Abstract
Introduction
The COVID-19 pandemic context led to a relevant burden on essential sectors of society; hospital sector capacity is tested in this period.
Methods
A cross-sectional study of admissions in hospitals reporting DRG data for 2018-2020. Trend analysis of admissions and deaths in hospitals was carried out for identifying annual patterns and deviations from the 2010-2020 trend. Data aggregated by year, month, diagnosis, death in hospital. Graph analysis for time and diagnosis comparisons and correlation identifying associations.
Results
There is an annual change in admission and death patterns recorded in Romanian hospitals. An important contraction in number of acute hospital admissions was recording during the COVID-19 pandemic; patients’ hesitancy to seek healthcare and limited capacity to treat patients other than COVID-19 patients due to legal regulations limiting the admissions number could explain this pattern of admission only for serious condition or emergency surgery. In Romania excess deaths in second half 2020 was generally greater than COVID-19 deaths. Overall, excess mortality between March and December 2020 was more than double than reported COVID-19 deaths. The same mortality pattern persists, but with significant decreases for some diagnoses.
Conclusions
The Romanian healthcare system has been challenged due to COVID-19 pandemic, leading to temporary reorganization of hospitals with consequences on all acute care diagnostics and therapeutic pathways. It is a challenge to identify causes of reduced inpatient treatment rates and to provide evidence on hospital activity for understanding future optimal management of patients with COVID-19, but also with other acute and chronic conditions.
Keywords: COVID-19, burden, hospitalization, indicators, Romania
Introduction
Current evidence shows COVID-19 is burdensome for society and this can be reflected in the values of complex indicators. Life expectancy in Romania declined by 1.3 years in 2020 because of COVID-19, following an increase by more than four years between 2000 and 2019. COVID-19 put also a great pressure on the main sectors of the system. Testing capacity did not keep pace with community transmission, and during the pandemic excess deaths outnumbered COVID-19 deaths, indicating underreporting of the latter.1 Owing to the dominance of hospital care, the pressures of COVID-19 on hospitals undermined access to non-COVID-19 care, leading to a higher proportion of people forgoing care in Romania than across the EU in the first year of the pandemic, i.e. 29% in Romania vs. 21% in EU.2
For Romania, per capita spending on prevention is the second lowest in the EU.3 This meant that, prior to the pandemic public health was under-resourced and underperforming. Health spending on primary care is also the lowest in absolute terms among EU countries.3 The weakness of primary care and prevention may explain Romania’s high excess mortality rates from COVID-19 reported in hospitals almost entirely. In the second half of 2020, the number of excess deaths in Romania was much higher than the number of reported COVID-19 deaths, indicating the COVID-19 deaths were being undercounted.2,4
Thus, in the context of pandemic, hospital sector is one of the main health sectors under pressure and the capacity and ability to cope with such a situation can be overcome in a fairly short time. Although, generally, the hospital activity does not change very frequently, there are modest fluctuations in terms of volume of activity (i.e., seasonal or annual variations, collective emergencies etc.), diversity in services offered to patients (i.e., change in access of population) or variations in productivity and performance or variations in outcomes.
Normally, the organization and operation of a hospital is expected to cope with these modest fluctuations, and sometimes the level of flexibility of a hospital must prove the resolution of these situations. In this sense, there is evidence that organizational and management techniques can be used effectively to address unwarranted variation.5,6
A great challenge for proving the flexibility of a hospital, respectively of an entire hospital system is represented by the current pandemic context due to COVID-19 leading to modulations in providing different acute care inpatients7,8 and in proving the capacity of a health system to respond rapidly to a new health threat and in convergence with international efforts.
The decision-making process must be evidence based and in terms of COVID-19 this evidence is early and incomplete. Even if there are a lot of studies focused on hospital admissions and deaths in the context of the COVID-19 pandemic,9-11 for Romania there is a gap in evidence and it requires the production of such evidence in order to have a real image at national level.
