Abstract
The modern principles in pelvic surgery imply the preservation of the nervous structures that are involved in the physiological functioning of the pelvic and genital organs. The main pelvic nervous element is represented by the inferior hypogastric plexus. This plexus receives sympathetic afferent fibres from the hypogastric nerve, parasympathetic afferent fibres from the pelvic splanchnic nerves and also sympathetic afferent fibres coming from the sympathetic sacral chain via the sacral splanchnic nerves. We aimed to demonstrate the anatomy of these structures through dissection and we exposed the origins, pathway and manner of distribution of the splanchnic nerves of the pelvis. We managed to clarify the main anatomical relations of these nerves, among which we highlighted the relation to the branches of the internal iliac artery. The parasympathetic fibres reach the pelvis by running through the anterior rami of the spinal nerves, which are the origin of the sacral plexus. We managed to exhibit the way in which the parasympathetic fibres emerge from the sacral nerves and form the pelvic splanchnic nerves. Pelvic surgery nowadays is focused on nerve-sparing, which essentially means the conservation of the integrity of splanchnic nerves, hypogastric nerves and inferior hypogastric plexuses in order to maintain the normal functioning of the anatomical sphincters and genital organs. In this respect, it is crucial for the surgeon who performs pelvic procedures to be more than well-acquainted to the anatomy of the pelvic splanchnic nerves, which are considered to be the erectile nerves, and to that of the sacral splanchnic nerves.
Keywords:pelvic autonomic nervous system, inferior hypogastric plexus, pelvic sacral nerves, sacral splanchnic nerves.
INTRODUCTION
In ample pelvic surgeries (for example, in rectal resections and Wertheim’s radical hysterectomy) there is a considerable risk of damage to the nervous structures in this region. This operative incident is followed by disfunctions concerning the sexual activity and the functioning of the urinary and digestive sphincters (1, 2). Thus, the identification and conservation of the inferior hypogastric plexus and its pelvic afferences (i.e., the sacral and pelvic splanchnic nerves) is a matter of great importance.
The aforementioned nervous structures lie deep into the pelvis, in the pelvisubperitoneal space, where they are surrounded by an adipose- connective tissue atmosphere that makes their surgical exposure and, consecutively, protection, extremely difficult to achieve. The inferior hypogastric plexus is comprised of a vast network of nervous anastomoses and represents the ending of the hypogastric nerve. The latter is located pararectally and contains sympathetic fibres that originate in the abdomen and pass through the superior hypogastric plexus (3, 4). The parasympathetic component arises from the pelvic parasympathetic nucleus, S2-S4. The axons of the pelvic parasympathetic nucleus neurons join the somatic fibres of the sacral nervous plexus and enter the pelvis via these branches. Distal to the emergence of the anterior rami of the plexus through the anterior sacral foramina, the parasympathetic fibres exit the S2, S3 and S4 somatic nerves and then form the pelvic splanchnic nerves (5). These (usually three) nerves run towards and enter the inferior hypogastric plexus. The pelvic splanchnic nerves play a crucial role in the physiology of the erection and thus, they are named Eckhardt’s erector nerves (nervi erigentes) (6, 7).
Prediabetes is an intermediate stage between normal carbohydrate metabolism and T2D. This term includes two potentially overlapping groups: individuals with impaired fasting glucose (IFG) disorder, defined as a serum fasting glucose between 100-125 mg/dL (5.6-6.9 mmol/L), and individuals with impaired glucose tolerance (IGT), defined as serum fasting glucose concentration between 140-199 mg/dL (≥ 7.8 to < 11.0 mmol/L) two hours after a load with 75 g of glucose per os (13). Prediabetes is associated with presence of resistance in peripheral tissues to the action of insulin as well as dysfunction of pancreatic beta cells, disorders that occur before changes in glucose levels become detectable. Patients with essential hypertension have an increased prevalence of tissue insulin resistance (11, 12) and a 2.5 times higher risk of developing T2D compared to normotensive individuals (7). There is evidence that among antihypertensive treatment options, RAS blockers play an important role in prevention of new-onset T2D (14-16), CCBs have a neutral effect, while β-blockers and thiazide diuretics increase the risk of T2D (15, 16).
