Abstract
Objectives
Evidence-based strategies to reduce loneliness in later life are needed because loneliness impacts all domains of health, functioning, and quality of life. Volunteering is a promising strategy, as a large literature of observational studies documents associations between volunteering and better health and well-being. However, relatively few studies have used randomized controlled trials (RCTs) to examine benefits of volunteering, and none have examined loneliness. The primary objective of the Helping Older People Engage (HOPE) study is to examine the social-emotional benefits of a social volunteering program for lonely older adults. This manuscript describes the rationale and design of the trial.
Methods
We are randomly assigning adults aged 60 or older (up to 300) who report loneliness to 12 months of either AmeriCorps Seniors volunteering program or an active control (self-guided life review). Co-primary outcomes are assessed via self-report—loneliness (UCLA Loneliness Scale) and quality of life (WHOQOL-Bref). Enrollment was completed in May 2022 and follow-up assessments will continue through May 2023, with completion of primary outcomes soon thereafter.
Conclusions
Since older adults who report loneliness are less likely to actively seek out volunteering opportunities, if results support efficacy of volunteering for reducing loneliness, dissemination and scaling up efforts may involve connecting primary care patients who are lonely with AmeriCorps Seniors through aging services agencies.
This RCT is registered at clinicaltrials.gov (NCT03343483).
Keywords: Volunteerism, Social connection, Loneliness, Aging, Older adult, Quality of life
Loneliness in later life increases risk for reduced quality of life [1], morbidity [[2], [3], [4]], and mortality [[5], [6], [7]]. While not the norm, a significant portion of older adults experience loneliness [6,8,9] and its health impacts may be more pronounced in later life [10]. Humans have a ‘need to belong’ to social relationships and groups [11,12]. When this need is unmet, loneliness—perceptions of social isolation—emerges [13]. Loneliness in later life is due in part to objective circumstances—disability and frailty, environmental barriers to socialization, and bereavement [[14], [15], [16]], as well as subjective perceptions (e.g., thinking of oneself as useless) [12,17,18].
Meta-analytic reviews indicate that loneliness is responsive to behavioral interventions [19,20]. However, the evidence-base to support recommending one program over another is limited by an absence of replication; lack of clarity on mechanisms and essential intervention components (e.g., group delivery); low generalizability (e.g., enrolling socially connected participants); and limited program engagement outside research studies [21]. Few studies test existing programs; thus, there is scant data supporting effectiveness of routinely recommended programs (e.g., senior centers, friendly calling). These programs are likely effective for some older adults, to some degree, but providing social contact does not necessarily address loneliness [21]. Finally, there is lack of attention to providing, versus receiving support, as a means of fostering social connection [22], which is important given that older adults are typically motivated to maintain balanced, reciprocal relationships [23,24], and providing, versus receiving support, is more strongly associated with well-being in later life [22].
Observational studies documented numerous associated benefits of volunteering for older adults, including better mental and physical health, better physical and cognitive functioning, lower pain, higher life satisfaction, and reduced/delayed mortality [[25], [26], [27]]. Observational studies also documented changes in several dimensions of social relationships, including enhanced social support [28,29], increased social engagement [26,30,31], opportunities to meet new people [32,33], and increased number of social ties [33,34]. However, relatively few studies used randomized controlled trials (RCTs) to examine benefits of volunteering to rule out confounding and reverse causality. Two published RCTs of volunteering in later life examined volunteering in city schools for 15 h per week and documented greater physical activity, physical strength, social support (people one could turn to for help), and cognitive functioning compared to controls at 4–8 month follow-up [28]. The second trial documented increased mobility [35], physical activity [36], and prevention of atrophy in brain volume [37], as well as increases in physical, social, and cognitive activity, suggesting intensive volunteering may promote health through increased activity [38,39]. A third trial of a different intervention examined benefits of a brief intervention targeting motivation for volunteering in older adults and found benefit regarding reduced depressive symptoms for those subjects who increased their volunteering hours [40]. None of these trials examined loneliness as an outcome or required that subjects report loneliness at baseline.
The objective of the Helping Older People Engage (HOPE) study is to examine the social-emotional benefits of a social volunteering program for lonely older adults. The volunteering program is the Retired Senior Volunteer Program (RSVP)—a division of AmeriCorps Seniors, a national program administered by AmeriCorps that links adults 55 years and older to volunteer opportunities in their communities in a wide range of roles that take best advantage of their skills and experience. The U.S. Aging Services Network (ASN) is a national network of community-based social service agencies overseen by the Administration on Aging, including Area Agencies on Aging that commonly provide local support to administer RSVP programs. For the HOPE study, the volunteering intervention involves participation in the RSVP Program overseen by Lifespan of Greater Rochester, which provides aging services to older adults in the Monroe County, NY region [23]. We selected this volunteering program due to its availability nationwide, thus promoting scalability; its focus on matching older adults to valued activities that match their skill set, promoting acceptability and engagement; and its emphasis on supporting volunteers through regular contact with the volunteer coordinator to navigate problems and provide standardized training, all promoting motivation to start and sustain volunteering.
Testing an existing community program available nationwide with an RCT with an active control, HOPE is a Stage III efficacy design (NIH Stage Model for Intervention Development). [41] Given promising findings, it will lead to study of implementation/dissemination and pragmatic trial designs to rapidly move intervention science into practice. We are randomly assigning adults aged 60 or older who report loneliness to 12 months of volunteering or active control (self-guided life review). An active control was selected instead of care-as-usual in order to control for (and minimize confounding by) potential non-specific effects of participating in a study intervention; expectancies about benefit; and starting a new cognitively engaging activity. Life review is a reasonable active control because it is intellectually stimulating (also true of volunteering) but its social component is negligible (unlike volunteering).
1. Study aims
Our first aim tests whether one-year of volunteering results in reduced loneliness and increased health-related quality of life compared to active control. We will also explore whether health-related quality of life domains of social and emotional quality of life demonstrate the greatest improvement (compared to physical and environmental domains).
Our second aim examines mechanisms whereby volunteering reduces loneliness. Based on prior observational studies of volunteering, we hypothesize that increased purpose in life and increased social engagement (satisfaction with social activities) will account for reductions in loneliness.
