Abstract
Objective
Assess the feasibility of a virtually-delivered, physiotherapist-guided knee health program (SOAR) that targets self-management of knee health and osteoarthritis risk after an activity-related knee injury.
Design
In this quasi-experimental feasibility study, individuals with varied lived experience of knee trauma completed a 4-week SOAR program. This included: 1) Knee Camp (group education, 1:1 exercise and activity goal-setting); 2) weekly home-based exercise and activity program with tracking, and; 3) weekly 1:1 physiotherapy-guided action-planning. SOAR program feasibility was assessed with implementation (attrition, adherence, intervention fidelity), practicality (adverse events, goal completion), acceptability and efficacy (change in Knee injury and Osteoarthritis Outcome Score subscales, Patient Specific Functional Scale (PSFS), Godin Leisure-Time Exercise Questionnaire (GLTEQ), Partner in Health Scale (PHS)) outcomes. Descriptive statistics, disaggregated by gender, were calculated.
Results
Thirty participants (60% women, median (min-max) age 30 years (19–50), time from injury 5.6 years (1.2–25.2)) were enrolled. No participant attrition or adverse events were reported, and 90% of mandatory program components were completed. Participants rated their adherence at 80%, and 96% of exercise-therapy and 95% of activity goals were fully or partially achieved. Both women and men reported significant group mean (95%CI) improvements in GLTEQ scores (women: 22 METS (6,37), men: 31 METS (8,54)), while women alone reported improvements in PHS (−7 (−11,-3) and PSFS (1.7 (0.6,2.8) scores.
Conclusion
The SOAR program is feasible for persons at various timepoints post-knee trauma, and gender may be an important consideration for SOAR implementation and assessment. A randomized controlled trial to assess intervention efficacy is warranted.
Keywords: Anterior cruciate ligament, Knee trauma, Post-traumatic osteoarthritis, Physiotherapy
Abbreviations: OA, Osteoarthritis; SOAR, Stop OsteoARthritis; PT, Physiotherapy or Physical Therapy; RCT, Randomized Controlled Trial; ACL, Anterior Cruciate Ligament; KOOS, Knee injury and Osteoarthritis Outcome Score; GLTEQ, Godin Leisure Time Exercise Questionnaire; PSFS, Patient Specific Functional Scale; PHS, Partners in Health Scale; CARE, Consultation and Relational Empathy Measure; EARS, Exercise Adherence Rating Scale; RPE, Rating of Percieved Effort; SMART, Specific, Measurable, Attainable, Relevant, Time-bound; BAP, Brief Action Planning
1. Introduction
The Global Burden of Disease Study reports osteoarthritis (OA) as one of the fastest growing and burdensome conditions worldwide [1], driven primarily by knee OA [2]. As there is no cure for OA, effective and accessible prevention interventions that strategically target at-risk populations are urgently needed [3].
Knee trauma is associated with a 6-fold elevated risk of radiographic OA [4], and arthroplasty [5]. This risk varies by injury type with cruciate ligament, meniscal, fracture, dislocation and collateral ligament injuries associated with 5-fold or higher risk [4]. Knee trauma is most prevalent in persons aged 16–35 years, and most commonly activity-related [6]. We have also shown that youth who experienced activity-related knee trauma up to 10-years previous have more independent OA risk factors (i.e., quadricep weakness, inactivity, adiposity) [[7], [8], [9]] than uninjured peers. Despite carrying these modifiable risk factors, people at-risk of OA after knee trauma are often not aware of the risk, nor do they seek, or receive care to manage the risk [10,11].
The benefits of exercise for musculoskeletal health is well supported [12] and exercise-therapy and physical activity are essential to evidence-based knee trauma [13] and OA [14] management. Exercise also ameliorates several mechanisms (altered loading [15], inflammation [16]) and independent risk factors (muscle weakness [17], inactivity, adiposity [18]) for OA. Despite this, the current standard of care after discharge from knee trauma treatment (e.g., physiotherapy, surgery) is no care, and the value of exercise-based activities to modify OA risk factors after trauma is unclear [19]. Given that knee trauma permanently elevates OA risk, strategies that enhance self-management, exercise adherence, and healthy lifestyles, such as informational support and action-planning, are valuable adjuncts to exercise [[20], [21], [22]].
SOAR (Stop OsteoARthritis) is a virtually-delivered, physiotherapist (PT)-guided knee health program. SOAR aims to increase the capacity of persons living with elevated OA risk due to an activity-related knee injury to self-manage their knee health and knee OA risk. The program was developed alongside patient and clinician partners, and is based on past research [7,8,23,24], clinical practice guidelines [17], guidance from Developing and Evaluating Complex Interventions [25], and is consistent with patient-centered care [26], shared decision making [27] and behaviour change theory [28]. Preliminary information about the feasibility of the SOAR program is required before assessing it in ideal (efficacy) and then real-life (effectiveness) settings. The primary objective of this study was to evaluate the feasibility (i.e., program implementation, practicality, acceptability and preliminary efficacy) of a 4-week SOAR program in preparation for a randomized controlled trial (RCT). We hypothesized the SOAR program would be feasible for use with persons living with increased risk of post-traumatic knee osteoarthritis.
2. Methods
2.1. Study design and ethics
A quasi-experimental feasibility study. Feasibility assessments were guided by Bowen et al. [29] Reporting follows the Guidelines for Reporting Non-randomized Pilot and Feasibility studies [30], and Consensus on Exercise Reporting Template (CERT) [31]. The research was conducted at the University of British Columbia (UBC) and Arthritis Research Canada, Vancouver, Canada between October 2020 and March 2021 during the Corona Virus Disease of 2019 (COVID-19) pandemic. The study was approved by the UBC Clinical Research Ethics Board (REB #H20-00158) and all participants provided informed consent.
2.2. Participants
Participants were a convenience sample of individuals that had experienced an activity-related knee injury under the age of 45 years. Although SOAR targets active youth and young adults, older individuals with lived experience of a youth knee injury, and subsequent OA were included to gain their perspective. For this study, activity-related knee injury referred to a self-reported traumatic knee injury that required both medical consultation (i.e., physician, PTs, surgeon) and disrupted regular sport or recreational activity participation (i.e., missed at least one recreational, training or competition session). Injuries were categorized as including an anterior cruciate ligament (ACL) tear or other. Exclusion criteria included: inability to communicate in English; residency outside British Columbia (licensing jurisdiction for study PTs); pregnancy; inflammatory arthritis or systemic condition diagnosis; lower limb injury, surgery, or intra-articular injection in the past six-months; no email address or daily access to a computer with internet; or refusal to wear an activity tracker for the study duration.
2.3. Recruitment
To ensure the diversity of data, we balanced recruitment on gender (women and men), age (≤30 years or >30 years), injury type (ACL tear or other), and time since injury (≤5 years or >5 years). Participants were recruited through patient and clinician partners from community physiotherapy clinics, sport organizations, and social media channels (i.e., Twitter, Facebook, Instagram).
2.4. Sample size
Given the aim to assess program feasibility, sample size calculations were not undertaken. A convenience sample of 30 participants allowed for calculation of feasibility estimates and sufficient piloting of measurement procedures to inform a future RCT.
