Abstract
Following a traumatic event, coping strategies may affect the natural course of posttraumatic stress symptoms (PTSS). In particular, cognitive coping strategies (how one thinks about stressors) may reduce PTSS by increasing individuals’ perceived control over events, appraising them as less threatening, particularly for individuals who experience self-blame after trauma. Individuals who experience a traumatic event (n =344) completed assessments at baseline (T1), one month (T2), and two months (T3). We tested whether T1 cognitive coping strategies (positive reinterpretation, acceptance, religious coping) predicted reduced T3 PTSS and whether this reduction was mediated by increased perceived control at T2. We tested whether this effect was particularly strong for individuals experiencing self-blame. Positive reinterpretation predicted decreases in, religious coping predicted increases in, and acceptance had no direct effect on PTSS. Overall, acceptance showed the greatest potential for reducing PTSS through increased perceived control over one’s life. In a fully moderated mediation model, positive reinterpretation significantly interacted and acceptance marginally interacted with self-blame to predict increased perceived control and, subsequently, decreased T3 PTSS. Specifically, acceptance and positive reinterpretation were most helpful for those with higher levels of self-blame. Religious coping interacted with self-blame to predict decreased perceived control and subsequent increased PTSS. For trauma survivors experiencing self-blame, cognitive coping strategies that utilize compassionate self-talk, such as positive reinterpretation and acceptance, may be particularly helpful at increasing perceived control after trauma, while religious coping may have deleterious effects.
Keywords: positive reinterpretation, acceptance, religious coping, trauma, control, PTSD, blame, posttraumatic cognitions
Introduction
Posttraumatic stress symptoms (PTSS) often arise following highly stressful experiences (NCPTSD, 2018). PTSS (e.g., hyperarousal, intrusive memories of the event) may be due to cognitively appraising future stressful events and trauma reminders as dangerous, prompting an ongoing threat response in daily life (Ehlers & Clark, 2000). This increased threat response to event reminders may be due to perceptions that triggering cues pose the same threat as the original trauma. The Meaning-Making Model (Park, 2010) posits that individuals experience PTSS due to dissonance between their global belief systems and appraised meaning of the potentially traumatic event (PTE). That is, if an individual has a global belief that the world is a controllable place yet appraised the circumstances of the PTE as beyond his or her control, this belief violation may cause severe distress until coherence is created between their global beliefs and appraised event meaning (Currier, Holland, & Mallott, 2015). Cognitive coping styles such as reappraisal and acceptance may aid in bringing about such coherence (Park & George, 2013).
Most of the current literature on coping and PTSD focuses on broad dimensions of coping (approach versus avoidance; emotion-focused versus behavior/problem-focused; Allen, Mercer, & Lilly, 2016; Hébert, Daspe, & Cyr, 2018; Roth & Cohen, 1986; Vaughn-Coaxum et al., 2018). While informative, these views of coping lack specificity and typically lack a grounding in trauma theory; more information on types of coping grounded specifically in trauma theory are needed to develop a deeper understanding of how individuals’ responses to trauma influence their subsequent adjustment. We can increase this understanding by identifying the mechanisms that underlie relationships between coping and various aspects of post-trauma adjustment. In this study we focus on cognitive coping, a specific form of coping strongly based in multiple trauma theories.
The Meaning-Making Model posits that individuals can reappraise, make re-attributions regarding the cause, or accept the PTE to bring cohesion between their event appraisals and their global beliefs about the world. Individuals can use these same cognitive strategies to re-evaluate and change their overarching belief systems (Park, 2010; Park & Ai, 2006). Most studies of coping in the context of trauma have focused on maladaptive strategies (e.g., negative cognitive appraisals; Agar et al., 2006; Kleim et al., 2013; Mitchell et al., 2017), but adaptive cognitive strategies may have greater treatment implications. Bussell and Naus (2010) defined cognitive coping as including positive reappraisal, acceptance, and religious coping. Strategies that rely on cognitive processes have been associated with lower levels of posttraumatic stress, primarily in cross-sectional studies (e.g., Boden et al., 2012; Hanley et al., 2017).
Positive reappraisal is a commonly studied aspect of cognitive coping in the context of trauma. An experimental study that had trauma survivors implement cognitive coping strategies such as positive reappraisal and putting the trauma “into perspective” saw a relationship between use of these strategies and reductions in later PTSS (Wisco, Sloan, & Marx, 2013). In a cross-sectional study, cognitive coping was more effective than non-cognitive coping strategies (i.e., emotion-focused coping, disengagement) after trauma for a range of different stressors including trauma reminders, loss reminders, and family conflict (Howell et al., 2015). Acceptance is another cognitive strategy that has demonstrated inverse associations with distress following trauma (Thompson, Arnkoff, & Glass, 2011). Beneficial effects of acceptance-based coping for the reduction of PTSS have been found in a range of populations (Feder et al., 2016; Mong, Noguchi, & Ladner, 2012; Ssenyonga, Owens, & Olema, 2013).
Evidence regarding effects of religious coping on PTSS is less consistent, variously showing positive associations (Park et al., 2017; Witvliet et al., 2004), negative associations (Watlington & Murphy, 2006), and no association (Chan & Rhodes, 2013) with PTSS. This conflicting evidence suggests that the effectiveness of religious coping may depend on type of religious response used (e.g., spiritual doubting vs. positive religious coping) and the race of those using the responses (Ahrens et al., 2010; Feder et al., 2013; Watlington & Murphy, 2006).
While limited research has identified cognitive coping strategies as useful, almost no research has examined how each cognitive coping strategy predicts subsequent changes in PTSS. The little literature that has examined associations of adaptive cognitive coping and PTSS were cross-sectional (Boden et al., 2012; Hanley et al, 2017). The few studies that examined cognitive coping longitudinally have typically considered only isolated components of cognitive coping for PTSS (Bryant-Davis et al., 2014; Wisco, Sloan, & Marx, 2013).
Our first research question, whether each of these cognitive strategies predicts changes in later PTSS, aims to use our longitudinal design and causal inference to build on previous cross-sectional findings that positive reinterpretation and acceptance strategies lead to decreased PTSS. In addition, we aim to add clarity to the discrepancy surrounding the effectiveness of two types of religious responses for reducing PTSS as there is currently mixed evidence (Chan & Rhodes, 2013; Park et al., 2017; Watlington & Murphy, 2006;).
In addition to examining effects of cognitive coping on PTSS longitudinally, we aim to add to the limited evidence regarding the mechanism by which this type of coping exerts salutary effects. One potential mediator may be increased perceived control over events when using cognitive coping; that is, decreased violation of perceived control over one’s life may link cognitive coping and subsequent PTSS. Our second research question, whether the relationship between cognitive coping and later PTSS is due to the mediating changes in the amount of control an individual perceives over one’s life, also builds upon the Meaning-Making Model and Cognitive Theory frameworks.
