Abstract
Introduction
Small bowel obstruction (SBO) is recognized as the most common surgical emergency following abdominal procedures. Moreover, a pneumothorax secondary to an SBO is an infrequent phenomenon less commonly reported in recent literature. Clinical presentation includes progressive dyspnea and fatigue. The diagnosis was made with imaging. In this case report, the authors present a rare case of concurrent surgical complications (pneumothorax, SBO, perforation of the stomach, and hiatal hernia).
Case presentation
A 62 years-old African American patient who presented with severe sudden onset difficulty breathing two days following laparoscopic toupet fundoplication procedure. She was given oxygen via cannula and the underwent chest tube insertion. She was then transferred to different facility under care of a cardio thoracic surgeon.
Clinical discussion
Although SBO is most common emergency following an abdominal procedure, pneumothorax is rarely reported. This case report depicts a unique presentation of pneumothorax secondary to SBO and a discussion section conferring complication risk versus benefits of diverse management modalities (surgical or conservative), and a review of recent literature, further aiding healthcare professionals in the diagnosis and management of patients with SBO complications.
Conclusion
Review of this case and the literature show a rare presentation of secondary pneumothorax following exploratory laparotomy for SBO. Recognizing the clinical signs and even a small suspicion should prompt one to order imaging. Chest X-ray is inexpensive and can rapidly rule out pneumothorax. These complications have high mortality in patients above the age of 60 years, hence, timely management is of utmost importance.
Keywords: Secondary pneumothorax, Small bowel obstruction, Hiatal hernia, Incisional hernia, Case report, Laparoscopic, Complication
Highlights
-
•
A patient presented with severe dyspnea two days after exploratory laparotomy.
-
•
Imaging showed secondary pneumothorax post small bowel obstruction.
-
•
The patient was put on oxygen and chest tube insertion was done.
-
•
The patient was transferred to a facility under care of a cardio-thoracic surgeon.
1. Introduction
SBO is a surgical emergency characterized by mechanical obstruction of the small bowel posing a structural barrier, further impeding physiologic, structural flow [1]. The most common etiologies for SBO are post-surgical adhesions following procedures of the abdomen and/or incarcerated hernias [1]. Other occasional causes include inflammatory bowel disease (IBD): Crohn's disease (CD) and ulcerative colitis (UC), tuberculosis (TB), and malignancy affecting the abdomen [1]. Adhesions of the bowel can be further described as a cluster of fibrous intraperitoneal strands of scar tissue [1]. SBOs can be categorized as partial or complete blockage and further complicated by strangulation [1]. Clinical manifestations of SBO include abdominal pain, nausea, vomiting, constipation, abdominal distention, and decreased bowel sounds. As observed in this patient, secondary spontaneous pneumothorax is commonly reported in subjects aged 60–65 years with an incidence of 2 cases per 100,000 in females and approximately three times more common in males with 6.3 cases. In this case report, we describe a 62-year-old female who developed pneumothorax two days following an SBO.
2. Methodology
The authors of this manuscript performed an electronic database search of scientific platforms such as PubMed, PubMed Central (PMC), Google Scholar, and SCOPUS. Alongside reporting a unique case presentation, the authors reviewed and reported recent literature on the topic of interest. Peer-reviewed published articles were selected based on the keywords mentioned above. This case has been reported in line with the SCARE 2020 criteria and guidelines [2].
