Abstract
Background and Aims
Health care workers (HCWs) are thought to be high‐risk population for acquiring coronavirus disease (COVID‐19). The COVID‐19 emergence has had a profound effect on healthcare system. We sought to investigate the COVID‐19 among HCWs and their effects on the healthcare system.
Methods
A cross sectional observational study was conducted at Timergara teaching hospital. The study included HCWs with positive real time polymerase chain reaction (Q‐PCR) for severe acute respiratory syndrome coronavirus (SARS‐CoV‐2). The study duration was from April to September, 2020. The demographic profile of each recruited subject was collected through structured interview. The patient's admissions to hospital were collected for the 5 months before (October 2019–February 2020) and 5 months after lockdown (March–July 2020).
Results
A total of 72 out of 689 (10%) HCWs were tested positive for SARS‐CoV‐2, of whom 83% were front‐liners. The majority were male (72%), with comorbidities (14%) and no mortality. The structured interview of all participants showed that the healthcare setting was the major possible source of infection (97%). The patient admissions into the hospital were reduced by 42% during lockdown than prelockdown period. The patients admission was significantly decreased in the medical ward during lockdown (60% decrease; p < 0.01) with slightly similar trends in other departments.
Conclusion
In conclusion, we found increased risk of COVID‐19 for front‐line HCWs. Lack of mortality was the favorable outcome. Lack of replacing the infected HCWs possibly explained the marked decrease in hospital admissions, and potential inadequate healthcare delivery during the lockdown. Understanding SARS‐CoV‐2 among HCWs and their impact on health‐care system will be crucial for countries under COVID‐19 crises or in case of future pandemic to deliver proper health services.
Keywords: COVID‐19, health care, health crises, healthcare workers, hospital admission
1. INTRODUCTION
At the end of 2019, a cluster of pneumonia cases of unknown etiology associated with a novel coronavirus emerged in Wuhan city, China, 1 which was later identified as severe acute‐respiratory‐syndrome‐coronavirus‐2 (SARS‐CoV‐2) 2 and officially called coronavirus‐disease‐2019 (COVID‐19). 3 , 4 Considering COVID‐19 mode of transmission through air droplets, 5 it was expected that a high transmission rate would be observed leading to high infectivity particularly in front liners including health care workers (HCWs). 6 Furthermore, asymptomatic HCWs COVID‐19 carriers act as a potential source of transmission to their patients, increasing the disease burden.
Appropriate use of personal protective equipment's (PPEs) among health care workers is important to reduce nosocomial transmission SARS‐CoV‐2 and other respiratory viruses. 7 However, worldwide shortage of masks, face shields, gowns and respirators, caused by supply chain disruptions and exceed demand, have led to scarce supply with a negative effect on best practices among HCWs. 8 Usually, N‐95 respirators are intended for single use before disposal but disinfection protocols have been established to inactivate SARS‐CoV‐2 on N‐95 respirators. 9
SARS‐CoV occurring in 2003, MERS outbreak in 2012, and now the COVID‐19 pandemic, all have claimed the lives of HCWs. Such record of past high mortality rate, put a high psychological pressure on health care professional. 10 , 11 Health care workers unlike the rest of the global population that was mandated to stay at home, had to call on to their workplace and provide their service for the good of the population. Indeed, it was reported that about 20%, front line HCWs were infected by COVID‐19 in Italy, with a proportion dying. 12 Public health mitigation measures are essential to detect, prevent and control public health risks. 13 Due to limited or lack of resources, many countries (low income and middle income countries) are struggling to develop or maintain their health capacities for better management of health emergencies. 13 The COVID‐19 pandemic has had a profound effect on healthcare workers and the healthcare system. Health care workers play a key role in the prevention and management of emerging outbreaks. The severe impact of SARS‐CoV‐2 infection, coupled with an unstable health care system and shortage of health care workers, might have deterrent effects on the country amidst the COVID‐19 crises. 14 , 15
The spread of Covid‐19 in Pakistan disproportionately affected the healthcare systems. 16 Additionally, COVID‐19 have led to significant economic impact on the health‐care system. The quality of care to patients in hospital is expected to be impacted including the emergency therapies such as for cardiovascular emergencies, as HCWs are shifted from their normal duties to care for COVID‐19 patients. 17 Having an understanding of the working environment and wellbeing of HCWs is a high priority. 12 , 18 The aim of this study was to investigate COVID‐19 infectivity rate among health‐care workers at Timergara teaching hospital, their wellbeing, and their access to protective measures. The objective was to assess the impact of COVID‐19 and healthcare workers on hospital admissions during the 5 months of lockdown on comparison to the preceding prelockdown 5 months period.
