Abstract
Background
Discharge to acute rehabilitation is strongly correlated with functional recovery after traumatic injury, including spinal cord injury (SCI). However, services such as acute care rehabilitation and Skilled Nursing Facilities (SNF) are expensive. Our objective was to understand if high-cost, resource-intensive post-discharge rehabilitation or alternative care facilities are utilized at disparate rates across socioeconomic groups after SCI.
Methods
We performed a cohort analysis using the National Trauma Data Bank® tabulated from 2012-2016. Eligible patients had a diagnosis of cervical or thoracic spine fracture with spinal cord injury (SCI) and were treated surgically. We evaluated associations of sociodemographic and psychosocial variables with non-home discharge (e.g., discharge to SNF, other healthcare facility, or intermediate care facility) via multivariable logistic regression while correcting for injury severity and hospital characteristics.
Results
We identified 3933 eligible patients. Patients who were older, male (OR=1.29 95% Confidence Interval [1.07-1.56], p=.007), insured by Medicare (OR=1.45 [1.08-1.96], p=.015), diagnosed with a major psychiatric disorder (OR=1.40 [1.03-1.90], p=.034), had a higher Injury Severity Score (OR=5.21 [2.96-9.18], p<.001) or a lower Glasgow Coma Score (3–8 points, OR=2.78 [1.81-4.27], p<.001) had a higher chance of a non-home discharge. The only sociodemographic variable associated with lower likelihood of utilizing additional healthcare facilities following discharge was uninsured status (OR=0.47 [0.37-0.60], p<.001).
Conclusions
Uninsured patients are less likely to be discharged to acute rehabilitation or alternative healthcare facilities following surgical management of SCI. High out-of-pocket costs for uninsured patients in the United States may deter utilization of these services.
Keywords: Discharge disposition, Insurance status, Healthcare utilization, Socioeconomic, Spinal cord injury, Trauma
Background
Each year, 12,000 patients experience traumatic spinal cord injury (SCI) in the United States [1]. SCI is most commonly caused by motor vehicle accidents, sports injuries, work-related accidents, and falls [2]. Traumatic SCIs are life changing events for patients and their families and weigh heavily on the economy of United States healthcare system. SCIs frequently lead to chronic disability resulting in long-term social and financial difficulties for patients [3]. Prior studies have estimated that the mean average lifetime cost per SCI is roughly $1.2 million [4]. A significant portion of this cost is tied to the rehabilitation for patients following discharge from the hospital [1].
Discharge to acute rehabilitation is strongly correlated with functional recovery after traumatic injury, including SCI. Prior literature has shown that access to rehabilitation following SCI can result in improvements in outcomes and higher rates of patient return to work and rate of economic self-sufficiency [5]. Early rehabilitation following surgical decompression and/or fusion is imperative to prevent joint contractures, loss of muscle strength, and improve respiratory and gastrointestinal function [6], [7], [8]. Increased time between injury and rehabilitation is associated with worse long-term quality of life and decreased odds of functional independence [1]. Additionally, acute rehabilitation provides patient education to avoid costly complications of spinal cord injury such as urinary tract infections, pneumonia, and pressure ulcers [9], [10], [11].
Services such as acute rehabilitation and care in skilled nursing facilities (SNF) are remarkably expensive. For example, mean charges for inpatient rehabilitation are about $20,000 for an average length of stay of 46 days [12] While insurers cover some of these costs, patients often are obligated to pay a portion of their expenses through cost sharing [13]. Prior literature has revealed that patients with governmental forms of insurance (e.g., Medicare or Medicaid) are referred to rehabilitation 55% of the time, while patients with private insurance are referred to rehabilitation services 84.6% of the time, despite both populations having similar injury severity [14].
Disparate utilization of healthcare resources based on sociodemographic characteristics have been observed across other specialties as well [15], [16], [17], [18]. However, there remains a paucity of literature on how discharge dispositions and rehabilitation resources may be utilized following traumatic SCI with respect to these variables. We hypothesized that non-home discharge to high-cost, high-resource healthcare facilities occur at disparate rates between socioeconomic groups following traumatic spine fracture in the United States.
Methods
We performed a cohort analysis of the National Trauma Data Bank® (NTDB) from 2012–2016. The NTDB is supported by the American College of Surgeons (ACS) Committee on Trauma and is a publicly available dataset [19]. The present analysis is exempt from Institutional Review Board (IRB) review. Patient consent was not required in accordance with local IRB procedures and there is no protected health information herein. This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Patient selection
Patients greater than or equal to 16 years of age who presented to an ACS Level I or II trauma center emergency department (ED) with any traumatic cervical or thoracic spine fractures with concurrent SCI, and who were treated with surgical management, were included in the present study. International Classification of Diseases (ICD)-9 CM procedure codes described by Daly et al. (2016) were applied for the present study [20]. Specifically, the presence of a fracture in the cervical or thoracic spine, associated with SCI, were identified using cervical spine code sets 806.0x and 806.1x, and thoracic spine code sets 806.2x and 806.3x. Given that our study aim was to identify factors that predict acute to post-acute care, eligible patients were excluded if they were dead on arrival or died in the ED; expired during their admission; were discharged to hospice or left against medical advice. Patients were also excluded if they presented with a major injury to the head, thorax, or abdomen [Abbreviated Injury Scale (AIS) severity ≥3]; or major polytrauma [Injury Severity Score (ISS) ≥27] or if they did not have sufficient baseline covariates necessary for inclusion in multivariate analysis.
Outcome measures
The primary outcome measure was non-home discharge disposition, including discharge to another healthcare facility, SNF, or acute rehabilitation center. The NTDB defines home discharge disposition as return to the patient's current place of residence with or without at-home services. All other discharge dispositions were coded as non-home [21].