Cognitive Theory’s assertion that PTSS stems from appraisals of events and stimuli as presenting a current threat (Ehlers & Clark, 2000) suggests that an individual may feel incapable of preventing or responding effectively to trauma stimuli. Lower perceived internal locus of control has been associated with higher levels of PTSS (Dunmore, Clark, & Ehlers, 2001; Frazier, Berman, & Steward, 2001; Smith et al., 2018). For this reason, cognitive coping strategies that boost one’s perceived control may decrease PTSS by allowing individuals to appraise stressful stimuli as less threatening (Ehlers et al., 2005; Resick et al., 2016; Simmen-Janevska et al., 2012). Further, based on the Meaning-Making Model, coping strategies that help individuals decrease a perception their global beliefs of control have been violated may be helpful as this theory posits that cohesion is needed between global beliefs, situational beliefs, and appraisals (Park, 2010; Park & Ai, 2006). Little research has examined whether cognitive coping leads to increased perceived control over one’s life (or decreased perceived control violation) over time.
Each cognitive coping method may be differentially effective in reducing PTSS based on differences in how individuals initially respond to trauma, though this notion has yet to be explored. We hone in on one specific type of response that has been shown to be important in recovery following trauma, self-blame. Much of the research regarding self-blame in PTSS conceptualizes it as a maladaptive coping strategy rather than a distinct appraisal of the trauma that may drive PTSS (Boyraz & Waits, 2018; Britt et al., 2017; Schmied et al., 2015). We take the perspective that self-blame constitutes an ongoing appraisal of one’s role relative to the event or situation rather than a coping response (i.e., coping typically refers to effortful strategies people use to manage stressors while appraisals refer to how people understand their stressor; Aldwin, 2007). Our study explores the coping strategies that may be most helpful for individuals who experience high self-blame.
Our final research question, whether cognitive coping strategies that increase perceived control over one’s life as a means of reducing symptoms of PTSS are particularly helpful for individuals who experience high self-blame, aims to determine whether individuals who experience high levels of self-blame may especially benefit from these control-restoring coping strategies. As self-blame is associated with higher levels of PTSS (Kline et al., 2018; Moscardino et al., 2014; Schmied, 2015), individuals experiencing high self-blame may benefit more from cognitive coping strategies that make them feel greater control over their lives. Self-blame may be related to feeling incapable of controlling something they felt they should have been able to control. This link is evidenced by studies that show perceived control fully mediates the relationship between self-blame and PTSS (Larsen & Fitzgerald, 2011), perceived control over the event may moderate the relationship between self-blame and later general adjustment and distress (Arora, 1999), and adaptive coping mechanisms mediate the relationship between perceived control and self-blame on PTSS (Najdowski & Ullman, 2009).
Cognitive strategies that increase perceived control may function by reducing dissonance between whether the event could be controlled in a general sense and one’s own personal ability to control the event, or by increasing perceived self-efficacy, thereby rendering future stressors as less threatening (Frazier et al., 2011; Jerusalem, & Schwarzer, 1992). Many studies have tested associations between self-blame and coping strategies on PTSS but we could not locate any studies examining the potential for cognitive coping to buffer the effects of self-blame on subsequent PTSS (i.e., moderate its effects).
Survivors with high levels of self-blame may especially benefit from adaptive coping that facilitates gaining a personal sense of control. In this study, we examine how different types of cognitive coping styles may lead to reductions in PTSS and the extent to which these reductions occurred through the mechanism of perceived control violation. We expect that this mechanism is particularly relevant to those higher in self-blame. We pose the following hypotheses:
All three cognitive coping strategies – acceptance, positive reinterpretation, and religious coping– will be negatively associated with PTSS over time.
The relationship between cognitive coping strategies at baseline (T1) and PTSS two months later (T3) will be mediated by perceived control at one month (T2), after controlling for T1 PTSS and T1 perceived control.
This proposed mediation effect will be moderated by self-blame, such that cognitive coping strategies that predict increased perceived control will be more effective at reducing PTSS for individuals higher in self-blame.
Methods
Participants
Data for the present study were drawn from a larger study examining narrative writing as an intervention. All participants previously indicated they had experienced a PTE based on DSM-IV criteria (DSM-IV was used for this study as this version was still the commonly used edition when the larger study was originally designed). Participants were recruited through a university psychology department and received partial course credit for their participation. Participants were assessed at baseline (n=436), one (n=405), and two (n=344) months. Our sample was predominantly women (69%; n=307). The sample was 80.9% White (n=360), 7.2% Asian or Pacific Islander (n=32), 5.4% Black or African American (n=24), 3.1% multi-racial (n=14), 2.9% another race not listed (n=13), and .4% American Indian or Alaska Native (n=2). The majority of the sample was non-Hispanic or Latino (94.5%). The mean reported age was 18.79 years with 47.2% aged 18 years old (n=210) and 34.6% of participants aged 19 years old (n=154). Almost the entire sample (98.2%) was never married (n=435). This was a high-income sample with 59.2% of participants reporting their family income as $70,000 or more per year.
Measures
COPE Inventory.
We used the COPE (Carver, Scheier, & Weintraub, 1989) to measure how individuals manage stressors. We selected three subscales that have previously been defined as “cognitive coping”: acceptance, positive reinterpretation, and religious coping (Bussell & Naus, 2010; Park & George, 2013). Participants answer on a scale of 1 (I don’t usually do this at all) to 4 (I usually do this a lot). The COPE has been shown to have high validity (Carver et al., 1989). Scales in our sample ranged from good to excellent internal consistency reliability (positive reinterpretation: a = 0.77; acceptance: a = 0.77; religious coping: a = 0.94).
RCOPE scale.
For more detailed analysis, we included the RCOPE (Pargament, Koenig, & Perez, 2000) which categorizes religious coping into positive religious coping (i.e., “I sought God’s love and care”) and spiritual struggle (i.e., “I wonder what I did for God to punish me”). Items were rated on a scale of 1 (I don’t usually do this at all) to 4 (I usually do this a lot). The RCOPE has been shown to have acceptable validity across a wide range of samples (Pargament, Feuille, & Burdzy, 2011). Both subscales had excellent internal consistency reliability within our sample (positive religious coping: a = 0.96; spiritual struggle: a = 0.94).
Posttraumatic Cognitions Inventory (PTCI)- self-blame subscale.
The PTCI assesses the content of negative thoughts after a PTE (Foa et al., 1999). The 5-item self-blame subscale was used for this study with questions regarding individuals’ beliefs about their role in the event (e.g., “the event happened because of the way I acted”). Responses range from 0 (totally disagree) to 7 (totally agree). The subscale has shown high reliability (Foa et al., 1999) and had strong internal consistency reliability in our sample (a = 0.84).
Perceived control.
To measure perceived control, we used a single item from the Global Meaning Violations Scale (Park et al., 2016). The item, “How much does this event violate your sense of being in control of your life?” was rated on a scale of 1 (not at all) to 5 (very much). It was reverse-coded such that higher scores indicated greater perceived control (i.e. less violation of perceived control).
Posttraumatic Diagnostic Scale (PDS).
