Abstract
Background and Objective
Anxiety influences job burnout and health. This study aimed to establish a nomogram to predict the anxiety status of medical staff during the coronavirus disease (COVID-19) pandemic.
Methods
A total of 600 medical members were randomized 7:3 and divided into training and validation sets. The data was collected using a questionnaire. Logistic regression analysis and Akaike information criterion (AIC) were applied to investigate the risk factors for anxiety. Odds ratio (OR) and 95% confidence interval (95% CI) were calculated to establish a nomogram.
Results
Participation time (OR=44.28, 95% CI=13.13~149.32), rest time (OR=38.50, 95% CI=10.43~142.19), epidemic prevention area (OR=10.16, 95% CI=3.51~29.40), epidemic prevention equipment (OR=15.24, 95% CI=5.73~40.55), family support (OR=9.63, 95% CI=3.55~26.11), colleague infection (OR=6.25, 95% CI=2.18~19.11), and gender (OR=3.30, 95% CI=1.15~9.47) were the independent risk factors (P<0.05) for anxiety in medical staff. The areas under the receiver operating characteristic (ROC) curves of the training and validation sets were 0.987 and 0.946, respectively. The decision curve’s net benefit shows the nomogram’s clinical utility.
Conclusion
The nomogram established in this study exhibited an excellent ability to predict anxiety status with sufficient discriminatory power and calibration. Our findings provide a protocol for predicting and identifying anxiety status in medical staff during the COVID-19 pandemic.
Keywords: nomogram, anxiety, COVID-19, medical staff
Introduction
The COVID-19 outbreak has caused widespread psychological distress among the public. The unexpected nature of the illness, home isolation and confinement, a lack of clarity from authorities about the severity of the risk, or individual emotional spillover are all risk factors for this rise.1,2 The psychological burden is exceptionally high among medical personnel, who face additional group-specific demands.3 Long work hours, strict instructions and safety procedures, a constant need for focus and alertness, restricted social connection, and participation in tasks for which they may not be trained are all examples of exceptionally high job-related stressors.4,5 These stressors have been linked to medical personnel’s emotional distress during the COVID-19 pandemic, which may have become a source of anxiety.6,7 According to recent research, medical professionals may be experiencing the highest levels of anxiety8 because they are often responsible for treating COVID-19 patients and are more psychologically stressed. The fear of getting sick of an increasing virus load, and—most importantly—all types of discourses and approaches that undervalue the work of healthcare professionals who put their health at risk are main contributors to burnout during epidemic periods like COVID-19. People who work in fields like “health”, which directly benefit people and place a premium on interpersonal relationships, are more likely to experience burnout.9,10 Anxiety is a risk factor for job burnout.11–13 In addition, medical staffs are prone to anxiety when encountering emergencies.10,14–16 Since December 2019, novel coronavirus pneumonia (COVID-19) has broken and swept worldwide.17
Physicians, nurses, and other healthcare professionals who have frequent contact with patients may experience stress, anxiety, and burnout, which may impair their ability to perform their jobs, deteriorate their health and lower their quality of life. When it comes to healthcare workers, the anxiety that develops during or after a crisis intervention may affect their capacity for abstract thought, mental reasoning, and coordination. Their ability to solve problems can be impacted by various emotions, including fear and anxiety. Reduced problem-solving skills could result in less effective services being offered to safeguard public health, improve living conditions, and protect individual health.7,18,19
Therefore, it is significantly necessary to identify and predict anxiety in medical staff early, which contributes to reasonable and optimized medical staff configuration during COVID-19 pandemic. Herein, a cross-sectional study was conducted to identify anxiety in medical staff during epidemic prevention and mediating risk factors. Study employed a questionnaire collecting the data of participants, which included basic information (age, gender, marital status, occupation, professional title, hospital level, educational background), information relevant to work against COVID-19 (workplace, participation time, convenience of traffic, case of colleague infection, family supports as well as sufficient or insufficient mask, isolation clothes and salary) and Hamilton anxiety scale. Following data generated from respondents, a nomogram was established and validated internally and externally. Results in this study showed that the nomogram exhibits an excellent ability to predict anxiety status with sufficient discriminatory power and calibration. Therefore, in line with the preceding points, our proposed model may provide a protocol for anticipating and detecting anxiety in medical personnel during the COVID-19 pandemic.