2.5. Procedures
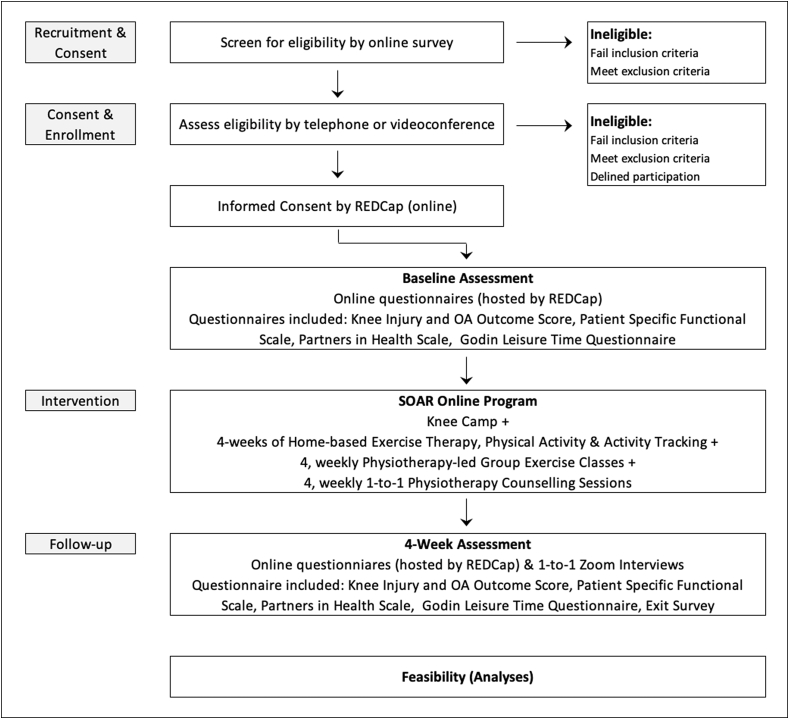
Fig. 1 outlines enrollment and study phases. After completing an online consent form, participants were sent a unique URL to a survey (REDCap 10.9.4, Vanderbilt University, US) consisting of a study questionnaire (demographic, socioeconomic, injury, treatment, medical history) and four self-report instruments (Knee Injury and OA Outcome Score; KOOS [32], the Patient Specific Functional Scale; PSFS [33], the Partners in Health Scale; PHS [34], Godin Leisure Time Exercise Questionnaire; GLTEQ) described below [35]. After survey completion, participants were scheduled for the intervention. At the end of the intervention, participants repeated the four self-report instruments and an online exit survey that included questions about satisfaction, and perceived value of SOAR, the Consultation and Relational Empathy Measure (CARE) [36], and Exercise Adherence Rating Scale (EARS) [37]. Participants were asked to answer all questions in reference to their past knee injury, or in the case of bilateral knee injuries, the one currently most symptomatic. Participants were advised to continue with their usual medication if applicable, during the study.
Fig. 1.
Flow of participants through the study.
2.6. Intervention
The intervention was a 4-week virtually-delivered PT-guided knee health program called SOAR (Stop OsteoARthritis). The program has three components: 1) one-time Knee Camp; 2) individualized weekly home-based exercise-therapy, physical activity and tracking, and; 3) weekly 1:1 PT-guided exercise-therapy and activity action-planning with optional group exercise class. Before starting, participants received a Fitbit Inspire™ activity tracker (Google, Mountain View, CA, USA), workbook (educational materials), and resistance loop set (Chimaera, Amazon, Seattle, WA, USA https://amzn.to/3mn7U7x) providing up to 100 pounds of resistance to enable exercise progression. Four registered PTs delivered the program.
Knee Camp: This 2-h videoconferencing (Zoom®, San Jose, CA, USA) session included a 1-h interactive group-based education session, 1:1 knee exam and exercise-therapy and physical activity goal-setting with a PT, and Fitbit® set-up. The education session covered topics approved by patient partners, consistent with shared decision making theory [27], clinical guidelines [13] and current understanding of OA (Table 1, Supplementary File 1 - Education session content). During the knee exam, PTs and participants co-identified and prioritized functional limitations. Exercise-therapy and activity goal-setting followed a Brief Action Planning (BAP) [22] approach (Fig. 1, Supplementary File 1 - BAP overview). Briefly, PTs guided participants to identify at least one individualized home-based exercise-therapy and one physical activity SMART (specific, measurable, attainable, relevant, and time-bound) goal with tasks and adequate dose (target Rating of Perceived Effort; RPE) [38] to address their unique functional limits (Table 2, Supplementary File 1 - Exemplar SMART Goals) for week 1. Participants could use the resistance band kit, body weight, common household materials (i.e., furniture, stairs), or any exercise equipment that they had access to when developing their dose. Given that higher confidence levels are associated with increased likelihood of success in carrying out a plan [22,47], goals were modified until participant's confidence to execute them rated 7/10 (0 = no confidence, 10 = full confidence). Actions to address perceived barriers were discussed. After agreeing to Fitbit's® privacy policy, participants were instructed to wear it 24-hrs/day and share their Fitbit® activity ‘Dashboard’ (proprietary Fitbit® software displaying information about daily step count, floors climbed, distance travelled, calories expended, and minutes of activity) with the research team through Fitbits®’ cloud-based platform. Finally, participants were orientated to TeleHab® (VALD Health, Newstead, QLD, Australia), a commercially available exercise tracking platform.
Table 1.
Outcomes, method and timeline of collection.
| Category | Outcome | Method | T0 | T1 | End |
|---|---|---|---|---|---|
| Participant Characteristics | Age, sex, gender, ethnicity, employment, education, sport participation, knee injury and medical history | Self-reported - study questionnaire | ✓ | ||
| Implementation | Participant Attrition | Drop-out rate – Master list | ✓ | ||
| Program Adherence | Mandatorya program component completion (%)- Study tracking form | Weekly | |||
| Non-mandatoryb program component completion (%) - Study tracking form | Weekly | ||||
| Exercise therapy tracking app use (%) – TeleHab® | Weekly | ||||
| Fitbit® wear daysc (number) - Fitbit® Dashboard | Weekly | ||||
| Participant Adherence | Self-reported - EARS | ✓ | |||
| Participant reported NRS of action plan completion | ✓ | ||||
| PT reported NRS of participant action plan completion | ✓ | ||||
| PT Intervention Fidelity | Fidelity checklist completion (%) | ✓ | |||
| Therapeutic Alliance | Self-reported - CARE | ✓ | |||
| Practicality | Adverse Events | PT Tracking form | Weekly | ||
| SMART goal completion | Exercise-therapy goal completion (%) - PT tracking form | Weekly | |||
| Physical activity goal completion (%) - from PT tracking form | Weekly | ||||
| Acceptability | Program component acceptability | Participant NRS of acceptability - Exit Survey | ✓ | ||
| Efficacy | Change in self-reported knee symptoms, function, QoL | KOOS | ✓ | ✓ | |
| Change in self-reported functional restrictions | PSFS | ✓ | ✓ | ||
| Change in self-reported perceived self-management | PHS | ✓ | ✓ | ||
| Change in self-reported physical activity | GLTQ | ✓ | ✓ | ||
CARE (Consultations and Relational Empathy Scale), EARS (Exercise Adherence Rating Scale), GLTEQ (Godin Leisure Time Exercise Questionnaire), KOOS (Knee Injury and Osteoarthritis Outcome Score), NRS (Numerical Rating Scale), PHS (Partner in Health Scale), PSFS (Patient Specific Functional Scale), QoL (quality-of-life), SMART (Specific, Measurable, Achievable, Relevant, Timebound), T0 (Baseline), T1 (4-weeks).