The PDS is a 17-item measure to assess PTSD symptom severity as recognized by DSM-IV criteria (Foa et al., 1997; please see the PDS-5 for the DSM-V version as validated in Foa et al, 2016). It assesses symptoms such as hyperarousal, avoidance of trauma reminders, and negative memories of the trauma. Items are rated on a scale of 0 (not at all/only once) to 3 (5 or more times a week/almost always). Higher scores indicate higher symptom frequency. The scale has shown good sensitivity, specificity, and reliability (Foa et al., 1997). Within our sample, the scale showed strong internal consistency (a = 0.91).
Data Analysis
For preliminary analyses, we computed descriptive statistics on each variable including means, standard deviations, and distributions. We conducted a paired sample t-test to determine change in PTSS over time. We conducted a Pearson’s r correlation coefficient analysis between each cognitive coping scale, PTSS, perceived control, and self-blame for every time point at which each variable was assessed to test variable associations with each other.
We conducted all mediation and moderated mediation analyses in IBM’s SPSS PROCESS macro (Hayes, 2013). Simple mediation analyses followed Hayes’ model 4. Model 4 tests whether the relationship between the independent variable (IV) and dependent variable (DV) is due to a third variable (i.e., mediator). Tests of moderated mediation used Hayes’ model 8 (Hayes, 2013). Model 8 analyses test interaction effects between the IV and the moderator variable on the proposed mediator variable as the outcome as well as conditional effects of the moderator between the IV and DV. For our study, the IVs were measured at T1, the mediator and moderator at T2, and the DV at T3 (See Figure 1 for diagrams). Extended decimal point placements are included when two decimal points do not convey significance effects based on a 95% confidence interval. All indirect effects used bootstrapping analysis with 5000 simulations.
Figure 1.
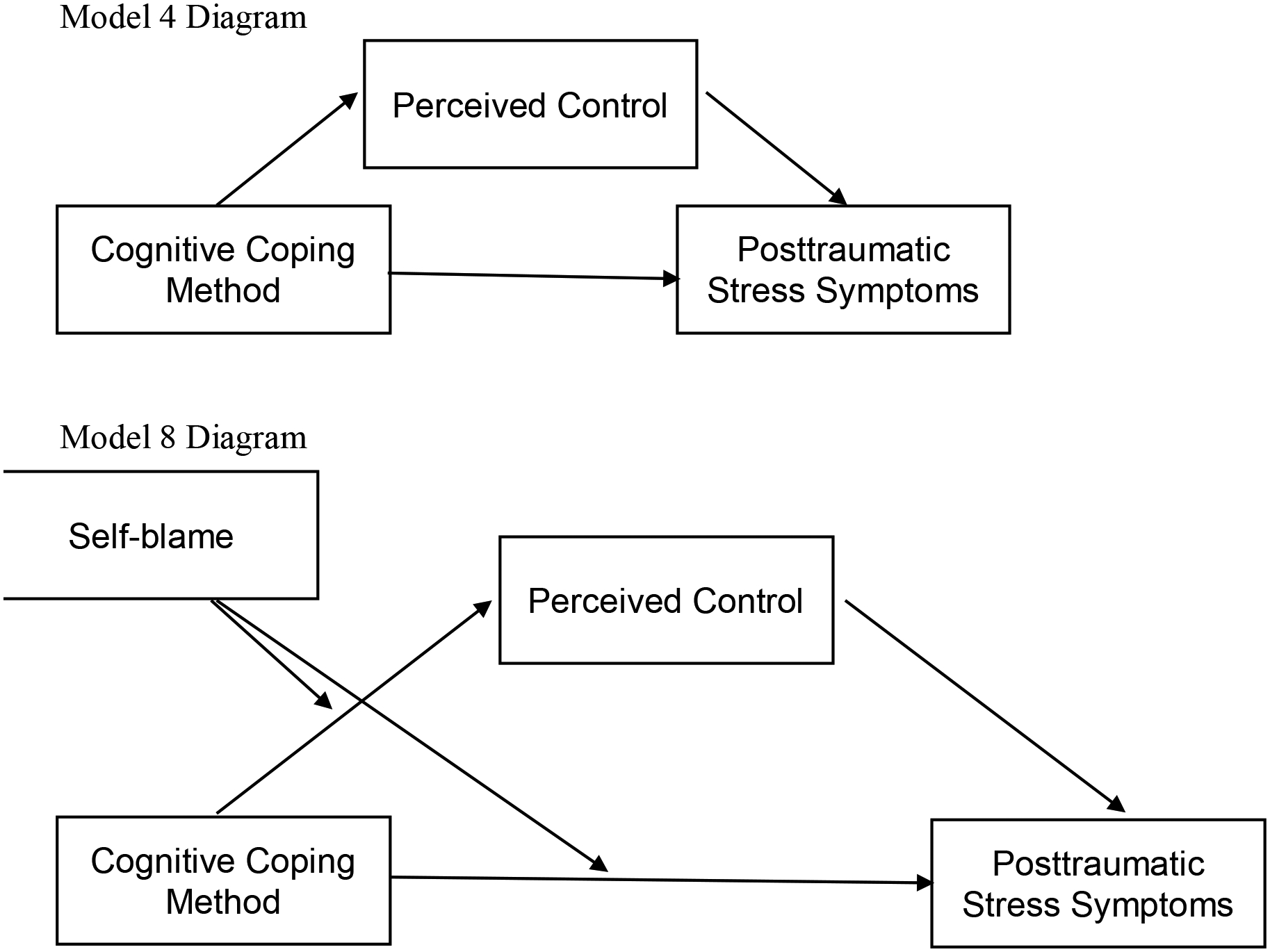
Diagrams of Hayes’ Models
We address missing data with Multiple Imputation (MI). More than 5% of data missing may change results significantly (Dong & Peng, 2013); 7.1% of individual responses to specific questions were missing from our data set and 32.8% of participants were missing at least one data point. We conducted Little’s Test to confirm that our data was missing completely at random for each of our primary measures (PDS x2= 127.48, p=.998; COPE x2=4646.284, p=.263; PTCI x2= 16.951, p=.151). We conducted MI in SPSS. MI has been shown to result in greater accuracy and power than other missing data approaches (Enders, 2017). Settings were set to five imputations with the automatic imputation setting. When pooled imputation outputs were not generated, we used the original data outcomes. We ran the models with and without the multiply imputed data. While the directionality of all of our variables remained the same, our results were not significant without the MI. Given the large number of variables and covariates for which we controlled in our models, we were likely underpowered to detect effects without the MI. We conducted a three-way ANOVA using the multiply-imputed data set for each of the writing groups for each of our variables to determine if there were group differences between the groups. There were no group differences so we combined all participants into one group for analysis.
