Abstract
The monkeypox virus outbreak continues to evolve worldwide. While most people recover without treatment, primary care clinicians may be the first point of contact for those affected. Prompt assessment, diagnosis, isolation, treatment and prophylaxis will reduce the risk of community transmission. The current public health advice is to test suspected cases and monitor close contacts. If individuals test positive for the monkeypox virus, self-isolation at home is recommended for most people with mild symptoms. If patients report severe symptoms, referral and admission to hospital will be needed, where further interventions such as antivirals may be administered. The infection can spread through close contact; therefore, healthcare professionals must take precautions, such as using appropriate personal protective equipment for possible or probable cases.
Keywords: Evidence-based practice, guidelines, infectious diseases, public health
Introduction
Since its discovery in 1958 in monkeys, the monkeypox virus has been rarely found outside west and central Africa until the current outbreak. The first human case of the virus was in an infant from the Democratic Republic of Congo (DRC) in 1970; the infection has since spread to other regions, primarily in Africa. The first case of the current outbreak was confirmed on 6 May 2022, in the UK and was linked to travel to Nigeria. 1 Two subsequent UK cases were detected a week later; however, neither affected individuals reported contact with the primary case in the UK nor travel to Africa. 1 On 23 July 2022, the World Health Organization (WHO) declared the current monkeypox outbreak a public health emergency of international concern, as the number of cases increased rapidly around the world. 2 As of 9 September 2022, 57,016 cases have been confirmed in 96 non-endemic regions, with the UK having one of the highest number of cases worldwide (3484 cases). 3
As we understand more about the current outbreak, particularly the community transmission of the virus, primary care clinicians may be the first point of healthcare access. 4 Therefore, awareness of the signs and symptoms of the disease and current management strategies is crucial to providing optimal care and advice to patients. This article discusses the diagnosis and management of monkeypox in the UK primary care system.
What is monkeypox?
Monkeypox is a rare viral zoonotic disease caused by the monkeypox virus, which belongs to the Poxiviridae family and Orthopoxvirus genus. 5 The Orthopoxvirus genus also includes the variola virus, which causes smallpox. 6 While smallpox and monkeypox share similar disease patterns, the latter is less virulent. 5 Two common clades of monkeypox virus exist: central African and west African. 5 Of the two, the central African clade is a more common cause of the disease and can be transmitted between humans. 5 Common reservoirs of the monkeypox virus include rodents and primates. 5 The virus can be transmitted through contact with infected animals or other infected material, such as blood, bodily fluids, spots, blisters or scabs. 7 Monkeypox can also be caught by eating uncooked meat from an infected animal. 3 Additionally, human-to-human transmission can occur through contact via bodily fluids and skin lesions. 7 The virus enters intradermally or through the respiratory system. 7 Monkeypox may also be vertically transmitted during pregnancy or birth. 5 Viral replication occurs at the entry site, before dissemination to local lymph nodes and throughout the body. 7
Epidemiology of monkeypox
Before the emergence of monkeypox in non-endemic regions around the globe in May 2022, 5 cases commonly emerged in central and western Africa, mainly the DRC,8,9 with sporadic cases arising globally and linked to travel from endemic countries. As of 2017, monkeypox cases within Nigeria began to rise, making it the second most affected country in Africa. 8 The first case reported outside Africa was in 2003 in the USA. 8 Cases were linked to contact with infected prairie dogs, which were in contact with rodents from Ghana. Other countries outside Africa, including Israel, UK and Singapore, have previously seen sporadic monkeypox cases. 8
There has been a notable increase in monkeypox incidence in Africa recently. In 2001, the incidence within DRC was 0.64/100,000, and in 2013 it increased to 2.82/100,000. 8 The case fatality ratio (CFR) is around 3%–6% globally, 8 although historically, when comparing the CFR between the two clades, the central African clade (10.6%) is significantly higher than the west African clade (3.6%) based on case numbers from 1970 to 2019. 8 In the current outbreak, as of 9 September 2022, the UK has reported no deaths from the monkeypox virus. 3
What are the risk factors for monkeypox?
