Abstract
Individuals with high levels of blood-injection-injury (BII) fears are more likely to avoid health screenings, vaccination, and even minor medical interventions. This could result in more serious health issues, lower quality of life, and even shorter life expectancy. However, still little is known about how various emotions (i.e., fear and disgust) affect subjective evaluation on phobia-related stimuli, and what are the potential risk and protective factors that may change the perception of such stimuli throughout these emotions. We investigated the role of fear of medical interventions and the degree of disgust sensitivity in the evaluation of BII phobia-related content and whether previous relevant experience and age may provide protection against the development of a phobia. We collected online survey data from multiple university sources. Participants (N = 228) completed measures of medical fear, disgust sensitivity, prior relevant experience and medical knowledge. Participants were also asked to rate images related to medical settings on dimensions of valence, arousal, disgust, and threat. Our results suggest that high disgust sensitivity and fear of medical interventions may be a risk factor for avoiding medical settings. However, previous relevant medical experience may function as protective factor. The pandemic of recent years underscored the importance of medical intervention and screening tests. These results have implications for professionals helping (e.g., as counselors) people with BII phobia, and physicians and nurses in informing and treating patients.
Keywords: Threat assessment, Medical fear, Disgust sensitivity, Anxiety, Valence, Arousal
Threat assessment; Medical fear; Disgust sensitivity; Anxiety; Valence; Arousal.
1. Introduction
Blood-injury-injection (BII) phobia is a specific anxiety disorder characterized by an irrational fear associated with blood, injury, injections, or other medical interventions (American Psychiatric Association [APA], 2013). Due to the heightened anxiety induced by such stimuli, individuals with BII phobia are more likely to avoid various health screening tests, vaccination, and even minor medical interventions which could result in more serious health issues, lower quality of life, and shorter life span (Öst et al., 1992). Based on previous epidemiological studies, approximately 3% of the population could be affected by BII phobia (Fredrikson et al., 1996; Wardenaar et al., 2017). The fear reaction is based on the need to protect our physical integrity and avoid painful situations (Panksepp et al., 1991). For this reason, pain is a very powerful aversive signal. Stimuli that predict pain can capture the focus of attention (Miron et al., 1989), even when our attention is focused elsewhere (Eccleston and Crombez, 1999). This can help to activate defensive or avoidance behaviors to protect our body (Vlaeyen et al., 2016). Accordingly, fear, and as a consequence avoidance behavior, may be triggered by medical interventions (e.g., surgery) and injections, to avoid potential physical injuries or pain even though these interventions can improve our health and even save our lives.
It has been widely argued that disgust, besides fear, plays a central role in the development and maintenance of specific phobias (Curtis et al., 2011; Olatunji et al., 2007; Tolin et al., 1997). Research on animal phobias has found that some animals evoke disgust rather than fear (Polák et al., 2020; Rádlová et al., 2020; Woody et al., 2005). Animals that are feared but do not attack humans (e.g., spiders, cockroaches) and animals that are generally considered disgusting (e.g., worms, slugs) are associated with disgust and fear of contamination (Matchett and Davey, 1991). Fear of infection and disgust regarding these animals are provoked by certain external traits (e.g., slime) (Merckelbach et al., 1987). Similarly, BII phobia may also be triggered by stimuli associated with the possibility of infection and the transmission of diseases (e.g., infected wounds, blood). Indeed, previous research (Sawchuk et al., 2002; Tolin et al., 1997) has shown that individuals with BII phobia have a higher disgust sensitivity towards mutilation, blood, and surgery than nonphobic controls. Further, the increased disgust sensitivity in BII phobia is not limited to medical-related stimuli, but also extends to much more general objects or situations, for example, rotten food, unpleasant odors, or bodily products. Regarding these theories, we can assume that both fear and disgust play a prominent role in defending the integrity of our body (Nesse, 1990). However, they work in different ways, fear plays a role in avoiding injuries and painful situations, while disgust can help avoid possible contamination.
Past studies have shown that besides emotional factors, genetic (e.g., sex), environmental (e.g., education, relevant experience), and personality factors (e.g., anxiety) also play a crucial role in the development of BII phobia. However, still little is known about how these other factors influence the acquisition and maintenance of BII-related fears and whether they increase or mitigate the fear and disgust response. On the one hand, past studies (Birkás et al., 2022; Bland et al., 1988; Kessler et al., 2005; Magee et al., 1996) found that women are much more affected by specific phobias than men. Lower education and the absence of a spouse (divorced or widowed) were also found to be risk factors (Stinson et al., 2007). Furthermore, individuals with anxiety disorders or related symptoms are more likely to develop phobias (Eaton et al., 2018). In contrast, the emotional response to a phobia decreases with age (Birkás et al., 2022; Karlsson et al., 2016; Stinson et al., 2007). On the other hand, prior relevant pleasant experience and harmless exposure to the object of the phobia may reduce the severity of symptoms and the degree of fear or disgust induced by the next exposure (Coelho and Purkis, 2009; Olatunji et al., 2012a, 2012b). In such situations, one’s sense of control is greater (Coelho and Purkis, 2009), which might reduce the fear experienced towards dogs (Doogan and Thomas, 1992), snakes (Coelho et al., 2021), and even in dental phobia (Berge et al., 2002). Exposure therapies also rely on this effect, reducing anxiety, fear or disgust through repeated presentations of the triggering stimuli or setting (Botella et al., 2017; Hofmann et al., 2012; Morina et al., 2015). The method has been shown to be effective in treating a variety of anxiety disorders, such as needle phobia (Meindl et al., 2019) and spider phobia (Geraets et al., 2019; Lindner et al., 2020; Maskey et al., 2014; Miloff et al., 2019). Similarly, it has been shown (Olatunji et al., 2012a, 2012b) that repeated viewing of video recordings of blood draws reduced the level of disgust perceived by test subjects. Nonetheless, the number of studies exploring risk and protective factors regarding BII is still scarce and further studies are necessary to discover the key factors that may be focused on in prevention or intervention. Overall, therefore, it seems plausible to claim, that more anxious individuals and the female sex may be more vulnerable to BII phobia. Further, it also seems probable, that individuals who have encountered more medical situations during their lifetimes experience lower levels of fear when they have to undergo screening or other medical interventions.
