Abstract
Background
Anterior cruciate ligament (ACL) injury is extremely common among athletes. Rate of second ACL injury due to surgical graft rupture or contralateral limb ACL injury is approximately 15-32%. Psychological readiness to return to sport (RTS) may be an important predictor of successful RTS outcomes. Psychological readiness can be quantified using the ACL Return to Sport after Injury (ACL-RSI) questionnaire, with higher scores demonstrating greater psychological readiness.
Purpose
The purpose of this study was to investigate differences in functional performance and psychological readiness to return to sport among athletes who have undergone primary ACL reconstruction (ACLR).
Study Design
Descriptive cohort study
Methods
Eighteen athletes who had undergone primary ACLR were tested at time of RTS clearance. The cohort was divided into two groups, high score (HS) and low score (LS), based on median ACL-RSI score, and performance on static and dynamic postural stability testing, lower extremity isokinetic and isometric strength testing, and single leg hop testing was compared between the groups using an independent samples t-test.
Results
The median ACL-RSI score was 74.17. The average ACL-RSI score was 83.1±6.2 for the HS group and 61.8±8.0 for the LS group. High scorers on the ACL-RSI performed significantly better on isometric knee flexion as measured via handheld dynamometry (22.61% ±6.01 vs. 12.12% ±4.88, p=0.001) than the low score group.
Conclusion
The findings suggest that increased knee flexion strength may be important for psychological readiness to RTS after primary ACLR. Further research is indicated to explore this relationship, however, a continued emphasis on improving hamstring strength may be appropriate during rehabilitation following ACLR to positively impact psychological readiness for RTS.
Level of Evidence
III
Keywords: anterior cruciate ligament reconstruction, psychological readiness, return to sport
INTRODUCTION
Anterior cruciate ligament (ACL) injury is common among athletes.1,2 Rate of second injury due to surgical graft rupture or contralateral limb injury is approximately 15-32%, with increased risk during the first two years postoperatively.3–7 Known factors associated with successful return to sport (RTS) include delay of return until at least nine months postoperatively, symmetric quadriceps strength measured as a ratio of knee extensor torque normalized to body mass, lower levels of pain and knee joint effusion, lower levels of kinesiophobia, and extended preoperative rehabilitation.4,6,8–10 Successful return to sport is primarily defined as avoidance of second injury, but can also include return to pre-injury activity levels or avoidance of pain with activity. Despite the identification of these predictors, ACL reinjury rates remain high, suggesting that other factors may play an important role in successful RTS. One of these additional factors may be psychological readiness to RTS, which includes fear of reinjury, anxiety, anger, and stress, and lack of confidence to return to sport.11 Approximately 40-63% of athletes return to their preinjury level of sport after primary ACL injury,12–14 and among athletes who do not return, fear of injury is the most common reason they cite for this decision.15 Lack of psychological readiness is a major barrier for return to preinjury level of sport after ACL reconstruction (ACLR).13,16–18 Psychological factors, in addition to physical readiness, are important to consider in RTS evaluation.8,11,15
Several authors have indicated that psychological readiness predicts successful RTS.13,14,19–23 Psychological readiness to return to sport may be quantified using a questionnaire known as the ACL Return to Sport after Injury (ACL-RSI) scale.24 Webster et al. developed this 12-item questionnaire in 2008 to assess the psychological impact of returning to sport after ACLR.10,24 The scale measures psychological readiness to RTS after an ACL injury in three main categories: emotions, confidence, and risk appraisal, and a higher score suggests greater psychological readiness for return to sport.21,24,25 The ACL-RSI has been shown to be a good indicator of successful RTS.10,11,23 Sadeqi et al. describes that ACL-RSI score improves throughout the rehabilitation process, and that higher ACL-RSI score is correlated with an athlete’s return to sport.25 Athletes who return to sport after ACLR have higher ACL-RSI scores than athletes who do not return to their sport even after being medically cleared to do so.10,13 Importantly, young athletes (<20 years of age) who sustain a second ACL injury after RTS had lower psychological readiness scores at 12 months after ACLR and a smaller change in their ACL-RSI score from preoperative evaluation to 12 months postoperative evaluation than their counterparts who do not sustain a second injury.21,22 ACL-RSI score indicates psychological readiness for successful RTS, and therefore may be a useful tool in RTS evaluations for athletes.
Although there is strong evidence demonstrating that psychological readiness plays a significant role in successful RTS, the predictors of psychological readiness remain largely unknown. The purpose of this study was to investigate differences in functional performance and psychological readiness to return to sport among athletes who have undergone primary ACLR. Predictors of high ACL-RSI scores will be determined based on single leg functional performance in single leg hop for distance, quadriceps strength testing, and single leg static postural stability and Dynamic Postural Stability Index (DPSI). Because athletes with higher ACL-RSI scores are shown to have greater success in RTS, it was hypothesized that subjects in this study with higher ACL-RSI scores will perform better in functional testing at time of RTS than athletes with lower ACL-RSI scores. Findings from this study may guide clinicians when determining how psychological factors contribute to functional performance. These results may also affect both physical and psychological rehabilitation for athletes after ACLR to improve RTS outcomes.
METHODS
Study design and participants
This descriptive cohort study utilized individuals who had undergone a primary ACLR at a single academic institution. Subjects were recruited to participate if they were 12 years or older and had undergone primary ACL reconstruction with a contributing author orthopaedic surgeon. A total of 18 participants enrolled in the study voluntarily. All subjects were cleared by their orthopaedic surgeon to return to their previous level of activity prior to participation in the study.