2. MATERIALS AND METHODS
2.1. Study design and participants
A cross‐sectional observational study design was followed at the teaching hospital (Timergara Teaching hospital Dir Lower, Khyber Pakhtunkhwa, Pakistan 500+ beds), where a total of 689 health care workers are employed. 19
All health‐care workers at Timergara teaching hospital that tested positive (RT‐PCR) during, April 2 to September 28, 2020 for SARS‐CoV‐2 and were either symptomatic or asymptomatic, were included in our study. All these HCWs with confirmed SARS‐CoV‐2 infection were interviewed to record their medical history and other socio‐demographic data (Supporting Information: A). The HWCs were stratified according to their duty in the different departments (emergency, intensive care unit, cardiac care unit, COVID‐19, medical, surgical, labor room, and operation theater wards). HCW's works with Covid‐19 patients throughout COVID‐19 lockdown period in isolation ward. Three shift including morning, evening and night, each shift with 8 h time.
This study was conducted by following the STROBE guidelines for observational studies. 19 In addition we followed the guidelines of Assel and colleagues for proper and clear justification of the study. 20
2.2. Data collection methods
Information was obtained through detail questionnaire that was developed by one of the authors (FH) (Supporting Information: A). Briefly, the study participants were interviewed to provide demographic factors and socioeconomic status. Participant were asked about their history of contact with patients, symptom/s of infection, duration of illness and their place of isolation during the infective period. Participants were also asked about having had either direct contact with infected patient or indirect contact.
For our study analyses, we defined front line HCWs as doctors, nurses, assistant nurses, nursing students and medical students. Health care workers were asked about the use of PPE—(gloves, gowns, goggles, hair cover, surgical masks, and N95 masks) and their availability during their line of work. In addition, study participants were interviewed about their medical comorbidity, smoking status, knowledge about COVID‐19, whether they experienced any anxiety or fear of COVID‐19 and whether they received any administrative support. The infectivity of COVID‐19 among HCWs was noted along with whether their absence from work led to a negative impact on the health care system. This was evaluated in terms of whether a replacement HCW was allocated in their absence from work due to COVID‐19 infection. Impact on health care system was also evaluated in terms of allocation of HCWs from their usual place of work to care for COVID‐19 patients and the admission rates in various wards. In fact, the admission rate of patient to the different wards of the hospital was collected for the 5 months preceding COVID‐19 (October 2019–February 2020) and the admissions for the months of lockdown (March to July 2020).
2.3. Ethical statement
Written informed consent form was obtained from all participated HCWs for SARS‐CoV‐2 related data collection. Study approval was obtained from hospital Incharge.
2.4. Statistical analysis
The results are shown as absolute values and percentages for continuous and categorical variables. A retrospective analysis approach was followed. The change in number of patients' admission to different department of the hospital between the 5 months preceding the lockdown and 5 months during lockdown was calculated.
Mann‐Whitney U‐test was used to determine the mean, standard deviation and significant of change (p value) for hospital admissions over the two periods before lockdown and during lockdown. All tests were two sided and p < 0.05 were considered statistically significant. Statistical analyses were done using Statistical Package for the Social Sciences (SPSS) (version 25.0).
3. RESULTS
Between April 2 and September 28, 2020, 72 (10%) of the 689 health care workers tested positive for SARS‐CoV‐2 RNA at Timergara teaching hospital. Among the HCWs, the highest infection rates were reported among nurses 42 (58%) followed by medical doctors 18 (25%) as opposed to paramedics 7 (10%) and others staff 5 (7%). Baseline characteristics of these 72 COVID‐19 positive HCWs are shown in Table 1. Of note, the age group 31–40 years was the most affected as were the males which reflects the higher proportion of male HCWs in the hospital. Most of the HCWs did not report any comorbidities although a small proportion reported suffering from cardiac problems (3%), diabetes (4%), and hypertension (7%).
Table 1.
