Abstract
Purpose
Helicobacter pylori (H. pylori) infection is a high-risk factor for gastric cancer (GC). The main aim of this study was to evaluate the effect of H. pylori on gastritis staging systems and the value of H. pylori combined with gastritis staging systems in predicting GC risk.
Patients and Methods
This study enrolled 609 patients with gastric atrophy (GA) and 527 patients with gastric intestinal metaplasia (GIM), who were graded by the OLGA and OLGIM staging systems, respectively. Each individual underwent serum pepsinogen (PG) test, H. pylori detection and questionnaire investigation. We did a real-world retrospective follow-up survey for them in April 2022.
Results
Compared with H. pylori-negative patients, H. pylori-positive patients had higher serum PGs/gastrin-17 (G-17) levels and lower PGR levels, regardless of OLGA/OLGIM stages I–II or III–IV. Furthermore, eight patients with atrophic gastritis who progressed to GC were previously in OLGA stages III–IV and OLGIM stages II–IV. The average duration of this process was 2.19±1.03 years. Logistic regression analysis indicated that PGI and H. pylori infection were independent risk factors of individuals with OLGA stages III–IV. Age and PGR were independent risk factors of patients with OLGIM stages III–IV. PGI and PGR had good clinical diagnostic values for OLGA stages III–IV and OLGIM stages III–IV, respectively.
Conclusion
Patients with OLGA/OLGIM stages III–IV should undergo endoscopic surveillance regardless of H. pylori infection. H. pylori-positive patients with OLGIM stage II also have a high risk of GC. H. pylori combined with PGI and PGR is helpful to evaluate the severity of chronic gastritis.
Keywords: atrophy, metaplasia, Helicobacter pylori, gastric cancer, risk factors
Introduction
Gastric cancer (GC) is the fifth most common cancer and the third most common cause of cancer death in the world.1 Its risk factors include H. pylori infection, age, smoking, alcohol consumption, family susceptibility and poor dietary habits.1,2 GC is often diagnosed at an advanced stage and its mortality rate is high.3 Therefore, early detection and treatment are the keys to reducing the mortality of GC.4
Gastric atrophy (GA) and gastric intestinal metaplasia (GIM) are important risk factors for intestinal-type gastric cancer.5,6 Therefore, endoscopic surveillance of them is conducive to early detection of GC.7 Operative link on gastritis assessment (OLGA) is a visual analog grading using the biopsy sampling protocol and the Houston updated Sydney system recommendation.8 Atrophy staging is the result of combining the degree of atrophy scored on histology with the morphology of atrophy as determined by biopsy mapping.9 For patients with GIM, the operative link on gastric intestinal metaplasia assessment (OLGIM) is a tool for risk stratification.10 Multiple studies found that patients with OLGA stages III–IV have a high risk of developing GC.11,12 According to the findings of the European Society for Gastrointestinal Endoscopy, endoscopic surveillance is recommended for patients with OLGIM III–IV.13 However, China has an enormous population and the living habits of different regions vary greatly. Therefore, the incidence of gastric cancer varies in different regions of China, and large-scale follow-up studies are still lacking.
Serum pepsinogen (PG) and gastrin-17 (G-17) produced by gastric-associated cells could reflect the state of the gastric mucosa to a certain extent.14–16 H. pylori was classified as a group I carcinogen of GC by the International Agency of the World Health Organization in 1994.17 Helicobacter pylori is a gram-negative motile bacterium that causes acute and chronic gastrointestinal and extragastrointestinal infections in humans.18 It takes a long time for gastritis to develop into GC, so the secondary prevention of GC is worth exploring.19,20 However, the lack of standardization of treatment in most patients with gastritis in China makes it difficult to perform regular endoscopic surveillance. Therefore, exploring the relationship among H. pylori, serum PGs levels, and the severity of gastritis would be more meaningful for predicting the risk of GC. The aim of this study was to analyze the effect of H. pylori on OLGA/OLGIM staging and to validate the appropriate timing of endoscopic surveillance in high-risk groups.
Materials and Methods
Patients Selection
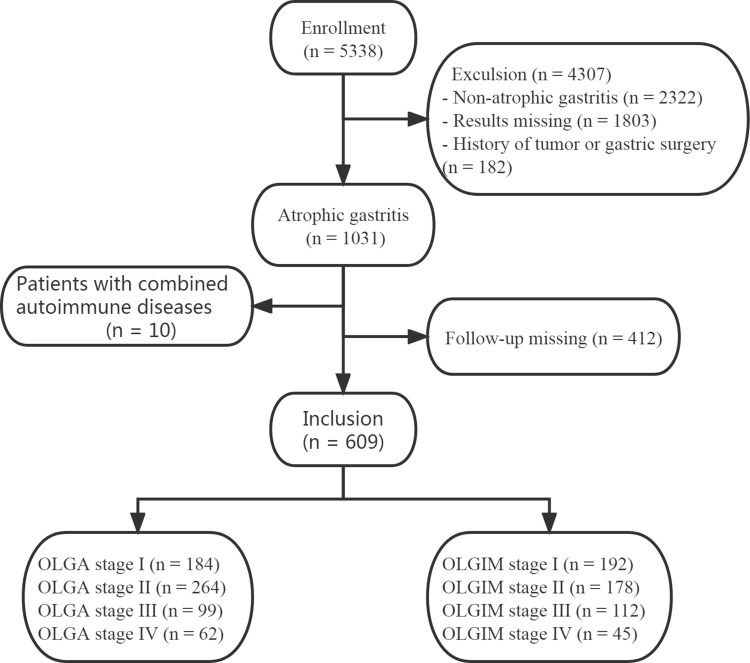
This cross-sectional study was carried out at the First Affiliated Hospital of University of Science and Technology of China from April 2015 to April 2020, including physical examination centers and outpatient populations in Anhui Province, eastern China. All patients had no renal dysfunction. Inclusion criteria: patients (age > 18 years old) with gastroscopic biopsy. The exclusion criteria: patients with a history of tumor or gastric surgery; missing results; pathological results were non-atrophic gastritis; lost to follow-up. It is worth mentioning that there were 10 patients with atrophic gastritis combined with autoimmune diseases. Therefore, they were not included in the analysis. The case-selection flow chart has been presented in Figure 1.