Subjects were included in this study if they participated in a sport at any level prior to their injury, and intended to return back to sport after being cleared to do so. Subjects were excluded if they had a history of any prior major lower extremity injuries, prior lower extremity or back surgery, any medical diagnosis that could affect balance, or any multi-ligamentous injury. Concurrent meniscal injury was not an exclusion criterion. Subject demographics for the cohort are outlined in Table 1. All subjects read and signed an informed consent form prior to participating in the study.
Table 1. Participant demographics.
| Age (years) Range: 13-36 |
Height (cm) | Mass (kg) | Tegner Activity Level | ||||||||
| Mean | ±SD | Mean | ±SD | Mean | ±SD | Mean | ±SD | ||||
| Females (n=8) | 19.4 | 5.73 | 165.88 | 7.38 | 76.33 | 25.82 | 6.75 | 1.58 | |||
| Males (n=10) | 20.8 | 7.04 | 178.97 | 8.02 | 76.89 | 10.74 | 7.70 | 1.25 | |||
| Total (n=18) | 20.2 | 6.35 | 173.15 | 10.06 | 76.64 | 18.32 | 7.28 | 1.44 | |||
Instrumentation
Ground reaction forces (GRF) for static and dynamic postural stability testing were collected at 1000 Hz with an AMTI force plate (Advanced Mechanical Technologies, Inc., Watertown, MA, model BP600900). Knee isokinetic strength was measured using an isokinetic dynamometer (Biodex Medical Systems, Inc., Shirley, NY), and knee isometric strength was measured using a handheld dynamometer (Lafayette Instrument Company, Lafayette, IN).
Procedures
Participants completed the ACL Return to Sport after Injury (ACL-RSI) 12-item questionnaire at time of RTS clearance, as previously described. Several studies have used the ACL-RSI, and the questionnaire shows high internal consistency (Cronbach alpha = 0.96).14,15,20,21,23,26–28
Subjects also completed the Tegner Activity Scale prior to functional performance testing. The Tegner Activity Scale is a scored assessment from zero to ten that assesses the activity level in daily life and sport or recreation that a participant can comfortably complete.29–31 Participants may only achieve a score of five or greater if they participate in recreational or competitive sports.29 The activity scale has been shown to have high test-retest reliability.29,31 Average Tegner Activity Level for the cohort at time of RTS testing is reported in Table 1.
Static postural stability testing was assessed under eyes open (EO) and eyes closed (EC) conditions. Participants assumed a single-leg stance on their injured leg on the force plate with their hands on their hips and were asked to focus on a marker at eye level approximately ten feet in front of them for a total of ten seconds in EO condition. Subjects assumed the same stance with their eyes closed for EC condition. Subjects completed one practice trial for each condition before three ten second trials were collected for data analysis. Trials were repeated if the subject shifted their standing foot on the force plate or touched down with their opposite foot off of the force plate. This protocol has been previously described and found to have excellent inter-session reliability.32–37 The standard deviation of the GRF were calculated for each trial in the anterior-posterior, medial-lateral, and vertical directions. In addition, an overall composite GRF was calculated for each trial. These values were averaged across the three trials for the eyes open and eyes closed conditions following data reduction.
For dynamic postural stability testing, participants were instructed to jump forward from a two-legged stance over a 30.5 cm hurdle to a force plate that was positioned at a distance of 40% of their height. Subjects were asked to land on their injured leg on the force plate and hold the stance for at least five seconds after landing. Trials were discarded if the subject did not land with one foot entirely on the force plate or if they were unable to hold a single leg stance after landing for at least five seconds. This procedure has been previously described in the literature and has good inter-session reliability.8,35–39 The dynamic postural stability index (DPSI) for each GRF component was calculated for the anterior-posterior, medial-lateral, and vertical directions, as well as an overall composite index following data reduction.40
Knee strength was first assessed using an isokinetic dynamometer with concentric testing at 60° per second. Subjects were positioned on the isokinetic dynamometer according to manufacturer specifications. Participants were tested for average peak torque for knee flexion and knee extension. Strength was tested on the injured limb. Subjects performed three practice trials of knee flexion and extension at 50% of their maximum strength, followed by three practice trials at maximum strength. Following one minute of rest, participants proceeded with five consecutive repetitions of flexion and extension at maximum strength. This protocol has been previously described in the literature, and has been shown to have good between-group and side-to-side reliability.34,41 Average peak torque for knee flexion and knee extension were calculated and normalized to body mass in kilograms.
A handheld dynamometer was also used to assess isometric knee flexion and extension strength. For knee flexion testing, participants were in the prone position on an exam table with their injured knee in 30-45° of flexion. The subject then accelerated into full flexion strength while the examiner resisted the subject’s flexion using a handheld dynamometer placed on the distal one-third of the calf. For knee extension, participants sat on the edge of the exam table with their legs hanging off in 30-45° of flexion. Using a gait belt strap, the dynamometer was secured on the distal one-third of the tibia of the injured leg, participants accelerated into maximum extension. Each trial with the handheld dynamometer was repeated three times. Handheld dynamometry has been previously described and validated for intra-rater, inter-rater, and inter-device reliability, especially for proximal muscle testing.42–44 Peak force was averaged over the three trials and normalized to body mass in kilograms. One tester performed all of the handheld strength testing. Intra-rater reliability of this tester using the protocol employed in the current study was 0.94 or greater.
Hop distance was assessed for both triple hop and crossover hop. For each hop test, individuals were asked to complete three consecutive hops on the affected foot, jumping as far as possible along a ¾” tape measure on the ground. For the triple hop, all three jumps were made on the same side of a tape measure secured to the floor. For the crossover hop, participants alternated on which side of the tape they jumped with each hop in a lateral-medial-lateral pattern. Trials were discarded if participants landed on the tape or if participants did not stick the landing on their final hop. This procedure has been described previously,45,46 with intraclass correlation coefficients of 0.82-0.93.47 Participants performed a practice trial for each hop test, and data were recorded for two test trials, with the results averaged and normalized to the participant’s height in centimeters.