Taken together, the overarching goal of the current study was to assess the effect of potential protective and risk factors in the development of BII phobia. More specifically, we aimed to identify relevant factors, which affect the subjective evaluation of images associated with BII phobia. We tested the following hypotheses: (1) people with greater medical fear and disgust sensitivity will find BII-related images more negative, threatening, and disgusting; (2) higher levels of anxiety and female sex will increase the negative evaluation of the images; (3) previous relevant experience and age will serve as a protective factor. Our aim was to test the explanatory power of these factors and to present a possible conceptual model through pathway analysis.
2. Method
2.1. Participants and procedure
A total of 228 (175 female and 53 male) individuals participated in the study on a voluntary basis. The mean age of the sample was 26.4 (SD = 9.8) with an age range of 18–59. The required sample size for this experiment was determined by computing estimated statistical power with a conservative approach (AGFI = .95, β > .95, α = .05, df = 81) using the semPower package for R (Moshagen and Erdfelder, 2016; R Core Team, 2020). The analysis indicated a required total sample size of 201; thus, our study was adequately powered. The data was collected from the spring of 2021 to the fall of 2021. The questionnaire was distributed via various social media groups and e-mail lists. All respondents filled out the questionnaires online, using Google Forms. Participants first completed demographic and other questions related to relevant medical experiences, followed by the questionnaires. After completing the self-reports, they were asked to rate a total of 43 images on arousal, valence, threat, and disgust scales.
As for inclusion criteria, participants had to be at least 18 years old to take part in the study. They had to declare if they had no neurological disorders and were not under psychiatric treatment or mental illness. Based on self-report, none of the participants were diagnosed with or received treatment for phobias, or other psychiatric disorders. See Table 1 for further details on the sample. The research was approved by the Hungarian United Ethical Review Committee for Research in Psychology and was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki). Informed and written consent was obtained from all participants.
Table 1.
Demographic features (number and percentage) of the sample concerning education and place of residence.
| N | % | |
|---|---|---|
| Education | ||
| Elementary | 11 | 4.8% |
| High school | 127 | 56.2% |
| BA/BSc | 60 | 26.5% |
| MA/MSc |
30 |
12.5% |
| Place of residence | ||
| Village | 55 | 24.1% |
| City | 81 | 35.5% |
| Big city | 49 | 21.5% |
| Capitol | 43 | 18.9% |
2.2. Questionnaires
We used the short, 25-item version of the Medical Fear Survey (MFS) to measure BII phobia (Birkás et al., 2022; Olatunji et al., 2012a, 2012b). The MFS measures a broad spectrum of medically related fears on five subscales: Blood, Injections and Blood Draws, Sharp Objects, Examinations and Symptoms, and Mutilation. Respondents are asked to rate each statement from 0 (no fear/concern) to 3 (intense fear/concern). A higher score indicates that the individual is more afraid of medical situations. The reliability of the MFS was excellent (McDonald’s omega = .912).
We measured disgust sensitivity with the Revised Disgust Scale (DS-R) (Olatunji et al., 2009a, 2009b). DS-R measures the extent to which people find certain situations disgusting, including concepts related to food, animals, bodily products, sex, death, etc. The revised scale has three subscales, such as Core disgust, Animal Reminder disgust, and Contamination disgust. The questionnaire consists of 13 true/false items and 12 items that are rated on 3-point Likert-type scales. Individuals with higher scores are more likely to experience disgust in the given situations. The DS-R showed an acceptable value of reliability (McDonald’s omega = .721).
To measure trait anxiety we used the short, 5-item version of the Spielberger State-Trait Anxiety Inventory (STAI) (Zsido et al., 2020). STAI measures trait anxiety (how one feels in general). Respondents have to mark their answers on 4-point Likert scales (from 0 to 3 points). Higher scores indicate higher trait anxiety levels. The reliability of the scale on our sample was satisfactory (McDonald’s omega = .846).
Participants' relevant experiences of medical situations were assessed with questions related to the types of medical situations (e.g., blood tests, screening tests) consistent with the MFS subscales and formulated by the researchers. Possible health-related education or work experiences were also asked. Items included true-false questions and they had to select the appropriate interval for frequency (e.g., daily, weekly, monthly, etc.). Answers to the questions were worth 1 point for Yes and 0 for No. Regarding the frequency of particular experiences or exposures, the more times a situation was encountered, the higher score was given. The total score for frequency responses was calculated by adjusting the values to be between 0 and 1 (each number value was divided by the largest number value that could be given). The resulting scores were added together to form the final experience score, where a lower number represented a lower level of relevant experience, and a higher number represented a higher level of relevant experience.