This study aims to provide scientific evidence by investigating in a comparative manner: 1) the main causes of admissions and deaths in hospitals reporting data at patient level for the period 2018-2020 and 2) the impact of COVID-19 on the volume and distribution of in-hospital morbidity and mortality.
Methods
This is a cross-sectional study of admissions in hospitals that report data in the national DRG (diagnosis-related group) system. All admissions in the 513 Romanian hospitals reporting clinical data in the DRG National database for the period 2018-2019-2020 (secondary data) were included, in order to compare the patterns of in-hospital morbidity and mortality between pre-pandemic and pandemic periods. In Romania, the DRG system for hospitals dates from 2003 (adaptation to US system) with a switch in 2007 (to Australian system) and a version adopted by Romania in 2010 using the same International Classification of the Diseases. All Romanian hospitals report monthly data to the National DRG Database that is managed by the National School of Public Health, Management and Professional Development (NSPHMPDB) in Bucharest.12
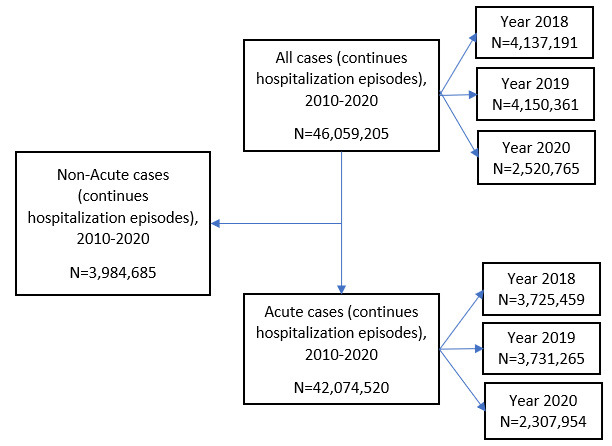
The survey sample included all continuous hospitalization episodes discharged from Romanian hospitals (Figure 1) reporting clinical data at patient level in 2018, 2019 and 2020. For the year 2020, the periods are analyzed belong to pre-pandemic period (1 January to mid-March 2020), National Emergency Status (mid-March to mid-May 2020) and National Alert Status (mid-May to 31 December 2020).
Figure 1. Study flow-diagram showing data extraction process.
A trend analysis of total number of admissions and deaths in the Romanian hospitals was carried out in order to provide a whole image and for identifying annual patterns from the trend in the period 2010-2020 and deviations from this trend recorded in 2020. Data on number of admissions (patients with >12 hours of hospital stay) and number of deaths (patients with discharge status: deceased) were extracted, compared and aggregated at national level, by year and by month (for the last three years: 2018-2020), and by main discharge diagnosis – where COVID-19 was coded for all episodes with U07.1 and U07.2 codes as diagnostic (primary or secondary) – or DRGs for patients admitted, respectively died in hospital.
The expected values were calculated on the baseline from previous years (linear regression), assuming that the model of morbidity, respectively of mortality from the previous years would have been preserved in 2020. The excess of in-hospital deaths related to 2020 was calculated as the difference between the observed deaths (at the level of 2020) and the deaths from the previous period (as average of 2018-2019), by using a P-score using two-years average baseline method. Statistic tests (t-test for means, z-test for distribution; Pearson correlation for numeric variables) were used for comparation. Graph analysis was used for time and diagnosis comparisons, and correlation analysis was used to identify associations between two variables. All analyses were performed using SPSS version 20.0 and p<0.05 was considered statistically significant.
Results
In-hospital admissions analysis
The annual trend
The analysis of the absolute admissions through each study period according to data at patient level reported by about the 513 hospitals shows a slight decrease in number of acute discharged cases in the pre-pandemic period, from 4,717,904 in 2010 to 3,731,265 cases in 2019; a constant value of about 3700000 acute cases was recorded for the period 2016-2019); In contrast, there is an abrupt decrease in 2020 so that the value reached in 2020 a total of 2,307,954 acute hospitalized cases that represents only 61.8% from the value recorded in 2019 (Figure 2).
