Abstract
Background:
Regaining preinjury levels of activity and progressing rehabilitation factors after anterior cruciate ligament (ACL) reconstruction have shown mixed results.
Purpose:
To evaluate the timing and rate of return for knee range of motion (ROM), stability, strength, and subjective scores after ACL reconstruction with contralateral patellar tendon graft (PTG).
Study Design:
Case series; Level of evidence, 4.
Methods:
Included were 2148 patients (1238 male patients, 910 female patients) who underwent primary ACL reconstruction with a contralateral PTG between 1995 and 2017 and had complete objective data through 3 months of follow-up. All patients participated in a rehabilitation program specific to goals for each knee. Patients were evaluated objectively with goniometric measurement of ROM, isokinetic quadriceps strength testing, and laxity with a KT-2000 arthrometer. Subjective data were collected at 2 and 5 years.
Results:
Normal extension on the reconstructed knee was attained for 95% of patients at 1 week postoperatively; normal flexion on the reconstructed knee was reached by 77% of patients by 3 months. At 3 months postoperatively, mean limb symmetry index strength was 104%, and the strength on the ACL-reconstructed and graft-donor knees was 87% and 86% of their respective preoperative strength. Mean manual maximum side-to-side difference in laxity was 2.0 mm at 1 month. Most patients (90%) returned to level 8 sports or higher and did so at an average of 5.7 months. Mean International Knee Documentation Committee scores for the ACL-reconstructed and graft-donor knees were 89 and 91 at 2 years (n = 1015 patients) and 84 and 90 at 5 years (n = 1275 patients), respectively. Mean Cincinnati Knee Rating Scale scores for the ACL-reconstructed and graft-donor knees were 92 and 96 at 2 years (n = 1184) and 88 and 94 at 5 years (n = 1236), respectively.
Conclusion:
For patients who underwent ACL reconstruction with a contralateral PTG, postoperative ROM and strength were restored quickly by splitting the rehabilitation into different goals between the two knees. Using a contralateral PTG, this structured rehabilitation plan can lead to a relatively quick return to sport and good subjective long-term outcomes.
Keywords: anterior cruciate ligament, rehabilitation, patellar tendon graft, long-term outcomes
Attaining preinjury function in regard to range of motion (ROM), strength, stability, and sports participation after an anterior cruciate ligament (ACL) reconstruction has, at times, shown to be difficult. 19,25 Studies show that ACL reconstructions can successfully restore stability in the long term, evident by adequate stability testing up to 20 years postoperatively. 8,17,28,46,59 However, patients can show a wide range of return to sports at the preinjury participation level, with rates ranging from 31% to 92%. 4,17,23,25 The reasons for this wide range have been related to graft type, surgical fixation, stiffness, quadriceps muscle weakness, 13,14,25,42 psychological readiness, and sex. 12,14,19,20,25,64 Given that 91% of patients expect to return to play at their preinjury level after surgery, determining strategies and factors that allow them to reach this goal should be the focus of orthopaedic surgeons and physical therapists treating patients with ACL tears. 16
It is well known that loss of knee extension after an ACL reconstruction is one of the most debilitating complications after surgery, yet it continues to occur at a fairly high rate, with an incidence ranging from 1.9% to 10.9%. 21,35,38 Regaining quadriceps muscle strength has also been difficult regardless of graft source, and when the involved leg is asymmetrically weak compared with the contralateral limb, this can lead to low levels of return to sport. 25,39,43 Knowing the progression and the rate at which patients achieve normal levels for these objective measures will allow clinicians to properly treat and counsel patients throughout the postoperative rehabilitation process.
In postoperative rehabilitation, the goal is to attain symmetry between knees in terms of ROM, strength, and stability. 10 The senior author (K.D.S.) has used the patellar tendon graft (PTG) solely for all ACL reconstructions because of its strength obtained from bone-to-bone healing; its lower risk for subsequent ACL reinjury, especially with young athletes; and its ability to allow patients who rehabilitate fully to return to sports at a high rate. 46,54 Ipsilateral PTGs were consistently used between 1982 and 1995, and patients were doing fairly well overall; however, some problems occurred with the donor site, including poor strength recovery and anterior knee pain, that needed to be addressed. Although the PTG provided excellent stability, rehabilitating the donor site was difficult early in the rehabilitation process because any intensive strengthening conflicted with the goals of limiting swelling and achieving full ROM. Insufficient rehabilitation of the donor site after surgery can lead to suboptimal results like anterior knee pain and quadriceps weakness. 15,64 Consequently, many other surgeons chose to abandon the PTG for other graft sources. 6
One way to restore symmetry after surgery is by performing an ACL reconstruction using a contralateral PTG. 10,45,56,57 We initially used a contralateral PTG with revision surgery, and our approach began to yield superior ROM and decreased swelling on the ACL-reconstructed knee as well as better quadriceps muscle strength return in the graft-donor knee when compared with the same measures for patients with an ipsilateral PTG. 55 However, the donor site on the contralateral side still showed some problems, and the rehabilitation on this side needed to be refined. It is possible for the patellar tendon donor site to regenerate to normal, but the donor site needs consistent stimulation for regrowth. More thought went into improving the rehabilitation on the graft-donor knee including attaining full ROM immediately after surgery and quickly starting low-resistance and high-repetition strength exercises to regenerate the patellar tendon. We consistently began using the contralateral PTG for primary ACL reconstruction in 1995. In an initial study of 434 patients by Shelbourne and Urch, 56 patients undergoing ACL reconstruction with a contralateral PTG were able to attain symmetric ROM and quadriceps muscle strength faster and returned to sports quicker compared with patients who received an ipsilateral PTG. Given the results found in this initial study, the senior author has performed primary ACL reconstructions predominantly using a contralateral PTG for >25 years.
The purpose of this study was to evaluate, in a large group of patients, the timing and rate of return of normal knee extension and flexion, stability, and quadriceps muscle strength after ACL reconstruction with a contralateral PTG. We also sought to determine the postoperative outcomes regarding return to sport rates, activity level, and subjective scores on the International Knee Documentation Committee (IKDC) and Cincinnati Knee Rating Scale (CKRS).