Results
The most common PTEs in our sample were a sudden loss of a family member or friend (42%), “other” trauma (21%), or a motor vehicle accident (10%). Other types of PTEs participants reported included experiencing a natural disaster (1.4%), combat or warfare (.7%), robbery with a weapon (.9%), assault (.9%), witnessing an assault (1.2%), being threatened with death or serious harm (1.4%), physical abuse growing up (2.1%), intimate partner violence (1.6%), sexual contact under the age of 13 with someone five or more years older (1.4%), unwanted sexual contact before age 13 with someone of similar age (.7%), and unwanted sexual contact as a teenager or adult (4%). If participants reported more than one PTE, they were asked to choose the event they found most distressing and to complete all measures in regard to that event. Baseline distress was moderate with the mean score on the PDS of 9.63 exceeding the PTSD cutoff score of eight suggested by Winters and colleagues (2014). Based on a paired samples t-test, mean levels of PTSS significantly decreased between T1 and T3 (p=.001, 95% C.I.= 0.732, 2.827). The PTSS distribution was positively skewed due to floor effects of symptoms, which is typical within trauma samples (Bonanno & Diminich, 2013). Due to the skewed distribution PTSS in the sample, we also compared T1 to T3 PTSS using the Wilcoxon signed rank test as a non-parametric test to account for this skewed distribution. With this test we found the same result that PTSS significantly decreased from T1 to T3 (Z=−4.55, p=.000).
T1 positive reinterpretation was negatively correlated with T2 self-blame. T1 acceptance was negatively correlated with T1 perceived control. Religious coping at T1 was positively correlated with T1and T3 PTSS and inversely with T1 perceived control. T3 PTSS was positively correlated with self-blame at T2 and negatively with perceived control at T1 and T2 (See Table 1). In a hierarchical multiple regression, controlling for T1 PTSS, positive reinterpretation negatively predicted (B=−1.21, p<.001), religious coping positively predicted (B=0.74, p<.001), and acceptance did not predict T3 PTSS (B=0.15, p=.270).
Table 1.
Correlations of Baseline Coping with T2 Sense of Control and Self-blame and T3 Perceived Stress Symptoms
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | M | SD |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 Pos Reint | - | .45*** | .21*** | .05 | −.03 | −.02 | −.10* | −.05 | 2.96 | .64 |
| 2. T1 Accept | - | - | .04 | .09 | −.10* | .03 | .01 | .01 | 2.69 | .65 |
| 3. T1 Religious Coping | - | - | - | .15** | −.12* | −.06 | .00 | .12* | 1.75 | .93 |
| 4. T1 PTSS | - | - | - | - | −.38*** | −.32*** | .29*** | .43*** | 9.63 | 8.40 |
| 5. T1 Perceived Control | - | - | - | - | - | .53*** | −.22*** | −.23*** | 3.71 | 1.19 |
| 6. T2 Perceived Control | - | - | - | - | - | - | −.30*** | −.23*** | 3.61 | 1.19 |
| 7. T2 Self-Blame | - | - | - | - | - | - | - | .21*** | 2.15 | 1.36 |
| 8. T3 PTSS | - | - | - | - | - | - | - | - | 7.90 | 9.34 |
Correlations use pooled data from five multiple imputations. M= original data mean (pooled multiply imputed mean and SD not produced); SD= original data standard deviation; Pos Reint= Positive Reinterpretation; Accept=acceptance; PTSS= posttraumatic stress symptoms; T1=Time 1; T2= Time 2; T3= Time 3.
p<.05,
p<.01,
p<.001
In our simple mediation models, T2 perceived control did not mediate the relationship between T1 positive reinterpretation and T3 PTSS, as the indirect effect was not significant (B=−0.01, 95% C.I. [−0.07, 0.03]) while the direct effect was significant (B=−0.92, t=−3.50, 95% C.I. [−1.44, −.40], p=.001; see Figure 2a). T2 perceived control fully mediated the relationship between T1 acceptance and T3 PTSS, such that there was a significant indirect effect (B=−0.06, 95% C.I. [−.12, −.01]) and the direct effect was not significant (B=−0.31, t=−1.18, 95% C.I. [−.83, .20], p=.24; see Figure 2b). T2 perceived control did not mediate the link between T1 religious coping and T3 PTSS, as the indirect effect was not significant (B=−0.03, 95% C.I. [−.07, .01]), while the direct effect was significant (B=0.53, t=2.95, 95% C.I. [.18, .88], p=.003; see Figure 2c). All analyses controlled for T1 PTSS and T1 perceived control.
Figure 2.
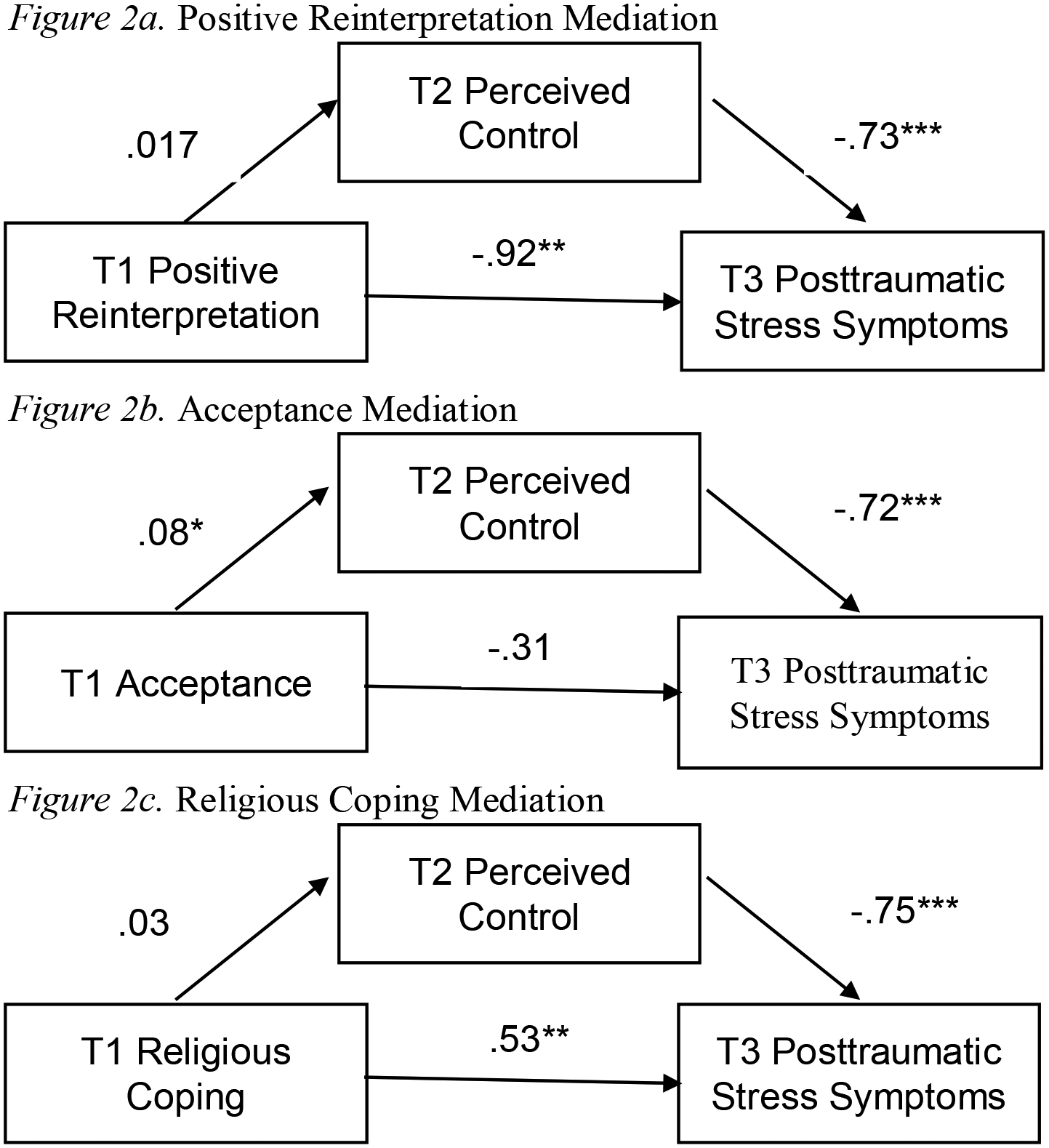
Meditation of Perceived Control Between Cognitive Coping Styles and PTSS
*p<.05, **p<.01, ***p<.001
We tested for interactions and conditional effects in a moderated mediation model while controlling for T1 PTSS and T1 perceived control. Positive reinterpretation interacted with self-blame to predict increased perceived control and subsequently decreased PTSS (B=−0.03, 95% C.I. [−.07, −.01]). Specifically, positive reinterpretation was particularly helpful at decreasing PTSS by means of increasing perceived control for those with medium to high levels of self-blame. T1 acceptance coping’s effect on change in PTSS through increased perceived control did not significantly vary based on levels of self-blame (B=−0.02, 95% C.I. [−.05, .002]), though our results suggest potential marginal effects. Religious coping interacted with self-blame to predict decreased perceived control and subsequent increased PTSS, suggesting a partially moderated mediation (B=0.04, 95% C.I. [.01, .07]). Specifically for individuals who experienced medium to high levels of self-blame, more religious coping resulted in lower perceived control over one’s life and increased PTSS. (For all conditional direct and indirect effects, see Table 2).