Materials and Methods
Study Subjects
600 medical staff participating in battle against COVID-19 epidemic in China from February 1st, 2020, to May 30th, 2020, were enrolled in this study. The inclusion criteria were as follows: (1) medical personnels were on duty, and they were working in the fever clinics, isolation wards and quarantine hotels, and engaging in pre-inspection and quarantine; (2) the time for medical staff to engage themselves in epidemic prevention and control was no less than two weeks.
Exclusion Criteria: medical staff who were not involved in the battle against the COVID-19 epidemic and those who did not cooperate with the questionnaire.
Data Collection
The basic information and relevant data of included medical staff who participated in the epidemic prevention of the COVID-19 pandemic in China from February 1st, 2020, to May 30th, 2020, were collected through a questionnaire. Questionnaires were distributed randomly to included medical staff by two investigators. The recording and collation of obtained data were in charge of a specially-assigned person. The quality control of the entered data was supervised by two investigators each other to ensure integrity and authenticity.
Nomogram Establishment and Validation
Included cases were randomized 7:3 and divided into a training set of 420 and a validation set of 180 cases. Logistic regression analysis was applied to investigate the risk factors for anxiety. Next, the independent risk factors for anxiety were identified based on the Akaike information criterion (AIC). The odds ratio (OR) and 95% confidence interval (95% CI) were calculated and a nomogram model was established. The established nomogram was assessed by discrimination and calibration and validated internally and externally using the training and validation sets. The area evaluated the discrimination ability of the nomogram under the receiver operating characteristic (ROC) curve. The area under the ROC curve ranges from 0.5 to 1.0, with 0.5 ~ 0.7, 0.7 ~ 0.85 and 0.85 ~ 0.95 indicating low, fair and high predictive value, respectively. The accuracy of the constructed nomogram was assessed by a calibration plot (ie, the comparison of nomogram-predicted probabilities and actual anxiety in medical staff). The close value of predicted probabilities to standard curve indicated positive predictive value and high accuracy. The decision curve analysis (DCA) was used to analyze the net benefit of the nomogram and assess the clinical utility.
Statistical Analysis
Enumeration data were expressed as the number of cases and constituent ratio, and the chi-square test and Fisher’s exact test were used to compare groups. All statistical analyses were conducted using Stata15 software, and the nomogram was constructed using R software. All reported P values were two-sided and P-value <0.05 was statistically considered significant.
Results
Basic Information
The demographic characteristics and baseline data of the study sample are shown in Table 1. A total of 258 cases were identified as anxious according to the criteria of Anxiety (Hamilton Anxiety Scale scored > 14), and the incidence rate of anxiety was 43%. This high incidence rate of anxiety indicates excessive perceived stress of a person.
Table 1.
