Summary
Objective
To model potential cost savings associated with implementing a first-line management program for moderate-severe knee osteoarthritis (OA) at a national level in Australia.
Methods
A budget impact analysis was undertaken using published trial data and publically available data. Australian population projections and OA prevalence data were used to forecast likely need for total knee replacement (TKR) surgery for 2019–2029. Published data were sourced on TKR avoidance following a 12-week non-surgical knee OA management program (exercise therapy, education, insoles, dietary advice, analgesia) and cost per TKR in Australia. The cost of providing the first-line program was estimated on a sliding scale ($AUD750-$3000), with a base case of $AUD1,500. These inputs were used to model potential annual savings associated with national implementation of the program.
Results
The number of people in Australia with moderate-severe knee OA requiring TKR was estimated to be 56,007 in 2019, rising to 69,038 by 2029. Avoidance of TKR by 34%–68% of people after the first-line management program could translate to savings of $AUD303million-690 million in 2019. Successively lowering the proportion of people who avoided TKR demonstrated that only 1 in 12 program recipients would need to avoid surgery for the program to generate savings.
Conclusions
National implementation of a first-line OA management program as an alternative to TKR could produce substantial cost savings for the Australian healthcare system. Longer term data on TKR avoidance is needed to establish whether cost savings are realised or simply shifted to later years.
Keywords: Exercise therapy, Health care costs, Non-surgical management, Osteoarthritis, Total knee arthroplasty, Total knee replacement
1. Introduction
Knee osteoarthritis (OA) is an important public health issue for many countries, given multiple contributing factors including ageing populations [1] and an increasing global prevalence of obesity [2]. The growing burden of total knee replacement (TKR) procedures is undeniable, with the lifetime risk of TKR rising in many countries [3,4]. More than 55,000 primary TKRs are now performed in Australia each year (predominantly for advanced knee OA), representing a 152% growth since 2003 [5]. We have previously forecast an alarming increase in the future number of TKR procedures, should recent surgery and obesity trends continue [6]. While TKR surgery can be highly effective and cost-effective (although this depends on appropriate patient selection [7]), it is associated with surgical risks [8] and up to 20% of recipients are dissatisfied with their surgical outcome [[9], [10], [11], [12]] or have persistent pain [13]. Contemporary OA clinical guidelines recommend that TKR surgery only be considered once first-line management options have been exhausted [14,15]. However, surgical referral rates for knee OA in Australia are substantially higher than referrals to physiotherapists, and provision of lifestyle management support is relatively infrequent [16]. There is also evidence that people with OA commonly do not receive care that aligns with quality indicators; in a meta-analysis involving 16,103 patients, only 39% received a referral or recommendation to exercise [17] while a study involving 489 people with knee OA reported that 54% had never tried muscle strengthening exercises [18].
There is currently no co-ordinated approach to OA management in Australia and many other countries, resulting in care that is commonly fragmented and often low-value in nature [19]. However, region-wide or national OA first-line management programs, which align with clinical guidelines, have been successfully implemented in several countries. These include the Better Management of Patients with Osteoarthritis (BOA) program in Sweden [20] and the Good Life with Arthritis: Denmark (GLA:D®) program in Denmark [21]. Data from the national GLA:D registry (spanning all five healthcare regions in Denmark) for 7,333 people with knee OA have demonstrated a 19% absolute reduction in analgesia use and a 29% relative reduction in pain scores at 3 months [22]. At 12 months, a 20% relative improvement in knee-related quality of life was evident and only 5% had undergone joint replacement for their most affected joint [22]. The GLA:D initiative has now expanded to other countries including Canada, China and Australia [23,24]. GLA:D™ Australia was developed in 2016. As of 2019, over 800 physiotherapists had been trained, the program was offered at over 250 physiotherapy clinics, and almost 3,000 Australians with knee or hip OA had been registered. Broadly, these first-line management programs are group-based and focus on disease-relevant education and engagement in supervised structured exercise therapy. The GLA:D program was developed based on compelling evidence supporting the use of education and exercise therapy in managing hip and knee OA [22]. The benefits of a program involving the same education and exercise therapy components administered over 12 weeks was shown in a Danish randomised controlled trial (RCT), which is described below.
Given the volume of TKRs performed each year and estimated increasing burden, avoidance (or even delay) of surgery by a proportion of patients could offer important savings for the health system when extrapolated to the population level. Using a budget impact analysis approach, this study aimed to estimate the potential healthcare savings associated with national implementation of a first-line management program (such as GLA:D Australia) for moderate-severe knee OA, should a proportion of TKR procedures be avoided.
2. Methods
2.1. Study design
Budget impact analysis examining the financial implications of adopting a new intervention. This study adopts a health system perspective, which underpins the current decision-making process in Australia. A societal perspective was also not taken as robust national data on indirect costs (for knee OA-related loss of income, use of carers, or transport costs) were not available.
2.2. Ethics approval
Ethics approval was not required as all data were publically available.
2.3. Data sources
A range of published data sources (encompassing national population projections, OA prevalence, TKR avoidance following a first-line OA management program, and TKR costs) were utilised, as outlined below.
2.3.1. Population projections
Australian national population projections for the years 2019–2029, by age group and sex, were obtained from the Australian Bureau of Statistics (ABS) [25]. Population projections are based on assumptions regarding expected rates of fertility, life expectancy and migration. The ABS considers three potential scenarios in their population projections, pertaining to low, medium, and high population growth. We used the medium growth (Series B) projections for our analyses, with assumptions of medium fertility, life expectancy and net overseas migration.