Methods
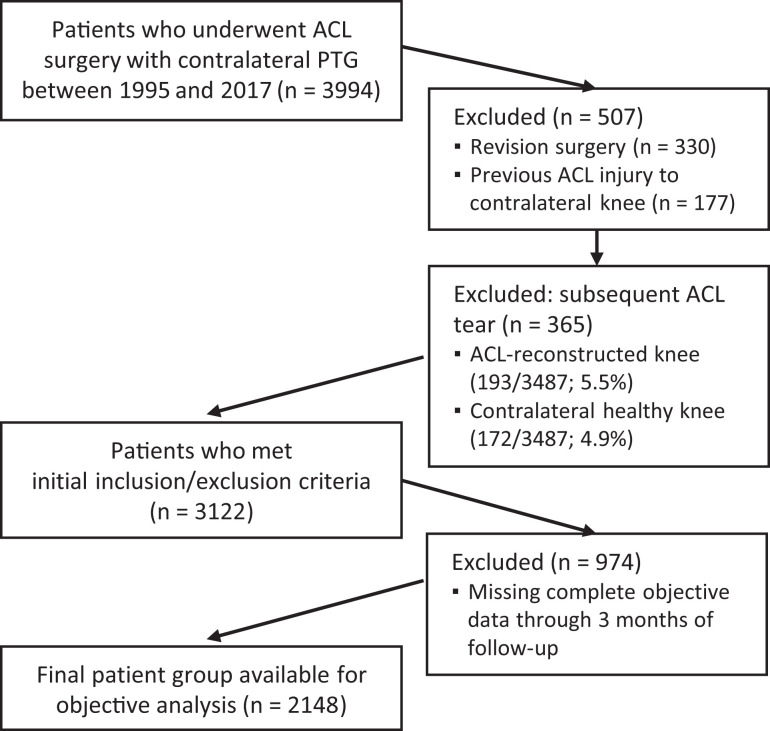
Primary ACL reconstruction with contralateral autogenous PTG was performed on 3994 patients between January 1995 and December 2017. All patients gave informed consent to participate in the study, and it was approved by the institutional review board at the institution where surgery was performed. Before undergoing surgery, patients were enrolled in a long-term prospective outcome study approved by the institutional review board at the participating hospital. We excluded patients who underwent revision ACL surgery (n = 330) and patients who had previous ACL injury to the contralateral knee (n = 177). Of the remaining 3487 patients, 193 experienced a subsequent ACL graft tear (5.5%) and 172 experienced a subsequent contralateral ACL tear (4.9%); these patients were excluded from the analysis. We required that patients have complete objective follow-up data through 3 months, of which 974 (31%) patients did not meet that requirement and were excluded. Ultimately, 2148 patients met the exclusion and inclusion criteria for analysis (Figure 1).
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flowchart of patient inclusion and exclusion process. ACL, anterior cruciate ligament; PTG, patellar tendon graft.
Surgical Procedure
The surgical technique for ACL reconstruction using a PTG from the contralateral normal knee has been described in detail previously. 56,57 A tourniquet was used on both knees during the surgery. The surgery was performed through a mini-arthrotomy to allow for the independent drilling of both the femoral and tibial tunnels. Of particular importance, the patellar and tibial defects caused by harvesting the graft were packed with bone graft that was obtained from drilling the femoral and tibial tunnels. When appropriate, a notchplasty was performed to accommodate the 10-mm graft. The patellar tendon defect was closed with a No. 1 vicryl suture, after which the ACL-reconstructed knee was put through full knee ROM, compared with the contralateral knee, from full hyperextension to flexion with the heel touching the buttock. Achieving full hyperextension at the time of surgery ensures that the patient can achieve full hyperextension the night of surgery. Patients stayed in the hospital overnight, and a perioperative pain management program was used, which has been described previously. 53
Rehabilitation
A summary of the perioperative rehabilitation program that was prescribed is shown in Appendix Table A1; it has also been described in detail elsewhere. 10,48,52,56 The purpose of using a contralateral PTG was to divide conflicting rehabilitation goals between knees. The early goals for each knee were quite different; activities in the graft-donor knee were aimed at restoring strength, whereas the focus for the ACL-reconstructed knee was to control a hemarthrosis and recover full ROM.
Rehabilitation was provided by a staff of physical therapists who worked directly with the physicians, whose orthopaedic practice is limited to the knee only and has a high volume of ACL reconstructions. Patients were treated by the same physical therapist throughout the rehabilitation process before and after surgery for consistency and to control for any potential problems.
Data Collection
Patient demographic characteristics and details of surgery were prospectively collected and entered into a database. Patients were seen at routine intervals for patient care and rehabilitation, where objective data were collected. Evaluation was performed by physical therapists who had extensive experience with knee rehabilitation and testing procedures. Knee ROM was evaluated on both knees with the patient in a long-sitting position, and it was measured with a goniometer as described by Norkin and White. 37 Knee extension was evaluated with the patient’s heel elevated on a bolster to allow the knee to go into hyperextension, if present. Knee flexion was measured with the patient in a long-sitting position and by having the patient bend the knee as far as possible toward the buttock. According to IKDC objective evaluation criteria, normal knee extension is considered to be within 2° of the opposite normal knee and normal flexion is considered to be within 5° of the opposite normal knee. 1 We evaluated for the percentage of patients who achieved normal knee extension and normal flexion at each time postoperatively. Objective knee stability was evaluated with a KT-2000 arthrometer (MEDmetric). The manual maximum difference, in millimeters, between knees was used for analysis.
Quadriceps muscle strength was evaluated at 1, 2, 3, and 6 months postoperatively, using isokinetic testing (Cybex dynamometer; Lumex) at 60 deg/s and 180 deg/s. The mean postoperative isokinetic strength was calculated using 3 formulas as shown in Table 1. We also evaluated the percentage of patients who achieved ≥90% strength compared with their preoperative normal value at each time postoperatively.
Table 1.
Formulas for Calculating Quadriceps Muscle Strength
| Strength Evaluation | Calculation to Obtain Percentage Strength Value |
|---|---|
| % Strength of involved knee | |
| ACL-reconstructed knee strength | |
| Graft-donor knee strength |
Subjective evaluation was performed using the CKRS and the IKDC subjective surveys. 1,7 An activity rating survey was sent to patients yearly after surgery, and we obtained the highest rating a patient achieved postoperatively. 50 For this activity rating scale, high-risk sports such as basketball, soccer, and football played at the professional or college level are defined as level 10, the school-age level is defined as level 9, and the recreational level is defined as level 8. 50 Patients were also sent a survey at 4, 6, 9, 12, and 13 months after surgery that asked, “At what time (in months) after surgery did you return to full sports/activities and at full capability?” If the survey was returned and the patient responded with the option of “I have not returned to sports at full capability yet,” the survey was sent again at the next interval; the survey was stopped being sent when the patient confirmed a return to full sports activity.