Demographic Characteristics and Baseline Data of the Study Sample
| Characteristic | Category | Cases of Anxiety | Cases of Un-Anxiety | X2 value | P value |
|---|---|---|---|---|---|
| Gender | Males | 7 | 81 | 7.223 | 0.007 |
| Females | 58 | 226 | |||
| Age, years | 20~29 | 20 | 87 | 6.144 | 0.1.5 |
| 30~39 | 35 | 143 | |||
| 40~49 | 5 | 62 | |||
| 50~59 | 5 | 15 | |||
| Marital status | Not married | 5 | 60 | 10.892 | 0.004 |
| Married | 60 | 227 | |||
| Divorced | 0 | 20 | |||
| Occupation | Physician | 31 | 138 | 0.162 | 0.687 |
| Nurse | 34 | 169 | |||
| Professional title | No title | 5 | 30 | 7.953 | 0.047 |
| Primary | 10 | 82 | |||
| Intermediate | 33 | 152 | |||
| Senior | 17 | 43 | |||
| Educational background | Specialist Education | 14 | 51 | 1.339 | 0.512 |
| Bachelor degree | 40 | 211 | |||
| Master degree | 11 | 45 | |||
| Work place | Intersection quarantine point | 32 | 148 | 28.072 | <0.001 |
| Follow-up for pre-inspection | 0 | 60 | |||
| Fever clinics | 26 | 94 | |||
| Isolation wards | 7 | 5 | |||
| Case of colleague infection | Uninfected | 37 | 301 | 108.941 | <0.001 |
| Infected | 28 | 6 | |||
| Family supports | Supported | 30 | 188 | 53.229 | <0.001 |
| Not care | 19 | 114 | |||
| Not supported | 16 | 5 | |||
| Mask | Very sufficient | 0 | 15 | 11.857 | 0.018 |
| Relatively sufficient | 5 | 36 | |||
| Generally sufficient | 23 | 132 | |||
| Relatively inadequate | 20 | 47 | |||
| Inadequate | 17 | 77 | |||
| Isolation clothes | Very sufficient | 5 | 15 | 12.675 | 0.013 |
| Relatively sufficient | 22 | 57 | |||
| Generally sufficient | 11 | 105 | |||
| Relatively inadequate | 17 | 94 | |||
| Inadequate | 10 | 36 | |||
| Salary | Very reasonable | 5 | 12 | 17.368 | 0.002 |
| Relatively reasonable | 18 | 88 | |||
| Generally reasonable | 25 | 136 | |||
| Relatively irreasonable | 17 | 36 | |||
| Irreasonable | 0 | 35 | |||
| Convenience of traffic | Very convenient | 5 | 42 | 12.5 | 0.014 |
| Relatively convenient | 17 | 105 | |||
| Generally convenient | 17 | 88 | |||
| Relatively inconvenient | 16 | 57 | |||
| Inconvenient | 10 | 15 | |||
| Participation time | <1 week | 0 | 5 | 23.995 | <0.001 |
| 1~2 weeks | 0 | 5 | |||
| 2~3 weeks | 5 | 42 | |||
| 3~4 weeks | 0 | 63 | |||
| >4 weeks | 60 | 192 | |||
| Break time | One day a week | 37 | 205 | 45.923 | <0.001 |
| One day every two weeks | 12 | 17 | |||
| One day every three weeks | 6 | 0 | |||
| One day every four weeks | 5 | 20 | |||
| No time to rest | 5 | 65 | |||
| Epidemic prevention area | In Hubei Province | 21 | 11 | 56.144 | <0.001 |
| Outside Hubei Province | 44 | 296 |
Logistic Regression Analysis
Anxiety or non-anxiety was the outcome and logistic regression analysis was performed. The variance inflation factors (less than 5) indicated the collinearity between the various variables and the eligibility for logistic regression analysis. Univariate logistic regression analysis on the training set showed that participation time, rest time, epidemic prevention area, epidemic prevention equipment, family support, colleague infection, gender and years of work were risk factors for Anxiety (P < 0.05) (Table 2). Multivariate logistic regression analysis demonstrated that participation time (OR=44.28, 95% CI=13.13~149.32), rest time (OR=38.50, 95% CI=10.43~142.19), epidemic prevention area (OR=10.16, 95% CI=3.51~29.40), epidemic prevention equipment (OR=15.24, 95% CI=5.73~40.55), family support (OR=9.63, 95% CI=3.55~26.11), colleague infection (OR=6.25, 95% CI=2.18~19.11), gender (OR=3.30, 95% CI=1.15~9.47) were the independent risk factors for anxiety (P < 0.05, minimized AIC=137.39) (Table 3).
Table 2.