Figure 2. Trend of in-hospital admissions and deaths, Romania, 2010-2020.
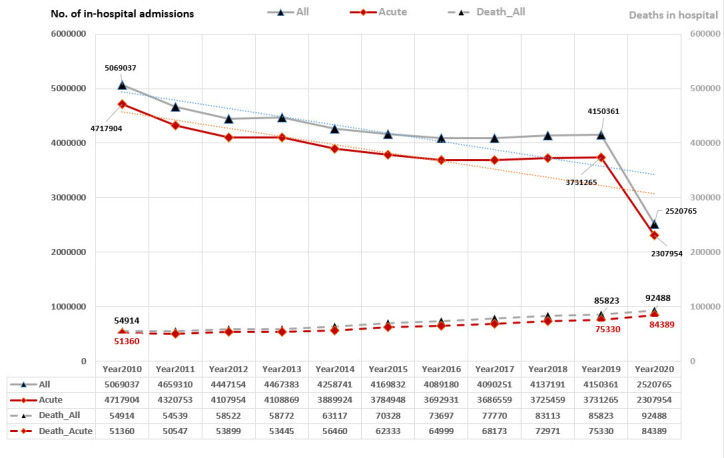
Expected values were calculated using a linear regression model
The monthly trend in 2020
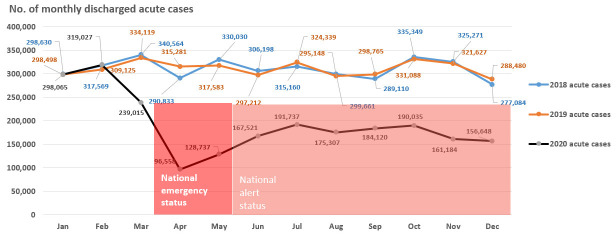
The cumulative number of hospitalizations in the first two months of 2020 was slightly higher than the similar period in previous years, but this trend was abruptly interrupted so that admissions were significant below (t-test; p>0.05) the expected monthly levels for the period following the first two months of the year 2020 (Figure 3).
Figure 3. No. of discharged cases, by month, in 2018-2020, Romania.
The first significant decrease was encountered in March 2020, with 71.5% from the value expected (239,015 in March 2020 vs. 334,119 acute admissions in March 2019); the most drastic decrease was recorded in April 2021 (only 30.6% from the expected value) and May 2021 (only 40.5% from he expected value) which corresponds to the period of National emergency status that was established for a period of two consecutive months (April and May 2021) with important restrictions on hospital admissions regulations.13
According to this order, in addition to organizational measures for the management of patients with COVID-19 (support networks for the infectious diseases hospital), the hospitalizations scheduled for the next period were limited, in relation to the level of bed occupancy, including intensive care unit (ICU) beds and the local epidemiological evolution as follows:
Planned hospitalizations are reduced by up to 80%, such as planned surgeries for chronic patients in university centers hospitals, and by up to 50% for outpatient units, compared to February 2020.
Hospitals will report day-to-day in the centralized electronic system of the Ministry of Health the rate of bed occupancy.13
The following period of the year 2020 corresponds to the National alert status (with fewer general restrictions that are stipulated in the Law no. 55 of May 15, 2020 on some measures to prevent and combat the effects of the COVID-19 pandemic and subsequent decisions) and it was characterized by monthly values ranging from 50.1% (November) to 61.6% (September) from the monthly expected values (Figure 3).
