Abstract
Currently, one of the most pressing public health challenges is encouraging people to get vaccinated against COVID-19. Due to limited supplies, some people have had to wait for the COVID-19 vaccine. Consumer research has suggested that people who are overlooked in initial distribution of desired goods may no longer be interested. Here, we therefore examined people’s preferences for proposed vaccine allocation strategies, as well as their anticipated responses to being overlooked. After health-care workers, most participants preferred prioritizing vaccines for high-risk individuals living in group-settings (49%) or with families (29%). We also found evidence of reluctance if passed over. After random assignment to vaccine allocation strategies that would initially overlook them, 37% of participants indicated that they would refuse the vaccine. The refusal rate rose to 42% when the vaccine allocation strategy prioritized people in areas with more COVID-19 — policies that were implemented in many areas. Even among participants who did not self-identify as vaccine hesitant, 22% said they would not want to vaccine in that case. Logistic regressions confirmed that vaccine refusal would be largest if vaccine allocation strategies targeted people who live in areas with more COVID-19 infections. In sum, once people are overlooked by vaccine allocation, they may no longer want to get vaccinated, even if they were not originally vaccine hesitant. Vaccine allocation strategies that prioritize high-infection areas and high-risk individuals in group-settings may enhance these concerns.
Keywords: COVID-19, vaccine allocation, vaccine hesitancy
Introduction
Vaccines are central to public-health strategies aiming to mitigate the SARS-CoV-2 (COVID-19) pandemic, with vaccines now being rolled out in different countries. Due to supply constraints, initial vaccine allocation in the United States (US) first targeted health-care workers, with experts disagreeing about who to vaccinate next (Gayle et al. 2020; Kocher & Goldman 2020). US residents also disagreed about who to vaccinate after prioritizing vaccines for health-care workers (Gollust et al. 2020). While COVID-19 vaccines are now more widely available in the US, some people initially had to wait. In countries where supplies are still limited, many people are still waiting.
There is a potential concern that being overlooked by initial vaccine allocation strategies may unintentionally contribute to vaccine hesitancy. According to classic studies in consumer research, being overlooked during a limited sale of a desired product can cause disinterest in the product (Biraglia et al. 2021; Farrell 1983; Hirschman 1970; Rusbult et al. 1982). As a result, after being denied initial vaccinations, people may refuse the COVID-19 vaccine. In national sample recruited in the United States, we therefore examined people’s preferences for vaccine allocation strategies, and effects of specific (vs. undefined) vaccine allocation strategies on whether or not they would refuse the vaccine.
Methods
Sample
Participants were 5,968 of 7,699 (77%) invited members of the Understanding America Study (UAS), a nationally representative online panel of US residents. UAS members were recruited from randomly selected US addresses, oversampling underrepresented populations. To avoid traditional biases of online panels, interested individuals received internet access and tablets if needed (Alattar et al. 2018). Surveys were offered in English and Spanish. All analyses used statistical weights to ensure representativeness regarding age, gender, race/ethnicity, and location (https://uasdata.usc.edu/page/Weights). Respondents’ demographics were comparable to the US population and to non-responders, except that responders were slightly less likely than non-responders to be older than 65 (16% vs. 20%; Table 1).
Table 1.
Demographic characteristics of 2018 US population, responders and nonresponders.
| Demographic characteristic | 2018 US population | Responders (N=5968) | Nonresponders (N=1801) | Test of difference between responders and nonresponders |
|---|---|---|---|---|
|
| ||||
| At risk age group 65+ | 17% | 21% | 86% | χ2(1)=2586.00, p<0.001 |
| Male | 49% | 48% | 48% | χ2(1)=0.00, p=0.96 |
| College degree | 32% | 47% | 44% | χ2(1)=4.42, p=0.15 |
| African-American | 13% | 12% | 13% | χ2(1)=2.37, p=0.32 |
| Hispanic-Latinx | 18% | 16% | 18% | χ2(1)=4.41, p=0.44 |
| Other minority | 9% | 6% | 5% | χ2(1)=2.43, p=0.29 |
| White | 60% | 66% | 64% | χ2(1)=1.15, p=0.48 |
Note: Statistical weights were used in all analyses.