2.3. Picture material
Pictures were sourced from three image collections, the EmoMadrid (Carretié et al., 2019), the Geneva Affective Picture Database (Dan-Glauser and Scherer, 2011) and the Nencki Affective Picture System (Marchewka et al., 2013). Our goal was to select as many pictures as possible that corresponds to the content of the MFS questionnaire subscales and they are also not too harsh. We found a total of 45 images, of which two were dropped because their mean valence value fell in the positive range. Participants rated the selected 45 pictures on valence (pleasant-unpleasant), arousal (weak-strong), disgust (not disgusting-disgusting), and threat (non-threatening - threatening) dimensions using 9-point Likert-type scales. We asked participants to rate images according to how they felt while watching them. Higher points meant more unpleasant, arousing, disgusting, and threatening content. See Table 2 for the central tendencies of the ratings.
Table 2.
Means (M) and standard deviations (SD) for the picture ratings for related content on four emotional dimensions: valence, arousal, disgust and threat; separately for males and females and the total sample.
| Valence |
Arousal |
Threat |
Disgust |
|||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |
| Male | 3.22 | 1.27 | 3.94 | 1.9 | 3.4 | 1.88 | 3.17 | 1.72 |
| Female | 3.3 | 1.34 | 4.62 | 1.72 | 3.97 | 1.90 | 3.48 | 1.67 |
| Full sample | 3.29 | 1.32 | 4.46 | 1.79 | 3.86 | 1.91 | 3.41 | 1.68 |
2.4. Statistical analysis
All self-reports were fully completed by all participants thus, all questionnaire data were included into the analysis.
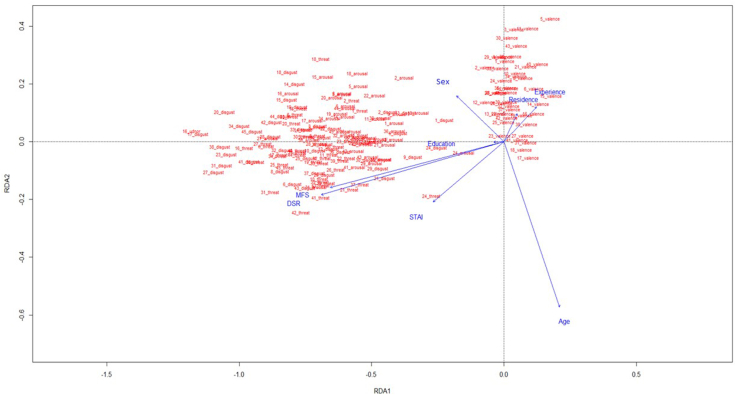
First, we used Redundancy Analysis (RDA) to determine how questionnaire scores and demographic factors affect the picture ratings, and to select those that have a significant effect. The RDA was implemented in the R package vegan (Oksanen et al., 2005; R Core Team, 2020). RDA is a multivariate direct gradient method (Braak and Smilauer, 2018). RDA summarizes and extracts the variations of a set of response variables and plots both the response variables and the explanatory variables in the space defined by the extracted gradients. By this, we could calculate the joint variability (redundancy) between the response variables and the explanatory variables. In our study, the explanatory variables were gender, age, relevant experience, and the scores on the MFS and DS-R subscales, and STAI-5 scores. The analysis was used to examine how these variables contribute to the valence, arousal, disgust, and threat scores of BII phobia-related images.
Then, we used General Linear Modelling (GLM) to explore the questionnaires and demographic factors that are significant predictors of MFS and DS-R scores. We used Jamovi statistical software version 2.2.5 (The jamovi project, 2021) for GLM analysis. We tested two models with the summaries of the MFS and the DS-R scores as the dependent variables. The independent predictors in both models were sex, relevant experience, age, level of education and STAI scores. The assumption of normality was not violated, the absolute value of Skewness and Kurtosis were less than 2 for both the MFS and DS-R.
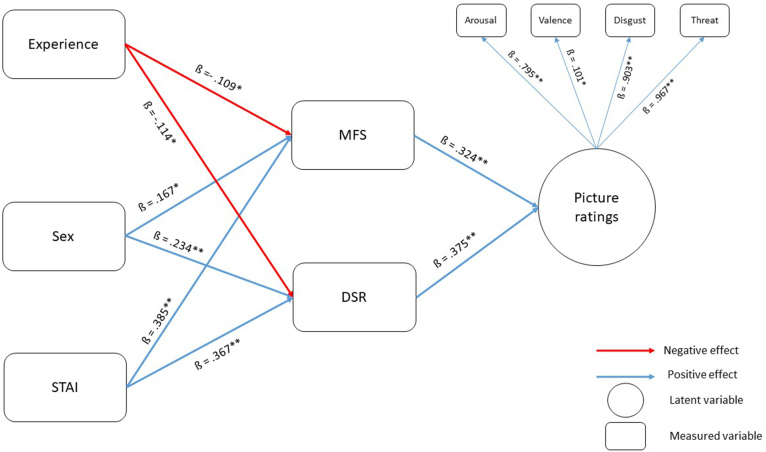
Finally, we performed Structural Equation Modelling (SEM) using the JASP statistical software version: 0.14.1.0 for Windows (JASP Team, 2022). To construct our model, we relied on the outcome of the RDAs and GLMs. Figure 1 shows the model tested. The model had one latent outcome variable, comprised of the picture ratings (arousal, threat, disgust and valence). This was predicted by the factors of MFS and DS-R (both entered as measured variables). These, in turn, were predicted by experience, sex, and STAI (entered as measured variables). To test our model, we used the diagonally weighted least squares (DWLS) estimator. To determine the model fit, we used the comparative fit index (CFI), Tucker-Lewis index (TLI), root mean square error of approximation (RMSEA) and standardized root mean square residual (SRMR). Cutoff points of .95 or higher for CFI and TLI (Hu and Bentler, 1998), and 0.08 or lower for RMSEA and SRMR (Browne and Cudeck, 1992) were used to determine a good model fit.