Beside the lumbo-abdominal sympathetic afferences, the inferior hypogastric plexus also receives fibres coming from the sacral paravertebral sympathetic chain. The nervous fibres stem from the sacral ganglia and form the sacral splanchnic nerves that also enter the inferior hypogastric plexus (8, 9).
MATERIALS AND METHODS
Dissections on seven female formalin-preserved cadavers were conducted by us in the Anatomy laboratory of the Faculty of Medicine, „Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania. The preservation was done by injection of the cadavers with 9% formalin solution and consequent immersion in a same-concentration formalin bath for 30 days. We sectioned the pelvises in a parasagittal plane and dissected them in anatomical planes. We captured photographs of the dissections and digitally processed them without altering the anatomical aspects.
Cadaver manipulation was done according to the Romanian law no. 104/27.03.2003 (republished), which allows the Departments of Anatomy of Faculties of Medicine in Romania to receive cadavers for scientific research use that have been abandoned and not claimed by any relatives, as ascertained by a formal investigation.
In Figure 1, at the level of the greater ischiadic notch, we can observe the fibres of the pyriformis muscle, among which the rami of the sacral plexus is passing. The ischiadic notch is turned into an orifice by the insertion of the sacro- ischiadic ligament on the ischiadic spine. The posterior trunk of the internal iliac artery divides into three arteries: the superior gluteal artery, inferior gluteal artery (which gives off the lateral sacral artery) and internal pudendal artery. The internal pudendal artery exits the pelvis along with the pudendal nerve, passing in contact with the ischiadic spine and with the superior edge of the sacro-ischiadic ligament. On the lateral aspect of the sacrum, the sacral sympathetic paravertebral chain passes in a cranio-caudal direction. In the lower part of the picture, the inferior hypogastric plexus is tractioned towards medial. The plexus receives recurrent branches that stem from the pudendal nerve.
In Figure 2, the hypogastric nerve becomes visible in the pelvisubperitoneal space by contralaterally pulling the rectum. The hypogastric nerve is the main inflow of sympathetic fibres into the inferior hypogastric plexus. The sacral sympathetic paravertebral chain descends on the anterior surface of the sacrum, medial to the sacral foramina. The sacral plexus and the pyriformis muscle (previously highlighted in Figure 1) are covered by the pelvic parietal fascia. Laterally to the sympathetic chain, the origins of the pelvic splanchnic nerves are visible. Data from the literature point out that these nerves originate from the S2, S3 and S4 sacral nerves. Despite this, we have observed nervous fascicles with a similar distribution, originating, though, in the S1-S2 and S5 nerves. These nerves penetrate the pelvic parietal fascia and, after a short trajectory of about 2 centimetres through the pelvisubperitoneal space, they end up by anastomosing with the inferior hypogastric plexus. It shall also be underlined that the pelvic splanchnic nerves are applied to the pelvic wall and shaped according to it. In our image, they can be seen in a sagittal plane, due to the fact that they have first been isolated and then detached from the pelvic wall by tractioning the hypogastric nerve and the inferior hypogastric plexus towards medial.
