Abstract
BACKGROUND
Factors and trends associated with hypertension control (BP < 130/80 mm Hg) and mean blood pressure (BP) among hypertensive adults (BP ≥1 30/80 mm Hg or medicated for hypertension).
METHOD
Data on 22,911 hypertensive US adults from the 1999–2016 National Health and Nutrition Examination Survey.
RESULTS
For men, hypertension control prevalence increased from 8.6% in 1999–2000 to 16.2% in 2003–2004 (P < 0.001), and continued the increasing trend afterwards to 23.2% in 2011–2012 (P < 0.001) and then plateaued. For women, hypertension control prevalence increased from 1999–2000 to 2009–2010 (10.8–26.3%, P < 0.001) and then plateaued. For men with hypertension, systolic BP decreased from 1999–2000 to 2011–2012 (135.7–132.8 mm Hg, P < 0.001) and then increased to 135.3 mm Hg in 2015–2016 (P < 0.001). For women with hypertension, systolic BP decreased from 1999–2000 to 2009–2010 (139.7–131.9 mm Hg; P < 0.001) and then increased to 134.4 mm Hg in 2015–2016 (P = 0.003). Diastolic BP decreased from 1999–2000 to 2015–2016 (men: 79.1–75.5 mm Hg and women: 76.4–73.7 mm Hg, P < 0.001 for both). In 2011–2016, hypertension control was 22.0% for men and 25.2% for women. The adjusted prevalence ratio (PR) of hypertension control were lower for non-Hispanic black men and women (PR = 0.72, 95% confidence interval (CI) = 0.61–0.86; PR = 0.83, 95% CI = 0.70–0.99, respectively; non-Hispanic white (NHW) as reference), Hispanic and non-Hispanic Asian men (PR = 0.70, 95% CI = 0.54–0.92; PR = 0.59, 95% CI = 0.39–0.86; respectively; NHW as reference).
CONCLUSION
Hypertension control significantly increased from 1999–2000 to 2011–2012 (men) and 2009–2010 (women) and then plateaued. About a quarter of US adults with hypertension were controlled in 2011–2016.
Keywords: blood pressure, blood pressure control, hypertension, NHANES, systolic and diastolic BP ACC/AHA 2017 guidelines
Recently, the Global Burden of Disease report identified elevated systolic blood pressure (BP), as one of the 10 largest contributors to disability-adjusted life years lost during 2015.1 Effective BP management, resulting in a reduction in BP values, has been shown to decrease the incidence of mortality, stroke, heart attack, and heart failure.2–8
Using the most recent NHANES data, and the new 2017 American College of Cardiology/American Heart Association (ACC/AHA) hypertension guidelines, our analysis focused on hypertension control with three objectives.9 The first objective was to assess trends in hypertension control from 1999 to 2016 by gender. The second objective was to assess trends in mean systolic and diastolic BP among those with hypertension and those with controlled hypertension from 1999 to 2016. The third objective was to describe the association between hypertension control during 2011–2016 and demographic, health care utilization, risk factors, and comorbidities. Survey years 2011–2016 were used because they include non-Hispanic Asian American and three survey cycles of data provide sufficient sample size to generalize to US adult population.
METHODS
Survey description
The National Health and Nutrition Examination Survey (NHANES) of the National Center for Health Statistics is a cross-sectional, nationally representative health examination surveys of the US civilian noninstitutionalized population. The survey uses a complex, stratified, multistage probability cluster-sampling design.10 Participants are interviewed in their homes to obtain information on health history, health behaviors, and risk factors. Subsequently, they undergo a physical examination at a mobile examination center (MEC). The procedures to select the sample and conduct the interview and examination have been previously specified.10,11 Informed consent is obtained from all participants, and the Research Ethics Review Board of the National Center for Health Statistics approved the NHANES protocol.
Sample
The unweighted sample size for each 2-year NHANES cycle appears in Supplementary Table 1-e. Overall, the response rate for the MEC exam varied from 71% (4,976/7,038) in 1999–2000 to 59% (5,735/9,800) in 2015–2016. Of those examined during survey years 1999–2016, 3,778 persons were excluded from this analysis for the following reasons: 1,533 were pregnant, and 2,245 had missing systolic and diastolic BP data. These exclusions resulted in a final sample of 47,056 participants aged 18 years and older out of which 22,911 individuals were classified as having hypertension.
For the analysis using 2011–2016 NHANES, 17,274 (62%) were examined in the MEC. Of those examined, 809 persons were excluded for the following reasons: 192 were pregnant, and 456 had missing systolic and diastolic BP data. These exclusions resulted in a final sample of 16,465 (59%) participants aged 18 years and older out of which 7,972 individuals were classified as adults with hypertension.