Mandatory Program components include knee camp and weekly 1:1 PT counselling sessions.
Non-mandatory Program components include the weekly group exercise classes.
A Fitbit wear day is ≥ 15 h of wear.
Table 2.
Participant characteristics.
| Characteristica | Womenb n = 18 | Menb n = 12 | Overall n = 30 |
|---|---|---|---|
| Age (years) | 30.5 (22.9–46.8) | 31.7 (19.5–50.8) | 30.8 (19.5–50.8) |
| Ethnicity (White), n (%) | 11 (61) | 9 (75) | 20 (67) |
| Highest education attained (Bachelor degree), n (%) | 9 (50) | 5 (42) | 14 (47) |
| Main pre-injury sport level (recreational), n (%) | 3 (17) | 7 (58) | 10 (33) |
| Injury age (years) | 22.0 (14.0–44.0) | 20.0 (17.0–34.0) | 21.4 (14–44) |
| Index knee injury type (ACL tear), n (%) | 9 (50) | 5 (42) | 12 (40) |
| Multi-structure index injury (yes), n (%) | 12 (67) | 3 (25) | 15 (50) |
| Index knee injury surgery (yes), n (%)c | 13 (72) | 4 (33) | 17 (57) |
| Index injury physiotherapy (yes), n (%) | 17 (94) | 10 (83) | 27 (90) |
| Sport participation in last year (yes), n (%) | 16 (89) | 11 (92) | 27 (90) |
| Time from injury to baseline (years) | 5.0 (1.2–18.1) | 7.6 (1.4–25.2) | 5.6 (1.2–25.2) |
Assessed at T0 (Baseline) with a self-reported study questionnaire.
Values represent median (min-max) unless otherwise noted.
14 participants had an Anterior Cruciate Ligament Reconstruction (10 women (8 primary ACL tears and 2 Tibio-femoral dislocations, 4 men (primary ACL tears)).
Weekly Home-based Exercise-Therapy, Physical Activity and Activity Tracking: At home, participants worked to meet their exercise-therapy and physical activity goals. Degree of exercise-therapy goal completion, RPE, and any associated pain was recorded in the TeleHab® application, and physical activity (Fitbit®) data synchronized with the Fitbit® online ‘Dashboard’.
Weekly PT-guided Exercise-Therapy and Physical Activity Action-Planning: Each week participants attended a short (∼15–30) 1:1 virtual PT counselling session and had the option of supplementing their program with a regularly scheduled 1-h virtual PT-guided group exercise class (Table 3, Supplementary File 1 - Group exercise class menu). At these sessions, PTs asked and recorded responses to questions related to adverse events, medication and healthcare use, reviewed Fitbit® wear (based on a synopsis of weekly Fitbit® data provided by the research team), and SMART goal completion on a bespoke PT tracking form. Participants and their PT progressively modified or added SMART exercise-therapy and physical activity goals (using a BAP approach) based on the past weeks goal completion, physical activity (Fitbit® Dashboard), symptoms and obstacles encountered. At group class, participants received added instruction and feedback about exercise performance and progression. Participants were able to email their PT between sessions as needed.
Table 3.
SOAR program implementation and practicality outcomes.
| Characteristic | Target | Womena n = 18 | Mena n = 12 |
|---|---|---|---|
| Mandatoryd components attendance (% participants with entire attendance)b | 80% | 89 | 92 |
| Non-mandatoryecomponents attenance (% participants with entire, and partial attendancef)b | – | 22, 44 | 17, 33 |
| Exercise tracking app use (number of participants, %)c | – | 14 (78) | 3 (25) |
| Fitbit daily wear (minutes)c | – | 1058 (950–1440) | 1107 (1010–1440) |
| Fitbit daily wear (hours)c | – | 18 (16–24) | 19 (17–24) |
| Fitbit wear daysg (number of days with ≥15 h)c | 24 days | 30 (20–30) | 29 (4–30) |
| Fitbit feasibility (number of participants ≥24 wear days, %)c | – | 10 (56) | 7 (58) |
| Exercise Adherence Rating Scale Scoreb | 18 (75%) | 22 (14–24) | 22 (17–24) |
| Exercise Adherence Rating Scale feasibility (n of participants ≥18, %)b | – | 17 (94) | 11 (92) |
| Participant rating of action plan completionh (%)b | 80 | 94 (81–100) | 93 (85–100) |
| Participant rating of action plan completionh feasibility (number of participants ≥80%)b | – | 18 (100) | 12 (100) |
| PT rating of action plan completioni (%)b | 80 | 80 (70–100) | 90 (60–100) |
| PT rating of action plan completioni feasibility (number of participants ≥80%)b | – | 17 (94) | 9 (75) |
| Consultation and Relational Empathy Scale Scoreb | 38 (75%) | 50 (35–50) | 50 (35–50) |
| Consultation and Relational Empathy Scale feasibility (n of participants ≥75%)b | – | 17 (94) | 11 (92) |
| Physical activity SMART goal entire or partial completion (% entire, % partial)c | 80 | 98 (77, 21) | 91 (81, 10) |
| Exercise-therapy SMART goal entire or partial completion (% entire, % partial)c | 80 | 99 (70, 29) | 93 (78, 15) |
‘-’ No ‘a priori’ target set.
Values represent median (min-max) unless otherwise noted.
Assessed at the end of the study.
Assessed weekly throughout the study.
Mandatory Program components include knee camp and four weekly 1:1 PT counselling sessions.
Non-mandatory Program components include 4 weekly group exercise classes.
Partial attendance refers to participants that attended 1, 2 or 3 of the 4 weekly group exercise classes.
Days with ≥15 h Fitbit wear up to a maximum of 30 days (study length).
Numercial rating scale (Overall, I completed the exercises and physical activities I planned as part of my weekly goals during the study, 0 = strongly disagree, 100 = strongly agree).
Numercial rating scale (Overall, the participant I worked with completed the exercises and physical activities as planned as part of their weekly goals during the study, 0 = strongly disagree, 100 = strongly agree).
Exercise-therapy and physical activity promote psychological and physical capability to modify knee health and OA risk factors, with all other program components supporting their regular performance [28]. Individualized exercise and physical activity tasks leverage automatic motivation and ensure relevant experiences [28]. Knee camp builds psychological capability with informational support [28], and opportunity for participants and PTs to initiate a therapeutic relationship [39]. Knee camp and weekly group classes provide social opportunity [23,28]. BAP builds reflexive motivation [28] and promotes self-efficacy, health behavior change, and long-term outcomes [22]. Goal-setting, and exercise and activity tracking facilitate adherence, and promote accountability and reflexive motivation [28,40]. Regular PT contact provides participants timely support to navigate obstacles by a health professional competent in exercise prescription for patient populations [41] and promotes exercise adherence [40]. Virtual delivery increases accessibility and physical opportunity [24,28].