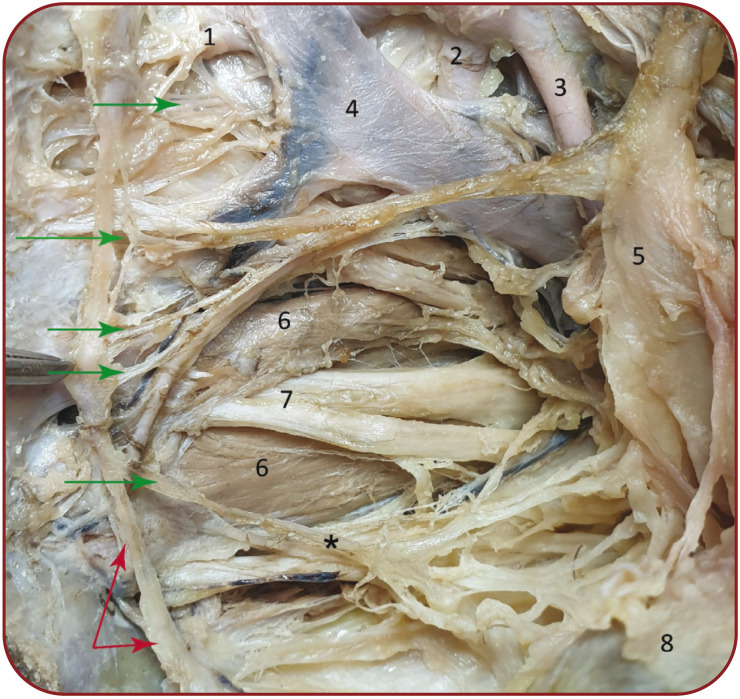
Given the importance of anatomical landmarks for both anatomists and surgeons, we would like to first emphasize the location of the superior and inferior gluteal arteries and the internal pudendal arteries that form the deep arterial plane at the level of the greater ischiadic notch. The superficial vascular plane is represented by the internal iliac vein. In the centre of the image illustrated by Figure 3, the S2, S3 and S4 branches of the sacral plexus can be observed, as they intertwine with the pyriformis muscle fibre and head towards their exit from the pelvis, at the level of the greater ischiadic notch. The hypogastric nerve and the inferior hypogastric plexus are tractioned towards superior and medial.
The sacral sympathetic chain descends on the anterior aspect of the sacrum. At this level, the sacral sympathetic ganglia are easy to identify. From these ganglia, narrow nerve fibres emerge and variably form anastomoses, forming the sacral splanchnic nerves. These nerves ultimately enter the inferior hypogastric plexus. However, there are also fibres from the S3 sympathetic ganglion that head directly towards the rectum.
DISCUSSION
For the pelvic splanchnic nerves, the first neuron is found at the level of the pelvic parasympathetic nucleus, at the level of the spinal cord S2-S4 (10). The preganglionic fibres are attached to the trunks of the spinal nerves S2-S4, from which then they emerge after the sacral nerves exit through the anterior sacral foramina (11). After running through the pelvic parietal fascia, the preganglionic axons go into the pelvic splanchnic nerves and enter the inferior hypogastric plexus, where they form the synapse with the second neuron on the pathway. The postganglionic fibres approach the target organs and, in the case of the genital innervation, as the cavernous or clitoral nerves, the fibres get to the penis or, respectively, the clitoris (12, 13).
Concerning the sacral splanchnic nerves, the trajectory is slightly more complicated. The first neuron is found in the lateral horns of the L1-L2 segment of the spinal cord. The preganglionic axons arrive into the laterovertebral sympathetic chain, through which they pass towards inferior, down to the level of the sacral ganglia. Some of the fibres synapse with the second neuron, located in the paravertebral ganglia. Their corresponding postganglionic fibres enter the sacral nerves via the grey communicating rami and extend up to the skin (14). Other preganglionic fibres give rise to the sacral splanchnic nerves, which enter the inferior hypogastric plexus, where they synapse with the second neuron. Their respective postganglionic fibres head towards the pelvic and genital organs, either directly, via branches of the plexus, or via the perivascular plexuses (15).
We managed to highlight narrow branches that behave similarly to the sacral splanchnic nerves but emerge from the other branches of the sacral plexus. Indeed, though, the S2, S3 and S4 are the best represented. Intraoperatively, by tractioning the parietal peritoneum, the surgeon can identify the posterior edge of the inferior hypogastric plexus and the sacral splanchnic nerves. Applying traction to the peritoneum is a surgical gesture that is paramount, should the identification and isolation of the splanchnic nerves and of the inferior hypogastric plexus be aimed for (16).
