Summary
Objective
Patient satisfaction is considered an important outcome measure after total knee replacement, but the construct is complex. There is large variation both in how satisfaction is measured and estimates of the proportion of people who are satisfied after surgery. The aim of this systematic review was to i) evaluate the proportion of people reported to be satisfied after total knee replacement for osteoarthritis; and ii) assess the content validity of the utilised satisfaction measures.
Methods
We searched four literature databases with search phrases ‘Total Knee Arthroplasty’ OR ‘Total Knee Replacement’ AND ‘Patient satisfaction’ for studies that measured satisfaction at least 6 month post-unilateral primary total knee replacement for knee osteoarthritis. Identified studies were assessed for risk of bias, and studies at high risk of bias were excluded (PROSPERO: CRD42017058936). Meta-analysis was not appropriate due to the heterogeneity in satisfaction instruments, thus satisfaction scores were described. The content validity of satisfaction questionnaires was assessed using the COnsensus-based Standards for the selection of health status Measurement Instruments criteria.
Results
The present review found heterogeneity in the satisfaction questions used, as well as the satisfaction estimates from the various studies. Only two satisfaction instruments were relevant for a Total Knee Replacement population and both failed assessment for content validity due to lack of patient involvement during development and testing in accordance with the COnsensus-based Standards for the selection of health status Measurement Instruments criteria.
Conclusion
Future research should focus on qualitative methods to elicit patients' perspectives of satisfaction to build theoretical understanding.
Keywords: Satisfaction, Total knee replacement, Total knee arthroplasty, Osteoarthritis, Content validity
1. Introduction
Total knee replacement (TKR) surgery is considered the gold standard treatment for end stage knee osteoarthritis (OA) due to its cost effectiveness [1] and high rates of symptomatic and functional improvement [2]. However, despite near-flawless surgical procedures, up to 30% of people fail to have clinically meaningful improvements in pain and disability levels post-operatively [3]. These rates of poor response highlight the importance of appropriately determining and measuring success with this procedure to facilitate improvement in outcomes.
The lack of concordance between the surgeon's and patient's appraisals of the intervention [4,5] underscores the importance of understanding the success of a TKR from the patient's perspective. As such, the Osteoarthritis Research Society International (OARSI) has identified cut points of patient-reported changes in pain and function as valid and reliable markers of response to TKR [6]. In addition to this, patient satisfaction is considered an important outcome measure post TKR, as endorsed by a patient and surgeon derived Delphi study conducted by the Outcome Measures in Rheumatology [7].
Despite the importance of measuring patient satisfaction as a reflection of the value of the orthopaedic intervention, the satisfaction instruments and quantification methods used after TKR are highly heterogeneous [8]. A previous systematic review [8] investigated the available literature on satisfaction after TKR and found only 13% of the included studies used a satisfaction instrument which had demonstrated some form of validity. Furthermore, 21.2% did not define how they measured satisfaction, and the remaining 65.8% drew on a variety of questions and quantification methods to measure this construct [8]. These observations may explain why satisfaction estimates have been reported to vary extensively, from as high as 99% [9], to findings as low as 70% [10,11]. The reasons for such heterogeneity have not been rigorously investigated, however a recent study [12] indicates the importance of how the satisfaction questions are framed. The authors found the focus of the satisfaction question (such as general satisfaction as compared to satisfaction with recreational activities) significantly affected the rates of satisfaction by as much as 10% [13].
These findings highlight the importance of understanding the different aspects of satisfaction. According to satisfaction theory, satisfaction is multifactorial and includes numerous variables that are likely to contribute to a patient's appraisal [14]. When considering the complexity of satisfaction theory in combination with the heterogeneity and lack of validation of the commonly used satisfaction instruments, it is not possible for researchers and clinicians to have an understanding of what is actually being captured by the various instruments.
To create certainty around what is being measured by patient reported outcome measures (PROMs), including those assessing satisfaction, confirmation of content validity is essential [15]. Content validity is the degree to which the content of a PROM is an adequate reflection of the construct to be measured, and is considered the most important measurement property of a PROM [15]. Content validity comprises three key aspects: content relevance (all items should be relevant for the construct of interest), content comprehensiveness (no key aspects of the construct should be missing), and content comprehensibility (the items should be understood by patients as intended) [15]. To achieve these three key aspects of content validity, the involvement of the patient in PROM development is essential. This includes patient involvement in theory development, item development, and item testing in terms of understanding of content and response categories.
To facilitate a better and more consistent understanding of patient satisfaction, the aims of this review were therefore to i) evaluate the proportion of people reported to be satisfied after TKR for osteoarthritis; and ii) assess the content validity of the utilised satisfaction measures.
2. Methods
The review protocol was prospectively registered on PROSPERO (CRD42017058936) and reported according to PRISMA guidelines [16]. Assessment of content validity of measures was additional to this protocol as the need for this aspect became apparent during the review process.
2.1. Literature search
We developed an electronic search strategy (See Appendix 1) of all available data from inception until September 2018 to identify eligible studies in the MEDLINE, EMBASE, CINAHL databases and the Cochrane Database of Registered Trials. We searched the databases using the following terms: ‘Total Knee Arthroplasty’ OR ‘Total Knee Replacement’ AND ‘Patient satisfaction’ and imported retrieved titles and abstracts into the Endnote software (Clarivate Analytics, Philadelphia, PA, USA) and removed duplicates.
2.2. Study selection
The inclusion criteria (Table 1) were devised by the research team with clinical and research expertise in TKR (AS, MD, PC); and systematic reviews (AS, PK, RF, SB). Titles and abstracts were uploaded into Covidence (Covidence, Melbourne, Victoria, Australia) to facilitate the screening process. Two reviewers (SB, RF) independently screened titles and abstracts for inclusion. Where information was not explicitly presented in the title and abstract e.g. unilateral versus bilateral TKR, the full text article was retrieved for screening. Full text articles were independently screened by three authors (SB, RF, NK). Disagreements were resolved by consultation with the other authors until consensus was reached. Given the volume of papers requiring screening, if the information to meet inclusion was not reported in the full text article, the articles were excluded without contacting the study authors.
Table 1.
Inclusion criteria.
| Criteria | Definition/justification |
|---|---|
| Unilateral, primary total knee replacement | We included studies in which participants underwent total knee replacement. We excluded studies in which participants underwent unicompartmental knee replacement as satisfaction levels may differ significantly between patients with unicompartmental and total knee replacement [17]. We included studies where <5% of participants underwent simultaneous bilateral TKR*. This is because satisfaction levels may be significantly different among people who receive a unilateral versus simultaneous bilateral TKR [18]. Studies involving participants undergoing their second primary TKR were included. Where it was unclear whether the bilateral TKRs were simultaneous or staged, it was assumed that they were simultaneous. We included studies where <5% of participants underwent revision TKR. This is because satisfaction levels may be significantly different among people who receive a primary versus revision TKR [19]. The 5% cut-off enabled us to include relevant studies where 95% of participants met our criteria. We anticipated that a 5% threshold would not significantly impact satisfaction outcomes reported in this review. |
| Total knee replacement for osteoarthritis of the knee | We included studies where <5% of participants underwent TKR for pathologies other than osteoarthritis. This is because the concerns and priorities of patients undergoing TKR differ according to their underlying diagnosis and the satisfaction levels may be significantly different between people undergoing TKR for osteoarthritis versus other pathology [20]. Accordingly, we excluded studies that did not explicitly state the reason for performing TKR. |
| Satisfaction measured ≥6 months post-operatively | We included studies that assessed satisfaction ≥6 months post TKR in order to capture satisfaction with outcome rather than process of care, and in light of evidence that 6 months would be a sufficient minimum time-frame in which to assess satisfaction given the majority of improvement in function after TKR takes place in the first 6 months post-surgery [21]. |
| Satisfaction with total knee replacement outcome | We excluded studies that assessed satisfaction with the process of care, as this is a different construct to satisfaction with treatment outcome. We also excluded studies that did not include a measure of satisfaction with treatment outcome, but instead, inferred patient satisfaction from changes in knee pain or function following TKR [22]. |
| Quantitative studies | We excluded any qualitative studies as our aim was to quantify satisfaction with TKR. |
| Original, full text articles | We excluded review papers and conference abstracts. |
| Articles written in English | Given the large scope of this review, for pragmatic reasons we excluded studies that were not written in English |
2.3. Assessment of methodological quality
Two reviewers (SB and NK) independently assessed risk of bias using a purposely adapted tool based on an existing tool for assessing risk of bias in prevalence studies [17]. The existing tool was modified to accommodate the range of study designs included in this review such as prospective cohort studies, retrospective studies of registry data and randomised control trials. The adapted tool comprises ten domains; each domain was scored as low or high risk of bias (see Appendix 2). Of the ten assessment items, seven were ‘asterisked’, which indicated immediate exclusion of a study with failure of any of these items (see Appendix 2). Studies meeting all seven asterisked items were included in the review, with studies that failed any of the remaining three non-asterisked items considered to be moderate risk. The risk of bias tool was piloted using studies that did not meet the inclusion criteria to ensure familiarity and consistency of use. The two (SB and NK) reviewers resolved disagreements by consultation until arriving at a consensus decision.
2.4. Data extraction
Two reviewers (SB and NK) independently extracted data from each study using a standardised extraction sheet. Data extracted included characteristics of the study (geographical location, sample size); characteristics of the participants (age, percentage female); characteristics of the outcomes (satisfaction measure, duration of follow-up); and satisfaction outcome scores. Data extraction sheets from the two reviewers were compared for consistency and accuracy.
2.5. Data synthesis and analysis
2.5.1. Description of satisfaction after TKR
Given the multiple ways in which satisfaction was measured the authorship team took various steps to extract percentage satisfied from each study included in the review, which are detailed in Table 2.
Table 2.