Contact with infected animals, such as rodents or primates, is a risk factor for contracting monkeypox, 5 increasing susceptibility in individuals who handle animals, hunt or cook meat. 9 Furthermore, men are more likely to contract monkeypox. 8 Historically, this was because men held the hunter role in endemic regions, explaining why many cases were seen in this population. 7 In addition, travel to endemic areas such as countries in the west or central Africa has increased the disease risk, 5 especially in rural and forested regions. 8 Close physical contact with infected individuals also increases the likelihood of infection. Those at risk include caregivers, healthcare personnel and those with multiple sexual partners, including men who have sex with men. 8 Evidence suggests that monkeypox nucleic acid can be found in semen after an acute infection. 10 Additionally, the monkeypox attack rate is higher among individuals not vaccinated with the smallpox vaccine, which is 85% protective. 11
While previous outbreaks have documented cases of human-to-human transmission, 9 current epidemiological patterns differ, as cases without any link to endemic regions emerged in May 2022. 12 Moreover, many cases during the 2022 outbreak have arisen from individuals with multiple sexual partners, including gay, bisexual and other men who have sex with men (GBMSM). 1
Clinical signs of monkeypox
The incubation period for monkeypox is 5–21 days; however, individuals generally present 6–16 days after exposure. 13 Symptoms are usually self-limiting and resolve within 2–4 weeks. 14 However, individuals at risk for a more severe infection may experience complications leading to death. Patients classically present with symptoms in two stages. In the prodromal stage, individuals may experience fever, chills, lymphadenopathy, myalgia, headache and fatigue, lasting for about 1–5 days. 7 These symptoms are often difficult to distinguish from those caused by many other viral illnesses.
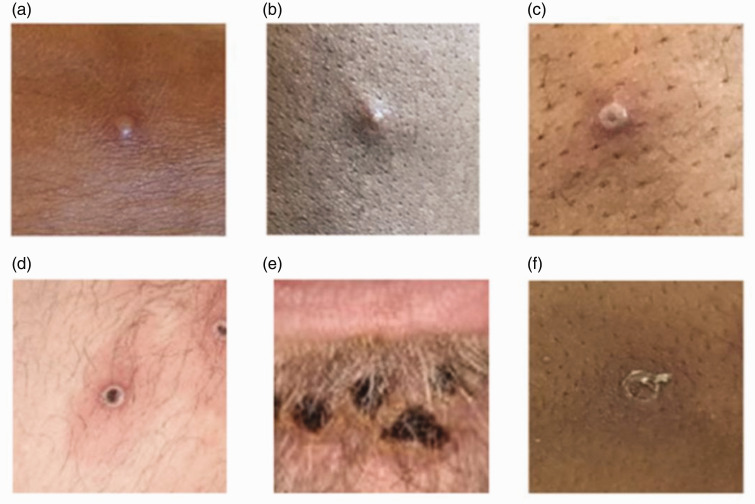
During the second stage, rashes and ulcers appear, while other symptoms during the first stage dissipate. 7 Initially, a maculopapular rash appears and evolves into vesicles and then pustules (Figure 1). 7 The rash eventually ulcerates and crusts before the scab falls off and the lesion heals (Figure 1). 7 In addition, patients may initially present with an enanthem, 14 which then turns into a rash near their face or genitalia before it spreads peripherally to their hands and feet. 7
Figure 1.
This image is obtained from the UKHSA’s Monkeypox: background information guidance published in 2018. 11 The image depicts the monkeypox lesions and how they change over the course of the disease from a vesicle to a pustule, which then ulcerates and crusts before the scab falls off. (a) Early vesicle, 3 mm diameter. (b) Small pustule, 2 mm diameter. (c) Umbilicated pustule, 3–4 mm diameter. (d) Ulcerated lesion, 5 mm diameter. (e) Crusting of mature lesions and (f) Partially removed scab.
