Abstract
Introduction:
This study compares rural and urban differences in the rates of nonfatal self-harm in the U.S. in 2018.
Methods:
Nationwide Emergency Department Sample and Census data were analyzed to calculate the RR of emergency department visits for self-harm between rural and urban residents. The analyses were conducted in 2021.
Results:
Among a weighted total of 488,000 emergency department visits for self-harm in the U.S., 80.5% were urban residents, and 18.3% were rural residents. In both settings, poisoning was the most common mechanism for self-harm, followed by cutting. Firearm-related self-harm and suffocation each accounted for <2% of total self-harm cases. Overall, the age-adjusted emergency department visit rate for self-harm was 252.3 per 100,000 for rural residents, which was 1.5 (95% CI=1.4, 1.6) times greater than the rate for urban residents (170.8 per 100,000 residents). The rates of self-harm among rural residents were higher than those of urban residents for both male and female residents, for all age groups except people aged ≥65 years, and by all mechanisms.
Conclusions:
Comprehensive suicide prevention strategies tailored to rural communities may mitigate the rural–urban disparity in morbidity from suicidal behavior.
INTRODUCTION
Suicide is the 10th leading cause of death in the U.S.1 Rural residents are disproportionately affected by suicide compared with their urban counterparts.2,3 Still, suicide is only a snapshot of a complex public health problem. For every suicide, there exist, on average, about 10 emergency department (ED) visits for nonfatal self-harm.4 Nonfatal self-harm varies from suicides in the pattern of demographic characteristics and mechanisms used.5 Despite the well-documented rural–urban disparity in suicide rates, there is a paucity of data on rural–urban differences in nonfatal self-harm. Such information is necessary to generate a more complete picture of the rural–urban gap in the morbidity and mortality of suicidal behavior to guide prevention strategies in improving rural health. To address this gap, this study, using nationally representative data, compares the rates of ED visits for self-harm between rural and urban residents.
METHODS
The Nationwide Emergency Department Sample (NEDS) (https://www.hcup-u.ahrq.gov/nedsoverview.jsp) is the largest all-payer ED database in the U.S. It contained 36 million ED visits from 37 states in 2018. Nationally representative estimates were derived using sampling weights.
External Cause-of-Injury Matrices (https://www.cdc.gov/nchs/injury/injury_tools.htm) were applied to 2018 NEDS to identify ED visits for self-harm for people aged ≥10 years. The mechanism of self-harm was classified as firearm, suffocation, poisoning, cutting, and other. Following this lethality order for mechanisms,5 people who used multiple mechanisms were categorized by the most lethal mechanism recorded. Rural–urban designation for patient’s county of residence was provided in NEDS. Population estimates for rural and urban locations in 2018 were obtained by linking the 2013 National Center for Health Statistics Urban–Rural Classification Scheme for Counties (https://www.cdc.gov/nchs/data_access/urban_rural.htm) to Annual County Resident Population Estimates that U.S. Census Bureau released in 2020 (https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-detail.html). For both NEDS and census data, the 4 metropolitan categories (large central metropolitan, large fringe metropolitan, medium metropolitan, and small metropolitan) were classified as urban, and the 2 nonmetropolitan categories (micropolitan and those that are neither metropolitan nor micropolitan) were classified as rural.
The rates of ED visits for self-harm were calculated for rural and urban residents. RR of self-harm was calculated as the rate ratio between rural and urban populations. Delta methods were used to derive SEs for all rates and rate ratios.6 All analyses were stratified by age group (10–19 years, 20–44 years, 45–64 years, ≥65 years), sex, and mechanism. The analyses were conducted using SAS, version 9.4, and SUDAAN, version 11.0.3. This study involving secondary analyses of publicly available data was exempt from the Centers for Disease Control and Prevention IRB review.