Method of extracting percentage satisfied.
| Study reporting method | Approach to extract percentage satisfied |
|---|---|
| Means and SD, or proportion values of categorical satisfaction scales | Percentage satisfied was derived from the sample size |
| Visual analogue scales reported | A satisfaction threshold was chosen based on the ‘smile face’ scale, where the point at which the face begins to smile was considered to be ‘satisfied’ (see Fig. 1); in a 1–10 scale, a score of 7 or more was chosen; in a 1–5 scale, 4 or more was chosen. The percentage of satisfied people was derived by calculating the number of people in the sample who had scores above the appropriate threshold for the data reported. This was achieved by converting the difference between the sample mean and the threshold into a z-score (the number of SD the threshold was away from the mean). The z-score was then converted to a percentile using the NORMDIST function in Excel v16.11 (Microsoft Corp, Redmond, WA, USA) |
| Only medians reported | An approximation of mean values was derived from the median range and sample size using the method of Hozo [18] to attain the percentage satisfied |
| Likert Scales | Outcomes of ‘satisfied’ or ‘very satisfied’ was regarded as a satisfied outcome |
| Knee Society Knee Score Satisfaction scale [19]. Total score of 40 from 5 items each with a maximum score of 8 | A threshold of 28 was selected to indicate satisfaction. This represented a minimum of 4 satisfied answers and 1 neutral answer across the 5 satisfaction items. |
| The Self-Administered Patient Satisfaction Scale for Primary Hip and Knee Arthroplasty [20]. The items are scored on a 4-point Likert scale, with 4 response options: 25 pts (very dissatisfied), 50 pts (somewhat dissatisfied), 75 pts (somewhat satisfied), or 100 pts (very satisfied), which are averaged to give a total score. | A threshold of 68 was selected. The sum score of 68 represented 3 somewhat satisfied and 1 somewhat dissatisfied responses. |
| Multiple satisfaction questions under the one questionnaire | Where possible, these were individually reported as well as reporting a composite score |
| Papers reporting multiple follow-ups | The time point closest to twelve months was selected to be included in the review, based on evidence that this is when maximum improvement in pain and function is attained [21]. |
| Papers only reporting satisfaction outcomes for subgroups of the sample | These subgroup scores were combined into one total group summary score. |
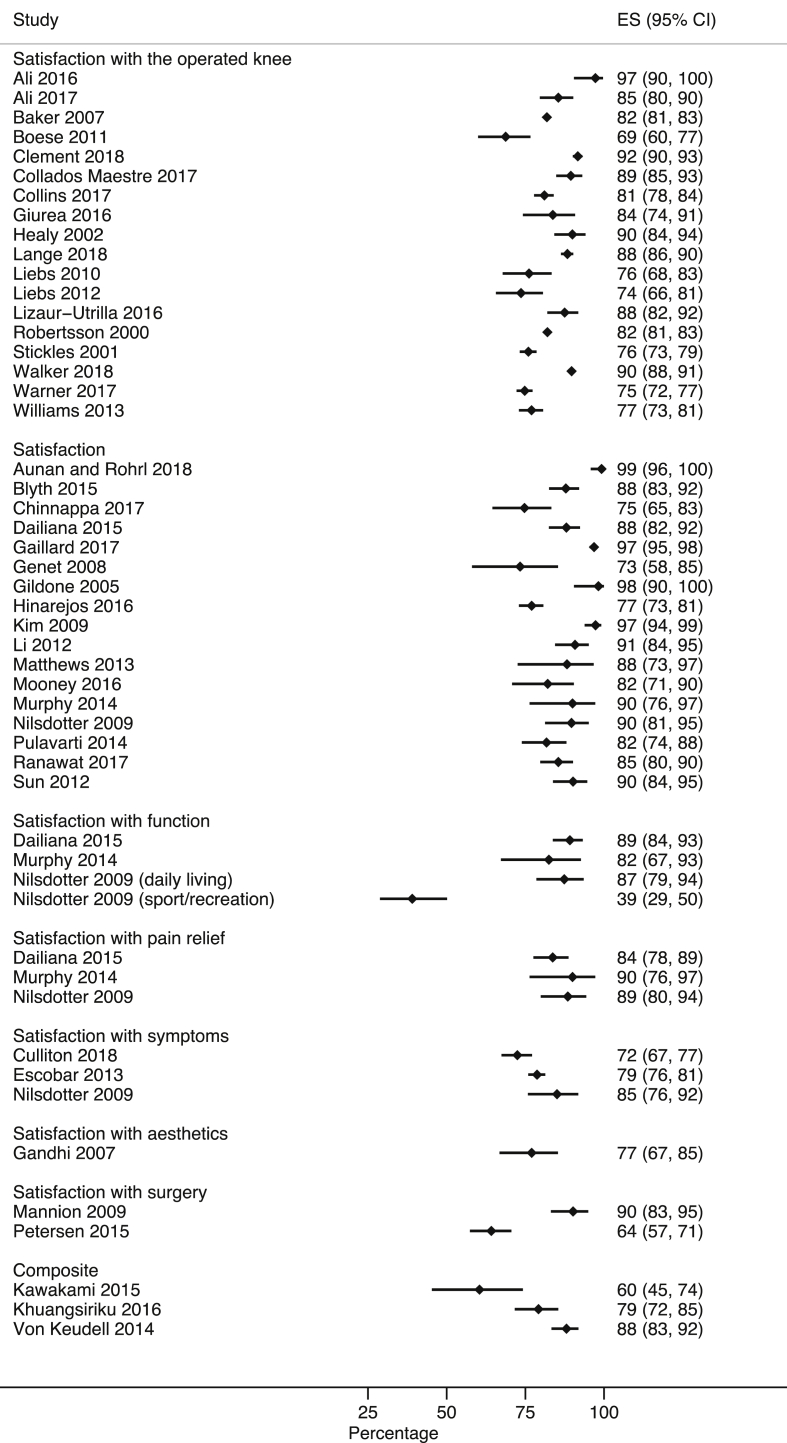
Given the heterogeneity of the satisfaction instruments, it was not appropriate to meta-analyse the results [22]. Therefore, the satisfaction results of each paper are displayed in a forest plot with corresponding description (see Fig. 1).
Fig. 1.
0–10 Smile face satisfaction scale.
2.5.2. Assessment of content validity
Studies included in the review were assessed as to whether a citation was provided for the satisfaction instrument used. The citations were evaluated according to their support for content validity of the satisfaction measure, in terms of either a development study or secondary content validity study. In addition, a specific search strategy was developed to retrieve any studies of content validity for specific satisfaction instruments used by studies in this review, which was approved by the university librarian (see Appendix 3).
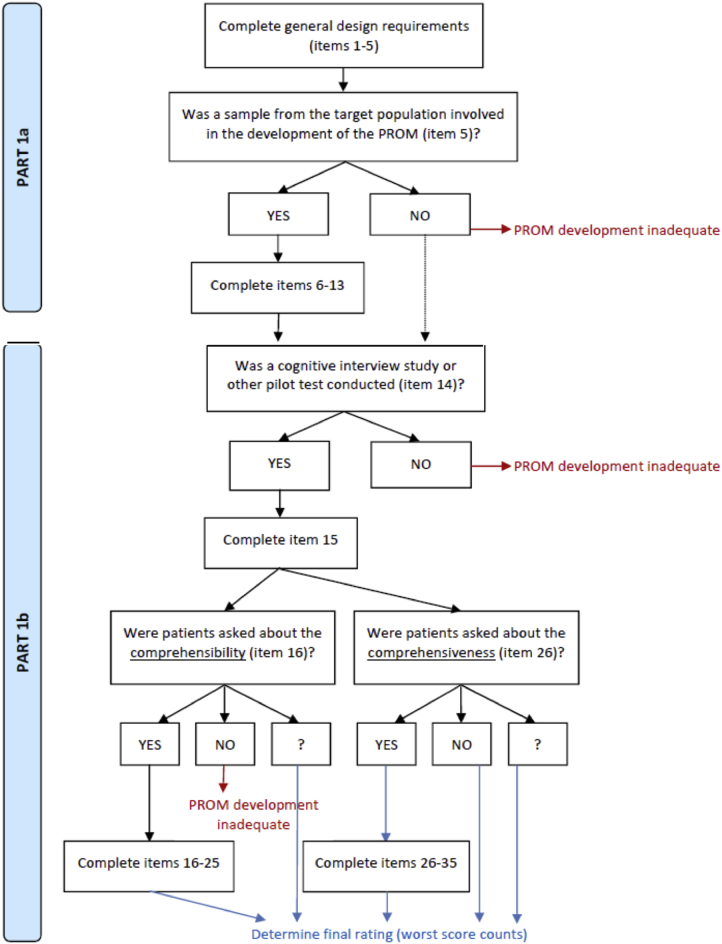
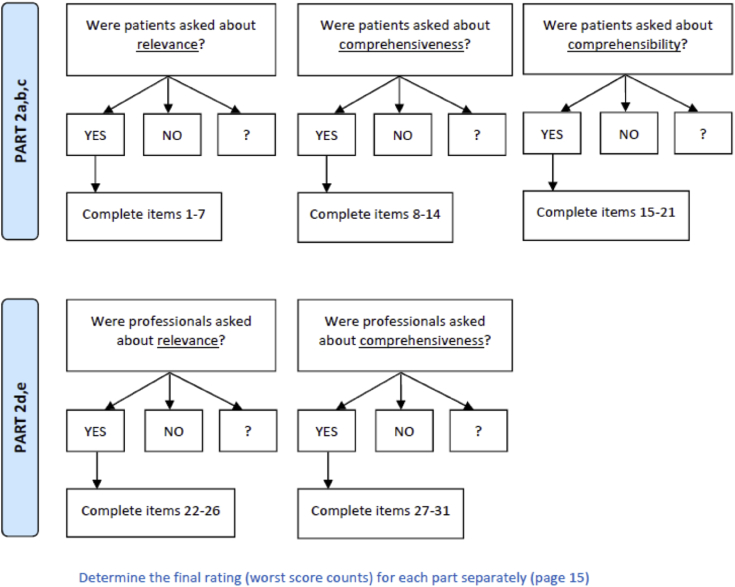
Content validity of satisfaction measures was evaluated using the COnsensus-based standards for the selection of health Status Measurement INstruments (COSMIN) content validity assessment checklist. The COSMIN methodology details that strong evidence of good content validity is achieved through adequate content relevance, comprehensiveness, and comprehensibility. For a PROM to be assessed on these three aspects, the COSMIN methodology has expanded them to create the ten criteria for good content validity, which includes five items under ‘relevance’, one item under ‘comprehensiveness’, and four items under ‘comprehensibility’ (see column 1 of Table 4a, Table 4ba and 4b). To assess whether these ten criteria have been met, the COSMIN methodology details a systematic three step process, whereby the final stage rates the PROM against the ten criteria. Single questions used by studies that were unsupported by the literature could not be assessed for evidence of content validity, in accordance with the COSMIN assessment. This process was conducted by two authors (AS and NK).