Table 2.
Conditional Direct and Indirect Effects of Self-blame of each Cognitive Coping Method on PTSS
| B (95% C.I.) | ||||
|---|---|---|---|---|
| Level of Self-Blame | Positive Reinterpretation | Acceptance Coping | Religious Coping | |
| 1.00 (minimum value; −1 S.D. would be .80) | Indirect Effect | 0.06 (0.01,0 .13)* | −0.02 (−0.07, 0.03) | −0.06 (−0.12, −0.02)* |
| Direct Effect | 0.19 (−0.51, 0.89) | 0.94 (0.28, 1.60)* | 0.83 (0.36, 1.30)* | |
| 2.15 (Mean) | Indirect Effect | 0.02 (−0.02, 0.07) | −0.04 (−0.10, −0.001)* | −0.01 (−0.06, 0.02) |
| Direct Effect | −0.66 (−1.18, −0.14)* | −0.18 (−0.69, 0.34) | 0.57 (0.22, 0.92)* | |
| 3.50 (+1 S.D.) | Indirect Effect | −0.02 (−0.09, 0.03) | −0.07 (−0.15, −0.02)* | 0.05 (0.0001, 0.10)* |
| Direct Effect | −1.67 (−2.32, −1.01)* | −1.49 (−2.15, −0.84)* | 0.27 (−0.24, 0.78) |
Note: Positive indirect effects suggest increased sense of control for those higher in self-blame, while negative indirect effects suggest decreased sense of control for those higher in self-blame. Positive direct effects suggest that the coping results in increased PTSS for those higher in self-blame, while negative direct effects suggest a decrease in PTSS for those higher in self-blame. The minimum value is used as the lower parameter of self-blame, as one standard deviation below the mean falls below the minimum reported score.
B=Unstandardized beta coefficient; S.D.= standard deviation;
significant 95% confidence interval range.
Regarding conditional direct effects on PTSS (excluding “perceived control” mediator effects), both positive reinterpretation and acceptance significantly interacted with self-blame to result in changes in PTSS. Positive reinterpretation reduced PTSS for those high in self-blame (Interaction: B= −0.71, 95% C.I. [−1.09, −.39], p<.001). Acceptance reduced PTSS for those high in self-blame but increased PTSS for those low in self-blame (Interaction: B=−0.97, 95% C.I. [−1.31, −.64], p<.001). Self-blame did not interact with religious coping to predict PTSS when not accounting for perceived control (Interaction: B= −0.23, 95% C.I. [−.50, .05], p=.10). See Figure 3 and Table 2 for conditional direct and indirect effects of self-blame on PTSS.
Figure 3.
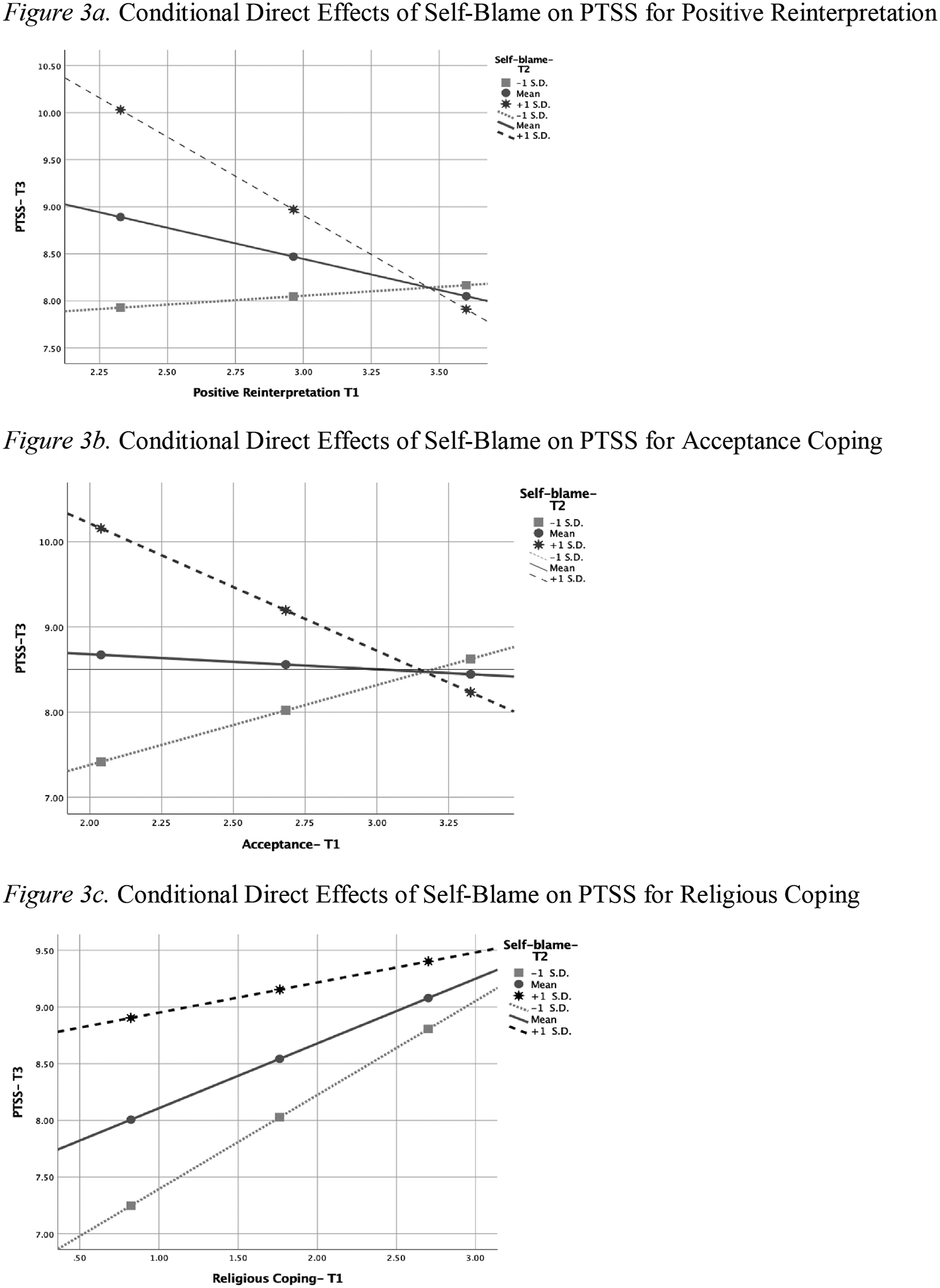
Conditional Direct Effects of Self-Blame on PTSS for Cognitive Coping Methods
As a post-hoc analysis, we separately assessed positive religious coping and negative spiritual struggle, both of which were positively correlated with the overall COPE religious coping scale (positive religious coping: r=.65, p<.001; spiritual struggle: r=.32, p<.001). For spiritual struggle (B=0.04, 95% C.I. [.003, .10]), this moderated mediation remained significant, predicting increased PTSS by means of decreased perceived control for those high in self-blame. For positive religious coping, the relationship was not significant (B=0.02, 95% C.I. [−.001, .06]) but suggested a marginally significant trend towards increased PTSS (See Table 2).