RESULTS
Among a weighted total of 488,000 estimated ED visits for self-harm in the U.S., 18.3% were rural residents, 80.5% were urban residents, and 1.2% were missing in rural/urban location. Rural and urban self-harm cases showed similar distributions in age (78.5% in urban and 80.0% in rural were aged <45 years) and sex (60.2% in rural and 60.8% in urban were female). For both rural and urban residents, poisoning was the most common mechanism for self-harm, followed by cutting. Firearm-related self-harm and suffocation each accounted for <2% of total self-harm cases (Table 1).
Table 1.
Characteristics of ED Visits for Self-Harm, by Rural and Urban Locations
| Characteristics | Rural (unweighted n=18,845, weighted n=89,000) Weighted n (in thousands) (%) | Urban (unweighted n=99,312, weighted n=393,000) Weighted n (in thousands) (%) |
|---|---|---|
|
| ||
| Age group,a years | ||
| 10–19 | 28.9 (32.4) | 125.8 (32) |
| 20–44 | 42.5 (47.6) | 182.6 (46.5) |
| 45–64 | 14.8 (16.6) | 70.1 (17.9) |
| ≥65 | 3.0 (3.4) | 14.3 (3.6) |
| Sex | ||
| Male | 35.4 (39.8) | 154 (39.2) |
| Female | 53.7 (60.2) | 238.7 (60.8) |
| Mechanisma | ||
| Firearm | 1.3 (1.5) | 3.1 (0.8) |
| Suffocation | 1.3 (1.4) | 4.8 (1.2) |
| Poisoning | 53.9 (60.4) | 241.9 (61.6) |
| Cutting | 20.7 (23.3) | 91.4 (23.3) |
| Other mechanisms | 12.0 (13.4) | 51.7 (13.1) |
Data sources: NEDS, available at https://www.hcup-us.ahrq.gov/nedsoverview.jsp.
The distribution between rural and urban residents was significantly different at p<0.05.
ED, Emergency Department; NEDS, National Emergency Department Sample.
Overall, the age-adjusted ED visit rate for self-harm was 252.3 per 100,000 for rural residents, which was 1.5 (95% CI=1.4, 1.6) times the rate for urban residents (170.8 per 100,000 residents). Male and female residents showed a similar rural–urban gap for self-harm rates (RR=1.5, 95% CI=1.4, 1.6) for both male and female residents. Rural residents had higher risk for self-harm by all mechanisms, particularly by firearm, than urban residents (RR=2.6, 95% CI=2.1, 3.1 for firearm; RR=1.8, 95% CI=1.5, 2.1 for suffocation; RR=1.4, 95% CI=1.3, 1.5 for poisoning; RR=1.5, 95% CI=1.4, 1.6 for cutting; and RR=1.5, 95% CI=1.4, 1.7 for other mechanisms). When stratified by age group, the rural–urban difference in ED visit rates for self-harm was observed for all groups aged <65 years (RR=1.4, 95% CI=1.2, 1.6 for age 10–19 years; RR=1.6, 95% CI=1.4, 1.8 for age 20–44 years; and RR=1.2, 95% CI=1.1, 1.4 for age 45–64 years) (Figure 1).
Figure 1.