Data Reduction
Custom MATLAB (Mathworks, v7.0.4, Natick, MA) scripts were used for filtering and processing data for static and dynamic postural stability testing. The data was filtered with a low-pass Butterworth filter using a cutoff frequency of 20 Hz. For static postural stability, the GRF from each of the three successful trials were normalized to body mass in kilograms and averaged. The standard deviation of the GRF in the anterior-posterior, medial-lateral, and vertical directions were calculated, as well as a combined measure from all three directions. For dynamic postural stability, a stability index in the anterior-posterior, medial-lateral, and vertical directions was calculated, in addition to a composite score from all three directions. These values were calculated using the first three seconds after initial contact on the force plate, as determined by the time in which vertical GRF was recorded at greater than five percent of the subject’s body mass. The calculations are based on a mean square standardization around a zero point, with lower values for all variables indicating a better score.39
Statistical analysis
The median ACL-RSI score was calculated across the cohort. Participants were divided into two groups of equal participants based on the median score. Groups were designated as “high score” or “low score” ACL-RSI group, relative to the median.
The data for each variable (height, mass, age, ACL-RSI score, time to RTS, static and dynamic postural stability testing, isokinetic knee flexion/extension, isometric knee flexion/extension, triple/crossover hop) was assessed for normality using a Shapiro-Wilk test. Trial data from the participant’s injured limb was assessed. Data from the non-injured limb was not included in this study. An independent samples t-test was used to compare the functional performance, strength, and postural stability testing between the high and low score ACL-RSI groups for each variable, and a Mann-Whitney U test was used if the data did not meet normality criteria. All statistical analysis was performed using IBM SPSS Statistics (IBM SPSS, Version 24). Statistical significance was set a priori at p < 0.05.
RESULTS
The Shapiro-Wilk normality test showed that the data was normally distributed for all variables tested except for age. There was no significant difference in age between the two groups (mean age 18.67±5.17 years and median 17 years in the high-score ACL-RSI group vs. mean age 21.67±7.33 years and median age 18 in the low-score ACL-RSI group, p=0.331). The height, body mass, and age demographics between the two groups are presented in Table 2.
Table 2. ACL-RSI Group demographics.
| HS Group (n= 9) | LS Group (n = 9) | p-value | |||||
| Mean | ± SD | Mean | ± SD | ||||
| Height (cm) | 176.43 | 10.77 | 169.87 | 8.66 | 0.173 | ||
| Mass (kg) | 74.48 | 11.68 | 78.80 | 23.80 | 0.631 | ||
| Age (yrs) | 18.67 | 5.17 | 21.67 | 7.33 | 0.331 | ||
| ACL-RSI Score | 83.06 | 6.22 | 61.76 | 8.00 | <0.0001* | ||
| Mean time to RTS clearance (months) | 8.74 | 1.54 | 9.50 | 2.75 | 0.475 | ||
*denotes statistically significant difference
HS= high score ACL-RSI group, LS = low score ACL-RSI group
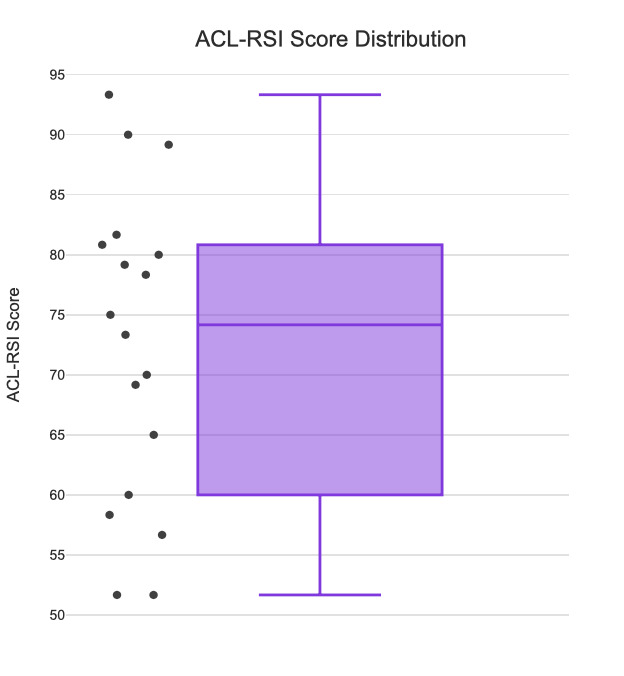
The median ACL-RSI score was 74.17. The average ACL-RSI score was 83.1±6.2 for the “high score” group (HS) and 61.8±8.0 for the “low score” group (LS). There was a significant difference in ACL-RSI score between groups (HS= 83.06, LS=61.76, p<0.001). The distribution of scores is shown in Figure 1.
Figure 1. Distribution of ACL-RSI scores.
The means, standard deviations, and p-values for the HS and LS group for static and dynamic postural stability tasks are presented in Table 3. None of the comparisons between groups achieved statistical significance. The means, standard deviations, and p-values between groups for strength testing are presented in Table 4. High scorers on the ACL-RSI had statistically significant greater isometric knee flexion strength normalized to body mass as measured via handheld dynamometry (36.6±11.4 vs. 32.9±11.8, p=0.001). There were no other statistically significant findings in isometric and isokinetic strength testing. The means, standard deviations, and p-values for hop testing between groups are presented in Table 5. There were no statistically significant differences in performance between the HS and LS groups for hop testing.