Discussion
Our research sought to determine how different forms of cognitive coping predict change in PTSS longitudinally. Our first hypothesis was partially supported as positive reinterpretation reduced PTSS over time, which is consistent with existing cross-sectional literature (Boden et al., 2012; Hanley et al., 2017; Kleim et al., 2013). Results regarding the direct effects of acceptance and religious coping were not entirely in line with existing literature. Acceptance did not directly predict PTSS, contrary to the majority of existing studies (e.g., Bonn-Miller et al., 2010; Ssenyonga et al, 2013; Thompson et al., 2011), though this is not the first study to find no relationship between the two variables (e.g., Park, Riley, & Snyder, 2012). Finally, religious coping led to increased PTSS, lending credence to the side of the literature that has found negative effects of religious coping (Park et al., 2017; Witvliet et al., 2004;); further, we not only found a positive association between spiritual struggle and PTSS, but also a trend towards negative effects of positive religious coping on PTSS. Our sample demographics may have contributed to our findings that religious coping resulted in poorer outcomes, as past literature shows that religious coping may be effective for People of Color (e.g., Ahrens et al., 2010; Feder et al., 2013), while our sample was primarily White.
Next, we examined a variable that may be responsible for change in PTSS after use of each coping method based on current theoretical frameworks, perceived control over one’s life (Janoff-Bulman, 1979). Our second hypothesis was also partially supported in that self-blame mediated the effect of acceptance coping on PTSS, but not the effect of reinterpretation or religious coping on PTSS. The mediation of acceptance and PTSS through perceived control suggests for individuals who feel that the trauma violated their belief they were in control of what happened to them, acceptance is an effective method for regaining a sense of control of their lives. Interestingly, perceived control did not act as a mediator between positive reinterpretation or religious coping and PTSS. This finding suggests that perceived control may not serve as a primary mechanism for the effects of these coping strategies on changes in PTSS. While higher perceived control over one’s life predicted decreased PTSS in each model, only acceptance predicted significant increases in perceived control over time.
Finally we examined self-blame relative to the trauma, which may drive symptoms. We reasoned that those high in self-blame may particularly benefit from cognitive coping strategies. Our third hypothesis was supported as our study observed effects of each coping strategy differed based on level of self-blame. For those high in self-blame, positive reinterpretation resulted in decreased PTSS by means of increasing perceived control while religious coping resulted in increased PTSS by means of decreasing perceived control. The difference in effectiveness of coping style based on levels of self-blame suggests different coping approaches may be more beneficial for a high self-blame trauma population than a general trauma population. For example, for individuals low in self-blame religious coping may increase PTSS while for individuals with medium to high levels of self-blame, positive reappraisal may decrease symptoms. Acceptance, surprisingly, increases PTSS for those low in self-blame and decreases PTSS for those high in self-blame. Religious coping may be harmful to those with low levels of self-blame because these individuals may have a stronger external locus of control, which may prompt less perceived ability to stop future traumas from occurring. For those high in self-blame, positive reappraisal may be helpful at decreasing PTSS because it may allow individuals to find benefits or positive outcomes related to the trauma, making the fear of future PTEs occurring less pervasive. Acceptance may be helpful at reducing PTSS for those high in self-blame because it may lead these individuals to reflect on ways that they believe they may have played a role in the event, thereby providing a sense of control over future events. Acceptance may be detrimental to those low in self-blame because those who accept the event as being due to external circumstances may experience fear and a lack of control over the event happening again in the future.
While reestablishing a sense of control may be important for all trauma survivors (Dunmore et al., 2001; Frazier et al., 2001; Smith et al., 2018), these results suggest it may be even more important for individuals high in self-blame. Thus, it would be beneficial for clinicians to assess self-blame in trauma survivors as the presence of self-blame may call for different treatment modalities. While past literature has shown that religious coping can be helpful (e.g., Ahrens et al, 2010; Feder et al., 2013), it was not helpful for the sample of survivors in this study, especially for the subset of survivors high in self-blame. These individuals may benefit from interventions that utilize positive reinterpretation or acceptance.
Limitations
Regarding limitations of our study, our sample was largely homogenous, composed primarily of White, non-Hispanic women attending college, so these findings may not generalize to more diverse populations. Further, the age at time of trauma and time since trauma were not collected in this study; therefore, we could not control for these in our analyses. Our study also took place over the course of two months, which may not fully capture symptom change over time when compared to more long-term trauma studies. In addition, our study uses DSM-IV PTSD diagnostic criteria, rather than DSM-5 diagnostic criteria. This is due to this being a secondary analysis on a previous, larger study that was originally designed in 2011 when the DSM-IV was still commonly used. Finally, the most common DSM-IV classified PTE reported for our study was the sudden loss of a family member or friend. Each PTE may require different coping strategies. The effectiveness of each coping style and the impact of self-blame on PTSS as we see in the present study may manifest differently for assaultive traumas as opposed to more general PTEs (Guina et al., 2018). For example, specific types of trauma, such as sexual trauma, may result in higher rates of self-blame (Moor & Farchi, 2011).