Patient covariates
We assessed sociodemographic, psychosocial, injury-specific, and hospital-specific covariates in our analysis. Sociodemographic variables included age, gender, recorded race, and insurance status. Patients were classified as Black if they identified as Black, regardless of Hispanic ethnicity. Other patients listed as Hispanic were placed in the Hispanic group. Additional racial minority groups, such as Asian and Indian American, were excluded due to reasonably low proportional representation in the NTDB (<0.5%). Patients were designated into one of four insurance groups. These included private, Medicare, Medicaid, or uninsured. Insurance status was aggregated into private insurance (Blue Cross/Blue Shield, commercial insurance, workers compensation, other government, no fault automobile), Medicare, Medicaid, and uninsured (self-pay, no charge). Psychosocial covariates included previous diagnosis of a major psychiatric disorder, alcohol use disorder (AUD), or substance use disorder (SUD). We also assessed injury specific variables including mechanism of injury, injury intent, type of injury, injury severity, fracture location, and presenting Glasgow Coma Scale (GCS) in the ED. Injury severity was assessed using the facility-reported ISS. Fracture location is grouped as cervical, thoracic, or cervicothoracic (defined as ≥1 cervical and ≥1 thoracic vertebral fractures) based on the ICD codes previously described above. Hospital-specific variables included admitting hospital teaching status, non-profit status, trauma level, and geographic region.
Statistical analysis
We first analyzed baseline covariates between the cohorts of patients who did or did not have a non-home discharge using bivariate statistics (Pearson χ2 test) to identify significant differences between the groups. A p-value of <.05 was considered significant. Univariate logistic regression was then performed individually for all covariates and the outcome variable (non-home discharge) to determine independent association of each covariate. From the univariate analysis, covariates were then selected for inclusion in the multivariate logistic regression model. To avoid overfitting, statistical variable selection methods were not employed. An area under the receiver operating characteristic curve (AUC) value was computed for the multivariate model to assess overall predictive value. Stata statistical software version 17 (StataCorp LP, College Station, Texas) and R version 4.1.1 (R Foundation for Statistical Computing, Vienna, Austria) were used for data management, statistical analysis, and figure generation.
Results
Patient characteristics
We identified 3,933 eligible patients with a median age of 48 years (Interquartile Range: 29, 47) with 997 (25.3%) females. Three thousand fifty-nine (77.8%) patients were identified as white, 371 (9.4%) as Black, and 503 (12.8%) as Hispanic. Two thousand twenty-five (54.0%) patients had private insurance, 821 (20.9%) had Medicare, 529 (13.5%) had Medicaid, and 458 (11.6%) were uninsured (Fig. 1). Three-hundred forty (8.6%) patients had been diagnosed with a major psychiatric disorder, 492 (12.5%) with AUD, and 323 (8.2%) with SUD (Fig. 2). In total, 1,040 (26.4%) patients were discharged directly to home and 2,893 (73.6%) were discharged to another healthcare facility. Multiple statistically significant differences were identified between groups on bivariate analysis, including most notably differences in age, insurance status, comorbid psychiatric diagnosis, mechanism and severity of injury, and hospital geographic region and teaching status (Table 1). Race, gender, AUD, and SUD did not differ significantly with respect to non-home discharge disposition.
Fig. 1.
Summary for sociodemographic variables of patient population.
Fig. 2.
Summary for psychosocial variables of patient population.
Table 1.
Comparison of sociodemographic, psychosocial, injury, and facility covariates between the populations of surgically managed traumatic cervicothoracic fracture patients by discharge status (N=3933).
| Characteristic | Discharge to home N = 1,040 (26.4%) |
Non-home discharge N = 2,893 (73.6%) |
P-Value |
|---|---|---|---|
| Age (years) | <0.001 | ||
| 16 – 25 | 225 (21.6%) | 542 (18.7%) | |
| 26 – 45 | 372 (35.8%) | 686 (23.7%) | |
| 46 – 65 | 345 (33.2%) | 973 (33.6%) | |
| 66 – 75 | 61 (5.9%) | 396 (13.7%) | |
| >75 | 37 (3.6%) | 296 (10.2%) | |
| Gender (male) | 760 (73.1%) | 2176 (75.2%) | 0.174 |
| Race | 0.083 | ||
| White | 791 (76.1%) | 2268 (78.4%) | |
| Hispanic | 116 (11.2%) | 255 (8.8%) | |
| Black | 133 (12.8%) | 370 (12.8%) | |
| Insurance Status | <0.001 | ||
| Private | 595 (57.2%) | 1530 (52.9%) | |
| Medicare | 114 (11%) | 707 (24.4%) | |
| Medicaid | 126 (12.1%) | 403 (13.9%) | |
| Uninsured | 205 (19.7%) | 253 (8.7%) | |
| Major Psychiatric Disorder | 70 (6.7%) | 270 (9.3%) | 0.010 |
| Alcohol Use Disorder | 114 (11%) | 378 (13.1%) | 0.079 |
| Substance Use Disorder | 87 (8.4%) | 236 (8.2%) | 0.834 |
| Intent of Injury | 0.182 | ||
| Unintentional | 1017 (97.8%) | 2796 (96.6%) | |
| Assault | 19 (1.8%) | 82 (2.8%) | |
| Self-inflicted | 4 (0.4%) | 15 (0.5%) | |
| Mechanism of Injury | <0.001 | ||