Figure 1.
Our proposed model of the relationship between medical fears, disgust sensitivity, relevant experience and emotional appraisal of BII phobia-related images. All pathways and variables included in the analysis are displayed. The reported estimates are standardized estimates (β). Positive effects are marked with solid blue lines, negative effects are marked with solid red lines. ∗ = p < 0.05; ∗∗ = p < 0.001 MFS = Medical Fear Survey, DSR = Disgust Scale Revised, STAI = State-Trait Anxiety Inventory.
3. Results
3.1. Redundancy analysis
The RDA model (see Figure 2) of the arousal, threat, disgust, and valence ranks of the medical-related images as response variables have generated 8 constrained axes, which explained 17.84% of the full variability. We then performed a permutation test (number of permutations = 999) to confirm the significance of each of the independent variables (constraints) in a sequential (‘type I’) test: DSR, F(1,219) = 30.303, p = .001; STAI, F(1,219) = .542, p = .744; MFS F(1,219) = 5.718, p = .003; Sex F(1,219) = 1.175, p = .282; Age F(1,219) = 4.404, p = .012; Education, F(1,219) = 3.984, p = .007; Residence, F(1,219) = .736, p = .539; Experience, F(1,219) = 0.688, p = .577.
Figure 2.
Redundancy analysis (RDA) of the respondents' age, sex, blood-injury-injection-related fears and disgust sensitivity, and their effect on valence, arousal, disgust and threat ratings of 42 BII phobia related images. The model explained 17.84% of the full variability. MFS = Medical Fear Survey - Blood, Injections and Blood Draws, Sharp Objects, Examinations and Symptoms and Mutilation subscales, DSR = Disgust Scale Revised - core disgust, animal reminder disgust and contamination disgust subscales, STAI = State-Trait Anxiety Inventory.
3.2. General linear models
Regarding medical fear, the general linear model (F(6,221) = 8.2869, p < .001, η2p = .184) showed that sex (F(1,221) = 6.6808, p = .010, η2p = .029), STAI scores (F(1,221) = 29.5118, p < .001, η2p = .118), had a significant effect, while age (F(1,221) = 1.1789, p = .279, η2p = .005), level of education (F(1,221) = .0006, p = .980, η2p = .000), residence (F(1,221) = .0103, p = .919, η2p = .000) and experience (F(1,221) = 2.1026, p = .148, η2p = .009) had a non-significant effect.
In the case of disgust sensitivity, the GLM (F(6,221) = 9.60948, p < .001, η2p = .207) showed a significant effect with sex (F(1,221) = 14.68794, p < .001, η2p = .062), STAI (F(1,221) = 30.65892, p < .001, η2p = .122). While it showed no significant effect with age (F(1,221) = 1.41e-6, p = .999, η2p = .000), level of education (F(1,221) = .89619, p = .345, η2p = .004), residence (F(1,221) = .00966, p = .922, η2p = .000) and with experience (F(1,221) = 2.33515, p = .128, η2p = .0010).
3.3. Structural equation modelling
The SEM analysis (see Figure 1) showed a good model fit (X2(21) = 47.894, p < .001, CFI = .968 TLI = .95, RMSEA = .075, [90%CI = .047 to .103], SRMR = .080). The MFS score (R2 = .208) were predicted positively by the STAI scores (ß = .385, p < .001), Sex (ß = .167, p = .001) and negatively by the Experience (ß = −.109, p < .05). The DSR scores (R2 = .230) were predicted positively by the STAI scores (ß = .367, p < .001), Sex (ß = .234, p < .001) and negatively by Experience (ß = −.114, p < .001). The Picture Ratings (R2 = .299) were predicted by MFS scores (ß = .324, p < .001), and DSR scores (ß = .375, p < .001). All observed variables loaded significantly on the latent variable of Picture ratings: Arousal (ß = .795, p < .001), Valence (ß = .101, p < .05), Disgust (ß = .903, p < .001), and Threat (ß = .967, p < .001).
Regarding the indirect pathways, we found that Experience significantly predicted Picture Ratings through DS-R scores (ß = −.051, p = .049), but not through MFS scores (ß = −.042, p = .064). STAI scores significantly predicted Picture Ratings through DS-R (ß = .148, p < .001) and MFS (ß = .131, p < .001) scores. Sex significantly predicted Picture Ratings through DS-R (ß = .095, p < .001) and MFS (ß = .060, p = .010) scores.