2.3.2. Prevalence of osteoarthritis in Australia
The national prevalence of OA, by age group and sex, was obtained from the most recent National Health Survey (2017–18) [26]. The survey comprised 21,315 participants from 16,384 randomly selected private dwellings across Australia. One adult (aged 18 years or over) from each dwelling was selected for inclusion. Within the arthritis module, participants were asked whether they had, or ever had, OA and whether they had ever been told by a doctor or nurse that they have the condition. Collection of self-reported doctor-diagnosed OA data is common in large-scale population-based studies where it is not feasible to collect clinical and/or radiographic diagnosis data.
2.3.3. Outcomes of first-line management
Data on first-line management outcomes were obtained from a Danish RCT that investigated the effectiveness of TKR plus non-surgical treatments, compared to non-surgical interventions alone [27]. For this trial, 100 patients were recruited from Aalborg University Hospital in Denmark. Patients with moderate-severe knee OA who were eligible for TKR were included (Kellgren Lawrence radiographic score ≥2 indicating definite OA). Patients were excluded if they had a visual analogue pain scale score of greater than 60 mm (range 0–100 mm, higher scores indicate greater pain) for pain during the previous week, if they had a previous TKR in the same knee, or if they needed a bilateral simultaneous TKR. Baseline mean pain intensity for the sample was 49 mm, similar to previous studies evaluating pain severity prior to TKR [[28], [29], [30]]. Inclusion of patients with more severe OA was evidenced by scores for worst pain during the previous 24 h (42% of the sample reported their worst pain within the previous 24 h to be greater than 60 mm). Participants were randomised to either TKR followed by 12 weeks of non-surgical treatments, or 12 weeks of non-surgical treatments only. Non-surgical treatments were identical for each group. Delivered by physiotherapists and dieticians, treatments consisted of exercise therapy, education, non-custom-made insoles, dietary advice, and pain medication, if appropriate. Pre-defined criteria for crossover to surgery were based on Knee Injury and Osteoarthritis Outcome Scores and agreement between the participant and orthopaedic surgeon that TKR was necessary. Free access to surgery was available to all participants within the publicly-funded Danish health system. Although both groups reported significant improvements in pain, health-related quality of life and functional outcomes, the TKR group experienced greater improvements at 12 months. Only 26% of the non-surgical group had TKR in the following year, indicating the non-surgical intervention delayed the need for surgery for 74% of participants [27]. Recently published data indicate that 68% of the non-surgical group had still avoided TKR surgery at two years [31].
2.3.4. Cost of knee replacement surgery
The cost of TKR was estimated using the average cost per Australian Refined Diagnosis Related Group (AR-DRG) for unilateral knee replacement with minor complexity, as reported in the most recent National Hospital Cost Data Collection (Round 20, 2015–16) [32]. The cost per procedure was inflated to 2019–2029 prices using the Total Health Price Index (THPI) [33]. This resulted in a cost per TKR procedure of $AUD20,340 in 2019, rising to $AUD24,215 by 2029.
2.3.5. Cost of first-line management
The cost of the 12-week first-line management program was estimated at $905 per participant, based on actual costs data for the trial undertaken by Skou et al. [27] or $1250 per participant, based on discussions with the GLA:D Australia research team (extending the current six-week program to 12 weeks). However, actual costs would vary depending on the program setting and the provision of weight loss support, which is only applicable for people with a body mass index ≥25 kg/m2 [27]. Given differing healthcare systems and labour costs in Denmark and Australia, we chose to use a sliding scale of costs for our analyses, ranging from $AUD750 to $AUD3,000 per recipient. These costs incorporate physiotherapist training, patient assessment and intervention delivery. For the base-case analysis, a mid-range program cost of $AUD1,500 per recipient was used for 2019 (inflated using the THPI to a cost of $AUD1,786 per recipient by the year 2029).
2.4. Data analyses
All analyses were performed using Microsoft Excel™ (Microsoft, USA). A population-level model for the years 2019–2029 was constructed using the following steps:
-
1.
Similar to methods used previously [34], the number of people with OA in Australia was forecasted for the years 2019–2029 by applying the age- and sex-specific national OA prevalence data to Australian population projections for each year.
-
2.
As joint-specific prevalence data are not available from the National Health Survey, we estimated the proportion of people with knee OA among the overall population with OA. To do this, we used data from a national study that reported on 489,900 OA-related general practitioner presentations in Australia according to affected joints and age [16]. Using these age-specific data, we estimated the proportion of OA patients that was likely to have affected knees.
3. To estimate the proportion of people likely to need TKR, we utilised published data from the Global Burden of Disease (GBD) Study and the Australian Orthopaedic Association National Joint Registry. While the GBD estimated the proportion of severe OA in high income countries to be 2% [35], when applied to the anticipated number of people with knee OA in 2019–2029, the resulting number was substantially lower than the number of TKRs performed in Australia each year [5]. This likely reflects that TKR is not restricted to severe knee OA, in that people with moderate knee OA are also undergoing surgery [36]. To more closely align our estimates with the annual utilisation of primary TKR surgery in Australia (55,042 procedures in 2017 [5]), we estimated that 9.45% of the overall knee OA population each year would be undergoing TKR (equating to N = 56,007 in 2019).
4. To estimate the potential cost savings related to first-line management programs for moderate-severe knee OA, we assumed that a proportion of patients with OA were able to avoid TKR after intervention and, therefore, TKR-related costs for these individuals would be avoided for that particular year. The proportion avoiding TKR up to two years after intervention (68% at 2 years) was obtained from the study by Skou et al. [31].
5. Potential cost savings were calculated by subtracting the costs for the first-line management group (who received first-line management and TKR (32%) or first-line management alone (68%)) from the costs for a ‘usual care’ surgery group (who all received TKR). All costs are reported in Australian dollars for the years 2019–2029 (1 AUD = 0.67 USD or 0.52 GDP or 0.61 Euros).
A range of scenario analyses was also undertaken to assess the impact of varying the model inputs:
-
•
Scenario 1: The price at which the first-line management program would cease to be cost saving at the population level (the break-even point) was calculated, assuming a 68% avoidance of TKR.