In sum, these results suggest that while cognitive coping may impact PTSS, the directionality and mechanisms of each of their effects may depend on levels of self-blame. These findings illustrate how self-appraisals of blame may impact a sense of control after a traumatic event, and, therefore, should be considered in treatment. Treatment can be adapted to target risk factors of self-blame and perceived control over one’s life in order to diminish PTSS over time.
Funding:
This project was supported by the National Institute of Mental Health under Grant 5R21MH75737-2, awarded to Crystal L. Park.
Footnotes
The authors do not have any declarations of interest to disclose.
All procedures were approved by the University of Connecticut Institutional Review Board.
References
- Agar E, Kennedy P, & King N (2006). The role of negative cognitive appraisals in PTSD symptoms following spinal cord injuries. Behavioural and Cognitive Psychotherapy, 34(4), 437–452. [Google Scholar]
- Ahrens C, Abeling S, Ahmad S, & Hinman J (2010). Spirituality and well-being: The relationship between religious coping and recovery from sexual assault. Journal of Interpersonal Violence, 25(7), 1242–1263. [DOI] [PubMed] [Google Scholar]
- Aldwin C (2007). Stress, coping, and development: An integrative perspective. Guilford Press. [Google Scholar]
- Allen C, Mercer M, & Lilly M (2016). Duty-related posttraumatic stress symptoms in 9/11 telecommunicators. Journal of Aggression, Maltreatment & Trauma, 25(7), 686–701. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th Ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Arora J (1999). Implications of behavioral and characterological self-blame for the adjustment to negative life events. ProQuest Dissertations and Theses.
- Boden M, Bonn-Miller M, Kashdan T, Alvarez J, & Gross J (2012). The interactive effects of emotional clarity and cognitive reappraisal in posttraumatic stress disorder. Journal of Anxiety Disorders, 26(1), 233–8. [DOI] [PubMed] [Google Scholar]
- Bonanno G & Diminich E (2013). Positive adjustment to adversity–trajectories of minimal–impact resilience and emergent resilience. Journal of Child Psychology and Psychiatry, 54(4), 378–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonn-Miller M, Vujanovic A, Twohig M, Medina J, & Huggins J (2010). Posttraumatic stress symptom severity and marijuana use coping motives. Mindfulness, 1(2), 98–106. [Google Scholar]
- Boyraz G, & Waits J (2018). Interpersonal trauma and physical health symptoms in college students. Journal of Loss and Trauma, 23(1), 70–87. [Google Scholar]
- Britt T, Adler A, Sawhney G, & Bliese P (2017). Coping strategies as moderators of the association between combat exposure and posttraumatic stress disorder symptoms. Journal of Traumatic Stress, 30(5), 491–501. [DOI] [PubMed] [Google Scholar]
- Bryant-Davis T, Ullman S, Tsong Y, Anderson G… Gray A (2014). Healing Pathways: Longitudinal effects of religious coping and social support on PTSD symptoms in African American sexual assault survivors. Journal of Trauma & Dissociation, 16(1), 114–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussell V, & Naus M (2010). A longitudinal investigation of coping and posttraumatic growth in breast cancer survivors. Journal of Psychosocial Oncology, 28(1), 61–78. [DOI] [PubMed] [Google Scholar]
- Carver C, Scheier M, & Weintraub J (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56, 267–283. [DOI] [PubMed] [Google Scholar]
- Chan C, & Rhodes J (2013). Religious coping, posttraumatic stress, psychological distress, and posttraumatic growth among female survivors four years after Hurricane Katrina. Journal of Traumatic Stress, 26(2), 257–265. [DOI] [PubMed] [Google Scholar]
- Currier J, Holland J, & Malott J (2015). Moral injury, meaning making, and mental health in returning veterans. Journal of Clinical Psychology, 71(3), 229–240. [DOI] [PubMed] [Google Scholar]
- Dong Y & Peng C (2013). Principled missing data methods for researchers. SpringerPlus, 2(1), 222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunmore E, Clark D, & Ehlers A (2001). A prospective investigation of the role of cognitive factors in persistent posttraumatic stress disorder (PTSD) after physical or sexual assault. Behaviour Research and Therapy, 39(9), 1063–1084. [DOI] [PubMed] [Google Scholar]
- Ehlers A, & Clark D (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Clark D, Hackmann A, McManus F, & Fennell M (2005). Cognitive therapy for post-traumatic stress disorder. Behaviour Research and Therapy, 43(4), 413–431. [DOI] [PubMed] [Google Scholar]
- Enders C (2017). Multiple imputation as a flexible tool for missing data handling in clinical research. Behaviour Research and Therapy, 98, 4–18. [DOI] [PubMed] [Google Scholar]
- Feder A, Ahmad S, Lee E, Morgan J… Charney D (2013). Coping and PTSD symptoms in Pakistani earthquake survivors: Purpose in life, religious coping and social support. Journal of Affective Disorders, 147(1–3), 156–163. [DOI] [PubMed] [Google Scholar]
- Feder A, Mota N, Salim R, Rodriguez J.. & Reissman DB (2016). Risk, coping and PTSD symptom trajectories in World Trade Center responders. Journal of Psychiatric Research, 82, 68–79. [DOI] [PubMed] [Google Scholar]
- Foa E, Cashman L, Jaycox L, & Perry K (1997). The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment, 9(4), 445–451. [Google Scholar]
- Foa E, Ehlers A, Clark D, Tolin D…& Haynes S (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11(3), 303–314. [Google Scholar]
- Foa EB, McLean CP, Zang Y, Zhong J, Powers MB, Kauffman BY, … Knowles K (2016). Psychometric properties of the Posttraumatic Diagnostic Scale for DSM-5 (PDS-5). Psychological Assessment, 28, 1166–1171. doi: 10.1037/pas0000258 [DOI] [PubMed] [Google Scholar]
- Frazier P, Berman M, & Steward J (2001). Perceived control and posttraumatic stress: A temporal model. Applied and Preventive Psychology, 10(3), 207–223. [Google Scholar]
- Frazier P, Keenan N, Anders S, Perera S, Shallcross S, & Hintz S (2011). Perceived past, present, and future control and adjustment to stressful life events. Journal of Personality and Social Psychology, 100(4), 749–765. [DOI] [PubMed] [Google Scholar]
- George L Park C, & Chaudoir S (2016). Examining the relationship between trauma centrality and posttraumatic stress disorder symptoms. Traumatology, 22(2), 85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guina J, Nahhas R, Sutton P, & Farnsworth S (2018). The influence of trauma type and timing on PTSD symptoms. The Journal of Nervous and Mental Disease, 206(1), 72–76. [DOI] [PubMed] [Google Scholar]
- Hanley A, Garland E, & Tedeschi R (2017). Relating dispositional mindfulness, contemplative practice, and positive reframing with posttraumatic cognitive coping, stress, and growth. Psychological Trauma: Theory, Research, Practice, and Policy, 9(5), 526–536. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis. Journal of Educational Measurement, 51(3), 335–337. [Google Scholar]