Outcome variables
All BP readings were obtained during a single examination visit. Trained physicians followed a standard protocol measuring BP at the MEC using a Bauman true gravity mercury wall model and standard Bauman cuffs. Appropriate BP cuff sizes were based on the measurement of the participant’s mid-arm circumference. After a 5 min rest, participants had their systolic and diastolic BPs (onset of K1 and fading of K5) measured; systolic and diastolic BP measurements were taken 30 s apart.11,12
The average of up to three brachial systolic and diastolic BP readings was used as the participants’ systolic and diastolic BP values. For participants with only one reading, that single reading was used as the average. Using the new 2017 ACC/AHA guidelines, an individual was defined as having stage I hypertension if at least one of the following conditions was satisfied: systolic BP of 130 mm Hg or greater, diastolic BP of 80 mm Hg or greater, or the participant reported currently taking medication to lower high BP.9 Hypertension control was defined as systolic BP less than 130 mm Hg and diastolic BP less than 80 mm Hg among those with hypertension.9 Mean systolic and diastolic trends were assessed among adults having hypertension and among adults who controlled their hypertension.
Covariates
Demographics.
Age was categorized as 18–39, 40–59, 60–79, and 80 years and older. Data on race/Hispanic origin were categorized as non-Hispanic white, non-Hispanic black, non-Hispanic Asian, Hispanic, and other in 2011–2016.
Income and health care utilization.
Family income to poverty ratio (FIPR) is the ratio of a family’s income to its appropriate poverty guidelines as established by the US Department of Health and Human Services.13 Four categories of approximately equal number of individuals in each category were used for these analyses: <1.00, 1.00–1.99, 2.00–2.99, and ≥3.00. Larger FIPRs indicate higher income. Frequency of visits to a health care provider was self-reported based on the answer to the home interview question, “During the past 12 months, how many times have you seen a doctor or other health care professional about your health at a doctor’s office, a clinic, hospital emergency room, at home, or some other place?”.12
Risk factors.
A number of risk factors are associated with hypertension and hypertension control and were included in this analysis as covariates, among them are body mass index, physical activity, diabetes, and chronic kidney disease.3,8,14–18
Fasting and nonfasting weights were obtained in kilograms using a digital scale while wearing a standardized two piece examination outfit. Height in cm was obtained using a stadiometer with a fixed vertical backboard and an adjustable head piece.12 Body mass index (BMI) was calculated as measured weight over measured height in meters squared (kg/m2), and was categorized using criteria established by the National Institutes of Health as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥30.0 kg/m2).19 Due to the relatively small number of participants in the underweight category, the underweight category was combined with the normal weight category after a sensitivity analysis showed little difference in the results when excluding the underweight category or when including it in the normal weight category.
Leisure time physical activity (LTPA) was calculated from the NHANES physical activity questionnaire.20 Respondents reported the usual amount of time, per week, spent in moderate and vigorous recreational activities. Minutes of vigorous LTPA was doubled and added to moderate LTPA to get total LTPA. Based on physical activity guidelines, total LTPA was categorized into: none; some, but less than 150 min/week; and 150 or more min/week.18
Diabetes was defined as “diagnosed diabetic” if a participant reported being told by a doctor or health care provider that he/she has diabetes.12
The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation was used to estimate glomerular filtration rate (GFR) or, the presence of albuminuria (creatinine to albumin ratio). CKD was defined as a GFR less than 60 ml/min per 1.73 m2 or albumin-to-creatinine ratio greater than 30 mg/g.17
Statistical methods
All statistical analyses were performed using survey procedures in SAS 9.4 for Windows (SAS Institute, Inc., Cary, NC) and SUDAAN 10.0 software (Research Triangle Institute, Research Triangle Park, NC). All estimates were weighted using the MEC sample weights and incorporated sampling design information; the sample weights accounted for the unequal probabilities of selection resulting from the complex sample design, survey nonresponse, and the planned oversampling of selected population subgroups.
The trend analysis was applied to 1999–2016 survey years and followed the recent analytic method used by Ogden et al.21 Trends in hypertension and hypertension control and trends in mean systolic and diastolic BP were examined using regression models with the survey period treated as a continuous variable. Linear trend and quadratic trends were tested separately; the latter included both linear and quadratic terms in the models. If a quadratic trend was found, Joinpoint software was used to find the inflection point(s) (Joinpoint version 3.0.1, National Cancer Institute). After an inflection point (or points) was found, the differences in slopes between the adjacent segments were tested using piecewise linear regression (surveylogistic and surveyreg procedures, SAS v9.4). The hypertension control trends for males and females were statistically significantly different (significant survey cycle and gender interaction), so we conducted analyses stratified by gender.