Table 4a.
Content validity assessment of the SAPSS.
| PROM development study 1 | PROM development study 2 | Content validity study | Rating of reviewers | Overall rating per PROM | Quality of evidence | |
|---|---|---|---|---|---|---|
| Self-administered patient satisfaction scale | Development study [67] | Development study [20] | NA | +/−/? | +/−/± | High, moderate, low, very low |
| Relevance | ||||||
|
– | – | + | |||
|
– | – | + | |||
|
+ | + | + | |||
|
– | – | + | |||
|
– | – | ? | |||
| Relevance rating | – | – | NA | + | ± | Low |
| Comprehensiveness | ||||||
|
– | – | – | |||
| Comprehensiveness rating | – | – | NA | – | – | Low |
| Comprehensibility | ||||||
|
– | – | ||||
|
– | – | ||||
|
+ | |||||
|
+ | |||||
| Comprehensibility rating | – | NA | + | ± | Low | |
| Content validity rating | – | Low | ||||
Legend: - Fail + Pass ? Insufficient information ± Inconsistent.
Table 4b.
Content validity assessment of the new KSKSS.
| PROM development study | Content validity study | Rating of reviewers | Overall rating per PROM | Quality of evidence | |
|---|---|---|---|---|---|
| Satisfaction domain of the New Knee Society Knee Scoring System | Development Study [68] | NA | +/−/? | +/−/± | High, moderate, low, very low |
| Relevance | |||||
|
– | + | |||
|
– | + | |||
|
+ | + | |||
|
– | + | |||
|
– | ? | |||
| Relevance rating | – | NA | + | ± | Low |
| Comprehensiveness | |||||
|
– | – | |||
| Comprehensiveness rating | – | NA | – | – | Low |
| Comprehensibility | |||||
|
– | ||||
|
– | ||||
|
+ | ||||
|
+ | ||||
| Comprehensibility rating | – | NA | + | ± | Low |
| Content validity rating | – | Low | |||
Legend: - Fail + Pass ? Insufficient information ± Inconsistent.
The first phase of this process involved assessment of any development study of the satisfaction measure against steps 1a and 1b in the COSMIN assessment (see Appendix 4). Any further content validity studies in addition to development studies were assessed against steps 2a – 2e (see Appendix 5). Step 3 was a final appraisal of the ten criteria for good content validity. Step 3 involved appraising the development study, the content validity study (if available) as well as the reviewers’ opinion against the ten criteria for good content validity (see column 5 of Table 4a, Table 4ba and 4b).
3. Results
3.1. Literature search and risk of bias assessment
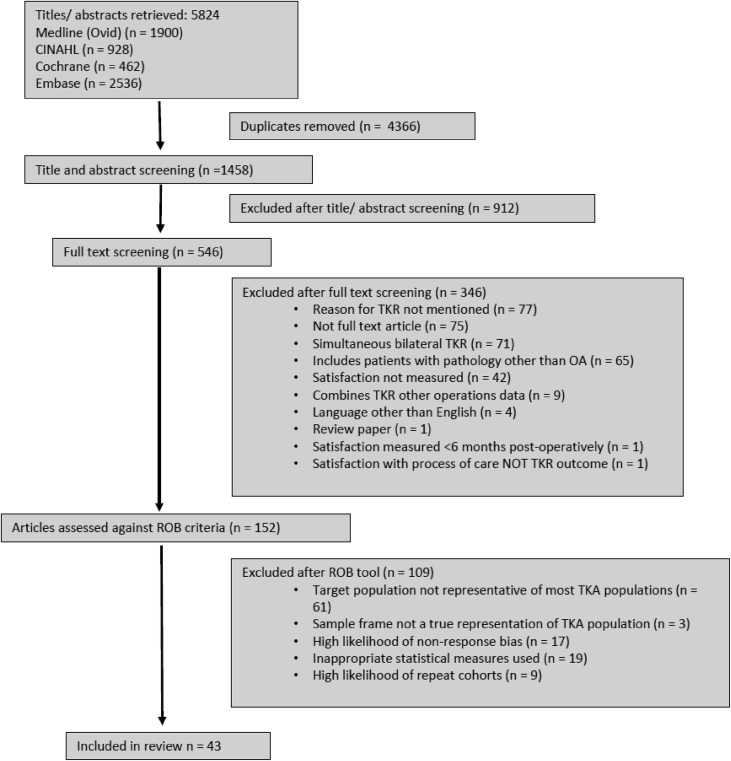
Our search strategy identified a total of 5824 records of which 2828 records were non-duplicates. After screening of titles and abstracts, 546 papers remained for full text screening. Following this, we excluded a further 346 articles leaving 152 articles for analysis of risk of bias. Forty-three articles passed the risk of bias assessment to be included in this systematic review (see Fig. 2), with 35 considered moderate risk due to failing one or more of the non-asterisked risk of bias items and eight considered low risk (see Appendix 6).
Fig. 2.
Study selection flow diagram.
3.2. Study characteristics
Individual study characteristics are presented in Table 3.
Table 3.
Study characteristics.
| Study | Year | Country | Mean age (SD) | Design | Sample Size | Female (n) | Satisfaction question | Construct |
|---|---|---|---|---|---|---|---|---|
| Ali et al. [23] | 2016 | Sweden | 68.5 (4) | RCT | 74 | 21 | Degree of satisfaction with the operated knee: ‘very satisfied’, ‘satisfied’, ‘uncertain’, ‘dissatisfied’ | Satisfaction with the operated knee |
| Ali et al. [24] | 2017 | Sweden | 72.9 (9.7) | RCT | 186 | 16 | Degree of satisfaction with the operated knee: ‘very satisfied’, ‘satisfied’, ‘uncertain’, ‘dissatisfied’ | Satisfaction with the operated knee |
| Aunan and Rohl [25]. | 2018 | Norway | 69.3 (7.4) | Prospective cohort | 129 | 73 | Patient satisfaction measures on a VAS | Satisfaction |
| Baker et al. [26] | 2007 | England and Wales | 70.8 (9.4) | Retrospective cohort | 8231 | 4675 | “Are you satisfied with your knee replacement?”: ‘yes’, ‘no’ and ‘not sure’. | Satisfaction with the operated knee |
| Blyth et al. [27] | 2015 | Scotland | 65.5 | Prospective cohort | 198 | 116 | Overall satisfaction: ‘very satisfied’, ‘satisfied’, ‘don't know’, ‘unsatisfied’, ‘very unsatisfied’ | Satisfaction |
| Boese et al. [28] | 2011 | USA | 64 | Retrospective cohort | 128 | 90 | “How happy are you with your implanted knee?”: measured on a scale of 1–5 where 1 = completely dissatisfied to 5 = completely satisfied | Satisfaction with the operated knee |
| Clement et al. [12] | 2018 | United Kingdom | 68.6 (9.3) | Retrospective cohort | 1255 | 757 | ‘How satisfied are you with the results of your knee replacement surgery?’ ‘Very satisfied’, ‘somewhat satisfied’, ‘somewhat dissatisfied’, and ‘very dissatisfied’ | Satisfaction with the operated knee |
| Collados-Maestre et al. [29] | 2017 | Spain | 71.2 (6.4) | Prospective cohort | 237 | 164 | ‘Patient satisfaction was evaluated yearly on a 5-point Liker scale’ ‘very satisfied’, ‘satisfied’, ‘neutral’, ‘dissatisfied’, and ‘very dissatisfied’ | Satisfaction with the operated knee |
| Collins et al. [30] | 2017 | USA | 69.5 (8.5) | Prospective cohort | 633 | 375 | ‘How satisfied are you with the results of your knee replacement surgery?’ ‘very satisfied’ ‘somewhat satisfied’ ‘somewhat dissatisfied’ and ‘very dissatisfied’ | Satisfaction with the operated knee |
| Culliton et al. [31] | 2018 | Canada | 63.5 (8) | Prospective cohort | 345 | 221 | Patient Acceptable Symptom State | Satisfaction with symptoms |
| Dailiana et al. [32] | 2015 | Greece | 69.2 (6.7) | Prospective cohort | 204 | 162 | Patient satisfaction with the results of TKR was assessed in three aspects: overall satisfaction, satisfaction with pain relief, and satisfaction with functional improvement/ability to perform daily activities. Patients were categorized as very/mostly satisfied, somewhat satisfied, and dissatisfied. (modified Self-Administered Patient satisfaction Scale) | Satisfaction Satisfaction with function Satisfaction with pain relief |
| Escobar et al. [33] | 2013 | Spain | 71.4 (6.9) | Prospective cohort | 912 | 641 | Patient Acceptable Symptom State | Satisfaction with symptoms |
| Gaillard et al. [34] | 2017 | Germany | 72.7 | Retrospective cohort | 1059 | 650 | Not specified. ‘Very satisfied’, ‘satisfied’, ‘disappointed’ | Satisfaction |
| Gandhi et al. [35] | 2007 | Canada | 69.2 (8.8) | Prospective cohort | 87 | 56 | Are you satisfied with your limb alignment? ‘Yes’ or ‘No’ | Aesthetics |
| Genet et al. [36] | 2008 | France | 71.7 (7) | Prospective cohort | 45 | 28 | Patient satisfaction measured on a VAS (0–100) | Satisfaction |
| Gildone et al. [37] | 2005 | Italy | 74.1 (4.8) | Prospective cohort | 56 | 39 | Satisfaction questionnaires. No response categories provided | Satisfaction |
| Giurea et al. [38] | 2016 | Austria | 66 (NA) | Prospective cohort | 86 | 48 | Satisfaction with response categories: ‘Yes’ or ‘No’ | Satisfaction with the operated knee |
| Healy et al. [9] | 2002 | USA | 69.9 (8.7) | Prospective cohort | 159 | – | Patient satisfaction measured with response categories: ‘yes’ or ‘no’ | Satisfaction with the operated knee |
| Hinarejos et al. [39] | 2016 | Spain | 72.2 (7) | Prospective cohort | 474 | 360 | Satisfaction measured on a VAS (0 = absolutely dissatisfied, 10 = absolutely satisfied) | Satisfaction |
| Kawakami et al. [40] | 2015 | Japan | 74.3 (7.8) | Prospective cohort | 48 | 25 | Satisfaction domain of the new Knee Society Knee Scoring System questionnaire | Composite |
| Khuangsiriku et al. [41] | 2016 | Thailand | 76.9 (7.4) | Prospective cohort | 144 | 130 | The Self-Administered Patient Satisfaction Scale | Composite |
| Kim et al. [42] | 2009 | Korea | 68.5 (5.6) | Prospective cohort | 186 | 177 | British Orthopaedic Association Patient Satisfaction Score | Satisfaction |