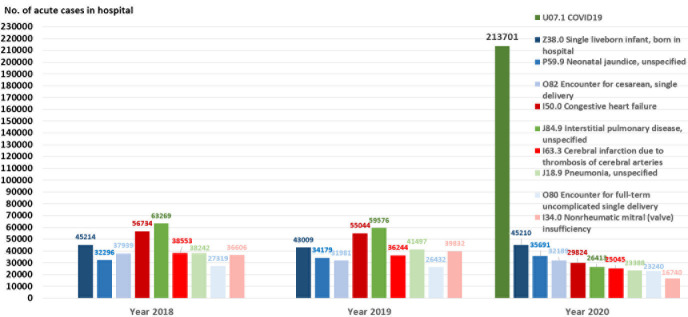
Main causes of admissions (discharge diagnosis) in hospitals
The comparative analysis of the first 10 DRGs registered in the last three years highlights major changes (both in terms of top position and absolute number and distribution) of the main diagnoses representing the reasons for hospitalizations in 2018, 2019 and 2020 (Figure 4).
Figure 4. Main discharge diagnoses in hospitals (grouped in DRGs), Romania, 2018-2020.
A first finding consists in existence of many similarities between the top 10 DRGs in 2018 and top 10 DRGs in 2019 (in term of positions and weights).
For 2020, the most significant change is the emergence of DRGs related to COVID-19 (U07.1 and U07.2) which positions this pathological condition on the first place in the top with a number of admissions almost equal to the sum of the other pathologies in the top 10 for 2020.
The next DRGs in the top 2020 occupy different places, with different weights and levels measured as the number of acute admissions, compared to previous years (2018 and 2019):
„Interstitial pulmonary disease”, unspecified, which ranked first in 2018 and 2019 is ranked 5th in 2020; „Congestive heart failure” which was on the 2nd place in 2018 and 2019 and reaches the 4th place in 2020; „Pneumonia, unspecified”, on 3rd and 4th place in 2018 and 2019 is placed on the 7th place in 2020.
As can be seen in Figure 4, in terms of number of admissions, there is no significant decrease (t-test; p<0.05) for births (spontaneous or by cesarean section), but for the rest of DRGs in the top 10, the number of admissions has almost halved.
In-hospital deaths analysis
The annual trend
From the time trend analysis on the number of hospital deaths, two distinct periods can be observed: the pre-pandemic period (the last ten years before the COVID-19 pandemic: 2010-2019) and the 2020 pandemic period.
In terms of absolute numbers of hospital deaths, the trend does not suggest a steep increase for the last year, but only a significant increase that can be attributed to deaths by COVID-19 (t-test; p<0.05).
Instead, in terms of in-hospital mortality rates, the figures suggest an in-depth analysis to identify changes in the in-hospital mortality model. If for the pre-pandemic period there was an increase of 1%, from 1.1% to 2.1% (corresponding to a growth rate of only 0.1% per year), only for the last year 2020 it was recorded an annual increase of 1.6% (from 2.1% in 2019 to 3.6% in 2020) – Figure 5. Much of this abrupt increase in hospital mortality is explained by the high rate of hospitalization through COVID-19, but a comparative analysis of the main pathologies for which the deceased patients were hospitalized may be relevant and our study continued to focus on this analysis. In order to have a larger image on mortality in Romania, it is worth to mention the deaths in hospitals represent about 31.5% (in 2018), 33.0% (in 2019) and 31.1% (in 2020) of all deaths in general population in Romania.
Figure 5. Trend of in-hospitals deaths, Romania, 2010-2020.
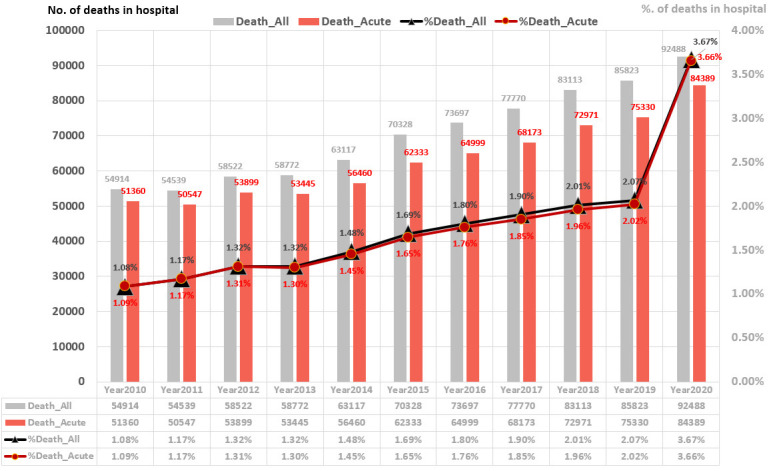
Death_All = All in-hospital deaths. Death_Acute = All deaths for acute cases.