For the NHANES 2011–2016 hypertension control prevalence analysis, the weighted prevalence and 95% confidence intervals (CIs) of hypertension control were calculated by gender and selected covariates among adults classified as having hypertension. Because hypertension is more prevalent among older individuals, we followed the Crim et al. recommendations and calculated age-adjusted prevalence of hypertension control using the direct method and the distribution of the subpopulation of individuals who had defined hypertension in NHANES 2007–2016 with age groups 18–39, 40–59, 60–79, and 80 years and older.22 Ten years of NHANES data were used to derive reliable age distribution of the most recent hypertensive population. Multivariate logistic regression models were used to examine the independent association of the covariates with the response variable hypertension control among those with hypertension. Prevalence ratios (PRs) with a 95% CI not including 1.0 were considered statistically significant. We derived PR in this article to avoid overestimating the strength of the association of the prevalence odds ratio (OR).23,24
Means systolic and diastolic BP estimates among adults with hypertension and adults with controlled hypertension were age-adjusted by the direct method to the subpopulation of individuals who had defined hypertension in NHANES 2007–2016 with age groups 18–39, 40–59, 60–79, and 80 years and older.22 Hypertension prevalence estimates were age-adjusted by the direct method to the 2000 US census population using age groups 18–39, 40–59, 60–79, and 80 and older.23
RESULTS
Trends in hypertension control and mean systolic and diastolic values, 1999–2016
Figure 1 and Supplementary Table 2-e show the gender-specific age-adjusted trends in hypertension and hypertension control from 1999 to 2016 for adults aged 18 years and older. Since 1999, there was a statistically significant linear decreasing trend in the prevalence of hypertension among men (51.8% in 1999–2000, 47.3% in 2015–2016, slope = −0.02, P = 0.004), however, there was no significant change in the prevalence of hypertension among women (42.0% in 1999–2000, 39.8% in 2015–2016, slope = −0.01, P = 0.09) (Figure 1). Overall, hypertension control prevalence increased from 9.7% in 1999–2000 to 23.8% in 2009–2010 and then plateaued to 21.7% in 2015–2016. Joinpoint analysis and piecewise regression analysis showed two break points for men at 2003–2004 and 2011–2012 and one break point for women at 2009–2010 (for men, slope before 2003–2004 was 0.33, P ≤ 0.001, slope between 2003–2004 and 2011–2012 was 0.13, P ≤ 0.001, and slope after 2011–2012 was −0.08, P = 0.28; and for women, slope before 2009–2010 was 0.22, P ≤ 0.001 and slope after 2009–2010 was −0.04, P = 0.42). For men, these changes in slopes were due to hypertension control increasing from 8.6% in 1999–2000 to 16.2% in 2003–2004, and continuing the increasing trend afterwards, but at a slower speed, to 23.2% in 2011–2012, and then being stable with no further increase between 2013 and 2016. For women, hypertension control was increasing from 10.8% in 1999–2000 to 26.3% in 2009–2010, and then being stable afterwards with no further increase between 2011 and 2016.
Figure 1.

Gender-specific and age-adjusteda trends in hypertension among adults aged 18 years and older and age-adjustedb hypertension controlc among adults aged 18 and older: United States, 1999–2016. *Significant linear decreasing trend from 99–00 to 15–16. **Significant linear increasing trend from 99–00 to 03–04, and from 03–04 to 11–12. ***Significant linear increasing trend from 99–00 to 09–10. aHypertension estimates are age-adjusted by the direct method to the 2000 US Census population using age groups 18–39, 40–59, 60–79, and 80 and older. bEstimates of controlled hypertension are age-adjusted by the direct method using computed weights based on the subpopulation of persons with hypertension in the 2007–2016 National Health and Nutrition Examination Survey, 18–39, 40–59, 60–79, and 80 and older with weights 0.1661, 0.4061, 0.3446, and 0.0832. cHypertension control (BP < 130/80 mm Hg) among those with hypertension. Note: Numbers in green box refer to hypertension control of females; numbers in gray box refer to hypertension control of males.
Figure 2 shows the trends in mean systolic and diastolic BP across the nine survey-periods for adults with hypertension. For men, mean SBP decreased (P ≤ 0.001) from 135.7 mm Hg in 1999–2000 to 132.8 mm Hg in 2011–2012, and then increased (P ≤ 0.001) to 135.3 mm Hg in 2015–2016. For women, SBP decreased (P ≤ 0.001) from 139.7 mm Hg in 1999–2000 to 131.9 mm Hg in 2009–2010, and then increased (P = 0.003) to 134.4 mm Hg in 2015–2016. No changes in directions were found in DBP trends for both men and women. Among men mean DBP decreased from 79.1 mm Hg in 1999–2000 to 75.5 mm Hg in 2015–2016 (P ≤ 0.001); whereas, for women mean DBP decreased from 76.4 mm Hg in 1999–2000 to 73.7 mm Hg in 2015–2016 (P ≤ 0.001).
Figure 2.