Procedure
The present study was approved by the University of Southern California’s Institutional Review Board, as part of their ongoing Understanding America Study (UP-14–00148-CR005). The funding source had no role in the study. Participants provided consent and completed an online survey between September 30 and October 28, 2020. The survey and associated data are publicly available from the University of Southern California’s Understanding America Study (https://uasdata.usc.edu; survey 264).
Preferences for vaccine allocation strategies
Participants were asked “when a COVID-19 vaccine becomes available, health-care workers and nursing home workers will likely get it first. If you had to choose, who do you think should be vaccinated next?” Recommended vaccine allocation strategies were taken from the literature (Gayle et al. 2020; Gollust et al. 2020; Kocher & Goldman 2020), and appeared in random order:
“People at high risk of getting sick or dying from COVID-19 who live in group-housing. For example: people who are older, or have heart disease, diabetes, and other health conditions”;
“People at high risk of getting sick or dying from COVID-19 who live with their families. For example: people who are older, or have heart disease, diabetes, and other health conditions”;
“People who are more likely to spread COVID-19 to others, because of their social behavior or employment. For example: young adults and teachers”;
“People who live in areas with more COVID-19 infections”; and
-
“People who are selected randomly through a lottery.”
Participants indicated their preferred vaccine allocation strategy, and ranked remaining strategies.
Concerns associated with vaccine allocation
Participants rated how concerned they were with the fairness of vaccine allocation strategies, and with reducing the number of infections and deaths of vaccine allocation strategies (1=not at all; 5=very much).
Responses to randomly assigned vaccine allocation strategy.
Participants were randomly assigned to one of the five vaccine allocation strategies above, excluding vaccine allocation strategies that targeted groups of which participants indicated being a member. Hence, in each case, participants would initially have to wait to get vaccinated. In an additional control condition, participants also had to wait to get vaccinated, but the vaccine allocation strategy was unspecified. Subsequently, participants were asked “If this were to happen, what would you do?” They answered yes or no to “I would get the vaccine once it became available to me” (Farrell 1983; Hirschman 1970; Rusbult et al. 1982).
Control variables
Control variables reflect questions that already appeared on the Understanding America Study and were not specifically designed for this study (https://uasdata.usc.edu). As in previous research (Szilagyi et al. 2021), participants were determined vaccine hesitant (vs. not), if they answered ‘very unlikely or ‘somewhat unlikely’ (vs. ‘unsure,’ ‘somewhat likely,’ ‘very likely’) to “How likely are you to get vaccinated for coronavirus once a vaccine is available to the public?”
Statistical analysis
To examine preferences for vaccine allocation strategies, we computed the percent of participants who indicated preferring it and mean rank-order preference (Table 2). To examine participants’ responses to the randomly assigned vaccine allocation strategy that would initially overlook them, we conducted two sets of logistic regressions. The first set predicted reported vaccine refusal to each vaccine allocation strategy (vs. control condition with unspecified vaccine allocation strategy), while controlling for vaccine hesitancy and demographics (Table 3). To check for robustness, analyses were repeated for participants who indicated that they were not in any of the groups targeted by vaccine allocation strategies (henceforth: low-risk sample), as well as participants who had indicated that they were vaccine hesitant, and participants who had indicated that they were not vaccine hesitant (Table 3). We also examined interactions between randomly assigned vaccine allocation strategies and participants’ vaccine hesitancy, in the full sample and the low-risk sample (Table S1). Additional analyses of the low-risk, vaccine hesitant, and not vaccine hesitant samples controlled for concerns with fairness, and reducing the number of infections and deaths in relation to vaccine allocation preferences (Table S2).
Table 2:
Preferences for vaccine allocation strategies.
| Vaccine allocation strategy | Percent of participants preferring it | Mean (SD) rank |
|---|---|---|
|
| ||
| (1) High-risk individuals living in group-housing. | 49% | 1.87 (1.07) |
| (2) High-risk individuals living with their families. | 29% | 2.14 (1.02) |
| (3) People who are more likely to spread COVID-19 to others. | 11% | 3.14 (1.09) |
| (4) People who live in areas with more COVID-19 infections. | 10% | 3.14 (1.03) |
| (5) People who are selected randomly through a lottery. | 1% | 4.68 (0.81) |
Note: Vaccine allocation strategies were presented to participants in random order. Rank 1=most preferred, 5=least preferred. Statistical weights were used in all analyses.
