Abstract
Background: Migraine is a primary headache and a complicated neurological disorder with sensory and autonomic abnormalities. Many variables, including genetic and psychological ones, contribute to migraine onset and development. Anxiety and depression are typical psychiatric comorbidities among migraineurs. This kind of comorbidity increased migraine chronicity, treatment effectiveness, and the likelihood of additional comorbidities. The purpose of this research was to determine the prevalence of depression among Saudi migraine sufferers in AlAhsa.
Methods: Descriptive cross-sectional research of 101 migraine patients at King Fahd Hospital-Hofuf, AlAhsa, Saudi Arabia from May to December 2021. Depression was assessed by Patient Health Questionnaire which is a reliable tool (PHQ-9). The PHQ-9 measures the presence and severity of depression. Consider sociodemographic, clinical, and individual variations that impact migraine development and prognosis.
Results: The inclusion criteria were satisfied by 94 migraine patients in total, with a mean age of 36.9 ± 9 years and they are predominantly females 75.5%. The majority of the participants (76.6%) were on medication to relieve migraine attacks and only 13.9% reported that >75% of attacks were relieved by medication. Almost all of the patients (96.8%) used to drink coffee and tea. The prevalence of depression and migraine was revealed to be 42.6% mild and 8.5% severe among the participants. Four statistically significant correlations (p < 0.05) were young age, being female, low level of education at higher risk to have depression compared to another group of migraineurs.
Conclusion: A neurological disorder that commonly causes disability is migraine. Numerous studies have shown that mood disorders and migraines are often co-occurring, and these individuals are more likely to have a migraine-related disability. This research has shown that it is beneficial to prevent psychiatric comorbidity by using PHQ-9 as a regular screening tool for migraine patients.
Keywords: alahsa, saudi arabia, depression, psychological impact, headache, migraine
Introduction
Migraines vary from other headache types by the following symptoms: lasting four to 72 h; unilateral location; pulsing nature; moderate to severe severity; increased by physical activity; and progresses with nausea, vomiting, phonophobia, or photophobia. Aura symptoms may precede migraine headaches [1]. Migraine is also a multifactorial disorder, with hormonal, genetic, environmental, nutritional, and psychological factors, as well as sleep quality, each playing a distinct role [2]. Migraines and headaches are often related to emotional issues. Depression comorbidity is a common psychiatric illness among migraine headache sufferers. According to a meta-analysis of 12 studies [3] the prevalence of depression among migraineurs ranges from 8.6% to 47.9%. Depression in migraineurs is considered a risk factor for chronic migraine headache, resistance to migraine therapies, drug misuse, suicidal behavior connected to psychosocial impairment, and the influence on migraineur quality of life [4-6]. The brains of migraineurs with comorbid depression differ from those of people with just migraine or simply depression. Many migraine neuroimaging studies revealed brain alterations, noted abnormal functions of specific brain regions, and speculated that these regions might contribute to migraine without aura depressive symptoms [7-10]. Recurrent migraine headache episodes, on the other hand, increase the chance of depression [11]. The variations in the symptoms profiles of migraineurs with and without considerable depression were minimal; the incidence of aura symptoms and migraine aggravation by physical activity were more severe in migraineurs with major depression than in those without depression [12]. Cortical spreading depression (CSD) has been proposed as the condition that causes migraine aura [13]. Furthermore, persons who suffer from migraine have a 2.2-4.0 times greater risk of getting depression than the general population [14].
Materials and methods
The outpatient neurology service department at King Fahd Hospital-Hofuf in AlAhsa, Saudi Arabia, was the site of the descriptive, observational, and correlational study. All patients who visited a neurology clinic from May to December 2021 and were diagnosed with a migraine headache and receiving regular follow-up care. A brief description of the study was given to the participants who had autonomy for rejection. The privacy and confidentiality of results were maintained. The criteria for inclusion were adults≥18 years of age and diagnosed with primary migraine by a physician at least 6 months ago and not having other comorbidities or psychiatric illnesses. The patients were given access to an online or paper-based questionnaire. The questionnaire was divided into three sections: the first section asked about biographical information. The second section included both conventional and alternative treatment options that individuals utilized to relieve migraine attacks. The Patient Health Questionnaire serves as the last component for the measurement of the prevalence of depression using scales that have been validated and translated (PHQ-9) into Arabic [15-16]. The PHQ-9 scale is a nine-item test that evaluates the presence and severity of depression during the last two weeks. The PHQ-9 items are graded on a Likert scale of 0 (not at all) to 3 (nearly every day) for each item. According to the PHQ-9, depression scores were divided into five groups: little or no depression (0-4), mild depression (5-9), moderate depression (10-14), moderate-severe depression (15-19), and severe depression (20-27).