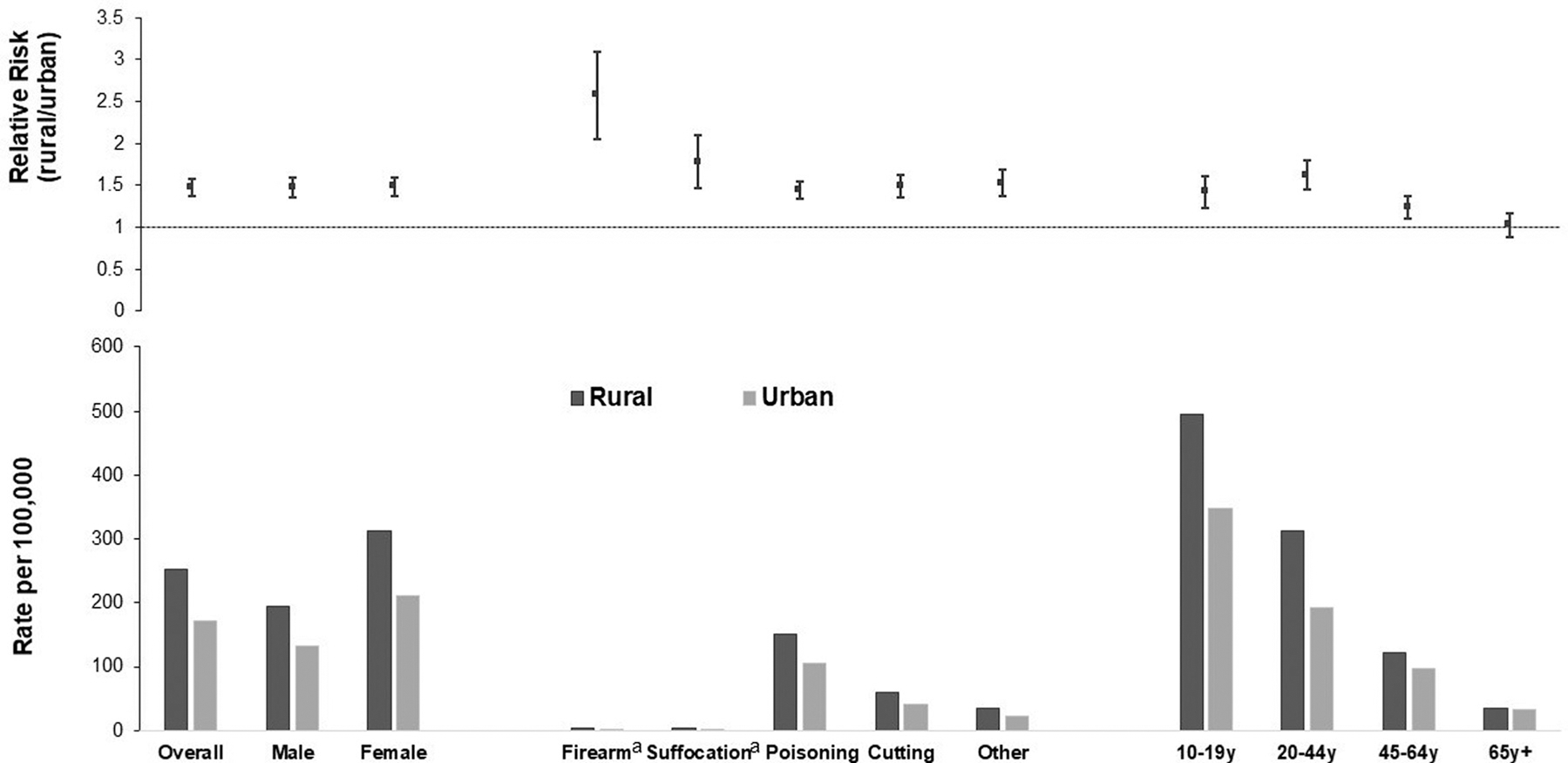
Rates and RRs of ED visits for self-harm for rural and urban residents, U.S. 2018.
Notes: The error bars for RRs indicate their 95% CIs. Data sources include NEDS, available at https://www.hcup-us.ahrq.gov/nedsoverview.jsp, and 2009‒2019 Annual County Resident Population Estimates that U.S. Census Bureau released in June 2020, available at https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-detail.html. The rates for overall, by sex, and by mechanisms were age adjusted to 2000 U. S. standard population. RR was calculated as the rate ratio on ED visits for self-harm between rural and urban populations.
aThe rates for nonfatal self-harm by firearm (3.23 per 100,000 for rural and 1.25 per 100,000 for urban) or suffocation (3.7 per 100,000 for rural and 2.08 per 100,000 for urban) were low because self-harm by these mechanisms tends to be more lethal.
ED, Emergency Department; NEDS, National Emergency Department Sample; y, year.
