ABSTRACT
Background:
For many patients suffering from COVID-19, Emergency Departments (ED) facilitate the first contact with clinicians. There is a high rate of psychiatric symptoms in COVID-19 survivors, including anxiety, depression, fatigue and sleep disturbance, which persist months after the acute phase.
Aims:
To investigate if COVID-19 patients discharged from ED have a higher prevalence of mental health symptoms than those admitted.
In addition, this study will investigate if discharged ED patients who now require COVID-19 follow-up with the respiratory team had a higher prevalence of mental health symptoms than admitted patients requiring follow-up.
Methods:
This was a retrospective cohort study (n = 472) with the PHQ2 and GAD-2 scoring systems to quantify current anxiety and depression symptoms via a telephone consultation.
Results:
The PHQ-2 and GAD-2 scores were significantly higher for discharged ED patients than the admitted patients. There was a higher proportion of females with a positive PHQ2 or GAD-2 score. Of the patients requiring respiratory follow-up, discharged ED patients were more likely to have a positive PHQ-2 or GAD-2 score than those admitted.
Conclusions:
Clinicians should maintain a low threshold for referring patients with psychiatric complaints post-COVID alongside respiratory symptoms irrespective of admission. It is imperative that available psychological services, crisis lines and other avenues of support post-COVID-19 are signposted to patients before discharge to facilitate earlier intervention.
Introduction
As the gatekeepers of the hospital, Emergency Physicians must quickly determine which patients require admission. Although patients may not require immediate admission, they may require further clinical input. As healthcare systems begin to understand the importance of early clinical intervention, ED is primly positioned to aid in this transition. The novel coronavirus, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), causing the disease Coronavirus 2019 (COVID-19) was first identified in December 2019 in Wuhan, China and has since spread across the world. Following the SARS epidemic, caused by another coronavirus, 25.6% of survivors had Post Traumatic Stress Disorder (PTSD), and 15.6% had depressive disorders.1 As the first and second wave of COVID-19 recedes, it is imperative to anticipate an increase in mental illness related to the infection and the nationwide lockdown measures and prepare mental health services for the added burden they will face.
Early research has indicated that those with a milder form of COVID-19 had a greater frequency of depressive symptoms than those with a critical form of the disease2,3. Furthermore, there is an inverse correlation between the length of stay amongst admitted patients and symptoms of depression at three months post-discharge4. Discharged COVID-19 patients, by definition, should have a milder form of the disease, and it is, therefore possible that these patients have a more significant psychiatric burden than those admitted. Specialist funding has been allocated for COVID-19 survivors, with patients describing persisting symptoms and high rates of anxiety, depression, fatigue, and sleep disturbance3. Guidelines are beginning to emerge for the management of these patients, with General Practitioners expected to make many of the referrals5.
The ED is often the first clinical contact for COVID-19 patients and can, therefore, start a holistic COVID-19 pathway facilitating early clinical intervention. The British Thoracic Society (BTS) released a guideline in May 2020 recommending that clinicians undertake a ‘Post-COVID-19 holistic assessment’ of patient needs6. Following the publication of the BTS guidelines, we rapidly established a follow-up pathway that included screening for psychological issues. In this study, we will explore whether those attending ED and being discharged had higher rates of mental health symptoms than patients admitted. In addition, this study will investigate if discharged ED patients who now require COVID-19 follow-up with the respiratory team had a higher prevalence of mental health symptoms than admitted patients.
Methods
This retrospective cohort study investigated the proportion of patients suffering from anxiety and depressive symptoms in patients with confirmed or suspected COVID-19 infection presenting to our London ED during March, April and May 2020. Our study compared the proportion of patients with anxiety or depressive symptoms between those admitted and those discharged without admission from ED.
Participants
During the early stages of COVID-19 in the United Kingdom, many patients were not tested, and false negatives were commonplace. Therefore, in agreement with the literature, a positive COVID-19 test was not a prerequisite for diagnosis7. Criteria for inclusion were therefore as follows: all patients with proven or suspected COVID-19 managed in the Intensive Care Unit (ICU) or with Non-Invasive Ventilation (NIV), any patient coded as “COVID-19” in the hospital’s patient record system and all patients with a chest X-ray that identified COVID-19.
Screening
Sixteen doctors of similar grade telephoned patients and screened patients per BTS guidance to determine if a respiratory review was required. The criteria are detailed in Table 1. In addition, clinicians screened for mental health symptoms. Staff were told to keep broadly to a defined script so that this screening programme could be performed by non-clinical staff in the future whilst simultaneously minimising variability. We used the Patient Health Questionnaire-2 (PHQ-2) score as a screening tool for depression and the Generalised Anxiety Disorder-2 (GAD-2) tool to assess anxiety symptoms. Although these tools cannot be used for diagnostic purposes, their high specificity and sensitivity could permit use in the Emergency Department to identify at-risk patients who can be signposted to appropriate avenues of support8.
Table 1.