| Motor vehicle driver/occupant | 449 (43.2%) | 1030 (35.6%) | |
| Pedestrian | 11 (1.1%) | 53 (1.8%) | |
| Other transportation | 138 (13.3%) | 281 (9.7%) | |
| Fall | 374 (36%) | 1318 (45.6%) | |
| Struck by/against | 53 (5.1%) | 132 (4.6%) | |
| Other | 15 (1.4%) | 79 (2.7%) | |
| Fracture Location | 0.026 | ||
| Cervical | 652 (62.7%) | 1819 (62.9%) | |
| Thoracic | 234 (22.5%) | 729 (25.2%) | |
| Cervicothoracic | 154 (14.8%) | 345 (11.9%) | |
| Injury Severity Score (ISS) | <0.001 | ||
| Minor (1 – 8) | 28 (2.7%) | 31 (1.1%) | |
| Moderate (9 – 15) | 534 (51.3%) | 524 (18.1%) | |
| Severe (16 – 26) | 478 (46%) | 2338 (80.8%) | |
| Glasgow Coma Score (GCS) | <0.001 | ||
| 12 – 15 | 1007 (96.8%) | 2596 (89.7%) | |
| 9 – 11 | 5 (0.5%) | 81 (2.8%) | |
| 3 – 8 | 28 (2.7%) | 216 (7.5%) | |
| Hospital Teaching Status (%) | 0.044 | ||
| University | 697 (67%) | 1838 (63.5%) | |
| Community | 343 (33%) | 1055 (36.5%) | |
| Hospital Type (for-profit) | 91 (8.8%) | 290 (10%) | 0.234 |
| Hospital Region | <0.001 | ||
| Midwest | 288 (27.7%) | 878 (30.3%) | |
| Northeast | 90 (8.7%) | 349 (12.1%) | |
| South | 439 (42.2%) | 977 (33.8%) | |
| West | 223 (21.4%) | 689 (23.8%) | |
| ACS Trauma Level | 0.108 | ||
| I | 789 (75.9%) | 2121 (73.3%) | |
| II | 251 (24.1%) | 772 (26.7%) |
ACS = American College of Surgeons
Predictors of discharge disposition
We then performed multivariate logistic regression to adjust for confounders. Patients who were older (age 46-65 OR=1.27, 95% Confidence Interval [1.01-1.59], p=.004; age 66-75 OR=2.58 [1.75-3.82], p<.001; age>75 OR=3.59 [2.26-5.71], p<.001), male (OR=1.29 [1.07-1.56], p=.007), insured by Medicare (OR=1.45 [1.08-1.96], p=.015), or were diagnosed with major psychiatric comorbidity (OR=1.40 [1.03-1.90], p=.034) were significantly more likely to have a non-home discharge (Table 2). The only sociodemographic variable that was associated with a lower odds of utilizing additional healthcare facilities following discharge was uninsured status (OR=0.47 [0.37-0.60], p<.001). This finding was stable across race category. Additionally, patients with ‘severe’ ISS (16-26 points, OR=5.21 [2.96-9.18], p<.001) and lower GCS (3-8 points, OR=2.78 [1.81-4.27], p<.001; 9-11 points, OR=4.80 [1.90-12.11], p=0.001) on admission had a significantly higher chance of a non-home discharge, while hospital location in the Southern United States was associated with lower odds of utilizing a healthcare facility following discharge (OR=0.78 [0.64-0.96], p=.020, Fig. 3). Overall, the multivariate model showed reasonable predictive value for non-home discharge after SCI, with computed AUC value of 0.774 (Fig. 4).
Table 2.
Factors predictive of non-home discharge after surgical management of traumatic cervicothoracic spine fracture on multivariable logistic regression.
| Variable | Odds Ratio | 95% CI | P-value |
|---|---|---|---|
| Age | |||
| 16-25 | 1 | (Base) | (Base) |
| 26-45 | 0.86 | 0.69 - 1.08 | 0.189 |
| 46-65 | 1.27 | 1.01 - 1.59 | 0.044 |
| 66-75 | 2.58 | 1.75 - 3.82 | <0.001 |
| >75 | 3.59 | 2.26 - 5.71 | <0.001 |
| Gender | |||
| Female | 1 | (Base) | (Base) |
| Male | 1.29 | 1.07 - 1.56 | 0.007 |
| Race | |||
| White | 1 | (Base) | (Base) |
| Hispanic | 0.88 | 0.67 - 1.16 | 0.356 |
| Black | 1 | 0.78 - 1.30 | 0.975 |
| Insurance Status | |||
| Private | 1 | (Base) | (Base) |
| Medicare | 1.45 | 1.08 - 1.96 | 0.015 |
| Medicaid | 1.08 | 0.84 - 1.39 | 0.546 |
| Uninsured | 0.47 | 0.37 - 0.60 | <0.001 |
| Major Psychiatric Disorder | |||
| No | 1 | (Base) | (Base) |
| Yes | 1.40 | 1.03 - 1.90 | 0.034 |
| Alcohol Use Disorder | |||
| No | 1 | (Base) | (Base) |
| Yes | 1.19 | 0.92 - 1.53 | 0.188 |
| Substance Use Disorder | |||
| No | 1 | (Base) | (Base) |
| Yes | 1.22 | 0.91 - 1.64 | 0.190 |
| Fracture Region | |||
| Cervical | 1 | (Base) | (Base) |
| Thoracic | 1.42 | 1.16 - 1.72 | 0.001 |
| Cervicothoracic | 0.81 | 0.64 - 1.03 | 0.091 |
| Injury Severity Score (ISS) | |||
| Minor (1 - 8) | 1 | (Base) | (Base) |
| Moderate (9 - 15) | 0.90 | 0.51 - 1.59 | 0.715 |
| Severe (16 - 26) | 5.21 | 2.96 - 9.18 | <0.001 |
| Glasgow Coma Score (GCS) | |||
| 12 – 15 | 1 | (Base) | (Base) |
| 9 – 11 | 4.8 | 1.90 - 12.11 | 0.001 |
| 3 - 8 | 2.78 | 1.81 - 4.27 | <0.001 |
| Intent of Injury | |||
| Unintentional | 1 | (Base) | (Base) |
| Assault | 1.05 | 0.5 - 2.22 | 0.899 |
| Self-inflicted | 1.44 | 0.41 - 5.02 | 0.567 |
| Mechanism of Injury | |||
| Motor vehicle driver/occupant | 1 | (Base) | (Base) |
| Pedestrian | 1.47 | 0.73 - 2.99 | 0.283 |
| Other transportation | 0.86 | 0.66 - 1.13 | 0.282 |
| Fall | 1.30 | 1.07 - 1.57 | 0.007 |
| Struck by/against | 1.33 | 0.90 - 1.98 | 0.157 |
| Other | 1.48 | 0.68 - 3.24 | 0.329 |
| Hospital Type | |||
| Non-profit | 1 | (Base) | (Base) |
| For profit | 1.27 | 0.96 - 1.69 | 0.094 |
| Region | |||
| Midwest | 1 | (Base) | (Base) |
| Northeast | 1.30 | 0.96 - 1.76 | 0.085 |
| South | 0.78 | 0.64 - 0.96 | 0.020 |
| West | 1.07 | 0.85 - 1.34 | 0.581 |
| Hospital Teaching Status | |||
| University | 1 | (Base) | (Base) |
| Community | 1 | 0.80 - 1.24 | 0.982 |
| ACS Trauma Level | |||
| I | 1 | (Base) | (Base) |
| II | 1.18 | 0.93 - 1.49 | 0.167 |
ACS = American College of Surgeons.