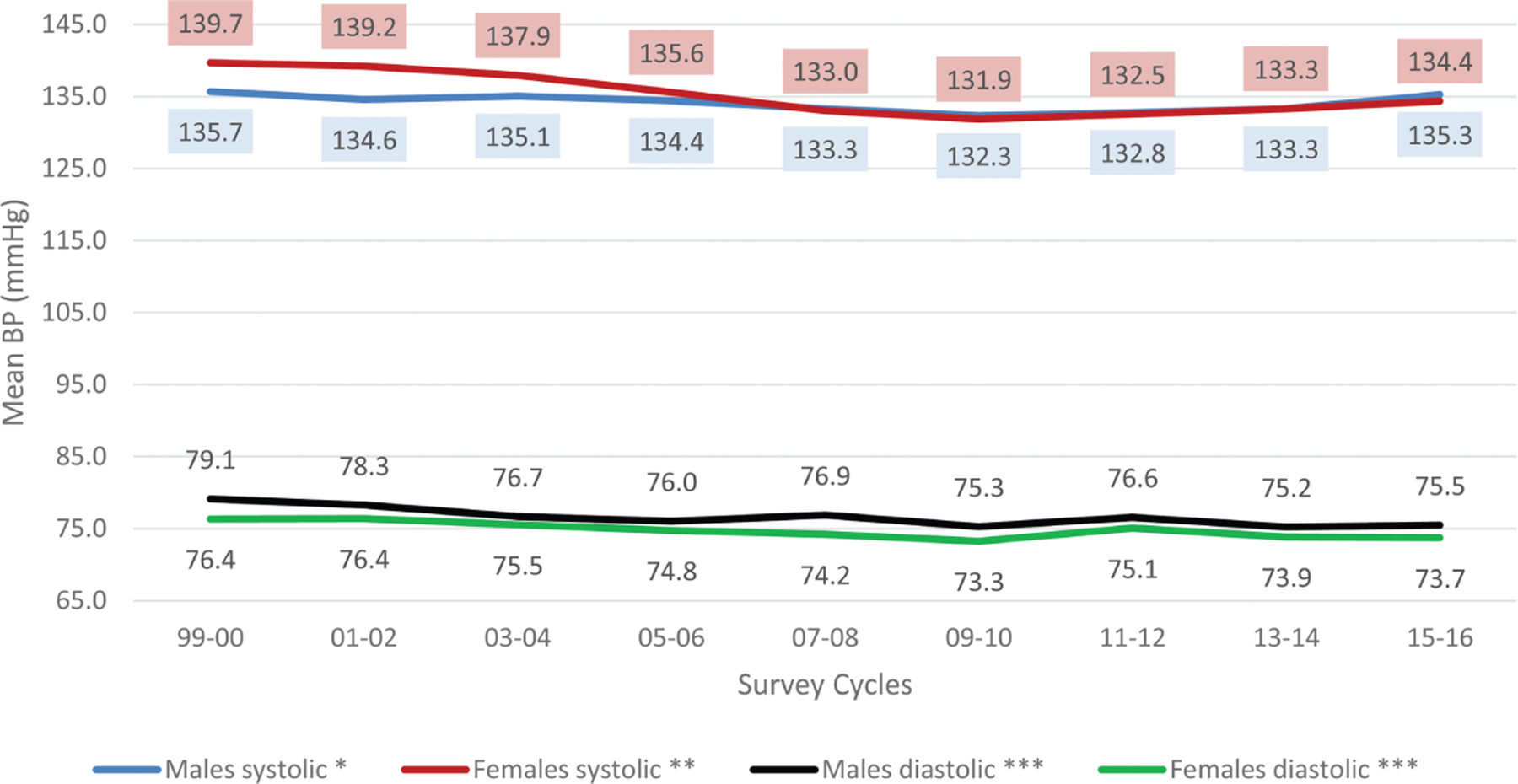
Gender-specific and age-adjusteda mean systolic and diastolic blood pressure among adults aged 18 and older with hypertension: United States, 1999–2016. *Significant linear decreasing trend from 99–00 to 11–12, significant linear increasing trend from 11–12 to 15–16. **Significant linear decreasing trend from 99–00 to 09–10, significant linear increasing trend from 09–10 to 15–16. ***Significant linear decreasing trend from 99–00 to 15–16. aEstimates of controlled hypertension are age-adjusted by the direct method using computed weights based on the subpopulation of persons with hypertension in the 2007–2016 National Health and Nutrition Examination Survey, 18–39, 40–59, 60–79, and 80 and older with weights 0.1661, 0.4061, 0.3446, and 0.0832. Note: numbers in red box refer to female systolic; numbers in blue box refer to male systolic.
Figure 3 shows the trends in mean systolic and diastolic BP across the nine survey periods for adults with controlled hypertension. There were no significant linear trends in SBP and DBP among those with controlled hypertension for both men and women. Mean SBP was 115.2 mm Hg in 1999–2000 and 117.7 mm Hg in 2015–2016 for men, and 117.7 mm Hg in 1999–2000 and 116.6 mm Hg in 2015–2016 for women. Mean DBP was 69.4 mm Hg in 1999–2000 and 68.2 mm Hg in 2015–2016 for men, and 66.2 mm Hg in 1999–2000 and 64.5 mm Hg in 2015–2016 for women.
Figure 3.