2.7. Physiotherapist training
Prior to delivering the intervention, four registered musculoskeletal PTs completed BAP certification, SOAR program orientation and participated in a group debrief after completing a knee assessment and goal setting session with a simulated patient. BAP skills training and certification were conducted in coordination with the Centre for Collaboration, Motivation and Innovation (Vernon, BC, Canada). Certification (1-h role-play scenario) followed a 4-h asynchronous online course and three, 1-h group practice and feedback sessions. During SOAR orientation PTs were instructed in how use Zoom®, deliver the group education content, guide a standardized virtual knee exam, enter exercise-goals into TeleHab®, and complete a weekly PT Tracking form. After reviewing the recorded practice knee assessment and goal setting session, the principal investigator met with the PTs to review key components of BAP and SOAR program fidelity.
2.8. Outcomes
Outcomes, methods and timepoints for data collection are summarized in Table 1. Participant characteristics (i.e., age, sex, gender, ethnicity, socioeconomic status), sport and physical activity participation in the past year, knee injury history and treatment, as well as medical history were captured using a study questionnaire. The feasibility of the SOAR program was assessed with implementation, practicality, acceptability and preliminary efficacy outcomes [29].
SOAR Implementation outcomes included participant attrition (% of participants who withdrew or lost to follow-up), program adherence (% of knee camp, weekly 1:1 PT counselling sessions and weekly group classes attended, % of exercise therapy tracking completed, number of days with ≥15 h of Fitbit® wear), participant adherence (EARS, Participant Numerical Rating Scale of Action Plan Completion, PT Numerical Rating Scale of Participant Action Plan Completion), PT intervention fidelity (% of a 41-item checklist completed during one randomly recorded 1:1 knee camp and one weekly counselling sessions per PT; Table 4, Supplementary File 1 – Intervention Fidelity Checklist), and relational empathy (CARE) which is a key component of therapeutic relationship. A 15-h cut-off to define a ‘Fitbit® wear day’ was chosen to understand the proportion of participants that would wear the device for a duration equivalent to typical waking hours (16-h) less 1 h for bathing (i.e., the typical daily period during which participants would have the potential for being physically active). The EARS is a six-item self-report tool for measuring adherence to home exercise. Scores range from 0 to 42, with higher scores indicating better adherence [37]. The CARE is a 10-item self-report tool that measures empathy in the context of the therapeutic relationship between a clinician and a patient. Scores range from 10 to 50, with higher scored reflecting more empathy [36].
Table 4.
SOAR Efficacy Outcomes (intention to treat)a.
| Outcome | Women (n = 18) |
Men (n = 12) |
||||
|---|---|---|---|---|---|---|
| Baseline (T0) Median (min-max) | End (T1) Median (min-max) | Change (T1-T0) Mean (95%CI) | Baseline (T0) Median (min-max) | End (T1) Median (min-max) | Change (T1-T0) Mean (95%CI) | |
| KOOSPaind | 83 (58–100) | 86 (47–100) | 1.3 (−3.5,6.0) | 88 (69–97) | 86 (75–100) | 2.1 (−3.3,7.5) |
| KOOSSympd | 55 (36–79) | 54 (39–75) | 1.8 (−1.7,5.3) | 57 (43–71) | 63 (43–68) | 1.2 (−4.2,6.6) |
| KOOSADLd | 98 (79–100) | 96 (53–100) | −1.6 (−8.1,4.8) | 98 (81–100) | 96 (81–100) | 0.6 (−3.4,4.6) |
| KOOSSR | 73 (45–95) | 90 (25–100) | 8.3 (−2.3,19.0) | 75 (50–100) | 75 (50–100) | 3.8 (−6.7,14.1) |
| KOOSQoL | 47 (25–81) | 56 (0–88) | 6.6 (−1.4,14.6) | 50 (25–88) | 56 (44–88) | 6.8 (−2.5,16.1) |
| KOOSPF | 74 (41–91) | 78 (27–96) | 6.3 (−1.3,14.0) | 76 (50–91) | 71 (57–96) | 1.5 (−6.2,9.2) |
| PSFSb | 5 (0–7) | 6 (2–9) | 1.7 (0.6,2.8) | 6 (3–8) | 6 (4–8) | −0.4 (−1.9,1.1) |
| PHS | 20 (5–37) | 8 (0–32) | −7 (-11,-3) | 20 (0–41) | 11 (2–30) | −5 (−13,4) |
| GLTQc | 56 (13–118) | 71 (37–224) | 22 (6,37) | 66 (23–92) | 90 (35–185) | 31 (8,54) |
T0 (Baseline), T1 (4-weeks).
Bold: mean change 95% confidence interval does not contain the null value.
See Supplementary File 1 for a sensitivity analysis where data from one participant who experienced a time loss knee injury in the first week of the program during a non-SOAR related event is removed.
Average across three goals.
Metabolic equivalents.
As per Collins et al., 2016,37 KOOS pain, symptoms and function in daily living have limited validity for this patient group and would not be expected to change.
SOAR Practicality outcomes included the number of self-reported adverse events (requiring medical treatment or medications, and/or interferes with function for two or more days directly related to SOAR) [42] over the course of the intervention, and exercise-therapy and physical activity goal completion (% of goals entirely, partially or not completed) tracked weekly at the PT counselling sessions. Exercise-therapy and physical activity goals were coded as ‘completed’, ‘partially completed’ or ‘not completed’ when the participant reported ‘entirely achieving a weekly goal’, ‘achieving some (but not all) of a weekly goal’, or ‘not achieving any part of a weekly goal’, respectively.
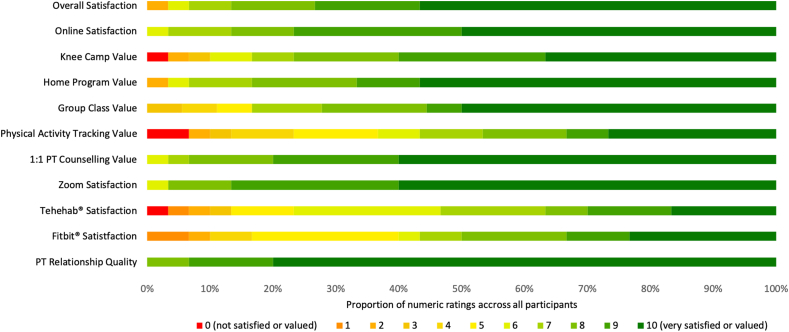
Finally, SOAR acceptability was assessed with an exit survey consisting of 10 questions that asked participants to rate the value of various aspects of the SOAR program (i.e., overall program, online delivery, knee camp, home-based component, weekly group classes, weekly PT counselling, Zoom® platform, TeleHab® for exercise-tracking, Fitbit for physical activity tracking, quality of the relationship with their PT) on a 0–10 numerical rating scale (i.e., 0 = not satisfied or valued, 10 = very satisfied or valued).