Table 3. Static and dynamic postural stability testing.
| HS Group (n= 9) | LS Group (n = 9) | p-value | |||||
| Mean | ± SD | Mean | ± SD | ||||
| Static Balance GRF - AP, EO | 2.68 | 0.73 | 2.71 | 1.10 | 0.947 | ||
| Static Balance GRF - ML, EO | 3.53 | 1.29 | 3.53 | 1.73 | 0.993 | ||
| Static Balance GRF - V, EO | 5.64 | 1.68 | 5.17 | 2.34 | 0.630 | ||
| Static Balance GRF - Combined, EO | 7.20 | 2.15 | 6.85 | 3.05 | 0.780 | ||
| Static Balance GRF - AP, EC | 5.33 | 1.53 | 6.29 | 4.02 | 0.510 | ||
| Static Balance GRF - ML, EC | 9.09 | 4.39 | 10.80 | 7.02 | 0.545 | ||
| Static Balance GRF - V, EC | 12.48 | 5.09 | 12.85 | 7.02 | 0.898 | ||
| Static Balance GRF - Combined, EC | 16.42 | 6.65 | 17.99 | 10.59 | 0.711 | ||
| DPSI | 0.35 | 0.05 | 0.36 | 0.04 | 0.479 | ||
| APSI | 0.14 | 0.01 | 0.14 | 0.01 | 0.303 | ||
| MLSI | 0.03 | 0.00 | 0.03 | 0.01 | 0.950 | ||
| VSI | 0.32 | 0.05 | 0.33 | 0.04 | 0.505 | ||
GRF= ground reaction forces, EO= eyes open, EC = eyes closed, AP= anterior-posterior, ML= medial-lateral, V= vertical, HS= high score ACL-RSI group, LS = low score ACL-RSI group
Table 4. Strength testing.
| HS Group (n= 9) | LS Group (n = 9) | p-value | |||||
| Mean | ± SD | Mean | ± SD | ||||
| Isokinetic Knee flexion avg peak torque/ BM *100 | 124.98% | 25.87 | 102.03% | 46.49 | 0.214 | ||
| Isokinetic Knee extension avg peak torque / BM * 100 | 189.06% | 45.63 | 192.68% | 67.99 | 0.896 | ||
| Handheld dynamometry knee flexion avg peak force/ BM * 100 | 22.61% | 6.01 | 12.12% | 4.88 | 0.001* | ||
| Handheld dynamometry knee extension avg peak force/ BM *100 | 36.55% | 11.37 | 32.90% | 11.82 | 0.528 | ||
*denotes statistical significance
HS= high score ACL-RSI group, LS = low score ACL-RSI group, BM = body mass (kg)
Table 5. Hop testing.
| HS Group (n= 9) | LS Group (n = 9) | p-value | |||||
| Mean | ± SD | Mean | ± SD | ||||
| Triple hop distance / height | 265.19 | 55.65 | 209.74 | 65.66 | 0.071 | ||
| Crossover hop distance / height | 238.94 | 54.17 | 187.58 | 73.91 | 0.112 | ||
HS= high score ACL-RSI group, LS = low score ACL-RSI group
DISCUSSION
The purpose of this study was to evaluate if greater psychological readiness for RTS was associated with better performance on strength, postural stability, and hop testing at time of RTS clearance among athletes who had undergone primary ACL reconstruction. It was hypothesized that participants with greater psychological readiness, as determined by ACL-RSI score, would have greater strength, static and dynamic postural stability, and greater hop distance than participants with lower ACL-RSI scores. The hypothesis was partially supported by the finding that participants with greater psychological readiness for RTS had greater mean isometric knee flexor strength. However, no other statistically significant differences were found between groups in any other performance test measured.
Both psychological readiness to RTS and return of knee flexor strength have been shown to be an important predictor of successful RTS outcomes. Athletes with greater ACL-RSI scores, a marker of psychological readiness, are more likely to return to sport after injury recovery.13,25 Further, athletes with lower ACL-RSI scores and a smaller improvement in ACL-RSI score throughout postoperative rehabilitation are more likely to experience a second ACL injury upon returning to sport.21 Knee flexor strength deficits after ACLR have been associated with an increased second injury risk.48,49
Previous studies have also identified relationships between strength and functional performance testing with psychological readiness to return to sport. Paterno et al identified that athletes with greater fear, a component of psychological readiness, were less likely to return to previous levels of activity and were more likely to have isometric knee extensor strength asymmetry and hop testing asymmetry between legs at time of RTS, and were more likely to experience second ACL injuries.50 Lepley et al. observed that lower levels of presurgical pain and greater knee extensor strength in both the injured and uninjured limbs at time of RTS clearance were associated with greater psychological readiness to return to sport.27 Burland et al found that greater isometric and isokinetic extensor strength were associated with higher ACL-RSI scores at three and six months postoperative in adolescent patients.26 Meierbachtol et al. and Muller et al. found a positive correlation between ACL-RSI score and triple hop for distance.20,28
The time before recovery of static and postural stability skill after ACLR remains controversial,51–54 but has been shown to improve upon training and is often trained in postoperative rehabilitation programs.55–58 Balance deficits may persist six months to three years after ACL injury.54 It is possible that no difference was observed between the high and low score groups on static and postural stability testing because all athletes had been exposed to balance testing throughout rehabilitation and had adequately recovered their balance at time of return to sport testing.