Table 3.
Odds ratios (95% confidence intervals) in logistic regressions predicting vaccine refusal.
| Vaccine refusal | ||||
|---|---|---|---|---|
|
|
||||
| Full sample N=5,968 | Low-risk sample N=2,627 | Vaccine hesitant N=1,775 | Not vaccine hesitant N=4,193 | |
|
| ||||
| Vaccine allocation strategy | ||||
| (1) High-risk individuals living in group-housing | 1.41* (1.04, 1.91) | 1.48 (0.90, 2.44) | 2.18** (1.25, 3.80) | 1.15 (0.77, 1.71) |
| (2) High-risk individuals living with their families | 1.45* (1.03, 2.05) | 1.34 (0.81, 2.24) | 1.28 (0.74, 2.21) | 1.44 (0.95, 2.18) |
| (3) People who are more likely to spread COVID-19 to others. | 1.06 (0.76, 1.48) | 1.45 (0.86, 2.45) | 1.14 (0.68, 1.91) | 0.95 (0.61, 1.49) |
| (4) People who live in areas with more COVID-19 infections | 1.63** (1.17, 2.26) | 1.78* (1.08, 2.95) | 1.56 (0.88, 2.77) | 1.57* (1.06, 2.33) |
| (5) People who are selected randomly through a lottery | 1.22*** (0.90, 1.65) | 1.45 (0.90, 2.36) | 1.21 (0.76, 1.95) | 1.18 (0.81, 1.70) |
| (6) Allocation strategy unspecified (control-group) | (omitted) | (omitted) | (omitted) | (omitted) |
|
| ||||
| Control variables | ||||
| Vaccine hesitancy | 17.68*** (14.46, 21.61) | 25.50*** (18.54, 35.06) | - | - |
| Public spaces or crowds’ avoidance | - | - | - | - |
| Over 65 years old (vs. not) | 0.41*** (0.32, 0.52) | 0.38*** (0.26, 0.55) | 0.31*** (0.21, 0.45) | 0.48*** (0.35, 0.66) |
| Male (vs. female) | 0.69** (0.57, 0.84) | 0.84 (0.64, 1.12) | 0.72 (0.52, 1.00) | 0.67** (0.53, 0.85) |
| College degree (vs. not) | 0.57** (0.48, 0.69) | 0.47*** (0.35, 0.62) | 0.83 (0.60, 1.14) | 0.47*** (0.37, 0.60) |
| Non-Hispanic African-American (vs. white) | 1.39* (1.00, 1.92) | 1.38 (0.80, 2.38) | 0.67 (0.42, 1.07) | 1.98*** (1.38, 2.85) |
| Hispanic/Latinx (vs. white) | 0.92 (0.67, 1.27) | 1.14 (0.71, 1.82) | 0.50** (0.32, 0.80) | 1.29 (0.89, 1.88) |
| Other minority (vs. white) | 0.63 (0.39, 1.03) | 0.56 (0.27, 1.17) | 0.23*** (0.11, 0.49) | 1.04 (0.64, 1.69) |
Note:
p<0.001
p<0.01
p<0.05. Statistical weights were used in all analyses. Low-risk sample includes participants who do not identify as a member of the first four vaccine allocation strategies in Table 2
Results
Vaccine allocation preferences
Table 2 shows that, after health-care workers, most participants wanted vaccine allocation to prioritize high-risk individuals living in group-housing (49%) or with their families (29%). In order, vaccine allocation strategies were less preferred if they prioritized individuals who are more likely to spread COVID-19 (11%), who live in areas with more COVID-19 infections (10%), and who are randomly selected through a lottery (1%). Mean ranks also suggest this preference order (Table 2). Reasons for choosing vaccine allocation strategies included, in order, concerns about reducing deaths (M=4.13; SD=1.14), reducing infections (M=3.77; SD=1.22), and fairness (M=3.65; SD=1.37).