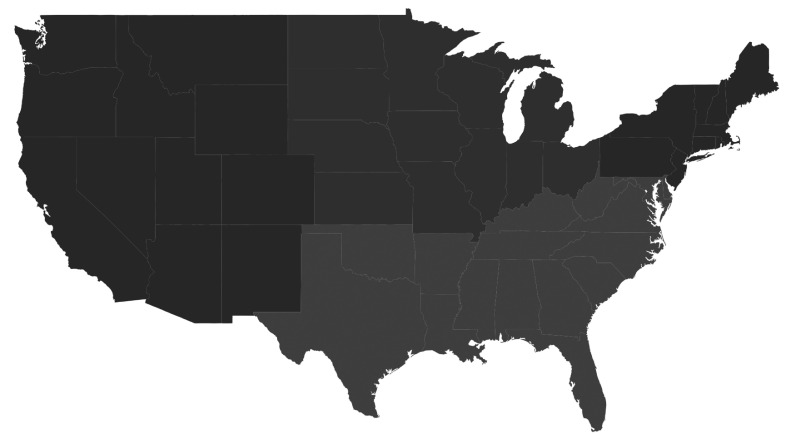
Fig. 3.
Propensity to be discharged to a non-home destination by geographic region.
Fig. 4.
The multivariate model showed reasonable predictive value for non-home discharge after SCI, with a computed AUC value of 0.774.
Discussion
Prior evidence suggests that rehabilitation following spinal cord injury is important for improving neurological and functional recovery [5], [6], [7], [8]. However, it is unclear how sociodemographic and psychosocial variables may influence patient access to these critical yet costly healthcare resources amidst the current United States healthcare landscape. To further elucidate these relationships, we analyzed a national trauma database finding that there may be barriers to care for patients without insurance post-SCI. In the present article, we found that patients with no insurance were significantly less likely to access medical resources following discharge from the hospital after surgical management.
Our findings are consistent with the previously published literature related to insurance status and discharge disposition after trauma admissions [21], [22], [23], [24], [25], [26], [27]. In their 2011 article, Sacks et al. [28] conducted a retrospective cohort analysis of all trauma patients in the NTDB for the years 2002–2006, encompassing the same duration of data exactly 10 years prior to the present study's cohort. The researchers performed a multivariate logistic regression finding that uninsured patients had the lowest odds of being discharged to a SNF (CI=0.73–0.80), home health (CI=0.49–0.53), and rehabilitation (CI=0.44–0.46). Uninsured patients had the highest odds, however, of being discharged directly to home (CI=1.30–1.34). Similarly, Graham et al. (2020) [21] studied the 2015 NTDB of all trauma patients. The group reported that uninsured patients were significantly less likely to have a non-home discharge (CI=0.42-0.46). Lastly, Lu et al. (2022) [27] found that patients without insurance were less likely to be discharged to SNF or another healthcare facility (CI=0.44–0.54) and inpatient rehabilitation/long-term care facility (CI=0.43–0.50) following moderate-to-severe traumatic brain injury. Evidently, this is a trend in the United States which has persisted over more than a decade.
We augment these authors’ previous findings using a larger number of more recent years of the NTDB and extending their findings specifically to the SCI population–a population that particularly benefits from post-discharge rehabilitation services. In addition to focusing specifically on patients with SCI, unlike previous the previous literature mentioned above, we also performed additional multivariate analysis on fracture region, alcohol use disorder, substance use disorder, GCS score, intent of injury, and mechanism of injury to better understand how these factors are associated with home or non-home discharge disposition in the context of SCI.
Notably, our NTDB cohort encompasses those treated in years after the Affordable Care Act (ACA) was enacted, suggesting patients may still be at risk of not utilizing critical healthcare resources due to cost despite more Americans being insured overall. The main aim of the ACA was to improve healthcare delivery and outcomes for patients [29]. The ACA has had the most poignant effect on reducing the number of uninsured by improving the availability of health insurance through a variety of mechanisms [30,31]. From 2010 to 2016 the uninsured rate fell by nearly half [32]. While there have been many tangible benefits since the law's authorization in 2010, studies have found that it has had its shortcomings [33]. Particularly germane to the present study, Moffett et al. (2017) [22] found that uninsured patients were slightly less likely (OR: .48, p<.001) to be discharged to a non-home destination after the ACA as compared to before (OR: .56, p<.001). Despite this, the unique characteristics of the post-ACA uninsured population, which may contribute to this finding, remain poorly understood. Still, approximately 30 million Americans currently do not have health insurance [32]. Half of these constituents qualify for an ACA subsidy via Medicaid coverage or through the Marketplaces but do not access them [32]. The reasons for these phenomena are beyond the scope of the present discussion, but highlight the areas for improvement in care for uninsured patients with SCI.