-
•
Scenario 2: Potential cost savings were estimated assuming a 50% relative reduction in TKR avoidance compared to published outcomes (that is, if 34% of patients avoided TKR after the first-line management program rather than 68%).
-
•
Scenario 3: This scenario considered the potential impacts should the first-line program be even less effective than in Scenario 2 (using a program cost of $AUD1,500). The proportion of people avoiding TKR after the first-line management program was successively lowered from 68% to identify the point at which the program would cease to produce savings at a population level in 2019.
-
•
Scenario 4: The costs of post-operative complications following TKR were also considered. We obtained the average cost of a TKR procedure (inclusive of the costs of complications, readmissions, reoperations or emergency department presentations within 30 days) from an earlier study conducted at a single Australian public hospital [37]. The mean cost per TKR in 2011–12 was $AUD 21,357, which was inflated to 2019–2029 prices using the THPI (resulting in a cost range from $AUD25,198–29,999). Program cost was maintained at $AUD1,500 per recipient, with 68% avoidance of TKR.
-
•
Scenario 5: Finally, we calculated potential cost savings should the cost of surgery be even higher. This scenario used a TKR cost of $AUD28,400 in 2018, based on 2017-18 claims data for a major Australian private health insurance fund [38], which was inflated using the THPI to a 2019 price of $AUD28,952 and a 2029 price of $AUD34,468.
3. Results
3.1. Forecasting the total knee replacement population
As shown in Table 1, the number of people in Australia with moderate-severe knee OA likely to require TKR was estimated to be 56,007 in 2019, rising to 69,038 by 2029. This equates to 23% growth (or 2.3% annual growth) over this time period.
Table 1.
Estimated population likely to require total knee replacement in 2019–2029.
|
Year |
Estimated population |
|||
|---|---|---|---|---|
| National population | Population with OA | Population with knee OA | Population with moderate-severe knee OAa | |
| 2019 | 25,619,895 | 2,446,932 | 592,665 | 56,007 |
| 2020 | 26,037,356 | 2,503,707 | 605,794 | 57,248 |
| 2021 | 26,452,147 | 2,560,513 | 618,848 | 58,481 |
| 2022 | 26,866,209 | 2,618,711 | 631,768 | 59,702 |
| 2023 | 27,279,046 | 2,677,592 | 645,037 | 60,956 |
| 2024 | 27,690,209 | 2,738,388 | 658,867 | 62,263 |
| 2025 | 28,099,273 | 2,800,364 | 672,954 | 63,594 |
| 2026 | 28,505,871 | 2,865,502 | 687,811 | 64,998 |
| 2027 | 28,909,776 | 2,929,710 | 702,452 | 66,382 |
| 2028 | 29,311,467 | 2,992,684 | 716,717 | 67,730 |
| 2029 | 29,710,682 | 3,053,818 | 730,561 | 69,038 |
Who are likely to require TKR (based on 9.45% of the population with knee OA).
3.2. Base case analysis
Assuming successful completion of the first-line management program (with similar outcomes to those previously published [31]), the number of people who could potentially avoid TKR each year would range from 38,085 in 2019 to 46,946 in 2029 (Table 2). For the base case analysis (assuming a program price of $AUD1,500 per recipient in 2019), avoidance of TKR would translate to savings of over $AUD690 million in 2019 and $AUD1.01 billion by 2029 (Table 3). To put these numbers in context, this would equate to an average saving of $AUD12,331 for each person likely to require TKR in 2019.
Table 2.
Estimated number of people who could avoid knee replacement in 2019–2029.
| Year | Population with moderate-severe knee OAa | Usual care |
Non-surgical management program |
|
|---|---|---|---|---|
| Number estimated to receive TKR | Number estimated to receive TKRb | Number estimated to avoid TKRc | ||
| 2019 | 56,007 | 56,007 | 17,922 | 38,085 |
| 2020 | 57,248 | 57,248 | 18,319 | 38,928 |
| 2021 | 58,481 | 58,481 | 18,714 | 39,767 |
| 2022 | 59,702 | 59,702 | 19,105 | 40,597 |
| 2023 | 60,956 | 60,956 | 19,506 | 41,450 |
| 2024 | 62,263 | 62,263 | 19,924 | 42,339 |
| 2025 | 63,594 | 63,594 | 20,350 | 43,244 |
| 2026 | 64,998 | 64,998 | 20,799 | 44,199 |
| 2027 | 66,382 | 66,382 | 21,242 | 45,140 |
| 2028 | 67,730 | 67,730 | 21,674 | 46,056 |
| 2029 | 69,038 | 69,038 | 22,092 | 46,946 |
Table 3.
Potential savings due to the non-surgical management programa for 2019–2029.
| Age group | Year |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | 2021 | 2022 | 2023 | 2024 | 2025 | 2026 | 2027 | 2028 | 2029 | |
| 15–24 | $2,545,912 | $2,611,119 | $2,688,114 | $2,768,544 | $2,856,204 | $2,948,347 | $3,116,090 | $3,237,984 | $3,253,722 | $3,367,938 | $3,482,025 |
| 25–34 | $8,480,841 | $8,724,991 | $8,955,711 | $9,186,744 | $9,404,276 | $9,610,878 | $9,855,450 | $10,066,137 | $10,209,780 | $10,419,976 | $10,637,978 |
| 35–44 | $47,060,648 | $49,166,014 | $51,381,586 | $53,634,087 | $55,941,942 | $58,260,543 | $62,280,313 | $64,011,402 | $64,550,424 | $66,260,318 | $67,952,581 |
| 45–54 | $97,464,243 | $100,198,134 | $102,984,827 | $105,846,540 | $108,627,699 | $111,302,867 | $115,429,421 | $118,969,316 | $120,137,299 | $124,321,833 | $128,959,699 |
| 55–64 | $185,399,090 | $191,045,129 | $196,164,809 | $201,206,765 | $206,428,043 | $212,219,478 | $223,194,159 | $229,655,622 | $231,655,559 | $237,562,777 | $243,347,078 |
| 65–74 | $200,269,483 | $209,548,700 | $219,128,045 | $226,195,064 | $234,835,016 | $244,479,905 | $264,252,524 | $274,683,463 | $275,322,110 | $285,348,182 | $294,971,183 |
| 75+ | $149,398,211 | $158,074,246 | $167,306,653 | $179,429,050 | $190,840,914 | $202,085,257 | $227,521,878 | $239,662,767 | $238,195,978 | $251,113,410 | $264,163,333 |
| Total | $690,618,428 | $719,368,333 | $748,609,745 | $778,266,795 | $808,934,093 | $840,907,274 | $905,649,835 | $940,286,691 | $943,324,870 | $978,394,434 | $1,013,513,877 |
Assuming a base-case program cost of $1500 per recipient and 68% avoidance of TKR.