We would like to point out that there are two regional vascular planes that are located between the origins of the inferior hypogastric plexus and the pelvic wall. The deep plane is represented, as we managed to demonstrate, by the posterior branches of the internal iliac artery, whereas the superficial plane is formed by the internal iliac vein and its branches. Basically, the nervous structures that we set out to feature are located between the pelvic vessels and the peritoneum.
CONCLUSION
The inferior hypogastric plexus and the splanchnic nerves are located deep inside the pelvis, postero-laterally to the rectum, in the pelvisubperitoneal space. Essentially, the space where these nervous structures can be identified and isolated is located on the anterior aspect of the sacrum, in close relation to the origins of the pyriformis muscle and the origins of the sacral plexus branches. The risk area (i.e., the area where the splanchnic nerves can be damaged) extends laterally up to the ramification point of the internal iliac artery, and medially up to the sacral sympathetic chain. The easiest to identify are the pelvic splanchnic nerves S2 and S3. By applying traction to the peritoneum and to the hypogastric nerve, the pelvic splanchnic nerves can be detached from the pelvic wall and can be positioned in a sagittal plane that allows for their extrication and, thus, protection, which is a vital aspect during pelvic surgery.
We also demonstrate the existence of nerve fibres that have a similar behaviour to that of the pelvic splanchnic nerves but originate at the level of the sacral trunks of S1-S2 and S5.
Regarding the sacral splanchnic nerves, we found, as well, a sympathetic fibre fascicle that emerges from the sacral sympathetic chain and reaches the rectum directly, without passing through the inferior hypogastric plexus at all.
During laborious pelvic surgeries that necessitate large resections or lymph node dissections, it is essential to protect the splanchnic nerves. In this respect, we believe that this study brings clarity in the systematization of the splanchnic nerves, their location and relations, by using both crucial and accessible anatomical landmarks.
Conflicts of interest: none declared.
Financial support: none declared.
Authorship: All authors contributed equally to this material.
FIGURE 1.
Arterial and nervous structures at the level of the greater ischiadic notch – left medial view. 1-5: anterior branches of the sacral nerves, immediately after their emergence through the anterior sacral foramina; 6: left inferior hypogastric plexus; 7: sacro-ischiadic ligament; 8: left superior gluteal artery; 9: left inferior gluteal artery; 10: left internal pudendal artery; 11: left sympathetic sacral chain; 12: left internal iliac artery. The red dotted line shows the border of the greater ischiadic notch
FIGURE 2.
The inferior hypogastric plexus and the pelvic splanchnic nerves (erectile nerves) – left medial view. 1: left internal iliac artery; 2: left hypogastric nerve; 3: pelvic parietal fascia; 4: left inferior hypogastric plexus; 5: rectum, pulled towards antero-medial; 6: left sacral sympathetic paravertebral chain. The red arrows point towards the left pelvic splanchnic nerves.
FIGURE 3.
The sacral splanchnic nerves – origin, distribution, relations – left medial view. 1: sacral branch from the left superior gluteal artery; 2: left inferior gluteal artery; 3: left internal pudendal artery; 4: left internal iliac vein; 5: left inferior hypogastric plexus; 6: origins of the pyriformis muscle, ran through by the radices of the sacral plexus; 7: bifurcation of the anterior branch of the S3 nerve; 8: rectum; *branch that goes directly towards the rectum, without passing through the inferior hypogastric plexus. The green arrows point towards the sacral splanchnic nerves, and the red arrows towards the sacral sympathetic paravertebral chain.