We also report that patients with Medicare have higher odds of non-home discharge. Prior analyses have come to similar conclusions, with Medicare patients more likely to be discharged to another healthcare facility after hospitalization [25,27,34,35]. However, these studies exclusively focused on patients of all types of trauma in the NTDB or patients with traumatic brain injuries, but no patients with traumatic SCI as was the focus of the present study. There may be several reasons for this paradigm found in previous studies and identified in our own. First, Medicare patients, by definition, are older and therefore may require more assistance to regain their functional independence. Second, the initial period of a Medicare-covered SNF stay has no cost-sharing or daily copayments for the patient [13]. This period, generally of 20-days, is fully subsidized by Medicare which has raised concerns that some of this care may be unnecessarily driving up costs for Medicare beneficiaries [13]. Interestingly, cost-sharing of this first portion of SNF placement has resulted in shorter length of stays, suggesting implementing cost sharing to potentially reduce unnecessary Medicare claims [13]. Extending these findings to the present study, particularly the uninsured population, suggests that patients may not be utilizing healthcare resources, such as SNFs, due to personally borne costs without insurance coverage.
We initially hypothesized that psychosocial variables such as a diagnosis of a major psychiatric disorder, AUD, and SUD influences healthcare utilization after discharge. Only a diagnosis of a major psychiatric disorder was found to be predictive of an increased chance of a non-home discharge. Prior studies have similarly reported an increased utilization of healthcare resources in patients with mental illness [16,36,37]. For example, our previously published research demonstrated that patients diagnosed with major psychiatric disorder, alcohol use disorder, and substance use disorder were more likely to receive an MRI following spinal trauma [38]. Additionally, Wagner et al. and Baillargeon et al. found that patients with similar disorders had increased likelihoods of overnight hospital stays and emergency room treatment [39,40]. While these studies did not prove causality, authors have advocated that patients with psychiatric illness may benefit from mental health services surrounding their respective illness, and recovery following illness, to reduce unnecessary medical visits [36].
Furthermore, we show that patients with severe ISS [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26] were significantly associated with higher odds of non-home discharge compared to patients with minor ISS scores. In a single-institutional cohort study, Claridge et al. similarly found that increasing ISS was an independent predictor or discharge to a rehabilitation facility following hospitalization for spinal cord injury (p<0.002) [41]. This finding is also complemented by our group's recent work which found that high ISS and low GCS scores were associated with longer lengths of stay, suggesting more severe injury and need for rehabilitation post-hospitalization [42].
Lastly, we found that patients in the Southern United States are significantly less likely to be discharged to another healthcare or rehab facility following SCI, after correcting for other patient specific covariates. Prior analyses have also found regional variation of discharge disposition [27,43]. Interestingly, the largest overall proportion of home health agencies (48.3%) are located in the South, which could explain this phenomenon as patients may have more access to home healthcare services following their injury [44]. It is also possible families of patients may be more willing to take care of patients at home following their injury. Sociology literature has suggested the there is an emphasis on the solidarity of the nuclear family in the Southern United States rooting back to traditional values of an agrarian rural class [45]. However, the present analysis is not designed to prove causality in this relationship, and whether home healthcare is indeed providing the same proven outcome benefit as acute post-SCI rehabilitation for patients in this region is unclear.
Limitations
The present article is not without limitations, most of which are inherent in administrative data analysis. While the NTDB is a large database powered to answer our question, it lacks data granularity specifically regarding to the type of spine fracture and SCI severity (e.g., American Spinal Injury Association, or ‘ASIA,’ classification). Decision to discharge a patient to another healthcare facility for rehabilitation following SCI depends to some degree on the severity of the injury and type of fracture, which we were unable to include as a covariate. However, given this weakness of the database to account for injury severity, we utilized the GCS and ISS scales, which are not directly related to the spine, but lend some, albeit incomplete, information regarding the patient's injury severity upon presentation. Another reason GCS and ISS scales were utilized stems from the NTDB's lack of information on fracture morphologies, possibly more relevant metrics such as the ASIA impairment scale, and specific injury mechanisms such as distraction or translocation injuries. Therefore, given the limitations of the dataset, GCS and ISS scales were employed to characterize the overall severity of the patients’ injuries upon presentation. Additionally, we were only able to include the presenting GCS of each patient and not the GCS at discharge as the NTDB does not contain such information. Including the GCS at discharge as a covariate may have augmented our findings, but we were unable to do so due to the limitations of the NTDB.
We were also able to include information on the fracture location within the spine, which lends pertinent information as spinal fractures at different levels carry unique motor and sensory deficits, differing outcomes, and differing long-term sequalae [46,47]. Still, the NTDB does not contain an ideal set of variables to objectively assess in which instances non-home discharge was indicated and justified and in which cases home discharge would have been appropriate. This lack of granularity may conceal potential confounding variables that we were unable to account for within the regression models.
It is possible that some patients may have been transiently in the region in which they received surgery and reside in another region. The place of residence is not available within the NTDB, only the region in which the patient was treated is present within the dataset. Thus, we were unable to correct for place of residence in the present analysis. While injury and subsequent treatment may have occurred in a region outside of where the patient resides, this is likely a relatively uncommon phenomenon, given that the majority of injuries in our study were caused by motor vehicle accidents or falls, a finding previously documented in the literature [48]. As motor vehicle accidents and falls most commonly occur at home or near home, it is unlikely that many patients in the present study were injured in non-home regions [49], [50], [51], [52]. Finally, the NTDB is a voluntary database prone to missing coding data leading to sampling bias. This potentially limits the present study's generalizability to only those institutions that electively submit data. Future studies should survey patients' reasons for not accessing rehabilitation even when medically indicated.