| Li et al. [43] | 2012 | China | 67.2 (7.2) | Retrospective cohort | 130 | 97 | The British Orthopaedic Association Patient Satisfaction Score | Satisfaction |
| Liebs et al. [44] | 2010 | Germany | 69.8 (7.9) | RCT | 136 | 114 | Total Hip Arthroplasty Outcome Evaluation Questionnaire | Satisfaction with the operated knee |
| Liebs et al. [45] | 2012 | Germany | 69.8 (8.1) | RCT | 158 | 133 | Total Hip Arthroplasty Outcome Evaluation Questionnaire | Satisfaction with the operated knee |
| Lizaur-Utrilla et al. [46] | 2016 | Spain | 69.7 (5.9) | Prospective cohort | 192 | 127 | Satisfaction measured with response categories: ‘very satisfied’, ‘satisfied’, ‘neutral’, ‘dissatisfied’, ‘very dissatisfied’ | Satisfaction with the operated knee |
| Mannion et al. [47] | 2009 | Switzerland | 67 (9) | Prospective cohort | 112 | 7 | Satisfaction with surgery measured with the response categories: ‘very satisfied’, ‘somewhat satisfied’, ‘somewhat dissatisfied’, ‘very dissatisfied’ | Satisfaction with surgery |
| Matthews et al. [48] | 2013 | UK | 69.2 (7.7) | Prospective cohort | 34 | 20 | Patient satisfaction measured on a 10-point VAS. | Satisfaction |
| Mooney et al. [49] | 2016 | Australia | 68 (11.3) | Cross-sectional | 67 | 43 | Knee Society Score containing post-operative satisfaction scores | Satisfaction |
| Murphy et al. [50] | 2014 | Australia | 70.8 (9.9) | RCT | 40 | 25 | Satisfaction with pain relief, physical function and overall outcome measured on a VAS (0 = completely unsatisfied to 10 = completely satisfied) | Satisfaction with function |
| Nilsdotter et al. [51] | 2009 | Sweden | 72 (8) | Cross-sectional | 87 | 50 | Satisfaction with result in general measured on 5-point Likert scale from ‘totally satisfied’ to ‘very dissatisfied’. Questions about satisfaction in relation to pain relief; symptom relief; improvement in activities of daily living; and improvements in sport and recreational function. Dimensions measured on 5-point Likert scale from ‘totally satisfied’ to ‘very dissatisfied’. |
Satisfaction Satisfaction with function (activities of daily living and sports and recreation) Satisfaction with symptoms |
| Petersen et al. [10] | 2015 | Denmark | 65 (6.3) | Cross-sectional | 215 | 139 | Satisfaction with surgery measured with response categories: ‘very satisfied’, ‘satisfied’, ‘not completely satisfied’, ‘not satisfied’ | Satisfaction with surgery |
| Pulavarti et al. [52] | 2014 | UK | 69.9 (8.3) | RCT | 126 | 68 | Satisfaction measured with response categories: ‘excellent’, ‘good’, ‘fair’, ‘poor’ | Satisfaction |
| Ranawat et al. [53] | 2017 | USA | 71 (7.3) | Prospective cohort | 193 | 138 | Satisfaction measured on a VAS (0−10) | Satisfaction |
| Robertsson et al. [54] | 2000 | Sweden | – | Cross-sectional | – | – | Satisfaction with the operated knee measured with response categories: ‘very satisfied’, ‘satisfied’, ‘uncertain’, ‘dissatisfied’ | Satisfaction with the operated knee |
| Stickles et al. [55] | 2001 | USA | 69.9 (11.9) | Cross-sectional | 1011 | 637 | “How satisfied are you with the results of your joint replacement?”: ‘very satisfied’, ‘somewhat satisfied’, ‘neutral’, ‘somewhat dissatisfied’, ‘very dissatisfied’ | Satisfaction with the operated knee |
| Sun et al. [56] | 2012 | China | 64.7 (4.4) | RCT | 132 | 80 | Satisfaction (reported as % satisfied) | Satisfaction |
| Von Keudell et al. [57] | 2014 | USA | 62.6 (11.2) | Cross-sectional | 245 | 165 | Satisfaction in respect to pain, motion, daily living function, return to sport activities and ability to kneel. Each dimension measured on a VAS (0 = not satisfied, 10 = very satisfied) | Composite |
| Walker et al. [58] | 2018 | UK | 68.9 (9.6) | Retrospective cohort | 2578 | 1396 | ‘How satisfied are you with the results of your knee replacement surgery’ ‘very satisfied’, ‘somewhat satisfied’, ‘somewhat dissatisfied’, and ‘very dissatisfied’ | Satisfaction with the operated knee |
| Warner et al. [59] | 2017 | UK | 73.1 (8.7) | Prospective cohort | 1151 | 653 | ‘Individuals were asked to state how satisfied they felt with their total joint replacement using an ordinal scale’ ‘very satisfied’, ‘not very satisfied’, and ‘dissatisfied’ | Satisfaction with the operated knee |
| Williams et al. [60] | 2013 | UK and Ireland | 70.9 (8.6) | Prospective cohort | 486 | 314 | ‘How do you feel overall about your replaced joint?’ ‘very happy’, ‘happy’, ‘OK (not perfect)’, or ‘never happy’ | Satisfaction with the operated knee |
3.3. Satisfaction estimates
Due to the heterogeneity in the focus of the satisfaction questions used by the studies, results were grouped into ‘like’ constructs. Composite scales consisting of questions with different foci of satisfaction are reported as composite, and also as single items under specific constructs where possible (see Fig. 3).
Fig. 3.
Proportion of patients satisfied after TKR. ES = effect size.
3.3.1. Single item satisfaction questions
The construct ‘Satisfaction with the operated knee’ included all questions that asked about satisfaction with the total joint replacement (TJR), TKR, operated knee, or surgery on the operated knee. Eighteen studies were included under this construct and the proportion satisfied ranged from as high as 97% (CI 90 to 100) to as low as 69% (CI 60 to 77). Two studies used a question which is part of the multi-domain Total Hip Arthroplasty Outcome Evaluation Questionnaire (THAOEQ) [44,45]. Thirteen studies provided no citation in support of the single item question used [9,23,24,26,28,30,38,54,55,[58], [59], [60], [61]], while 3 studies cited another study that had utilised the same single item question [12,29,46]; however, there was no further citation to support the validity of these questions.
The construct ‘Satisfaction’ included all questions that did not focus on any particular aspect of satisfaction. Of the 17 studies included, the proportion satisfied ranged from as high as 99% (CI 96 to 100) to as low as 73% (CI 58 to 85). One study used a question that was an item from the Self-Administered Patient Satisfaction Scale (SAPSS) [32], and 2 used an item from the surgeon-completed multi-domain British Orthopaedic Association (BOA) grading system [42,43]. Of the remaining studies, 13 provided no citation in support of the single item question used [25,27,34,36,37,39,48,50,52,53,56,62,63], and 1 study provided a citation that had no evidence of satisfaction content [49].
The construct ‘Satisfaction with function’ included all questions that asked about satisfaction with function, ADLs, sport, or recreation. The proportion satisfied from the 3 studies included ranged from 89% (CI 84 to 93) to to 39% (CI 29 to 50). One study used an item from the SAPSS [32], the remaining 2 studies used single items with no supporting citation [50,63].
The construct ‘Satisfaction with pain relief’ included all questions that asked about satisfaction with pain relief. Three were included and ranged from 90% (CI 76 to 97) to 84% (CI 78 to 89). One study cited a questionnaire, the SAPSS [32], while the remaining 2 studies did not have a supporting citation for their single item question [50,63].
The construct ‘Satisfaction with symptoms’ included all questions that asked about satisfaction with symptoms. Three were included and ranged from 85% (CI 76 to 92) to 72% (CI 67 to 77). Two studies used a question previously considered as a Patient Acceptable Symptom State (PASS) estimate [31,33]. The remaining study did not provide a citation in support of the single item question [63].
The construct ‘Satisfaction with aesthetics’ included questions that asked about the visual appearance of the knee. Only 1 study was included, which reported a satisfaction rate of 77% (CI 67 to 85), and did not provide a citation in support of the single item question [35].
