Abstract
Introduction: The oblique popliteal ligament (OPL), chief posterior support of the knee, is an extension of the semimembranosus (SM) tendon and runs superolaterally to the lateral femoral condyle. Due to variations and immense functional value of the OPL, the present study was undertaken to explore the OPL morphology and morphometry.
Materials and methods:Thirty cadaveric lower limbs were dissected to observe the OPL in the floor of the popliteal fossa, and its general shape, number of bands and extensions were noted. The morphometry was done using digital callipers in which the length of the upper and lower margins as well as the width of the OPL at the medial and lateral attachments were measured. The width of bands and extensions were also recorded. The mean and standard deviation (SD) of all parameters have been also calculated.
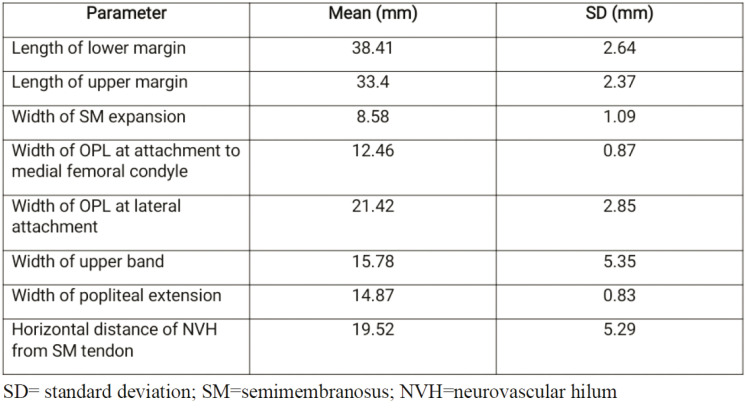
Results:The morphological types of the OPL were categorized into four types, which were found in 40%, 50%, 6.6% and 3.3% of specimens, respectively. Types 1 and 2 OPL were band like. Type 1 showed an accessory upper band and type 2, a broad medial attachment. Type 3 was cord like, whereas type 4 was fan like and showed two upper bands. The mean length (upper), length (lower), width of the SM tendon expansion, width at attachment to the medial femoral condyle and width at the lateral attachment were 33.4 mm, 38.41 mm, 8.58 mm, 12.46 mm and 21.42 mm, respectively.
Conclusion:The different morphological types of OPL may produce minor alterations in the stability of the knee, especially in trauma. The anatomical knowledge of OPL and its extensions is mandatory for knee surgery in all patients to avoid postoperative complications.
Keywords:oblique popliteal ligament, semimembranosus, posterior knee.
INTRODUCTION
The oblique popliteal ligament (OPL) is the chief support of knee joint on its posterior aspect. The distal tendon of the semimembranosus (SM) muscle has five insertions, with the oblique popliteal ligament being one of them (1-3). This ligament arises as an extension of the tendon of the SM muscle and runs superolaterally to get attached to the lateral femoral condyle. It is oriented in an oblique direction behind the capsule of the knee joint (1, 2, 4).
In the literature there are various discrepancies regarding the medial and lateral attachments of OPL. This ligament has been documented in various studies as arising from the sheath of the SM tendon. Occasionally, both the sheath and the tendon contribute to the OPL (5-7). Additionally, the OPL may have an unusual attachment to the posterior aspect of the medial femoral condyle (8).
The lateral attachment of the OPL to the posterior aspect of the lateral femoral condyle is constant. Moreover, the fabella and plantaris muscle may also receive extensions from the OPL (1).
The oblique popliteal ligament plays pivotal role in the stabilisation of the knee during terminal extension and prevents hyperextension of the knee. It has been implicated in the posttraumatic genu recurvatum (9).
Anatomical insight of the OPL has been largely ignored previously, although it plays a major role in providing rotatory stability due to its tibial attachment (8). Therefore, the anatomical study of the posterior supports of the knee joint, especially the OPL, will prove to be of immense value for orthopedic surgeons. These anatomical details confirmed by dissection will augment the scanty data on the OPL which are currently available.