Descriptive statistics were obtained, and objective data were analyzed for all patients at 1, 2, and 3 months after surgery as well as at 6 months for those available. Any available subjective data for patients meeting the criteria for objective follow-up were used for analysis.
Results
Of the 2148 patients meeting criteria for this study, the mean age was 24.3 ± 10.1 years (range, 12.0-71.0 years). The mean age for female patients (n = 910) was 22.1 ± 9.8 years (range, 12.4-71.0 years). The mean age for male patients (n = 1238) was 25.9 ± 9.9 years (range, 12.0-64.2 years).
The mean ROM for extension, flexion, and difference between knees for extension and flexion through 6 months postoperative is shown in Table 2. Normal extension (within 2° of normal knee) was achieved for 95% of patients at 1 week, 96% at 2 weeks, and 98% at 1 month postoperatively. Normal flexion (within 5° of noninvolved knee) was achieved by 49% of patients at 2 months, 77% at 3 months, and 89% at 6 months postoperatively.
Table 2.
Range of Motion From 1 Week Through 6 Months Postoperatively a
| Time Postoperatively | ||||||
|---|---|---|---|---|---|---|
| 1 wk | 2 wk | 1 mo | 2 mo | 3 mo | 6 mo b | |
| Extension c | 5 ± 3 | 5 ± 3 | 5 ± 3 | 5 ± 2 | 5 ± 3 | 5 ± 2 |
| Flexion | 109 ± 14 | 121 ± 12 | 132 ± 11 | 139 ± 8 | 144 ± 7 | 146 ± 7 |
| Difference: extension | 0 ± 1 | 0 ± 1 | 0 ± 1 | 0 ± 2 | 0 ± 1 | 0 ± 1 |
| Difference: flexion | –31 ± 16 | –23 ± 14 | –15 ± 11 | –8 ± 8 | –4 ± 5 | –2 ± 5 |
a Data are reported as mean ± SD.
b n = 1503.
c Positive value represents degree of hyperextension.
The manual maximum difference in laxity between knees, as measured with the KT-2000 arthrometer, was 2.0 ± 1.4 mm at 1 month postoperatively, and stability was maintained through time (Table 3).
Table 3.
Objective Stability Values as Measured With KT-2000 Arthrometer
| Time Postoperatively | |||||
|---|---|---|---|---|---|
| 1 mo | 2 mo | 3 mo | 6 mo a | 2 y b | |
| Laxity, manual maximum difference, mean ± SD | 2.0 ± 1.4 | 1.9 ± 1.3 | 2.0 ± 1.5 | 2.0 ± 1.5 | 1.9 ± 1.4 |
| Laxity, % of patients | |||||
| ≤3 mm | 91 | 92 | 90 | 90 | 90 |
| 4-5 mm | 8 | 7 | 8 | 8 | 8 |
| >5 mm | 1 | 1 | 2 | 2 | 2 |
a n = 1471.
b n = 674.
Isokinetic testing of quadriceps muscle strength showed that the mean percentage strength of the involved knee compared with the noninvolved knee at 3 months postoperatively was 104% for the 180 deg/s speed and 115% for the 60 deg/s speed. More important, when compared with the preoperative normal baseline measurement, the mean strength of the ACL-reconstructed knee was 87% for the 180 deg/s speed and 79% for the 60 deg/s speed and the mean strength of the graft-donor knee was 86% for the 180 deg/s speed and 71% for the 60 deg/s speed at 3 months after surgery (Table 4). The percentage of patients who achieved strength ≥90% of their preoperative normal value by 6 months postoperatively was 64% for the ACL-reconstructed knee for the 180 deg/s speed and 47% for the 60 deg/s speed. For the graft-donor knee at the same time point, 61% achieved strength ≥90% for the 180 deg/s speed and 30% for the 60 deg/s speed.
Table 4.
Isokinetic Testing of Quadriceps Muscle Strength a
| Time Postoperatively | ||||
|---|---|---|---|---|
| Isokinetic test | 1 mo | 2 mo | 3 mo | 6 mo b |
| 180 deg/s speed | ||||
| % Strength of involved kneec | 113 ± 37 | 105 ± 25 | 104 ± 24 | 104 ± 20 |
| ACL-reconstructed knee strength | 60 ± 18 | 76 ± 21 | 87 ± 24 | 99 ± 29 |
| Graft-donor knee strength | 56 ± 18 | 75 ± 21 | 86 ± 21 | 97 ± 23 |
| 60 deg/s speed | ||||
| % Strength of involved kneec | 150 ± 59 | 123 ± 39 | 115 ± 33 | 114 ± 27 |
| ACL-reconstructed knee strength | 55 ± 18 | 70 ± 20 | 79 ± 22 | 90 ± 26 |
| Graft-donor knee strength | 40 ± 15 | 60 ± 17 | 71 ± 19 | 82 ± 21 |
| Patients within 10% difference between knees, % | ||||
| 180 deg/s speed | 30 | 38 | 47 | 52 |
| 60 deg/s speed | 15 | 25 | 33 | 40 |
| Patients with ≥90% strength vs preoperative normal value, % | ||||
| ACL-reconstructed knee | ||||
| 180 deg/s speed | 5 | 22 | 42 | 64 |
| 60 deg/s speed | 3 | 13 | 27 | 47 |
| Graft-donor knee | ||||
| 180 deg/s speed | 3 | 19 | 39 | 61 |
| 60 deg/s speed | 0 | 5 | 15 | 30 |
a Data are reported as mean ± SD or % of patients.
b n = 1480.
c Calculated as % strength of involved knee.