The construct ‘Satisfaction with surgery’ included all questions that asked about satisfaction with the surgery but did not have reference to knee TJR, TKR, or operated knee. Two studies were included and ranged from 90% (CI 83 to 95) to 64% (57–71), neither of which provided a citation in support of the single item questions [10,47].
3.3.2. Composite scores
Three studies used composite instruments of items covering different components of satisfaction, with satisfaction estimates ranging from 88% (CI 83 to 92) to 60% (45–74). One study used the five-item satisfaction component of the New Knee Society Knee Scoring System (KSKSS) [40] which covers satisfaction with pain level while sitting, pain level while lying in bed, knee function while performing light household duties, and knee function while performing leisure recreational activities. One study used the four item SAPSS [41] covering overall satisfaction with surgery, satisfaction with pain relief, satisfaction with home and yard work, and satisfaction with recreational activities, and 1 study reported an unreferenced composite score of 5 items including satisfaction in respect to pain, motion, daily living function, return to sport activities, and ability to kneel [57].
3.4. Assessment of content validity
Of the 43 articles included in the review, 15 provided a citation for the satisfaction instrument used. Of these, only 9 studies, using a total of 6 satisfaction instruments, had a citation in support of content validity, in the form of a development study. These instruments included BOA, the new KSKSS, THAOEQ, and SAPSS, and questions previously considered indicators of Patient Acceptable Symptom State (PASS). The latter were excluded from further assessment as they pertain to current symptom state rather than to aspects related to TKR per se [64]. The BOA was excluded as it is completed by the surgeon and therefore not a PROM [65]. The THAOEQ was excluded as it was designed for a total hip replacement population rather than a TKR population [66], and in accordance with COSMIN criteria of ‘relevance’ cannot be considered for assessment of content validity [15]. Furthermore, the extent of development for the THAOEQ was poor and did not include patient appraisal [66]. An additional search was conducted for the SAPSS and new KSKSS to retrieve any further development or content validity studies (See Appendix 3), but none were identified. Both of these instruments were then assessed for content validity as per the COSMIN criteria (see Table 4a, Table 4ba and 4b and Appendix 4, Appendix 5).
Two development studies were retrieved for SAPSS: an abstract from 1998 [67] and a full text article from 2011 [20]. Both of these studies failed to demonstrate all three key aspects of content validity (see Table 4a). Although a Delphi panel of experts was used for development of the SAPSS, this did not include patient input, which is required for content validity. Reviewer rating of the instrument passed relevance and comprehensibility. The overall rating was a low quality PROM (see Table 4a). One development study was retrieved for the new KSKSS [68] and this study failed to demonstrate all three key aspects of content validity. Although the new KSKSS did have patient input in its development, this did not include the satisfaction items [68]. The five satisfaction items of the new KSKSS were based on the four item SAPSS, which as previously described did not include patient appraisal. Reviewer rating of the instrument passed relevance and comprehensibility. The overall rating was a low quality PROM (see Table 4b). Overall, none of the satisfaction instruments included in the review had adequate evidence of content validity.
4. Discussion
The aims of this review were to evaluate rates of patient reported satisfaction after TKR for OA across the literature, and to assess the content validity of the satisfaction measures utilised in evaluated studies. The results demonstrate heterogeneity in not only the focus of the satisfaction questions, but also the estimate of the proportion satisfied across studies.
From the 43 included studies, 8 satisfaction constructs were identified. In addition to heterogeneity in the satisfaction question used, heterogeneity in the estimate of satisfaction was also observed within constructs; most notably 39% (CI 29 to 50) compared to 89% (CI 84 to 93) in satisfaction with function. Due to the heterogeneity in satisfaction questions, it was not possible to pool all estimates, as per the Cochrane guidelines for systematic reviews [22]. Cochrane state that in the absence of longitudinal evidence of correlation of 2 or more PROMs, data pooling should not be conducted, but instead, grouping of like constructs as decided intuitively by the authorship team [22]. These findings are in alignment with the results of Kahlenberg [8] who also reported heterogeneous methods of measuring patient satisfaction after TKR [8].
The present review extends that of Kahlenberg [8] by evaluating the evidence for content validity of the utilised instruments. Two satisfaction instruments (SAPSS and new KSKSS) were cited by Kahlenberg [8] as being validated, but this was only in reference to construct validity, defined as the degree to which the scores of a PROM are consistent with hypotheses, based on the assumptions that the PROM validity measures the construct to be measured [15], or structural validity, which relates to how well the PROM scores reflect the dimensionally of the construct [15], not content validity. These 2 instruments were specifically evaluated for evidence of content validity in this current review, and no evidence for content validity was identified. Although reviewer ratings determined that both instruments had reasonable content relevance and comprehensiveness, the lack of patient involvement in the development of these instruments is a key concern for content validity.
Without patient consultation it is difficult to know whether these instruments include relevant items to accurately capture an individual's satisfaction with their TKR, whether they capture all aspects of satisfaction, or how patients comprehend/interpret the questions. Prior to designing a PROM, theoretical understanding of the construct of interest should be robust so to inform the content of the instrument [14,69]. In the case of satisfaction, PROM development has preceded theoretical understanding, compounding the difficulty in understanding how to measure this construct. This leaves researchers and clinicians to make assumptions regarding what satisfaction instruments are actually measuring. This lack of theoretical grounding in patient satisfaction instruments is a likely contributor to the variability in satisfaction instruments and estimates.
Given the limited understanding of patient satisfaction after TKR, some authors have based the design of satisfaction instruments on other correlates, such as improved pain or other disease-specific questionnaires. This approach is discussed by Robertsson et al. [54], who used a single item question: ‘three questions were asked, including one on satisfaction regarding the operated knee with four possible answers; 1) very satisfied, 2) satisfied, 3) uncertain, or 4) dissatisfied’. This question has not been validated, but has been replicated in three other studies included in the present review [23,29,46]. The authors suggest that a strategy to overcome the lack of content validity in satisfaction instruments is to demonstrate construct validity [54]. However, the presence of an association between a satisfaction instrument and other measures, such as self-reported disability or pain, does not mean the construct of satisfaction has been adequately captured in terms of relevance and comprehensiveness. For example, in the aforementioned study, 11% of patients chose ‘uncertain’ as the response option, and understanding this response is difficult due to a lack of the patients' perspective [54].
The results of the present review also highlighted numerous concerns regarding the appropriateness and consistency of satisfaction instruments. As mentioned earlier, the BOA, which was utilised by two studies [42,43], is designed to be completed by the surgeon rather than the patient, therefore this assessment cannot be considered a PROM [65]. The THOEQ, utilised by two studies [44,45], in addition to not being relevant to the target population, lacked any patient involvement and was only developed from the perspective of an orthopaedic task force that aimed to design a questionnaire from a patient perspective [66]. Questions considered indicators of PASS were utilised by two studies [31,33]. Although development of PASS questions has included patient involvement regarding the relevance and the external anchors during a special interest group meeting [64], they pertain to current symptom state rather than to aspects related to TKR per se [64]. Additionally, the Osteoarthritis Research Society International, which developed the PASS, has identified problems with the consistency of the PASS question and timeline of measurement in this population, suggesting further development studies are required [70]. Lastly, Dailiana [32], who cited the SAPSS, modified the instrument to include only three items of satisfaction as opposed to the four-item questionnaire designed by Mahomed [25], therefore not accurately representing the original intentions of the validated instrument.
Other measures such as ‘would you recommend a joint replacement to a friend?’, ‘would you have a joint replacement again?’, or the Forgotten Joint Score [71] have also been considered to reflect patient satisfaction after TKR in the literature. Although it may seem reasonable to assume these questions would align with satisfaction, this has not been investigated in a TKR population. Patient expectations have also been attributed to patient satisfaction after TKR [11,72]. Despite the literature search retrieving many studies measuring expectations as a means of gauging satisfaction, the authorship team chose not to include expectations as a measure of satisfaction due to it being undertheorised in a healthcare context [14,73]. Presently, expectations are understood from their historical origins in market research, whereby satisfaction is considered an evaluation of a purchase [73]. The role of expectation theory in understanding satisfaction with TKR remains unclear.
This review highlights a need for a better understanding of patient satisfaction after TKR, and suggests more care should be taken in how we interpret studies that use satisfaction as an end point. Future research should focus on conducting qualitative investigations on patient satisfaction after TKR, to build theoretical understanding and provide strong evidence of content validity. To achieve this, researchers may consider conducting focus groups or one on one interviews with patients who have undergone TKR, who have experienced a range of satisfaction, and pain and function outcomes. This has been demonstrated in the development of the Forgotten Joint Score, which sought patient opinion, in addition to multidisciplinary expert opinion, in choosing the items of the instrument [71]. The instrument was then further tested with a second group of patients to test the interpretation of the questions, and refine the question phrasings [74]. These same methods to achieve content validity should be applied to satisfaction instruments after TKR. A better understanding of what patient satisfaction is and how to measure it will optimise the delivery of high quality, patient-centred care in orthopaedics.
Author contributions
All authors have read and approved the present submission to Osteoarthritis and Cartilage Open. Substantial contributions to the research design, or the acquisition, analysis or interpretation of data was completed by NK, SB, PK, MD, PO, RS, RF and AS. Drafting the paper, or critical revisions were completed by NK, SB, PK, MD, PO, RS, PC and AS.
Declaration of Competing Interest
This work was supported by the Centre for Research Excellence in Total Joint Replacement (APP1116325), under a National Health & Medical Research Council, Australia, grant. In addition, personal declarations are as follows:
COI Anne Smith reports grants from National Health & Medical Research Council, during the conduct of the study.
COI Peter O'Sullivan reports grants from National Health & Medical Research Council, during the conduct of the study.