Baseline characteristics of health care workers with positive severe acute respiratory syndrome coronavirus‐2 at Timergara teaching Hospital, Pakistan
| Health care workers (n = 72) | |
|---|---|
| Sex | |
| Male | 52 (72%) |
| Female | 20 (28%) |
| Age | |
| 20–30 | 24 (33%) |
| 31–40 | 38 (53%) |
| >41 | 10 (14%) |
| Marital status | |
| Married | 61 (85%) |
| Unmarried | 11 (15%) |
| Family structure | |
| Nuclear | 30 (42%) |
| Extended | 42 (58%) |
| Comorbidities | |
| Cardiac problem | 2 (3%) |
| Diabetics | 3 (4%) |
| Hypertension | 5 (7%) |
| No problems | 52 (72%) |
| Missing data | 10 (14%) |
| Cadre/profession | |
| Medical doctors | 18 (25%) |
| Nurses | 42 (58%) |
| Paramedics | 7 (10%) |
| Other staffa | 5 (7%) |
Note: Data are n (%) are calculated based on the total number of only positive COVID‐19 study participants with available data. Some data are missing for comorbidities.
Other staff include pharmacist and housekeeping staff.
Table 2 summarizes the reported symptoms by COVID‐19 positive HCWs, their PPE use and other COVID‐19 related information. Indeed, fever 59 (82%), cough 56 (78%), and myalgia 42 (58%) were the most common reported symptoms. In addition, one patient had myocardial infarction as a result of COVID‐19. Only 11 (15%) of the infected HCWs reported to have had access to the full protection kit. These HCWs either worked in the COVID‐19 isolation center or were in direct contact with confirmed COVID‐19 patients. Of note, 28 (39%) of the study's HCWs reported to have been the source of COVID‐19 transmission to others, including their family members. The training session organized by the hospital on COVID‐19 was only attended by 17 (24%) of the participating HCWs.
Table 2.
Symptoms, PPE use, session attended on COVID‐19, isolation place, duration of illness, exposures, infection source for others, and plasma exchange among healthcare workers with COVID‐19
| Health care workers (n = 72) | |
|---|---|
| Symptoms | |
| Fever | 59 (82%) |
| Cough | 56 (78%) |
| Chest pain | 12 (17%) |
| Myalgia | 42 (58%) |
| Dyspnea | 19 (26%) |
| Other symptoms | 15 (21%) |
| Asymptomatic | 7 (10%) |
| PPE use | |
| Surgical mask | 54 (75%) |
| N‐95 mask | 18 (25%) |
| Gown | 32 (44%) |
| Gloves | 48 (67%) |
| Goggles | 7 (10%) |
| Kit | 11 (15%) |
| Reuse mask | 12 (17%) |
| Training session attended on COVID‐19 | |
| Yes | 17 (24%) |
| No | 55 (76%) |
| Place of isolation during infection | |
| Hospital isolation center | 16 (22%) |
| Home | 56 (78%) |
| Duration of illness | |
| 10–14 days | 42 (58%) |
| 14–21 days | 19 (26%) |
| >21 days | 11 (15%) |
| Possible source of exposure | |
| Hospital | 70 (97%) |
| Other place | 2 (3%) |
| Transmitting Infection to others | |
| Yes | 28 (39%) |
| No | 44 (61%) |
| Plasma exchange | |
| Donate | 4 (6%) |
| Receive | 2 (3%) |
| No | 66 (91%) |
Note: Data are n (%) are calculated based on the total number of only positive COVID‐19 study participants with available data. Other symptoms mean tasteless, weakness, nausea. Kit includes all the PPE (surgical face mask, filtering face piece mask, first pair of gloves (nitrile), eye goggles, face shield, gown/coverall, second pair of gloves, a pair of boots).
Abbreviation: PPE, personal protective equipment.
The majority of the infected HCWs experienced anxiety (74%) during their infectivity period as well as felt scared of the outcome (75%) after they recovered. These HCWs reported that most of their colleagues, staff members and relatives expressed concern and feared them after recovery (Table 3). The highest infectivity rate was among the HCWs working in the emergency department (29%) followed by those working in the labor room (19%) and within the COVID‐19 (15%) isolation ward (Figure 1).
Table 3.