MATERIAL & METHODS
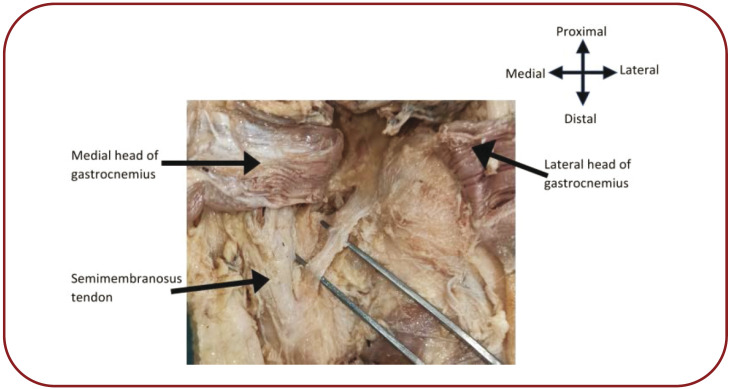
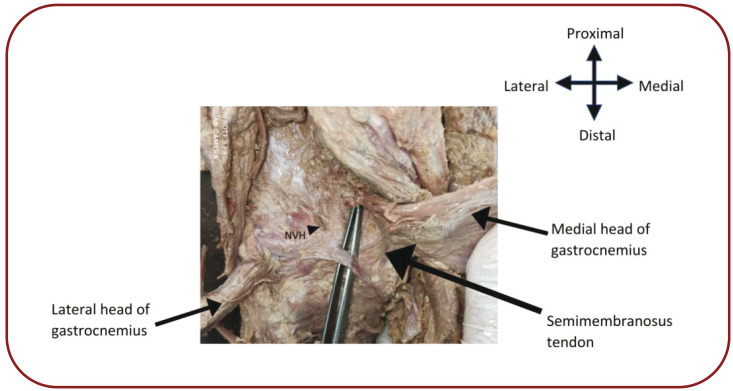
Thirty lower limbs obtained from fifteen cadavers were dissected. The contents and boundaries of the popliteal fossa were cleaned. The two heads of the gastrocnemius and plantaris were cut below the knee joint and reflected proximally. The tibial and common peroneal nerves and the popliteal vessels were also cut to view the floor of the popliteal fossa. The OPL was observed, with the gross morphological features including its general shape (band like or cord like), number of bands and presence of any extensions. Subsequently, OPL morphometry was performed using digital vernier callipers accurate to 0.1 mm.
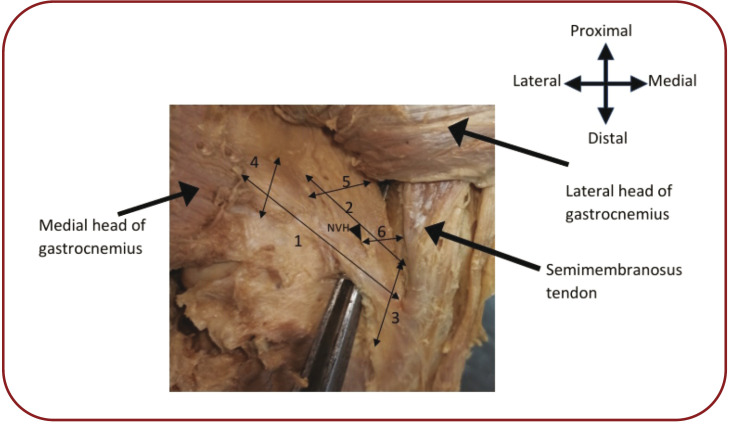
The following morphometric parameters were included by us (Figure 1): 1) length of the lower margin was observed between the SM tendon and the lateral head of the gastrocnemius; 2) length of the upper margin was measured between the SM tendon and the medial border of the lateral femoral condyle; 3) width at the medial attachment of the OPL (width of SM expansion and width of attachment to the medial femoral condyle); 4) width at the lateral attachment of the OPL; 5) width of bands, if any; 6) width of extensions, if any; and 7) horizontal distance of the neurovascular hilum (NVH) from the SM tendon.