COI Peter Choong reports grants from National Health & Medical Research Council, during the conduct of the study; personal fees from Stryker, personal fees from Johnson & Johnson, grants from Medacta, personal fees from Kluwer, outside the submitted work. Additionally, COI Peter Choong is supported by a National Health & Medical Research Council Practitioner Fellowship (APP1154203).
COI Michelle Dowsey reports grants from National Health & Medical Research Council, during the conduct of the study; grants from Medacta, outside the submitted work.
Additionally, COI Michelle Dowsey is supported by a National Health & Medical Research Council Career Development Fellowship (APP1122526).
Acknowledgements
The authorship teams does not wish to declare any acknowledgements.
Appendix 1. Search strategy in Medline
|
mp denotes keyword.
Appendix 2. Satisfaction with Total Knee Replacement - Risk of Bias Tool
This tool is designed to assess the risk of bias in studies of satisfaction after Total Knee Replacement (TKR). Please read the additional notes for each item when initially using the tool. Note: If there is insufficient information in the article to permit a judgement for a particular item, please answer No (HIGH RISK) for that particular item.
| Risk of bias item | Criteria for answers (please circle one option) | Additional notes and examples |
|---|---|---|
| External Validity | ||
| 1. Was the study's target population representative of most TKR populations on relevant demographic and clinical variables, e.g. age, sex, pain severity, osteoarthritis grade?* |
|
The target population refers to the group of patients to which the results of the study will be generalised. Examples:
|
| 2. Was the sampling frame a true or close representation of the TKR population?* |
|
The sampling frame is a list of the sampling units in the target population and the study sample is drawn from this list. Examples:
|
| 3. Was some form of consecutive or random selection used to select the sample? |
|
In a survey, only part of the sampling frame is sampled. In these instances, consecutive or random selection of the sample helps minimise study bias. Examples:
|
| 4. Was the likelihood of non-response bias minimal?* |
|
Examples:
|
| Internal Validity | ||
| 5. Were data collected* directly from the participants (as opposed to a proxy)? |
|
A proxy is a representative of the subject. Examples:
|
| 6. Was an acceptable participant definition TKR used in the study?* |
|
In a study, the following participant definition was used: “All participants must have had a TKR, which is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability.” The answer is: Yes (LOW RISK).
|
| 7. Was the study instrument that measured satisfaction shown to have reliability and validity (if necessary)? |
|
|
| 8. Was the same mode of data collection used for all participants? |
|
The mode of data collection is the method used for collecting information from the subjects. The most common modes are face-to-face interviews, telephone interviews and self-administered questionnaires. Examples:
|
| 9. Was the length of the measurement period of satisfaction with TKR appropriate?* |
|
The measurement period is the length of time post-surgery. The shorter the measurement period, the greater the likelihood of the participant's satisfaction being about the operative and rehabilitation process rather than about the medium-term or longer-term residual pain and functional capacity. Examples:
|
| 10. Were the statistical measures of satisfaction appropriate?* |
|
|
| 11. Summary item on the overall risk of study bias | ||
| ||
Items with an asterisk will exclude a paper from further consideration (items 1, 2, 4, 5, 6, 9 and 10).
Appendix 3. Content validity search strategy example
Eg: New Knee Society Knee Scoring System.
MEDLINE, SCOPUS, Embase.
Appendix 4. COSMIN assessment of PROM development studies.
Appendix 5. COSMIN assessment of PROM content validity studies.
Appendix 6. Risk of Bias results of all included studies
| Study target population representative of TKR populations* | Sampling frame a true or close representation of TKR populations* | Consecutive or random sample used | Likelihood of non-response bias minimal* | Data collected directly from participants* | Acceptable participant definition TKR used* | Study instrument that measured satisfaction shown to have reliability and validity | Same mode of data collection used for all participants | Appropriate length of measurement period of satisfaction with TKR* | Appropriate statistical measures of satisfaction* | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ali et al., 2016 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Ali et al., 2017 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Aunan and Rohl 2018 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Baker et al., 2007 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Blyth et al., 2015 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Boese et al., 2011 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Chinnappa et al., 2017 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Clement et al., 2013 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Collados Maestre et al., 2016 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Collins et al., 2017 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Culliton et al., 2018 | + | + | + | + | + | + | + | + | + | + | Low risk |
| Dailiana et al., 2015 | + | + | + | + | + | + | + | + | + | + | Low risk |
| Escobar et al., 2013 | + | + | + | + | + | + | + | + | + | + | Low risk |
| Gaillard et al., 2017 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Gandhi et al., 2007 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Genet et al., 2008 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Gildone et al., 2005 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Giurea et al., 2016 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Healy et al., 2002 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Hinarejos et al., 2016 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Kawakami et al., 2015 | + | + | + | + | + | + | + | + | + | + | Low risk |
| Khuangsirku et al., 2016 | + | + | + | + | + | + | + | – | + | + | Moderate risk |
| Kim et al., 2009 | + | + | + | + | + | + | + | + | + | + | Low risk |
| Lange et al., 2018 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Li et al., 2012 | + | + | + | + | + | + | + | + | + | + | Low risk |
| Liebs et al., 2010 | + | + | + | + | + | + | + | + | + | + | Low risk |
| Liebs et al., 2012 | + | + | + | + | + | + | + | + | + | + | Low risk |
| Lizaur Utrilla et al., 2016 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Mannion et al., 2009 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Matthews et al., 2013 | + | + | – | + | + | + | – | + | + | + | Moderate risk |
| Mooney et al., 2016 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Murphy et al., 2014 | + | + | – | + | + | + | – | + | + | + | Moderate risk |
| Nilsdotter et al., 2009 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Petersen et al., 2015 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Pulavarti et al., 2014 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Ranawat et al., 2017 | + | + | + | + | + | + | – | – | + | + | Moderate risk |
| Robertsson et al., 2000 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Stickles et al., 2001 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Sun et al., 2012 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Von keudell et al., 2014 | + | + | – | + | + | + | – | – | + | + | Moderate risk |
| Walker et al., 2018 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Warner e al. 2017 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
| Williams et al., 2013 | + | + | + | + | + | + | – | + | + | + | Moderate risk |
An asterisk (*) denotes a 'fatal flaw' criteria, where failure of any of these items results in immediate exclusion.
References
- 1.Higashi H., Barendregt J.J. Cost-effectiveness of total hip and knee replacements for the Australian population with osteoarthritis: discrete-event simulation model. PloS One. 2011;6(9) doi: 10.1371/journal.pone.0025403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ethgen O., Bruyere O., Richy F., Dardennes C., Reginster J.Y. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J. Bone Jt. Surg. Am. 2004;86-A(5):963–974. doi: 10.2106/00004623-200405000-00012. https://www.ncbi.nlm.nih.gov/pubmed/15118039 [cited May]; Available from: [DOI] [PubMed] [Google Scholar]
- 3.Nashi N., Hong C.C., Krishna L. Residual knee pain and functional outcome following total knee arthroplasty in osteoarthritic patients. Knee Surg. Sports Traumatol. Arthrosc. 2015;23(6):1841–1847. doi: 10.1007/s00167-014-2910-z. [cited Jun] [DOI] [PubMed] [Google Scholar]
- 4.Janse A.J., Gemke R.J., Uiterwaal C.S., van der Tweel I., Kimpen J.L., Sinnema G. Quality of life: patients and doctors don't always agree: a meta-analysis. J. Clin. Epidemiol. 2004;57(7):653–661. doi: 10.1016/j.jclinepi.2003.11.013. [cited Jul] [DOI] [PubMed] [Google Scholar]
- 5.Brokelman R.B., van Loon C.J., Rijnberg W.J. Patient versus surgeon satisfaction after total hip arthroplasty. J. Bone Jt. Surg. Br. 2003;85(4):495–498. https://www.ncbi.nlm.nih.gov/pubmed/12793551 [cited May]; Available from: [PubMed] [Google Scholar]