Figure 1.
A flow chart for screening the study subjects was established.
Endoscopy and Histology
Based on the Sydney system, five pathology samples were taken: two from the gastric body; one from the mucosa of the incisura, and two from the antral mucosa. The tissues were processed in the same pathology laboratory. Patients with gastric atrophy were staged I–IV by the OLGA staging system from the combination of “antrum score” and “corpus score” (no atrophy = 0%, score = 0; mild atrophy = 1–30%, score = 1; moderate atrophy = 31–60%, score = 2; and severe atrophy ≥60%, score = 3).21,22 OLGIM staging adopted the same scoring system based on the severity and morphology of GIM.10 Stages III–IV were defined as high-risk stages for both of them. All tissue sections were read by two senior pathologists.
Serum Pepsinogen Test, H. Pylori Detection and Questionnaire Survey
Each patient collected 5 mL of venous blood at 8:00 am and submitted it for inspection within 30 minutes. The levels of serum PGs (PGI, serum pepsinogen I; PGII, serum pepsinogen II) and G-17 were analyzed by ELISA (BioHit, Helsinki, Finland) and PGR (PGI and PGII ratio) was calculated. All patients were informed to stop taking PPI (proton pump inhibitor) for two weeks before the H. pylori detection. After that, we tested the levels of serum PGs/G-17. Each individual was given a 13C-urea or 14C-urea breath test on the same day as the endoscopy. Furthermore, they all received a detailed questionnaire investigation, including age, gender, height and weight, smoking, alcohol consumption, and family history of gastrointestinal tumors.
Statistical Analysis
Pearson’s Χ test was conducted to analyze the categorical variables. Significant differences in age and BMI among groups were assessed by analysis of variance (ANOVA) or t-test. Two-sample rank-sum test and multi-sample rank-sum test were used to analyze skewed data. Univariate and multivariate logistic regression models were used to analyze the high-risk factors of OLGA stages III–IV and OLGIM stages III–IV. The optimal index was selected by the ROC curve to reflect the clinical diagnostic value of high-risk groups. Data analysis was performed using SPSS 25.0 software. We conducted a retrospective follow-up of gastritis patients in April 2022 and summarized the characteristics of patients with GC. Two-sided p-value < 0.05 was considered statistically significant.
Results
Baseline Data of the Study Subjects
609 atrophic patients had a mean age of 51.13 (SD = 9.95) years, of whom 359 were male and 250 were female. According to OLGA stage, 184 patients (30.21%), 264 patients (43.35%), 99 patients (16.26%) and 62 patients (10.18%) were in stage I–IV, respectively. There were 527 patients had atrophy combined with intestinal metaplasia, including 283 males and 244 females. Their mean age was 50.83 (SD = 9.95) years. According to OLGIM stage, 192 patients (36.43%), 178 patients (33.78%), 112 patients (21.25%) and 45 patients (8.54%) were in stage I–IV, respectively. Meanwhile, the rate of H. pylori infection was 42.53% in GA patients and 38.90% in GIM patients (Table 1).
Table 1.
Baseline Characteristics of Patients with Atrophic Gastritis in This Study
| GA (n = 609) | GIM (n = 527) | |||
|---|---|---|---|---|
| Age, years, mean (SD) | 51.13 (9.95) | 50.83 (9.95) | ||
| BMI, kg/m², mean (SD) | 24.28 (2.92) | 24.06 (3.27) | ||
| Gender, Male, n (%) | 359 (58.95) | 283 (53.70) | ||
| Smoking, n (%) | 253 (41.54) | 225 (42.69) | ||
| Alcohol consumption, n (%) | 262 (43.02) | 239 (45.35) | ||
| Family history, n (%) | 60 (9.85) | 58 (11.01) | ||
| H. pylori infection, n (%) | 259 (42.53) | 205 (38.90) | ||
| OLGA stage I, n (%) | 184 (30.21) | OLGIM stage I, n (%) | 192 (36.43) | |
| OLGA stage II, n (%) | 264 (43.35) | OLGIM stage II, n (%) | 178 (33.78) | |
| OLGA stage III, n (%) | 99 (16.26) | OLGIM stage III, n (%) | 112 (21.25) | |
| OLGA stage IV, n (%) | 62 (10.18) | OLGIM stage IV, n (%) | 45 (8.54) | |
Abbreviations: GA, gastric atrophy; GIM, gastric intestinal metaplasia; BMI, body mass index; SD, standard deviation; OLGA, operative link on gastritis assessment; OLGIM, operative link on gastric intestinal metaplasia assessment.
Serum PGs in OLGA/OLGIM Stage
There was a statistical difference in serum PGI, PGR, G-17, family history rate (all p < 0.001) and H. pylori infection rate (p = 0.002) in OLGA staging. As OLGA stage increased, PGI and PGR levels decreased, while H. pylori infection rate increased. The G-17 level and family history ratio were the highest in OLGA stage IV. Meanwhile, there were significant differences in serum PGI (p = 0.001), PGR, PGII, G-17, H. pylori infection rate (all p < 0.001) and family history ratio (p = 0.008) in OLGIM staging. Besides, the mean age of patients with OLGIM III–IV was older than patients with OLGIM I–II (p = 0.003) (Table 2).
Table 2.