There are several limitations to this study. First, there was a relatively small enrollment size. Generalization of these findings should be done with caution, given the small sample size and small age range of athletes enrolled. Participants volunteered to enroll in the study, so enrollment was limited by their willingness to complete testing leading to selection bias. Additionally, the type of surgical graft used intraoperatively, and postoperative rehabilitation programs were not controlled among participants. Athletes may have exhibited reduced hamstring strength if they received a hamstring autograft, which would be unrelated to psychological readiness. Graft type for each participant was not recorded for this study, therefore we were unable to stratify results based on this finding. Postoperative rehabilitation protocols are not standardized after ACLR,57,59,60 which could contribute to varying levels of familiarity or preparation for the test battery used in this study. However, because participants were tested after RTS clearance by their clinicians, it is assumed that all subjects had demonstrated some level of competency with strength, balance, and functional performance testing prior to enrollment in this study.
CONCLUSION
This study demonstrated an association between greater isometric knee flexor strength and ACL-RSI score, a surrogate of psychological readiness to RTS, partially supporting the hypothesis. We found no association between greater psychological readiness to RTS and knee extensor strength, static or dynamic postural stability, or hop testing among the cohort. Findings from this study indicate that improving hamstring strength may contribute to greater psychological readiness to return to sport, both of which may help reduce second ACL injury rates. Given that psychological readiness has been shown to be related to successful RTS outcomes and lower second injury rates, future research should explore ways to train and optimize psychological readiness in additional to functional strength prior to an athlete’s return to sport.
Conflicts of interest and financial disclosures
None
IRB Protocol
Pro00088033 DUHS IRB
References
- Sanders Thomas L., Maradit Kremers Hilal, Bryan Andrew J., Larson Dirk R., Dahm Diane L., Levy Bruce A., Stuart Michael J., Krych Aaron J. The American Journal of Sports Medicine. 6. Vol. 44. SAGE Publications; Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study; pp. 1502–1507. [DOI] [PubMed] [Google Scholar]
- Mall Nathan A., Chalmers Peter N., Moric Mario, Tanaka Miho J., Cole Brian J., Bach Bernard R. Jr, Paletta George A. Jr. The American Journal of Sports Medicine. 10. Vol. 42. SAGE Publications; Incidence and trends of anterior cruciate ligament reconstruction in the United States; pp. 2363–2370. [DOI] [PubMed] [Google Scholar]
- Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Wiggins M.E., Fadale P., Barrach H., Ehrlich M., WW 2016Am J Sport Med. 44(7):1861–1876. doi: 10.1177/0363546515621554.Risk. doi: 10.1177/0363546515621554.Risk. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Return to preinjury sports participation following anterior cruciate ligament reconstruction: Contributions of demographic, knee impairment, and self-report measures. Lentz Trevor A., Zeppieri Giorgio, Jr., Tillman Susan M., Indelicato Peter A., Moser Michael W., George Steven Z., Chmielewski Terese L. Nov;2012 Journal of Orthopaedic & Sports Physical Therapy. 42(11):893–901. doi: 10.2519/jospt.2012.4077. doi: 10.2519/jospt.2012.4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan Matthew D., Salmon Lucy J., Waller Alison, Roe Justin P., Pinczewski Leo A. The American Journal of Sports Medicine. 2. Vol. 44. SAGE Publications; Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger; pp. 384–392. [DOI] [PubMed] [Google Scholar]
- Simple decision rules reduce reinjury risk after anterior cruciate ligament reconstruction: The Delaware-Oslo ACL cohort study. Grindem H., Snyder-Mackler Lynn, Moksnes H, Engebretsen L, Risberg M.A. 2016Br J Sports Med. 50(13):804–808. doi: 10.1136/bjsports-2016-096031.SIMPLE. doi: 10.1136/bjsports-2016-096031.SIMPLE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. Dekker Travis J., Godin Jonathan A., Dale Kevin M., Garrett William E., Taylor Dean C., Riboh Jonathan C. Jun 7;2017 Journal of Bone and Joint Surgery. 99(11):897–904. doi: 10.2106/jbjs.16.00758. doi: 10.2106/jbjs.16.00758. [DOI] [PubMed] [Google Scholar]
- Factors informing fear of reinjury after anterior cruciate ligament reconstruction. Ross Cheryl A., Clifford Amanda, Louw Quinette A. Jan 17;2017 Physiotherapy Theory and Practice. 33(2):103–114. doi: 10.1080/09593985.2016.1271847. doi: 10.1080/09593985.2016.1271847. [DOI] [PubMed] [Google Scholar]
- Failla Mathew J., Logerstedt David S., Grindem Hege, Axe Michael J., Risberg May Arna, Engebretsen Lars, Huston Laura J., Spindler Kurt P., Snyder-Mackler Lynn. The American Journal of Sports Medicine. 10. Vol. 44. SAGE Publications; Does extended preoperative rehabilitation influence outcomes 2 years after ACL reconstruction? pp. 2608–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Müller Ulrike, Krüger Michael, Schmidt Michael, Rosemeyer Bernd. 2015Knee Surgery, Sports Traumatology, Arthroscopy. 23(12):3623–3631. doi: 10.1007/s00167-014-3261-5. doi: 10.1007/s00167-014-3261-5. [DOI] [PubMed] [Google Scholar]