Data analysis
The data were collected, reviewed, and then fed to Statistical Package for Social Sciences version 21 (IBM Corp., Armonk, NY). All statistical methods used were two-tailed with an alpha level of 0.05 considering significance if the p-value is less than or equal to 0.05. As for PHQ-9, the overall score was obtained by summing all discrete scores for the items which ranged from 0 to 24 points. Participants’ classification according to depression severity was applied in reference to the scale documented cut-off points. Descriptive analysis was done by prescribing frequency distribution and percentage for study variables including participants' bio-demographic data, using drugs and other methods to relieve migraine attacks, medical history, and PHQ-9 items, with depression prevalence and severity. Cross tabulation for showing the distribution of participants’ depression severity according to their bio-demographic data was carried out with the Pearson chi-square test for significance and exact probability test for small frequency distributions.
Results
A total of 94 participants fulfilling the inclusion criteria with clinically diagnosed migraine completed the study questionnaire. Participants' ages ranged from 18 to more than 45 years with a mean age of 36.9 ± 12.4 years old. Exactly 70 participants (74.5%) were females. Single participants were 19 (20.2%) while 70 (74.5%) were married. As for education, 62 (66%) participants were university graduates and 23 (24.5%) had below university level of education. Exactly 50 (53.2%) participants were not employed, 30 (31.9%) were non-healthcare workers or students and 14 (14.9%) were healthcare workers/students. A monthly income of less than 5000 SR was reported among 28 (29.8%) participants, and 30 (31.9%) had a monthly income of 5000-10000 SR. Exactly 16 (17%) participants complained of chronic health problems (Table 1).
Table 1. Socio-demographic data of study participants with migraine, Al-Ahsa, Saudi Arabia.
| Socio-demographic data | Count | Column N % |
| Age in years | ||
| < 25 | 16 | 17.0% |
| 25-35 | 30 | 31.9% |
| 36-45 | 31 | 33.0% |
| > 45 | 17 | 18.1% |
| Gender | ||
| Male | 24 | 25.5% |
| Female | 70 | 74.5% |
| Marital status | ||
| Single | 19 | 20.2% |
| Married | 70 | 74.5% |
| Divorced / widow | 5 | 5.3% |
| Educational level | ||
| Below university | 23 | 24.5% |
| University | 62 | 66.0% |
| Post graduate | 9 | 9.6% |
| Job title | ||
| Not employed | 50 | 53.2% |
| Non-healthcare worker / student | 30 | 31.9% |
| Healthcare worker / student | 14 | 14.9% |
| Monthly income | ||
| < 5000 SR | 28 | 29.8% |
| 5000-10000 SR | 30 | 31.9% |
| 10000-20000 SR | 27 | 28.7% |
| > 20000 SR | 9 | 9.6% |
| Have chronic health problem | ||
| Yes | 16 | 17.0% |
| No | 78 | 83.0% |
Drugs and methods used by study participants to relieve migraine attacks, Al-Ahsa, Saudi Arabia. Exactly 72 (76.6%) participants reported using drugs to relieve migraine attacks. The attack severity was relieved by less than 25% of its severity among 24 (33.3%) of them, while 23 (31.9%) reported relief of 25%-50%, and only 10 (13.9%) were relieved by more than 75%. As for alternative methods, 33 (35.1%) reported using Islamic therapy (Ruqia, Quran), 30 (31.9%) used traditional medicine (herbs), and 24 (25.5%) used Cupping therapy, while 24 (25.5%) did not use any of them. Among users, attack severity was relieved by less than 25% among 34 (48.6%), while 10 (14.3%) relived by more than 75%. Smoking was reported among 10 (10.6%) participants while 91 (96.8%) had coffee and tea but soft drinks were taken among 29 (30.9%) (Table 2).