Similar to that among urban residents, among rural residents, female residents had higher ED visit rates for self-harm than male residents (313.1 per 100,000 for female residents vs 195.1 per 100,000 for male residents), the rate was the highest for self-harm by poisoning, and rates declined with age. Rural adolescents aged 10–19 years showed the highest rate among all age groups of both settings (Figure 1).
DISCUSSION
Rural residents experienced higher rates of ED visits for nonfatal self-harm than urban residents for all individuals aged <65 years and by all mechanisms. In complement to the current understanding of the national rural–urban gap based on suicide data,2 this study provided additional information to facilitate prevention efforts in reducing rural–urban disparities in nonfatal suicidal behavior. This study also showed using a large ED database as a viable option to study suicidal behavior for rural populations, especially if suicide counts are small.
Previous studies suggest unique risk factors among rural residents that may contribute to their increased risk for suicidal behavior, such as social isolation, lack of access to healthcare services, economic hardship, stigma around help seeking for mental health problems, and cultural and social beliefs encouraging self-sufficiency.7,8 Furthermore, on the basis of suicide data, using a firearm was identified as an important contributor to the rural–urban suicide gap.9 Firearm was the leading mechanism used for suicide among rural residents, with the firearm-related suicide rate more than 50% higher in rural areas than in urban areas.3 Conversely, given the high lethality of firearms,5 using a firearm was not common and only accounted for <2% of nonfatal self-harm cases in this study. Therefore, reducing access to lethal means among people at risk of suicide may help to reduce the rural–urban gap in suicide rates,8,9 although additional strategies are needed to prevent nonfatal self-harm. The findings on the rural–urban gaps in self-harm by all mechanisms shown in this study underscore the importance of comprehensive primary suicide prevention strategies to address upstream risk factors in reducing the rural–urban disparity. As documented in detail in the Centers for Disease Control and Prevention’s suicide prevention technical package, these evidence-based strategies may include strengthening social connectedness, promoting social norms that view help seeking as a sign of strength, increasing access to care, and strengthening economic supports.10 It is noteworthy that for people aged ≥65 years, no rural–urban difference in nonfatal self-harm was found in this study, whereas there is a well-documented rural–urban gap in suicide.2 For this age group, because the rural–urban disparity was mainly observed in suicides, strategies targeting to prevent suicide such as reducing access to lethal means among at-risk individuals may make a large difference in mitigating the rural–urban disparity.
Limitations
This study is subject to some limitations. The findings on self-harm ED visits may not be generalized to all self-harm cases, about half of whom did not seek care.11 There were possible misclassifications of self-harm cases as unintentional or undetermined injuries that could not be accounted for.12 Self-harm may be suicidal or nonsuicidal in nature, but using ICD-10-CM diagnosis codes did not allow the authors to define suicidal intent for self-harm. Nevertheless, both suicidal and nonsuicidal self-harm behaviors are risk factors for suicide and need to be prevented.13 Because race/ethnicity is not available in NEDS, potential modification by race/ethnicity on the rural–urban self-harm disparity as suggested in a previous study was not evaluated in this study.14
CONCLUSIONS
This study suggests that comprehensive prevention strategies tailored to rural locations and circumstances are essential for mitigating the rural–urban inequities in nonfatal self-harm.
ACKNOWLEDGMENTS
We would like to thank Tracey Foster-Butler from National Center for Injury Prevention and Control, Centers for Disease Control and Prevention for editing the manuscript.
The authors confirm that this manuscript has not been published previously and is not under consideration in any other peer-reviewed media.
No financial disclosures were reported by the authors of this paper.
Footnotes
CREDIT AUTHOR STATEMENT
Jing Wang: Conceptualization, Data curation, Formal Analysis, Methodology, Writing - Original Draft, Writing - Review & Editing. Melissa M. Brown: Writing - Original Draft, Writing - Review & Editing. Asha Z. Ivey-Stephenson: Writing - Original Draft, Writing - Review & Editing. Likang Xu: Data Curation, Methodology, Validation, Writing - Review & Editing. Deborah M Stone: Conceptualization, Writing - original draft, Writing - review & editing, Supervision.