Our third aim examines conditions under which volunteering is most effective at reducing loneliness, including ‘dose’ of volunteering (number of hours volunteered) and satisfaction with volunteer placements. Given that functional impairment impacts all proposed mechanisms, we will explore whether benefits of volunteering on loneliness are greatest for those with less functional impairment at baseline. We will also conduct exploratory analyses to examine sexual and gender minority (SGM; e.g., lesbian, gay, bisexual, transgender) identity as a potential moderator of primary outcomes, given significant health disparities faced by this group [42] and the potential for volunteering to function differently in this sub-group of lonely older adults [43]. This work is supported by an NIH Administrative Supplement to enhance recruitment and enrollment of diverse participants in aging research, specifically older SGM individuals.
Given that the COVID-19 pandemic began in Year 3, we will examine whether study participation pre- or post-COVID study modifications impacted findings.
2. Methods
Overview. This RCT is registered at clinicaltrials.gov (NCT03343483). All procedures were approved by the Research Subjects Review Board at the University of Rochester. Subjects participate in study interventions for up to one year, with repeated assessments over the course of the study (baseline, 3, 6, 9, 12 months). Those randomly assigned to volunteering receive the intervention at Lifespan as well as volunteer placements in the community or at home (during COVID restrictions) per standard Lifespan policy and procedures. Those randomly assigned to life review receive the intervention via the phone (for training) and their homes via email/mail. Enrollment is complete; data collection is ongoing while currently enrolled subjects complete interventions and follow-up assessments; analyses are planned for spring, 2023.
Participants. The target number of randomized subjects is 150 in each group. Inclusion and exclusion criteria appear in Table 1, including changes made for remote procedures for COVID precautions. Subjects are asked to refrain from initiating new long-term volunteer activities during their 12 months of involvement with the study. Mental/physical health diagnoses or symptoms are not cause for inclusion/exclusion, but are assessed over the course of the study. Subjects are required to be able to read and write in English (per requirements of study interventions).
Table 1.
Baseline variables to assess inclusion/exclusion criteria and characterize the sample and modifications due to COVID-19.
| Construct | Measure Name and Citation | Description & Psychometric Data | COVID modification |
|---|---|---|---|
| Demographics | Age, race, ethnicity, gender, sexual orientation, marital status, employment status, living alone, income, volunteering history | Demographic characteristics to characterize the sample, many of which are associated with loneliness in later life. | No change |
| Loneliness (inclusion) | 3-item UCLA Loneliness Short Form [57] | A score of 6 or above has been shown to predict mortality [6,57] and is required for inclusion. | No change |
| Cognitive impairment | Six item cognitive screener [58] | Two or more errors on phone screen indicate exclusion. | No change |
| Cognitive impairment | Montreal Cognitive Assessment (MoCA) [59] | Scores less than 22 (consistent with mild dementia) indicate exclusion. | Once remote administration was initiated, we removed the executive functioning items and administered the MoCA Blind version [60] for ease of remote administration, with subjects scoring less than 15 excluded |
| Alcohol misuse | The CAGE Questionnaire [61] | A score of 2 or above indicates exclusion. | No change |
| Psychosis | Psychosis in past month | Self-report of hallucinations and/or paranoid delusions in the past month. | No change |
| Transportation | Able to supply their own transportation or have alternate transportation services, including the city bus or services such as Liftline | Prior to COVID precautions, this was an RSVP and Lifespan requirement for volunteering. | This requirement was lifted due to expansion of remote volunteering opportunities that could be completed in the home. |
| Communication | Able to speak English and hear well-enough to speak on the phone. | These are required to participate as a volunteer. | No change |
| Volunteering | Currently serving as an RSVP volunteer | Exclusion criterion if a potential subject is already engaging in the study intervention. | No change |
| Social network | Lubben Social Network Scale [62] | Social network size and frequency of contact, designed for older adults and shown to be associated with premature mortality. | No change |
| Minority stress | Sexual Orientation Concealment Scale (SOCS) [63] | Questions designed to assess lesbian, gay, and bisexual (LGB) individual's active concealment of their sexual minority status; subjects who endorse LGB at baseline complete this form regarding their experiences in general as well as at follow-up if assigned to volunteering (regarding concealment during their volunteer activities). Baseline for those who answered as LGB on demographic form. | No change |
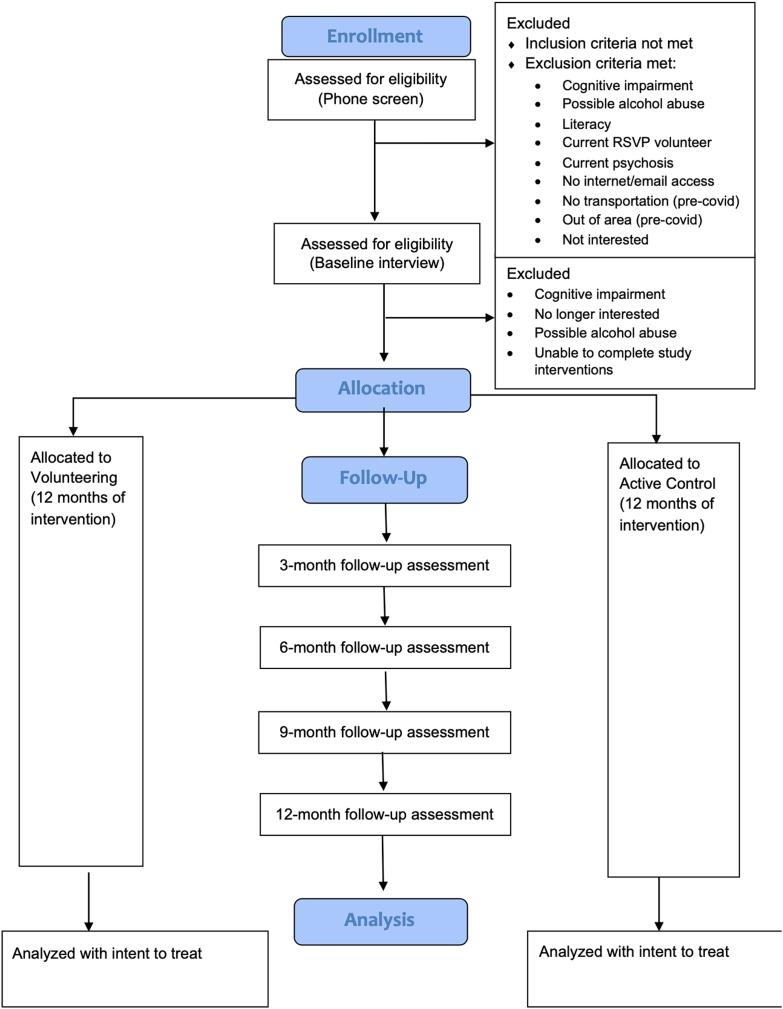
Procedures. Our primary recruitment strategy was mailing study brochures to adults 60 and older who received primary care within the UR Medicine healthcare system in the prior 2 years. Additional recruitment strategies included paid advertisements in local periodicals, flyers at various community sites, community presentations at senior centers and libraries, informational presentations to clinical providers likely to encounter lonely older adults (e.g., geriatricians, geriatric psychiatrists, neurologists) for direct referrals, and brochures distributed to Meals on Wheels clients. Potential subjects who contacted study staff completed a brief phone screen to assess eligibility and receive additional information about the study purpose and activities. Those who were eligible and interested were invited to schedule a baseline interview in the PI's laboratory at the University of Rochester or via Zoom/phone (during COVID restrictions). The baseline interview includes a structured protocol for assessing capacity for informed consent, followed by assessment of additional exclusion criteria and baseline characteristics (Fig. 1).