Conclusions
After correcting for injury severity, mechanism, and location, uninsured patients are significantly less likely to be discharged to alternative healthcare facilities, such as acute rehabilitation centers or SNFs, following surgical management for spine fracture with SCI. Cost-related barriers accessing rehabilitation services still seem to exist for patients following surgical management of traumatic cervical or thoracic spine fracture with SCI. We suggest further research regarding solutions to this issue, such as the efficacy of commercial health center or Community Health Center-run programs assisting uninsured individuals apply for insurance following illness, emergency funds reimbursing hospital and healthcare providers treating uninsured patients with severe injury, and the efficacy of patient navigators in addressing health disparities and facilitating healthcare access and quality among the uninsured following debilitating injury. SCI also carries a significant burden globally, with patients in developing countries facing disparities concerning access to surgical intervention and patient follow-up. More research into variations in discharge disposition for patients with surgically managed traumatic SCI is needed.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
Footnotes
FDA device/drug status: Not applicable.
Author disclosures: MJH: Nothing to disclose. NJP: Nothing to disclose. OPL: Nothing to disclose. AG:Nothing to disclose. RS:Nothing to disclose. KX: Nothing to disclose. BZ: Nothing to disclose. MB: Nothing to disclose. JQC-Q: Nothing to disclose. TN: Nothing to disclose. PZS: Nothing to disclose. JFA: Nothing to disclose. AET: Nothing to disclose. ZLG: Nothing to disclose. AAO: Nothing to disclose. JSF: Nothing to disclose.
Summary sentence: Uninsured patients are less likely to be discharged to acute rehabilitation or alternative healthcare facilities following surgical management of SCI. High out-of-pocket costs for uninsured patients in the United States may deter utilization of these services.
References
- 1.Merritt C.H., Taylor M.A., Yelton C.J., Ray S.K. Economic impact of traumatic spinal cord injuries in the United States. Neuroimmunol Neuroinflamm. 2019;6 doi: 10.20517/2347-8659.2019.15. 33869674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sekhon L.H., Fehlings M.G. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine. 2001;26(24 Suppl) doi: 10.1097/00007632-200112151-00002. (Phila Pa 1976)S2-12.11805601. [DOI] [PubMed] [Google Scholar]
- 3.Hagen E.M. Acute complications of spinal cord injuries. World J Orthop. 2015;6(1) doi: 10.5312/wjo.v6.i1.17. 17-23.25621207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDaid D., Park A.L., Gall A., Purcell M., Bacon M. Understanding and modelling the economic impact of spinal cord injuries in the United Kingdom. Spinal Cord. 2019;57(9):778–788. doi: 10.1038/s41393-019-0285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerszten P.C., Witham T.F., Clyde B.L., Welch W.C. Relationship between type of health insurance and time to inpatient rehabilitation placement for surgical subspecialty patients. Am J Med Qual. 2001;16(6) doi: 10.1177/106286060101600605. 212-5.11816852. [DOI] [PubMed] [Google Scholar]
- 6.Nas K., Yazmalar L., Şah V., Aydın A., Öneş K. Rehabilitation of spinal cord injuries. World J Orthop. 2015;6(1) doi: 10.5312/wjo.v6.i1.8. 8-16.25621206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berlowitz D.J., Tamplin J. Respiratory muscle training for cervical spinal cord injury. Cochrane Database Syst Rev. 2013;(7) doi: 10.1002/14651858.CD008507.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Astorino T.A., Harness E.T., Witzke K.A. Effect of chronic activity-based therapy on bone mineral density and bone turnover in persons with spinal cord injury. Eur J Appl Physiol. 2013;113(12) doi: 10.1007/s00421-013-2738-0. 3027-37.24097172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burns A.S., Marino R.J., Kalsi-Ryan S., Middleton J.W., Tetreault L.A., Dettori J.R., et al. Type and timing of rehabilitation following acute and subacute spinal cord injury: a systematic review. Glob Spine J. 2017;7(3_suppl) doi: 10.1177/2192568217703084. 175S-94S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.French D.D., Campbell R.R., Sabharwal S., Nelson A.L., Palacios P.A. Health care costs for patients with chronic spinal cord injury in the veterans health administration. J Spinal Cord Med. 2007;30(5) doi: 10.1080/10790268.2007.11754581. 477-81.18092564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brem H., Maggi J., Nierman D., Rolnitzky L., Bell D., Rennert R., et al. High cost of stage IV pressure ulcers. Am J Surg. 2010;200(4):473–477. doi: 10.1016/j.amjsurg.2009.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGinnis G.E., Osberg J.S., Seward M.L., Campion E.W., Branch L.G., DeJong G. Total charges for inpatient medical rehabilitation. Health Care Financ Rev. 1988;9(4) 31-40.10312630. [PMC free article] [PubMed] [Google Scholar]