Criteria for follow-up divided into urgent and non-urgent pathways.
| Patients for immediate follow up: Chest X-ray and inflammatory markers to influence further action. | Patients for non-urgent follow up: Chest X-ray within 12 weeks of discharge. |
|---|---|
| • Critical care input or non-invasive ventilation required (Irrespective of current symptoms) • MRC breathlessness score decrease ≥2 • Ongoing pneumonitis symptoms concerning clinician |
• All patients with changes on CXR raising suspicion of covid-19 • All patients that required oxygen therapy ≥4L • Patients that had high clinical suspicion of COVID Infection, now recovering WITH mild ongoing symptoms of pneumonitis |
Follow-up
All patients with a positive PHQ-2 or GAD-2 were directed to IAPT (Improving Access to Psychological Therapies); however, at present, no local, trust, regional or national clinical guidance exists on managing new or worsening mental health symptoms under COVID-19. Patients were discussed on a case-by-case basis when IAPT was insufficient or appropriate.
Statistics
A chi-square test of independence was used to compare our patient outcome groups with the p-value set to <0.05 for a result to be considered significant.
Ethics
The telephone screening discussed in this report is part of an ongoing post-COVID-19 follow-up pathway. This pathway aims to identify, screen and refer patients with confirmed or suspected COVID-19 infection for appropriate follow-up. All data was routinely collected as part of that process, and ethical approval was not required. All patients consented verbally to undertake the screening questionnaire.
Results
Age and Sex
The Mean age of those admitted was sixty-three, whilst the mean age of those discharged was forty-six. Of the discharged patients, 52% were female, and 48% were male, whilst the admitted had a higher proportion of males (57%) than females (43%).
PHQ-2
Four hundred seventy-two patients answered the PHQ-2 screening questions correctly, of which 15% were positive. A significantly greater number of positive PHQ-2 scores was observed in discharged ED patients at 21% compared to admitted patients at 12% (p=.0177). In addition, 32% of the discharged ED patients who required respiratory follow-up had a positive PHQ-2 compared to 11% of the admitted patients. In the discharged patient group with a positive PHQ-2 score, 63% were female and 37% were male, whilst in the admitted group, 58% were female and 42% were male.
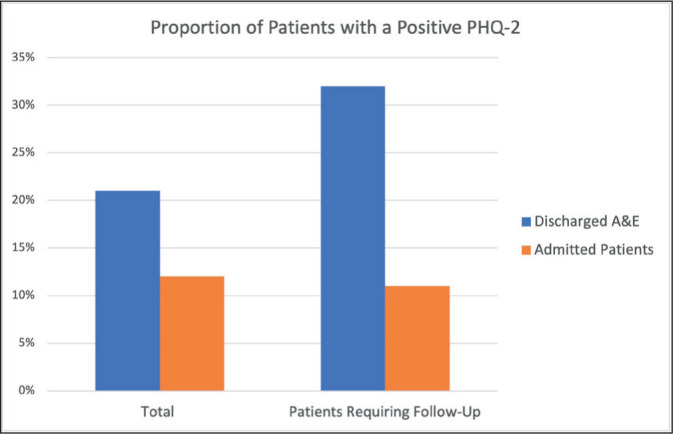
GRAPH 1
GAD-2
Similarly, we determined the GAD-2 score of 465 patients, of which 13% were positive. A significantly greater number of positive GAD-2 scores were observed in discharged ED patients at 17% compared to admitted patients at 10% (p = .0295). In addition, 22% of the discharged ED patients who required respiratory follow-up had a positive GAD-2 compared to 9% of the admitted patients. In the discharged patient group with a positive GAD-2 score, 61% were female and 39% male, while 60% were female and 40% male in the admitted group.
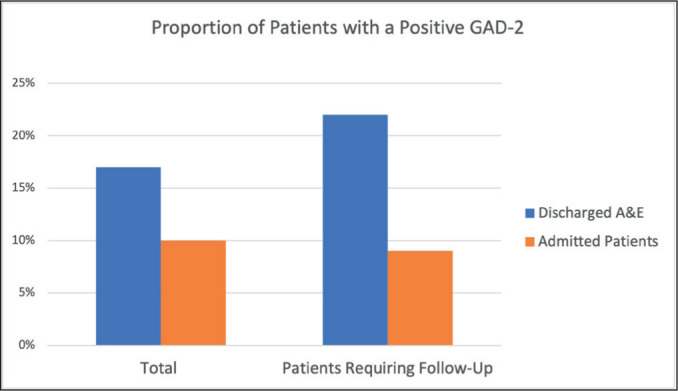
GRAPH 2
Discussion
To our knowledge, this is the first comparison of post-COVID-19 GAD-2 and PHQ-2 scores between discharged ED patients and those admitted. Although unique to COVID-19, it has been previously established that ED attendance is higher for patients with pre-existing mental health conditions9. Our study will likely further support the idea that mental health continues to be a significant challenge for ED clinicians.