4. Discussion
The aim of our study was to investigate factors, such as medical fears and disgust sensitivity, that previous research has suggested may play a prominent role in the development and maintenance of BII phobias. Further, we sought to test how the emotional factors mediate the effect of genetic, environmental, and personality factors that has been shown to play a relevant role in the development and maintenance of various specific phobias. Overall, we wanted to identify these as either risk or protective factors. BII phobia is among the most prevalent specific phobias with a lifetime prevalence of approximately 3% (Fredrikson et al., 1996; Wardenaar et al., 2017). Due to the intensive emotional responses triggered by stimuli related to blood, injections, and injuries (including medical settings), individuals with BII phobia and high levels of BII-related fears are more likely to avoid health screenings, vaccination, and even minor medical interventions. This could result in more serious health issues, lower quality of life, and a shorter life span (Öst et al., 1992). Previous studies (Olatunji et al., 2017; Sawchuk et al., 2000; Tolin et al., 1997) showed that fear and disgust might be equally important in the acquisition and maintenance of BII. However, still little is known about how fear and disgust affect the subjective evaluation of phobia-related stimuli, and what are the potential risk and protective factors that may change the perception of such stimuli throughout these emotions. Understanding the triggering factors of developing BII phobia may contribute to the prevention and treatment of such disorders. Our results show that both medical fears and disgust sensitivity play a crucial role in how people perceive BII phobia-related images. More specifically, participants who experience greater fear of medical situations and have a higher sensitivity to disgust find BII phobia-related content more negative, threatening, and disgusting. Further, experience, sex, and anxiety levels showed very similar effect sizes across measures of medical fear and disgust sensitivity. The relevance of disgust in addition to fear in the development and maintenance of BII phobia is consistent with former findings (Koch et al., 2002; Olatunji et al., 2007; Sawchuk et al., 2002; Tolin et al., 1997). Fear as an emotional response can help avoid situations that are too painful or potentially harmful. While disgust can play a more important role in avoiding infections (Davey, 1991).
According to our results, the more relevant experience one has (i.e., more encounters with blood, injections, or injuries, worked in a health-related job, are trained in first aid) the lower levels of fear and disgust sensitivity they have, and, consequently, rate BII-related stimuli as less negative. These findings may suggest that exposure to content associated with BII phobia may also be a protective factor in developing overly high levels of fear. This is in line with the results of previous studies on other specific phobias, such as fear of snakes, heights, and dogs (Coelho et al., 2021; Donker et al., 2019; Doogan and Thomas, 1992), as well as an earlier study on BII phobia (Olatunji et al., 2012a, 2012b). This may be the result of habituation due to repeated exposure (Olatunji et al., 2009a, 2009b). It could also be explained by the fact that more positive or neutral experiences give the person more control over the situation and thus easier to regulate their emotional reactions in such a threatening situation (Coelho and Purkis, 2009).
We found that higher levels of anxiety were associated with higher levels of fear and disgust sensitivity, resulting in more negative rating of BII-related images, and thus may be a risk factor for BII phobia. It has been shown that lifelong specific phobia may be a predictor of anxiety disorders (Stinson et al., 2007). Several neurological studies have shown that in anxiety disorders (e.g. specific phobias), increased activation of certain areas of the amygdala and insula can be observed (Etkin and Wager, 2007). These areas play an important role in the development of the fear response. Previous epidemiological studies (Bland et al., 1988; Kessler et al., 2005; Magee et al., 1996) showed that women are more vulnerable to specific phobias compared to men. Our results on sex differences are in line with these former findings since women reported higher levels of medical fear and disgust sensitivity and perceived the images presented as more negative suggesting, that women are more affected by BII phobias than men. Contrary to our expectations, age was not found to be a protective factor in our study. On the one hand, this might be due to the relatively narrow age distribution of the current sample consisting predominantly of young adults. On the other hand, an alternative ultimate approach may be helpful to understand the sex differences together with the lack of age-effect we obtained (Bracha, 2006; Bracha et al., 2005, 2007). Bracha suggests that in the Middle Paleolithic, mating strategies included intense competition and physical fights predominantly between young males to gain access to females of reproductive age. Thus, little or no fear of blood or sharp objects could have been a significant advantage for males in mating. On the contrary, females may have benefited from a heightened emotional response to such situations, as this reduced the risk of injury and death.
Some limitations of the present study shall be noted. Even though gender differences are well-documented in specific phobias, the gender imbalance may have confounded the results and could have made the comparison of females and males problematic. Further, although we used structural equation modeling for statistical analysis, our study was cross-sectional in design. Therefore, some aspects of the relationship between some of the variables remain uncontrolled. For instance, previous experiences prohibit developing BII phobia and an elevated disgust sensitivity However the opposite direction may be also true thus, the lack of BII-related fears and lower disgust sensitivity allow individuals to have more experiences with BII-related stimuli. Since avoidance of phobia-associated stimuli and situations is an essential feature of all phobias, there is probably an interplay between these different effects. Future studies, perhaps longitudinal in design should be performed to gather more information regarding this interplay. Another limitation is that we used self-report surveys and asked participants to rate images on Likert-type scales but did not collect (more objective) physiological data.
Despite these limitations, our study has successfully demonstrated that both fear and disgust are important factors in the development and maintenance of BII phobia. Further, we also identified certain protective (previous experience) and risk (higher levels of anxiety and female gender) factors of BII phobia. Factors, that may affect the strength of emotional reaction and how one perceives certain stimuli. Thus, the results presented here might be useful for preventive work and interventions that aim to facilitate the willingness of individuals to undergo medical screenings, get vaccinated and stop avoiding medical procedures. Also, the results might be feasible for medical personnel to better understand the motives of individuals who avoid screening or treatment. Increased comprehension may improve the communication between healthcare personnel and these individuals, also improving their life-quality. Nevertheless, further studies employing behavioral (such as eye-tracking and behavioral avoidance task), as well as physiological measures (such as skin conductance and heart rate variability) should be utilized to gain a more detailed understanding of the processes underlying phobias.
Declarations
Author contribution statement
Botond László Kiss; Léna Zilahi: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Béla Birkás: Analyzed and interpreted the data; Wrote the paper.