REFERENCES
- 1.Kochanek KD, Xu JQ. Arias E. Mortality in the United States, 2019. NCHS Data Brief. 2020;395(395):1–8. https://www.cdc.gov/nchs/data/databriefs/db395-H.pdf. Accessed November 19, 2021. [PubMed] [Google Scholar]
- 2.Ivey-Stephenson AZ, Crosby AE, Jack SPD, Haileyesus T, Kresnow-Sedacca MJ. Suicide trends among and within urbanization levels by sex, race/ethnicity, age group, and mechanism of death - United States, 2001–2015. MMWR Surveill Summ. 2017;66(18):1–16. 10.15585/mmwr.ss6618a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pettrone K, Curtin SC. Urban–rural differences in suicide rates, by sex and three leading methods: United States, 2000–2018. NCHS Data Brief. 2020;373(373):1–8. https://www.cdc.gov/nchs/products/databriefs/db373.htm. Accessed March 1, 2022. [PubMed] [Google Scholar]
- 4.Center for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-Based Injury Statistics Query and Reporting System (WISQARS). Atlanta, GA: Centers for Disease Control and Prevention; 2021. https://www.cdc.gov/injury/wisqars/index.html. Updated December 2. Accessed January 14, 2022. [Google Scholar]
- 5.Wang J, Sumner SA, Simon TR, et al. Trends in the incidence and lethality of suicidal acts in the United States, 2006 to 2015. JAMA Psychiatry. 2020;77(7):684–693. 10.1001/jamapsychiatry.2020.0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rao CR. Linear Statistical Inference and Its Applications. 2nd ed. New York, NY: John Wiley & Sons, 1973. [Google Scholar]
- 7.Hirsch JK, Cukrowicz KC. Suicide in rural areas: an updated review of the literature. J Rural Ment Health. 2014;38(2):65–78. 10.1037/rmh0000018. [DOI] [Google Scholar]
- 8.Mohatt NV, Kreisel CJ, Hoffberg AS, Wendleton L, Beehler SJ. A systematic review of factors impacting suicide risk among rural adults in the United States. J Rural Health. 2021;37(3):565–575. 10.1111/jrh.12532. [DOI] [PubMed] [Google Scholar]
- 9.Nestadt PS, Triplett P, Fowler DR, Mojtabai R. Urban-rural differences in suicide in the State of Maryland: the role of firearms. Am J Public Health. 2017;107(10):1548–1553. 10.2105/AJPH.2017.303865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stone D, Holland K, Bartholow B, Crosby A, Davis S, Wilkins N. Preventing suicide: a technical package of policies, programs, and practices. Atlanta, GA: National Center for Injury Prevention and ControlCenters for Disease Control and Prevention; 2017. https://www.cdc.gov/violenceprevention/pdf/suicidetechnicalpackage.pdf. Accessed November 19, 2021. [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2019 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020. (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55) https://www.samhsa.gov/data/. Published Accessed January 11, 2022. [Google Scholar]
- 12.Cwik JC, Teismann T. Misclassification of self-directed violence. Clin Psychol Psychother. 2017;24(3):677–686. 10.1002/cpp.2036. [DOI] [PubMed] [Google Scholar]
- 13.Office of the Surgeon General (U.S.), National Action Alliance for Suicide Prevention (U.S.). 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action: A Report of the U.S. Surgeon General and of the National Action Alliance for Suicide Prevention. Washington, DC: HHS; 2012. https://www.ncbi.nlm.nih.gov/books/NBK109917/. Accessed November 19, 2021. [Google Scholar]
- 14.Peltzman T, Gottlieb DJ, Levis M, Shiner B. The role of race in rural-urban suicide disparities. J Rural Health. 2021. In press. Online June 15. 10.1111/jrh.12603. [DOI] [PubMed] [Google Scholar]