3. Case presentation
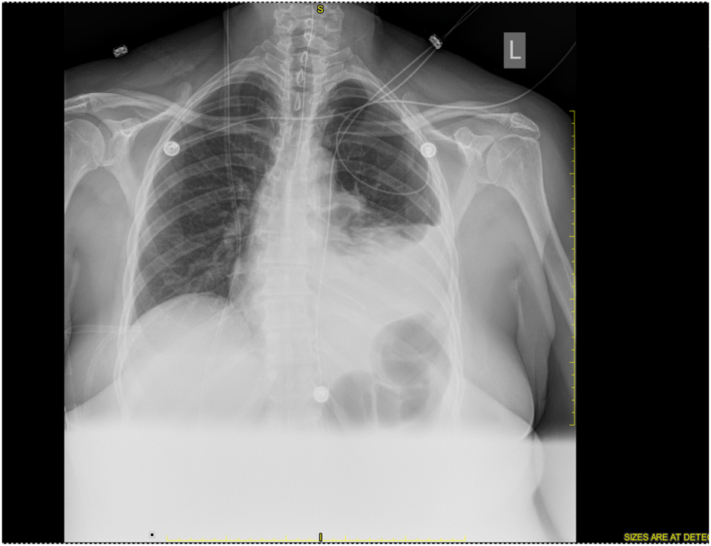
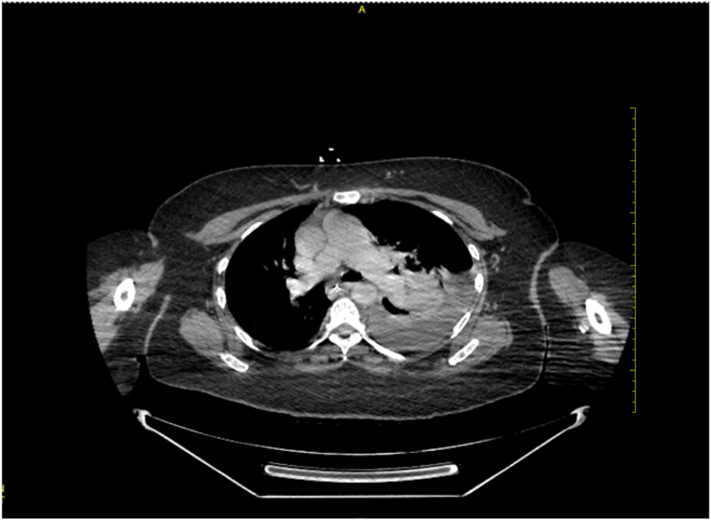
A 62-year-old African American female was admitted to the emergency room post-op day 2 with severe sudden onset difficulty breathing following a laparoscopic toupet fundoplication procedure. A chest X-ray (CXR) revealed a large left-sided pneumothorax (Fig. 1). The patient had a recent laparoscopic toupet fundoplication performed two days prior, which further resulted in a closed-loop SBO complication. Furthermore, the patient had a nasogastric tube (NG) tube placed with difficulty, further causing a stomach perforation (2–2.5 L/day secretions) alongside increased backpressure, progressing to a herniation of her abdominal cavity into the thorax without obstruction or gangrene (Fig. 2). The surgeon (Dr. Rizwan Chaudhry) also performed a ventral hernia repair and paraesophageal hiatal hernia repair alongside the toupet fundoplication procedure. A computed tomography (CT) scan was conducted, which further confirmed the large left-side pneumothorax and NG tube in the thoracic cavity (Fig. 3). The patient has a past surgical history of carcinoid tumor of the right colon that was resected by laparoscopic extended right hemicolectomy in 2008, appendectomy in 2007, total abdominal hysterectomy in 2004, and cholecystectomy in 2003, incisional hernia repair in 2021, and paraesophageal hiatal hernia repair in 2021. The patient also has past medical history of arthritis, sulfa allergy, hypertension, high cholesterol, occipital headaches, anemia, acid reflux, and heart murmur. She takes the following medications: hydrochlorothiazide (HCTZ). 25 mg tablet 1 orally QD, omeprazole 20 mg capsule delayed release 2 capsule 30 min before morning meal orally prn, DayVigo 5 mg tablet at bedtime orally once a day, losartan potassium-HCTZ 100–25 mg 1 tablet at bedtime orally once a day, rosuvastatin calcium 10 mg one tablet orally once a day, gabapentin 300 mg one capsule orally QHS. She has family history of alcohol abuse (father), and her mother had seizure disorder, coronary artery disease. To manage her current symptoms, a chest tube was inserted to alleviate the difficulty with breathing, and the patient was further planned for care of her pneumothorax by a cardiothoracic surgeon.
Fig. 1.
Chest X-ray of left sided pneumothorax.
Fig. 2.
CT-scan demonstrating pneumothorax and NG tube in thoracic cavity.
Fig. 3.
CT-scan demonstrating pneumothorax.
4. Discussion
Acute small bowel obstruction is the most common post-op complication and is considered a surgical emergency [4]. There are about 35,000 cases per annum and the overall mortality with SBO is 10 % but increases to 30 % with bowel necrosis/perforation [4]. Thus, early diagnosis and prompt treatment are crucial in reducing the mortality rate.
There are small reliable data on the mortality of pneumothorax, but the lethality of this condition is low among young people and markedly higher in the elderly patient population [5]. Primary spontaneous pneumothorax incidence is 7 per 100,000 men and 1 per 100,000 women per year [3]. Here we present a case of pneumothorax caused secondary to increased intraluminal pressure due to the presence of the SBO in an elderly African American female with extensive surgical history.