All measurements were recorded, and the mean and standard deviation (SD) was calculated.
RESULTS
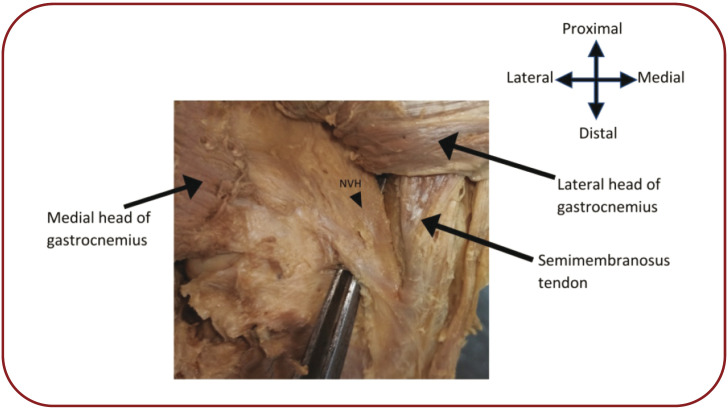
In the present study, the OPL was observed in all knee specimens. The morphological types of the OPL were categorized into four types. Type 1 was seen in 12 (40%) specimens, in which the OPL was mainly band like, with the medial at tachment at the SM tendon only and lateral attachment at the lateral head of the gastrocnemius and medial border of the lateral femoral condyle; in this type, an accessory upper band attached to the intercondylar line of the femur was seen (Figure 2).
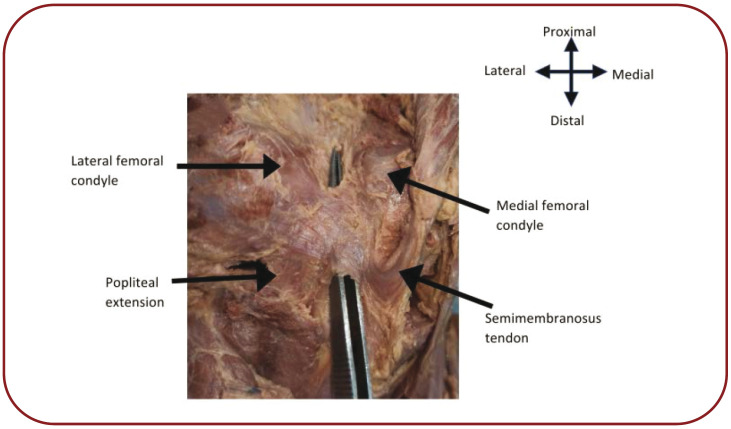
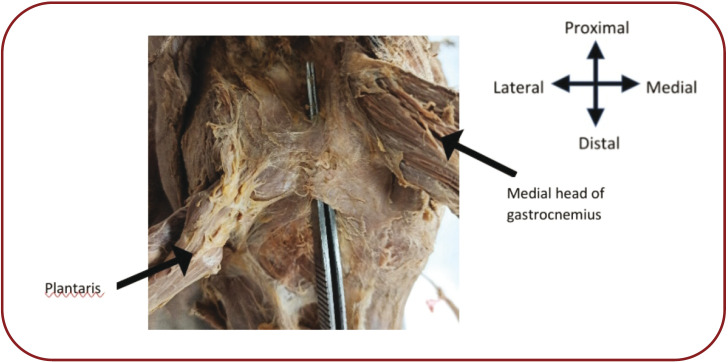
Type 2 was found in 15 (50%) specimens. Similarly to type 1, it was also like a band, with a broad medial attachment to both the SM tendon and medial femoral condyle. The lateral attachment was similar to type 1. In 12 specimens of this type, an extension to the anterior surface of the popliteus was also found (Figure 3), and in three specimens, lateral attachment intermingled with the origin of the plantaris (Figure 4).