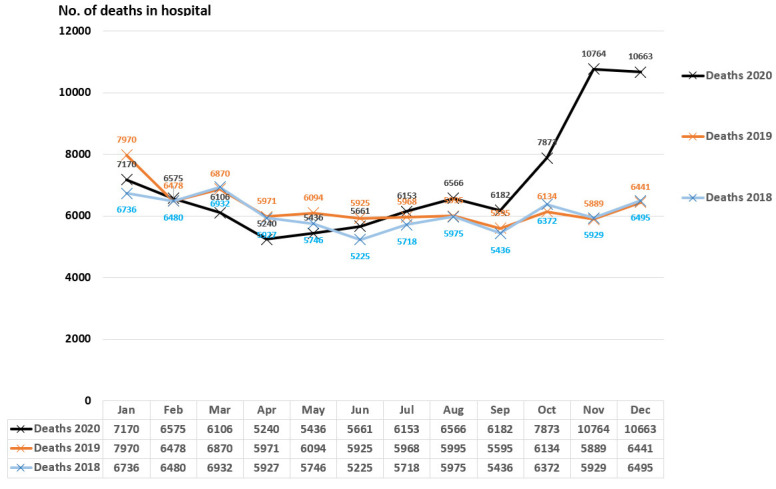
The monthly trend
There is an excess of mortality for October-November-December 2020 (almost doubling the number of in-hospital deaths compared to the expected deaths), although until May the level of hospital deaths was below the multiannual values; this finding appears against the background of a direct correlation between the share of positive patients and the share of deaths in the total number of hospitalizations during November 2020 – January 2021 (corr = 0.8; p>0.05) and in correlation with other findings.14
It is expected this excess to be attributable to COVID-19, but deepening the analysis on the main diagnoses of the deceased is useful.
Main discharge diagnoses of in-hospital deaths
The comparative analysis for the last three years of the analyzed period (2018, 2019 and 2020) on the first 10 DRGs registered as main diagnosis for patients who died in hospital during hospitalization does not highlight major changes (Figure 6).
Figure 6. Monthly trend of in-hospital deaths, Romania, 2018-2019-2020.
If we exclude deaths with COVID-19 (which by far places COVID-19 on the first position of the top diagnoses of patients who died in hospital), the top 10 in 2020 looks very similar to the top 10 in previous years, both in terms of positions and absolute number of deaths) – Figure 7.
Figure 7. Main discharge diagnoses of patients who died in hospital, Romania, 2018-2019-2020.
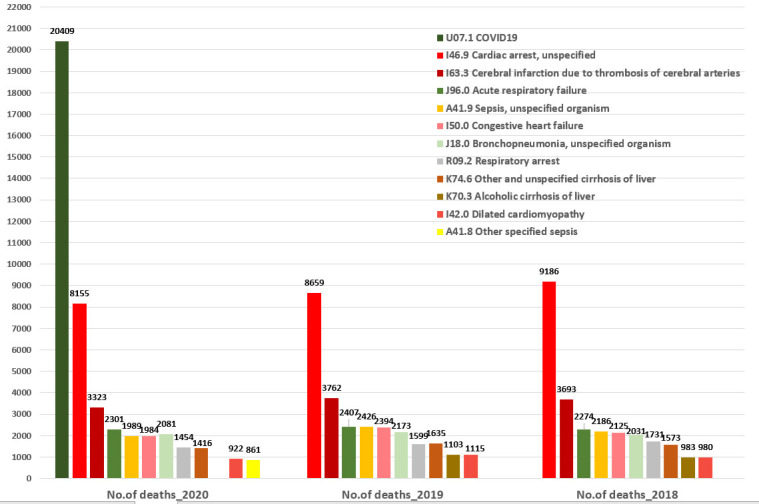
As a general trend, it is worth mentioning that, compared to 2019, the number of deaths of patients with the main diagnosis in the top 10 in 2020 is slightly decreasing, for all positions in the top; the largest decrease (11%-18%) was recorded for: A41.9 Sepsis, unspecified organism; I42.0 Dilated cardiomyopathy; I50.0 Congestive heart failure; K74.6 Other and unspecified cirrhosis of liver and I63.3 Cerebral infarction due to thrombosis of cerebral arteries. The deaths of patients with R09.2 Respiratory arrest and I46.9 Cardiac arrest, unspecified decreased with 9% and respectively 6%. For the rest of positions, the decrease was under 5%.