Serum PGs/G-17 Levels and Population Characteristics in OLGA/OLGIM Stage
| OLGA | OLGIM | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Stage I (n = 184) | Stage II (n = 264) | Stage III (n = 99) | Stage IV (n = 62) | p-value | Stag I (n = 192) | Stage II (n = 178) | Stage III (n = 112) | Stage IV (n = 45) | p-value | |
| PGI, µg/L Median (IQR) | 120.59 (83.78–168.36) | 101.72 (78.03–130.07) | 100.02 (76.40–110.15) | 58.70 (46.18–72.31) | < 0.001 | 103.42 (81.46–134.43) | 101.15 (75.56–128.03) | 89.50 (63.87–127.26) | 71.12 (54.85–107.52) | 0.001 |
| PGII, µg/L Median (IQR) | 11.50 (6.67–21.33) | 9.56 (6.49–15.83) | 9.92 (6.45–14.73) | 9.93 (6.09–14.76) | 0.060 | 7.58 (5.32–11.77) | 9.84 (6.67–17.17) | 12.29 (7.10–20.43) | 14.15 (9.62–20.62) | < 0.001 |
| PGR, Median (IQR) | 10.53 (7.65–13.48) | 10.60 (7.10–14.01) | 9.43 (6.67–14.16) | 6.26 (4.02–10.71) | < 0.001 | 13.70 (10.58–16.29) | 10.13 (7.09–12.59) | 7.65 (5.90–9.85) | 4.61 (2.66–6.36) | < 0.001 |
| G-17, pmol/L Median (IQR) | 3.01 (1.34–7.70) | 2.48 (1.33–6.56) | 2.33 (1.29–5.89) | 4.75 (2.54–29.24) | < 0.001 | 2.08 (1.16–5.13) | 3.10 (1.33–6.46) | 3.10 (1.69–10.33) | 8.28 (3.61–36.38) | < 0.001 |
| Age, years, mean (SD) | 51.41 (9.48) | 51.10 (9.99) | 50.32 (9.15) | 52.52 (11.67) | 0.369 | 49.63 (9.03) | 49.96 (10.09) | 53.52 (10.70) | 52.60 (10.01) | 0.003 |
| BMI, kg/m², mean (SD) | 24.56 (2.95) | 24.18(3.03) | 24.27 (2.98) | 23.95 (3.26) | 0.469 | 24.26 (3.15) | 23.89 (3.41) | 24.13 (3.31) | 23.62 (3.36) | 0.595 |
| H. pylori infection, n (%) | 68 (36.96) | 104(39.40) | 48 (48.48) | 39 (62.90) | 0.002 | 50 (26.04) | 71 (39.89) | 52 (46.43) | 32 (71.11) | < 0.001 |
| Smoking, n (%) | 80 (43.48) | 105 (39.78) | 45 (45.45) | 23 (37.10) | 0.625 | 83 (43.23) | 78 (43.82) | 52 (46.43) | 12 (26.67) | 0.140 |
| Alcohol consumption, n (%) | 83 (45.11) | 108 (40.91) | 44 (44.44) | 27 (43.55) | 0.826 | 85 (44.27) | 85 (47.75) | 55 (49.11) | 14 (31.11) | 0.185 |
| Family history, n (%) | 16 (8.70) | 18 (6.82) | 7 (7.07) | 19 (30.65) | < 0.001 | 16 (8.33) | 14 (7.87) | 18 (16.07) | 10 (22.22) | 0.008 |
| Gender, Male, n (%) | 122 (66.30) | 143 (54.17) | 61 (61.61) | 33 (53.23) | 0.052 | 109 (56.77) | 91 (51.12) | 65 (58.04) | 18 (40.00) | 0.142 |
Abbreviations: PGI, serum pepsinogen I; PGII, serum pepsinogen II; PGR, pepsinogen I and II ratio; G-17, gastrin-17; BMI, body mass index; SD, standard deviation; IQR, interquartile range.
Serum PGs in OLGA/OLGIM I-II and III-IV
Combined with the status of H. pylori infection, we further found that the levels of PGI was lower in H. pylori-positive patients with OLGA III–IV. For H. pylori-negative patients with GA, the levels of PGI (p < 0.001) was lower in the high-risk stages. Besides, H. pylori-positive patients and H. pylori-negative patients were analyzed separately. Lower levels of PGI/PGR and higher levels of PGII/G-17 were observed in OLGIM stages III–IV compared to OLGIM stages I–II in this study. Regardless of OLGA/OLGIM stages I–II or III–IV, H. pylori-positive patients had higher PGI, PGII, G-17 levels, and lower PGR levels compared to H. pylori-negative patients (Table 3).
Table 3.
Serum PGs/G-17 in OLGA/OLGIM Stages I–II and III–IV
| OLGA | OLGIM | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| PGI, µg/L Median (IQR) | PGII, µg/L Median (IQR) | PGR, Median (IQR) | G-17, pmol/L Median (IQR) | PGI, µg/L Median (IQR) | PGII, µg/L Median (IQR) | PGR, Median (IQR) | G-17, pmol/L Median (IQR) | ||
| H. pylori-Positive | Stages I–II | 136.09(107.43–164.03) | 19.81(12.68–24.38) | 7.08(5.60–9.43) | 6.81(4.28–14.06) | 114.52(99.52–153.44) | 14.74(11.26–22.52) | 7.96 (5.91–12.77) | 6.02(3.18–10.01) |
| Stages III–IV | 89.00(70.85–111.90) | 13.41(9.08–18.81) | 6.69(5.08–8.90) | 5.13(2.48–11.31) | 108.98(67.23–141.50) | 17.80(13.84–24.72) | 5.68(4.46–6.66) | 6.48(4.14–19.02) | |
| p-value | <0.001 | <0.001 | 0.252 | 0.075 | 0.018 | 0.015 | <0.001 | 0.030 | |
| H. pylori-Negative | Stages I–II | 90.12(73.67–121.54) | 7.29(5.66–10.46) | 12.7(10.27–14.83) | 1.70(1.08–3.26) | 90.36(71.42–118.56) | 6.92(5.02–9.46) | 13.20(11.11–15.95) | 1.61(1.08–3.22) |
| Stages III–IV | 74.92(54.23–111.66) | 6.55(4.85–9.96) | 11.28(7.40–15.78) | 1.71(1.20–4.03) | 70.70(59.13–93.19) | 7.55(6.02–11.74) | 9.00(6.94–11.10) | 2.10(1.30–6.66) | |
| p-value | <0.001 | 0.132 | 0.009 | 0.308 | <0.001 | 0.006 | <0.001 | 0.008 | |
| Stages I–II | H. pylori-negative | 90.12 (90.12–73.67) | 7.29 (5.66–10.46) | 12.70 (10.27–14.83) | 1.70(1.08–3.26) | 90.36(71.42–118.56) | 6.92(5.02–9.46) | 13.20(11.11–15.95) | 1.61(1.08–3.22) |
| H. pylori-positive | 136.09(107.43–164.03) | 19.81(12.68–24.38) | 7.08(5.60–9.43) | 6.81(4.28–14.06) | 114.52(99.25–153.44) | 14.74(11.26–22.52) | 7.96(5.91–10.01) | 6.02(3.18–10.01) | |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Stages III–IV | H. pylori-negative | 74.92(54.23–101.95) | 6.55(4.85–9.96) | 11.28(7.40–15.78) | 1.71(1.20–4.03) | 70.70(59.13–93.19) | 7.55(6.02–11.74) | 9.00(6.94–11.10) | 2.10(1.30–6.66) |
| H. pylori-positive | 89.00(70.85–111.90) | 13.41(9.08–28.88) | 6.69(5.08–8.90) | 5.13(2.48–11.31) | 108.98(67.23–141.50) | 17.80(13.84–24.72) | 5.68(4.46–6.66) | 6.48(4.14–19.02) | |
| p-value | 0.002 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
Abbreviations: PGI, serum pepsinogen I; PGII, serum pepsinogen II; PGR, pepsinogen I and II ratio; IQR, interquartile range; G-17, gastrin-17.