Preliminary efficacy was assessed as the change in self-reported knee-related symptoms, function and quality-of-life (KOOS) [32], self-chosen functional restrictions (PSFS) [33] perceived self-care (PHS) [34], and physical activity (GLTEQ) [35] over the 4-week program. The KOOS consists of 53 items, scored on a 5-point Likert scale, organised in six subscales (i.e., pain, other symptoms, function in daily living, function in sport and recreation, quality-of-life, patellofemoral symptoms). Subscale scores are summed, and the total score transformed to a 0–100 scale with higher scores indicating better outcome. The KOOS has been validated in various knee injury, surgery and OA populations, and has been shown to have high test-retest reliability [32,43]. The PSFS prompts participants to identify three activities important to them and rate their ability to perform each on a 10-point numerical rating scale. Individual scale scores are summed and transformed to a 0–100 scale with higher scores indicating better outcomes. The PSFS is valid and reliable for use in persons with a knee injury [44]. The PHS consists of 11-items across three domains (i.e., self-efficacy, knowledge of health condition and treatment, and self-management behaviour) scored on a nine-point Likert scale. Individual items are summed to produce a total score, out of 88 with lower scores representing greater perceived self-management [34]. The PHS is valid and reliable across numerous chronic conditions [45]. Finally, the GLTEQ uses the number of 15-min bouts of mild, moderate, and strenuous physical activity that a person engages in over a typical week to estimate weekly metabolic equivalents (METS) of physical activity. The GLTEQ is a valid measure of leisure time physical activity [46].
2.9. Patient and clinician partner involvement
Three patient partners (young adult with lived experience of a sport-related ACL reconstruction, middle-aged adult with lived experience of a sport-related ACL reconstruction, re-injury, and recent knee OA diagnosis, and a middle-aged adult with lived experience of a sport-related ACL reconstruction, knee OA and knee arthroplasty), and three clinician partner (two PTs with 9-years of clinical experience and one PT with 3-years) were engaged throughout the study. The patient and PT partners provided guidance on research objectives, appropriateness of outcomes, funding applications, and the development of the exit survey, SOAR participant workbook and Knee Camp content. They also participated in recruitment, and data analysis interpretation.
2.10. Statistical analyses
Descriptive statistics for all participant characteristics, outcomes and open-ended survey responses were summarized by gender given their socio-cultural nature. A priori benchmarks were set for key implementation and practicality outcomes based on past feasibility studies [47,48] and clinical experience. These included: participant attrition 10%; 80% knee-camp and weekly session attendance; 24 out of 30 Fitbit wear days (≥15-h of daily wear); median EARS score of 18 (75% adherence); 80% participant numerical rating of adherence, 80% PT numerical rating of participant adherence, 75% intervention fidelity; median CARE measure score of 38 (75% relationship empathy); 80% full or partial SMART goal completion.
3. Results
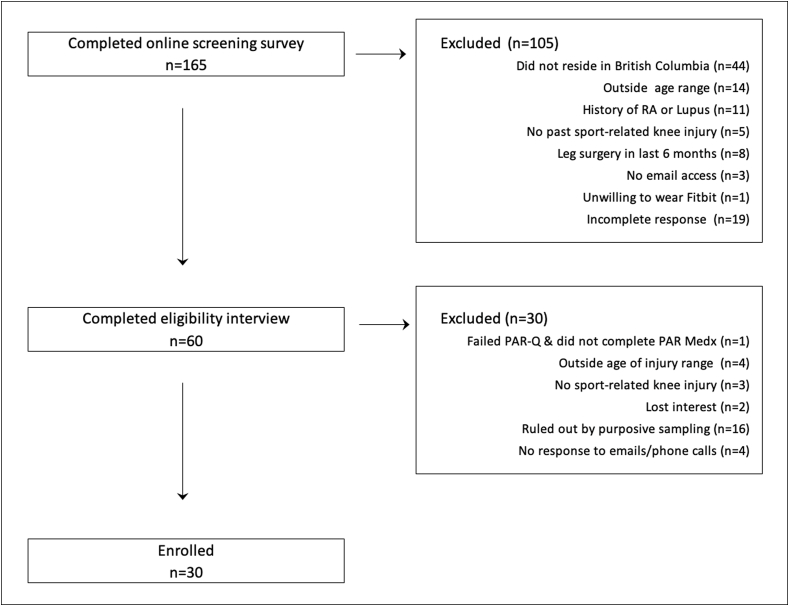
Enrollment is outlined in Fig. 2 and participant characteristics are summarized in Table 2. The majority of participants were in their twenties (37%) and thirties (33%), White (67%), cis-gendered (100%), and had participated in organized sport in the last year (90%). Main pre-injury sports included soccer (20%), volleyball (17%), basketball (10%), ice hockey (10%), American football (10%), rugby (7%), ultimate frisbee (7%), biking (3%), boxing (3%), downhill skiing (3%), horse sport (3%), running (3%), wakeboarding (3%).
Fig. 2.
Overview of study enrollment. PAR-Q (Physical Activity Readiness Questionnaire), PAR MEDx (Physical Activity Readiness Medical Examination).
No participants were lost to follow-up. One participant suffered a time loss index knee injury (MRI-confirmed traumatic medial meniscal tear) in the first week during a non-SOAR related event which required significant program modifications, and one was rescheduled and completed the program at a later start date due to an unexpected non-related minor medical procedure. No adverse events (event directly related to SOAR requiring medical treatment or medications, and/or interfered with function for two or more days) occurred, and all participants completed the assessment protocol.
Program implementation and practicality outcomes are summarized in Table 3, and acceptability outcomes in Fig. 3. All participants attended knee camp and 27 (90%) attended all weekly PT counselling sessions. Of the three (10%) participants that missed a weekly PT counselling session, two were due to scheduling difficulties and one requested two weeks to work on their goals. Although weekly group exercise classes were not mandatory, 60% of participants attended one or more exercise classes (43% attended ≥ two, 30% attended ≥ three, and 20% attended all four classes). Seventeen (56.7%) participants used the exercise-tracking application, and Fitbit® data was available for 23 (77%) participants (five women and two men failed to synchronize their device with the Fitbit® Dashboard and did not register data). Participants self-reported high rates of program adherence, with 95% of physical activity and 96% of exercise-therapy SMART goals either entirely or partially completed across the study period. One participant did not set a week one physical activity goal deciding to focus on therapeutic exercises only.
Fig. 3.
Summary of participants numerical rating of SOAR program components acceptability.
The median (range) proportion of intervention fidelity checklist items completed across the four PTs was 91% (61–98). The most common BAP element not completed was the approach PTs took to offer an ‘Exercise or Activity Menu’ to participants when they did not know where to start working on their knee health, or requested ideas. Participants reported high relational empathy, and 28 (93%) highly valued (≥9/10) their relationship with their PT.