Fig. 1.
CONSORT diagram.
COVID-19 procedural modifications. Due to the COVID-19 pandemic, enrollment was paused in March 2020 until the University was allowed to resume research activities in April 2020. All study procedures were switched to remote. In-person study visits were changed to Zoom (HIPAA-compliant version) or phone. Study COVID restrictions have remained in place, with subject assessments remaining remote given that our subjects are older and thus more vulnerable to serious complications from COVID-19. While some potential subjects have declined participation due to the remote nature of assessments, that number is very small; study staff are available by phone to help subjects access email and learn to use Zoom.
Randomization. Subjects are randomized (using the REDCap randomization module) to receive either volunteering or control intervention. We used permuted blocked randomization with varying block lengths (unknown to PI and assessors). Neither assessors nor subjects are blind to condition. We have found that having the same assessor complete each assessment significantly improves retention.
Volunteering intervention. Subjects assigned to volunteering were linked with the RSVP program and follow their standard process for placement. Subjects began training at Lifespan within two weeks of randomization. The target expectation for volunteering is 4 times per month. Lifespan collects monthly timesheets, which include the number of hours and types of volunteer activities. RSVP provides a small reimbursement for travel to volunteers as needed for travel related to volunteering. The other component of the intervention is on-going training, volunteer support groups, and educational activities offered by Lifespan. These gatherings for volunteers serve to promote retention in the program, assist volunteers with any problems/issues that have arisen, and promote social connectedness among volunteers. The initial design for the study involved a single volunteer placement for all subjects that involved providing in-home companionship and respite care for older adults with dementia. However, acceptability of this placement was very low and potential subjects reported concerns about their capability to safely provide respite services for adults with more advanced dementia. In consultation with our community partner, Data and Safety Monitoring Committee, and with approval from our funder, the volunteering intervention was expanded to include the full range of volunteering placements available through RSVP, which significantly increased interest in the project. While some subjects chose to provide respite for adults with dementia, there is a diverse range of other volunteer opportunities, including volunteering at animal shelters, delivering for Meals on Wheels, helping at a food bank, driving older Veterans to appointments, mentoring and tutoring youth, and helping run educational and wellness programs (e.g., Tai Chi, Matter of Balance). The program also creates new placements for volunteers based on interests and capabilities. All placements are documented by Lifespan and research staff. To establish new RSVP placements, the volunteer coordinator establishes a Memorandum of Understanding regarding information sharing to best support volunteers (and act as a liaison and ombudsman if needed) and to document hours served for reporting purposes (and mileage reimbursement).
Volunteering COVID-19 modifications. Once study procedures switched to entirely remote (Year 3), volunteering activities were only completed in the home, such as friendly calling to other older adults, including those in long-term care settings experiencing significant isolation. In June 2020, the University IRB approved volunteering options returning to the community in addition to at home opportunities, when such opportunities were deemed safe by our community partner. Placements in the community were reviewed by RSVP and Lifespan staff and must have a documented COVID-19 safety plan in place before volunteers engage in volunteer opportunities. Before resuming these in-person activities, we consulted our Data Safety Monitoring Committee for consultation and approval. At the time of writing this paper, subjects are allowed to volunteer in the community if they prefer, or continue volunteering activities that can be completed at home (e.g., friendly calling) in line with RSVP practices of personalizing the volunteer experience to match preferences. Other safe remote options have included delivery of meals for Meals on Wheels (using physical distancing procedures) and projects for Lifespan and other agencies that involve graphic design, photography, or writing.
Control condition. Those subjects assigned to control complete a series of self-guided (with email/postal mail support) life review writing exercises over 12 months. The active control condition was chosen to control for (and minimize confounding by) potential non-specific effects of participating in a study intervention; expectancies about benefit; and starting a new cognitively engaging activity. This standardized and evidence based intervention is commonly used to reduce depression and promote well-being in later life; further, it was validated as a self-guided intervention to improve well-being [44]. To minimize the social nature of providing the intervention (i.e., minimizing confounding our conditions), the life review is largely self-guided, including replacing the counselor (and one-on-one sessions) with email/postal mail support and a self-help book [44]. Subjects complete two sections of the life review (with the self-help book) each month and send ‘assignments’ twice per month to the ‘Life Review Coach’ who responds with brief supportive comments to promote ongoing engagement.