Risk Factors for OLGA/OLGIM Stages III-IV
We performed risk factors analysis for OLGA/OLGIM stages III–IV (Tables 4 and 5). Univariate logistic regression results showed that PGI, PGR, G-17, H. pylori infection, and family history were significantly associated with OLGA stages III–IV. Multivariate logistic regression results suggested PGI (p = 0.001) and H. pylori infection (p < 0.001) were independent risk factors of OLGA stages III–IV. Independent risk factors for OLGIM stages III–IV were age (p = 0.027) and PGR (p < 0.001).
Table 4.
Univariate Logistic Regression Analysis of Risk Factors for Patients with OLGA/OLGIM III–IV
| Risk factors | OLGA I–II VS OLGA III–IV | OLGIM I–II VS OLGIM III–IV | ||||||
|---|---|---|---|---|---|---|---|---|
| OLGA I–II (n = 448) | OLGA III–IV (n = 161) | p-value | OR (95% CI) | OLGIM I–II (n = 370) | OLGIM III–IV (n = 157) | p-value | OR (95% CI) | |
| Gender, Male, n (%) | 265 (59.15) | 94 (58.39) | 0.865 | 0.969 (0.672–1.397) | 200 (54.05) | 83 (52.87) | 0.803 | 0.953 (0.658–1.386) |
| Age, years, mean (SD) | 51.33 (9.78) | 51.10 (10.30) | 0.798 | 0.998 (0.980–1.016) | 49.79 (9.58) | 53.29 (10.39) | <0.001 | 1.036 (1.017–1.057) |
| BMI, kg/m², mean (SD) | 24.32 (2.92) | 24.16 (2.90) | 0.545 | 0.981 (0.922–1.044) | 24.09 (3.27) | 23.97 (3.28) | 0.712 | 0.989 (0.934–1.048) |
| Smoking, n (%) | 185 (41.29) | 68 (42.24) | 0.835 | 1.039 (0.722–1.497) | 161 (43.51) | 64 (40.76) | 0.560 | 0.893 (0.612–1.305) |
| Alcohol consumption, n (%) | 191 (42.63) | 71 (44.10) | 0.747 | 1.061 (0.738–1.526) | 170 (45.95) | 69 (43.95) | 0.674 | 0.922 (0.634–1.343) |
| Family history, n (%) | 34 (7.59) | 26 (16.15) | 0.002 | 2.345 (1.358–4.050) | 30 (8.11) | 28 (17.83) | 0.001 | 2.460 (1.414–4.279) |
| H. pylori infection, n (%) | 172 (38.39) | 87 (54.04) | 0.001 | 1.887 (1.311–2.714) | 121 (32.70) | 84 (53.50) | <0.001 | 2.368 (1.617–3.468) |
| PGI, µg/L Median (IQR) | 107.05 (79.49–141.21) | 79.53 (64.36–107.90) | <0.001 | 0.986 (0.981–0.990) | 101.97 (78.42–132.98) | 85.31 (62.33–122.29) | 0.019 | 0.995 (0.992–0.999) |
| PGII, µg/L Median (IQR) | 10.35 (6.57–17.80) | 9.92 (6.45–14.73) | 0.283 | 0.989 (0.970–1.009) | 8.50 (6.01–13.04) | 13.84 (7.68–20.81) | <0.001 | 1.055 (1.034–1.076) |
| PGR, Median (IQR) | 10.58 (7.34–17.02) | 8.01 (5.86–12.64) | <0.001 | 0.925 (0.888–0.964) | 11.89 (8.73–14.87) | 6.67 (4.98–9.13) | <0.001 | 0.739 (0.695–0.787) |
| G-17, pmol/L Median (IQR) | 2.85 (1.33–7.05) | 3.06 (1.54–9.52) | 0.040 | 1.015 (1.001–1.029) | 2.37 (1.28–5.89) | 4.32 (2.06–14.38) | <0.001 | 1.062 (1.040–1.085) |
Abbreviations: PGI, serum pepsinogen I; PGII, serum pepsinogen II; PGR, pepsinogen I and II ratio; G-17, gastrin-17; BMI, body mass index; SD, standard deviation; IQR, interquartile range.
Table 5.