Results of the activity rating survey showed that 90% of patients (1643/1830) returned to jumping and pivoting sports at the recreational level (level 8) or higher after surgery. Overall, 81% of patients (1486/1830) were able to return to their preinjury activity level after surgery. For patients involved in jumping and pivoting sports, the percentage who were able to return to their preoperative sport level was 67% for college and professional athletes, 70% for school-age athletes, and 88% for recreational athletes (Table 5). Of the 1222 patients responding to the survey regarding time of return to sport, the mean time patients reported that they returned to full sports at full capability was 5.7 ± 2.3 months after surgery. The mean subjective CKRS and IKDC scores at 2 and 5 years after surgery are shown in Table 6.
Table 5.
Preoperative Sport or Activity Level Compared With Maximum Activity Rating Achieved After Surgery
| Postoperative Level Achieved, n | |||||
|---|---|---|---|---|---|
| 10 | 9 | 8 | ≤7 | Achieved Preoperative Level or Higher, n (%) | |
| Preoperative level | |||||
| 10 (n = 137) | 92 | 5 | 31 | 9 | 92 (67.2) |
| 9 (n = 736) | 153 | 365 | 191 | 27 | 518 (70.4) |
| 8 (n = 684) | 38 | 43 | 522 | 81 | 603 (88.2) |
| ≤7 (n = 273) | 6 | 19 | 178 | 70 | 273 (100) |
| Total (n = 1830) | 289 | 432 | 922 | 187 | |
Table 6.
Subjective Survey Results a
| 2 y Postoperatively | 5 y Postoperatively | |||
|---|---|---|---|---|
| ACL-Reconstructed Knee | Graft-Donor Knee | ACL-Reconstructed Knee | Graft-Donor Knee | |
| n = 1015 | n = 1275 | |||
| IKDC | 88.6 ± 12.5 | 91.4 ± 11.4 | 84.3 ± 17.3 | 89.5 ± 14.4 |
| n = 1184 | n = 1236 | |||
| CKRS | 92.4 ± 9.6 | 95.6 ± 7.2 | 88.3 ± 14.6 | 94.1 ± 9.9 |
a Data are reported as mean ± SD. ACL, anterior cruciate ligament; CKRS, Cincinnati Knee Rating Scale; IKDC, International Knee Documentation Committee.
Discussion
The results of this study showed a clear progression for the timing and rate of return for normal knee extension and flexion, stability, and quadriceps muscle strength after ACL reconstruction using a contralateral PTG. Patients returned to jumping and pivoting sports at a high rate at around 6 months after surgery. Furthermore, subjective results showed that patients achieved normal values for both the ACL-reconstructed and graft-donor knees at 2 and 5 years postoperatively.
Previous studies have looked at ROM after an ACL reconstruction and its importance on outcomes; however, few have discussed its significance in the early postoperative phase and how this progresses over time. 11,36,44,47 One major benefit of using a contralateral PTG is allowing the patient to work on 2 different goals simultaneously, separated between the ACL-reconstructed knee and the graft-donor knee. 56 The main goal for the ACL-reconstructed knee is to achieve full ROM quickly, which was evident in this study as 95% of patients reached normal knee extension by 1 week after surgery. For knee flexion, patients progressed slowly due to joint swelling, although steadily, as 49% were normal at 2 months (139°) and 89% were normal at 6 months (146°). Similar to our study, Shelbourne and Urch 56 looked at the postoperative objective differences between patients having an ACL reconstruction with an ipsilateral PTG versus a contralateral PTG and found similar knee extension between the 2 groups; however, results showed better knee flexion in the contralateral group.
Stiffness after an ACL reconstruction has shown to be a relatively common and devastating complication, with an incidence rate ranging from 1.9% to 10.9%. 35 A recent systematic review found 2 risk factors for developing postoperative stiffness, one being extension loss in the early postoperative phase and the other being poor quadriceps muscle control. 35,58 Our results indicate that full knee hyperextension can be accomplished early, as 95% of the patients achieved normal extension by 1 week after surgery, which is higher than reported by previous studies on the topic. 31,35,36,44 Furthermore, this study compared knee extension loss to the high standard of within 2° of knee extension of the opposite normal knee, in line with established IKDC criteria. 1 Current studies use much less stringent criteria of achieving 0° extension, without regard to hyperextension, or 5° extension loss compared with the opposite normal knee. 38,60 Having less stringent criteria means that the true incidence of extension loss is likely much worse in other reports if it were compared with the IKDC criteria, as in our current study.
Attaining normal knee hyperextension early after surgery plays a large role in the patient achieving a good outcome, and this can be done only with proper fit and positioning of the graft. Given that the ACL is an intra-articular ligament, the relationship between the graft and the intercondylar notch needs to be understood and appreciated. When the knee is in full hyperextension, the ACL fits perfectly in the intercondylar notch, without impingement, allowing for full function including normal gait and the ability to gain strength. To accommodate a 10-mm graft, a notchplasty is often done to allow the graft to fit in the notch and allow full hyperextension, thus avoiding any postoperative complications like stiffness.
Attaining good quadriceps muscle strength has been shown to be linked to the ability to return to sport, proper biomechanics, and overall quality of life after an ACL reconstruction, yet this parameter is difficult to regain. 8,22,39 –41,43,63,65 Using a contralateral PTG provides a unique advantage for regaining strength by splitting the rehabilitation between the two knees and allowing the patient to exclusively focus on strength for the graft-donor knee. In our current study, patients showed a consistent progression of quadriceps muscle strength through time (Table 4). Attaining symmetry early, followed by getting both knees back to preoperative normal values, is thought to allow for a quicker return to normal function and eventually sports.
Regaining quadriceps muscle strength is a variable that is difficult to normalize after surgery, regardless of graft choice. 15,24,26,41 Kobayashi et al 26 assessed isokinetic quadriceps muscle strength (180 deg/s) for patients undergoing ACL reconstruction with an ipsilateral PTG and showed a limb symmetry index of 69% and 82% at 6 months and 12 months, respectively. Feller and Webster 15 looked at the difference in isokinetic quadriceps muscle strength between hamstring tendon grafts and PTGs 4 months after surgery and found a significant deficit for both groups; however, patients who received a PTG had a larger deficit (hamstring tendon graft 27%; PTG 36%). Shelbourne and Urch 56 compared strength return between patients receiving an ipsilateral versus a contralateral PTG, and the results showed statistically significantly better strength return with the contralateral graft. Properly rehabilitating the donor site continues to be a problem, evident by significant strength deficits in the literature, further justifying the individual and focused attention to the donor site that the contralateral PTG approach can provide. 15,26 Studies are finding asymmetric quadriceps strength at the time when most athletes are returning to sport, 4 to 12 months, which appears to affect function negatively in the long-term. 15 Some studies have found long-term deficits in strength compared with the contralateral limb for up to 2 years, potentially providing a reason to delay a return to sport past this time. 29,34 Normalizing strength early on can give the patient a better chance at returning to sports successfully and in a timely manner.