Table 2. Drugs and methods used by study participants to relieve migraine attacks, Al-Ahsa, Saudi Arabia.
| Methods | No | % |
| Had drugs to relief migraine attacks | ||
| Yes | 72 | 76.6% |
| No | 22 | 23.4% |
| Degree of improvement in migraine attacks after having treatments | ||
| < 25% | 24 | 33.3% |
| 25-<50% | 23 | 31.9% |
| 50-75% | 15 | 20.8% |
| > 75% | 10 | 13.9% |
| Alternative medicine usage | ||
| Traditional medicine (herbs) | 30 | 31.9% |
| Chinese acupuncture | 5 | 5.3% |
| Cupping therapy | 24 | 25.5% |
| Islamic therapy (Ruqia, Quran) | 33 | 35.1% |
| Others | 13 | 13.8% |
| None | 24 | 25.5% |
| Degree of improvement in migraine attacks after these methods | ||
| < 25% | 34 | 48.6% |
| 25-<50% | 13 | 18.6% |
| 50-75% | 13 | 18.6% |
| > 75% | 10 | 14.3% |
| Usage any of the following frequently | ||
| Smoking | 10 | 10.6% |
| Power and soft drinks | 29 | 30.9% |
| Tea and coffee | 91 | 96.8% |
Distribution of patients’ health questionnaire items among study participants with migraine, Al-Ahsa, Saudi Arabia. Exactly 89.4% of the participants reported experiencing trouble concentrating on things, 85.1% felt tired or having little energy, 81.9% had little interest or pleasure in doing things, and 81.9% had trouble falling or staying asleep, or sleeping too much. Only 31.9% had thoughts that they would be better off dead or hurting themselves (Table 3).
Table 3. Distribution of PHQ items among study participants with migraine, Al-Ahsa, Saudi Arabia.
PHQ, Patient Health Questionnaire
| PHQ-9 items | Not at all | Several days | More than half the days | Nearly every day | ||||
| No | % | No | % | No | % | No | % | |
| Little interest or pleasure in doing things | 17 | 18.1% | 53 | 56.4% | 23 | 24.5% | 1 | 1.1% |
| Feeling down, depressed, or hopeless | 22 | 23.4% | 41 | 43.6% | 26 | 27.7% | 5 | 5.3% |
| Trouble falling or staying asleep, or sleeping too much | 17 | 18.1% | 37 | 39.4% | 24 | 25.5% | 16 | 17.0% |
| Feeling tired or having little energy | 14 | 14.9% | 36 | 38.3% | 29 | 30.9% | 15 | 16.0% |
| Poor appetite or overeating | 19 | 20.2% | 35 | 37.2% | 27 | 28.7% | 13 | 13.8% |
| Feeling bad about yourself or that you are a failure or have let yourself or your family down | 48 | 51.1% | 21 | 22.3% | 19 | 20.2% | 6 | 6.4% |
| Trouble concentrating on things | 10 | 10.6% | 47 | 50.0% | 22 | 23.4% | 15 | 16.0% |
| Moving or speaking so slowly that other people could have noticed. Or the opposite being so fidgety or restless that you have been moving around a lot more than usual | 28 | 29.8% | 40 | 42.6% | 17 | 18.1% | 9 | 9.6% |
| Thoughts that you would be better off dead, or of hurting yourself | 64 | 68.1% | 11 | 11.7% | 15 | 16.0% | 4 | 4.3% |
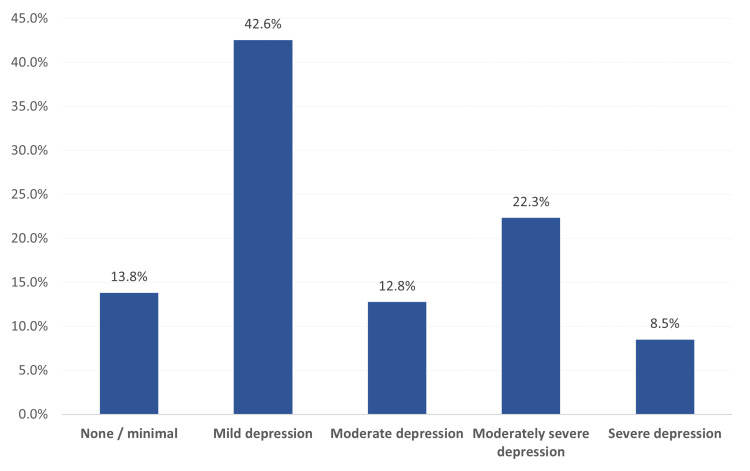
Degree of depression among study participants with migraine, Al-Ahsa, Saudi Arabia. Exactly 13 (13.8%) of the study participants with migraine had no or minimal depression, 40 (42.6%) had mild depression, 12 (12.8%) had moderate depression, 21 (22.3%) complained of moderately degree depression, and 8 (8.5%) had severe depression (Figure 1).