However, it surprised the team that patients requiring a respiratory review following COVID-19 infection had higher PHQ-2 and GAD-2 scores, which is significantly greater amongst the discharged ED patients. It is uncertain why discharged ED patients requiring follow-up were significantly more likely to have positive PHQ-2 and GAD-2 scores than the admitted patients. However, this study may simply identify the “worried well”, and this uncertainty remains without baseline PHQ-2 and GAD-2 scores before infection.
Although the severity of COVID-19 infection doesn’t correlate with the development of psychiatric symptoms, the literature suggests sex and previous psychiatric history as the principal risk factors with a possible influence by age3 an increasing proportion of individuals have reported the persistence and/or new onset of symptoms which collectively have been identified as post-COVID-19 syndrome by the National Institute for Health and Care Excellence. Although depressive symptoms in the acute phase of COVID-19 have been well characterized, the frequency of depression following recovery of the acute phase remains unknown. Herein, we sought to determine the frequency of depressive symptoms and clinically-significant depression more than 12 weeks following SARS-CoV-2 infection. A systematic search of PubMed, Ovid Medline and Google Scholar for studies published between January 1, 2020 and June 5, 2021 was conducted. Frequency and factors associated with depression in post-COVID-19 syndrome were recorded and qualitatively assessed through narrative synthesis. Methodological quality and risk of bias was assessed using a modified version of the Newcastle-Ottawa Scale (NOS. Unfortunately, our study did not include data on previous psychiatric history. Although 52% of discharged patients were female, 65% of those with a positive PHQ-2 score and 60% with a positive GAD-2 were female. Therefore, our data supports the literature on the female gender being a risk factor for developing psychiatric symptoms post Covid-19 infection. ED physicians should be mindful of these risk factors when considering the need for onward referral. However, literature investigating outcomes after COVID-19 infection continues to be limited by difficulty comparing data against non-COVID-19 patients3 and as a retrospective cohort study this work is no different. It remains imperative that further research includes or investigates this and reduces the risk of confounding factors. Longitudinal, prospective studies are required before firmer conclusions can be drawn.
Our team has now integrated mental health screening into our COVID-19 follow-up, as those with mental health symptomatology may be at greater risk in light of this surprising data. We were fortunate enough to have the capacity to phone all our COVID-19 patients as part of our follow-up. Available services and other avenues of support must be appropriately signposted to patients before discharge. Increasingly clinicians and politicians alike are beginning to understand how early intervention, or better yet, preventative medicine can decelerate the rise in ED attendance. COVID-19 is not independent of this; however, ED can now dovetail with this earlier interventional strategy by providing a holistic COVID-19 follow-up and referrals where indicated or signposting available avenues of support.
Footnotes
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31(4):318–26. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Den Borst B, Peters JB, Brink M, Schoon Y, Bleeker-Rovers CP, Schers H, et al. Comprehensive health assessment 3 months after recovery from acute coronavirus disease 2019 (COVID-19) Clin Infect Dis. 2021;73(5):E1089–98. doi: 10.1093/cid/ciaa1750.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Renaud-Charest O, Lui LM, Eskander S, Ceban F, Ho R, Di Vincenzo JD, et al. Onset and frequency of depression in post-COVID-19 syndrome: A systematic review. J Psychiatr Res. 2021;144:129–37. doi: 10.1016/j.jpsychires.2021.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mazza MG, Palladini M, De Lorenzo R, Magnaghi C, Poletti S, Furlan R, et al. Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: Effect of inflammatory biomarkers at three-monthfollow-up.[Internet] BrainBehavImmun. 2021;194:138–47. doi: 10.1016/j.bbi.2021.02.021. [cited 2022 Jun 26] Available from: https://pubmed.ncbi.nlm.nih.gov/33639239/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NICE Guideline [NG188] London: National Institute for Health and Care Excellence; 2021. COVID-19 rapid guideline: managing the long-term effects of COVID-19 [Internet] [cited 2022 Jun 26] Available from: https://www.nice.org.uk/guidance/ng188/chapter/Recommendations. [Google Scholar]
- 6.British Thoracic Society. British Thoracic Society guidance on respiratoryfollow up of patients with a clinico-radiological diagnosis of COVID-19 Pneumonia [Internet] 2020. May 11, [cited 2020 Jun 21] Available from: Available from: https://www.brit-thoracic.org.uk/about-us/covid-19-information-for-the-respiratory-community/
- 7.Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell AJ, Yadegarfar M, Gill J, Stubbs B. Case finding and screening clinical utility of the Patient Health Questionnaire (PHQ-9 and PHQ-2) for depression in primary care: a diagnostic meta-analysis of 40 studies. BJPsych Open. 2016;2(2):127–38. doi: 10.1192/bjpo.bp.115.001685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saini P, McIntyre J, Corcoran R, Daras K, Giebel C, Fuller E, et al. Predictors of emergency department and GP use among patients with mental health conditions: a public health survey. Br J Gen Pract. 2019;70(690):E1–8. doi: 10.3399/bjgp19X707093.. [DOI] [PMC free article] [PubMed] [Google Scholar]