Study variables. Outcome variables are described in Table 2. Our study has two primary outcomes, loneliness and quality of life. Loneliness is assessed at all time points (baseline, 3, 6, 9, and 12 months), while quality of life is assessed only at baseline and 12-months (as it is a lengthier assessment). Two secondary outcomes assess potential mechanisms whereby volunteering may reduce loneliness (social engagement and meaning/purpose in life). Given that few RCTs have been conducted with older adults to examine loneliness and there is a limited literature to guide selection of measures of social connection that are most sensitive to change, we also included two additional secondary outcomes that are similar to, but not redundant with, our primary loneliness scale (UCLA Loneliness Scale)—belonging (Interpersonal Needs Questionnaire) and perceived social isolation (PROMIS). Moderator variables include ‘dose’ of volunteering and satisfaction with volunteering, as well as functional impairment and proportion of study participation completed after COVID modifications were put in place. For exploratory analyses with sexual and gender minority identity (SGM), we assess SGM identity as well as one indicator of minority stress—concealment of one's SGM identity (Table 1). Finally, for all subjects, we conduct qualitative interviews to obtain perceptions of the benefits (and/or potential harms) of study interventions, including any impact aspects of subjects' identities may have had on their experiences (e.g., race, gender, sexuality, Veteran status).
Table 2.
Study variables.
| Measure Name and Citation | Description & Psychometric Data | ||
|---|---|---|---|
| Loneliness | Primary | UCLA Loneliness Scale, version 3 [64] | Self-report (20 items). Yields a continuous total score, with greater scores indicating greater loneliness (range 20–80). None of the items use the word ‘lonely’ to reduce under-reporting due to social desirability and stigma. It has demonstrated strong psychometric properties with older adult samples [64,65]. |
| Quality of life | Primary | World Health Organization Brief Quality of Life Scale (WHOQOL-Bref) [66]. | Self-report (26 items). Yields a continuous total score, with greater scores indicating greater quality of life (range 0–100). Scores for four domains (physical, psychological, social, and environmental) are also available; social and emotional quality of life are expected to improve most in our study. It has demonstrated strong psychometric properties [67]. |
| Social engagement | Secondary (mechanism) | PROMIS Satisfaction with Social Roles and Activities [68] | This computerized adaptive test (CAT) produces T scores with a mean of 50 and standard deviation of 10. Greater scores indicate greater satisfaction with social roles and activities. |
| Meaning & purpose | Secondary (mechanism) | Patient-Reported Outcomes Measurement Information System (PROMIS) Meaning and Purpose | This computerized adaptive test (CAT) produces T scores with a mean of 50 and standard deviation of 10. Greater scores indicate greater meaning and purpose. |
| Perceived social isolation | Secondary | PROMIS Social Isolation computerized adaptive test [69] | This computerized adaptive test (CAT) produces T scores with a mean of 50 and standard deviation of 10. Greater scores indicate greater isolation. |
| Belonging | Secondary | Interpersonal Needs Questionnaire, belonging subscale [70] | Self-report (9 items). Yields a continuous total score, with greater scores indicating greater belonging (range 0–18). It has demonstrated strong psychometric properties with older adults. |
| Volunteering quantity | Moderator | RSVP Volunteer Timesheet | Collected by the volunteer coordinator, this standard reporting form documents amount of time spent volunteering each month. |
| Volunteering quality | Moderator | Satisfaction with Volunteering Scale | This is a standard AmeriCorps Seniors program evaluation survey. |
| Functional impairment | Moderator | World Health Organization Disability Assessment Schedule (WHODAS) total score [71]. | Functional impairment across several domains, mobility, cognition, self-care, social, emotional. |
| Participation during COVID | Moderator | Proportion of study participation completed after COVID modifications were in place. | Calculated by randomization date and COVID procedural modifications start date of April 2020. |
| Experiences in study interventions | Exploratory | Qualitative interview | Open-ended feedback on study interventions. |
Sample size calculation. A power analysis was conducted to test treatment effects by the intent-to-treat (ITT) analysis for the primary outcomes. We assumed a conservative 20% attrition rate and a 0.3 within-subject correlation. A sample size of N = 300 (or N = 150 per treatment group) will allow us to detect a small effect size of 0.2 for loneliness, with 80% power based on a two-sided type I alpha = 0.05. The assumed within-subject correlation of 0.3 reflects the relatively long time lag between consecutive assessments. For Aim 2 examining mechanisms, the proposed sample size also has 80% power to detect 32% mediation effects for loneliness, a continuous outcome. If full mediation is not achieved for any of the mediators considered, 32% mediation effects are sufficiently large to be of clinical importance for the outcomes of interest.
3. Data analytic strategy
Descriptive statistics will summarize distributions of each outcome, with means and standard deviations for continuous outcomes and percent for categorical outcomes. Two-sample t tests (or the Mann-Whitney-Wilcoxon rank sum test) and Chi-square tests will be used to examine balance of treatment randomization for continuous (if distributions are highly skewed, highly skewed, especially with outliers) and categorical variables. We will examine the potential impact of COVID-19-related study modifications by computing the proportion of intervention time after COVID modifications were implemented.
Aim 1, the effect of volunteering on the co-primary outcomes of loneliness and quality of life (both continuous variables), will be tested using semiparametric weighted generalized estimating equations (WGEE) for longitudinal regression analysis. WGEE imposes no analytic model for the distribution of the response (dependent variable) and thus provides valid inference regardless of how the response variable is distributed. Moreover, it provides valid inference under the missing at random (MAR) mechanism, the most common in clinical research studies, if the missing data is correctly modeled [45]. These models use an Intent to Treat design, with all subjects randomized to either condition included in the analysis, regardless of their compliance to their assigned interventions, to ensure replicability of treatment effects in similar study populations. For Hypothesis 1a, loneliness will be the response variable, with condition, time and their interaction as the predictors, controlling for age and gender. We hypothesize that there will be an effect of condition on loneliness at all follow-up points indicating differing levels of loneliness in the direction: control > volunteering. If a significant difference exists (a significant time by condition interaction), appropriate linear contrasts will confirm the hypothesized directional effects (greater loneliness for the control group). For Hypothesis 1 b, the same analytic strategy will be used, but with quality of life as the response variable and anticipating greater quality of life in the volunteering condition. For both models, we will include a time-varying indictor to examine whether the intervention time once COVID modifications were implemented is associated with loneliness and quality of life. Moderation analyses for Aim 3 (functional impairment) will be conducted using the same analytic strategy.