- 6.Pham T., Van Der Heijde D., Lassere M., Altman R.D., Anderson J.J., Bellamy N., et al. Outcome variables for osteoarthritis clinical trials: the OMERACT-OARSI set of responder criteria. J. Rheumatol. 2003;30(7):1648–1654. https://www.ncbi.nlm.nih.gov/pubmed/12858473 [cited Jul]; Available from: [PubMed] [Google Scholar]
- 7.Singh J., Dowsey M., Choong P. 2017. Patient Endorsement of the Outcome Measures in Rheumatology (OMERACT) Total Joint Replacement (TJR) Clinical Trial Draft Core Domain Set [Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kahlenberg C.A., Nwachukwu B.U., McLawhorn A.S., Cross M.B., Cornell C.N., Padgett D.E. Patient satisfaction after total knee replacement: a systematic review. HSS J [Review] 2018;14(2):192–201. doi: 10.1007/s11420-018-9614-8. [cited Jul] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Healy W.L., Iorio R., Ko J., Appleby D., Lemos D.W. Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. J. Bone Jt. Surg. Am. 2002;84-A(3):348–353. doi: 10.2106/00004623-200203000-00003. https://www.ncbi.nlm.nih.gov/pubmed/11886902 [cited Mar]; Available from: [DOI] [PubMed] [Google Scholar]
- 10.Petersen K.K., Simonsen O., Laursen M.B., Nielsen T.A., Rasmussen S., Arendt-Nielsen L. Chronic postoperative pain after primary and revision total knee arthroplasty. Clin. J. Pain. 2015;31(1):1–6. doi: 10.1097/AJP.0000000000000146. [cited Jan] [DOI] [PubMed] [Google Scholar]
- 11.Bourne R.B., Chesworth B.M., Davis A.M., Mahomed N.N., Charron K.D. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin. Orthop. Relat. Res. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [cited Jan] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clement N.D., Bardgett M., Weir D., Holland J., Gerrand C., Deehan D.J. Three groups of dissatisfied patients exist after total knee arthroplasty: early, persistent, and late. Bone Joint J. 2018;100-B(2):161–169. doi: 10.1302/0301-620X.100B2.BJJ-2017-1016.R1. [cited Feb] [DOI] [PubMed] [Google Scholar]
- 13.Clement N.D., Bardgett M., Weir D., Holland J., Gerrand C., Deehan D.J. The rate and predictors of patient satisfaction after total knee arthroplasty are influenced by the focus of the question: a standard satisfaction question is required. Bone Joint J. 2018;100B(6):740–748. doi: 10.1302/0301-620X.100B6.BJJ-2017-1292.R1. [cited June] [DOI] [PubMed] [Google Scholar]
- 14.Batbaatar E., Dorjdagva J., Luvsannyam A., Amenta P. Conceptualisation of patient satisfaction: a systematic narrative literature review. Perspect. Public Health. 2015;135(5):243–250. doi: 10.1177/1757913915594196. [cited Sep] [DOI] [PubMed] [Google Scholar]
- 15.Terwee C.B., Prinsen C.A.C., Chiarotto A., Westerman M.J., Patrick D.L., Alonso J., et al. 2018. COSMIN Methodology for Assessing the Content Validity of PROMs.https://cosmin.nl/wp-content/uploads/COSMIN-methodology-for-content-validity-user-manual-v1.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [cited Jul 21] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoy D., Brooks P., Woolf A., Blyth F., March L., Bain C., et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 2012;65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014. [cited Sep] [DOI] [PubMed] [Google Scholar]
- 18.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005;5(13) doi: 10.1186/1471-2288-5-13. [cited Apr 20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scuderi G.R., Bourne R.B., Noble P.C., Benjamin J.B., Lonner J.H., Scott W.N. The new knee society knee scoring system. Clin. Orthop. Relat. Res. 2012;470(1):3–19. doi: 10.1007/s11999-011-2135-0. [cited Jan] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mahomed N., Gandhi R., Daltroy L., Katz J.N. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis. 2011;2011:591253. doi: 10.1155/2011/591253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams D.P., Blakey C.M., Hadfield S.G., Murray D.W., Price A.J., Field R.E. Long-term trends in the Oxford knee score following total knee replacement. Bone Joint Lett. J. 2013;95-B(1):45–51. doi: 10.1302/0301-620X.95B1.28573. [cited Jan] [DOI] [PubMed] [Google Scholar]
- 22.Cochrane Cochrane. In: Handbook for sysetmatic reviews. Higgins J., Green S., editors. 2011. [Google Scholar]
- 23.Ali A., Lindstrand A., Nilsdotter A., Sundberg M. Similar patient-reported outcomes and performance after total knee arthroplasty with or without patellar resurfacing. Acta Orthop. 2016;87(3):274–279. doi: 10.3109/17453674.2016.1170548. [cited Jun] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ali A., Lindstrand A., Sundberg M., Flivik G. Preoperative anxiety and depression correlate with dissatisfaction after total knee arthroplasty: a prospective longitudinal cohort study of 186 patients, with 4-year follow-up. J. Arthroplasty. 2017;32(3):767–770. doi: 10.1016/j.arth.2016.08.033. [cited Mar] [DOI] [PubMed] [Google Scholar]
- 25.Aunan E., Rohrl S.M. No detrimental effect of ligament balancing on functional outcome after total knee arthroplasty: a prospective cohort study on 129 mechanically aligned knees with 3 years' follow-up. Acta Orthop. 2018:1–7. doi: 10.1080/17453674.2018.1485283. [cited Jun 08] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baker P.N., van der Meulen J.H., Lewsey J., Gregg P.J. National Joint Registry for E, Wales. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J. Bone Jt. Surg. Br. 2007;89(7):893–900. doi: 10.1302/0301-620X.89B7.19091. [cited Jul] [DOI] [PubMed] [Google Scholar]
- 27.Blyth M.J., Smith J.R., Anthony I.C., Strict N.E., Rowe P.J., Jones B.G. Electromagnetic navigation in total knee arthroplasty-a single center, randomized, single-blind study comparing the results with conventional techniques. J. Arthroplasty. 2015;30(2):199–205. doi: 10.1016/j.arth.2014.09.008. [cited Feb] [DOI] [PubMed] [Google Scholar]
- 28.Boese C.K., Gallo T.J., Plantikow C.J. Range of motion and patient satisfaction with traditional and high-flexion rotating-platform knees. Iowa Orthop. J. 2011;31:73–77. https://www.ncbi.nlm.nih.gov/pubmed/22096424 Available from: [PMC free article] [PubMed] [Google Scholar]
- 29.Collados-Maestre I., Lizaur-Utrilla A., Gonzalez-Navarro B., Miralles-Munoz F., Marco-Gomez L., Lopez-Prats F., et al. 2017. Better Functional Outcome after Single-Radius TKA Compared with Multi-Radius TKA. [Article] [DOI] [PubMed] [Google Scholar]
- 30.Collins J.E., Donnell-Fink L.A., Yang H.Y., Usiskin I.M., Lape E.C., Wright J., et al. Effect of obesity on pain and functional recovery following total knee arthroplasty. J. Bone Jt. Surg. Am. 2017;99(21):1812–1818. doi: 10.2106/JBJS.17.00022. [cited Nov 01] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Culliton S., Bryant D., MacDonald S., Hibbert K., Chesworth B. 2018. Effect of an E-Learning Tool on Expectations and Satisfaction Following Total Knee Arthroplasty: a Randomized Controlled Trial. [Article In Press] [DOI] [PubMed] [Google Scholar]
- 32.Dailiana Z.H., Papakostidou I., Varitimidis S., Liaropoulos L., Zintzaras E., Karachalios T., et al. Patient-reported quality of life after primary major joint arthroplasty: a prospective comparison of hip and knee arthroplasty. BMC Muscoskel. Disord. 2015;16:366. doi: 10.1186/s12891-015-0814-9. [cited Nov 26] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Escobar A., Garcia Perez L., Herrera-Espineira C., Aizpuru F., Sarasqueta C., Gonzalez Saenz de Tejada M., et al. Total knee replacement; minimal clinically important differences and responders. Osteoarthritis Cartilage. 2013;21(12):2006–2012. doi: 10.1016/j.joca.2013.09.009. [cited Dec] [DOI] [PubMed] [Google Scholar]
- 34.Gaillard R., Gaillard T., Denjean S., Lustig S. No influence of obesity on survival of cementless, posterior-stabilised, rotating-platform implants. Arch. Orthop. Trauma Surg. 2017;137(12):1743–1750. doi: 10.1007/s00402-017-2801-0. [cited Dec] [DOI] [PubMed] [Google Scholar]
- 35.Gandhi R., de Beer J., Petruccelli D., Winemaker M. Does patient perception of alignment affect total knee arthroplasty outcome? Can. J. Surg. 2007;50(3):181–186. https://www.ncbi.nlm.nih.gov/pubmed/17568489 [cited Jun]; Available from: [PMC free article] [PubMed] [Google Scholar]
- 36.Genet F., Schnitzler A., Lapeyre E., Roche N., Autret K., Fermanian C., et al. Change of impairment, disability and patient satisfaction after total knee arthroplasty in secondary care practice. Ann. Readapt. Med. Phys. 2008;51(8):671–676. doi: 10.1016/j.annrmp.2008.08.002. 676-82. [cited Nov] [DOI] [PubMed] [Google Scholar]
- 37.Gildone A., Manfredini M., Biscione R., Faccini R. Patella resurfacing in posterior stabilised total knee arthroplasty: a follow-up study in 56 patients. Acta Orthop. Belg. 2005;71(4):445–451. https://www.ncbi.nlm.nih.gov/pubmed/16185000 [cited Aug]; Available from: [PubMed] [Google Scholar]
- 38.Giurea A., Fraberger G., Kolbitsch P., Lass R., Schneider E., Kubista B., et al. The impact of personality traits on the outcome of total knee arthroplasty. BioMed Res. Int. 2016;2016:5282160. doi: 10.1155/2016/5282160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hinarejos P., Puig-Verdie L., Leal J., Pelfort X., Torres-Claramunt R., Sanchez-Soler J., et al. No differences in functional results and quality of life after single-radius or multiradius TKA. Knee Surg. Sports Traumatol. Arthrosc. 2016;24(8):2634–2640. doi: 10.1007/s00167-015-3894-z. [cited Aug] [DOI] [PubMed] [Google Scholar]
- 40.Kawakami Y., Matsumoto T., Takayama K., Ishida K., Nakano N., Matsushita T., et al. Intermediate-Term comparison of posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty using the new knee scoring system. Orthopedics. 2015;38(12):e1127–e1132. doi: 10.3928/01477447-20151123-03. [cited Dec] [DOI] [PubMed] [Google Scholar]