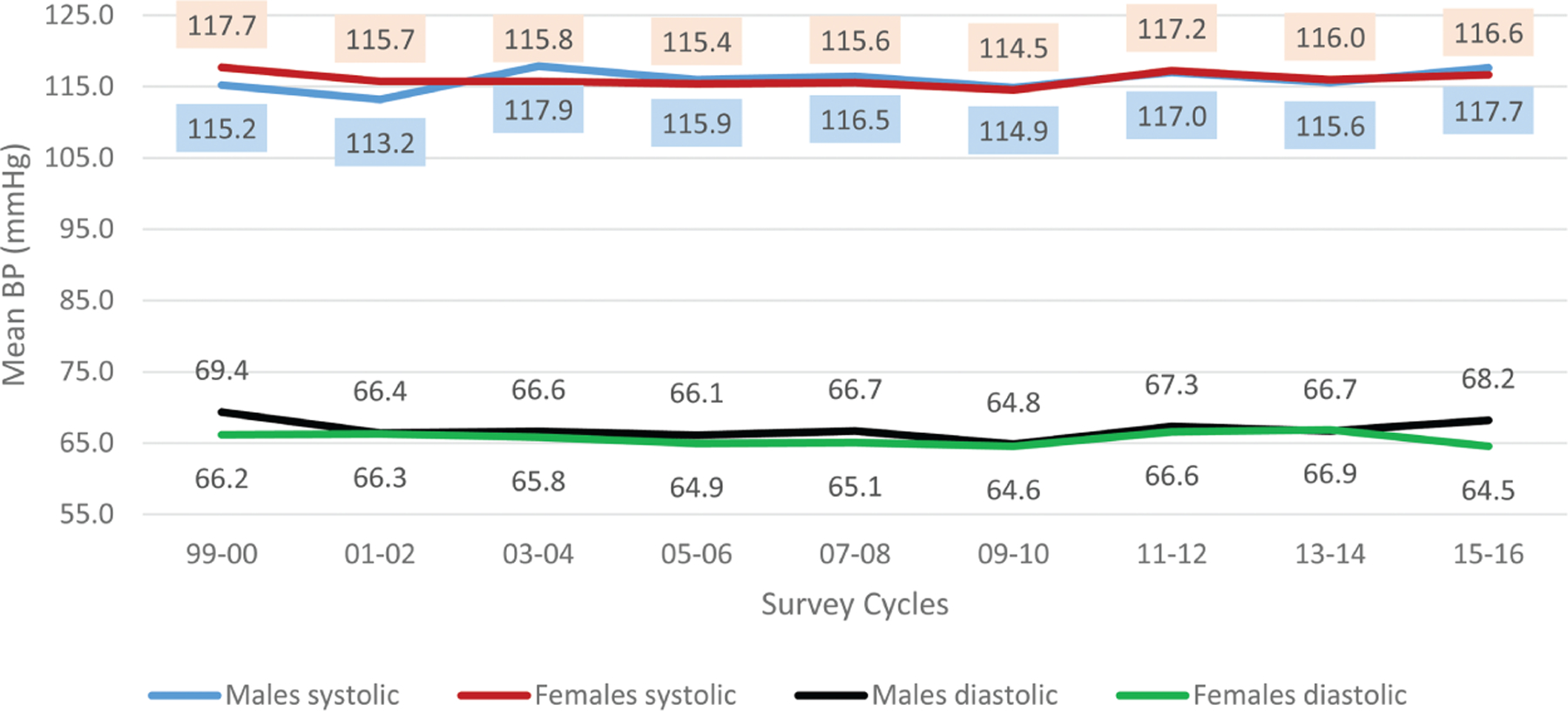
Gender-specific and age-adjusteda mean systolic and diastolic blood pressure among adults aged 18 and older with controlled hypertension,b 1999–2016. aEstimates of controlled hypertension are age-adjusted by the direct method using computed weights based on the subpopulation of persons with hypertension in the 2007–2016 National Health and Nutrition Examination Survey, 18–39, 40–59, 60–79, and 80 and older with weights 0.1661, 0.4061, 0.3446, and 0.0832. bHypertension control (BP < 130/80 mm Hg) among those with hypertension. Note: numbers in red box refer to female systolic; numbers in blue box refer to male systolic.
Characteristics of adults with controlled hypertension, 2011–2016
The percent of adults with controlled hypertension by various characteristics stratified by gender is presented in Table 1. Among adults aged 18 years and older with hypertension, the age-adjusted prevalence of hypertension control in 2011–2016 was 22.0% among men and 25.2% among women. Controlled hypertension for men was 4.0% for those aged 18–39 years; 21.3% for 40–59 years; 30.5% for 60–79 years; and 26.7% for 80 years and older. Controlled hypertension for women was 17.0% for those 18–39 years; 26.1% for 40–59 years; 29.5% for 60–79 years; and 19.8% for 80 years and older. Age-adjusted controlled hypertension among men was 24.1% for NHW; 18.1% for NHB; 15.7% for Hispanic; and 13.0% for NHA. Controlled hypertension among women was 26.5% for NHW; 24.0% for NHB; 23.4% for Hispanic; and 15.9% for NHA. Controlled hypertension prevalence estimates by survey cycles, gender, income, health care utilization, BMI categories, diagnosed, and defined CKD appear in Table 1.
Table 1.