Figure 1. Degree of depression among study participants with migraine, Al-Ahsa, Saudi Arabia.
Distribution of depression severity among participants with migraine by their bio-demographic data. Exactly 68.8% of migraine patients aged less than 25 years had severe depression compared to 23.5% of those who were aged 45 years or more with recorded statistical significance (p=0.030). Also, severe depression was detected among 34.3% of females with migraine in comparison to 20.8% of males (p=0.005). About 39.1% of participants with below university education had severe depression compared to 33.3% of those with post-graduate degree (p=0.002). Severe depression was detected among 35.7% of participants with low income compared to 11.1% of those with the highest income level (p=0.004) (Table 4).
Table 4. Distribution of depression severity among participants with migraine by their bio-demographic data.
*p < 0.05 (significant)
| Degree of depression | p-value | |||||||
| None / minimal | Mild / moderate | Severe depression | ||||||
| No | % | No | % | No | % | |||
| Age in years | < 25 | 0 | 0.0% | 5 | 31.3% | 11 | 68.8% | 0.030* |
| 25-35 | 5 | 16.7% | 19 | 63.3% | 6 | 20.0% | ||
| 36-45 | 5 | 16.1% | 18 | 58.1% | 8 | 25.8% | ||
| > 45 | 3 | 17.6% | 10 | 58.8% | 4 | 23.5% | ||
| Gender | Male | 8 | 33.3% | 11 | 45.8% | 5 | 20.8% | 0.005* |
| Female | 5 | 7.1% | 41 | 58.6% | 24 | 34.3% | ||
| Marital status | Single | 1 | 5.3% | 8 | 42.1% | 10 | 52.6% | 0.059 |
| Married | 12 | 17.1% | 42 | 60.0% | 16 | 22.9% | ||
| Divorced / widow | 0 | 0.0% | 2 | 40.0% | 3 | 60.0% | ||
| Educational level | Below university | 2 | 8.7% | 12 | 52.2% | 9 | 39.1% | 0.002* |
| University | 6 | 9.7% | 39 | 62.9% | 17 | 27.4% | ||
| Post graduate | 5 | 55.6% | 1 | 11.1% | 3 | 33.3% | ||
| Job title | Not employed | 3 | 6.0% | 27 | 54.0% | 20 | 40.0% | 0.081 |
| Non-healthcare worker / student | 7 | 23.3% | 18 | 60.0% | 5 | 16.7% | ||
| Healthcare worker / student | 3 | 21.4% | 7 | 50.0% | 4 | 28.6% | ||
| Monthly income | < 5000 SR | 3 | 10.7% | 15 | 53.6% | 10 | 35.7% | 0.004* |
| 5000-10000 SR | 0 | 0.0% | 19 | 63.3% | 11 | 36.7% | ||
| 10000-20000 SR | 5 | 18.5% | 15 | 55.6% | 7 | 25.9% | ||
| > 20000 SR | 5 | 55.6% | 3 | 33.3% | 1 | 11.1% | ||
| Diseases | Yes | 1 | 6.3% | 12 | 75.0% | 3 | 18.8% | 0.216 |
| No | 12 | 15.4% | 40 | 51.3% | 26 | 33.3% | ||
| Had drugs to relief migraine attacks | Yes | 7 | 9.7% | 41 | 56.9% | 24 | 33.3% | 0.105 |
| No | 6 | 27.3% | 11 | 50.0% | 5 | 22.7% | ||
| Degree of improvement in migraine attacks after having treatments | < 25% | 0 | 0.0% | 16 | 66.7% | 8 | 33.3% | 0.190 |
| 25-<50% | 4 | 17.4% | 11 | 47.8% | 8 | 34.8% | ||
| 50-75% | 1 | 6.7% | 7 | 46.7% | 7 | 46.7% | ||
| > 75% | 2 | 20.0% | 7 | 70.0% | 1 | 10.0% | ||
| Alternative medicine usage | Traditional medicine (herbs) | 6 | 20.0% | 14 | 46.7% | 10 | 33.3% | 0.282 |
| Chinese acupuncture | 0 | 0.0% | 1 | 20.0% | 4 | 80.0% | ||
| Cupping therapy | 4 | 16.7% | 13 | 54.2% | 7 | 29.2% | ||
| Islamic therapy (Ruqia, Quran) | 3 | 9.1% | 18 | 54.5% | 12 | 36.4% | ||
| Others | 3 | 23.1% | 9 | 69.2% | 1 | 7.7% | ||
| None | 3 | 12.5% | 15 | 62.5% | 6 | 25.0% | ||
| Usage any of the following frequently | Smoking | 3 | 30.0% | 5 | 50.0% | 2 | 20.0% | 0.306 |
| Power and soft drinks | 1 | 3.4% | 19 | 65.5% | 9 | 31.0% | ||
| Tea and coffee | 13 | 14.3% | 50 | 54.9% | 28 | 30.8% | ||
Discussion