Anxiety, fear, and health related problems linked with COVID‐19 among health care workers
| n (%) | |
|---|---|
| Anxiety during COVID‐19 infection | |
| Yes | 53 (74%) |
| No | 19 (26%) |
| Fear from COVID‐19 after recovery | |
| Yes | 54 (75%) |
| No | 18 (25%) |
| Fear of others from you after recovery | |
| Mostly | 52 (72%) |
| Some | 13 (18%) |
| None | 07 (10%) |
| Felling unsafe among family | |
| Yes | 63 (88%) |
| No | 09 (12%) |
| Days absent from hospital due to Covid‐19 | |
| 20–30 days | 57 (79%) |
| >30 days | 08 (11%) |
| None | 07 (10%) |
| Effect on health systema | |
| Yes | 62 (86%) |
| No | 10 (14%) |
| Replacement for HCW that were absence from work | |
| Available | 30 (42%) |
| No | 42 (58%) |
Note: Data are n (%) are calculated based on the total number of only positive COVID‐19 study participants with available data.
Abbreviation: HCW, Health care workers.
“Effect on health system” was defined as the absence of replacement HCW to replace those that got sick with Covid‐19 and the effect on the admission rate due to lack of staff.
Figure 1.
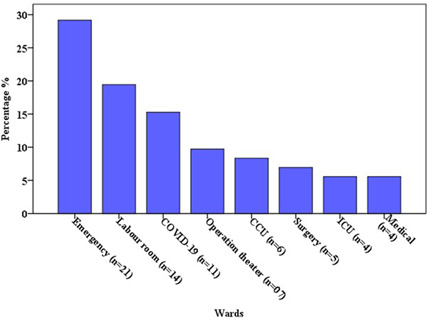
Infected healthcare workers according to their duty wards
The various COVID‐19 factors impacting on the health care system at Timergara teaching hospital is shown in Table 3. It was observed that HCW replacement for COVID‐19 positive HCWs was absent for 42 (58%) (Table 3). Shortage of health care workers during COVID‐19 crises were the main concern in our teaching hospital. In this situation the health care workers declared that their absence from work had significant effect on health care system (Table 3).
Between October 01, 2019 and February 29, 2020 (i.e., 5 months before lockdown in Pakistan) a total of 5861 patients were consecutively admitted in different wards of the hospital (Supporting Information: B; Table 4). During lockdown period between March to the end of July, 2020, a total of 3419 patients were admitted (Supporting Information: B; Table 4). This represented a mark decrease in patient's admissions during COVID‐19 lockdown period in comparison with the number of hospital admission before lockdown to the different wards. Some data was missing for few wards which were closed (i.e., ICU) during lockdown period due to shortage of health care workers and facilities. The decrease in patients admission in ENT (ear, nose, and throat) ward was significant during lockdown period from 774 to 248 (68%; p < 0.05). Similarly, the decrease in patients admissions in medical ward from 864 to 347 (60%; p < 0.01) was also noted. There was also decrease in patients admissions in male surgical ward from 411 to 248 (40%; p < 0.01). Overall, there was decrease in patient's admissions in different departments during COVID‐19 lockdown period.
Table 4.
Number of patient admission in different wards of Timergara teaching hospital, Pakistan before and during lockdown
| Wards | Before lockdown (October–February) | During lockdown (March–July) | p Value |
|---|---|---|---|
| Medical | |||
| Admission (n) | 864 | 347 | <0.01 |
| Mean | 172.8 (17.6) | 69.4 (63.5) | |
| CCU | |||
| Admission (n) | 915 | 721 | <0.05 |
| Mean | 183 (18) | 144.2 (25.5) | |
| Surgical (Male) | |||
| Admission (n) | 411 | 248 | <0.01 |
| Mean | 82.2 (5) | 49.6 (13.6) | |
| Surgical (female) | |||
| Admission (n) | 591 | 313 | <0.05 |
| Mean | 118.2 (40.3) | 62.6 (31) | |
| OT | |||
| Admission (n) | 1113 | 928 | ˃0.05 |
| Mean | 222.6 (43.3) | 185.6 (47.3) | |
| Neurology | |||
| Admission (n) | 615 | 358 | ˃0.05 |
| Mean | 123 (39.7) | 71.6 (39.9) | |
| Gynecology | |||
| Admission (n) | 578 | 256 | <0.05 |
| Mean | 115.6 (24) | 51.2 (45.3) | |
| ENT | |||
| Admission (n) | 774 | 248 | <0.05 |
| Mean | 154.8 (22.5) | 49.6 (48.11) | |
| Total | 5861 | 3419 | |
Note: Data are n, mean (SD). Mean was calculated based on total number of admission in 5 months in each ward. p Value is for the comparison of two groups before lockdown and after lockdown using Mann–Whitney U‐test. Some data for few wards are missing.