Aim 2 examines mechanisms (mediation) whereby volunteering reduces loneliness and improves quality of life. This aim will be examined by structural equation models (SEM)46 47 to test the putative mediators of purpose in life and social engagement. If the outcome and mediator have highly skewed distributions, we will use semiparametric methods for more robust inference in these models as well as apply appropriate variable transformation to improve efficiency [47,48]. We will report standard goodness-of-fit measures—chi-square test, the comparative fit index (CFI), the index of Tucker and Lewis (TLI), and Root Mean Square Error of Approximation (RMSEA) [46,49,50]. Increases in social engagement (PROMIS Satisfaction with Social Roles & Activities) at 6 months is hypothesized to mediate the effect of intervention condition on decreased loneliness at 12 months. The SEM-based mediation models will be applied to test the hypothesis, with social engagement as the mediator, intervention condition as the predictor and loneliness as the outcome, controlling for age and gender. If the null of full mediation is rejected, we will estimate direct, indirect and total effects to assess the strength of mediation. The same analytic strategy will be used for Purpose in Life.
Aim 3 examines conditions under which volunteering may provide maximal benefit, including ‘dose’ (greater hours volunteering) and greater satisfaction with the intervention. Dose-response relationships (Aim 3) will be examined by structural mean models to supplement the ITT analysis, which provides intervention effects averaged over all subjects randomized to the intervention conditions. When intervention compliance (volunteering hours/satisfaction for subjects in the volunteering condition) demonstrates a dose-response relationship, as we hypothesize in Aim 3, complier average causal effects (CACE) will model and test such a dose-response relationship. CACE is a compliment to ITT analyses, which answers the question whether the intervention has any treatment effect for the study population as a whole regardless of compliance, rather than the question whether the intervention has any therapeutic value and if so, how the therapeutic effect changes with increased dose [51]. CACE provides different intervention effects for individuals depending on their levels of compliance, which can be quite informative, especially when there is large variability in intervention compliance and strong dose-response relationships. Since volunteering time is only required for the volunteering condition, standard statistical models cannot be used to perform CACE analysis. The CACE approach enables an estimate of the treatment effect at each level of “compliance” (i.e., amount of hours volunteered), without the need for a measure of compliance in the control group. In this way, we will be able to tell how well volunteering reduces loneliness at different “doses” of volunteering. If results regarding study participation during the pandemic suggest differential efficacy as a function of participation once COVID-related study modifications were put in place, we will also conduct a CACE analysis accordingly to examine ‘dose’ of volunteering pre-COVID (i.e., before volunteer opportunities were restricted). Given that the control condition was unchanged during the pandemic, this analysis may be best to detect potential effects of COVID-19 on study outcomes.
We will use the latest semi-parametric structural mean model (SMM) [[52], [53], [54]] based on the structural functional response models (SFRM) for our CACE analysis, which not only allows for continuous, but also multiple dose variables [[52], [53], [54]]. We are particularly interested in potential non-linear dose-response relationships so that we may determine optimal dose intervention whereby increased exposure (i.e., number of hours volunteered) becomes less worthwhile (in terms of reducing loneliness). We will apply the SFRM-based SMM to analyze dose-response relationships. We will first model dose using non-parametric methods such as LOWESS curves and then characterize the patterns using parametric methods for inference and improved efficiency. This allows us to capture detailed dose and response relationships and provide more interpretable findings.
Data and safety monitoring is overseen by a committee composed of individuals independent of the study as well as the PI and one Co–I; none are at a different institution given the low-risk nature of the study intervention; selection of a non-clinical population; and study design without blinding. Per the NIH Data Sharing Policy, de-identified data will be available to interested investigators under a data use agreement.
Timeline. Enrollment was completed in May 2022 and completion of follow-up assessments will continue through May 2023, with completion of primary outcome analyses soon thereafter.
4. Discussion
The COVID-19 pandemic and the need for physical distancing introduced loneliness into everyday conversation and powerfully demonstrated the deleterious effect of loneliness on health and well-being. However, unlike other countries where social and health services are more fully integrated, such as the UK's national strategy for addressing loneliness [55], in the U.S., fee-for-service payment models and the separate funding and functioning of health and human services disincentivize provision of non-medical services by health care providers and systems. The COVID pandemic further stretched the health care sector, making attention to social determinants less feasible. However, the pandemic also made clear that loneliness contributes powerfully to illness as well as utilization and cost of health services. Raised awareness of the adverse health consequences of loneliness may reinvigorate efforts to address the problem as a component of integrated health care [56].
In order to do so, the evidence-base on interventions for loneliness must be improved. This Stage III efficacy trial (NIH Stage Model) is designed to examine efficacy with the intervention provided as it is in the community, nationwide, to reduce the time from testing to dissemination and implementation with older adults who might benefit. This study design has both strengths and limitations that will impact findings and next steps. The need to tailor the volunteering activity to individual preferences is the foundation of the national RSVP model and was needed to promote acceptability of the project; while a single volunteer placement for all volunteers would have reduced heterogeneity in the intervention, such a restriction was both not feasible and not representative of volunteering programs available in the community. The RCT design increases internal validity, but introduces other challenges, including the fact that participating in a research study is itself a volunteer opportunity that provides ongoing social contact (potentially confounding conditions and attenuating effects). Our study was also impacted by the COVID-19 pandemic, including a pause in enrollment (though relatively brief), as well as changes in the types and variety of volunteering placements offered.