Responses to randomly assigned vaccine allocation strategy
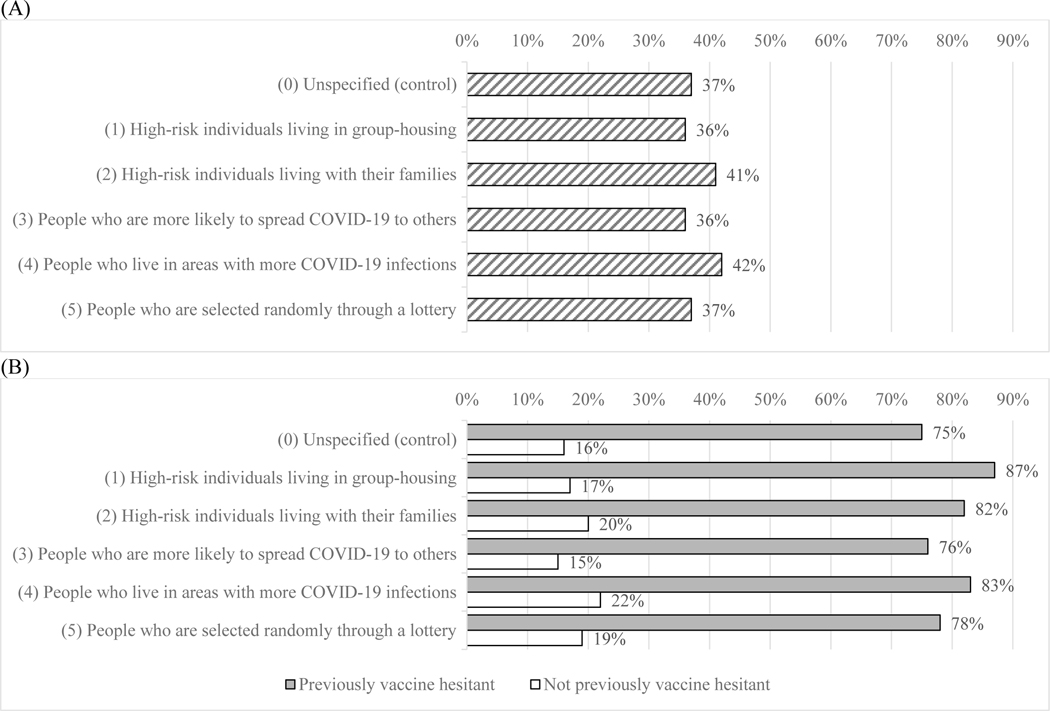
After random assignment to vaccine allocation strategies that would initially require participants to wait to get vaccinated, reported vaccine refusal was highest (42%) among participants who were overlooked due to prioritization of other people in areas with more COVID-19 (Figure 1A). By comparison, 37% of participants indicated that they would refuse the vaccine in the control group, which considered being overlooked by a vaccine allocation strategy targeting unspecified “others” (Figure 1). Logistic regressions suggested that this pattern held in the full sample and in the low-risk sample, even after controlling for previously reported vaccine hesitancy and demographics (Table 3). Interestingly, it also held among participants who had previously indicated that they were not actually vaccine hesitant, while controlling for demographics (Table 3). Of participants who had previously indicated that they were not vaccine hesitant, 22% indicated wanting to refuse the vaccine if others in high-risk areas were vaccinated first (vs. 16% if it want to unspecified others in the control group.)
Figure 1.
Participants’ reports of vaccine refusal after being randomly assigned to one of vaccine allocation strategies that would pass them over, in (A) overall sample and (B) overall sample by previously reported vaccine hesitancy. Note: Statistical weights were used in all analyses.
Overall, 30% of participants had already indicated that they were hesitant to take the vaccine. Those vaccine hesitant participants reported much greater inclinations to refuse vaccines after being overlooked by vaccine allocation strategies as compared participants who had indicated that they were not vaccine hesitant (Figure 1B). Moreover, participants who had previously indicated that they were vaccine hesitant wanted to refuse the vaccine in the condition that prioritized high-risk individuals in group-housing rather than the control condition that prioritized unspecified “others” (87% vs. 75%). That distinction did not affect participants who had indicated that they were not vaccine hesitant (17% vs. 16%; Figure 1B). This significant interaction is also confirmed in logistic regressions (Table S1; Table 3). Yet, 15%−22% of participants who had previously indicated that they were not vaccine hesitant reported that they would no longer want the vaccine if they were overlooked in the initial vaccine allocation (Figure 1B).