3.3. Sliding scale of program costs
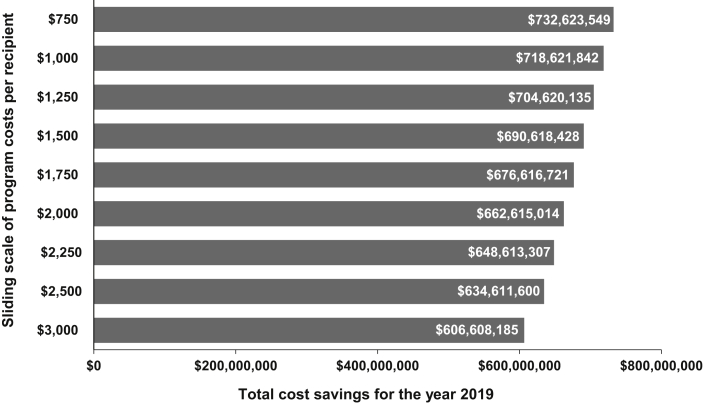
In 2019, the potential cost savings at the national level would range from AUD$732 million down to AUD$606 million (Fig. 1), depending on program pricing (ranging from a program cost of $AUD750 to $AUD3,000 per recipient).
Fig. 1.
Potential savings in 2019 according to varying price assumptions.
3.4. Potential savings under alternative scenarios
Under Scenario 1 (in which the proportion who avoided TKR was fixed at 68% and the program cost was inflated), the first-line management program still produced savings in 2019 up to a cost of $AUD13,500 per program recipient.
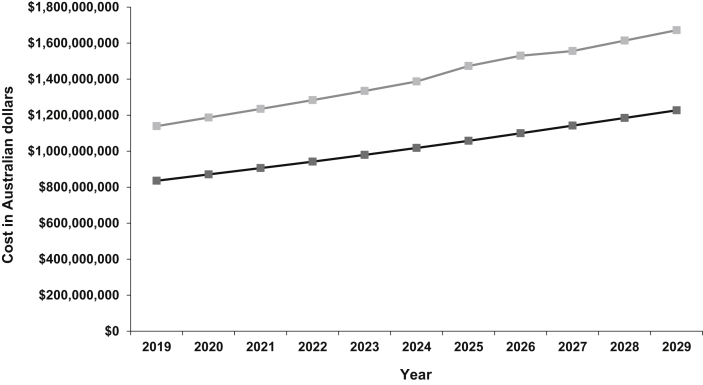
Under Scenario 2 (in which the program cost was fixed at $AUD1,500 per recipient and the proportion who avoided TKR was halved), the program would produce savings even if only 34% of patients avoided TKR (that is, where 66% of those who received first-line management had subsequent TKR and 34% avoided TKR). In this context, the potential cost savings would range from AUD$303 million in 2019 to AUD$445 million in 2029 (Fig. 2).
Fig. 2.
Projected costs of surgical and non-surgical management∗ for 2019–2029 under a reduced program effectiveness scenario. ∗ Assuming a base-case cost of $1,500 per recipient for the non-surgical management program and 34% TKR avoidance (Scenario 2). The grey line indicates the cost of TKR surgery (usual care) and the black line indicates the cost of the non-surgical management program.
Under Scenario 3 (in which the program cost was fixed at $AUD1,500 per recipient and the proportion who avoided TKR was successively lowered), the program produced notional savings in 2019 up to the point at which only 8% of people avoided TKR (that is, where 92% of those who received first-line management had subsequent TKR and 8% avoided TKR). This scenario would provide savings of $AUD7 million in 2019.
Under Scenario 4 (in which the proportion who avoided TKR was fixed at 68% and the program cost was fixed at $AUD1,500 per recipient, but the price per TKR was increased to incorporate the cost of complications and readmissions within 30 days), the first-line program would produce savings of over $AUD875 million in 2019 and over AUD$1.28 billion by 2029. This equates to a saving of $AUD15,634 for each person likely to require TKR in 2019.
Under Scenario 5 (in which the proportion who avoided TKR was fixed at 68% and the program cost was fixed at $AUD1,500 per recipient, but an even higher TKR price was used, based on private health insurance claims), the cost savings would range from $AUD1.01 billion in 2019 to $AUD1.49 billion in 2029. This reflects a 47% increase in total savings (compared to the base case analysis which applied the AR-DRG cost per TKR) and equates to a saving of $AUD18,187 per person likely to require TKR in 2019.
4. Discussion
This budget impact analysis is the first to estimate healthcare savings that could result from the national implementation of a comprehensive, evidence-based management program for knee OA. We have taken a key directive from the new Australian OA strategy [19] (optimising first-line management) and forecast what could be achieved should we follow the path taken in countries such as Denmark and Canada. Although published RCT data indicate that 68% of people with knee OA avoided TKR surgery following a structured non-surgical program [31], program effectiveness in clinical settings rarely mimics trial outcomes. For this reason, we adopted a deliberately conservative approach to examine the potential budget impacts within a real-world context. These analyses demonstrated that even at a 50% relative reduction in effectiveness, potential savings would range from $AUD303 million in 2019 to $AUD445 million in 2029.
