doi: 10.1007/s11136-018-1929-x. [DOI] [PubMed] [Google Scholar]
- 53.Morris S.B., DeShon R.P. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol. Methods. 2002;7(1):105–125. doi: 10.1037/1082-989x.7.1.105. [DOI] [PubMed] [Google Scholar]
- 54.Briani R.V., Ferreira A.S., Pazzinatto M.F., Pappas E., De Oliveira Silva D., Azevedo F.M. What interventions can improve quality of life or psychosocial factors of individuals with knee osteoarthritis? A systematic review with meta-analysis of primary outcomes from randomised controlled trials. Br. J. Sports Med. 2018;52(16):1031–1038. doi: 10.1136/bjsports-2017-098099. [DOI] [PubMed] [Google Scholar]
- 55.Health D.o. Physiotherapists 2017 Factsheet. 2019 [Google Scholar]
- 56.Davis A.M., Kennedy D., Wong R., Robarts S., Skou S.T., McGlasson R., et al. Cross-cultural adaptation and implementation of Good Life with osteoarthritis in Denmark (GLA:D™): group education and exercise for hip and knee osteoarthritis is feasible in Canada. Osteoarthritis Cartilage. 2018;26(2):211–219. doi: 10.1016/j.joca.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 57.Jönsson T., Eek F., Dell'Isola A., Dahlberg L.E., Ekvall Hansson E. The better management of patients with osteoarthritis program: outcomes after evidence-based education and exercise delivered nationwide in Sweden. PloS One. 2019;14(9) doi: 10.1371/journal.pone.0222657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Walker A., Boaz A., Gibney A., Zambelli Z., Hurley M.V. Scaling-up an evidence-based intervention for osteoarthritis in real-world settings: a pragmatic evaluation using the RE-AIM framework. Implement Sci Commun. 2020;1:40. doi: 10.1186/s43058-020-00032-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Barton C.J., King M.G., Dascombe B., Taylor N.F., de Oliveira Silva D., Holden S., et al. Many physiotherapists lack preparedness to prescribe physical activity and exercise to people with musculoskeletal pain: a multi-national survey. Phys. Ther. Sport. 2021;49:98–105. doi: 10.1016/j.ptsp.2021.02.002. [DOI] [PubMed] [Google Scholar]
- 60.Leahy E., Chipchase L., Calo M., Blackstock F.C. Which learning activities enhance physical therapist practice? Part 1: systematic review and meta-analysis of quantitative studies. Phys. Ther. 2020 doi: 10.1093/ptj/pzaa107. [DOI] [PubMed] [Google Scholar]
- 61.Leahy E., Chipchase L., Calo M., Blackstock F.C. Which learning activities enhance physical therapist practice? Part 2: systematic review of qualitative studies and thematic synthesis. Phys. Ther. 2020 doi: 10.1093/ptj/pzaa108. [DOI] [PubMed] [Google Scholar]
- 62.Whiteley R., Napier C., van Dyk N., Barton C.J., Mitchell T., Beales D., et al. Clinicians use courses and conversations to change practice, not journal articles: is it time for journals to peer-review courses to stay relevant? Br. J. Sports Med. 2020 doi: 10.1136/bjsports-2020-102736. [DOI] [PubMed] [Google Scholar]
- 63.Bunzli S., O'Brien P., Ayton D., Dowsey M., Gunn J., Choong P., et al. Misconceptions and the acceptance of evidence-based nonsurgical interventions for knee osteoarthritis. A qualitative study. Clin. Orthop. Relat. Res. 2019;477(9):1975–1983. doi: 10.1097/CORR.0000000000000784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Caneiro J.P., O'Sullivan P.B., Roos E.M., Smith A.J., Choong P., Dowsey M., et al. Three steps to changing the narrative about knee osteoarthritis care: a call to action. Br. J. Sports Med. 2020;54:256–258. doi: 10.1136/bjsports-2019-101328. [DOI] [PubMed] [Google Scholar]
- 65.Wallis J.A., Taylor N.F., Bunzli S., Shields N. Experience of living with knee osteoarthritis: a systematic review of qualitative studies. BMJ Open. 2019;9(9) doi: 10.1136/bmjopen-2019-030060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Baumbach L., List M., Grønne D.T., Skou S.T., Roos E.M. Individualized predictions of changes in knee pain, quality of life and walking speed following patient education and exercise therapy in patients with knee osteoarthritis - a prognostic model study. Osteoarthritis Cartilage. 2020;28(9):1191–1201. doi: 10.1016/j.joca.2020.05.014. [DOI] [PubMed] [Google Scholar]
- 67.Pihl K., Roos E.M., Taylor R.S., Grønne D.T., Skou S.T. Associations between comorbidities and immediate and one-year outcomes following supervised exercise therapy and patient education - a cohort study of 24,513 individuals with knee or hip osteoarthritis. Osteoarthritis Cartilage. 2020 doi: 10.1016/j.joca.2020.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ackerman I., Skou S., Roos E., Barton C., Kemp J., Crossley K., et al. Implementing a national first-line management program for moderate-severe knee osteoarthritis in Australia: a budget impact analysis focusing on knee replacement avoidance. Osteoarthritis and Cartilage Open. 2020;2(3):100070. doi: 10.1016/j.ocarto.2020.100070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Terwee C.B., Roorda L.D., Dekker J., Bierma-Zeinstra S.M., Peat G., Jordan K.P., et al. Mind the MIC: large variation among populations and methods. J. Clin. Epidemiol. 2010;63(5):524–534. doi: 10.1016/j.jclinepi.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 70.Pham T., Van Der Heijde D., Lassere M., Altman R.D., Anderson J.J., Bellamy N., et al. Outcome variables for osteoarthritis clinical trials: the OMERACT-OARSI set of responder criteria. J. Rheumatol. 2003;30(7):1648–1654. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.