- Psychological aspects of ACL injuries. Ardern Clare L., Kvist Joanna, Webster Kate E. 2015Operative Techniques in Sports Medicine. 24(1):77–83. doi: 10.1053/j.otsm.2015.09.006. doi: 10.1053/j.otsm.2015.09.006. [DOI] [Google Scholar]
- Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Ardern C. L., Webster K. E., Taylor N. F., Feller J. A. Mar 11;2011 British Journal of Sports Medicine. 45(7):596–606. doi: 10.1136/bjsm.2010.076364. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Langford J L, Webster K E, Feller J A. 2009British Journal of Sports Medicine. 43(5):377–381. doi: 10.1136/bjsm.2007.044818. doi: 10.1136/bjsm.2007.044818. [DOI] [PubMed] [Google Scholar]
- Ardern Clare L, Österberg Annika, Tagesson Sofi, Gauffin Håkan, Webster Kate E, Kvist Joanna. British Journal of Sports Medicine. 22. Vol. 48. BMJ; The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction; pp. 1613–1619. [DOI] [PubMed] [Google Scholar]
- How much do psychological factors affect lack of return to play after anterior cruciate ligament reconstruction? A systematic review. Nwachukwu Benedict U., Adjei Joshua, Rauck Ryan C., Chahla Jorge, Okoroha Kelechi R., Verma Nikhil N., Allen Answorth A., Williams Riley J. III. May 1;2019 Orthopaedic Journal of Sports Medicine. 7(5):1–7. doi: 10.1177/2325967119845313. doi: 10.1177/2325967119845313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Factors associated with psychological readiness to return to sport after an anterior cruciate ligament reconstruction surgery. Webster K., Nagelli C., Hewett T., Feller J. 2019Am J Sports Med. 46(7):1545–1550. doi: 10.1177/0363546518773757.Factors. doi: 10.1177/0363546518773757.Factors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardern Clare L., Taylor Nicholas F., Feller Julian A., Whitehead Timothy S., Webster Kate E. The American Journal of Sports Medicine. 7. Vol. 41. SAGE Publications; Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery; pp. 1549–1558. [DOI] [PubMed] [Google Scholar]
- Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Czuppon S., Racette B., Klein S., Harris-Hayes M. 2014Br J Sport Med. 48(5):356–364. doi: 10.1136/bjsports-2012-091786.Variables. doi: 10.1136/bjsports-2012-091786.Variables. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgi Ciara R, Peters Scott, Ardern Clare L, Magill John R, Gomez Christina D, Sylvain Jonathan, Reiman Michael P. British Journal of Sports Medicine. 18. Vol. 53. BMJ; Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review; pp. 1154–1161. [DOI] [PubMed] [Google Scholar]
- Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Müller Ulrike, Krüger-Franke Michael, Schmidt Michael, Rosemeyer Bernd. 2015Knee Surgery, Sports Traumatology, Arthroscopy. 23(12):3623–3631. doi: 10.1007/s00167-014-3261-5. doi: 10.1007/s00167-014-3261-5. [DOI] [PubMed] [Google Scholar]
- Mcpherson April L., Feller Julian A., Hewett Timothy E., Webster Kate E. The American Journal of Sports Medicine. 4. Vol. 47. SAGE Publications; Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries; pp. 857–862. [DOI] [PubMed] [Google Scholar]
- Mcpherson April L., Feller Julian A., Hewett Timothy E., Webster Kate E. The American Journal of Sports Medicine. 5. Vol. 47. SAGE Publications; Smaller change in psychological readiness to return to sport is associated with second anterior cruciate ligament injury among younger patients; pp. 1209–1215. [DOI] [PubMed] [Google Scholar]
- Factors affecting subjective and objective outcomes and return to play in anterior cruciate ligament reconstruction: A retrospective cohort study. Rosso Federica, Bonasia Davide E., Cottino Umberto, Cambursano Simone, Dettoni Federico, Rossi Roberto. Mar;2018 Joints. 6(1):23–32. doi: 10.1055/s-0038-1636931. doi: 10.1055/s-0038-1636931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Webster Kate E., Feller Julian A., Lambros Christina. Feb;2008 Physical Therapy in Sport. 9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Progression of the psychological ACL-RSI score and return to sport after anterior cruciate ligament reconstruction. Sadeqi Mansour, Klouche Shahnaz, Bohu Yoann, Herman Serge, Lefevre Nicolas, Gerometta Antoine. Dec 1;2018 Orthopaedic Journal of Sports Medicine. 6(12):1–7. doi: 10.1177/2325967118812819. doi: 10.1177/2325967118812819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical outcome measures and return-to-sport timing in adolescent athletes after anterior cruciate ligament reconstruction. Burland Julie P., Kostyun Regina O., Kostyun Kyle J., Solomito Matthew, Nissen Carl, Milewski Matthew D. May 1;2018 Journal of Athletic Training. 53(5):442–451. doi: 10.4085/1062-6050-302-16. doi: 10.4085/1062-6050-302-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadriceps function, knee pain, and self-reported outcomes in patients with anterior cruciate ligament reconstruction. Lepley Adam S., Pietrosimone Brian, Cormier Marc L. Apr 1;2018 Journal of Athletic Training. 53(4):337–346. doi: 10.4085/1062-6050-245-16. doi: 10.4085/1062-6050-245-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meierbachtol Adam, Yungtum William, Paur Eric, Bottoms John, Chmielewski Terese L. Journal of Orthopaedic & Sports Physical Therapy. 11. Vol. 48. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Psychological and functional readiness for sport following advanced group training in patients with anterior cruciate ligament reconstruction; pp. 864–872. [DOI] [PubMed] [Google Scholar]