Structured first-line management programs for knee OA (incorporating education, exercise therapy and dietary interventions) are cost-effective [39,40]. A recent health technology assessment reported an incremental cost-effectiveness ratio of $CAD23,967 per quality-adjusted life year gained [39], which sits well below a conventional $50,000–100,000 cost-effectiveness threshold. Most recently, supervised exercise therapy for hip or knee OA was found to be cost-effective from health system and societal perspectives, regardless of whether joint replacement was performed within the 2-year study period [41]. TKR surgery has also been shown to be cost-effective [42,43] (although conflicting evidence has recently emerged [44]) and can be highly effective for reducing pain and improving function [36]. However, there is a downside, with potential for persistent pain [13], dissatisfaction [9], post-operative complications, and revision surgery. With these issues in mind, provision of evidence-based, first-line management before consideration of TKR is a core tenet of OA care guidelines [14,15,45]. Importantly, appropriately-supervised exercise therapy is safe for older adults with knee OA [46]. A systematic review involving 49 studies and 8,920 participants found no evidence of serious adverse events associated with exercise or physical activity; only mild adverse events were reported (such as transient muscle soreness or a minor increase in joint pain) [46]. Beyond the joint-related benefits, exercise therapy can also benefit other bodily systems and overall health [47]. Seventy-nine per cent of Australians with arthritis have at least one other chronic disease, most commonly cardiovascular disease, back pain and mental health conditions [48]. All of these comorbid conditions stand to benefit from exercise and increased physical activity. As well as opportunities for health system savings, there may also be productivity impacts at the societal level (improving symptoms and delaying TKR may keep people in the workforce), although these are difficult to quantify. A national Danish study that followed 48,970 TKR recipients and 195,880 matched controls up to 12 years after surgery found the TKR group had substantially lower employment income per year and received higher sick pay and disability pension benefits [49].
Our results represent a ‘best case scenario’ assuming national rollout of the program and maximum patient uptake and compliance, although we did consider alternative effectiveness scenarios. Unpublished data from the GLA:D Australia registry (n = 1,142) indicate that compliance is high. With each scenario analysis (altering program pricing, TKR pricing and proportion of people who avoid TKR), the program still generated savings given the comparative cost of surgery. Only 1 in 12 program recipients would need to avoid TKR for the program to generate savings, and surgery avoidance could be systematically monitored through the GLA:D Australia registry. Current GLA:D Australia data indicate that a substantial proportion of people who desired surgery at baseline had not had surgery and no longer desired surgery after the program (54% at 3 months and 49% at 12 months). Unpublished data from the Danish GLA:D registry demonstrate similar results (49% of those who desired surgery at baseline had not had TKR and did not desire surgery at 12 months), reflecting a notable shift in attitudes after the program. Together, these registry data suggest a clear opportunity for minimising unwarranted surgery. An RCT investigating longer-term total hip replacement outcomes for people with hip OA in Norway also provides further evidence regarding joint replacement avoidance following a structured exercise therapy program. At the 6-year follow-up, only 42% of the exercise therapy plus patient education group had received total hip replacement versus 63% of the patient education only group [50]. The GLA:D Australia program is a 6-week education and exercise program rather than the 12-week multidisciplinary program used for the Danish trial, but unpublished outcomes data indicate an average knee pain reduction of 36% at 3 months, which is maintained at 12 months. This is comparable to the average 35% pain reduction observed in the trial [27], which included participants with moderate-severe knee OA. Data from the Danish GLA:D registry also demonstrate an average 27% knee pain reduction at 3 months, which is maintained at 12 months [51]. Taken together, these data highlight that the magnitude of pain relief achieved within a rigorous randomised trial can be replicated in conventional physiotherapy settings, despite the shortened program duration. The first-line management program that forms the basis for our analysis provides an appropriate amount of supervised exercise therapy [47,52], which is important given patients are often deemed to have ‘failed non-surgical management’ without having received a sufficient exercise dose. Given the chronic nature of knee OA, options for supporting longer-term adherence to exercise (for example, booster sessions after initial program completion) and maintenance of gains are also important, but are beyond the scope of the present study.
A key strength of this study was our use of national population data together with outcomes data from a rigorous RCT that formed the starting point for our analysis. We recognise that adverse events and hospital readmissions add to surgical episode costs and have considered this within the TKR pricing. Importantly, we also considered contemporary TKR costs in the private sector, given that 71% of TKRs in Australia are performed in private hospitals [5]. While quantifying uncertainty around the savings estimates is difficult, we addressed this through analysis of five alternative scenarios and a sliding scale of program costs. As the overall cost to payers for each of the 12 sessions in Australia is approximately $AUD40, we consider that the sliding scale captures the likely program costs incorporating physiotherapist training, patient assessment and intervention delivery. We also acknowledge the study limitations. The analysis is based on available outcomes data (drawn from the only RCT that has examined TKR avoidance after non-surgical management), but it is not known how the Danish study sample compares to the general Australian population. Based on current evidence, we do not know whether TKR can be delayed for more than two years; it is possible that treatment costs are being shifted to a later time point. However, there still may be clear benefits to this delay, including lower use of healthcare resources [49] and reductions in revision TKRs per person over their lifespan (given revisions are more expensive and generally less effective [53]). As we examined single-year (cross-sectional) outcomes based on the number of people likely to require TKR each year, the future benefits and costs were not discounted. We understand that TKR avoidance data at 5 years and 10 years are being collected for the Skou et al. trial [27] and these longer-term outcomes will enable future longitudinal modelling of downstream costs and benefits. While we were not able to apply the same explicit eligibility criteria to our sample (given the absence of population-level data on radiographic knee OA severity and pain), we note that both the RCT and our budget impact analysis focused on people with moderate-severe knee OA, as the most likely potential recipients of TKR. Finally, we acknowledge that our analyses focus on the economic viewpoint and do not consider the clinical perspective. While both interventions produced clinically important gains, TKR surgery was clearly associated with larger improvements in pain and quality of life, when added to non-surgical management [27,31]. However, we contend that avoidance of TKR following the program is a proxy indicator for acceptable symptom relief.