Increased severity of infection is seen in children, pregnant women and immunocompromised individuals, including those infected with HIV and those with skin conditions. 15 These individuals may also experience complications such as sepsis, encephalitis, pneumonia, permanent skin scarring or bacterial superinfection of the skin. 7 There have also been cases during the current outbreak that diverge from the usual presentation of monkeypox. 16 For example, asymptomatic cases may arise, or individuals may present with an atypical rash and prodrome. 16
How to approach patients
Although cases are rising globally, monkeypox remains a rare infection; therefore, it is essential to consider other potential causes for the rash and prodromal symptoms. The site and the appearance of the rash near the mouth or genitalia, 14 along with the clinical risk factors and manifestations, could help with the diagnosis. Moreover, it is crucial to consider the patients’ social and travel history. Other potential diagnoses could be sexually transmitted infections such as syphilis. 7 Additionally, causes of similar rashes may include allergic reactions, varicella zoster virus (VZV), herpes simplex virus, scabies and measles. 7
One of the most important differential diagnoses is chickenpox (VZV). In chickenpox, the rash is generally distributed around the trunk, while in monkeypox, the rash appears around the extremities and face. 14 In addition, the rash for VZV is itchy, 17 whereas, for monkeypox, it is painful initially until it scabs and becomes itchy. 14
Clinicians should also be alert to the social, economic and psychological impacts of the disease. Previous studies have shown the negative psychological impact of contracting an infectious disease during an outbreak, 18 including anxiety and depression. 19 Hence, clinicians may be able to provide resources to aid patients during their quarantine. Moreover, social history may also help local public health units with contact tracing.
How to manage patients with suspected or confirmed monkeypox
New information about monkeypox management is still being released frequently by the UK Health Security Agency (HSA). However, primary care may be the first port of call for individuals with monkeypox symptoms.
Monkeypox is a notifiable disease in the UK; therefore, general practitioners (GPs) must inform their local public health units of possible or probable cases. 20 The UK HSA defines a possible case as a person experiencing prodromal symptoms who was in contact with a confirmed case 21 days before symptom onset or a person the clinician highly suspects of having the disease. 21 A probable case is defined as someone who has a rash with one or more symptoms of monkeypox from 15 March 2022 onwards with one of the following: a link with another probable or confirmed case of monkeypox 21 days before symptom onset or travel history to endemic regions 21 days before symptom onset or is a GBMSM. 21 GPs can recommend testing to rule out other diagnoses. 21 A highly probable case is defined as an individual with a positive PCR result for orthopox viruses who is likely to have monkeypox. A confirmed case is an individual whose laboratory tests are positive for the monkeypox virus. 21
If an individual suspects that they have monkeypox, they can contact their local sexual health clinic or other healthcare providers and isolate themselves until they receive further instructions. 22 Currently, testing may involve collecting a throat swab, a urine or blood sample or samples of skin lesions, which can be tested for monkeypox DNA by real-time PCR. 23 Individuals may also request PCR testing of semen 12 weeks after an acute infection to ensure the virus is completely cleared.10
To control community spread, the UK HSA recommends identifying potential close contacts and contacting them to determine if they are symptomatic and recommend testing or quarantine. 23 Hence, GPs should enquire whether the patient has had contact with others and inform the patient to report this information to the local public health unit. In the UK, contact tracing and sample collection are the responsibility of the UK HSA, with support from local public health, hospital and sexual health teams.22,23
Self-isolation
If the test results are positive, symptoms are initially managed with supportive care. The UK HSA recommends that individuals isolate themselves at home until they are no longer contagious. Patients are infectious until the skin lesions and scabs disappear and heal over, 24 which may take up to 21 days. 7 Moreover, patients should limit their interaction with others and follow the guidance of public health officials to prevent infection of other household members and animals. This may involve remaining 3 m away from others, wearing a medical mask around other individuals and wearing clothing that will cover the lesions. 25 During their isolation, public health officials or other healthcare providers, including GPs, will be in contact with patients. In some cases, if patients present or report more severe symptoms, the medical team may refer them to hospitals for specialist care. 22