Generally, the reported findings in each sample (Table 3) held after controlling for participants’ concerns with fairness, and with reducing the number of infections and deaths (Table S2). Thus, these concerns did not statistically explain their vaccine allocation preferences.
Discussion
Supplies of COVID-19 vaccines were limited when they were first allocated in the United States, and are still limited in many other countries. Various experts have suggested that initial vaccine allocation should have prioritized health-care workers, at-risk populations, or those most likely to infect others (Gayle et al., 2020; Kocher & Goldman, 2020). US residents largely agreed on prioritizing vaccination of health-care workers, but disagreed who to vaccinate next (Gollust et al., 2020).
When people are overlooked in the initial allocation of desired products, the consumer research literature suggests that they may lose interest (Farrell, 1983; Hirschman, 1970; Rusbult et al., 1982). Here, we find that people may respond negatively to being overlooked by vaccine allocation, by refusing the vaccine, even if they had not previously considered themselves vaccine hesitant. That response may partially reflect the negative consequences highlighted in the consumer research literature, as well as a perception that vaccination may no longer be needed if others get vaccinated. Nevertheless, we found that vaccine refusal is somewhat sensitive to the specific vaccine allocation strategy by which people might be overlooked.
Most participants preferred that, after health care workers, vaccines go to high-risk individuals in group-settings and living with their families. Reported vaccine refusal was greatest when participants were passed over by vaccine allocation strategies that prioritized people in high-infection areas – even among those who had previously indicated that they were not vaccine hesitant. Participants who were vaccine hesitant (vs. not) were more likely to report vaccine refusal if they were passed over by vaccine allocation strategies that prioritized high-risk individuals living with their families.
Limitations
Like any study, ours had potential limitations. Since vaccines were not yet available at the time of this survey, all questions were hypothetical in nature. Furthermore, we were unable to identify why participants responded differently to vaccine allocation strategies, and whether reasons for vaccine hesitancy varied between different groups of participants. Concerns about fairness and concerns about effectiveness did not appear to statistically explain responses to vaccine allocation strategies. Thus, other unmeasured concerns may have contributed to differences in vaccine hesitancy in response to presented vaccine allocation strategies.
Conclusion
Some experts have recommended vaccine allocation strategies that prioritize individuals living in high-infection areas and high-risk individuals living in group-settings -- after health-care workers (Gayle et al., 2020). In line with previous suggestions that COVID-19 risk reduction strategies can have unintended negative consequences (Balog-Way & McComas 2020; Collins, Florin, & Renn 2020), our findings suggest that restricted vaccine allocation may unintentionally increase disease transmission due to subsequent vaccine refusal. Implementation of vaccine allocation strategies should therefore consider people’s responses, be transparent, and manage their expectations.
Supplementary Material
Acknowledgements
The project described in this paper relies on data from survey(s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research (CESR) at the University of Southern California. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of USC or UAS. The collection of the UAS COVID-19 survey data was supported in part by the Bill & Melinda Gates Foundation and by grants U01AG054580 and P30AG024968 (Roybal Center for Behaviorial Interventions in Aging) from the National Institute on Aging. Additional funding for the collection of the presented survey data was provided by the Schaeffer Center for Health Policy and Economics and the University of Leeds. Wändi Bruine de Bruin was supported by the National Science Foundation (#2028683) and the Swedish Riksbankens Jubileumsfond Program on Science and Proven Experience ‘Science and Proven Experience’ The funding agreements ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Marco Angrisani, Daniel Bennett, Jill Darling, Tania Gutsche, and Arie Kapteyn are gratefully acknowledged for their help with this study.