Older adults who report loneliness are less likely to actively seek out volunteering opportunities; if results support efficacy of volunteering for reducing loneliness and improving quality of life for older adults experiencing loneliness, dissemination and scaling up efforts may involve connecting primary care patients who are lonely with AmeriCorps Seniors through aging services agencies, which we have shown to be feasible in our companion study, The Senior Connection97 and enhancing interest in volunteering. National infrastructure for AmeriCorps Seniors ensures that volunteering is highly scalable. Existing infrastructure will make it possible to engage a large proportion of lonely older adults in volunteering. Future directions for research include examining cultural and other psychosocial determinants of loneliness that may impact willingness or ability to volunteer (e.g., history of psychological trauma), or that may require tailoring of activities (e.g., under-represented backgrounds or disabilities). Future work should examine health impacts of reducing loneliness to provide information on utilization and cost that is needed to support adoption of care and payment models that integrate assessment and treatment of loneliness into health care.
Authors’ contributions
KVO was the principal investigator and obtained funding. KVO, YC, XT, BC, SS, and GW designed the study. KVO oversaw its implementation and supervised the research assessments. JR directed the volunteering program at Lifespan and DP served as the volunteer coordinator and supervised volunteers and coordinated data collection on volunteer hours. AS and KVO developed the life review control condition materials. AB, EB, and AS helped with study set up and administration, development and implementation of COVID modifications, and development of recruitment and enrollment procedures. AB oversaw coordination with our community partner, Lifespan. In addition to KVO (first author), AB, AS, AVB, BC, XT, and YC were involved in writing the text. All authors reviewed and approved of the paper before submission.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The study was supported by a grant from the National Institute on Aging (R01AG054457, R01AG054457-02S1, Van Orden, PI). We wish to thank all members of the study team, the staff of Lifespan, the many agencies and clinicians who assisted in developing and implementing recruitment plans, and our study participants who generously gave their time and effort to study programs that can improve quality of life for older adults.
Footnotes
This research is supported by a grant from the National Institute on Aging (R01AG054457, R01AG054457-02S1).
References
- 1.Golden J., Conroy R.M., Bruce I., et al. Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. Int. J. Geriatr. Psychiatr. 2009;24(7):694–700. doi: 10.1002/gps.2181. [DOI] [PubMed] [Google Scholar]
- 2.Luo Y., Hawkley L.C., Waite L.J., Cacioppo J.T. Loneliness, health, and mortality in old age: a national longitudinal study. Soc. Sci. Med. 2012;74(6):907–914. doi: 10.1016/j.socscimed.2011.11.0283303190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawkley L.C., Thisted R.A., Masi C.M., Cacioppo J.T. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol. Aging. 2010;25(1):132–141. doi: 10.1037/a0017805.2841310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tomaka J., Thompson S., Palacios R. The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. J. Aging Health. 2006;18(3):359–384. doi: 10.1177/0898264305280993. 18/3/359 [pii] [DOI] [PubMed] [Google Scholar]
- 5.Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 6.Steptoe A., Shankar A., Demakakos P., Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc. Natl. Acad. Sci. U. S. A. 2013;110(15):5797–5801. doi: 10.1073/pnas.12196861103625264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perissinotto C.M., Stijacic Cenzer I., Covinsky K.E. Loneliness in older persons: a predictor of functional decline and death. Arch. Intern. Med. 2012:1–7. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wenger G.C., Burholt V. Changes in levels of social isolation and loneliness among older people in a rural area: a twenty-year longitudinal study. Can. J. Aging. 2004;23(2):115–127. doi: 10.1353/cja.2004.0028. http://www.ncbi.nlm.nih.gov/pubmed/15334812 [DOI] [PubMed] [Google Scholar]
- 9.AARP . 2010. Loneliness Among Older Adults: A National Survey of Adults 45+ [Google Scholar]
- 10.Charles S.T. Strength and vulnerability integration: a model of emotional well-being across adulthood. Psychol. Bull. 2010;136(6):1068–1091. doi: 10.1037/a0021232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baumeister R.F., Leary M.R. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol. Bull. 1995;117(3):497–529. doi: 10.1037/0033-2909.117.3.497. [DOI] [PubMed] [Google Scholar]
- 12.Cacioppo J.T., Cacioppo S., Boomsma D.I. Evolutionary mechanisms for loneliness. Cognit. Emot. 2014;28(1):3–21. doi: 10.1080/02699931.2013.837379PMC3855545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cacioppo S., Grippo A.J., London S., Goossens L., Cacioppo J.T. Loneliness: clinical import and interventions. Perspect. Psychol. Sci. 2015;10(2):238–249. doi: 10.1177/1745691615570616PMC4391342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen-Mansfield J., Hazan H., Lerman Y., Shalom V. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int. Psychogeriatr. 2015:1–20. doi: 10.1017/S1041610215001532. [DOI] [PubMed] [Google Scholar]
- 15.Hoogendijk E.O., Suanet B., Dent E., Deeg D.J., Aartsen M.J. Adverse effects of frailty on social functioning in older adults: results from the Longitudinal Aging Study Amsterdam. Maturitas. 2016;83:45–50. doi: 10.1016/j.maturitas.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 16.Theeke L.A. Sociodemographic and health-related risks for loneliness and outcome differences by loneliness status in a sample of U.S. older adults. Res. Gerontol. Nurs. 2010;3(2):113–125. doi: 10.3928/19404921-20091103-99. [DOI] [PubMed] [Google Scholar]