Antivirals
While GPs do not provide antiviral therapy, patients may need treatment in hospital if they present with severe disease. Antivirals can reduce symptoms in patients with severe disease; however, evidence for their use in monkeypox is limited. 15 The United States Centers for Disease Control and Prevention (CDC) and the UK HSA have approved the following treatments for monkeypox in patients with severe disease: Tecovirimat, Brincidofovir, Vaccinia Immune Globulin Intravenous (VIGIV) and Cidofovir. 15
Tecovirimat and Brincidofovir are oral antivirals used to treat smallpox in children and adults. The former inhibits the orthopoxvirus VP37 envelope wrapping protein, 26 and the latter is an orthopoxvirus DNA polymerase inhibitor (prodrug of Cidofovir). 27 VIGIV is traditionally used to treat complications after vaccinia vaccination. In addition, individuals with severe T cell immunodeficiency exposed to monkeypox may be given VIGIV to reduce symptoms. 15 Cidofovir is an antiviral used to treat severe adenovirus infection. 27 It is important to note that renal toxicity is seen with this drug; hence, Brincidofovir, a prodrug of Cidofovir, with less renal toxicity may be preferred. 15
Post-exposure vaccination
The UK HSA also recommends providing post-exposure vaccination with the live modified vaccinia Ankara vaccine (MVA-BN) ideally within 4 days, but up to 14 days after exposure in some patients. 28 GPs do not administer this vaccine in the UK; instead, they are available through local NHS clinics. The current recommendation includes administering the vaccine to people with a significant exposure deemed high risk for severe monkeypox disease. 28 This comprises some healthcare providers, pregnant women, children under 11 years and mildly immunosuppressed individuals. 28 Patients are given two doses of the vaccination 4 weeks apart. 7 The MVA-BN vaccine is contraindicated in patients with a previous anaphylactic reaction to the vaccine and its components. 29 The vaccine contains chicken protein, ciprofloxacin, gentamicin and benzonase; hence, individuals allergic to these components should not receive the vaccine. 29 In addition, patients with significant immunodeficiency or immunocompromise should not receive the vaccine, as it is a live-attenuated vaccine, and they could develop severe monkeypox infection as a result of the vaccine. 28 The vaccine has a good safety profile and rarely causes lasting side effects. 29 Common side effects of the MVA-BN vaccine include chills, fever, pruritis and redness near the injection site, headache and muscle aches; however, these should not last for more than a few days. 29 Some individuals may have an anaphylactic reaction to the vaccine and present with life-threatening symptoms such as difficulty breathing, prolonged loss of consciousness or confusion. 29 Side effects with the MVA-BN are more common among patients who have received a previous dose of the older version of the smallpox vaccine. 29
Discussing prevention with patients
WHO has outlined strategies to prevent monkeypox infection, including reducing zoonotic and human-to-human transmission and restricting animal trade. 5 However, advice on prevention should be given sensitively and tailored to individual patient’s circumstances.
To minimise transmission between humans, the UK has implemented contact tracing for close contacts of confirmed cases. In addition, the UK HSA recommends using personal protective equipment, which includes FFP3 respirators, aprons, eye protection and gloves for confirmed cases and fluid repellent surgical facemasks, gowns, gloves and eye protection for possible or probable cases. 30 Furthermore, individuals should be advised to avoid using or contacting soiled clothing or linen from suspected or confirmed cases. 22 Other advice includes practising safe sex 1 and maintaining regular hand hygiene. 22
Pre-exposure vaccination
As previous studies have demonstrated protection from monkeypox if vaccinated with the smallpox vaccine, the UK has started implementing pre-exposure vaccination for high-risk groups. This includes healthcare workers who will care for patients with monkeypox, staff working at sexual health clinics and GBMSM at the highest risk of becoming infected. 28 However, as stated above, the vaccine should not be given to severely immunocompromised individuals, as it is a live-attenuated viral vaccine. 28
Conclusion
The current monkeypox outbreak is rapid. Primary care clinicians have a crucial role in prompt assessment, diagnosis and advice to reduce the community transmission of the virus, especially among high-risk groups. This includes notifying public health authorities of suspected cases and guiding patients to appropriate specialist services.