Postoperative laxity is an important component of an ACL reconstruction that cannot be overlooked when determining success and failure of the surgery. Our study indicated that knee laxity, measured by a manual maximum KT arthrometer difference, was within normal limits at 1 month after surgery (2.0 mm) and was maintained through 2 years (1.9 mm). In terms of postoperative laxity, surgical success and failure are often defined as a manual maximum KT arthrometer difference of >5 mm between the surgical and nonsurgical side. 1,18 Our current study showed that 98% of patients had normal laxity, ≤5 mm manual-maximum difference between knees, when measured by the KT arthrometer at 6 months after surgery. As shown in our current study, as well as in previous studies by Shelbourne et al, 51 knowing that almost all patients have normal postoperative laxity in all stages, the physical therapy staff is able to confidently progress them through rehabilitation without the fear of a surgical failure.
A high percentage of patients in the current study (90%) were able to return to at least a recreational level (level 8) or higher after surgery. Of those involved in jumping and pivoting sports before surgery, many were able to attain this same level after surgery, 67% for college and professional athletes, 70% for school-age athletes, and 88% for recreational athletes. The average time to return to full sports participation was 5.7 months after surgery. Successful return to sports at 5.7 months after surgery appears to be faster than previously reported, as a recent systematic review on the topic showed that 14 of the 15 studies included reported a return to sport time of 6 months or longer. 27 Although faster than reported by most of the studies in the systematic review, 5.7 months is slower than previously reported data on ACL reconstructions that used a contralateral PTG; a study by Shelbourne and Urch 56 showed a return to sport time of 4.9 months for the population overall and 4.1 months in the young and highly active population. A main concern for early return to sport after surgery is a subsequent ACL injury to either knee; however, Shelbourne et al 49 showed that the rates of ACL injury in both knees were the same for patients returning before and after 6 months, with all rates ranging from 4.0% to 5.4%. In the study by Shelbourne and Urch, published in 2000, the investigators learned that athletes could get back to sports safely and quickly after surgery; however, their performance was not where they wanted it to be. Therefore, over the years, patients have been advised to take more time getting back to sport so that this aspect of the rehabilitation process could be improved.
Although athletes expect to return to their sport after surgery, and at a high level, some are unable to do so. 3,5,16,61 The overall rate of return to preinjury levels in the current study was 81%, which is on the high end of the range typically reported in the literature. 4,23 In the literature, return to preinjury levels of sport has a wide range, from 31% to 92% 3,5,23,27,62 ; therefore, it is important to note the differences in studies when assessing these rates, as many reasons, including age, sex, graft selection, lifestyle choices, psychological factors, and a host of rehabilitation factors, have been linked to having both high and low rates of return. 8,22,24,27,61,62
Many of the patients in the current study were able to maintain these positive outcomes long-term, as the average CKRS score at 2 years was 92 on the ACL-reconstructed knee and 96 on the graft-donor knee. At 5 years, on the same CKRS, the ACL-reconstructed knee was 88 and the graft-donor knee was 94. For the IKDC, our results at 2 years were 89 on the ACL-reconstructed knee and 91 on the graft-donor knee, and scores stayed relatively high at 5 years, at 84 on the ACL-reconstructed knee and 90 on the graft-donor knee. Our postoperative IKDC results are in line with the normative IKDC values for the general population for those around the average age of patients in our study, with normal values being 89 for men and 86 for women in the 18- to 35-year age bracket. 2 McCarthy et al 32 examined a sample of which the majority received PTGs, and Mohtadi et al 33 measured a group with hamstring tendon grafts; 2-year IKDC scores were 84 in both studies. The graft-donor knees from our study consistently scored higher on subjective scores long-term, further justifying the importance of properly rehabilitating the graft-donor knee. Splitting the rehabilitation between knees and independently working on different goals for the ACL-reconstructed knee and the graft-donor knee is thought to play a large role in returning each knee back to a normal level.
The clinical setting for this study entailed orthopaedic surgeons and in-house physical therapists whose practice was limited to knee treatment only. Over the years, the clinicians have seen a high volume of ACL reconstructions and have collected and continually analyzed data, with the goal of making incremental changes to improve outcomes. Among the benefits of a contralateral PTG, having an office setup like ours most likely helped make these outcomes possible.
Limitations
One of the main limitations of this study is that the results apply only to those undergoing ACL reconstruction with a contralateral PTG, as no other graft was used on our patients. Although not the aim of our study, donor site morbidity was not assessed with a donor site-specific questionnaire, which may be of concern for clinicians choosing a PTG, given that Mastrokalos et al 30 showed similar levels of pain in the graft-donor site for contralateral and ipsilateral PTG. Our study had long-term follow-up on 69% of patients initially enrolled, lower than the ideal 80%, thus possibly skewing our results. From a subjective standpoint, we received data regarding time to return to sport from only 57% of the patients, potentially skewing these results as well. Regarding follow-up, we had to exclude 974 patients for not having data at every time point through 3 months. Many patients had data at some time points during this 3-month period, as well as beyond, yet still had to be excluded for this study. The current study excluded those who sustained an ACL graft tear or contralateral ACL tear, thus not allowing us to determine the effects that a contralateral PTG would have on this type of outcome. Complications were not reported in this particular study; however, they have been reported extensively in previous publications. 9 We did not include long-term radiographs, in particular patellofemoral views from the graft-donor knee, which would help in determining long-term arthritic changes, if any, although this outcome was not an aim of the study. Last, the results from this study are a product of a unique practice setting, thus limiting the generalizability of the findings to other practice settings unlike ours. Simply performing an ACL reconstruction using a contralateral PTG is not the only factor in successful outcomes; instead, it must be accompanied by the specific rehabilitation principles described here.