Abbreviations: CCU, cardiac care unit, ENT, eye nose throat.
4. DISCUSSION
Up to our knowledge this is the first study investigating the impact of COVID‐19 among health care workers in Pakistan and the impact of HCWs on the health care system. We found that COVID‐19 infectivity rate was significantly higher in frontline health care workers (medical doctor and nurses) working in hospitals as compared to other health‐care professionals (paramedics, pharmacist, and hospital housekeeping staff). Indeed, this prevalence of SARS‐COV‐2 infection among HCWs coincides with the average prevalence reported by a recent meta‐analysis. 21 The study illustrated a higher prevalence of COVID‐19 infection among HCWs working in COVID‐19 isolation wards and emergency department, coinciding with the study by Iversen et al. 14
The demographic characteristics of this study's HCWs were similar to other global studies reporting a higher tendency for the infected HCWs to be young in age, 22 predominately male 14 with few underlying comorbidities. 22 The COVID‐19 symptoms reported by the study's HCWs corresponded to that of the literature. 23 Health care professionals are at high risk of being exposed to SARS‐CoV‐2 within the health facility but can also be a source of viral transmission to their family or others. It was noted that most of the participating HCWs were married with an extended family background. The extended family background is likely to be a chain of transmission among their family, coinciding with a recent study by Wang et al. 24
Protective wear availability was limited to those working in the COVID‐19 isolation ward only. Hence the rest of the HCWs were more vulnerable and at risk of acquiring the viral infection. Insufficient supply of PPE has been reported to be one of the confounding factors for transmission of COVID‐19 among HCWs. 12 Furthermore, our study also reported the reuse of PPE's, which is known to increase the risk of COVID‐19 infection. 8 Piapan et al. reported that 51.3% HCWs infection was attributed to patients exposure, 25 which is similar to our study's findings. Similarly, Vanderxam and colleagues found that 66% HCWs working in the COVID‐19 unit were mainly infected through patients contact. 23
In our study, anxiety levels were high among healthcare workers, while the majority expressed concern on the expected outcome after COVID‐19 recovery. Such emotion debacle is expected especially for those living with vulnerable family members. Indeed, it has been reported by the Center for disease and control (CDC) that even the concept of social distancing and the novel nature of disease can increase anxiety and stress. 26 The fear and worry about one's health, and the health of one's family are other significant factors associated with stress during COVID‐19. 27
The current pandemic challenged the health care system at our teaching hospital. The COVID‐19 occurrence among health care workers resulted in shortage of health care professionals at our hospital. Replacement for the COVID‐19 infected HCWs was very limited, which posed substantial effect on the health care system. As a result, pateints admissions into different departments significantly decreased during lockdown. Our results are consistent with those Nourazari and colleagues conducted in the USA. 28 In England, anxiety among the general public led to 29% decrease into admissions in the emergency department during March 2020 compared to March 2019. 29 Similar to France registry study, we found an approximate quarter decrease in admissions for acute myocardial infarction when comparing the period before and after lockdown was introduced. 30 In Pakistan, the Médecins Sans Frontières (MSF) at Timergara teaching hospital was faced with a significant challenge during COVID‐19 crises when more than 40% of their staff member had to either isolate or quarantine because of COVID‐19. However, the MSF women hospital in Peshawar stopped accepting new patient admissions. This inevitably led to the suspension of hospital activities. 31 Other reasons for the reduction in patients admissions during the pandemic could be following the fact that patients avoided seeking hospital care due to concerns of contracting SARS‐CoV‐2 infection in hospital or as a result of “stay safe at home” notice from the government. Lower admissions could also be due to reduced care support to patients other than COVID‐19 at hospital.
Of note, the swift spread of COVID‐19 has disrupted routine immunization services in Karachi, Pakistan COVID lockdown. 16 As COVID‐19 crises upended health services, it is likely that the disruption of routine immunization services can result in a secondary outbreak of a vaccine preventable disease.