Hypertension control among adults aged 18 years and older with hypertension by demographic, health care utilization, risk factors, and comorbidity: NHANES 2011–2016
| N | Total | Age-adjusteda |
Females (n = 3,825) | |
|---|---|---|---|---|
| Males (n = 4,147) | ||||
|
% Controlled (95% CI) | ||||
| Overall | 7,972 | 23.1 (21.3–25.0) | 22.0 (20.1–24.1) | 25.2 (22.7–28.0) |
| Survey period | ||||
| 2011–2012 | 2,587 | 23.1 (20.0–26.4) | 23.2 (20.7–26.0) | 24.2 (19.2–30.1) |
| 2013–2014 | 2,630 | 24.8 (21.9–27.8) | 22.6 (19.6–26.0) | 27.7 (24.1–31.6) |
| 2015–2016 | 2,755 | 21.7 (18.5–25.3) | 20.5 (16.8–24.8) | 23.8 (19.7–28.5) |
| Age group | ||||
| 18–39 years | 1,198 | 8.2 (6.2–10.9) | 4.0 (2.7–6.1) | 17.0 (12.8–22.1) |
| 40–59 years | 2,774 | 23.5 (20.7–26.7) | 21.3 (18.0–25.0) | 26.1 (22.3–30.4) |
| 60–79 years | 3,194 | 29.9 (27.1–33.0) | 30.5 (27.1–34.1) | 29.5 (25.8–33.4) |
| 80 years and older | 806 | 22.3 (18.4–26.7) | 26.7 (21.6–32.4) | 19.8 (15.3–25.3) |
| Race and Hispanic status | ||||
| Hispanic | 1,770 | 19.0 (17.0–21.2) | 15.7 (12.9–19.0) | 23.4 (20.4–26.7) |
| Non-Hispanic white | 3,013 | 24.6 (22.2–27.3) | 24.1 (21.4–26.9) | 26.5 (23.0–30.3) |
| Non-Hispanic black | 2,191 | 21.0 (18.9–23.4) | 18.1 (15.5–20.9) | 24.0 (21.1–27.2) |
| Non-Hispanic Asian | 774 | 14.5 (11.9–17.5) | 13.0 (9.2–18.2) | 15.9 (12.2–20.4) |
| Family income-to-poverty ratio | ||||
| Less than 1 | 1,659 | 22.7 (19.8–26.0) | 19.6 (15.1–25.1) | 26.6 (22.6–31.1) |
| 1 to less than 2 | 2,024 | 23.6 (21.2–26.2) | 20.6 (17.4–24.2) | 27.4 (23.1–32.2) |
| 2 to less than 4 | 1,852 | 23.6 (20.6–26.9) | 24.2 (20.4–28.5) | 23.9 (20.7–27.5) |
| 4 or more | 1,703 | 23.7 (20.6–27.0) | 23.7 (20.7–26.9) | 24.8 (20.2–30.1) |
| Health care visits in past year | ||||
| None | 986 | 4.7 (2.5–8.6) | 4.7 (2.0–10.8) | 5.3 (2.5–11.0) |
| 1–3 | 3,313 | 19.5 (17.1–22.1) | 19.0 (16.1–22.2) | 20.6 (17.7–23.7) |
| 4 or more | 3,666 | 31.5 (28.9–34.1) | 31.3 (28.1–34.6) | 31.9 (28.0–36.0) |
| Body mass index category | ||||
| Underweight/normal | 1,708 | 15.7 (12.6–19.4) | 14.4 (11.1–18.6) | 17.2 (12.9–22.5) |
| Overweight | 2,486 | 22.2 (19.4–25.3) | 22.0 (19.2–25.2) | 24.8 (20.2–30.1) |
| Obese | 3,667 | 26.7 (24.8–28.7) | 25.0 (22.4–27.8) | 28.9 (26.1–31.9) |
| Leisure time physical activity | ||||
| None | 4,547 | 24.5 (22.5–26.6) | 23.4 (21.0–26.0) | 26.4 (23.7–29.3) |
| Some, but <150 | 1,149 | 23.5 (20.8–26.5) | 21.9 (17.6–26.8) | 25.3 (21.0–30.2) |
| 150 or more | 2,259 | 21.2 (18.3–24.3) | 20.7 (17.6–24.2) | 23.0 (18.4–28.3) |
| Diagnosed diabetes | ||||
| Yes | 1,662 | 34.3 (30.5–38.3) | 31.6 (27.3–36.3) | 37.4 (31.9–43.3) |
| No | 6,308 | 21.2 (19.0–23.5) | 20.4 (18.1–22.9) | 23.1 (20.1–26.3) |
| Chronic kidney disease | ||||
| Yes | 1,996 | 24.3 (21.7–27.2) | 23.8 (20.4–27.6) | 25.1 (21.0–29.7) |
| No | 5,413 | 23.1 (20.9–25.6) | 22.2 (19.8–24.8) | 25.3 (22.3–28.5) |
Hypertension control (BP < 130/80 mm Hg) among those with hypertension.
Age-adjusted using the age groups 18–39, 40–59, 60–79, 80 years and older with weights 0.1661, 0.4061, 0.3446, and 0.0832.
Source: NHANES 2007–2016.