Preliminary efficacy outcomes are summarized in Table 4. Both women and men reported significant increases in self-reported physical activity, while women reported improvements in perceived self-management and functional activities identified on the PSFS. When data from one participant who experienced a time loss knee injury in the first week of the program during a non-SOAR related event was removed, women also demonstrated clinically relevant improvements in self-reported function in sport and recreation function, knee-related quality-of-life and patellofemoral symptoms (Supplementary File 2).
4. Discussion
This study demonstrates the feasibility of a virtually-delivered, PT-guided knee health program that targets self-management of knee health and OA risk after activity-related knee trauma. All a priori feasibility benchmarks were met or exceeded, including targets for participant attrition, program and participant adherence, intervention fidelity, and full or partial completion of weekly SMART goals. No adverse events were reported, and mean change improvements in self-reported physical activity (both men and women), perceived self-management (women only) and function (women only) were demonstrated. Participants also reported high perceived-value of the program including the online format, online platform, weekly PT-guided action-planning and group exercise sessions, and quality of the relationship with their PT. Components of the SOAR program that may require modification include aspects of PT training related to BAP, and method for tracking exercise-therapy and physical activities. These findings suggest it is appropriate to proceed with an RCT to determine the ideal length and efficacy of the SOAR program [51].
Two key aspects of program implementation of specific interest in exercise-based interventions are participant adherence, and intervention fidelity. Adherence refers to the extent to which a person's behaviour corresponds with agreed upon approach. Although difficult to measure, adherence is associated with exercise-therapy effectiveness in persons with knee conditions [49]. To fully understand participant adherence, we considered multiple outcomes (i.e., attendance, EARS score, participant numerical rating of action-plan completion, PT numerical rating of participant action-plan completion, SMART goal completion). Based on findings ranging from 80% on the PT numerical rating of participant action-plan completion to 96% full or partial completion of exercise-therapy SMART goals there was consistent evidence of high participant adherence across the program. These results are more favorable than those reported for other exercise intervention in similar populations [48], and may be related to the use of action-planning, a behavioural change technique positively associated with exercise adherence [28], and meaningful therapeutic relationships between participants and their PT [39].
With respect to intervention fidelity, we used a checklist (including items indicating meaningful relationship, knee assessment conduct, BAP, and record keeping) to assess one randomly recorded 1:1 knee camp and one weekly action-planning session per PT. Although the median intervention fidelity exceeded a priori targets (91%), we identified several areas with lower fidelity including consistent deviations in BAP when participants stated that they did not know where to start working on their knee health or requested ideas. Instead of offering two or three brief ideas together as a list without pauses, and then asking participants if they had any ideas come to mind as the last list item, PTs commonly assumed the ‘expert’ role, which is a deviation from the spirit of BAP, and chose exercises for participants. These findings will inform modifications to future PT training. Specifically, more opportunity to practice and receive feedback on BAP within the context of SOAR, completion of simulations of scenarios where a participant requests exercise or physical activity ideas from the PT, and addition of a requirement to shadow at least one action-planning session.
A unique aspect of the SOAR program which improves its accessibility, is the online approach and use of commercially available platforms (i.e., Zoom®, TeleHab®) and activity monitors (Fitbit®). Participants reported a high degree of acceptability for the Zoom® platform which was likely influenced by increased familiarity and acceptance of videoconferencing and online services during to the COVID-19 pandemic. Despite the value of exercise logs as an active coping strategy after injury [23], and activity trackers for motivating people to achieve activity goals [50], the least valued part of the program was using the TeleHab® application for exercise and physical activity tracking, and the Fitbit®. It is unclear if the high degree of acceptability of videoconferencing will persist beyond the COVID-19 pandemic or if there will be a need to move towards more in-person delivery of the program. Preliminary participant feedback from 1:1 interviews (which will be reported in-depth elsewhere) about barriers to using TeleHab® included lack of relevance (could remember without tracking), time, and technical issues. Barriers to Fitbit® use included a perception that it was less accurate than other commercially available activity trackers, and need for manual synchronization. These findings will inform adaptations for exercise-therapy and physical activity tracking. Options may include developing a purpose-built online tracking form with a user-friendly, mobile-device interface, having research staff set-up participants’ Fitbit® accounts, providing education and reminders for Fitbit® synchronization, or not requiring it be worn during sleep.
A strength of the study is that we have demonstrated the feasibility of the SOAR program with persons who have a wide range of time loss, medical-attention knee injuries and who may be at various stages of recovery and different levels of OA risk. Although mean changes in self-reported physical activity (women and men), perceived self-management (women only) and function (women only) were demonstrated, these findings must be interpreted with caution. As the aim of this study was to assess the feasibility of the SOAR program there was no control group, the intervention likely not of sufficient length to effect a true change, and no sample size calculations performed. A limitation of the intervention is the need for daily access to a computer and the internet which may have implications for equitable access if SOAR found to be effective in future studies. It is interesting to note that gender may play a role in the efficacy of the SOAR program. This is not surprising given that women and men have different preferences for exercise, physical activity and sport, and that social support facilitates exercise and physical activity behaviours by girls and women, more than with boys and men. These findings suggest that gender will be an important consideration for SOAR implementation (i.e., tailor for participant gender) and assessment going forward.
5. Conclusion
A novel exercise-based, PT-guided knee health program that targets self-management of knee health and osteoarthritis risk after an activity-related knee injury is feasible, and a RCT to assess its efficacy is warranted. Beyond meeting all feasibility criteria, opportunities for improving PT training and participant exercise and physical activity tracking were identified. The importance of considering gender during implementation and assessment of the program was also highlighted. This research represents a first, vital step towards mitigating the consequences of activity-related knee injuries and the burden of OA.
Author contributions
All authors were involved in the design of the study. Data collection and initial analyses was conducted by JLW, LKT, JML. JLW wrote the first draft of the manusript. All authors contributed to reviewing, editing, and revising the manuscript and approved the final submitted version. JLW is the guarantor.
Role of funding sources
Funding to conduct this study came from the BC support Unit, Canadian MSK Rehab Research Network (CIHR FRN: CFI-148081) and Arthritis Society. JLW is supported by the Michael Smith Foundation for Health Research and the Arthritis Society. JML is supported by the Arthritis Society. LKT is supported by a Canadian Institutes of Health Research Fellowship.
Declaration of competing interest
JLW is an Associate Editor of the British Journal of Sports Medicine (BJSM) and Journal of Orthopaedic and Sports Physical Therapy. ER is Deputy Editor of Osteoarthritis and Cartilage.
Acknowledgements
The authors would like to acknowledge the administrative support of Shireen Divecha, Kiran Dhiman, and Hussein Mamdani, as well as contributions of Declan Norris PT.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ocarto.2022.100239.
Contributor Information
Jackie L. Whittaker, Email: jackie.whittaker@ubc.ca.
Linda K. Truong, Email: linda.truong@ubc.ca.
Trish Silvester-Lee, Email: trishsl@telus.net.
Justin M. Losciale, Email: jlos18@student.ubc.ca.
Maxi Miciak, Email: maxi@ualberta.ca.
Andrea Pajkic, Email: apajkic@ualberta.ca.
Christina Y. Le, Email: cyle@ualberta.ca.