Three days post laparoscopic hiatal hernia repair with Toupet fundoplication and laparoscopic incisional hernia repair with mesh, the patient presented with symptoms of SBO. An open surgical laparotomy was performed to treat small bowel obstruction (SBO). Two days after the open surgical laparotomy for SBO the patient presented to ER with severe respiratory distress, dyspnea, and tachycardia. A CT scan was performed which showed evidence of pneumothorax. At that time a decision was made to insert a chest tube, and the patient was referred to a cardiothoracic surgeon.
According to our extensive literature research, there are currently no reported cases of both pathologies (pneumothorax secondary to small bowel obstruction) occurring concurrently. The lack of extensive medical data and research on this topic serves as a limitation for this study. Despite the uncommon etiology, a diagnosis of pneumothorax must be included in the differential diagnosis of any patient presenting with severe respiratory distress post open surgical laparotomy for SBO management.
Surgical management is the mainstay of postop complications such as small bowel obstruction [6]. This study will help in improving patient management and outcomes. It will help surgeons intervene promptly and contribute to decreasing postop mortality. Several studies have demonstrated the accuracy of CT in confirming the diagnosis, and location of pneumothorax [6], [7]. The CT scan also provides us with general information about the thoracic cavity and abdomen and is especially relevant in the emergency department in evaluating patients with pneumothorax [6].
5. Conclusion
In conclusion, we report a unique case presentation of simultaneous surgical complications, specifically secondary pneumothorax following SBO, perforation of the abdominal cavity, and hiatal hernia in a 62 years-old African American patient with a significant past surgical history. Although SBO is the most common cause of surgical emergency readmission following abdominal surgical procedures, a pneumothorax is a rare secondary complication of SBO with an increased risk for mortality in patients aged 60 years or older, further prompting timely management.
Provenance and peer review
Not commissioned, externally peer reviewed.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Nil.
Funding
Nil.
Guarantor
Abhishek Seth, Dr. Rizwan Chaudhry.
Research registration number
-
1.
Name of the registry: Nil
-
2.
Unique identifying number or registration ID: Nil
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): Nil.
CRediT authorship contribution statement
AS: Editing, drafting, and reviewing manuscript.
IP: Conceptualization, drafting, organizing, and editing manuscript.
RC: Supervision, editing, review and final approval of manuscript.
Declaration of competing interest
None to declare.
References
- 1.Schick M.A., Kashyap S., Meseeha M. StatPearls. StatPearls Publishing; Treasure Island (FL): July 22, 2021. Small bowel obstruction.https://pubmed.ncbi.nlm.nih.gov/28846346/ Accessed March 27. [PubMed] [Google Scholar]
- 2.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. https://pubmed.ncbi.nlm.nih.gov/33181358/ Accessed November 27. [DOI] [PubMed] [Google Scholar]
- 3.McKnight C.L., Burns B. StatPearls. StatPearls Publishing; Treasure Island (FL): August 11, 2021. Pneumothorax.https://pubmed.ncbi.nlm.nih.gov/28846346/ Accessed March 27. [Google Scholar]
- 4.Rami Reddy S.R., Cappell M.S. A systematic review of the clinical presentation, diagnosis, and treatment of small bowel obstruction. Curr. Gastroenterol. Rep. 2017;19(6):28. doi: 10.1007/s11894-017-0566-9. https://pubmed.ncbi.nlm.nih.gov/28439845/ Accessed April 1. [DOI] [PubMed] [Google Scholar]
- 5.Schnell J., Koryllos A., Lopez-Pastorini A., Lefering R., Stoelben E. Spontaeous pneumothorax. Dtsch. Arztebl. Int. 2017;114(44):739–744. doi: 10.3238/arztebl.2017.0739. https://www.aerzteblatt.de/int/archive/article/194215 Accessed April 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pujahari A.K. Decision making in bowel obstruction: a review. J. Clin. Diagn. Res. 2016;10(11) doi: 10.7860/JCDR/2016/22170.8923. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5198398/ Accessed April 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta K.B., Mishra D.S., Tandon S., Sindhwani G., Tanwar T. Role of chest CT scan in determining etiology of primary spontaneous pneumothorax. Indian J. Chest Dis. Allied Sci. 2003;45(3):173–177. https://pubmed.ncbi.nlm.nih.gov/12866634/ [Accessed April 2. [PubMed] [Google Scholar]