Conclusion
For patients having an ACL reconstruction with a contralateral PTG, postoperative ROM and strength can be progressed quickly and effectively by splitting the rehabilitation into two different goals, with ROM being the focus on the ACL-reconstructed knee and strength being the focus on the graft-donor knee. Performing the surgery in this way, followed by a structured rehabilitation plan, can allow patients to return to their desired activity level in a timely manner and achieve good subjective results at 2 and 5 years postoperatively.
APPENDIX
Table A1.
Rehabilitation Program for ACL Reconstruction With Contralateral Patellar Tendon Graft
| Goals | Exercises |
|---|---|
| Preoperative | |
| ACL-reconstructed knee | |
| Reduce swelling | Cold/compression; elevation |
| Obtain full ROM | Hyperextension device/heel slides 3×/day |
| Good leg control | Active terminal extension |
| Achieve normal gait | Gait training |
| Mental preparedness | Patient education of program and goals |
| Graft-donor knee | |
| Maintain leg strength | Practice step-up exercise used postoperatively for graft knee |
| Surgery | |
| ACL-reconstructed knee | |
| Maintain full ROM | Passive motion from full hypertension to full flexion (heel touches buttocks) |
| Prevent pain and swelling | Intravenous ketorolac pain prevention program 54 |
| Graft-donor knee | |
| Bone graft the defects in the patella and tibia | — |
| Close patellar tendon defect | — |
| Phase 1 (immediate postoperative through 1 wk postoperative) | |
| ACL-reconstructed knee | |
| Minimize hemarthrosis | Cold/compression to remain on the knee except during exercises; elevation |
| Full passive hyperextension | Heel prop, 10 min, 4×/day |
| Flexion to 125° | CPM set at highest flexion possible; leave leg in maximal flexion for 3 min, 3×/day |
| Gentle ROM | Heel slides; use measuring stick to monitor progress |
| Independent leg raise | CPM machine set to move from 0° to 30° continually when not doing exercises; knee is elevated above the heart in the CPM machine |
| Weightbearing as tolerated | Active quadriceps contractions; straight-leg raises; active terminal extension |
| Normal gait | Gait training |
| Graft-donor knee | |
| Minimize swelling | Cold pack; leg elevated on pillow |
| Full passive hyperextension | Heel prop exercise to allow for full hyperextension |
| Full flexion | Heel slides; pull heel to buttocks; use measuring stick to monitor progress |
| Donor site strengthening | Shuttle machine; set resistance so able to do 25 repetitions, 3×/day; progressively increase repetitions and resistance |
| Phase 2 (1 wk through 1 mo postoperative) | |
| ACL-reconstructed knee | |
| Maintain full extension | Heel prop |
| Be able to lock knee straight with full weightbearing | Single-leg stance; locking knee in extension |
| Increase flexion equal to opposite knee | Heel slide |
| Maintain minimal swelling | Cold/compression |
| Normal gait | Gait training in front of a mirror |
| Progress to light strengthening | Active terminal extension; progress to stationary bicycling |
| Graft-donor knee | |
| Maintain full extension and flexion | Heel prop; heel slide |
| No swelling | Ice after exercise |
| Donor site strengthening | ▪ Shuttle exercise: up to 100 repetitions 3×/day (through 2 wk postoperative) ▪ Step-box exercise at height to allow for 50-100 repetitions; perform 3-4×/day ▪ Progress to single-leg weight training exercises (still high repetition/low resistance): leg press, leg extension |
| Phase 3 (after 1 mo postoperative as patient is able to progress) | |
| ACL-reconstructed knee | |
| Maintain full ROM | Heel props as needed; sit on heels |
| Control swelling | Cold/compression; adjust activities to keep swelling to a minimum |
| Quadriceps strengthening | Bicycle; Stairmaster; can progress to leg press, leg extension, squats once strength symmetry is within 10% |
| Return to light sports | Functional progression from agility drills, sport-specific agility drills, to controlled practice drills |
| Graft-donor knee | |
| Donor site strengthening | Single-leg strengthening; increase weight and decrease repetitions for weight training exercises; can progress to double-leg strengthening once symmetry is within 10% |
| Phase 4 (after 3 mo postoperative as patient is able to progress) | |
| ACL-reconstructed knee | |
| Maintain full ROM | Exercises as needed; watch for motion loss and decrease activities if needed; monitor daily |
| Control swelling | Adjust activities to keep swelling to a minimum; continue using cold/compression |
| Return to full sports | Continue sport-specific and controlled practice drills and progress first to part-time competition and then full-time competition |
| Graft-donor knee | |
| Return donor site functional strength | ▪ Continue with weight training 3-4×/wk ▪ Increase functional strength through sport-specific activities; alternate intensity with hard and easy days |
a ACL, anterior cruciate ligament; CPM, continuous passive motion; ROM, range of motion.
Footnotes
Final revision submitted August 23, 2022; accepted August 30, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: R.B. has received consulting fees from Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Community Health Network (ref No. 201504005).