Multivariate Logistic Regression Analysis of Risk Factors for Patients with OLGA/OLGIM III–IV
| Risk Factors | OLGA stages III–IV | OLGIM Stages III–IV | ||
|---|---|---|---|---|
| p-value | OR (95% CI) | p-value | OR (95% CI) | |
| Age | - | - | 0.027 | 1.026 (1.003–1.050) |
| PGI | 0.001 | 0.982 (0.976–0.988) | 0.238 | 0.994 (0.985–1.004) |
| PGII | - | - | 0.825 | 1.007 (0.948–1.070) |
| PGR | 0.399 | 0.977 (0.925–1.031) | <0.001 | 0.726 (0.641–0.824) |
| G-17 | 0.605 | 0.995 (0.978–1.013) | 0.402 | 1.011 (0.985–1.037) |
| H. pylori infection | <0.001 | 2.916 (1.796–4.736) | 0.059 | 0.572 (0.320–1.021) |
| Family history | 0.166 | 1.536 (0.837–2.821) | 0.126 | 1.704 (0.861–3.372) |
Abbreviations: PGI, serum pepsinogen I; PGII, serum pepsinogen II; PGR, pepsinogen I and II ratio; G-17, gastrin-17.
Follow-Up Results
Eight patients with atrophic gastritis who progressed to GC were observed in this study which spanned 4.5 ±1.87 years (Table 6). Miraculously, they were all male, with an average age of 66.50 (SD = 8.94) years. In addition, eight patients were previously in OLGA stages III–IV and OLGIM stages II–III, and three of the OLGIM stage II patients were H. pylori-positive, but they failed anti-H. pylori therapy. Meanwhile, we found that five patients had smoked, four patients had drunk, and two patients had a family history of gastrointestinal tumors. Besides, the average time of progression to GC was 2.19±1.03 years.
Table 6.
Characteristics of Eight Patients with GC
| Gender | Age (y) | H. Pylori Infection | Treatment of H. Pylori | OLAG Stage | OLGIM Stage | The Lesion Location | The Lesion Type | Follow-up Time | Smoking | Alcohol Consumption | Family History |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | 69 | Positive | Failed | III | II | Corpus | HGIN | 1.5 years | N | N | N |
| Male | 65 | Negative | - | III | III | Antrum | HGIN | 1 year | Y | Y | N |
| Male | 68 | Negative | - | IV | III | Corpus | Adenocarcinom | 3 years | Y | Y | N |
| Male | 55 | Negative | - | III | II | Corpus | HGIN | 2.5 years | Y | N | Y |
| Male | 58 | Positive | Failed | III | II | Antrum | HGIN | 4 years | Y | N | N |
| Male | 83 | Negative | - | III | III | Antrum | HGIN | 2.5 years | N | Y | N |
| Male | 73 | Positive | Failed | III | II | Antrum | HGIN | 2 years | N | N | Y |
| Male | 61 | Positive | Failed | III | III | Corpus | Adenocarcinoma | 1 year | Y | Y | N |
Notes: Y, patient with a history of smoking, patient with a history of alcohol consumption, patient with family history of gastrointestinal tumors. N, patient without a history of smoking, patient without a history of alcohol consumption, patient without family history of gastrointestinal tumors.
Abbreviation: HGIN, high grade intraepithelial neoplasia.
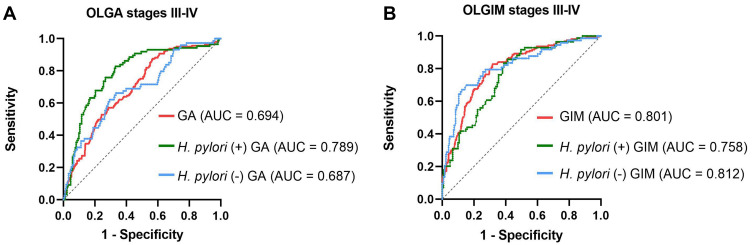
ROC Curves
We analyzed the diagnostic value of PGI for OLGA stages III–IV according to H. pylori status. We found that the area under the curve (AUC) was 0.789 (95% CI: 0.730–0.850, p < 0.001), the optimal cut-off value was 115.23, the sensitivity was 82.8% and the specificity was 66.9% for H. pylori-positive patients with GA. For all patients with GIM, the AUC was 0.801 (95% CI: 0.761–0.842, p < 0.001), the best cut-off value was 9.93, the sensitivity was 82.8% and the specificity was 68.1% (Figure 2).
Figure 2.
(A) ROC curves of PGI for the diagnosis of OLGA stages III–IV of atrophic gastritis (the green line is patients with H. pylori-positive; the blue line is patients with H. pylori-negative; the red line is all patients with GA). (B) ROC curves of PGR for the diagnosis of OLGIM stages III–IV of atrophic gastritis (the green line is patients with H. pylori-positive; the blue line is patients with H. pylori-negative; the red line is all patients with GIM).
Abbreviation: AUC, area under the curve.
Discussion
Chronic atrophic gastritis is a precancerous stage of GC. Most studies showed that severe atrophy and intestinal metaplasia are the risk factors of GC.9,23,24 Asia has a large population and the results of studies are variable. Most findings indicate that patients with OLGA or OLGIM III–IV have a higher risk of gastric cancer and that these patients could benefit from endoscopic surveillance.24–26 Serum PGs combined with H. pylori antibody (named ABC method) has been proposed as a predictive method for patients with GC.27 A multicenter study in China developed score-based prediction rules including variables such as age, sex, PG I/II ratio, G-17 concentration, anti-H. pylori IgG status, and consumption of pickled and fried foods for secondary prevention of GC.4 The 13C-urea/14C-urea breath test was chosen in our study, which reflected the current infection of H. pylori. We explored the relationship between the current infection of H. pylori and serum PGs in OLGA/OLGIM staging systems. This may provide us with a more accurate risk assessment method for GC. All H. pylori-positive patients are required to receive H. pylori eradication therapy. In this study, endoscopic biopsy was not performed on patients with mild lesions. However, there were few large-scale follow-up studies in China, which is why we followed up patients with definite atrophic gastritis to verify the risk stage of GC.