- 41.Khuangsirikul S., Lekkreusuwan K., Chotanaphuti T. 10-Year patient satisfaction compared between computer-assisted navigation and conventional techniques in minimally invasive surgery total knee arthroplasty. Comput. Assist. Surg. 2016;21(1):172–175. doi: 10.1080/24699322.2016.1249959. [cited Dec] [DOI] [PubMed] [Google Scholar]
- 42.Kim T.K., Cho H.J., Kang Y.G., Kim S.J., Chang C.B. Improved early clinical outcomes of RP/PS mobile-bearing total knee arthroplasties. Clin. Orthop. Relat. Res. 2009;467(11):2901–2910. doi: 10.1007/s11999-009-0787-9. [cited Nov] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li B., Bai L., Fu Y., Wang G., He M., Wang J. Comparison of clinical outcomes between patellar resurfacing and nonresurfacing in total knee arthroplasty: retrospective study of 130 cases. J. Int. Med. Res. 2012;40(5):1794–1803. doi: 10.1177/030006051204000517. [DOI] [PubMed] [Google Scholar]
- 44.Liebs T.R., Herzberg W., Ruther W., Haasters J., Russlies M., Hassenpflug J. Ergometer cycling after hip or knee replacement surgery: a randomized controlled trial. J. Bone Jt. Surg. Am. 2010;92(4):814–822. doi: 10.2106/JBJS.H.01359. [cited Apr] [DOI] [PubMed] [Google Scholar]
- 45.Liebs T.R., Herzberg W., Ruther W., Haasters J., Russlies M., Hassenpflug J., et al. Multicenter randomized controlled trial comparing early versus late aquatic therapy after total hip or knee arthroplasty. Arch. Phys. Med. Rehabil. 2012;93(2):192–199. doi: 10.1016/j.apmr.2011.09.011. [cited Feb] [DOI] [PubMed] [Google Scholar]
- 46.Lizaur-Utrilla A., Martinez-Mendez D., Miralles-Munoz F.A., Marco-Gomez L., Lopez-Prats F.A. Negative impact of waiting time for primary total knee arthroplasty on satisfaction and patient-reported outcome. Int. Orthop. 2016;40(11):2303–2307. doi: 10.1007/s00264-016-3209-0. [cited Nov] [DOI] [PubMed] [Google Scholar]
- 47.Mannion A.F., Kampfen S., Munzinger U., Kramers-de Quervain I. The role of patient expectations in predicting outcome after total knee arthroplasty. Arthritis Res. Ther. 2009;11(5):R139. doi: 10.1186/ar2811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Matthews D.J., Hossain F.S., Patel S., Haddad F.S. A cohort study predicts better functional outcomes and equivalent patient satisfaction following UKR compared with TKR. HSS J. 2013;9(1):21–24. doi: 10.1007/s11420-012-9326-4. [cited Feb] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mooney L.T., Smith A., Sloan K., Clark G.W. The effect of the native kinematics of the knee on the outcome following total knee arthroplasty. Bone Joint Lett. J. 2016;98-B(11):1471–1478. doi: 10.1302/0301-620X.98B11.BJJ-2016-0144.R1. [cited Nov] [DOI] [PubMed] [Google Scholar]
- 50.Murphy M., Journeaux S., Hides J., Russell T. Does flexion of the femoral implant in total knee arthroplasty increase knee flexion: a randomised controlled trial. Knee. 2014;21(1):257–263. doi: 10.1016/j.knee.2012.10.028. [cited Jan] [DOI] [PubMed] [Google Scholar]
- 51.Nilsdotter A.K., Toksvig-Larsen S., Roos E.M. A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthritis Cartilage. 2009;17(5):601–606. doi: 10.1016/j.joca.2008.11.007. [cited May] [DOI] [PubMed] [Google Scholar]
- 52.Pulavarti R.S., Raut V.V., McLauchlan G.J. Patella denervation in primary total knee arthroplasty - a randomized controlled trial with 2 years of follow-up. J. Arthroplasty. 2014;29(5):977–981. doi: 10.1016/j.arth.2013.10.017. [cited May] [DOI] [PubMed] [Google Scholar]
- 53.Ranawat C.S., White P.B., West S., Ranawat A.S. Clinical and radiographic results of attune and PFC sigma knee designs at 2-year follow-up: a prospective matched-pair analysis. J. Arthroplasty. 2017;32(2):431–436. doi: 10.1016/j.arth.2016.07.021. [cited Feb] [DOI] [PubMed] [Google Scholar]
- 54.Robertsson O., Dunbar M., Pehrsson T., Knutson K., Lidgren L. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop. Scand. 2000;71(3):262–267. doi: 10.1080/000164700317411852. [cited Jun] [DOI] [PubMed] [Google Scholar]
- 55.Stickles B., Phillips L., Brox W.T., Owens B., Lanzer W.L. Defining the relationship between obesity and total joint arthroplasty. Obes. Res. 2001;9(3):219–223. doi: 10.1038/oby.2001.24. [cited Mar] [DOI] [PubMed] [Google Scholar]
- 56.Sun Y.Q., Yang B., Tong S.L., Sun J., Zhu Y.C. Patelloplasty versus traditional total knee arthroplasty for osteoarthritis. Orthopedics. 2012;35(3):e343–e348. doi: 10.3928/01477447-20120222-14. [cited Mar 7] [DOI] [PubMed] [Google Scholar]
- 57.Von Keudell A., Sodha S., Collins J., Minas T., Fitz W., Gomoll A.H. Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee. 2014;21(1):180–184. doi: 10.1016/j.knee.2013.08.004. [cited Jan] [DOI] [PubMed] [Google Scholar]
- 58.Walker T., Zahn N., Bruckner T., Streit M.R., Mohr G., Aldinger P.R., et al. Mid-term results of lateral unicondylar mobile bearing knee arthroplasty: a multicentre study of 363 cases. Bone Jt. J. [Multicenter Study] 2018;100-B(1):42–49. doi: 10.1302/0301-620X.100B1.BJJ-2017-0600.R1. [cited Jan] [DOI] [PubMed] [Google Scholar]
- 59.Warner S.C., Richardson H., Jenkins W., Kurien T., Doherty M., Valdes A.M. Neuropathic pain-like symptoms and pre-surgery radiographic severity contribute to patient satisfaction 4.8 years post-total joint replacement. World J. Orthoped. 2017;8(10):761–769. doi: 10.5312/wjo.v8.i10.761. [cited Oct 18] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Williams D.P., O'Brien S., Doran E., Price A.J., Beard D.J., Murray D.W., et al. Early postoperative predictors of satisfaction following total knee arthroplasty. Knee. 2013;20(6):442–446. doi: 10.1016/j.knee.2013.05.011. [cited Dec] [DOI] [PubMed] [Google Scholar]
- 61.Lange J.K., Lee Y.Y., Spiro S.K., Haas S.B. Satisfaction rates and quality of life changes following total knee arthroplasty in age-differentiated cohorts. J. Arthroplasty. 2018;33(5):1373–1378. doi: 10.1016/j.arth.2017.12.031. [cited May] [DOI] [PubMed] [Google Scholar]
- 62.Chinnappa J., Chen D.B., Harris I.A., MacDessi S.J. Predictors and functional implications of change in leg length After total knee arthroplasty. J. Arthroplasty. 2017;32(9):2725–2729. doi: 10.1016/j.arth.2017.04.007. e1. [cited 09] [DOI] [PubMed] [Google Scholar]
- 63.Nilsdotter A.K., Toksvig-Larsen S., Roos E.M. Knee arthroplasty: are patients' expectations fulfilled? A prospective study of pain and function in 102 patients with 5-year follow-up. Acta Orthop. 2009;80(1):55–61. doi: 10.1080/17453670902805007. [cited Feb] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tubach F., Ravaud P., Beaton D., Boers M., Bombardier C., Felson D.T., et al. Minimal clinically important improvement and patient acceptable symptom state for subjective outcome measures in rheumatic disorders. J. Rheumatol. 2007;34(5):1188–1193. https://www.ncbi.nlm.nih.gov/pubmed/17477485 [cited May]; Available from: [PMC free article] [PubMed] [Google Scholar]
- 65.Aichroth P., Freeman M.A.R., Smillie I.S., Souter W.A. A knee function assessment chart. From the British Orthopaedic Association Research Sub-Committee. J. Bone Jt. Surg. Br. Vol. 1978;60-b(3):308–309. doi: 10.1302/0301-620X.60B3.681404. [DOI] [PubMed] [Google Scholar]
- 66.Katz J.N., Phillips C.B., Poss R., Harrast J.J., Fossel A.H., Liang M.H., et al. The validity and reliability of a total hip arthroplasty outcome evaluation questionnaire. J. Bone Jt. Surg. Am. 1995;77(10):1528–1534. doi: 10.2106/00004623-199510000-00007. https://www.ncbi.nlm.nih.gov/pubmed/7593061 [cited Oct]; Available from: [DOI] [PubMed] [Google Scholar]
- 67.Mahomed N., Sledge C., Daltroy L., Fossel A., K J. Self-administered patient satisfaction scale for joint replacement arthroplasty. J. Bone Jt. Surg. Br. 1998;80(Suppl 1:9) [Google Scholar]
- 68.Noble P.C., Scuderi G.R., Brekke A.C., Sikorskii A., Benjamin J.B., Lonner J.H., et al. Development of a new Knee Society scoring system. Clin. Orthop. Relat. Res. 2012;470(1):20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sitzia J., Wood N. Patient satisfaction: a review of issues and concepts. Soc. Sci. Med. 1997;45(12):1829–1843. doi: 10.1016/s0277-9536(97)00128-7. https://www.ncbi.nlm.nih.gov/pubmed/9447632 [cited Dec]; Available from: [DOI] [PubMed] [Google Scholar]
- 70.Tubach F., Giraudeau B., Ravaud P. The variability in minimal clinically important difference and patient acceptable symptom state values did not have an impact on treatment effect estimates. J. Clin. Epidemiol. 2009;62:725–728. doi: 10.1016/j.jclinepi.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 71.Behrend H., Giesinger K., Giesinger J.M., Kuster M.S. The "forgotten joint" as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J. Arthroplasty. 2012;27(3):430–436 e1. doi: 10.1016/j.arth.2011.06.035. [cited Mar] [DOI] [PubMed] [Google Scholar]
- 72.Noble P.C., Conditt M.A., Cook K.F., Mathis K.B. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin. Orthop. Relat. Res. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [cited Nov] [DOI] [PubMed] [Google Scholar]
- 73.Newsome P.R., Wright G.H. A review of patient satisfaction: 1. Concepts of satisfaction. Br. Dent. J. 1999;186(4 Spec No):161–165. doi: 10.1038/sj.bdj.4800052. https://www.ncbi.nlm.nih.gov/pubmed/10205951 [cited Feb 27]; Available from: [DOI] [PubMed] [Google Scholar]
- 74.Robinson P.G., Rankin C.S., Lavery J., Anthony I., Blyth M., Jones B. The validity and reliability of the modified forgotten joint score. J. Orthop. 2018;15(2):480–485. doi: 10.1016/j.jor.2018.03.029. [cited Jun] [DOI] [PMC free article] [PubMed] [Google Scholar]