Type 3 OPL was found in two (6.6%) specimens and was cord like, with medial attachment to the SM tendon and lateral attachment to the medial border of the lateral femoral condyle (Figure 5).
Type 4 was found in only one (3.3%) specimen. In this type, the OPL was fanning out from a narrow medial attachment to its lateral attachment to the lateral femoral condyle and lateral head of the gastrocnemius. There were two upper bands, each attaching to intercondylar line of the femur, with the neurovascular hilum located between them (Figure 6). Table 1 depicts the mean and SD of OPL morphometric parameters.
DISCUSSION
Various investigations on the knee anatomy have been performed in the past. However, the OPL has received less attention in this regard. The present study elucidates OPL morphology through detailed cadaveric dissection.
Wu XD et al classified the OPL into band-shaped, Y-shaped, Z-shaped, trident-shaped and complex- shaped configurations. In the present study, the OPL was classified into type 1, type 2, type 3 and type 4. Types 1 and 2 were band-shaped, type 3 cord like and type 4 fan-shaped. Wu XD et al postulated that prenatal heredity and postnatal development may be responsible for the different shapes of the OPL (10). These different types of OPL may produce minor alterations in the stability of the knee especially in trauma. The lined and split attachments of the OPL may predispose it to traumatic injuries.
Hedderwick et al found that the OPL consisted of two bands in 70% of explored specimens and considered both attachments of the OPL as bands (8). The authors of the current investigation have elucidated the attachments of OPL in a novel manner. The part of the OPL attaching to the lateral femoral condyle and lateral head of the gastrocnemius was considered as the main ligament, and the part of the OPL attaching to the intercondylar line of the femur as a ‘band’.
The position of the neurovascular hilum was usually observed between the main ligament and the upper band in type 1 specimens, whereas in type 4 specimen, it was noted between the two upper bands. Thus, the neurovascular hilum effectively divides the ligament and its bands, accounting for the varied morphology of the OPL.
The medial attachment of OPL has been variably described in many studies, most of which have confirmed that the OPL was an extension of the SM tendon (1, 8, 11). Hedderwick et al observed that in all specimens, except one, the OPL was attached to the medial femoral condyle and medial head of the gastrocnemius in addition to the SM tendon. The present study has also seen the attachment to the medial femoral condyle in 15 specimens. However, connections with the medial head of the gastrocnemius were not found in any of the explored specimens.
Laterally, the OPL was shown to be attached to the medial border of the lateral femoral condyle in most studies (1, 8, 11). Connections with the plantaris and fabella were also observed in previous studies (8). The present study found connections with the plantaris in only three specimens, but no extension to the fabella was documented. Connections between the OPL and plantaris may have functional repercussions, as suggested by Hedderwick et al, who have also reported a thin band of fibres from the OPL projecting towards the anterior aspect of the popliteus in nine (45%) specimens (8). The present study documents this popliteal extension in 12 specimens. Laprade et al found a similar band of fibres passing to the posterior aspect of the tibia, but did not coin this extension as passing to the popliteus (1).