Rugge et al conducted a follow-up study of 93 patients for more than 12 years and found that PGR was significantly negatively correlated with OLGA staging.11 In another study, serum PGI was negatively correlated with OLGA staging, and PGR was negatively correlated with OLGIM staging.25 Our study proposed that serum PGI, PGR, and G-17 were associated with OLGA staging, whereas serum PGs, PGR, and G-17 were related to OLGIM staging (Table 2). These results are generally consistent with the findings of previous studies, which demonstrates that serum-related indicators can reflect the severity of GA and GIM. In addition, H. pylori infection and age were found to be independent risk factors of gland atrophy or gastric intestinal metaplasia in most studies.28–30 In the results, the mean age of OLGIM III–IV patients was older than that of OLGIM I–II patients, but there was no statistical difference in age between OLGA stages. The study also observed that as the OLGA/OLGIM stage increased, the H. pylori infection rate increased. Furthermore, early studies presented that H. pylori infection resulted in increased serum pepsinogen levels.31 Higher levels of PGI, PGII, G-17 and lower level of PGR in H. pylori-positive patients were observed in our study compared to H. pylori-negative patients, regardless of OLGA stages I–II or III–IV. The same finding was also shown in patients with gastric intestinal metaplasia (Table 3). Therefore, serum PGs should be differentiated according to different H. pylori status to assess the severity of gastritis.
The majority of researches considered that one of two staging systems (OLGA or OLGIM staging) was recommended as a reference for endoscopic surveillance of severe chronic gastritis.32–34 In the staging of gastritis, intestinal metaplasia instead of atrophy significantly improved the interobserver agreement, and their correlation in gastritis severity remained pronounced.10 Simultaneous description of the OLGA and OLGIM staging systems may be more accurate than separate descriptions. Therefore, we focused on the OLGA/OLGIM stages III–IV. According to our retrospective follow-up results, eight patients who progressed to GC were in OLGA stages III–IV and OLGIM stages II–III previously. We noticed that three OLGIM stage II patients were H pylori-positive, and their anti-H pylori treatment failed. These results indicate that patients with OLGIM stage II are worthy of note as well, especially in terms of those who are H. pylori-positive and their anti-H. pylori treatment failed. Persistent H. pylori infection may accelerate disease progression. Microbial-host interactions depend on environmental changes in microbial virulence gene expression. Detection of H. pylori virulence gene expression in gastric biopsy specimens can help predict disease outcomes.35 In addition, gastric cancer is the result of multiple factors. In this regard, a larger scale and more rigorous experimental design are needed. Besides, the incidence of GC in men was twice as high as in women from a study.3 All patients in this follow-up outcome were male. A prospective, longitudinal, multicenter study conducted in Singapore found that patients with OLGIM III–IV and OLGIM II benefit from repeat endoscopic surveillance at 2 and 4–5 years, respectively.24 Previously, only OLGIM stages III–IV were used as being the priority endoscopic surveillance stages,23,36 and re-biopsy within 3 years was recommended.13 Our study showed that the average duration of progression to GC was 2.19±1.03 years. This result sparked our interest in exploring the risk factors of OLGA stages III–IV and OLGIM stages III–IV. Patients with OLGIM II are also worthy of further study.
According to a survey in the United States, there were many risk factors of GC, including H. pylori infection, smoking, low socioeconomic status, and high-salt diet.2 Therefore, these factors may be associated with severe gastritis. The results demonstrated that serum PGI and H. pylori infection were independent risk factors for OLGA stage III–IV, whereas age and PGR were independent risk factors for OLGIM stage III–IV. A study has shown that smoking is strongly associated with the development of GC, and after 10 years of smoking cessation, the risk of smokers suffering from GC could be reduced to the same as that of patients who never smoked.37 However, in the multiple logistic regression analysis of our study, age and smoking history had no statistical difference in OLGA III–IV, while age had statistical difference in OLGIM III–IV. The majority of patients participating in this study were middle-aged, making for statistically no differences. In addition, the family history ratio was highest at OLGA stage IV and increased with increasing OLGIM stage. There was statistically significant difference in the family history ratio between OLGIM stage I–II and OLGIM stages III–IV. Meanwhile, serum PG cut-off points derived from previous studies were considered as potential predictors of gastric cancer development, specifically PGI ≤ 70 ng/mL, and PGI: PGII serum ratio ≤ 3.0.38,39 Figure 2 presented that PGI was of great significance for patients with OLGA III–IV and PGR was more sensitive to patients with OLGIM III–IV. Therefore, we plotted ROC curves for different H. pylori status, which performed well in terms of sensitivity or specificity. Many studies based on high risk patients of GC have reported high sensitivity (> 90%) and high specificity (> 75%) of serum PGs.40,41 So we believe that the results may be more ideal by balancing gender, age and other factors. Particularly, these data indicated that H. pylori combined with serum PGs could reflect the severity of gastritis. Real-world follow-up results are more instructive for a multifactorial confounding reality.
The study also had some limitations. Some positive results were lost during real-world retrospective follow-up. Besides, lifestyle and special age groups at both ends (<18 and >85 years old) were not considered. Furthermore, our study only included patients living in eastern China, without extensive regional representation. Finally, the sample size was limited and more multicenter studies are needed to validate our findings.
To conclude, serum PGs were significantly correlated with severity of gastritis. According to the results of our follow-up, it could be seen that patients who progressed to GC were in OLGA stages III–IV and OLGIM stages II–III previously. Therefore, endoscopic surveillance should be performed for patients with OLGA stages III–IV or OLGIM stages III–IV. H. pylori-positive patients with OLGIM stage II also have a high risk of GC. Finally, H. pylori combined with PGI and PGR was helpful to evaluate the severity of GA and GIM.
Funding Statement
The authors received no financial support for the research, authorship, and/or publication of this article.