In conclusion, national implementation of a first-line OA management program to provide appropriate education and exercise therapy prior to considering TKR could produce substantial health system savings, based on currently available data and the relatively high cost of TKR. This study has examined short-term outcomes and longer-term TKR avoidance data are needed to establish whether savings are shifted to later years.
Author contributions
Study conception: INA, ZA, DL; study design: INA, ZA, DL; data acquisition: INA, ZA, STS, CB; data analysis: ZA; data interpretation: INA, ZA, STS, ER, CB, JLK, KMC, DL, ZA; manuscript drafting: INA, STS, ER, CB, JLK, KMC, DL, ZA. All authors have approved the final version of the manuscript.
Role of the funding source
A/Prof Ackerman is supported by a Victorian Health and Medical Research Fellowship awarded by the Victorian Government. Dr Skou is currently funded by the Independent Research Fund Denmark (DFF – 6110–00045) and the Lundbeck Foundation. Dr Barton is supported by a Translating Research Into Practice Fellowship awarded by the Medical Research Future Fund. Dr Kemp is supported by an Early Career Fellowship (1119971) from the National Health and Medical Research Council of Australia. These institutions had no role in the study design, collection, analysis and interpretation of data, in the writing of the manuscript, or in the decision to submit the manuscript for publication.
Declaration of Competing Interest
All authors have completed the ICMJE disclosure form and declare: no support from any organisation for the submitted work. Dr Skou is associate editor of the Journal of Orthopaedic and Sports Physical Therapy, has received grants from The Lundbeck Foundation, and personal fees from Munksgaard, all of which are outside the submitted work. He is co-founder of GLA:D®, a not-for profit initiative hosted at University of Southern Denmark aimed at implementing clinical guidelines for osteoarthritis in clinical practice. Dr Roos is deputy editor of Osteoarthritis & Cartilage, the developer of the Knee injury and Osteoarthritis Outcome Score (KOOS) and several other freely available patient-reported outcome measures and co-founder of GLA:D®. Dr Barton, Dr Kemp and Prof Crossley are project leads for GLA:DTM Australia, which is a not-for-profit implementation initiative. Prof Crossley's institution has received payment for training GLA:D practitioners. Prof Liew has received consultancy payments and grants from pharmaceutical companies, all of which are outside the submitted work.
Contributor Information
Ilana N. Ackerman, Email: ilana.ackerman@monash.edu.
Søren T. Skou, Email: stskou@health.sdu.dk.
Ewa M. Roos, Email: eroos@health.sdu.dk.
Christian J. Barton, Email: C.Barton@latrobe.edu.au.
Joanne L. Kemp, Email: J.Kemp@latrobe.edu.au.
Kay M. Crossley, Email: K.Crossley@latrobe.edu.au.
Danny Liew, Email: danny.liew@monash.edu.
Zanfina Ademi, Email: zanfina.ademi@monash.edu.
References
- 1.World Health Organization . World Health Organization; Geneva: 2017. Global Strategy and Action Plan on Ageing and Health. [Google Scholar]
- 2.Organisation for Economic Co-operation and Development . Organisation for Economic Co-operation and Development; Paris: 2017. Obesity Update 2017. [Google Scholar]
- 3.Ackerman I.N., Bohensky M.A., De Steiger R., Brand C.A., Eskelinen A., Fenstad A.M., et al. Substantial rise in the lifetime risk of primary total knee replacement surgery for osteoarthritis from 2003-2013: an international, population-level analysis. Osteoarthritis Cartilage. 2017;25(4):455–461. doi: 10.1016/j.joca.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Henzell I.S., Zhou L., Frampton C., Hooper G., Ackerman I., Young S.W. Lifetime risk of primary total knee replacement surgery in New Zealand from 2000 to 2015. N. Z.Med. J. 2019;132(1489):48–56. [PubMed] [Google Scholar]
- 5.Australian Orthopaedic Association National Joint Replacement Registry . Australian Orthopaedic Association; Adelaide: 2018. Annual Report - Hip, Knee and Shoulder Arthroplasty. [Google Scholar]
- 6.Ackerman I.N., Bohensky M.A., Zomer E., Tacey M., Gorelik A., Brand C.A., et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Muscoskel. Disord. 2019;20(1):90. doi: 10.1186/s12891-019-2411-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferket B.S., Feldman Z., Zhou J., Oei E.H., Bierma-Zeinstra S.M.A., Mazumdar M. Impact of total knee replacement practice: cost effectiveness analysis of data from the Osteoarthritis Initiative. BMJ. 2017;356:j1131. doi: 10.1136/bmj.j1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berstock J.R., Beswick A.D., Lopez-Lopez J.A., Whitehouse M.R., Blom A.W. Mortality after total knee arthroplasty: a systematic review of incidence, temporal trends, and risk factors. J. Bone Joint Surg. Am. 2018;100(12):1064–1070. doi: 10.2106/JBJS.17.00249. [DOI] [PubMed] [Google Scholar]
- 9.Gunaratne R., Pratt D.N., Banda J., Fick D.P., Khan R.J.K., Robertson B.W. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J. Arthroplasty. 2017;32(12):3854–3860. doi: 10.1016/j.arth.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 10.Bryan S., Goldsmith L.J., Davis J.C., Hejazi S., MacDonald V., McAllister P., et al. Revisiting patient satisfaction following total knee arthroplasty: a longitudinal observational study. BMC Muscoskel. Disord. 2018;19:423. doi: 10.1186/s12891-018-2340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clement N.D., Bardgett M., Weir D., Holland J., Gerrand C., Deehan D.J. Three groups of dissatisfied patients exist after total knee arthroplasty: Early, persistent, and late. Bone Joint Lett. J. 2018;100-B(2):161–169. doi: 10.1302/0301-620X.100B2.BJJ-2017-1016.R1. [DOI] [PubMed] [Google Scholar]