Alison M. Hoens, Email: alison.hoens@ubc.ca.
Amber D. Mosewich, Email: amber.mosewich@ualberta.ca.
Michael A. Hunt, Email: michael.hunt@ubc.ca.
Linda C. Li, Email: lli@arthritisresearch.ca.
Ewa M. Roos, Email: eroos@health.sdu.dk.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Safiri S., Kolahi A.A., Smith E., Hill C., et al. Global, regional and national burden of osteoarthritis 1990-2017: a systematic analysis of the Global Burden of Disease Study 2017. Ann. Rheum. Dis. 2020;79(6):819–828. doi: 10.1136/annrheumdis-2019-216515. [DOI] [PubMed] [Google Scholar]
- 2.Yu D., Jordan K.P., Bedson J., Englund M., et al. Population trends in the incidence and initial management of osteoarthritis: age-period-cohort analysis of the Clinical Practice Research Datalink. Rheumatol. 2017;56(11):1902–1917. doi: 10.1093/rheumatology/kex270. 1992-2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whittaker J.L., Runhaar J., Bierma-Zeinstra S., Roos E.M. A lifespan approach to osteoarthritis prevention. Osteoarthritis Cartilage. 2021 doi: 10.1016/j.joca.2021.06.015. [DOI] [PubMed] [Google Scholar]
- 4.Snoeker B., Turkiewicz A., Magnusson K., Frobell R., et al. Risk of knee osteoarthritis after different types of knee injuries in young adults: a population-based cohort study. Br. J. Sports Med. 2020;54(12):725–730. doi: 10.1136/bjsports-2019-100959. [DOI] [PubMed] [Google Scholar]
- 5.Fernandes G.S., Parekh S.M., Moses J., Fuller C., et al. Prevalence of knee pain, radiographic osteoarthritis and arthroplasty in retired professional footballers compared with men in the general population: a cross-sectional study. Br. J. Sports Med. 2018;52(10):678–683. doi: 10.1136/bjsports-2017-097503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gianotti S.M., Marshall S.W., Hume P.A., Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J. Sci. Med. Sport. 2009;12(6):622–627. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Toomey C.M., Whittaker J.L., Nettel-Aguirre A., Reimer R.A., et al. Higher fat mass is associated with a history of knee injury in youth sport. J. Orthop. Sports Phys. Ther. 2017;47(2):80–87. doi: 10.2519/jospt.2017.7101. [DOI] [PubMed] [Google Scholar]
- 8.Whittaker J.L., Toomey C.M., Nettel-Aguirre A., Jaremko J.L., et al. Health-related outcomes following a youth sport-related knee injury. Med. Sci. Sports Exerc. 2018;51(2):255–263. doi: 10.1249/MSS.0000000000001787. [DOI] [PubMed] [Google Scholar]
- 9.Ezzat A.M., Brussoni M., Whittaker J.L., Emery C.A. A qualitative investigation of the attitudes and beliefs about physical activity and post-traumatic osteoarthritis in young adults 3-10years after an intra-articular knee injury. Phys. Ther. Sport. 2018;32:98–108. doi: 10.1016/j.ptsp.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 10.Feucht M.J., Cotic M., Saier T., Minzlaff P., et al. Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2016;24(1):201–207. doi: 10.1007/s00167-014-3364-z. [DOI] [PubMed] [Google Scholar]
- 11.Marshall D.A., Currie G.R., Whittaker J.L., Emery C.A. Matched comparison of health care use and costs 3-10 years after a youth sport-related knee injury. Osteoarthritis Cartilage. 2019;21(1):e65. [Google Scholar]
- 12.Bricca A., Wirth W., Juhl C.B., Kemnitz J., et al. Moderate physical activity and prevention of cartilage loss in people with knee osteoarthritis: data from the osteoarthritis initiative. Artherits Care Res. 2019;71(2):218–226. doi: 10.1002/acr.23791. [DOI] [PubMed] [Google Scholar]
- 13.Andrade R., Pereira R., van Cingel R., Staal J.B., et al. How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II) Br. J. Sports Med. 2019 doi: 10.1136/bjsports-2018-100310. [DOI] [PubMed] [Google Scholar]
- 14.Fransen M., McConnell S., Harmer A.R., Van der Esch M., et al. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br. J. Sports Med. 2015;49(24):1554–1557. doi: 10.1136/bjsports-2015-095424. [DOI] [PubMed] [Google Scholar]
- 15.Thorstensson C.A., Henriksson M., von Porat A., Sjodahl C., et al. The effect of eight weeks of exercise on knee adduction moment in early knee osteoarthritis--a pilot study. Osteoarthritis Cartilage. 2007;15(10):1163–1170. doi: 10.1016/j.joca.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Kim K.B., Kim K., Kim C., Kang S.J., et al. Effects of exercise on the body composition and lipid profile of individuals with obesity: a systematic review and meta-analysis. J. Obes. Metab. Syndr. 2019;28(4):278–294. doi: 10.7570/jomes.2019.28.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Logerstedt D.S., Scalzitti D., Risberg M.A., Engebretsen L., et al. Knee stability and movement coordination impairments: knee ligament sprain revision 2017. J. Orthop. Sports Phys. Ther. 2017;47(11):A1–A47. doi: 10.2519/jospt.2017.0303. [DOI] [PubMed] [Google Scholar]
- 18.Silverwood V., Blagojevic-Bucknall M., Jinks C., Jordan J.L., et al. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23(4):507–515. doi: 10.1016/j.joca.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 19.Duncan K.J., Chopp-Hurley J.N., Maly M.R. A systematic review to evaluate exercise for anterior cruciate ligament injuries: does this approach reduce the incidence of knee osteoarthritis? Open Access Rheumatol. 2016;8:1–16. doi: 10.2147/OARRR.S81673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holt C.J., McKay C.D., Truong L.K., Le C.Y., et al. Sticking to it: a scoping review of adherence to exercise therapy interventions in children and adolescents with musculoskeletal conditions. J. Orthop. Sports Phys. Ther. 2020;50(9):503–515. doi: 10.2519/jospt.2020.9715. [DOI] [PubMed] [Google Scholar]
- 21.Simonsmeier B.A., Flaig M., Simacek T., Schneider M. What sixty years of research says about the effectiveness of patient education on health: a second order meta-analysis. Health Psychol. Rev. 2021:1–25. doi: 10.1080/17437199.2021.1967184. [DOI] [PubMed] [Google Scholar]
- 22.Gutnick D., Reims K., Davis C., Gainforth H., et al. Brief action planning to facilitate behavior change and support patient self-management. J. Clin. Outcome Manag. 2014;21(1):17–29. [Google Scholar]
- 23.Truong L.K., Mosewich A.D., Holt C.J., Le C.Y., et al. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: a scoping review. Br. J. Sports Med. 2020 doi: 10.1136/bjsports-2019-101206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Truong L.K., Mosewich A.D., Miciak M., Pajkic A., et al. Balance, reframe, and overcome: the attitudes, priorities, and perceptions of exercise-based activities in youth 12-24 months after a sport-related ACL injury. J. Orthop. Res. 2021 doi: 10.1002/jor.25064. [DOI] [PubMed] [Google Scholar]
- 25.Craig P., Dieppe P., Macintyre S., Michie S., et al. Developing and evaluating complex interventions2019 January 13. 2020. https://mrc.ukri.org/documents/pdf/complex-interventions-guidance/ Available from:
- 26.Mead N., Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ. Counsel. 2002;48(1):51–61. doi: 10.1016/s0738-3991(02)00099-x. [DOI] [PubMed] [Google Scholar]
- 27.Legare F., Ratte S., Stacey D., Kryworuchko J., et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst. Rev. 2010;5:CD006732. doi: 10.1002/14651858.CD006732.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Michie S., van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bowen D.J., Kreuter M., Spring B., Cofta-Woerpel L., et al. How we design feasibility studies. Am. J. Prev. Med. 2009;36(5):452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lancaster G.A., Thabane L. Guidelines for reporting non-randomised pilot and feasibility studies. Pilot Feasibility Stud. 2019;5:114. doi: 10.1186/s40814-019-0499-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Slade S.C., Dionne C.E., Underwood M., Buchbinder R. Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br. J. Sports Med. 2016;50(23):1428–1437. doi: 10.1136/bjsports-2016-096651. [DOI] [PubMed] [Google Scholar]
- 32.Collins N.J., Prinsen C.A., Christensen R., Bartels E.M., et al. Knee Injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage. 2016;24(8):1317–1329. doi: 10.1016/j.joca.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 33.Stratford P., Gill C., Westaway M., Binkley J. Assessing disability and change on individual patients” a report of a patient specific measure. Physiother. Can. 1995;47:258–263. [Google Scholar]
- 34.Petkov J., Harvey P., Battersby M. The internal consistency and construct validity of the partners in health scale: validation of a patient rated chronic condition self-management measure. Qual. Life Res. 2010;19(7):1079–1085. doi: 10.1007/s11136-010-9661-1. [DOI] [PubMed] [Google Scholar]
- 35.Amireault S., Godin G. The Godin-Shephard leisure-time physical activity questionnaire: validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Percept. Mot. Skills. 2015;120(2):604–622. doi: 10.2466/03.27.PMS.120v19x7. [DOI] [PubMed] [Google Scholar]
- 36.Mercer S.W., Maxwell M., Heaney D., Watt G.C. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam. Pract. 2004;21(6):699–705. doi: 10.1093/fampra/cmh621. [DOI] [PubMed] [Google Scholar]
- 37.Newman-Beinart N.A., Norton S., Dowling D., Gavriloff D., et al. The development and initial psychometric evaluation of a measure assessing adherence to prescribed exercise: the Exercise Adherence Rating Scale (EARS) Physiotherapy. 2017;103(2):180–185. doi: 10.1016/j.physio.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 38.Lovegrove S., Hughes L.J., Mansfield S.K., Read P.J., et al. Repetitions in reserve is a reliable tool for prescribing resistance training load. J. Strength Condit Res. 2021 doi: 10.1519/jsc.0000000000003952. Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 39.Babatunde F., MacDermid J., MacIntyre N. Characteristics of therapeutic alliance in musculoskeletal physiotherapy and occupational therapy practice: a scoping review of the literature. BMC Health Serv. Res. 2017;17(1):375. doi: 10.1186/s12913-017-2311-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nicolson P.J.A., Hinman R.S., French S.D., Lonsdale C., et al. Improving adherence to exercise: do people with knee osteoarthritis and physical therapists agree on the behavioral approaches likely to succeed? Arthritis Care Res. 2018;70(3):388–397. doi: 10.1002/acr.23297. [DOI] [PubMed] [Google Scholar]
- 41.Davis A.M., Chahal J., Wong R., Steinhart K., et al. Limiting the risk of osteoarthritis after anterior cruciate ligament injury: are health care providers missing the opportunity to intervene? Arthritis Care Res. 2020 doi: 10.1002/acr.24419. [DOI] [PubMed] [Google Scholar]
- 42.Bennell K.L., Nelligan R.K., Kimp A.J., Wrigley T.V., et al. Comparison of weight bearing functional exercise and non-weight bearing quadriceps strengthening exercise on pain and function for people with knee osteoarthritis and obesity: protocol for the TARGET randomised controlled trial. BMC Muscoskel. Disord. 2019;20(1):291. doi: 10.1186/s12891-019-2662-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Crossley K.M., Macri E.M., Cowan S.M., Collins N.J., et al. The patellofemoral pain and osteoarthritis subscale of the KOOS (KOOS-PF): development and validation using the COSMIN checklist. Br. J. Sports Med. 2017 doi: 10.1136/bjsports-2016-096776. [DOI] [PubMed] [Google Scholar]
- 44.Chatman A.B., Hyams S.P., Neel J.M., Binkley J.M., et al. The patient-specific functional scale: measurement properties in patients with knee dysfunction. Phys. Ther. 1997;77(8) doi: 10.1093/ptj/77.8.820. [DOI] [PubMed] [Google Scholar]
- 45.Smith D., Harvey P., Lawn S., Harris M., et al. Measuring chronic condition self-management in an Australian community: factor structure of the revised Partners in Health (PIH) scale. Qual. Life Res. 2017;26(1):149–159. doi: 10.1007/s11136-016-1368-5. [DOI] [PubMed] [Google Scholar]
- 46.Miller D.J., Freedson P.S., Kline G.M. Comparison of activity levels using Caltrac accelerometer and five questionnaires. Med. Sci. Sports Exerc. 1994;26:376–382. [PubMed] [Google Scholar]
- 47.Li L.C., Sayre E.C., Xie H., Clayton C., et al. A community-based physical activity counselling program for people with knee osteoarthritis: feasibility and preliminary efficacy of the track-OA study. JMIR Mhealth Uhealth. 2017;5(6):e86. doi: 10.2196/mhealth.7863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Patterson B.E., Barton C.J., Culvenor A.G., Cooper R.L., et al. Exercise-therapy and education for individuals one year after anterior cruciate ligament reconstruction: a pilot randomised controlled trial. BMC Muscoskel. Disord. 2021;22(1):64. doi: 10.1186/s12891-020-03919-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brewer B.W., Cornelius A.E., Van Raalte J.L., Brickner J.C., et al. Rehabilitation adherence and anterior cruciate ligament reconstruction outcome. Psychol. Health Med. 2004;9(2):163–175. doi: 10.1080/13548500410001670690. [DOI] [Google Scholar]
- 50.Lewis Z.H., Lyons E.J., Jarvis J.M., Baillargeon J. Using an electronic activity monitor system as an intervention modality: a systematic review. BMC Publ. Health. 2015;15:585. doi: 10.1186/s12889-015-1947-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Whittaker JL, Truong LK, Losciale JM, Silvester-Lee TS, Miciak M, Pajkic A, Le CY, Hoens AM, Mosewich AD, Hunt MA, Li LC, Roos EM. Efficacy of the SOAR knee health program: protocol for a two-arm stepped-wedge randomized delayed-control trial. BMC Musculoskeletal Open. 2022;23:85. doi: 10.1186/s12891-022-05019-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.