Discussion
The COVID-19 pandemic resulted in a substantial temporary decline in life expectancy in many countries, including Romania, where it fell by 1.3 years to 74.2 years. In the last six years, these values keep Romania on the last places in the EU, with values below the average for the EU as a whole. In contrast, the average reduction across the EU in 2020 was 0.7 years.
The mortality rate from COVID-19 up to the end of August 2021 was about 12% higher in Romania than the average across EU countries, approximately 1 790 per million population compared with an EU average of about 1 590.2,15 However, the broader indicator of excess mortality suggests that the direct and indirect death toll related to COVID-19 could be substantially higher, placing Romania in the top 10 countries with the highest death rates due to COVID-19 (deaths per 100,000).16 The indicator of excess mortality (defined as the number of deaths from all causes exceeding the number expected based on the baseline from previous years, as regression model) can provide a broader measure of the direct and indirect deaths due to COVID-19 that is less affected by issues related to testing and cause of death registration2,16 and in this sense, this represents a limit of this study (cumulative P-score using projected baseline or P-score by using five-years average baseline methods would allow international comparation). The role of the excess mortality is to identify the impact of the pandemic context on hospital mortality and to see the correlation of this indicator with the excess of deaths in the general population.
There is a lot of evidence highlighting the official number of COVID-19 deaths underestimates the full impact of the pandemic in 2020 and the excess mortality needs to be measured according to a standardized methodology.17-21 In Romania, as in many other countries, the actual number of deaths from COVID-19 is likely to be higher than the number of reported deaths because of limited testing, as well as issues related to the attribution of cause of death.22
Thus, the current reporting of COVID-19 cases and general mortality does not reflect effects of factors such as: a) the reduction in mortality by conditions through conditions generated by reduced mobility associated with social distancing directives; b) the reduction in mortality due to reduced transmission of other viruses c) the reductions in mortality due to some chronic conditions (cardiovascular disorders and chronic respiratory illness) that occur when individuals in poor health who earlier would have died from these conditions died from COVID-19 instead and d) indirect deaths, i.e. possible surges in deaths from other causes that may arise during or after the pandemic – for example, evolving from reduced access to health services for non-COVID-19 patients and fewer people looking for treatment due to fear of catching the virus16,22 and i.e. even high rates of underreporting for COVID-19 cases mainly due to a low testing rate.15-17
Conclusions
The current study comes to cover some gaps in evidence on COVID-19 in-hospital morbidity and in-hospital mortality by interrogating and analyzing data from the DRG National database. In this regard, the results highlighted for Romania the COVID-19 pandemic led to a significant decrease in the volume of hospitalizations and changed the pattern of in-hospital admissions and deaths. Our analysis highlights an important contraction in number of acute hospital admissions was recording during the COVID-19 pandemic. This substantial decrease in hospital activity (with exception of COVID-19) may reflect both: the patients’ hesitancy to seek health care and the limited capacity to treat patients other than COVID-19 patients in 2020, due to the legal regulations which limits the number of admissions in hospitals that treat patients with COVID-19. These two aspects led to hospitalizations only of patients who were in a serious condition or in need of emergency surgery.