- 17.Qualter P., Vanhalst J., Harris R., et al. Loneliness across the life span. Perspect. Psychol. Sci. 2015;10(2):250–264. doi: 10.1177/1745691615568999. [DOI] [PubMed] [Google Scholar]
- 18.Aartsen M., Jylha M. Onset of loneliness in older adults: results of a 28 year prospective study. Eur. J. Ageing. 2011;8(1):31–38. doi: 10.1007/s10433-011-0175-7PMC3047676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masi C.M., Chen H.Y., Hawkley L.C., Cacioppo J.T. A meta-analysis of interventions to reduce loneliness. Pers. Soc. Psychol. Rev. 2011;15(3):219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hickin N., Kall A., Shafran R., Sutcliffe S., Manzotti G., Langan D. The effectiveness of psychological interventions for loneliness: a systematic review and meta-analysis. Clin. Psychol. Rev. 2021;88 doi: 10.1016/j.cpr.2021.102066. [DOI] [PubMed] [Google Scholar]
- 21.Sabir M., Wethington E., Breckman R., Meador R., Reid M.C., Pillemer K. A community-based participatory critique of social isolation intervention research for community-dwelling older adults. J. Appl. Gerontol. 2009;28(2):218–234. doi: 10.1177/0733464808326004PMC4142440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomas P.A. Is it better to give or to receive? Social support and the well-being of older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2010;65B(3):351–357. doi: 10.1093/geronb/gbp113. [DOI] [PubMed] [Google Scholar]
- 23.Hooyman N.R., Kawamoto K.Y., Kiyak H.A. Pearson; New York: 2015. Aging Matters: an Introduction to Social Gerontology. [Google Scholar]
- 24.Klein Ikkink K., Tilburg Tv. Broken ties: reciprocity and other factors affecting the termination of older adults' relationships. Soc. Network. 1999;21(2):131–146. doi: 10.1016/S0378-8733(99)00005-2. [DOI] [Google Scholar]
- 25.Okun M.A., Yeung E.W., Brown S. Volunteering by older adults and risk of mortality: a meta-analysis. Psychol. Aging. 2013;28(2):564–577. doi: 10.1037/a0031519. [DOI] [PubMed] [Google Scholar]
- 26.Jenkinson C.E., Dickens A.P., Jones K., et al. Is volunteering a public health intervention? A systematic review and meta-analysis of the health and survival of volunteers. BMC Publ. Health. 2013;13:773. doi: 10.1186/1471-2458-13-7733766013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderson N.D., Damianakis T., Kroger E., et al. The benefits associated with volunteering among seniors: a critical review and recommendations for future research. Psychol. Bull. 2014 doi: 10.1037/a0037610. [DOI] [PubMed] [Google Scholar]
- 28.Fried L.P., Carlson M.C., Freedman M., et al. A social model for health promotion for an aging population: initial evidence on the Experience Corps model. J. Urban Health. 2004;81(1):64–78. doi: 10.1093/jurban/jth0943456134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pilkington P.D., Windsor T.D., Crisp D.A. Volunteering and subjective well-being in midlife and older adults: the role of supportive social networks. J. Gerontol. B Psychol. Sci. Soc. Sci. 2012;67(2):249–260. doi: 10.1093/Geronb/Gbr154. [DOI] [PubMed] [Google Scholar]
- 30.Harris A.H., Thoresen C.E. Volunteering is associated with delayed mortality in older people: analysis of the longitudinal study of aging. J. Health Psychol. 2005;10(6):739–752. doi: 10.1177/1359105305057310. Published 2005/09/24. [DOI] [PubMed] [Google Scholar]
- 31.Morrow-Howell N., Hong S.-I., McCrary S., Blinne W. Changes in activity among older volunteers. Res. Aging. 2012;34(2) doi: 10.1177/0164027511419371. [DOI] [Google Scholar]
- 32.Morrow-Howell N., Kinnevy S., Mann M. The perceived benefits of participating in volunteer and educational activities. J. Gerontol. Soc. Work. 1999;32(2):65–80. doi: 10.1300/J083v32n02_06. [DOI] [Google Scholar]
- 33.Rook K.S., Sorkin D.H. Fostering social ties through a volunteer role: implications for older-adults' psychological health. Int. J. Aging Hum. Dev. 2003;57(4):313–337. doi: 10.2190/NBBN-EU3H-4Q1N-UXHR. http://www.ncbi.nlm.nih.gov/pubmed/15195981 [DOI] [PubMed] [Google Scholar]
- 34.Shmotkin D., Blumstein T., Modan B. Beyond keeping active: concomitants of being a volunteer in old-old age. Psychol. Aging. 2003;18(3):602–607. doi: 10.1037/0882-7974.18.3.602. [DOI] [PubMed] [Google Scholar]
- 35.Fried L.P., Carlson M.C., McGill S., et al. Experience Corps: a dual trial to promote the health of older adults and children's academic success. Contemp. Clin. Trials. 2013;36(1):1–13. doi: 10.1016/j.cct.2013.05.0034112377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Varma V.R., Tan E.J., Gross A.L., et al. Effect of community volunteering on physical activity: a randomized controlled trial. Am. J. Prev. Med. 2015 doi: 10.1016/j.amepre.2015.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carlson M.C., Kuo J.H., Chuang Y.F., et al. Impact of the baltimore experience corps trial on cortical and hippocampal volumes. Alzheimer's Dementia : the journal of the Alzheimer's Association. 2015 doi: 10.1016/j.jalz.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morrow-Howell N., Hong S.I., McCrary S., Blinne W. Changes in activity among older volunteers. Res. Aging. 2012;34(2):174–196. doi: 10.1177/0164027511419371. [DOI] [Google Scholar]
- 39.Parisi J.M., Kuo J., Rebok G.W., et al. Increases in lifestyle activities as a result of experience Corps(R) participation. J. Urban Health : Bull. N. Y. Acad. Med. 2015;92(1):55–66. doi: 10.1007/s11524-014-9918-zPMC4338117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jiang D., Warner L.M., Chong A.M., Li T., Wolff J.K., Chou K.L. Benefits of volunteering on psychological well-being in older adulthood: evidence from a randomized controlled trial. Aging Ment. Health. 2021;25(4):641–649. doi: 10.1080/13607863.2020.1711862. [DOI] [PubMed] [Google Scholar]
- 41.Onken L.S., Carroll K.M., Shoham V., Cuthbert B.N., Riddle M. Reenvisioning clinical science: unifying the discipline to improve the public health. Clin. Psychol. Sci. 2014;2(1):22–34. doi: 10.1177/2167702613497932PMC4374633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Institute of Medicine . National Academies Press; Washington, D.C.: 2011. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. [PubMed] [Google Scholar]