Protecting HCWs from high‐risk pathogens is vital to ensure their safety and safeguard the work force availability that is required for the resilience of the healthcare system. Moreover, their protection will strengthen the front line response against high risk respiratory organisms, such as SARS‐CoV‐2. Hence, the infection reduction among HCWs is critical for reducing nosocomial transmission as well as for the improvement in the continuity of patients care in the same healthcare setting.
The current study has several limitations. It was done in one teaching hospital limiting the data collection on the HCWs to only one institute. The family history was based on self‐reported data and was limited to what the HCWs reported, hence subject to self‐reporting bias. The study was limited only to health care workers so we cannot assess nosocomial transmission of COVID‐19 to general population. Data were missing for the hospital admissions after the lockdown was lifted. Number of hospital admission before the lockdown was not evaluated according to demographic characteristic, exact nature of infection, and outcome due to nature of this retrospective study.
Understanding the transmission and impact of SARS‐CoV‐2 infection among HCWs is crucial for countries, during the currently under COVID‐19 crises as well as in preparation for foreseen waves to come. Such information will also enable better planning for potential future pandemics or outbreaks. This study's findings have great significance for the health authorities to learn from the past experiences and be equipped with evidence‐based data to enable better policy planning and adequate health care delivery. Furthermore, the healthcare facility should provide sufficient quantity of PPE and develop additional strategies to protect and safeguard all HCWs from COVID‐19.
5. CONCLUSIONS
In conclusion, a tenth of the health care workers were infected by SARS‐CoV‐2 with an increased susceptibility among front‐line HCWs. Favorable characteristics including young age and limited comorbidities led to a positive outcome with absence of mortality among HCWs. It appears that the health care setting was the main source of infection. The decrease in general HCWs work power due to COVID‐19 infection challenged the health care system with marked reduction in hospital admissions. It is essential for the health authorities to be fully aware of the current health situation to deliver proper health services, instituted population specific policies, while being preparing for future pandemics.
In Summary, this is the first study in Pakistan targeting the HCWs infectivity rate and their post‐COVID experience. It is evident that those HCW working as front‐liners have a higher susceptibility to infection as well as anxiety repercussions. This resulted in a decrease in healthcare work force which had further negative repercussions on the healthcare system and the delivery of sufficient health services to the population. Adequate quantities of PPIs should be available to all HCWs along with psychological aid to ensure the health and wellbeing of HCWs is maintained.
AUTHOR CONTRIBUTIONS
Faiz Ul Haq: Conceptualization; data curation; formal analysis; investigation; methodology; writing – original draft; writing – review & editing. Saeed Ur Rahman: Conceptualization; investigation. Muhammad Imran: Conceptualization; supervision. Muhammad Romman: Formal analysis; writing – review & editing. Asaf Shah: Formal analysis. Zeenaf Aslam: Formal analysis. Farman Ullah: Writing – original draft. Shekiba Madadi: Formal analysis; writing – original draft. Carl Hermann Dino Steinmetz: Formal analysis; writing – review & editing. Sarah Cuschieri: Supervision; writing – review & editing. All authors have read and approved the final version of the manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Shekiba Madadi affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Supporting information
Supporting information.
Supporting information.
ACKNOWLEDGMENTS
We acknowledge with thanks friends and colleagues for supporting. Finally, we thank to all the health care workers participating in the study. Faiz Ul Haq had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
Haq FU, Rahman SU, Imran M, et al. COVID‐19 among health care workers and their impact on the health care system in a teaching hospital in Pakistan: a cross sectional observational study. Health Sci Rep. 2022;6:e975. 10.1002/hsr2.975
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article and its Supporting Information.