Abbreviations
H. pylori, Helicobacter pylori; GC, gastric cancer; GA, gastric atrophy; GIM, gastric intestinal metaplasia; OLGA, operative link on gastritis assessment; OLGIM, operative link on gastric intestinal metaplasia assessment; PGs, serum pepsinogens; G-17, gastrin-17; PGI, serum pepsinogen I; PGII, serum pepsinogen II; PGR, pepsinogen I and II ratio; PPI, proton pump inhibitor.
Data Sharing Statement
The primary contributions in this study are presented in the article. Contact the corresponding author directly for further inquiries.
Ethical Statement
The study was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. This study was reviewed and approved by the Medical Research Ethics Committee of the First Affiliated Hospital of the University of Science and Technology of China (No. 2022-RE-052). Each patient signed written informed consent.
Disclosure
The authors declare that there is no conflict of interest.
References
- 1.Smyth EC, Nilsson M, Grabsch HI, van Grieken NCT, Lordick F. Gastric cancer. Lancet. 2020;396(10251):635–648. doi: 10.1016/S0140-6736(20)31288-5 [DOI] [PubMed] [Google Scholar]
- 2.Thrift AP, El-Serag HB. Burden of gastric cancer. Clin Gastroenterol Hepatol. 2020;18(3):534–542. doi: 10.1016/j.cgh.2019.07.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 4.Cai Q, Zhu C, Yuan Y, et al. Development and validation of a prediction rule for estimating gastric cancer risk in the Chinese high-risk population: a nationwide multicentre study. Gut. 2019;68(9):1576–1587. doi: 10.1136/gutjnl-2018-317556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Correa P. Human gastric carcinogenesis: a multistep and multifactorial process--first American cancer society award lecture on cancer epidemiology and prevention. Cancer Res. 1992;52(24):6735–6740. [PubMed] [Google Scholar]
- 6.Kuipers EJ. Review article: exploring the link between Helicobacter pylori and gastric cancer. Aliment Pharmacol Ther. 1999;13(Suppl 1):3–11. doi: 10.1046/j.1365-2036.1999.00002.x [DOI] [PubMed] [Google Scholar]
- 7.de Vries AC, van Grieken NC, Looman CW, et al. Gastric cancer risk in patients with premalignant gastric lesions: a nationwide cohort study in the Netherlands. Gastroenterology. 2008;134(4):945–952. doi: 10.1053/j.gastro.2008.01.071 [DOI] [PubMed] [Google Scholar]
- 8.Genta RM. Recognizing atrophy: another step toward a classification of gastritis. Am J Surg Pathol. 1996;20:23–30. doi: 10.1097/00000478-199600001-00004 [DOI] [PubMed] [Google Scholar]
- 9.Rugge M, Meggio A, Pennelli G, et al. Gastritis staging in clinical practice: the OLGA staging system. Gut. 2007;56(5):631–636. doi: 10.1136/gut.2006.106666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Capelle LG, de Vries AC, Haringsma J, et al. The staging of gastritis with the OLGA system by using intestinal metaplasia as an accurate alternative for atrophic gastritis. Gastrointest Endosc. 2010;71(7):1150–1158. doi: 10.1016/j.gie.2009.12.029 [DOI] [PubMed] [Google Scholar]
- 11.Rugge M, de Boni M, Pennelli G, et al. Gastritis OLGA-staging and gastric cancer risk: a twelve-year clinico-pathological follow-up study. Aliment Pharmacol Ther. 2010;31(10):1104–1111. doi: 10.1111/j.1365-2036.2010.04277.x [DOI] [PubMed] [Google Scholar]
- 12.Rugge M, Genta RM, Fassan M, et al. OLGA gastritis staging for the prediction of gastric cancer risk: a long-term follow-up study of 7436 patients. Am J Gastroenterol. 2018;113(11):1621–1628. doi: 10.1038/s41395-018-0353-8 [DOI] [PubMed] [Google Scholar]
- 13.Pimentel-Nunes P, Libanio D, Marcos-Pinto R, et al. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019;51(4):365–388. doi: 10.1055/a-0859-1883 [DOI] [PubMed] [Google Scholar]
- 14.Annibale B, Esposito G, Lahner E. A current clinical overview of atrophic gastritis. Expert Rev Gastroenterol Hepatol. 2020;14(2):93–102. doi: 10.1080/17474124.2020.1718491 [DOI] [PubMed] [Google Scholar]
- 15.Chen XZ, Huang CZ, Hu WX, Ying L, Yao XQ. Gastric cancer screening by combined determination of serum helicobacter pylori antibody and pepsinogen concentrations: abc method for gastric cancer screening. Chin Med J. 2018;131(010):1232–1239. doi: 10.4103/0366-6999.231512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuipers EJ. In through the out door serology for atrophic gastritis. Eur J Gastroenterol Hepatol. 2003;15:877–879. doi: 10.1097/00042737-200308000-00007 [DOI] [PubMed] [Google Scholar]
- 17.Rugge M, Fassan M, Graham DY. Clinical guidelines: secondary prevention of gastric cancer. Nat Rev Gastroenterol Hepatol. 2012;9(3):128–129. doi: 10.1038/nrgastro.2012.19 [DOI] [PubMed] [Google Scholar]
- 18.Ranjbar R, Behzadi P, Farshad S. Advances in diagnosis and treatment of Helicobacter pylori infection. Acta Microbiol Immunol Hung. 2017;64(3):273–292. doi: 10.1556/030.64.2017.008 [DOI] [PubMed] [Google Scholar]
- 19.Rugge M, Genta RM, Graham DY, et al. Chronicles of a cancer foretold: 35 years of gastric cancer risk assessment. Gut. 2016;65(5):721–725. doi: 10.1136/gutjnl-2015-310846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Z, Graham DY, Khan A, et al. Incidence of gastric cancer in the USA during 1999 to 2013: a 50-state analysis. Int J Epidemiol. 2018;47(3):966–975. doi: 10.1093/ije/dyy055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney system international workshop on the histopathology of gastritis, Houston 1994. Am J Surg Pathol. 1996;20(10):1161–1181. [DOI] [PubMed] [Google Scholar]