The adjusted prevalence ratios (aPR) by gender and selected covariates derived from the logistic regression models appear in Table 2. The PRs of hypertension control were significantly higher among men aged 40–59 years (aPR = 4.45, 95% CI = 2.65–7.48), 60–79 years (aPR = 5.14, 95% CI = 3.12–8.48), and 80 years and older (aPR = 4.52, 95% CI = 2.57–7.94) compared with reference men aged 18–39 years. As for women, the PRs of hypertension control were significantly higher among aged 40–59 years (aPR = 1.53, 95% CI = 1.14–2.04), 60–79 years (aPR = 1.59, 95% CI = 1.21–2.09) compared with reference women aged 18–39 years. The PRs of hypertension control were significantly lower among NHB for both men and women (aPR = 0.72, 95% CI = 0.61–0.86 and aPR = 0.83, 95% CI = 0.70–0.99), among Hispanic and NHA men (aOR = 0.70, 95% CI = 0.54–0.92 and aPR = 0.59, 95% CI = 0.39–0.89, respectively) compared with their NHW counterparts. Health care visits were significantly associated with increased PR of hypertension control for both men and women compared with the reference of no health care visits ((1–3 visits: men, aPR = 3.64, 95% CI = 1.77–7.46; women, aPR = 3.36, 95% CI = 1.53–7.36) and (≧4 visits, men, aPR = 5.79, 95% CI = 2.69–12.47; women, aPR = 4.84, 95% CI =2.23–10.48)). The PR of hypertension control was significantly associated with men who were classified as overweight (aPR = 1.42, 95% CI = 1.04–1.93) and men and women classified as obese (aPR = 1.40, 95% CI = 1.07–1.82, and aPR = 1.48, 95% CI = 1.17–1.88, respectively) compared with women and men of normal weight. Lastly, the PR of hypertension control were significantly higher among women who were diagnosed as having diabetes (aPR = 1.43, 95% CI = 1.18–1.72) compared with women not diagnosed with diabetes.
Table 2.
Adjusteda prevalence ratios for hypertension control among adults aged 18 years and older with hypertension: NHANES 2011–2016
| Males (n = 4,147) | Females (n = 3,825) | |
|---|---|---|
|
Prevalence ratio (95% CI) | ||
| Survey period | ||
| 2011–2012 | Reference | Reference |
| 2013–2014 | 0.93 (0.75–1.16) | 1.15 (0.87–1.52) |
| 2015–2016 | 0.91 (0.71–1.16) | 1.02 (0.75–1.38) |
| Age group | ||
| 18–39 years | Reference | Reference |
| 40–59 years | 4.45 (2.65–7.48) | 1.53 (1.14–2.04) |
| 60–79 years | 5.14 (3.12–8.48) | 1.59 (1.21–2.09) |
| 80 years and older | 4.52 (2.57–7.94) | 1.17 (0.77–1.80) |
| Race and Hispanic status | ||
| Hispanic | 0.70 (0.54–0.92) | 0.85 (0.71–1.01) |
| Non-Hispanic white | Reference | Reference |
| Non-Hispanic black | 0.72 (0.61–0.86) | 0.83 (0.70–0.99) |
| Non-Hispanic Asian | 0.59 (0.39–0.89) | 0.78 (0.58–1.04) |
| Family income-to-poverty ratio | ||
| Less than 1 | Reference | Reference |
| 1 to less than 2 | 1.10 (0.77–1.57) | 0.97 (0.77—1.22) |
| 2 to less than 4 | 1.28 (0.97–1.669) | 0.91 (0.72–1.16) |
| 4 or more | 1.13 (0.86–1.48) | 0.91 (0.72–1.16) |
| Health care visits in past year | ||
| None | Reference | Reference |
| 1–3 | 3.64 (1.77–7.46) | 3.36 (1.53–7.36) |
| 4 or more | 5.79 (2.69–12.47) | 4.84 (2.23–10.48) |
| Body mass index category | ||
| Underweight/normal | Reference | Reference |
| Overweight | 1.42 (1.04–1.93) | 1.26 (0.95–1.67) |
| Obese | 1.40 (1.07–1.82) | 1.48 (1.17–1.88) |
| Leisure time physical activity | ||
| None | Reference | Reference |
| Some, but less than 150 min | 0.99 (0.78–1.27) | 0.98 (0.81–1.18) |
| 150 min or more | 0.89 (0.72–1.09) | 0.98 (0.78–1.23) |
| Diagnosed diabetes | ||
| Yes | 1.24 (0.98–1.55) | 1.43 (1.18–1.72) |
| No | Reference | Reference |
| Chronic kidney disease | ||
| Yes | 0.94 (0.77–1.14) | 0.91 (0.74–1.12) |
| No | Reference | Reference |
Each variable is adjusted for all other variables in the table.
DISCUSSION
Using 2017 ACC/AHA new definition for stage I hypertension, between1999–2000 and 2015–2016, there was an overall increase in hypertension control among adults with hypertension.9 For adult men, hypertension control increased from 8.6% in 1999–2000 to 23.2% in 2011–2012, and then stabilized. As for women, hypertension control increased from 10.8% in 1999–2000 to 26.3% 2009–2010 and then stabilized.
Among men with hypertension, systolic BP decreased from 1999–2000 to 2011–2012 and then increased from 2011–2012 to 2015–2016 was small (135.7 mm Hg vs. 135.3 mm Hg); whereas among women there was a 5 mm Hg difference in systolic BP between 1999–2000 and 2015–2016 (139.7 mm Hg vs. 134.4 mm Hg). For both genders with hypertension, diastolic BP decreased between 1999–2000 and 2015–2016, specifically for men by 4 mm Hg and for women by 3 mmHg. There were no significant changes in systolic BP and diastolic BP among those with controlled hypertension for both men and women between 1999–2000 and 2015–2016.