References
- 1. American Orthopedic Society for Sports Medicine. 2000. International Knee Documentation Committee Knee Evaluation Form. https://www.sportsmed.org/aossmimis/Staging/Research/IKDC_Forms.aspx
- 2. Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ; International Knee Documentation Committee. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1):128–135. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 4. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41(7):1549–1558. [DOI] [PubMed] [Google Scholar]
- 5. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. [DOI] [PubMed] [Google Scholar]
- 6. Arnold MP, Calcei JG, Vogel N, et al. ACL Study Group survey reveals the evolution of anterior cruciate ligament reconstruction graft choice over the past three decades. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3871–3876. [DOI] [PubMed] [Google Scholar]
- 7. Barber-Westin SD, Noyes FR, McCloskey JW. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati Knee Rating System in 350 subjects with uninjured, injured, or anterior cruciate ligament-reconstructed knees. Am J Sports Med. 1999;27(4):402–416. [DOI] [PubMed] [Google Scholar]
- 8. Barié A, Sprinckstub T, Huber J, Jaber A. Quadriceps tendon vs. patellar tendon autograft for ACL reconstruction using a hardware-free press-fit fixation technique: comparable stability, function and return-to-sport level but less donor site morbidity in athletes after 10 years. Arch Orthop Trauma Surg. 2020;140(10):1465–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Benner RW, Shelbourne KD, Freeman H. Infections and patellar tendon ruptures after anterior cruciate ligament reconstruction: a comparison of ipsilateral and contralateral patellar tendon autografts. Am J Sports Med. 2011;39(3):519–525. [DOI] [PubMed] [Google Scholar]
- 10. Biggs A, Jenkins WL, Urch SE, Shelbourne KD. Rehabilitation for patients following ACL reconstruction: a knee symmetry model. North Am J Sports Phys Ther. 2009;4(1):2–12. [PMC free article] [PubMed] [Google Scholar]
- 11. Bottoni CR, Liddell TR, Trainor TJ, Freccero DM, Lindell KK. Postoperative range of motion following anterior cruciate ligament reconstruction using autograft hamstrings: a prospective, randomized clinical trial of early versus delayed reconstructions. Am J Sports Med. 2008;36(4):656–662. [DOI] [PubMed] [Google Scholar]
- 12. Cheney S, Chiaia TA, de Mille P, Boyle C, Ling D. Readiness to return to sport after ACL reconstruction: a combination of physical and psychological factors. Sports Med Arthrosc Rev. 2020;28(2):66–70. [DOI] [PubMed] [Google Scholar]
- 13. Cristiani R, Mikkelsen C, Forssblad M, Engström B, Stålman A. Only one patient out of five achieves symmetrical knee function 6 months after primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3461–3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ekhtiari S, Horner NS, de Sa D, et al. Arthrofibrosis after ACL reconstruction is best treated in a step-wise approach with early recognition and intervention: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3929–3937. [DOI] [PubMed] [Google Scholar]
- 15. Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564–573. [DOI] [PubMed] [Google Scholar]
- 16. Feucht MJ, Cotic M, Saier T, et al. Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):201–207. [DOI] [PubMed] [Google Scholar]
- 17. Goodwillie AD, Shah SS, McHugh MP, Nicholas SJ. The effect of postoperative KT-1000 arthrometer score on long-term outcome after anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(7):1522–1528. [DOI] [PubMed] [Google Scholar]
- 18. Grassi A, Kim C, Marcheggiani Muccioli GM, Zaffagnini S, Amendola A. What is the mid-term failure rate of revision ACL reconstruction? A systematic review. Clin Orthop Relat Res. 2017;475(10):2484–2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hamrin Senorski E, Svantesson E, Beischer S, et al. Low 1-year return-to-sport rate after anterior cruciate ligament reconstruction regardless of patient and surgical factors: a prospective cohort study of 272 patients. Am J Sports Med. 2018;46(7):1551–1558. [DOI] [PubMed] [Google Scholar]
- 21. Herbst E, Hoser C, Gföller P, et al. Impact of surgical timing on the outcome of anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):569–577. [DOI] [PubMed] [Google Scholar]
- 22. Herrington L, Ghulam H, Comfort P. Quadriceps strength and functional performance after anterior cruciate ligament reconstruction in professional soccer players at time of return to sport. J Strength Cond Res. 2021;35(3):769–775. [DOI] [PubMed] [Google Scholar]
- 23. Ibrahim SAR, Abdul Ghafar S, Marwan Y, et al. Intratunnel versus extratunnel autologous hamstring double-bundle graft for anterior cruciate ligament reconstruction: a comparison of 2 femoral fixation procedures. Am J Sports Med. 2015;43(1):161–168. [DOI] [PubMed] [Google Scholar]
- 24. Ithurburn MP, Altenburger AR, Thomas S, Hewett TE, Paterno MV, Schmitt LC. Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):426–433. [DOI] [PubMed] [Google Scholar]
- 25. Ithurburn MP, Longfellow MA, Thomas S, Paterno MV, Schmitt LC. Knee function, strength, and resumption of preinjury sports participation in young athletes following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2019;49(3):145–153. [DOI] [PubMed] [Google Scholar]
- 26. Kobayashi A, Higuchi H, Terauchi M, Kobayashi F, Kimura M, Takagishi K. Muscle performance after anterior cruciate ligament reconstruction. Int Orthop. 2004;28(1):48–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52(2):128–138. [DOI] [PubMed] [Google Scholar]
- 28. Leiter JRS, Gourlay R, McRae S, de Korompay N, MacDonald PB. Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1061–1069. [DOI] [PubMed] [Google Scholar]
- 29. Maletis GB, Cameron SL, Tengan JJ, Burchette RJ. A prospective randomized study of anterior cruciate ligament reconstruction: a comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2007;35(3):384–394. [DOI] [PubMed] [Google Scholar]
- 30. Mastrokalos DS, Springer J, Siebold R, Paessler HH. Donor site morbidity and return to the preinjury activity level after anterior cruciate ligament reconstruction using ipsilateral and contralateral patellar tendon autograft: a retrospective, nonrandomized study. Am J Sports Med. 2005;33(1):85–93. [DOI] [PubMed] [Google Scholar]
- 31. Mauro CS, Irrgang JJ, Williams BA, Harner CD. Loss of extension following anterior cruciate ligament reconstruction: analysis of incidence and etiology using IKDC criteria. Arthroscopy. 2008;24(2):146–153. [DOI] [PubMed] [Google Scholar]
- 32. McCarthy M, Mallett K, Abola M, Vassallo S, Nguyen J. Hospital for Special Surgery ACL Registry: 2-year outcomes suggest low revision and return to OR rates. HSS J Musculoskelet J Hosp Spec Surg. 2017;13(2):119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mohtadi NG, Chan DS. A randomized clinical trial comparing patellar tendon, hamstring tendon, and double-bundle ACL reconstructions: patient-reported and clinical outcomes at 5-year follow-up. J Bone Joint Surg Am. 2019;101(11):949–960. [DOI] [PubMed] [Google Scholar]