- 13.Keohane L.M., Grebla R.C., Rahman M., Mukamel D.B., Lee Y., Mor V., et al. First-dollar cost-sharing for skilled nursing facility care in medicare advantage plans. BMC Health Serv Res. 2017;17(1):611. doi: 10.1186/s12913-017-2558-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Claridge J.A., Croce M.A., Weinberg J.A., Forsythe R.M., Miller C., Fabian T.C. The real predictors of disposition in patients with spinal cord injuries. J Trauma Acute Care Surg. 2006;60(1):178–186. doi: 10.1097/01.ta.0000198804.74514.0c. [DOI] [PubMed] [Google Scholar]
- 15.Larsson J., Kristensen S.L., Madelaire C., Schou M., Rossing K., Boesgaard S., et al. Socioeconomic disparities in referral for invasive hemodynamic evaluation for advanced heart failure: a nationwide cohort study. Circ Heart Fail. 2021;14(10) doi: 10.1161/CIRCHEARTFAILURE.121.008662. [DOI] [PubMed] [Google Scholar]
- 16.Hagan M.J., Pertsch N.J., Leary O.P., Xi K., Zheng B., Camara-Quintana J.Q., et al. Socioeconomic and psychosocial predictors of magnetic resonance imaging following cervical and thoracic spine trauma in the United States. World Neurosurg. 2022 doi: 10.1016/j.wneu.2022.02.093. 35231622. [DOI] [PubMed] [Google Scholar]
- 17.Hagan M.J., Pertsch N.J., Leary O.P., Zheng B., Camara-Quintana J.Q., Niu T., et al. Influence of psychosocial and sociodemographic factors in the surgical management of traumatic cervicothoracic spinal cord injury at level I and II trauma centers in the United States. J Spine Surg. 2021;7(3):277–288. doi: 10.21037/jss-21-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hagan M.J., Sastry R.A., Feler J., Shaaya E.A., Sullivan P.Z., Abinader J.F., et al. Neighborhood-level socioeconomic status predicts extended length of stay following elective anterior cervical spine surgery. World Neurosurg. 2022 doi: 10.1016/j.wneu.2022.03.124. [DOI] [PubMed] [Google Scholar]
- 19.Trauma Co . American College of Surgeons; Chicago, IL: 2012. NTDB Version 2012-2016. -2016. [Google Scholar]
- 20.Daly M.C., Patel M.S., Bhatia N.N., Bederman SS. The Influence of insurance status on the surgical treatment of acute spinal fractures. Spine. 2016;41(1):E37–E45. doi: 10.1097/BRS.0000000000001177. (Phila Pa 1976).26555838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Graham M., Parikh P., Hirpara S., McCarthy M.C., Haut E.R., Parikh P.P. Predicting discharge disposition in trauma patients: development, validation, and generalization of a model using the national trauma data bank. Am Surg. 2020;86(12) doi: 10.1177/0003134820949523. 1703-9.32915055. [DOI] [PubMed] [Google Scholar]
- 22.Moffet E.W., Zens T.J., Haines K.L., Beems M.V., McQuistion K.M., Leverson G.E., et al. Race, insurance status, and traumatic brain injury outcomes before and after enactment of the Affordable Care Act. Surgery. 2018;163(2):251–258. doi: 10.1016/j.surg.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Budnick H.C., Tyroch A.H., Milan S.A. Ethnic disparities in traumatic brain injury care referral in a Hispanic-majority population. J Surg Res. 2017;215:231–238. doi: 10.1016/j.jss.2017.03.062. [DOI] [PubMed] [Google Scholar]
- 24.Sacks G.D., Hill C., Rogers S.O., Jr Insurance status and hospital discharge disposition after trauma: inequities in access to postacute care. J Trauma Acute Care Surg. 2011;71(4):1011–1015. doi: 10.1097/TA.0b013e3182092c27. [DOI] [PubMed] [Google Scholar]
- 25.Kane W.G., Wright D.A., Fu R., Carlson K.F. Racial/ethnic and insurance status disparities in discharge to posthospitalization care for patients with traumatic brain injury. J Head Trauma Rehabil. 2014;29(6):E10–EE7. doi: 10.1097/HTR.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 26.McQuistion K., Zens T., Jung H.S., Beems M., Leverson G., Liepert A., et al. Insurance status and race affect treatment and outcome of traumatic brain injury. J Surg Res. 2016;205(2):261–271. doi: 10.1016/j.jss.2016.06.087. [DOI] [PubMed] [Google Scholar]
- 27.Lu J., Gormley M., Donaldson A., Agyemang A., Karmarkar A., Seel R.T. Identifying factors associated with acute hospital discharge dispositions in patients with moderate-to-severe traumatic brain injury. Brain Inj. 2022 doi: 10.1080/02699052.2022.2034180. 1-10.35213272. [DOI] [PubMed] [Google Scholar]
- 28.Sacks G.D., Hill C., Rogers S.O.J. Insurance status and hospital discharge disposition after trauma: inequities in access to postacute care. J Trauma Acute Care Surg. 2011;71(4) doi: 10.1097/TA.0b013e3182092c27. 1011-5.00005373-201110000-00035. [DOI] [PubMed] [Google Scholar]
- 29.Silvers J.B. The affordable care act: objectives and likely results in an imperfect world. Ann Fam Med. 2013;11(5):402–405. doi: 10.1370/afm.1567. .24019270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blumenthal D., Abrams M., Nuzum R. The affordable care act at 5 years. Mass Med Soc; 2015:2451–2458. doi: 10.1056/NEJMhpr1503614. [DOI] [PubMed] [Google Scholar]
- 31.Carman K.G., Eibner C. Changes in health insurance enrollment since 2013: evidence from the RAND health reform opinion study. Rand Health Q. 2014;4(3) [PMC free article] [PubMed] [Google Scholar]
- 32.Sommers B.D. Health insurance coverage: what comes after the ACA? an examination of the major gaps in health insurance coverage and access to care that remain ten years after the Affordable Care Act. Health Aff. 2020;39(3):502–508. doi: 10.1377/hlthaff.2019.01416. [DOI] [PubMed] [Google Scholar]