Particularly for the year 2020, the absolute number of deaths in hospitals decreased in the National Emergency Status and the months following this period, and then the number of deaths increased sharply after October 2020; in the context of COVID-19, the top 10 deaths remained approximately the same in terms of top positions (same pattern of mortality in hospitals), but with significant decreases for diagnoses such as: A41.9 Sepsis, unspecified organism (18%); I42.0 Dilated cardiomyopathy (17%); I50.0 Congestive heart failure (17%); K74.6 Other and unspecified cirrhosis (13%) of liver and I63.3 Cerebral infarction due to thrombosis of cerebral arteries (12%).
The Romanian healthcare system has been challenged due to the COVID-19 pandemic, which has led to a partial and temporary reorganization of the hospitals with consequences on all acute care diagnostic and therapeutic pathways. It is a challenge to identify justifications for these decreased inpatient rates and to provide evidence on hospital activity; this is important for estimation regarding how patients with COVID-19 but also of patients with other acute and chronic conditions should be managed.
Similar to other available evidence for Romania,14 our study highlights that, in the second half of 2020, the number of excess deaths in Romania was generally greater than that of COVID-19 deaths. Also, the excess mortality between early March and the end of December 2020 was more than double than for reported COVID-19 deaths. A possible explanation for this gap is the limited testing capacity in Romania, which might have left many positive cases unidentified coupled with the excess COVID-19 death rate, respectively deaths not reported as COVID-19 infection; another possible explanation in this increased mortality may be due to needed healthcare being delayed or deferred during the pandemic, especially in a country such as Romania where the health system traditionally relies more on hospital care (rather than primary care) than other EU countries. These possible explanations (including others such as foregone or late treatment) need to be validated by further studies considering all data from the beginning until the end of the pandemic period.
Hence, access to non-COVID-19 hospital care may have been hindered by pressure on the system in treating COVID-19 cases, leading to high rates of excess non-COVID-19 deaths15 and one way to have a clearer image of the impact of the COVID-19 pandemic on the overall morbidity is to take into account, in a comparative manner, the excess mortality.
Footnotes
Authors’ contributions statement: CV designed and supervised the study, analyzed the data, drafted the manuscript. MC conducted the statistical analyses, drafted the manuscript and performed the background literature review for the manuscript. AR collected and analyzed the data and performed the background literature review for the manuscript. All authors read and approved the final version of the manuscript.
Conflicts of interest: All authors – none to declare.
Funding: None to declare.
References
- 1.Eurostat - Data Explorer. 2021. Life expectancy by age and sex. [Accessed on: 24 September 2021]. Available at: https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=demo_mlexpec&lang=en.
- 2.Database - Eurostat. 2021. [Accessed on: 24 September 2021]. Available at: https://ec.europa.eu/eurostat/data/database.
- 3.Vlădescu C, Scîntee SG, Olsavszky V, Hernández-Quevedo C, Sagan A. Romania: Health system review. Health Systems in Transition. 2016;18:1–170. [PubMed] [Google Scholar]
- 4.Vlădescu V. The Romanian health system – perspectives; presentation given at the Medical Sciences Academy online conference: The Romanian health system. Problem. Performance. Perspective; Academia de Știinte Medicale - Academia de Stiinte Medicale Romania’s Zoom Meeting. Facebook; 19.05.2021. [accessed on: 27 September 2021]. Available at: https://www.facebook.com/academiadestiintemedicale/videos/academia-de-stiinte-medicale-romanias-zoom-meeting/507131663977906/
- 5.NHS Confederation. 2013. Changing care, improving quality. [Accessed on: 24 September 2021]. Available at: https://www.nhsconfed.org/publications/changing-care-improving-quality .