Declarations
Competing Interests
None declared.
Funding
AM is supported by the National Institute for Health Research, Applied Research Collaboration Northwest London.
Ethics approval
Not applicable.
Guarantor
SR.
Contributorship
SR wrote the article, incorporated feedback from co-authors and finalised the article. MSR conceived the article and contributed to the original draft, revisions and concept. AM and SD contributed to the revision and concept. All authors read and approved the final article.
Acknowledgements
The views expressed in this publication are those of the authors and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Provenance
Not commissioned; externally peer-reviewed.
ORCID iDs
Smrithi Rallapalli https://orcid.org/0000-0003-2907-0400
Mohammad S Razai https://orcid.org/0000-0002-6671-5557
Azeem Majeed https://orcid.org/0000-0002-2357-9858
References
- 1.UK Health Security Agency. Monkeypox cases confirmed in England – latest updates. See www.gov.uk/government/news/monkeypox-cases-confirmed-in-england-latest-updates (last checked 10 September 2022).
- 2.World Health Organization. WHO Director-General’s statement at the press conference following IHR Emergency Committee regarding the multi-country outbreak of monkeypox – 23 July 2022. See www.who.int/director-general/speeches/detail/who-director-general-s-statement-on-the-press-conference-following-IHR-emergency-committee-regarding-the-multi–country-outbreak-of-monkeypox–23-july-2022 (last checked 5 September 2022).
- 3.Centers for Disease Control and Prevention. 2022 Monkeypox Outbreak Global Map | Monkeypox | Poxvirus. See www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html (last checked 10 September 2022).
- 4.Schachner T, Bonatti J, Bonaros N, Poeltl R, Feuchtner G, Laufer G, et al. Risk factors of postoperative nephropathy in patients undergoing innovative CABG and intraoperative graft angiography. Eur J Cardiothorac Surg 2006; 30: 431–435. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Monkeypox. See www.who.int/news-room/fact-sheets/detail/monkeypox (last checked 19 June 2022).
- 6.Centers for Disease Control and Prevention. About Monkeypox | Monkeypox | Poxvirus. See www.cdc.gov/poxvirus/monkeypox/about.html (last checked 27 June 2022).
- 7.Moore MJ, Rathish B, and Zarah F. Monkeypox. In: StatPearls. Treasure Island (FL): StatPearls Publishing, http://www.ncbi.nlm.nih.gov/books/NBK574519/ (2022, accessed 19 June 2022). [Google Scholar]
- 8.Bunge EM, Hoet B, Chen L, Lienert F, Weidenthaler H, Baer LR, et al. The changing epidemiology of human monkeypox – a potential threat? A systematic review. PLOS Negl Trop Dis 2022; 16: e0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beer EM, Rao VB. A systematic review of the epidemiology of human monkeypox outbreaks and implications for outbreak strategy. PLOS Negl Trop Dis 2019; 13: e0007791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.UK Health Security Agency. Monkeypox: semen testing for viral DNA. See www.gov.uk/guidance/monkeypox-semen-testing-for-viral-dna (last checked 13 August 2022).
- 11.UK Health Security Agency. Monkeypox: background information. GOV.UK. See www.gov.uk/guidance/monkeypox (last checked 27 June 2022).