- 43.Lyons A., Alba B., Waling A., et al. Volunteering among older lesbian and gay adults: associations with mental, physical and social well-being. J. Aging Health. 2021;33(1–2):3–13. doi: 10.1177/0898264320952910. [DOI] [PubMed] [Google Scholar]
- 44.Lamers S.M., Bohlmeijer E.T., Korte J., Westerhof G.J. The efficacy of life-review as online-guided self-help for adults: a randomized trial. J. Gerontol. B Psychol. Sci. Soc. Sci. 2015;70(1):24–34. doi: 10.1093/geronb/gbu030. [DOI] [PubMed] [Google Scholar]
- 45.Tang W., He H., Tu X.M. Chapman & Hall/CRC; New York: 2012. Applied Categorical and Count Data Analysis. [Google Scholar]
- 46.Bollen K.A. John Wiley & Sons; Oxford, England: 1989. Structural Equations with Latent Variables. Wiley Series in Probability and Mathematical Statistics. Applied Probability and Statistics Section. Structural Equations with Latent Variables. Xiv; p. 514. England. [Google Scholar]
- 47.Gunzler D., Tang W., Lu N., Wu P., Tu X.M. A class of distribution-free models for longitudinal mediation analysis. Psychometrika. 2014;79(4):543–568. doi: 10.1007/S11336-013-9355-Z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Olsson U.H., Foss T., Troye S.V., Howell R.D. The performance of ML, GLS, and WLS estimation in structural equation modeling under conditions of misspecification and nonnormality. Struct. Equ. Model. 2000;7(4):557–595. doi: 10.1207/S15328007sem0704_3. [DOI] [Google Scholar]
- 49.Jaccard J., Wan C.K. No. vols. 07–114. Sage Publications, Inc; US; Thousand Oaks, CA: 1996. LISREL Approaches to Interaction Effects in Multiple Regression. (Quantitative Applications in the Social Sciences). [Google Scholar]
- 50.Kline R.B. Guilford; NY: 2004. Principles and Practice of Structural Equation Modeling. [Google Scholar]
- 51.Shrier I., Steele R.J., Verhagen E., Herbert R., Riddell C.A., Kaufman J.S. Beyond intention to treat: what is the right question? Clin. Trials. 2014;11(1):28–37. doi: 10.1177/1740774513504151. [DOI] [PubMed] [Google Scholar]
- 52.Robins J.M. Correcting for noncompliance in randomized trials using structural nested mean models. Commun. Stat. 1994;23:2379–2412. [Google Scholar]
- 53.Wu P., Gunzler D., Lu N., Chen T., Wymen P., Tu X.M. Causal inference for community-based multi-layered intervention study. Stat. Med. 2014;33(22):3905–3918. doi: 10.1002/sim.6199PMC4156555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Frangakis C.E., Rubin D.B. Principal stratification in causal inference. Biometrics. 2002;58(1):21–29. doi: 10.1111/j.0006-341X.2002.00021.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hm Government . 2019. A Connected Society: A Strategy for Tackling Loneliness. London, UK. [Google Scholar]
- 56.Conwell Y. Suicide later in life: challenges and priorities for prevention. Am. J. Prev. Med. 2014;47(3S2):S244–S250. doi: 10.1016/j.amepre.2014.05.040. [DOI] [PubMed] [Google Scholar]
- 57.Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res. Aging. 2004;26(6):655–672. doi: 10.1177/01640275042685742394670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Callahan C.M., Unverzagt F.W., Hui S.L., Perkins A.J., Hendrie H.C. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med. Care. 2002;40(9):771–781. doi: 10.1097/01.MLR.0000024610.33213.C8. [DOI] [PubMed] [Google Scholar]
- 59.Nasreddine Z.S., Phillips N.A., Bedirian V., et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 60.Wittich W., Phillips N., Nasreddine Z.S., Chertkow H. Sensitivity and specificity of the montreal cognitive assessment modified for individuals who are visually impaired. J. Vis. Impair. Blind. (JVIB) 2010;104(6):360–368. doi: 10.1177/0145482X1010400606. [DOI] [Google Scholar]
- 61.Olson K., Smyth J.D., Wang Y., Pearson J.E. The self-assessed literacy index: reliability and validity. Soc. Sci. Res. 2011;40(5):1465–1476. doi: 10.1016/j.ssresearch.2011.05.002. [DOI] [Google Scholar]
- 62.Lubben J., Blozik E., Gillmann G., et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontol. 2006;46(4):503–513. doi: 10.1093/geront/46.4.503. http://www.ncbi.nlm.nih.gov/pubmed/16921004 [DOI] [PubMed] [Google Scholar]
- 63.Jackson S.D., Mohr J.J. Educational Publishing Foundation; 2016. Conceptualizing the Closet: Differentiating Stigma Concealment and Nondisclosure Processes; pp. 80–92. [Google Scholar]
- 64.Russell D.W. UCLA loneliness scale (version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 65.Cacioppo J.T., Hawkley L.C., Thisted R.A. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol. Aging. 2010;25(2):453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Skevington S.M., Lotfy M., O'Connell K.A., Group W. The World Health Organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual. Life Res. 2004;13(2):299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- 67.World Health Organization Development of the world health organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol. Med. 1998;28(3):551–558. doi: 10.1017/s0033291798006667. http://www.ncbi.nlm.nih.gov/pubmed/9626712. Published 1998/06/17 [DOI] [PubMed] [Google Scholar]
- 68.Hahn E.A., Devellis R.F., Bode R.K., et al. Measuring social health in the patient-reported outcomes measurement information system (PROMIS): item bank development and testing. Qual. Life Res. 2010;19(7):1035–1044. doi: 10.1007/s11136-010-9654-0PMC3138729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Karayannis N.V., Baumann I., Sturgeon J.A., Melloh M., Mackey S.C. The impact of social isolation on pain interference: a longitudinal study. Ann. Behav. Med. 2019;53(1):65–74. doi: 10.1093/abm/kay017PMC6301311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Parkhurst K.A., Conwell Y., Van Orden K.A. The interpersonal needs questionnaire with a shortened response scale for oral administration with older adults. Aging Ment. Health. 2016;20(3):277–283. doi: 10.1080/13607863.2014.1003288PMC4520787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ustun T.B., Chatterji S., Kostanjsek N., et al. Developing the world health organization disability assessment schedule 2.0. Bull. World Health Organ. 2010;88(11):815–823. doi: 10.2471/BLT.09.0672312971503. [DOI] [PMC free article] [PubMed] [Google Scholar]