The current study was conducted to explore the psychological impacts of migraine headaches in Al-Ahsa, Saudi Arabia and to detect factors associated with migraine-related psychological factors. People who complain of frequent attacks of migraines are more likely to have mental health issues such as depression and anxiety [17-19]. Persons experiencing migraines are three times more likely to have depression, mainly if the migraine attacks are frequent [20]. Around 30%-50% of people with chronic migraines also develop anxiety, and 20% of those dealing with episodic migraines less than 15 occurrences per month have anxiety, too. There is also some evidence that migraines frequently co-occur with bipolar disorder [21].
The current study showed that depression with different degrees was detected among 86.2% of the migraine-diagnosed participants. It was mild depression among 42% and severe among 30.8% of the participants. The most reported mental health issue among participants was that they experienced trouble concentrating on things, feeling tired or having little energy, having little interest or pleasure in doing things, experiencing trouble falling or staying asleep, or sleeping too much. All were reported among more than three-quarters of the participants with migraine. As for determinants of depression among migraine patients, the study showed that young age, female gender, low educational level, low economic status, and separation were the most significant factors. A lower prevalence of depression was estimated by Dueland et al., who conducted a multinational study and found that 44% of adult females felt depressed because of their migraines [22]. Feeling of frustration due to migraine ranged from 32% in Italy to 84% in Finland; anxiety ranged from 21% in Norway to 57% in Italy, and feelings of confusion ranged from 13% in Greece to 61% in Italy. Also, Yalinay Dikmen et al. estimated that the most common illness among migraine patients was anxiety disorder (38%), followed by depressive disorders (26%), which is much lower than the estimated prevalence by the current study [23]. Jeyagurunathan et al. found that migraine headache was significantly associated with major depressive disorder [prevalence ratio (PR=1.8), bipolar disorder (PR=3.55), generalized anxiety disorder (PR=2.04), and obsessive compulsive disorder (PR=2.20)] [24]. Amouroux and Rousseau-Salvador, reviewed the literature to test for this relationship and concluded that most of the population studies show slightly higher scores on at least one of the anxiety or depression scales in the migraine group as compared to the control group [25]. However, the average score on anxiety and depression among children with migraines was below the pathological level, according to the norms established by the validated scales [14]. Therefore, specific authors use the term "sub-clinical.” Merikangas et al. assessed depression among adults in Zurich and stated a strong association between migraine and depression [odds ratio (OR) 2.2; 95% confidence interval (CI) 1.1-4.8], with an even stronger association between migraine and anxiety disorders (OR 2.7; 95% CI 1.5-5.1) [17]. Hamelsky and Lipton and Peterlin et al. found that persons with migraine had two to five times more likelihood of developing a depressive or anxiety disorder [20, 26]. With adjustment for the other chronic conditions, migraine continued to be significantly related to all psychiatric disorders compared to those without migraine, which is consistent with many other studies [27-28].
As for methods used to relieve migraine attacks associated with pain, the current study showed that three out of each four participants with migraine used drugs with reported low relief percent (<50%). Also, nearly one-third of them used herbs, Islamic therapy for relieving the pain, besides drugs. Cupping therapy was used by one-quarter of the participants, and many of them used more than one method. About half of those participants reported poor attack severity improvement with the methods used.