Results from Univariate Logistic Regression Analysis
| Variables | OR | 95% CI | P value |
|---|---|---|---|
| Work place for epidemic prevention | 1.32 | 1.01~1.74 | <0.05 |
| Participation time | 2.72 | 1.54~4.82 | <0.05 |
| Isolation clothes | 0.86 | 0.67~1.10 | >0.05 |
| Mask | 1.30 | 1.01~1.67 | <0.05 |
| Break time | 0.93 | 0.78~1.10 | >0.05 |
| Salary | 0.86 | 0.65~1.13 | >0.05 |
| Convenience of traffic | 1.46 | 1.15~1.86 | <0.05 |
| Personnel cooperation | 2.13 | 1.51~3.01 | <0.05 |
| Family supports | 2.62 | 1.71~4.00 | <0.05 |
| Case of colleague infection | 37.96 | 14.75~97.73 | <0.05 |
| Hospital level | 0.92 | 0.72~1.17 | >0.05 |
| Epidemic prevention area | 12.84 | 5.80~28.45 | <0.05 |
| Age | 0.87 | 0.62~1.21 | >0.05 |
| Marital status | 1.24 | 0.88~1.76 | >0.05 |
| Gender | 2.97 | 1.30~6.77 | <0.05 |
| Educational background | 0.92 | 0.58~1.47 | >0.05 |
| Professional title | 1.51 | 1.08~2.13 | <0.05 |
Abbreviations: OR, odds ratio; CI, confidence interval.
Table 3.
Results from Multivariate Logistic Regression Analysis
| Contributing Factors | OR | 95% CI | P value |
|---|---|---|---|
| Participation time | 7.35 | 3.10~17.45 | <0.05 |
| Convenience of traffic | 1.78 | 1.26~2.52 | <0.05 |
| Case of colleague infection | 32.51 | 10.51~100.59 | <0.05 |
| Work place for epidemic prevention | 10.29 | 3.21~33.03 | <0.05 |
| Gender | 4.31 | 1.40~13.24 | <0.05 |
| Professional title | 2.06 | 1.26~3.36 | <0.05 |
Abbreviations: OR, odds ratio; CI, confidence interval.
Establishment and Evaluation of a Nomogram
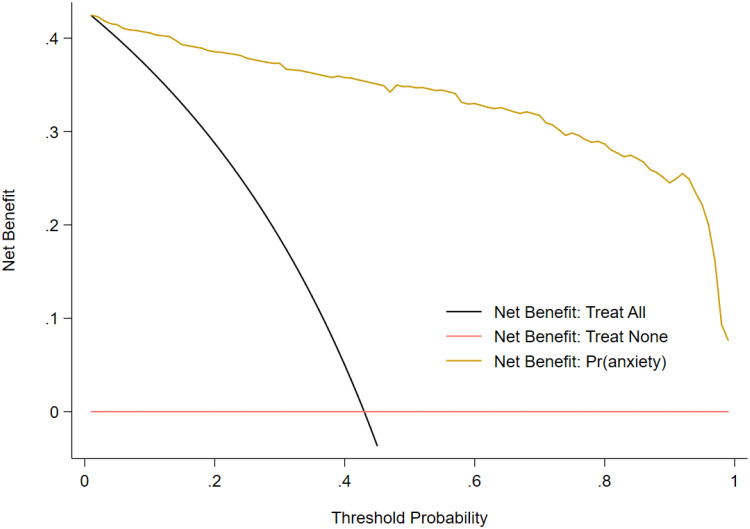
Based on the independent risk factors screened, a nomogram was established (Figure 1) and validated internally in the training set and externally in the validation set. The area under the ROC curve in the training set was 0.987, indicating the constructed nomogram’s good predictive accuracy and discriminative ability (Figure 2A). The calibration plot (Figure 2B) almost coincides with the idealized reference line, suggesting the well-calibrated nomogram. Results from the Hosmer-Lemeshow goodness of fit test (x2=104.88, P=0.99) also suggest good calibration of the nomogram. Similarly, the area under the ROC curve in the validation set was 0.946, indicating good predictive accuracy and discriminative ability of the nomogram (Figure 3A). The calibration plot (Figure 3B) almost coincides with the idealized reference line, suggesting that the nomogram was well calibrated. Results from the Hosmer-Lemeshow goodness of fit test (x2=80.35, P=0.98) also suggest good calibration of the nomogram. DCA demonstrated good net benefit when the threshold probability was 0.04~0.99 (Figure 4).