- Rating systems in the evaluation of knee ligament injuries. Tegner YELVERTON, Lysholm JACK. Sep;1985 Clinical Orthopaedics and Related Research. 198:42–49. doi: 10.1097/00003086-198509000-00007. doi: 10.1097/00003086-198509000-00007. [DOI] [PubMed] [Google Scholar]
- Briggs Karen K., Steadman J. Richard, Hay Connor J., Hines Sophia L. The American Journal of Sports Medicine. 5. Vol. 37. SAGE Publications; Lysholm score and tegner activity level in individuals with normal knees; pp. 898–901. [DOI] [PubMed] [Google Scholar]
- Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form. Collins N.J., Misra D., Felson D.T., Crossley K.M., Roos E.M. 2011Arthritis Care Res. 63(0 11):208–228. doi: 10.1002/acr.20632.Measures. doi: 10.1002/acr.20632.Measures. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steadiness in one-legged stance: development of a reliable force-platform testing procedure. Goldie Patricia A., Evans Owen M., Bach Timothy M. Apr;1992 Archives of Physical Medicine and Rehabilitation. 73(4):348–354. doi: 10.1016/0003-9993(92)90008-k. doi: 10.1016/0003-9993(92)90008-k. [DOI] [PubMed] [Google Scholar]
- Force platform measures for evaluating postural control: reliability and validity. Goldie P.A., Bach T.M., Evans O.M. 1989Arch Phys Med Rehabil. 70(7):510–517. [PubMed] [Google Scholar]
- Neuromuscular and biomechanical characteristics do not vary across the menstrual cycle. Abt John P., Sell Timothy C., Laudner Kevin G., McCrory Jean L., Loucks Tammy L., Berga Sarah L., Lephart Scott M. Mar 16;2007 Knee Surgery, Sports Traumatology, Arthroscopy. 15(7):901–907. doi: 10.1007/s00167-007-0302-3. doi: 10.1007/s00167-007-0302-3. [DOI] [PubMed] [Google Scholar]
- Gender differences in static and dynamic postural stability of soldiers in the Army’s 101st airborne division (air assault) Sell Timothy C., Lovalekar Mita T., Nagai Takashi, Wirt Michael D., Abt John P., Lephart Scott M. Mar 1;2018 Journal of Sport Rehabilitation. 27(2):126–131. doi: 10.1123/jsr.2016-0131. doi: 10.1123/jsr.2016-0131. [DOI] [PubMed] [Google Scholar]
- An examination, correlation, and comparison of static and dynamic measures of postural stability in healthy, physically active adults. Sell Timothy, House A., Abt J., Lephart S. May;2012 Physical Therapy in Sport. 13(2):80–86. doi: 10.1016/j.ptsp.2011.06.006. doi: 10.1016/j.ptsp.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Postural stability and isokinetic strength do not predict knee valgus angle during single-leg drop-landing or single-leg squat in elite male rugby union players. Akins Jonathan S., Longo Peter F., Bertoni Maurizio, Clark Nicholas C., Sell Timothy C., Galanti Giorgio, Lephart Scott M. Jan 31;2013 Isokinetics and Exercise Science. 21(1):37–46. doi: 10.3233/ies-2012-0469. doi: 10.3233/ies-2012-0469. [DOI] [Google Scholar]
- Time to Stabilization: A Method for Analyzing Dynamic Postural Stability. Ross S., Guskiewicz K. 2003Int J Athl Ther Train. 8(3):37–39. [Google Scholar]
- The addition of body amor diminishes dynamic postural stability in military soldiers. Sell Timothy C., Pederson Jonathan J., Abt John P., Nagai Takashi, Deluzio Jennifer, Wirt Michael D., McCord Larry J., Lephart Scott M. Jan;2013 Military Medicine. 178(1):76–81. doi: 10.7205/milmed-d-12-00185. doi: 10.7205/milmed-d-12-00185. [DOI] [PubMed] [Google Scholar]
- A new force-plate technology measure of dynamic postural stability: The dynamic postural stability index. Wikstrom E.A., Tillman M.D., Smith A.N., Borsa P.A. 2005J Athl Train. 40(4):305–309. [PMC free article] [PubMed] [Google Scholar]
- Isokinetic strength of fully operational U.S. Navy Seals with a previous history of shoulder and knee injury. Sell Timothy C., Clark Nicholas C., Abt John P., Lovalekar Mita, Lephart Scott M. Nov 28;2016 Isokinetics and Exercise Science. 24(4):349–356. doi: 10.3233/ies-160637. doi: 10.3233/ies-160637. [DOI] [Google Scholar]
- Intrarater reliability of hand held dynamometry in measuring lower extremity isometric strength using a portable stabilization device. Jackson Steven M., Cheng M. Samuel, Smith A. Russell, Jr., Kolber Morey J. Feb;2017 Musculoskeletal Science and Practice. 27:137–141. doi: 10.1016/j.math.2016.07.010. doi: 10.1016/j.math.2016.07.010. [DOI] [PubMed] [Google Scholar]
- Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: A reliability and validity study. Mentiplay Benjamin F., Perraton Luke G., Bower Kelly J., Adair Brooke, Pua Yong-Hao, Williams Gavin P., McGaw Rebekah, Clark Ross A. Oct 28;2015 PLoS One. 10(10):1–19. doi: 10.1371/journal.pone.0140822. doi: 10.1371/journal.pone.0140822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isometric muscle strength in youth assessed by hand-held dynamometry: A feasibility, reliability, and validity study: A feasibility, reliability, and validity study. Hébert Luc J., Maltais Désirée B., Lepage Céline, Saulnier Joanne, Crête Mélanie, Perron Marc. 2011Pediatric Physical Therapy. 23(3):289–299. doi: 10.1097/pep.0b013e318227ccff. doi: 10.1097/pep.0b013e318227ccff. [DOI] [PubMed] [Google Scholar]
- Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. Noyes F R, Butler D L, Grood E S, Zernicke R F, Hefzy M S. Mar;1984 The Journal of Bone & Joint Surgery. 66-A(3):344–352. doi: 10.2106/00004623-198466030-00005. doi: 10.2106/00004623-198466030-00005. [DOI] [PubMed] [Google Scholar]
- Haitz Karyn, Shultz Rebecca, Hodgins Melissa, Matheson Gordon O. Journal of Orthopaedic & Sports Physical Therapy. 12. Vol. 44. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Test-retest and interrater reliability of the functional lower extremity evaluation; pp. 947–954. [DOI] [PubMed] [Google Scholar]
- Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Reid Andrea, Birmingham Trevor B, Stratford Paul W, Alcock Greg K, Giffin J Robert. Mar 1;2007 Physical Therapy. 87(3):337–349. doi: 10.2522/ptj.20060143. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- Griffin Letha Y., Albohm Marjorie J., Arendt Elizabeth A., Bahr Roald, Beynnon Bruce D., DeMaio Marlene, Dick Randall W., Engebretsen Lars, Garrett William E., Hannafin Jo A., Hewett Tim E., Huston Laura J., Ireland Mary Lloyd, Johnson Robert J., Lephart Scott, Mandelbaum Bert R., Mann Barton J., Marks Paul H., Marshall Stephen W., Myklebust Grethe, Noyes Frank R., Powers Christopher, Shields Clarence Jr, Shultz Sandra J., Silvers Holly, Slauterbeck James, Taylor Dean C., Teitz Carol C., Wojtys Edward M., Yu Bing. The American Journal of Sports Medicine. 9. Vol. 34. SAGE Publications; Understanding and preventing noncontact anterior cruciate ligament injuries: A review of the Hunt Valley II Meeting, January 2005; pp. 1512–1532. [DOI] [PubMed] [Google Scholar]
- Kellis Eleftherios, Galanis Nikiforos, Kofotolis Nikolaos. Sports. 10. Vol. 7. MDPI AG; Hamstring-to-quadriceps ratio in female athletes with a previous hamstring injury, anterior cruciate ligament reconstruction, and controls; p. 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Paterno Mark V., Flynn Kaitlyn, Thomas Staci, Schmitt Laura C. 2018Sports Health: A Multidisciplinary Approach. 10(3):228–233. doi: 10.1177/1941738117745806. doi: 10.1177/1941738117745806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdowsi Forough, Rezaeian Zahra Sadat. Journal of Physical Therapy Science. 5. Vol. 30. Society of Physical Therapy Science; Evaluating equilibrium in anterior cruciate ligament reconstruction; pp. 726–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proprioceptive sensitivity and performance in anterior cruciate ligament-deficient knee joints. Fischer-Rasmussen T., Jensen P. E. Apr;2000 Scandinavian Journal of Medicine & Science in Sports. 10(2):85–89. doi: 10.1034/j.1600-0838.2000.010002085.x. doi: 10.1034/j.1600-0838.2000.010002085.x. [DOI] [PubMed] [Google Scholar]
- Clagg Sarah, Paterno Mark V., Hewett Timothy E., Schmitt Laura C. Journal of Orthopaedic & Sports Physical Therapy. 6. Vol. 45. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Performance on the modified star excursion balance test at the time of return to sport following anterior cruciate ligament reconstruction; pp. 444–452. [DOI] [PubMed] [Google Scholar]
- Lower limb kinematics and dynamic postural stability in anterior cruciate ligament-reconstructed female athletes. Delahunt Eamonn, Chawke Mark, Kelleher Judy, Murphy Katie, Prendiville Anna, Sweeny Lauren, Patterson Matt. Mar 1;2013 Journal of Athletic Training. 48(2):172–185. doi: 10.4085/1062-6050-48.2.05. doi: 10.4085/1062-6050-48.2.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapid and specific gray matter changes in M1 induced by balance training. Taubert Marco, Mehnert Jan, Pleger Burkhard, Villringer Arno. Jun;2016 Neuroimage. 133:399–407. doi: 10.1016/j.neuroimage.2016.03.017. doi: 10.1016/j.neuroimage.2016.03.017. [DOI] [PubMed] [Google Scholar]
- Y Balance TestTM anterior reach symmetry at three months is related to single leg functional performance at time of return to sports following anterior cruciate oigament reconstruction. Garrison J.C., Bothwell J.M., Wolf G., Aryal S., Thigpen C.A. 2015Int J Sports Phys Ther. 10(5):602–611. [PMC free article] [PubMed] [Google Scholar]
- Principles of postoperative anterior cruciate ligament rehabilitation. Saka Tolga. 2014World Journal of Orthopedics. 5(4):450–459. doi: 10.5312/wjo.v5.i4.450. doi: 10.5312/wjo.v5.i4.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ACL Rehabilitation progression: where are we now? Cavanaugh John T., Powers Matthew. Aug 8;2017 Current Reviews in Musculoskeletal Medicine. 10(3):289–296. doi: 10.1007/s12178-017-9426-3. doi: 10.1007/s12178-017-9426-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoneau Guy G., Wilk Kevin E. Journal of Orthopaedic & Sports Physical Therapy. 4. Vol. 42. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); The challenge of return to sports for patients post-ACL reconstruction; pp. 300–301. [DOI] [PubMed] [Google Scholar]
- A systematic review of anterior cruciate ligament reconstruction rehabilitation part II: open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. Wright Rick, Preston Emily, Fleming Braden, Amendola Annunziato, Andrish Jack, Bergfeld John, Dunn Warren, Kaeding Chris, Kuhn John, Marx Robert, McCarty Eric, Parker Richard, Spindler Kurt, Wolcott Michelle, Wolf Brian, Williams Glenn. 2008Journal of Knee Surgery. 21(3):225–234. doi: 10.1055/s-0030-1247823. doi: 10.1055/s-0030-1247823. [DOI] [PMC free article] [PubMed] [Google Scholar]