- Hébert M, Daspe M, & Cyr M (2018). An analysis of avoidant and approach coping as mediators of the relationship between paternal and maternal attachment security and outcomes in child victims of sexual abuse. Psychological Trauma: Theory, Research, Practice, and Policy, 10(4), 402–410. [DOI] [PubMed] [Google Scholar]
- Howell K, Kaplow J, Layne C, Benson M.. & Pynoos R (2015). Predicting adolescent posttraumatic stress in the aftermath of war: Differential effects of coping strategies across trauma reminder, loss reminder, and family conflict domains. Anxiety, Stress, & Coping, 28(1), 88–104. [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R (1979). Characterological versus behavioral self-blame: Inquiries into depression and rape. Journal of Personality and Social Psychology, 37(10), 1798–1809. [DOI] [PubMed] [Google Scholar]
- Jerusalem M, & Schwarzer R (1992). Self-efficacy as a resource factor in stress appraisal processes. In Schwarzer R (Ed.), Self-efficacy: Thought control of action. (pp. 195–213). Washington, DC: Hemisphere Publishing Corp. [Google Scholar]
- Kleim B, Grey N, Wild J, Nussbeck F.. & Ehlers A (2013). Cognitive change predicts symptom reduction with cognitive therapy for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81(3), 383–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline N, Berke D, Rhodes C, Steenkamp M, & Litz B (2018). Self-blame and PTSD following sexual assault. Journal of Interpersonal Violence. 10.1177/0886260518770652 [DOI] [PubMed] [Google Scholar]
- Larsen S & Fitzgerald L (2011). PTSD symptoms and sexual harassment: The role of attributions and perceived control. Journal of Interpersonal Violence, 26(13), 2555–2567. [DOI] [PubMed] [Google Scholar]
- Mitchell R, Brennan K, Curran D, Hanna D, & Dyer K (2017). A meta‐analysis of the association between appraisals of trauma and posttraumatic stress in children and adolescents. Journal of Traumatic Stress, 30(1), 88–93. [DOI] [PubMed] [Google Scholar]
- Mong M, Noguchi K, & Ladner B (2012). Immediate psychological impact of the Deepwater Horizon oil spill. Journal of Aggression, Maltreatment & Trauma, 21(6), 691–704. [Google Scholar]
- Moor A, & Farchi M (2011). Is rape-related self-blame distinct from other post traumatic attributions of blame? A comparison of severity and implications for treatment. Women & Therapy, 34(4), 447–460. [Google Scholar]
- Moscardino U, Scrimin S, Capello F, & Altoè G (2014). Self-blame and PTSD symptoms in adolescents exposed to terrorism. Journal of Adolescence, 37(1), 47–52. [DOI] [PubMed] [Google Scholar]
- Najdowski C & Ullman S (2009). PTSD symptoms and self-rated recovery among adult sexual assault survivors. Psychology of Women Quarterly, 33(1), 43–53. [Google Scholar]
- National Center for PTSD. (2018). Retrieved from https://www.ptsd.va.gov
- Pargament K, Feuille M, & Burdzy D (2011). The Brief RCOPE: Current psychometric status of a short measure of religious coping. Religions, 2(1), 51–76. [Google Scholar]
- Pargament K, Koenig H, & Perez L (2000). The many methods of religious coping: Development and initial validation of the RCOPE. Journal of Clinical Psychology, 56(4), 519–543. [DOI] [PubMed] [Google Scholar]
- Park CL (2010). Making sense of the meaning literature: An integrative review of meaning making. Psychological Bulletin, 136(2), 257–301. [DOI] [PubMed] [Google Scholar]
- Park C & Ai A (2006). Meaning making and growth: New directions for research on survivors of trauma. Journal of Loss and Trauma, 11(5), 389–407. [Google Scholar]
- Park C & George L (2013). Assessing meaning and meaning making in the context of stressful life events. The Journal of Positive Psychology, 8(6), 483–504. [Google Scholar]
- Park C, Riley K, George L, Gutierrez I.. & Braun T (2016). Assessing disruptions in meaning: Development of the Global Meaning Violation Scale. Cognitive Therapy and Research, 40(6), 831–846. [Google Scholar]
- Park C, Riley K, & Snyder L (2012). Meaning making coping, making sense, and post-traumatic growth following the 9/11 terrorist attacks. The Journal of Positive Psychology, 7(3), 198–207. [Google Scholar]
- Park C, Smith P, Lee S, Mazure C, & Piedmont R (2017). Positive and negative religious/spiritual coping and combat exposure as predictors of posttraumatic stress and perceived growth in Iraq and Afghanistan veterans. Psychology of Religion and Spirituality, 9(1), 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick P, Monson C, & Chard K (2016). Cognitive processing therapy for PTSD: A comprehensive manual. Guilford Publications. [Google Scholar]
- Roth S, & Cohen L (1986). Approach, avoidance, and coping with stress. American Psychologist, 41(7), 813–819. [DOI] [PubMed] [Google Scholar]
- Schmied E, Padilla G, Thomsen C, Lauby M..& Taylor M (2015). Sex differences in coping strategies in military survival school. Journal of Anxiety Disorders, 29, 7–13. [DOI] [PubMed] [Google Scholar]
- Simmen-Janevska K, Brandstätter V, & Maercker A (2012). The overlooked relationship between motivational abilities and posttraumatic stress: A review. European Journal of Psychotraumatology, 3(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith N, Sippel L, Presseau C, Rozek D.. & Harpaz-Rotem I (2018). Locus of control in US combat veterans. Psychiatry Research, 268, 152–156. [DOI] [PubMed] [Google Scholar]
- Ssenyonga J, Owens V, & Olema DK (2013). Posttraumatic cognitions, avoidance coping, suicide, and posttraumatic stress disorder among adolescent refugees. Procedia - Social and Behavioral Sciences, 82(C), 261–265. [Google Scholar]
- Thompson R, Arnkoff D, & Glass C (2011). Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma, Violence, & Abuse, 12(4), 220. [DOI] [PubMed] [Google Scholar]
- Vaughn-Coaxum R, Wang Y, Kiely J, Weisz J, & Dunn E (2018). Associations between trauma type, timing, and accumulation on current coping behaviors in adolescents. Journal of Youth and Adolescence, 47(4), 842–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watlington C, & Murphy C (2006). The roles of religion and spirituality among African American survivors of domestic violence. Journal of Clinical Psychology, 62(7), 837–857. [DOI] [PubMed] [Google Scholar]
- Winters L, Karow A, Reimer J, Fricke S..& Schäfer I (2014). Psychometric properties of the Posttraumatic Diagnostic Scale (PDS) in alcohol-dependent patients. Substance Abuse, 35(3), 262–267. [DOI] [PubMed] [Google Scholar]
- Witvliet C, Phipps K, Feldman M, & Beckham J (2004). Posttraumatic mental and physical health correlates of forgiveness and religious coping in military veterans. Journal of Traumatic Stress, 17(3), 269–273. [DOI] [PubMed] [Google Scholar]
- Wisco B, Sloan D, & Marx B (2013). Cognitive emotion regulation and written exposure therapy for Posttraumatic Stress Disorder. Clinical Psychological Science, 1(4), 435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]