Figure 1.
The nomogram to predict the anxiety in medical staff during the period of epidemic prevention and control. “Time” indicates the participation time, “rest” indicates rest time, “zone” indicates the epidemic prevention area, “equipment” indicates epidemic prevention equipment, “infection” indicates the colleague infection.
Figure 2.
Internal validation of the nomogram. (A) The ROC curve in the training set. (B) The calibration plot in the training set.
Figure 3.
External validation of the nomogram. (A) The ROC curve in the validation set. (B) The calibration plot in the validation set.
Figure 4.
Decision curve analyses. “Treat All” indicates the positive control that all subjects experienced treatment. “Treat None” indicates the negative control that all subjects experienced no treatment. “Pr(anxiety)” indicates the net benefit increment for the anxiety risk prediction using the constructed nomogram.
Discussion
Emergencies have been shown to make people more prone to anxiety,20–22 so medical personnel and places that prevent epidemics are recognized as independent risk factors for anxiety.23–26 For example, the coronavirus pandemic, which has significantly impacted the world and resulted in thousands of fatalities, has forced healthcare experts to labor at a frenetic pace.
Our current study has examined how the COVID-19 epidemic affected their quality of life. To meet the hypothesis and scope of the study, we went through the measuring of participation time, epidemic prevention area and epidemic prevention equipment utilized to identify the risk factors for anxiety in medical staff during the period of the COVID-19 pandemic in their workplaces. To find how medical staff involved in treating COVID-19 patients could be dealing with serious mental health issues that can be a root cause of anxiety, we determine the prevalence rates of anxiety in medical workers. Furthermore, our research contains data on the increase in insufficient rest time, unsupported family, and infected colleagues related to the overall anxiety prevalence. Our findings supplemented the rest time (OR = 38.50, 95% CI = 10.43 ~ 142.19), family support (OR = 9.63, 95% CI = 3.55 ~ 26.11), and colleague infection (OR = 6.25, 95% CI = 2.18 ~ 19.11) as independent risk factors for anxiety in medical staff. Our studies also showed the effect of insufficient rest time on anxiety more than that of unsupported family and colleague infection on anxiety.
There is a correlation between anxiety and burnout and anxious medical staff are prone to job burnout.27–29 The reasonable and optimized medical staff configuration during the COVID-19 pandemic, therefore, requires the prediction and identification of anxiety in the medical staff at an early stage. Our findings significantly link with previous studies.30,31 For example, a multicenter online survey conducted in China to assess the mental health of healthcare professionals revealed that 44.7% had signs of anxiety.32–34 On the other hand, only 15.7% of the respondents in global research carried out in Singapore and India displayed anxiety symptoms.35,36 Internal and external validation of the constructed nomogram in the present study demonstrated its accuracy in calculating the probability of anxiety in medical staff, with excellent discrimination and acceptable calibration.
There are still some limitations in this study. Firstly, there is a difference in the area under the ROC curve between the training and validation sets. Therefore, a more optimal prediction model can be constructed by increasing the sample size in a cross-sectional survey. Secondly, the established nomogram is limited to predicting the anxiety status of Chinese medical staff, because the data collected in this study are from within the territory of China.
Conclusions
In conclusion, the study reveals high stress, anxiety, and burnout among healthcare professionals working during the COVID-19 pandemic. In particular, the constructed nomogram can predict anxiety status with sufficient discriminatory power and calibration. The study provides a baseline protocol for predicting and identifying anxiety status in medical staff during the COVID-19 pandemic. Considering the advantage of simplicity, intuitiveness and practicability over the traditional methods, we believe that established nanogram has specific auxiliary value in the clinical application of identifying anxiety in medical staff.