- 22.Rugge M, Genta RM, Group O. Staging gastritis: an international proposal. Gastroenterology. 2005;129(5):1807–1808. doi: 10.1053/j.gastro.2005.09.056 [DOI] [PubMed] [Google Scholar]
- 23.Cho SJ, Choi IJ, Kook MC, et al. Staging of intestinal- and diffuse-type gastric cancers with the OLGA and OLGIM staging systems. Aliment Pharmacol Ther. 2013;38(10):1292–1302. doi: 10.1111/apt.12515 [DOI] [PubMed] [Google Scholar]
- 24.Lee JWJ, Zhu F, Srivastava S, et al. Severity of gastric intestinal metaplasia predicts the risk of gastric cancer: a prospective multicentre cohort study (GCEP). Gut. 2021;71(5):854–863. doi: 10.1136/gutjnl-2021-324057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang X, Lu B, Meng L, Fan Y, Zhang S, Li M. The correlation between histological gastritis staging- ‘OLGA/OLGIM’ and serum pepsinogen test in assessment of gastric atrophy/intestinal metaplasia in China. Scand J Gastroenterol. 2017;52(8):822–827. doi: 10.1080/00365521.2017.1315739 [DOI] [PubMed] [Google Scholar]
- 26.Yue H, Shan L, Bin L. The significance of OLGA and OLGIM staging systems in the risk assessment of gastric cancer: a systematic review and meta-analysis. Gastric Cancer. 2018;21(4):579–587. doi: 10.1007/s10120-018-0812-3 [DOI] [PubMed] [Google Scholar]
- 27.Miki K. Gastric cancer screening by combined assay for serum anti-Helicobacter pylori IgG antibody and serum pepsinogen levels - “ABC method”. Proc Jpn Acad Ser B Phys Biol Sci. 2011;87(7):405–414. doi: 10.2183/pjab.87.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kawaguchi H, Haruma K, Komoto K, Yoshihara M, Sumii K, Kajiyama G. Helicobacter pylori infection is the major risk factor for atrophic gastritis. Gastroenterology. 1996;108(5):959–962. [PubMed] [Google Scholar]
- 29.Kim N, Park YS, Cho SI, et al. Prevalence and risk factors of atrophic gastritis and intestinal metaplasia in a Korean population without significant gastroduodenal disease. Helicobacter. 2008;13:4. doi: 10.1111/j.1523-5378.2008.00604.x [DOI] [PubMed] [Google Scholar]
- 30.Ohkuma K, Okada M, Murayama H, et al. Association of Helicobacter pylori infection with atrophic gastritis and intestinal metaplasia. J Gastroenterol Hepatol. 2000;15(10):1105–1112. doi: 10.1046/j.1440-1746.2000.02305.x [DOI] [PubMed] [Google Scholar]
- 31.Miki K, Urita Y. Using serum pepsinogens wisely in a clinical practice. J Dig Dis. 2007;8(1):8–14. doi: 10.1111/j.1443-9573.2007.00278.x [DOI] [PubMed] [Google Scholar]
- 32.Dinis-Ribeiro M, Areia M, Vries ACD, et al. Management of precancerous conditions and lesions in the stomach (MAPS): guideline from the European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter Study Group (EHSG), European Society of Pathology (ESP), and the Sociedade Portuguesa de Endoscopia Digestiva (SPED). Virchows Archiv. 2012;44(1):74–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection-The Maastricht V/Florence consensus report. Gut. 2017;66(1):6–30. doi: 10.1136/gutjnl-2016-312288 [DOI] [PubMed] [Google Scholar]
- 34.Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015;64(9):1353–1367. doi: 10.1136/gutjnl-2015-309252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hedayati MA, Salavati S. Transcriptional profile of helicobacter pylori virulence genes in patients with gastritis and gastric cancer. Can J Infect Dis Med Microbiol. 2021;2021:1309519. doi: 10.1155/2021/1309519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yun CY, Kim N, Lee J, et al. Usefulness of OLGA and OLGIM system not only for intestinal type but also for diffuse type of gastric cancer, and no interaction among the gastric cancer risk factors. Helicobacter. 2018;23(6):e12542. doi: 10.1111/hel.12542 [DOI] [PubMed] [Google Scholar]
- 37.Maura G, Chaignot C, Weill A, Alla F, Heard I. Cervical cancer screening and subsequent procedures in women under the age of 25 years between 2007 and 2013 in France: a nationwide French healthcare database study. Eur J Cancer Prev. 2018;27(5):479–485. doi: 10.1097/CEJ.0000000000000360 [DOI] [PubMed] [Google Scholar]
- 38.Miki K. Gastric cancer screening using the serum pepsinogen test method. Gastric Cancer. 2006;9(4):245–253. doi: 10.1007/s10120-006-0397-0 [DOI] [PubMed] [Google Scholar]
- 39.Mizuno S, Kobayashi M, Tomita S, et al. Validation of the pepsinogen test method for gastric cancer screening using a follow-up study. Gastric Cancer. 2009;12(3):158–163. doi: 10.1007/s10120-009-0522-y [DOI] [PubMed] [Google Scholar]
- 40.Huang YK, Yu JC, Kang WM, et al. Significance of serum pepsinogens as a biomarker for gastric cancer and atrophic gastritis screening: a systematic review and meta-analysis. PLoS One. 2015;10(11):e0142080. doi: 10.1371/journal.pone.0142080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zagari RM, Rabitti S, Greenwood DC, Eusebi LH, Vestito A, Bazzoli F. Systematic review with meta-analysis: diagnostic performance of the combination of pepsinogen, gastrin-17 and anti-Helicobacter pylori antibodies serum assays for the diagnosis of atrophic gastritis. Aliment Pharmacol Ther. 2017;46(7):657–667. doi: 10.1111/apt.14248 [DOI] [PubMed] [Google Scholar]