Andras N. Zsido: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This study was supported by Innovációs és Technológiai Minisztérium [OTKA PD 137588], Nemzeti Kutatási, Fejlesztési és Innovációs Alap [ÚNKP-21-4 & ÚNKP-4-22], Innovációs és Technológiai Minisztérium [NKFIH “OTKA” K125437], Magyar Tudományos Akadémia [János Bólyai Research Scholarship], and Innovációs és Technológiai Minisztérium [NKFIH “OTKA K” 143254].
Data availability statement
Data associated with this study has been deposited at https://osf.io/nmh4r/
Declaration of interest’s statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- American Psychiatric Association . DSM 5 Diagnostic and Statistical Manual of Mental Disorders. 2013. DSM 5 diagnostic and statistical manual of mental disorders; p. 225. [Google Scholar]
- Berge M. Ten, Veerkamp J.S.J., Hoogstraten J. The etiology of childhood dental fear: the role of dental and conditioning experiences. J. Anxiety Disord. 2002;16(3):321–329. doi: 10.1016/s0887-6185(02)00103-2. [DOI] [PubMed] [Google Scholar]
- Birkás B., Csathó Á., Teleki S., Zsidó A. Confirming the factor structure and improving the screening function of the Medical Fear Survey - short in a Hungarian community sample. Hist. Philos. Logic. 2022;35(2):248–258. doi: 10.1080/10615806.2021.1913490. [DOI] [PubMed] [Google Scholar]
- Bland R.C., Orn H., Newman S.C. Lifetime prevalence of psychiatric disorders in edmonton. Acta Psychiatrica Scandinavica. Supplementum. 1988;338(338 S):24–32. doi: 10.1111/j.1600-0447.1988.tb08544.x. [DOI] [PubMed] [Google Scholar]
- Botella C., Fernández-Álvarez J., Guillén V., García-Palacios A., Baños R. Recent progress in virtual reality exposure therapy for phobias: a systematic review. Curr. Psychiatr. Rep. 2017;19(7) doi: 10.1007/s11920-017-0788-4. [DOI] [PubMed] [Google Scholar]
- Bracha H.S. Human brain evolution and the “Neuroevolutionary Time-depth Principle:” Implications for the Reclassification of fear-circuitry-related traits in DSM-V and for studying resilience to warzone-related posttraumatic stress disorder. Prog. Neuro Psychopharmacol. Biol. Psychiatr. 2006;30(5):827–853. doi: 10.1016/j.pnpbp.2006.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bracha H.S., Bienvenu O.J., Eaton W.W. Testing the Paleolithic-human-warfare hypothesis of blood–injection phobia in the Baltimore ECA Follow-up Study—towards a more etiologically-based conceptualization for DSM-V. J. Affect. Disord. 2007;97(1–3):1–4. doi: 10.1016/j.jad.2006.06.014. [DOI] [PubMed] [Google Scholar]
- Bracha H.S., Bracha A.S., Williams A.E., Ralston T.C., Matsukawa J.M. The human fear-circuitry and fear-induced fainting in healthy individuals. Clin. Auton. Res. 2005;15(3):238–241. doi: 10.1007/s10286-005-0245-z. [DOI] [PubMed] [Google Scholar]
- Browne M.W., Cudeck R. Alternative ways of assessing model fit. Socio. Methods Res. 1992;21(2):230–258. [Google Scholar]
- Carretié L., Tapia M., López-Martín S., Albert J. EmoMadrid: an emotional pictures database for affect research. Motiv. Emot. 2019;43(6):929–939. [Google Scholar]
- Coelho C.M., Purkis H. The origins of specific phobias: influential theories and current perspectives. Rev. Gen. Psychol. 2009;13(4):335–348. [Google Scholar]
- Coelho C.M., Polák J., Zsido A.N. 2021. Fear Inoculation Among Snake Experts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis V., Barra M. De, Aunger R. Disgust as an adaptive system for disease avoidance behaviour. Phil. Trans. Biol. Sci. 2011;366(1563):389–401. doi: 10.1098/rstb.2010.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dan-Glauser E.S., Scherer K.R. The Geneva affective picture database (GAPED): a new 730-picture database focusing on valence and normative significance. Behav. Res. Methods. 2011;43(2):468–477. doi: 10.3758/s13428-011-0064-1. [DOI] [PubMed] [Google Scholar]
- Davey G.C.L. Characteristics of individuals with fear of spiders. Anxiety. Res. 1991;4(4):299–314. [Google Scholar]
- Doogan S., Thomas G.V. Origins of fear of dogs in adults and children: the role of conditioning processes and prior familiarity with dogs. Behav. Res. Ther. 1992;30(4):387–394. doi: 10.1016/0005-7967(92)90050-q. [DOI] [PubMed] [Google Scholar]
- Eaton W.W., Bienvenu O.J., Miloyan B. Specific phobias. Lancet Psychiatr. 2018;5(8):678–686. doi: 10.1016/S2215-0366(18)30169-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etkin A., Wager T.D. Functional neuroimaging of anxiety: a meta-ana lysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am. J. Psychiatr. 2007;164(10):1476–1488. doi: 10.1176/appi.ajp.2007.07030504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrikson M., Annas P., Fischer H., Wik G. Gender and age differences in the prevalence of specific fears and phobias. Behav. Res. Ther. 1996;34(1):33–39. doi: 10.1016/0005-7967(95)00048-3. [DOI] [PubMed] [Google Scholar]
- Geraets C.N.W., Veling W., Witlox M., Staring A.B.P., Matthijssen S.J.M.A., Cath D. Virtual reality-based cognitive behavioural therapy for patients with generalized social anxiety disorder: a pilot study. Behav. Cognit. Psychother. 2019;47(6):745–750. doi: 10.1017/S1352465819000225. [DOI] [PubMed] [Google Scholar]
- Hofmann S.G., Asnaani A., Vonk I.J.J., Sawyer A.T., Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit. Ther. Res. 2012;36(5):427–440. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L.T., Bentler P.M. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol. Methods. 1998;3(4):424–453. [Google Scholar]
- JASP Team JASP (Version 0.16.1) [Computer software] 2022. https://jasp-stats.org/ Retrieved from.