Contributor Information
Ofelia-Costina GOIDESCU, Doctoral School, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Iulian-Alexandru DOGARU, Doctoral School, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Discipline of Anatomy, Department of Morphological Sciences, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Mihaly ENYEDI, Discipline of Anatomy, Department of Morphological Sciences, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Octavian ENCIU, Department of Surgery, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Daniela-Elena GHEOCA MUTU, Discipline of Anatomy, Department of Morphological Sciences, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
Florin-Mihail FILIPOIU, Discipline of Anatomy, Department of Morphological Sciences, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania.
References
- 1.Alkatout I, Wedel T, Pape J, et al. Review: Pelvic nerves – From anatomy and physiology to clinical applications. Transl Neurosci. 2021;12:362–378. doi: 10.1515/tnsci-2020-0184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daniels IR, Woodward S, Taylor FGM, et al. Female urogenital dysfunction following total mesorectal excision for rectal cancer. World J Surg Oncol. 2006;4 doi: 10.1186/1477-7819-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beveridge TS, Johnson M, Power A, et al. Anatomy of the nerves and ganglia of the aortic plexus in males. J Anat. 2015;226:93–103. doi: 10.1111/joa.12251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maas CP, Kenter GG, Trimbos JB, Deruiter MC. Anatomical basis for nerve-sparing radical hysterectomy: Immunohistochemical study of the pelvic autonomic nerves. Acta Obstet Gynecol Scand. 2005;84:868–874. doi: 10.1111/j.0001-6349.2005.00742.x. [DOI] [PubMed] [Google Scholar]
- 5.Haroun HS. Clinical anatomy of the splanchnic nerves. MOJ Anat Physiol. 2018;5:87–90. [Google Scholar]
- 6.Mauroy B, Demondion X, Bizet B, et al. The female inferior hypogastric (= pelvic) plexus: anatomical and radiological description of the plexus and its aVerences—applications to pelvic surgery. Surg Radiol Anat. 2007;29:55–66. doi: 10.1007/s00276-006-0171-3. [DOI] [PubMed] [Google Scholar]
- 7.Eckhard C. Ueber den Verlauf der Nervi erigentes innerhalb des Rückenmarks und Gehrirns. In: Beitr Anat etc. 1873;7:67–80. [Google Scholar]
- 8.Aurore V, Röthlisberger R, Boemke N, et al. Anatomy of the female pelvic nerves: a macroscopic study of the hypogastric plexus and their relations and variations. J Anat. 2020;237:487–494. doi: 10.1111/joa.13206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCausland C, Sajjad H. Anatomy, Back, Splanchnic Nerve. StatPearls, 2021. [PubMed]
- 11.Kale A, Basol G, Usta T, Aytuluk HG. Laparoscopic evaluation of female pelvic neuroanatomy and autonomic plexuses in terms of gynecologic perspective. J Endometr Pelvic Pain Disord. 2018;10:216. [Google Scholar]
- 12.Andersson KE, Hedlund P, Alm P. Sympathetic pathways and adrenergic innervation of the penis. Int J Impot Res. 2000;12:S5–S12. [PubMed] [Google Scholar]
- 13.Baader B, Herrmann M. Topography of the pelvic autonomic nervous system and its potential impact on surgical intervention in the pelvis. Clin Anat. 2003;16:119–130. doi: 10.1002/ca.10105. [DOI] [PubMed] [Google Scholar]
- 14.Sharabi AF, Lui F. Anatomy, Abdomen and Pelvis, Splanchnic Nerves. StatPearls, 2021. [PubMed]
- 15.Shiozawa T, Huebner M, Hirt B, et al. Nerve-preserving sacrocolpopexy: Anatomical study and surgical approach. Eur J Obstet Gynecol Reprod Bio. 2010;152:103–107. doi: 10.1016/j.ejogrb.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Kim NK, Kim YW, Cho MS. Total mesorectal excision for rectal cancer with emphasis on pelvic autonomic nerve preservation: Expert technical tips for robotic surgery. Surg Oncol. 2015;24:172–180. doi: 10.1016/j.suronc.2015.06.012. [DOI] [PubMed] [Google Scholar]