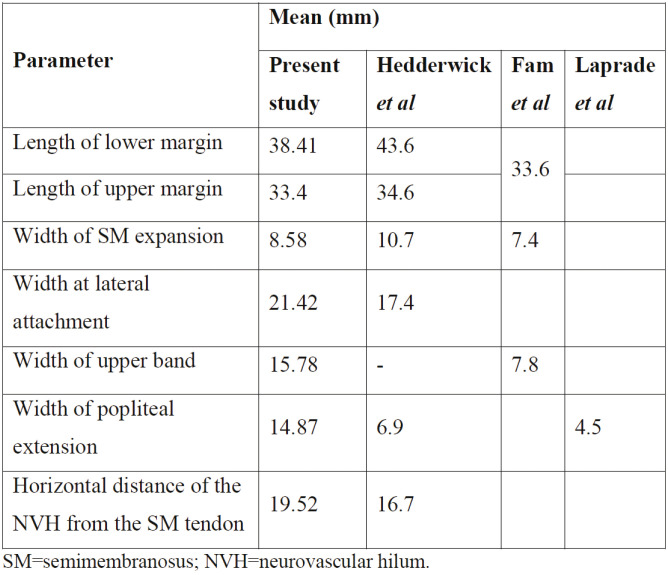
In the present study, the length of the lower margin of the OPL was shorter than that reported by Hedderwick et al (8) However, the lengths of the upper margin of the OPL were almost similar in the two studies. Fam et al measured the length of the OPL along both its middle and upper and lower margins (11). The width of SM expansion recorded by Hedderwick et al was higher, whereas that recorded by Fam et al was lower as compared to the present study (8, 11). In the present study, the width of the lateral attachment of the OPL was larger than that measured by Hedderwick et al (8). The width of popliteal extension was lower in the studies done by Hedderwick and Laprade (1, 8) as compared to the present study (Table 2).
Fam et al dissected 11 knees to measure the anatomical structure and relationships of OPL. They confirmed the role of OPL in controlling the knee hyperextension due to soft tissue recurvatum. Hyperextension affects walking, especially on uneven surfaces (11). Morgan et al (2010) performed a study exploring the biomechanics of the knee joint, in which they sectioned the structures on the posterior aspect of the knee joint one by one, and they found that the maximum degree of hyperextension occurred when the OPL was cut (9). The OPL serves as the main structure that prevents genurecurvatum. Therefore, this study is an attempt to understand the contribution of OPL in stabilizing the posterior knee.
Many scientists have attributed the rarity of studies on OPL to the paucity of the current literature on its reconstruction. However, the authors of the present study do not feel dissuaded as anatomical studies on OPL are imperative for understanding the functional implications of the SM complex. Another obstacle in the OPL investigative studies is that there is no authentication on the morphometry of the OPL or detailed description of its expansions. Therefore, this novel, yet simple, nomenclature describes the various attachments of the OPL. This classification of OPL anatomy into four types has been done for the first time and none of the previous studies has attempted such an anatomical description.
The morphology, attachments and dimensions of the OPL are of paramount importance in surgeries involving the posterior knee joint capsule. In tibial inlay reconstruction technique for the posterior cruciate ligament rupture, posterior knee capsulotomy is done, in which OPL resection is performed (12, 13). A detailed anatomical knowledge of the OPL and its extensions is mandatory for knee surgery in all patients to avoid postoperative complications. The adequacy of the current anatomical investigation of the OPL may facilitate the management of trauma in the posterior knee.
CONCLUSION
The morphology and attachments of the OPL are subject to variations. The anatomical details of the OPL outlined in the present study will lead to a better understanding of the biomechanical role of the OPL in supporting the posterior knee capsule and derangement of function due to trauma. Also, this knowledge will help knee surgeons while operating on the posterior aspect of the knee to optimize functional outcome after surgery
Conflicts of interest: none declared.
Financial support: none declared.
FIGURE 1.
Posterior view of the left knee with OPL morphometric parameters indicated by numbers: 1) length of the lower margin; 2) length of the upper margin; 3) width of the semimembranous (SM) tendon expansion; 4) width at the lateral attachment; 5) width of the upper band; and 6) horizontal distance of the neurovascular hilum (NVH) from the SM tendon
FIGURE 2.
Posterior view of the left knee to show type 1 OPL
FIGURE 3.
Posterior view of the left knee depicting type 2 OPL with an extension to the anterior surface of the popliteus
FIGURE 4.
Posterior view of the left knee depicting type 2 OPL with its lateral attachment confluent with the origin of the plantaris
FIGURE 5.