- Karlsson B., Sigström R., Östling S., Waern M., Börjesson-Hanson A., Skoog I. DSM-IV and DSM-5 prevalence of social anxiety disorder in a population sample of older people. Am. J. Geriatr. Psychiatr. 2016;24(12):1237–1245. doi: 10.1016/j.jagp.2016.07.023. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Berglund P., Demler O., Jin R., Merikangas K.R., Walters E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatr. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Koch M.D., O’Neill H.K., Sawchuk C.N., Connolly K. Domain-specific and generalized disgust sensitivity in blood-injection-injury phobia:The application of behavioral approach/avoidance tasks. J. Anxiety Disord. 2002;16(5):511–527. doi: 10.1016/s0887-6185(02)00170-6. [DOI] [PubMed] [Google Scholar]
- Lindner P., Rozental A., Jurell A., Reuterskiöld L., Andersson G., Hamilton W., Miloff A., Carlbring P. Experiences of gamified and automated virtual reality exposure therapy for spider phobia: qualitative study. JMIR Serious Games. 2020;8(2) doi: 10.2196/17807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee W.J., Eaton W.W., Wittchen H.U., McGonagle K.A., Kessler R.C. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch. Gen. Psychiatr. 1996;53(2):159–168. doi: 10.1001/archpsyc.1996.01830020077009. [DOI] [PubMed] [Google Scholar]
- Marchewka A., Żurawski Ł., Jednoróg K., Grabowska A. The Nencki Affective Picture System (NAPS): introduction to a novel, standardized, wide-range, high-quality, realistic picture database. Behav. Res. Methods. 2013;46(2):596–610. doi: 10.3758/s13428-013-0379-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maskey M., Lowry J., Rodgers J., McConachie H., Parr J.R. Reducing specific phobia/fear in young people with autism spectrum disorders (ASDs) through a virtual reality environment intervention. PLoS One. 2014;9(7) doi: 10.1371/journal.pone.0100374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matchett G., Davey G.C.L. A test of a disease-avoidance model of animal phobias. Behav. Res. Ther. 1991;29(1):91–94. doi: 10.1016/s0005-7967(09)80011-9. [DOI] [PubMed] [Google Scholar]
- Meindl J.N., Saba S., Gray M., Stuebing L., Jarvis A. Reducing blood draw phobia in an adult with autism spectrum disorder using low-cost virtual reality exposure therapy. J. Appl. Res. Intellect. Disabil. 2019;32(6):1446–1452. doi: 10.1111/jar.12637. [DOI] [PubMed] [Google Scholar]
- Merckelbach H., Van Den Hout M.A., Van Der Molen G.M. Fear of animals: correlations between fear ratings and perceived characteristics. Psychol. Rep. 1987;60(3II):1203–1209. doi: 10.1177/0033294187060003-240.1. [DOI] [PubMed] [Google Scholar]
- Miloff A., Lindner P., Dafgård P., Deak S., Garke M., Hamilton W., Heinsoo J., Kristoffersson G., Rafi J., Sindemark K., Sjölund J., Zenger M., Reuterskiöld L., Andersson G., Carlbring P. Automated virtual reality exposure therapy for spider phobia vs. in-vivo one-session treatment: a randomized non-inferiority trial. Behav. Res. Therapy. 2019;118:130–140. doi: 10.1016/j.brat.2019.04.004. [DOI] [PubMed] [Google Scholar]
- Miron D., Duncan G.H., Catherine Bushnell M. Effects of attention on the intensity and unpleasantness of thermal pain. Pain. 1989;39(3):345–352. doi: 10.1016/0304-3959(89)90048-1. [DOI] [PubMed] [Google Scholar]
- Morina N., Ijntema H., Meyerbröker K., Emmelkamp P.M.G. Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments. Behav. Res. Ther. 2015;74:18–24. doi: 10.1016/j.brat.2015.08.010. [DOI] [PubMed] [Google Scholar]
- Nesse R.M. Evolutionary explanations of emotions. Hum. Nat. 1990;1(3):261–289. doi: 10.1007/BF02733986. [DOI] [PubMed] [Google Scholar]
- Oksanen J., Kindt R., O’Hara B., Maintainer H. The vegan Package Title Community Ecology Package. 2005. https://cc.oulu.fi/∼jarioksa/
- Olatunji B.O., Berg H.E., Zhao Z. Emotion regulation of fear and disgust: differential effects of reappraisal and suppression. Cognit. Emot. 2017;31(2):403–410. doi: 10.1080/02699931.2015.1110117. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Ciesielski B.G., Wolitzky-Taylor K.B., Wentworth B.J., Viar M.A. Effects of experienced disgust on habituation during repeated exposure to threat-relevant stimuli in blood-injection-injury phobia. Behav. Ther. 2012;43(1):132–141. doi: 10.1016/j.beth.2011.04.002. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Ebesutani C., Sawchuk C.N., McKay D., Lohr J.M., Kleinknecht R.A. Development and initial validation of the medical fear survey-short version. Assessment. 2012;19(3):318–336. doi: 10.1177/1073191111415368. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Moretz M.W., McKay D., Bjorklund F., De Jong P.J., Haidt J., Hursti T.J., Imada S., Koller S., Mancini F., Page A.C., Schienle A. Confirming the three-factor structure of the disgust scaleg-revised in eight countries. J. Cross Cult. Psychol. 2009;40(2):234–255. [Google Scholar]