- 12.World Health Organization. Multi-country monkeypox outbreak in non-endemic countries. See www.who.int/emergencies/disease-outbreak-news/item/2022-DON385 (last checked 23 June 2022).
- 13.UK Health Security Agency. Monkeypox: information for primary care. See www.gov.uk/guidance/monkeypox-information-for-primary-care (last checked 27 June 2022).
- 14.Centers for Disease Control and Prevention. Monkeypox in the U.S. See www.cdc.gov/poxvirus/monkeypox/clinicians/clinical-recognition.html (last checked 6 July 2022).
- 15.Centers for Disease Control and Prevention. Treatment Information for Healthcare Professionals | Monkeypox | Poxvirus. See www.cdc.gov/poxvirus/monkeypox/clinicians/treatment.html (last checked 27 June 2022).
- 16.Moore ZS. –Poxviridae. In: Long SS, ed. Principles and Practice of Pediatric Infectious Disease (Third Edition). Edinburgh: W.B. Saunders, 2008:1006–1011.
- 17.Centers for Disease Control and Prevention. Chickenpox Signs and Symptoms. See www.cdc.gov/chickenpox/about/symptoms.html (last checked 6 July 2022).
- 18.Ogoina D, Izibewule JH, Ogunleye A, Ederiane E, Anebonam U, Neni A, et al. The 2017 human monkeypox outbreak in Nigeria – report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. PLoS One 2019; 14: e0214229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li J, Yang Z, Qiu H, Wang Y, Jian L, Ji J, et al. Anxiety and depression among general population in China at the peak of the COVID‐19 epidemic. World Psychiatry 2020; 19: 249–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iacobucci G. Monkeypox: doctors in England will have to notify local agencies of all suspected cases. BMJ 2022; 377: o1413. [DOI] [PubMed] [Google Scholar]
- 21.UK Health Security Agency. Monkeypox: case definitions. See www.gov.uk/guidance/monkeypox-case-definitions (last checked 6 July 2022).
- 22.National Health Service. Monkeypox. See www.nhs.uk/conditions/monkeypox/ (last checked 22 June 2022).
- 23.UK Health Security Agency. Monkeypox: diagnostic testing. See www.gov.uk/guidance/monkeypox-diagnostic-testing (last checked 27 June 2022).
- 24.UK Health Security Agency. De-isolation and discharge of monkeypox-infected patients: interim guidance. See www.gov.uk/guidance/de-isolation-and-discharge-of-monkeypox-infected-patients-interim-guidance (last checked 27 June 2022).
- 25.Centers for Disease Control and Prevention. Isolation and Infection Control: Home | Monkeypox | Poxvirus. See www.cdc.gov/poxvirus/monkeypox/clinicians/infection-control-home.html (last checked 27 June 2022).
- 26.Kennedy RB, Lane JM, Henderson DA, and Poland GA. Smallpox and vaccinia. In: Plotkin SA, Orenstein WA, Offit PA, Edwards KM, eds. Plotkin’s Vaccines (Seventh Edition). Amsterdam: Elsevier, 2017: 1001–1030.e12.
- 27.Sudhindra P, Knoll B, Nog R, Singh N, Dhand A. Brincidofovir (CMX001) for the treatment of severe adenoviral pneumonia in kidney transplant recipient. Cureus; 11: e5296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.UK Health Security Agency. Monkeypox vaccination recommendations. See www.gov.uk/government/publications/monkeypox-vaccination (last checked 2 September 2022).
- 29.UK Health Security Agency. Protecting you from monkeypox: information on the smallpox vaccination. See www.gov.uk/government/publications/monkeypox-vaccination-resources/protecting-you-from-monkeypox-information-on-the-smallpox-vaccination (last checked 5 September 2022).
- 30.UK Health Security Agency. Public health agencies issue monkeypox guidance to control transmission. See www.gov.uk/government/news/public-health-agencies-issue-monkeypox-guidance-to-control-transmission (last checked 9 July 2022).