Limitations
Our study's findings have certain limitations. First, as our data were cross-sectional, we were unable to evaluate the direction of the relationship between depression subtypes and migraine intensity. To evaluate the chronological sequence between the development of depression and migraine, longitudinal investigations are necessary. Another limitation is the relatively small number of sample size. They vary in gender proportions as the majority of the participants were females; thus, future research should include more men. There are also variances in comorbidity, disability, pain severity, and frequency of episodes. We did not make a distinction between episodic and chronic migraine, or between migraine with and without aura. Further retrospective and bidirectional research with a large sample size are recommended to investigate this disparity.
Conclusions
The current study established that migraine headache is a significant disorder associated with a higher occurrence of psychiatric disorders, especially depression and anxiety. Drug-induced pain relief was poor and alternative methods were also used with no satisfactory relief of pain attacks. These findings can help to create awareness and encourage comprehensive synchronized methods for the management of migraine in healthcare settings. Migraine-associated depression was higher among females, youth, and low socio-economic categories.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. King Fahad Hospital-Hofuf, AlAhsa, Saudi Arabia issued approval Non. Informed consent was obtained from all the participants after describing the aim of the study, and the participants had autonomy for rejection. Privacy and confidentiality of results maintained. Official permission was obtained from the Institutional Review Board (IRB) of King Fahad Hospital-Hofuf, AlAhsa, Eastern province of Saudi Arabia.
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.The International Classification of Headache Disorders, 3rd edition (beta version) Headache Classification Committee of the International Headache Society (IHS) Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 2.Anxiety and depression symptoms and migraine: a symptom-based approach research. Peres MF, Mercante JP, Tobo PR, Kamei H, Bigal ME. J Headache Pain. 2017;18:37. doi: 10.1186/s10194-017-0742-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Migraine and psychiatric comorbidity: a review of clinical findings. Antonaci F, Nappi G, Galli F, Manzoni GC, Calabresi P, Costa A. J Headache Pain. 2011;12:115–125. doi: 10.1007/s10194-010-0282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Depression and risk of transformation of episodic to chronic migraine. Ashina S, Serrano D, Lipton RB, et al. J Headache Pain. 2012;13:615–624. doi: 10.1007/s10194-012-0479-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Traditional and alternative treatments for depression: implications for migraine management. Peck KR, Smitherman TA, Baskin SM. Headache. 2015;55:351–355. doi: 10.1111/head.12521. [DOI] [PubMed] [Google Scholar]
- 6.Psychiatric comorbidity in the evolution from migraine to medication overuse headache. Radat F, Creac'h C, Swendsen JD, Lafittau M, Irachabal S, Dousset V, Henry P. Cephalalgia. 2005;25:519–522. doi: 10.1111/j.1468-2982.2005.00910.x. [DOI] [PubMed] [Google Scholar]
- 7.A diffusion tensor magnetic resonance imaging study of corpus callosum from adult patients with migraine complicated with depressive/anxious disorder. Li XL, Fang YN, Gao QC, et al. Headache. 2011;51:237–245. doi: 10.1111/j.1526-4610.2010.01774.x. [DOI] [PubMed] [Google Scholar]
- 8.Recalled maltreatment, migraine, and tension-type headache: results of the AMPP study. Tietjen GE, Buse DC, Fanning KM, Serrano D, Reed ML, Lipton RB. Neurology. 2015;84:132–140. doi: 10.1212/WNL.0000000000001120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voxel-based morphometry reveals gray matter abnormalities in migraine. Valfrè W, Rainero I, Bergui M, Pinessi L. Headache. 2008;48:109–117. doi: 10.1111/j.1526-4610.2007.00723.x. [DOI] [PubMed] [Google Scholar]