- Olatunji B.O., Smits J.A.J., Connolly K., Willems J., Lohr J.M. Examination of the decline in fear and disgust during exposure to threat-relevant stimuli in blood-injection-injury phobia. J. Anxiety Disord. 2007;21(3):445–455. doi: 10.1016/j.janxdis.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Wolitzky-Taylor K.B., Willems J., Lohr J.M., Armstrong T. Differential habituation of fear and disgust during repeated exposure to threat-relevant stimuli in contamination-based OCD: an analogue study. J. Anxiety Disord. 2009;23(1):118–123. doi: 10.1016/j.janxdis.2008.04.006. [DOI] [PubMed] [Google Scholar]
- Öst L.G., Hellström K., Kåver A. One versus five sessions of exposure in the treatment of injection phobia. Behav. Ther. 1992;23(2):263–281. [Google Scholar]
- Panksepp J., Sacks D.S., Crepeau L.J., Abbott B.B. In: Fear, Avoidance, and Phobias: A Fundamental Analysis. Denny M.R., editor. Lawrence Erlbaum Associates, Inc; 1991. The psycho- and neurobiology of fear systems in the brain; pp. 7–59. [Google Scholar]
- Polák J., Rádlová S., Janovcová M., Flegr J., Landová E., Frynta D. Scary and nasty beasts: self-reported fear and disgust of common phobic animals. Br. J. Psychol. 2020;111(2):297–321. doi: 10.1111/bjop.12409. [DOI] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A Language and Environment for Statistical Computing.http://www.R-project.org/ URL. [Google Scholar]
- Rádlová S., Polák J., Janovcová M., Sedláčková K., Peléšková Š., Landová E., Frynta D. Emotional reaction to fear- and disgust-evoking snakes: sensitivity and propensity in snake-fearful respondents. Front. Psychol. 2020;11:31. doi: 10.3389/fpsyg.2020.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawchuk C.N., Lohr J.M., Tolin D.F., Lee T.C., Kleinknecht R.A. Disgust sensitivity and contamination fears in spider and blood-injection-injury phobias. Behav. Res. Ther. 2000;38(8):753–762. doi: 10.1016/s0005-7967(99)00093-5. [DOI] [PubMed] [Google Scholar]
- Sawchuk C.N., Lohr J.M., Westendorf D.H., Meunier S.A., Tolin D.F. Emotional responding to fearful and disgusting stimuli in specific phobics. Behav. Res. Ther. 2002;40(9):1031–1046. doi: 10.1016/s0005-7967(01)00093-6. [DOI] [PubMed] [Google Scholar]
- Stinson F.S., Dawson D.S., Chou S.P., Smith S., Goldtein R.B., Ruan W.J., Grant B.F. The epidemiology of DSM-IV specific phobia in the USA: results from the national epidemiologic survey on alcohol and related conditions. Psychol. Med. 2007;37(7):1047–1059. doi: 10.1017/S0033291707000086. [DOI] [PubMed] [Google Scholar]
- The jamovi project jamovi (Version 1.6) [Computer Software] 2021. https://www.jamovi.org Retrieved from.
- Tolin D.F., Lohr J.M., Sawchuk C.N., Lee T.C. Disgust and disgust sensitivity in blood-injection-injury and spider phobia. Behav. Res. Ther. 1997;35(10):949–953. doi: 10.1016/s0005-7967(97)00048-x. [DOI] [PubMed] [Google Scholar]
- Vlaeyen J.W.S., Crombez G., Linton S.J. The fear-avoidance model of pain. Pain. 2016;157(8):1588–1589. doi: 10.1097/j.pain.0000000000000574. [DOI] [PubMed] [Google Scholar]
- Wardenaar K.J., Lim C.C.W., Al-Hamzawi A.O., Alonso J., Andrade L.H., Benjet C., Bunting B., de Girolamo G., Demyttenaere K., Florescu S.E., Gureje O., Hisateru T., Hu C., Huang Y., Karam E., Kiejna A., Lepine J.P., Navarro-Mateu F., Oakley Browne M., et al. The cross-national epidemiology of specific phobia in the World Mental Health Surveys. Psychol. Med. 2017;47(10):1744–1760. doi: 10.1017/S0033291717000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woody S.R., McLean C., Klassen T. Disgust as a motivator of avoidance of spiders. J. Anxiety Disord. 2005;19(4):461–475. doi: 10.1016/j.janxdis.2004.04.002. [DOI] [PubMed] [Google Scholar]
- Zsido A.N., Teleki S.A., Csokasi K., Rozsa S., Bandi S.A. Development of the short version of the spielberger state—trait anxiety inventory. Psychiatr. Res. 2020;291 doi: 10.1016/j.psychres.2020.113223. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data associated with this study has been deposited at https://osf.io/nmh4r/