- 33.Blumenthal D., Abrams M., Nuzum R. The affordable care act at 5 years. N Engl J Med. 2015;372(25):2451–2458. doi: 10.1056/NEJMhpr1503614. .25946142. [DOI] [PubMed] [Google Scholar]
- 34.Zogg C.K., Scott J.W., Metcalfe D., Seshadri A.J., Tsai T.C., Davis W.A., et al. The association between medicare eligibility and gains in access to rehabilitative care. Ann Surg. 2017;265(4):734–742. doi: 10.1097/SLA.0000000000001754. [DOI] [PubMed] [Google Scholar]
- 35.Haines K.L., Nguyen B.P., Vatsaas C., Alger A., Brooks K., Agarwal S.K. Socioeconomic status affects outcomes after severity-stratified traumatic brain injury. J Surg Res. 2019;235:131–140. doi: 10.1016/j.jss.2018.09.072. [DOI] [PubMed] [Google Scholar]
- 36.Wagner J.A., Pietrzak R.H., Petry N.M. Psychiatric disorders are associated with hospital care utilization in persons with hypertension. Soc Psychiatry Psychiatr Epidemiol. 2008;43(11):878–888. doi: 10.1007/s00127-008-0377-2. [DOI] [PubMed] [Google Scholar]
- 37.Jacques Baillargeon P.D., Chris R., Thomas M.D., Brie Williams M.D., Charles E., Begley P.D., Sarghi Sharma M.D., Brad H., Pollock P.D., et al. Medical emergency department utilization patterns among uninsured patients with psychiatric disorders. Psychiatr Serv. 2008;59(7):808–811. doi: 10.1176/ps.2008.59.7.808. .18587001. [DOI] [PubMed] [Google Scholar]
- 38.Hagan M.J., Pertsch N.J., Leary O.P., Xi K., Zheng B., Camara-Quintana J.Q., et al. Socioeconomic and psychosocial predictors of magnetic resonance imaging after cervical and thoracic spine trauma in the United States. World Neurosurg. 2022;161:e757–ee66. doi: 10.1016/j.wneu.2022.02.093. .35231622. [DOI] [PubMed] [Google Scholar]
- 39.Wagner J.A., Pietrzak R.H., Petry N.M. Psychiatric disorders are associated with hospital care utilization in persons with hypertension: results from the National Epidemiologic Survey on alcohol and related conditions. Soc Psychiatry Psychiatr Epidemiol. 2008;43(11):878–888. doi: 10.1007/s00127-008-0377-2. .18575791. [DOI] [PubMed] [Google Scholar]
- 40.Baillargeon J., Thomas C.R., Williams B., Begley C.E., Sharma S., Pollock B.H., et al. Medical emergency department utilization patterns among uninsured patients with psychiatric disorders. Psychiatr Serv. 2008;59(7):808–811. doi: 10.1176/ps.2008.59.7.808. .18587001. [DOI] [PubMed] [Google Scholar]
- 41.Claridge J.A., Croce M.A., Weinberg J.A., Forsythe R.M., Miller C., Fabian T.C. The real predictors of disposition in patients with spinal cord injuries. J Trauma. 2006;60(1):178–186. doi: 10.1097/01.ta.0000198804.74514.0c. .16456453. [DOI] [PubMed] [Google Scholar]
- 42.Hagan M.J., Pertsch N.J., Leary O.P., Sastry R., Ganga A., Xi K., et al. Influence of sociodemographic and psychosocial factors on length of stay following surgical management of traumatic spine fracture with spinal cord injury. World Neurosurg. 2022 doi: 10.1016/j.wneu.2022.07.128. .35940503. [DOI] [PubMed] [Google Scholar]
- 43.Akintoye E., Briasoulis A., Egbe A., Adegbala O., Sheikh M., Singh M., et al. Regional variation in mortality, length of stay, cost, and discharge disposition among patients admitted for heart failure in the United States. Am J Cardiol. 2017;120(5):817–824. doi: 10.1016/j.amjcard.2017.05.058. .28705376. [DOI] [PubMed] [Google Scholar]
- 44.Harris-Kojetin L.D., Sengupta M., Park-Lee E., Valverde R. Long-term care services in the United States: 2013 overview. 2013 [PubMed]
- 45.Vance R.B. Regional family patterns: the Southern family. Am J Sociol. 1948;53(6):426–429. doi: 10.1086/220233. [DOI] [PubMed] [Google Scholar]
- 46.Beeharry M.W., Moqeem K., Rohilla M.U. Management of cervical spine fractures: a literature review. Cureus. 2021;13(4):e14418. doi: 10.7759/cureus.14418. .33987067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Spiegl U.J.A., Schnake K.J., Hartmann F., Katscher S., Riehle M., Scheyerer M.J., et al. Traumatic fractures of the thoracic spine. Z Orthop Unfall. 2021;159(4):373–382. doi: 10.1055/a-1144-3846. .32392598. [DOI] [PubMed] [Google Scholar]
- 48.Leucht P., Fischer K., Muhr G., Mueller E.J. Epidemiology of traumatic spine fractures. Injury. 2009;40(2):166–172. doi: 10.1016/j.injury.2008.06.040. .19233356. [DOI] [PubMed] [Google Scholar]
- 49.Moreland B.L., Kakara R., Haddad Y.K., Shakya I., Bergen G. A descriptive analysis of location of older adult falls that resulted in emergency department visits in the United States, 2015. Am J Lifestyle Med. 2021;15(6):590–597. doi: 10.1177/1559827620942187. .34916877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cheney-Lippold J. Accidents happen. Soc Res An Int Q. 2019;86(2):513–535. [Google Scholar]
- 51.Burdett B.R.D., Starkey N.J., Charlton S.G. The close to home effect in road crashes. Saf Sci. 2017;98:1–8. [Google Scholar]
- 52.Burdett B.R., Charlton S.G., Starkey N.J. Not all minds wander equally: the influence of traits, states and road environment factors on self-reported mind wandering during everyday driving. Accid Anal Prev. 2016;95:1–7. doi: 10.1016/j.aap.2016.06.012. [DOI] [PubMed] [Google Scholar]