Funding
The project described in this paper relies on data from survey(s) administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research (CESR) at the University of Southern California. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of USC or UAS. The collection of the UAS COVID-19 survey data was supported in part by the Bill & Melinda Gates Foundation and by grants U01AG054580 and P30AG024968 (Roybal Center for Behavioral Interventions in Aging) from the National Institute on Aging. Additional funding for the collection of the presented survey data was provided by the Schaeffer Center for Health Policy and Economics and the University of Leeds. Wändi Bruine de Bruin was supported by the National Science Foundation (#2028683) and the Swedish Riksbankens Jubileumsfond Program on Science and Proven Experience ‘Science and Proven Experience’ The funding agreements ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Footnotes
Geolocation
Survey data were collected in the United States, through the University of Southern California’s Understanding America Study ((https://uasdata.usc.edu)
Financial disclosure
Wändi Bruine de Bruin reports consulting income from the UK’s Behavioural Insights Team and Save The Children. Aulona Ulqinaku has no financial disclosures. In the past three years, Dr. Goldman has received research support, speaker fees, travel assistance, or consulting income from the following sources: ACADIA Pharmaceuticals, Amgen, The Aspen Institute, Biogen, Blue Cross Blue Shield of Arizona, BMS, Cedars Sinai Health System, Celgene, Edwards Lifesciences, Gates Ventures, Genentech, Gilead Sciences, GRAIL, Johnson & Johnson, Kaiser Family Foundation, National Institutes of Health, Novartis, Pfizer, Precision Health Economics, Roche, and Walgreens Boots Alliance.
Data availability
The survey and data are publicly available from the University of Southern California’s Understanding America Study (https://uasdata.usc.edu; survey 264).
References
- Alattar L, Messel M, Rogofsky C. 2018. An introduction to the Understanding American Study internet panel. Social Security Bulletin. 78, 13–28. https://heinonline.org/HOL/Page?handle=hein.journals/ssbul78&div=11 [Google Scholar]
- Balog-Way DHP, & McComas K, (2020). COVID-19: Reflections on trust, trade-offs and preparedness. Journal of Risk Research, 23, 838–848. 10.1080/13669877.2020.1758192 [DOI] [Google Scholar]
- Biraglia A, Usrey B, & Ulqinaku A. (2021). The downside of scarcity: Scarcity appeals can trigger consumer anger and brand switching intentions. Psychology & Marketing. 10.1002/mar.21489 [DOI] [Google Scholar]
- Collins A, Florin MV, & Renn O. (2020). COVID-19 risk governance: Drivers, responses, and lessons to be learned. Journal of Risk Research, 23, 1073–1082. [Google Scholar]
- Farrell D. (2020). Exit, voice, loyalty, and neglect as responses to job dissatisfaction: A multidimensional scaling study. Acad Manage J 1983; 26(4): 596–607. 10.5465/255909 [DOI] [Google Scholar]
- Hirschman AO (1970). Exit, voice, and loyalty: Responses to decline in firms, organizations, and states (Vol. 25). Harvard university press. 10.1093/oxfordhb/9780199646135.013.30 [DOI] [Google Scholar]
- Gayle H, Foege W, Brown L, Kahn B Framework for equitable allocation of COVID-19 vaccine. The National Academy Press, Washington, DC, 10, 25917; 2020. https://www.nap.edu/read/25917 [PubMed] [Google Scholar]
- Gollust SE, Saloner B, Hest R, & Blewett LA. (2020). US Adults’ Preferences for Public Allocation of a Vaccine for Coronavirus Disease 2019. JAMA Network Open 3(9), e2023020-e2023020. 10.1001/jamanetworkopen.2020.23020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khubchandani J, Sarma S, Price JH, Wiblishauser MJ, Sharma M, & Webb FJ (2021). COVID-19 hesitancy in the United States: A rapid national assessment. Journal of Risk Research, 46, 270–277. 10.1007/s10900-020-00958-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusbult CE, Zembrodt IM, Gunn LK. (1982). Exit, voice, loyalty, and neglect: Responses to dissatisfaction in romantic involvements. Journal of Personlity and Social Psychology. 43(6), 1230–1242. 10.1037/0022-3514.43.6.1230 [DOI] [Google Scholar]
- Szilagyi PG, Thomas K, Shah MD, Vizuetha N, Cui Y, Vangala S, & Kapteyn A. (2021). National trends in the US public’s likelihood of getting a COVID-19 vaccine – April 1 to December 8, 2020. Journal of the American Medical Association, 325, 396–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.