REFERENCES
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727‐733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jiang S, Shi Z, Shu Y, et al. A distinct name is needed for the new coronavirus. Lancet. 2020;395(10228):949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Haq FU, Roman M, Ahmad K, et al. Artemisia annua: trials are needed for COVID‐19. Phytother Res. 2020;34:2423‐2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Organization WH. COVID‐19 weekly epidemiological update. 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update---12-january-2021
- 5. Ghinai I, McPherson TD, Hunter JC, et al. First known person‐to‐person transmission of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) in the USA. Lancet. 2020;395:1137‐1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Black JRM, Bailey C, Przewrocka J, Dijkstra KK, Swanton C. COVID‐19: the case for health‐care worker screening to prevent hospital transmission. Lancet. 2020;395(10234):1418‐1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Verbeek JH, Rajamaki B, Ijaz S, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2020;2020(4):1‐151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID‐19 among front‐line health‐care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475‐e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fischer RJ, Morris DH, van Doremalen N, et al. Effectiveness of N95 respirator decontamination and reuse against SARS‐CoV‐2 virus. Emerging Infect Dis. 2020;26(9):2253‐2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Elkholy AA, Grant R, Assiri A, Elhakim M, Malik MR, Van Kerkhove MD. MERS‐CoV infection among healthcare workers and risk factors for death: retrospective analysis of all laboratory‐confirmed cases reported to WHO from 2012 to 2 June 2018. J Infect Public Health. 2020;13(3):418‐422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jones DS. History in a crisis—lessons for Covid‐19. N Engl J Med. 2020;382(18):1681‐1683. [DOI] [PubMed] [Google Scholar]
- 12. Lancet T. COVID‐19: protecting health‐care workers. Lancet. 2020;395(10228):922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kandel N, Chungong S, Omaar A, Xing J. Health security capacities in the context of COVID‐19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. Lancet. 2020;395:1047‐1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Iversen K, Bundgaard H, Hasselbalch RB, et al. Risk of COVID‐19 in health‐care workers in Denmark: an observational cohort study. Lancet Infect Dis. 2020;20(12):1401‐1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rahman SU, Haq FU, Imran M, et al. Impact of the COVID‐19 lockdown on routine vaccination in Pakistan: a hospital‐based study. Hum Vaccines Immunother. 2021;17(12):4934‐4940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chandir S, Siddiqi DA, Setayesh H, Khan AJ. Impact of COVID‐19 lockdown on routine immunisation in Karachi, Pakistan. Lancet Glob Health. 2020;8(9):e1118‐e1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Carter P, Anderson M, Mossialos E. Health system, public health, and economic implications of managing COVID‐19 from a cardiovascular perspective. Eur Heart J. 2020;41(27):2516‐2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID‐19) in China. J Hosp Infect. 2020;105(1):100‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453‐1457. [DOI] [PubMed] [Google Scholar]
- 20. Assel M, Sjoberg D, Elders A, et al. Guidelines for reporting of statistics for clinical research in urology. BJU Int. 2019;123(3):401‐410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gómez‐Ochoa SA, Franco OH, Rojas LZ, et al. COVID‐19 in health‐care workers: a living systematic review and meta‐analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. 2021;190(1):161‐175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Baqui P, Bica I, Marra V, Ercole A, van Der Schaar M. Ethnic and regional variations in hospital mortality from COVID‐19 in Brazil: a cross‐sectional observational study. Lancet Glob Health. 2020;8(8):e1018‐e1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vandercam G, Simon A, Scohy A, et al. Clinical characteristics and humoral immune response in healthcare workers with COVID‐19 in a teaching hospital in Belgium. J Hosp Infect. 2020;106(4):713‐720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang Y, Wu W, Cheng Z, et al. Super‐factors associated with transmission of occupational COVID‐19 infection among healthcare staff in Wuhan, China. J Hosp Infect. 2020;106(1):25‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Piapan L, De Michieli P, Ronchese F, et al. COVID‐19 outbreak in healthcare workers in hospitals in Trieste, North‐east Italy. J Hosp Infect. 2020;106(3):626‐628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Control CfD, Prevention . Mental Health and Coping During COVID‐19 . Author Atlanta; 2020.
- 27. Seçer İ, Ulaş S, Karaman‐Özlü Z. The effect of the fear of COVID‐19 on healthcare professionals' psychological adjustment skills: mediating role of experiential avoidance and psychological resilience. Front Psychol. 2020;11:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nourazari S, Davis SR, Granovsky R, et al. Decreased hospital admissions through emergency departments during the COVID‐19 pandemic. Am J Emerg Med. 2020;42(2021):203‐210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carter B, Collins JT, Barlow‐Pay F, et al. Nosocomial COVID‐19 infection: examining the risk of mortality. the COPE‐Nosocomial Study (COVID in Older PEople). J Hosp Infect. 2020;106(2):376‐384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mesnier J, Cottin Y, Coste P, et al. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID‐19 and patient profile in France: a registry study. The Lancet Public Health. 2020;5(10):e536‐e542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. (MSF) MSF . Meeting regular health needs amid the COVID‐19 pandemic in Pakistan. MSF; 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and its Supporting Information.