- 34. Nagelli CV, Hewett TE. Should return to sport be delayed until two years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med. 2017;47(2):221–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Noailles T, Chalopin A, Boissard M, Lopes R, Bouguennec N, Hardy A. Incidence and risk factors for cyclops syndrome after anterior cruciate ligament reconstruction: a systematic literature review. Orthop Traumatol Surg Res. 2019;105(7):1401–1405. [DOI] [PubMed] [Google Scholar]
- 36. Noll S, Garrison JC, Bothwell J, Conway JE. Knee extension range of motion at 4 weeks is related to knee extension loss at 12 weeks after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2015;3(5):2325967115583632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Norkin C, White D. Measurement of Joint Motion: A Guide to Goniometry. 3rd ed. FA Davis ; 2003. [Google Scholar]
- 38. Ouweleen AJ, Hall TB, Finlayson CJ, Patel NM. Predictors of arthrofibrosis after pediatric anterior cruciate ligament reconstruction: what is the impact of quadriceps autograft? J Pediatr Orthop. Published online May 13, 2021. doi:10.1097/BPO.0000000000001860 [DOI] [PubMed] [Google Scholar]
- 39. Palmieri-Smith RM, Lepley LK. Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med. 2015;43(7):1662–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pietrosimone B, Lepley AS, Harkey MS, et al. Quadriceps strength predicts self-reported function post-ACL reconstruction. Med Sci Sports Exerc. 2016;48(9):1671–1677. [DOI] [PubMed] [Google Scholar]
- 41. Pottkotter KA, Di Stasi SL, Schmitt LC, et al. Timeline of gains in quadriceps strength symmetry and patient-reported function early after ACL reconstruction. Int J Sports Phys Ther. 2020;15(6):995–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rothrauff BB, Karlsson J, Musahl V, Irrgang JJ, Fu FH. ACL consensus on treatment, outcome, and return to sport. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2387–2389. [DOI] [PubMed] [Google Scholar]
- 43. Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Schreiber VM, Jordan SS, Bonci GA, Irrgang JJ, Fu FH. The evolution of primary double-bundle ACL reconstruction and recovery of early post-operative range of motion. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1475–1481. [DOI] [PubMed] [Google Scholar]
- 45. Shelbourne KD, Beck MB, Gray T. Anterior cruciate ligament reconstruction with contralateral autogenous patellar tendon graft: evaluation of donor site strength and subjective results. Am J Sports Med. 2015;43(3):648–653. [DOI] [PubMed] [Google Scholar]
- 46. Shelbourne KD, Benner RW, Gray T. Results of anterior cruciate ligament reconstruction with patellar tendon autografts: objective factors associated with the development of osteoarthritis at 20 to 33 years after surgery. Am J Sports Med. 2017;45(12):2730–2738. [DOI] [PubMed] [Google Scholar]
- 47. Shelbourne KD, Freeman H, Gray T. Osteoarthritis after anterior cruciate ligament reconstruction: the importance of regaining and maintaining full range of motion. Sports Health. 2012;4(1):79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Shelbourne KD, Gray T. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation: a two- to nine-year followup. Am J Sports Med. 1997;25(6):786–795. [DOI] [PubMed] [Google Scholar]
- 49. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. [DOI] [PubMed] [Google Scholar]
- 50. Shelbourne KD, Jari S, Gray T. Outcome of untreated traumatic articular cartilage defects of the knee: a natural history study. J Bone Joint Surg Am. 2003;85-A(suppl 2):8-16. [DOI] [PubMed] [Google Scholar]
- 51. Shelbourne KD, Klootwyk TE, Wilckens JH, De Carlo MS. Ligament stability two to six years after anterior cruciate ligament reconstruction with autogenous patellar tendon graft and participation in accelerated rehabilitation program. Am J Sports Med. 1995;23(5):575–579. [DOI] [PubMed] [Google Scholar]
- 52. Shelbourne KD, Klotz C. What I have learned about the ACL: utilizing a progressive rehabilitation scheme to achieve total knee symmetry after anterior cruciate ligament reconstruction. J Orthop Sci. 2006;11(3):318–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Shelbourne KD, Liotta FJ, Goodloe SL. Preemptive pain management program for anterior cruciate ligament reconstruction. Am J Knee Surg. 1998;11(2):116–119. [PubMed] [Google Scholar]
- 54. Shelbourne KD, Sullivan AN, Bohard K, Gray T, Urch SE. Return to basketball and soccer after anterior cruciate ligament reconstruction in competitive school-aged athletes. Sports Health. 2009;1(3):236–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Shelbourne KD, Thomas JA. Contralateral patellar tendon and the Shelbourne experience, part 2: results of revision anterior cruciate ligament reconstruction. Sports Med Arthrosc Rev. 2005;13(2):69–72. [Google Scholar]
- 56. Shelbourne KD, Urch SE. Primary anterior cruciate ligament reconstruction using the contralateral autogenous patellar tendon. Am J Sports Med. 2000;28(5):651–658. [DOI] [PubMed] [Google Scholar]
- 57. Shelbourne KD, Vanadurongwan B, Gray T. Primary anterior cruciate ligament reconstruction using contralateral patellar tendon autograft. Clin Sports Med. 2007;26(4):549–565. [DOI] [PubMed] [Google Scholar]
- 58. Sonnery-Cottet B, Lavoie F, Ogassawara R, et al. Clinical and operative characteristics of cyclops syndrome after double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(11):1483–1488. [DOI] [PubMed] [Google Scholar]
- 59. Van Yperen DT, Reijman M, van Es EM, Bierma-Zeinstra SMA, Meuffels DE. Twenty-year follow-up study comparing operative versus nonoperative treatment of anterior cruciate ligament ruptures in high-level athletes. Am J Sports Med. 2018;46(5):1129–1136. [DOI] [PubMed] [Google Scholar]
- 60. Von Essen C, Eriksson K, Barenius B. Acute ACL reconstruction shows superior clinical results and can be performed safely without an increased risk of developing arthrofibrosis. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2036–2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Webster KE, Feller JA. Return to level I sports after anterior cruciate ligament reconstruction: evaluation of age, sex, and readiness to return criteria. Orthop J Sports Med. 2018;6(8):2325967118788045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Webster KE, McPherson AL, Hewett TE, Feller JA. Factors associated with a return to preinjury level of sport performance after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2019;47(11):2557–2562. [DOI] [PubMed] [Google Scholar]
- 63. Welling W, Benjaminse A, Lemmink K, Dingenen B, Gokeler A. Progressive strength training restores quadriceps and hamstring muscle strength within 7 months after ACL reconstruction in amateur male soccer players. Phys Ther Sport. 2019;40:10–18. [DOI] [PubMed] [Google Scholar]
- 64. Widner M, Dunleavy M, Lynch S. Outcomes following ACL reconstruction based on graft type: are all grafts equivalent? Curr Rev Musculoskelet Med. 2019;12(4):460–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Zwolski C, Schmitt LC, Quatman-Yates C, Thomas S, Hewett TE, Paterno MV. The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(9):2242–2249. [DOI] [PubMed] [Google Scholar]