- 10.Intrinsic brain network abnormalities in migraines without aura revealed in resting-state fMRI. Xue T, Yuan K, Zhao L, et al. PLoS One. 2012;7:0. doi: 10.1371/journal.pone.0052927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Comorbidity of migraine and depression: investigating potential etiology and prognosis. Breslau N, Lipton RB, Stewart WF, Schultz LR, Welch KM. Neurology. 2003;60:1308–1312. doi: 10.1212/01.wnl.0000058907.41080.54. [DOI] [PubMed] [Google Scholar]
- 12.Migraine symptomatology and major depressive disorder. Ligthart L, Penninx BW, Nyholt DR, et al. Cephalalgia. 2010;30:1073–1081. doi: 10.1177/0333102410363492. [DOI] [PubMed] [Google Scholar]
- 13.Microemboli may link spreading depression, migraine aura, and patent foramen ovale. Nozari A, Dilekoz E, Sukhotinsky I, et al. Ann Neurol. 2010;67:221–229. doi: 10.1002/ana.21871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Migraine and psychopathology. Results of the Zurich cohort study of young adults. Merikangas KR, Angst J, Isler H. Arch Gen Psychiatry. 1990;47:849–853. doi: 10.1001/archpsyc.1990.01810210057008. [DOI] [PubMed] [Google Scholar]
- 15.The PHQ-9: validity of a brief depression severity measure. Kroenke K, Spitzer RL, Williams JB. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.An arabic translation, reliability, and validation of Patient Health Questionnaire in a Saudi sample. AlHadi AN, AlAteeq DA, Al-Sharif E, et al. Ann Gen Psychiatry. 2017;16:32. doi: 10.1186/s12991-017-0155-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Comorbidity of migraine and psychiatric disorders--a national population-based study. Jette N, Patten S, Williams J, Becker W, Wiebe S. Headache. 2008;48:501–516. doi: 10.1111/j.1526-4610.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- 18.On megrim, sick-headache, and some allied disorders, a contribution to the pathology of nerve-storms. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5175726/ Ind Med Gaz. 1873;8:305–306. [Google Scholar]
- 19.Comparison of clinical characteristics of migraine and tension type headache. Gupta R, Bhatia MS. Indian J Psychiatry. 2011;53:134–139. doi: 10.4103/0019-5545.82538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Psychiatric comorbidity of migraine. Hamelsky SW, Lipton RB. Headache. 2006;46:1327–1333. doi: 10.1111/j.1526-4610.2006.00576.x. [DOI] [PubMed] [Google Scholar]
- 21.Stress, anxiety, depression and migraine. Wacogne C, Lacoste JP, Guillibert E, Hugues FC, Le Jeunne C. Cephalalgia. 2003;23:451–455. doi: 10.1046/j.1468-2982.2003.00550.x. [DOI] [PubMed] [Google Scholar]
- 22.The impact of migraine on psychological well-being of young women and their communication with physicians about migraine: a multinational study. Dueland AN, Leira R, Cabelli ST. Curr Med Res Opin. 2005;21:1297–1305. doi: 10.1185/030079905X56394. [DOI] [PubMed] [Google Scholar]
- 23.The relationships between migraine, depression, anxiety, stress, and sleep disturbances. Yalinay Dikmen P, Yavuz BG, Aydinlar EI. Acta Neurol Belg. 2015;115:117–122. doi: 10.1007/s13760-014-0312-0. [DOI] [PubMed] [Google Scholar]
- 24.Prevalence and comorbidity of migraine headache: results from the Singapore Mental Health Study 2016. Jeyagurunathan A, Abdin E, Vaingankar JA, et al. Soc Psychiatry Psychiatr Epidemiol. 2020;55:33–43. doi: 10.1007/s00127-019-01755-1. [DOI] [PubMed] [Google Scholar]
- 25.[Anxiety and depression in children and adolescents with migraine: a review of the literature] Amouroux R, Rousseau-Salvador C. Encephale. 2008;34:504–510. doi: 10.1016/j.encep.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 26.The associations between migraine, unipolar psychiatric comorbidities, and stress-related disorders and the role of estrogen. Peterlin BL, Katsnelson MJ, Calhoun AH. Curr Pain Headache Rep. 2009;13:404–412. doi: 10.1007/s11916-009-0066-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Psychiatric morbidity in pain conditions: results from the Singapore Mental Health Study. Subramaniam M, Vaingankar JA, Abdin E, Chong SA. Pain Res Manag. 2013;18:185–190. doi: 10.1155/2013/798205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Depression and anxiety associated with three pain conditions: results from a nationally representative sample. McWilliams LA, Goodwin RD, Cox BJ. Pain. 2004;111:77–83. doi: 10.1016/j.pain.2004.06.002. [DOI] [PubMed] [Google Scholar]