Acknowledgments
This study was supported by Henan Provincial Medical science and Technology research Projects (No.2018020407, No.LHGJ20190625). The authors would like to thank professor Yudong Miao, at the Department of Health Policy and Management, Zhengzhou University, for advising on the statistical analyses.
Ethical Statement
The “Branch approved the study for Biomedicine Study, Henan University ethics committee”, and participants obtained consent. Moreover, the study has adopted all the guidelines outlined in the declaration of Helsinki’s ethical principles.
Disclosure
The authors declare no competing interest in this work.
References
- 1.Huremović D. Mental Health of Quarantine and Isolation, in Psychiatry of Pandemics. Springer; 2019:95–118. [Google Scholar]
- 2.Hu T, Wang S, She B, et al. Human mobility data in the COVID-19 pandemic: characteristics, applications, and challenges. Int J Digit Earth. 2021;14(9):1126–1147. [Google Scholar]
- 3.Liu C-Y, Yang YZ, Zhang XM, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol Infect; 2020:148:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soto-Cámara R, Navalpotro-Pascual S, Jiménez-Alegre JJ, et al. Influence of the cumulative incidence of COVID-19 cases on the mental health of the Spanish out-of-hospital professionals. J Clin Med. 2022;11(8):2227. doi: 10.3390/jcm11082227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martínez MM, Fernández-Cano MI, Feijoo-Cid M, et al. Health outcomes and psychosocial risk exposures among healthcare workers during the first wave of the COVID-19 outbreak. Saf Sci. 2022;145:105499. doi: 10.1016/j.ssci.2021.105499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elbay RY, Kurtulmuş A, Arpacıoğlu S, et al. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020;290:113130. doi: 10.1016/j.psychres.2020.113130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khattak S, Faheem M, Nawaz B, et al. Knowledge, Attitude, and perception of cancer patients towards COVID-19 in Pakistan: a cross-sectional study. Int J Environ Res Public Health. 2022;19(13):7926. doi: 10.3390/ijerph19137926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alnazly E, Khraisat OM, Al-Bashaireh AM, et al. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. 2021;16(3):e0247679. doi: 10.1371/journal.pone.0247679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kansoun Z, Boyer L, Hodgkinson M, et al. Burnout in French physicians: a systematic review and meta-analysis. J Affect Disord. 2019;246:132–147. doi: 10.1016/j.jad.2018.12.056 [DOI] [PubMed] [Google Scholar]
- 10.Khan NH, Hassan S, Bahader S, et al. How daily obstacles affect frontline healthcare professionals’ mental health during Omicron: a daily diary study of handwashing behavior. Int J Environ Res Public Health. 2022;19(14):8748. doi: 10.3390/ijerph19148748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caplan RP. Stress, anxiety, and depression in hospital consultants, general practitioners, and senior health service managers. BMJ. 1994;309(6964):1261–1263. doi: 10.1136/bmj.309.6964.1261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tyrer P, Eilenberg T, Fink P, et al. Health anxiety: the silent, disabling epidemic. Br Med J;2016. i2250. doi: 10.1136/bmj.i2250 [DOI] [PubMed] [Google Scholar]
- 13.Rimmer A. Covid-19: trust leaders express concern over levels of fatigue and anxiety among staff. Br Med J. 2020;370:m3004. [DOI] [PubMed] [Google Scholar]
- 14.Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133–2134. doi: 10.1001/jama.2020.5893 [DOI] [PubMed] [Google Scholar]
- 15.Mahase E. Covid-19: many ICU staff in England report symptoms of PTSD, severe depression, or anxiety, study reports. Br Med J. 2021;372:n108. [DOI] [PubMed] [Google Scholar]