- 12.Mahdi A., Svantesson M., Wretenberg P., Halleberg-Nyman M. Patients' experiences of discontentment one year after total knee arthroplasty - a qualitative study. BMC Muscoskel. Disord. 2020;21:29. doi: 10.1186/s12891-020-3041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beswick A.D., Wylde V., Gooberman-Hill R., Blom A., Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Australian Commission on safety and quality in health care. Clinical Care Standards - Osteoarthritis of the Knee. https://www.safetyandquality.gov.au/our-work/clinical-care-standards/osteoarthritis-clinical-care-standard/ Available from:
- 15.Royal Australian College of General Practitioners . second ed. Royal Australian College of General Practitioners; East Melbourne: 2018. Guideline for the Management of Knee and Hip Osteoarthritis. [Google Scholar]
- 16.Brand C.A., Harrison C., Tropea J., Hinman R.S., Britt H., Bennell K. Management of osteoarthritis in general practice in Australia. Arthritis Care Res. 2014;66(4):551–558. doi: 10.1002/acr.22197. [DOI] [PubMed] [Google Scholar]
- 17.Hagen K.B., Smedslund G., Østerås N., Jamtvedt G. Quality of community-based osteoarthritis care: a systematic review and meta-analysis. Arthritis Care Res. 2016;68(10):1443–1452. doi: 10.1002/acr.22891. [DOI] [PubMed] [Google Scholar]
- 18.Hinman R.S., Nicolson P.J.A., Dobson F.L., Bennell K.L. Use of nondrug, nonoperative interventions by community-dwelling people with hip and knee osteoarthritis. Arthritis Care Res. 2015;67(2):305–309. doi: 10.1002/acr.22395. [DOI] [PubMed] [Google Scholar]
- 19.National Osteoarthritis Strategy Project Group . The University of Sydney; Sydney: 2018. National Osteoarthritis Strategy. [Google Scholar]
- 20.Thorstensson C.A., Garellick G., Rystedt H., Dahlberg L.E. Better management of patients with osteoarthritis: development and nationwide implementation of an evidence-based supported osteoarthritis self-management programme. Muscoskel. Care. 2015;13(2):67–75. doi: 10.1002/msc.1085. [DOI] [PubMed] [Google Scholar]
- 21.University of Southern Denmark Good life with osteoArthritis in Denmark (GLA:D®) https://www.glaid.dk/english.html Available from:
- 22.Skou S.T., Roos E.M. Good Life with osteoArthritis in Denmark (GLA:D™): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Muscoskel. Disord. 2017;18(1):72. doi: 10.1186/s12891-017-1439-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roos E.M., Barton C.J., Davis A.M., McGlasson R., Kemp J.L., Crossley K.M., et al. GLA:D to have a high-value option for patients with knee and hip arthritis across four continents: Good Life with osteoArthritis from Denmark. Br. J. Sports Med. 2018;52(24):1544–1545. doi: 10.1136/bjsports-2017-098904. [DOI] [PubMed] [Google Scholar]
- 24.Davis A.M., McGlasson R.M. GLA:D™ Canada: Implementation and Outcomes. Inception to December 2017: Bone and Joint Canada. http://gladcanada.ca/ Available from:
- 25.Australian Bureau of Statistics Population Projections, Australia, 2017-2066. http://stat.data.abs.gov.au/Index.aspx?DatasetCode=POP_PROJ_2011 Available from:
- 26.Australian Bureau of Statistics 4364.0.55.001 - National Health Survey: First Results, 2017-18. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4364.0.55.001∼2017-18∼Main%20Features∼About%20the%20National%20Health%20Survey∼5 Available from:
- 27.Skou S.T., Roos E.M., Laursen M.B., Rathleff M.S., Arendt-Nielsen L., Simonsen O. A randomized, controlled trial of total knee replacement. N. Engl. J. Med. 2015;373(17):1597–1606. doi: 10.1056/NEJMoa1505467. [DOI] [PubMed] [Google Scholar]
- 28.Gossec L., Paternotte S., Maillefert J.F., Combescure C., Conaghan P.G., Davis A.M., et al. The role of pain and functional impairment in the decision to recommend total joint replacement in hip and knee osteoarthritis: an international cross-sectional study of 1909 patients. Report of the OARSI-OMERACT Task Force on total joint replacement. Osteoarthritis Cartilage. 2011;19(2):147–154. doi: 10.1016/j.joca.2010.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Keurentjes J.C., Fiocco M., So-Osman C., Onstenk R., Koopman-Van Gemert A.W., Poll R.G., et al. Patients with severe radiographic osteoarthritis have a better prognosis in physical functioning after hip and knee replacement: a cohort-study. PloS One. 2013;8(4) doi: 10.1371/journal.pone.0059500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wise B.L., Niu J., Felson D.T., Hietpas J., Sadosky A., Torner J., et al. Functional impairment is a risk factor for knee replacement in the Multicenter Osteoarthritis Study. Clin. Orthop. Relat. Res. 2015;473(8):2505–2513. doi: 10.1007/s11999-015-4211-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Skou S.T., Roos E.M., Laursen M.B., Rathleff M.S., Arendt-Nielsen L., Rasmussen S., et al. Total knee replacement and non-surgical treatment of knee osteoarthritis: 2-year outcome from two parallel randomized controlled trials. Osteoarthritis Cartilage. 2018;26(9):1170–1180. doi: 10.1016/j.joca.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 32.Independent Hospital Pricing Authority The National Hospital Cost Data Collection, Public Hospitals Cost Report, Round 20 (Financial year 2015-16) https://www.ihpa.gov.au/publications/national-hospital-cost-data-collection-public-hospitals-cost-report-round-20-0 Available from:
- 33.Australian Institute of Health and Welfare Table E2: total health price index and industry-wide indexes. http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=6442473791 Available from:
- 34.Ackerman I.N., Pratt C., Gorelik A., Liew D. Projected burden of osteoarthritis and rheumatoid arthritis in Australia: a population-level analysis. Arthritis Care Res. 2018;70(6):877–883. doi: 10.1002/acr.23414. [DOI] [PubMed] [Google Scholar]
- 35.Cross M., Smith E., Hoy D., Nolte S., Ackerman I., Fransen M., et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014;73(7):1316–1322. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 36.Price A.J., Alvand A., Troelsen A., Katz J.N., Hooper G., Gray A., et al. Knee replacement. Lancet. 2018;392(10158):1672–1682. doi: 10.1016/S0140-6736(18)32344-4. [DOI] [PubMed] [Google Scholar]
- 37.Peel T.N., Cheng A.C., Liew D., Buising K.L., Lisik J., Carroll K.A., et al. Direct hospital cost determinants following hip and knee arthroplasty. Arthritis Care Res. 2015;67(6):782–790. doi: 10.1002/acr.22523. [DOI] [PubMed] [Google Scholar]
- 38.Hospitals Contribution Fund of Australia Procedure cost indicator - knee replacement. https://www.hcf.com.au/cost-calculator?pid=2 Available from:
- 39.Health Quality Ontario Structured education and neuromuscular exercise program for hip and/or knee osteoarthritis: a health technology assessment. http://www.hqontario.ca/evidence-to-improve-care/journal-ontario-health-technology-assessment-series Available from: [PMC free article] [PubMed]
- 40.Losina E., Smith K.C., Paltiel A.D., Collins J.E., Suter L.G., Hunter D.J., et al. Cost-effectiveness of diet and exercise for overweight and obese knee osteoarthritis patients. Arthritis Care Res. 2018;71(7):855–864. doi: 10.1002/acr.23716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abbott J.H., Wilson R., Pinto D., Chapple C.M., Wright A.A., the MOA Trial Team Incremental clinical effectiveness and cost effectiveness of providing supervised physiotherapy in addition to usual medical care in patients with osteoarthritis of the hip or knee: 2-year results of the MOA randomised controlled trial. Osteoarthritis Cartilage. 2019;27:424–434. doi: 10.1016/j.joca.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 42.Elmallah R.K., Chughtai M., Khlopas A., Bhowmik-Stoker M., Bozic K.J., Kurtz S.M., et al. Determining cost-effectiveness of total hip and knee arthroplasty using the Short Form-6D utility measure. J. Arthroplasty. 2017;32(2):351–354. doi: 10.1016/j.arth.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 43.Higashi H., Barendregt J.J. Cost-effectiveness of total hip and knee replacements for the Australian population with osteoarthritis: Discrete-event simulation model. PloS One. 2011;6(9) doi: 10.1371/journal.pone.0025403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Skou S.T., Roos E., Laursen M., Arendt-Nielsen L., Rasmussen S., Simonsen O., et al. Cost-effectiveness of total knee replacement in addition to non-surgical treatment: a 2-year outcome from a randomised trial in secondary care in Denmark. BMJ Open. 2020;10(1) doi: 10.1136/bmjopen-2019-033495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.National Institute for Health and Care Excellence . National Institute for Health and Care Excellence; London: 2014. Osteoarthritis: Care and Management in adults. Clinical Guideline CG177. [Google Scholar]
- 46.Quicke J.G., Foster N.E., Thomas M.J., Holden M.A. Is long-term physical activity safe for older adults with knee pain? A systematic review. Osteoarthritis Cartilage. 2015;23(9):1445–1456. doi: 10.1016/j.joca.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 47.Skou S.T., Pedersen B.K., Abbott J.H., Patterson B., Barton C. Physical activity and exercise therapy benefit more than just symptoms and impairments in people with hip and knee osteoarthritis. J. Orthop. Sports Phys. Ther. 2018;48(6):439–447. doi: 10.2519/jospt.2018.7877. [DOI] [PubMed] [Google Scholar]
- 48.Australian Institute of Health and Welfare . Australian Institute of Health and Welfare; Canberra: 2019. Musculoskeletal Conditions and Comorbidity in Australia. [Google Scholar]
- 49.Kjellberg J., Kehlet H. A nationwide analysis of socioeconomic outcomes after hip and knee replacement. Dan. Med. J. 2016;63(8):A5257. [PubMed] [Google Scholar]
- 50.Svege I., Nordsletten L., Fernandes L., Risberg M.A. Exercise therapy may postpone total hip replacement surgery in patients with hip osteoarthritis: a long-term follow-up of a randomised trial. Ann. Rheum. Dis. 2015;74(1):164–169. doi: 10.1136/annrheumdis-2013-203628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Grønne D.T., Roos E., Skou S.T. University of Southern Denmark; 2017. Annual Report 2017 GLA:D. Odense. [Google Scholar]
- 52.Juhl C., Christensen R., Roos E.M., Zhang W., Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheum. 2014;66(3):622–636. doi: 10.1002/art.38290. [DOI] [PubMed] [Google Scholar]
- 53.Evans J.T., Walker R.W., Evans J.P., Blom A.W., Sayers A., Whitehouse M.R. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393(10172):655–663. doi: 10.1016/S0140-6736(18)32531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]