Posterior view of the right knee depicting type 3 OPL
FIGURE 6.
Posterior view of the left knee depicting type 4 OPL
TABLE 1.
Mean and standard deviation of OPL morphometric parameters
TABLE 2.
Summary of OPL measurements in the present study in comparison with those of previous studies
Contributor Information
Vandana MEHTA, Director Professor and Head, Department of Anatomy, Vardhman Mahavir Medical College and Safdarajung Hospital, New Delhi, India.
Pooja DAWANI, Assistant Professor, Department of Anatomy, Subharti Medical College and associated Chattrapati Shivaji Subharti Hospital, Meerut, UP, India.
Prabhat GOEL, Professor, Department of Anatomy, Vardhman Mahavir Medical College and Safdarajung Hospital, New Delhi, India.
References
- 1.LaPrade RF, Morgan PM, Wentorf FA, et al. The anatomy of the posterior aspect of the knee. An anatomic study. J Bone Jt Surg Am. 2007;89:758–764. doi: 10.2106/JBJS.F.00120. [DOI] [PubMed] [Google Scholar]
- 2.Beltran J, Matityahu A, Hwang K, et al. The distal semimembranosus complex: normal MR anatomy, variants, biomechanics and pathology. Skeletal Radiol. 2003;32:435–445. doi: 10.1007/s00256-003-0641-1. [DOI] [PubMed] [Google Scholar]
- 3.Robinson JR, Sanchez-Ballester J, Bull a MJ, et al . The posteromedial corner revisited. J Bone Joint Surg. 2004;86:674–681. doi: 10.1302/0301-620x.86b5.14853. [DOI] [PubMed] [Google Scholar]
- 5.Bejui J, Walch G, Gonon GP, et al. Anatomical and functional study on the musculus semimembranosus. Anat Clin. 1984;6:215–223. doi: 10.1007/BF01784316. [DOI] [PubMed] [Google Scholar]
- 6.Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am. 1979;61:56–62. [PubMed] [Google Scholar]
- 7.Loredo R, Hodler J, Pedowitz R, et al. Posteromedial corner of the knee: MR imaging with gross anatomic correlation. Skeletal Radiol. 1999;28:305–311. doi: 10.1007/s002560050522. [DOI] [PubMed] [Google Scholar]
- 8.Hedderwick M, Stringer MD, McRedmond L, et al. The oblique popliteal ligament: an anatomic and MRI investigation. Surg Radio Anat. 2017;39:1017–1027. doi: 10.1007/s00276-017-1838-7. [DOI] [PubMed] [Google Scholar]
- 9.Morgan PM, LaPrade RF, Wentorf FA, et al. The role of the oblique popliteal ligament and other structures in preventing knee hyperextension. Am J Sports Med. 2010;38:550–557. doi: 10.1177/0363546509348742. [DOI] [PubMed] [Google Scholar]
- 10.Wu XD, Yu JH, Zou T, et al. Anatomical characteristics and biomechanical properties of the oblique popliteal ligament. Sci Rep. 2017;42698 doi: 10.1038/srep42698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fam LPD, Fruheling VM, Pupim B, et al. Oblique popliteal ligament—an anatomical study. Rev Bras Ortop. 2013;48:402–405. doi: 10.1016/j.rboe.2012.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park SE, Stamos BD, DeFrate LE, et al. The effect of posterior knee capsulotomy on posterior tibial translation during posterior cruciate ligament tibial inlay reconstruction. Am J Sports Med. 2004;32:1514–1519. doi: 10.1177/0363546504265594. [DOI] [PubMed] [Google Scholar]
- 13.Seo SS, Seo JH, Kim do H, Park BY. Compression of the popliteal artery after posterior cruciate ligament reconstruction using the tibial inlay technique. Knee Surg Relat Res. 2015;27:27427. doi: 10.5792/ksrr.2015.27.4.274. [DOI] [PMC free article] [PubMed] [Google Scholar]