- 16.Rubin GJ, Amlôt R, Page L, et al. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ. 2009;339:b2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cao S, Venters CC, Di C, et al. Post-lockdown SARS-CoV-2 nucleic acid screening in nearly ten million residents of Wuhan, China. Nat Commun. 2020;11(1):1–7. doi: 10.1038/s41467-019-13993-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Çelmeçe N, Menekay M. The effect of stress, anxiety and burnout levels of healthcare professionals caring for COVID-19 patients on their quality of life. Front Psychol. 2020;11:597624. doi: 10.3389/fpsyg.2020.597624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang X, Yan E, Wang Z. The relieving effect of mental health education on patients with generalized anxiety disorder. Indian J Pharm Sci. 2020;82:39. [Google Scholar]
- 20.Shi L, Lu Z-A, Que J-Y, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(7):e2014053–e2014053. doi: 10.1001/jamanetworkopen.2020.14053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.González-Sanguino C, Ausín B, Castellanos MÁ, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hashemian F, Khoshnood K, Desai MM, et al. Anxiety, depression, and posttraumatic stress in Iranian survivors of chemical warfare. JAMA. 2006;296(5):560–566. doi: 10.1001/jama.296.5.560 [DOI] [PubMed] [Google Scholar]
- 23.Sampaio F, Sequeira C, Teixeira L. Impact of COVID-19 outbreak on nurses’ mental health: a prospective cohort study. Environ Res. 2021;194:110620. doi: 10.1016/j.envres.2020.110620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu W, Wang H, Lin Y, et al. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou C, Shi L, Gao L, et al. Determinate factors of mental health status in Chinese medical staff: a cross-sectional study. Medicine. 2018;97(10):e0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kash N, Silapunt S. A review of emerging and non-US FDA-approved topical agents for the treatment of basal cell carcinoma. Future Oncol. 2021;17(23):3111–3132. doi: 10.2217/fon-2020-1147 [DOI] [PubMed] [Google Scholar]
- 27.Zhou J, Yang Y, Qiu X, et al. Relationship between anxiety and burnout among Chinese physicians: a moderated mediation model. PLoS One. 2016;11(8):e0157013. doi: 10.1371/journal.pone.0157013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duan C, Deng H, Xiao S, et al. Accelerate gas diffusion-weighted MRI for lung morphometry with deep learning. Eur Radiol. 2022;32(1):702–713. doi: 10.1007/s00330-021-08126-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang M, Chen Y, Susilo W. PPO-CPQ: a privacy-preserving optimization of clinical pathway query for e-healthcare systems. IEEE Internet Things J. 2020;7(10):10660–10672. [Google Scholar]
- 30.Zhou T, Walther F, Eberlein-Gonska M, et al. Burnout and well-being of healthcare workers in the post-pandemic period of COVID-19: a perspective from the job demands-resources model. BMC Health Serv Res. 2022;22(1):1–15. doi: 10.1186/s12913-021-07414-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hou Y, Hou W, Zhang Y, et al. Relationship between working stress and anxiety of medical workers in the COVID-19 situation: a moderated mediation model. J Affect Disord. 2022;297:314–320. doi: 10.1016/j.jad.2021.10.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Selvaraj P, Muthukanagaraj P, Saluja B, et al. Psychological impact of COVID-19 pandemic on health-care professionals in India–a multicentric cross-sectional study. Indian J Med Sci. 2020;72(3):141. doi: 10.25259/IJMS_193_2020 [DOI] [Google Scholar]
- 33.Zeng Q, Bie B, Guo Q, et al. Hyperpolarized Xe NMR signal advancement by metal-organic framework entrapment in aqueous solution. Proc Natl Acad Sci. 2020;117(30):17558–17563. doi: 10.1073/pnas.2004121117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.He L, Mu L, Jean JA, et al. Contributions and challenges of public health social work practice during the initial 2020 COVID-19 outbreak in China. Br J Soc Work. 2022. doi: 10.1093/bjsw/bcac077 [DOI] [Google Scholar]
- 35.Chew NW, Lee GK, Tan BY, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yao L, Li X, Zheng R, et al. The impact of air pollution perception on urban settlement intentions of young talent in China. Int J Environ Res Public Health. 2022;19(3):1080. doi: 10.3390/ijerph19031080 [DOI] [PMC free article] [PubMed] [Google Scholar]