- 6.Appleby J, Raleigh V, Frosini F, Bevan G, Gao H, Lyscom T. Variations in health care: the good, the bad, and the inexplicable. London: The King's Fund; 2011. [Google Scholar]
- 7.Antoon JW, Williams DJ, Thurm C, et al. The COVID-19 pandemic and changes in healthcare utilization for pediatric respiratory and nonrespiratory illnesses in the United States. J Hosp Med. 2021;16:294–7. doi: 10.12788/jhm.3608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.König S, Hohenstein S, Meier-Hellmann A, et al. In-hospital care in acute heart failure during the COVID-19 pandemic: insights from the German-wide Helios hospital network. Eur J Heart Fail. 2020;22:2190–201. doi: 10.1002/ejhf.2044. [DOI] [PubMed] [Google Scholar]
- 9.Barcellos DDS, Fernandes GMK, de Souza FT. Data based model for predicting COVID-19 morbidity and mortality in metropolis. Sci Rep. 2021;11:24491. doi: 10.1038/s41598-021-04029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood) 2020;39:2010–7. doi: 10.1377/hlthaff.2020.00980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhaskaran K, Rentsch CT, Hickman G, et al. Overall and cause-specific hospitalisation and death after COVID-19 hospitalisation in England: A cohort study using linked primary care, secondary care, and death registration data in the OpenSAFELY platform. PLoS Med. 2022;19:e1003871. doi: 10.1371/journal.pmed.1003871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vlǎdescu C, Astǎrǎstoae V, Scintee SG. A health system focused on citizen’s needs. Romania. Financing, organization and drug policy. Solutions (II) Rev Rom Bioeticǎ. 2010;8:106–15. [Google Scholar]
- 13.ORDIN 533 29/03/2020 - Portal Legislativ. [Accessed on: 24 September 2021]. Available at: http://legislatie.just.ro/Public/DetaliiDocument/224501 .
- 14.Ghetau V. Criza COVID-19 și criza demograficǎ. “O nenorocire nu vine niciodatǎ singurǎ”. 2021. [Accessed on: 24 September 2021]. Available at: https://www.contributors.ro/criza-covid-19-si-criza-demografica-o-nenorocire-nu-vine-niciodata-singura/
- 15.WHO Regional Office for Europe, European Commission, European Observatory on Health Systems and Policies. 2021. COVID-19 Health Systems Response Monitor, Country assessment: Romania. [Accessed on: 24 September 2021]. Available at: https://www.covid19healthsystem.org/countries/romania/countrypage.aspx .
- 16.Institute for Health Metrics and Evaluation. 2021. Estimation of excess mortality due to COVID-19. [Accessed on: 15 May 2021]. Available at: http://www.healthdata.org/special-analysis/estimation-excess-mortality-due-covid-19-and-scalars-reported-covid-19-deaths.
- 17.ScienceDaily. 2021. Total deaths due to COVID-19 underestimated by 20 percent in U.S. counties, study finds: Deaths caused by indirect effects of the pandemic emphasize the need for policy changes that address widening health and racial inequities. [Accessed on: 08 March 2022]. Available at: https://www.sciencedaily.com/releases/2021/05/210520145335.htm .
- 18.Adam D. The pandemic’s true death toll: millions more than official counts. Nature. 2022;601:312–5. doi: 10.1038/d41586-022-00104-8. [DOI] [PubMed] [Google Scholar]
- 19.Kung S, Doppen M, Black M, et al. Underestimation of COVID-19 mortality during the pandemic. ERJ Open Res. 2021;7:00766–2020. doi: 10.1183/23120541.00766-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Official counts of COVID-19 deaths are underestimated in South Asia: World Bank report. The Times of India; 2021. [Google Scholar]
- 21.Iuliano AD, Chang HH, Patel NN, et al. Estimating under-recognized COVID-19 deaths, United States, March 2020-May 2021 using an excess mortality modelling approach. Lancet Reg Health Am. 2021;1:100019. doi: 10.1016/j.lana.2021.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The Economist. Tracking COVID-19 excess deaths across countries. [Accessed on: 27 September 2021]. https://www.economist.com/graphic-detail/coronavirus-excess-deaths-tracker .