The increase in hypertension control could be associated with the increased use of antihypertensive medication among US adults with hypertension. Using NHANES 2001–2010, Gu et al. showed the prevalence of antihypertensive medication use increased from 63.5% in 2001–2002 to 77.3% in 2009–2010. In addition, during this time period, there was a significant increase in the use of multiple antihypertensive medications from 36.8% to 47.7%.25 Similarly, using NHANES 1988–1994 and 1999–2010 data, Egan et al. showed a significant increase in antihypertension medication use among younger adults (≤60 years) from 34.6% to 54.7% and older adults (≧60 years) from 55.6% to 77.5%.26
On 13 November 2017, new guidelines establishing systolic and diastolic BP thresholds for classification of hypertension were published by ACC/AHA. These new guidelines updated the JNC 7 guideline by defining stage I hypertension as BP ≧130/80 mm Hg and stage II hypertension as BP ≧140/90 mm Hg (the latter is the JNC 7 old definition of hypertension).9 Younger people had lower stage I hypertension control compared to other age groups for both males and females in 2011–2016 (Table 1). A number of studies suggested that lower hypertension control among younger adults is driven mostly by young men being less aware and less treated than young women.15,27,28 However, the prevalence of stage II hypertension control for this age group was higher compared to those of the other age groups ((males: 74% for 18–39 years old; 67% for 40–59 years old; 62% for 60–79 years old; and 53% for 80 years and older) and (females: 80% for 18–39 years old; 75% for 40–59 years old; 61% for 60–79 years old; and 41% for 80 years and older)). Trends and factors associated with stage II hypertension control are out of scope of this article but deserve further study.
Healthy People 2020 Leading Health Indicators established BP control goals among adults with hypertension to be 61.2% by 2020.29 Our analyses showed this goal has yet to be met for stage I hypertension control.
The findings in this report are subject to some limitations. First, there is only a one-time assessment of BP by NHANES; therefore, the results may overestimate or under-estimate the prevalence of hypertension because of white-coat hypertension or masked hypertension. Together, both phenomena may represent 30% of all erroneous BP readings in a clinical setting.30 Second, misclassification of individuals could occur if they provide inaccurate information; for example, individuals reporting to be physically active when they were not, having being told by a physician that they have diabetes when they do not, individuals who were taking antihypertensive medications but did not acknowledge taking medications to lower their BP and were normotensive at the time of examination and were classified as normotensive. Also, hypertension control was defined based on use of medications. Other modalities such as low sodium diet and smoking cessation may independently contribute to BP reduction and hence increase hypertension control.31–33
Although overall from 1999 to 2010, hypertension control prevalence increased among adult men and women with stage I hypertension, these increases plateaued thereafter. Using the (ACC/AHA 2017) guidelines during 2011–2016, approximately 22% and 25% of men and women with hypertension were controlled, but this falls short of current national goals. In 2011–2016, non-Hispanic blacks of both genders, non-Hispanic Asian and Hispanic men, and women aged 80 years and older, all had lower PRs of controlling their hypertension. For both genders, increased health care visits were associated with increased PRs of hypertension control. Lastly, this is the first report using NHANES 1999–2016 data and the ACC/AHA 2017 guidelines.
Supplementary Material
Footnotes
SUPPLEMENTARY MATERIAL
Supplementary data are available at American Journal of Hypertension online.
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1.GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016; 388:1659–1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003; 42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 3.Ambrosius WT, Sink KM, Foy CG, Berlowitz DR, Cheung AK, Cushman WC, Fine LJ, Goff DC Jr, Johnson KC, Killeen AA, Lewis CE, Oparil S, Reboussin DM, Rocco MV, Snyder JK, Williamson JD, Wright JT Jr, Whelton PK; SPRINT Study Research Group. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the systolic blood pressure intervention trial (SPRINT). Clin Trials 2014; 11:532–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ezzati M, Oza S, Danaei G, Murray CJ. Trends and cardiovascular mortality effects of state-level blood pressure and uncontrolled hypertension in the United States. Circulation 2008; 117:905–914. [DOI] [PubMed] [Google Scholar]
- 5.Lawes CM, Bennett DA, Feigin VL, Rodgers A. Blood pressure and stroke: an overview of published reviews. Stroke 2004; 35:1024. [PubMed] [Google Scholar]
- 6.Zanchetti A, Thomopoulos C, Parati G. Randomized controlled trials of blood pressure lowering in hypertension: a critical reappraisal. Circ Res 2015; 116:1058–1073. [DOI] [PubMed] [Google Scholar]
- 7.Patel SA, Winkel M, Ali MK, Narayan KM, Mehta NK. Cardiovascular mortality associated with 5 leading risk factors: national and state preventable fractions estimated from survey data. Ann Intern Med 2015; 163:245–253. [DOI] [PubMed] [Google Scholar]
- 8.Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the U.S. by improvements in use of clinical preventive services. Am J Prev Med 2010; 38:600–609. [DOI] [PubMed] [Google Scholar]
- 9.Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017. doi: 10.1016/j.jacc.2017.11.005 [DOI] [PubMed] [Google Scholar]
- 10.Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National health and nutrition examination survey: sample design, 2011–2014. Vital Health Stat 2 2014; 162:1–33. [PubMed] [Google Scholar]
- 11.Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999–2010. National Center for Health Statistics. Vital Health Statistics 2013; 1–37. [PubMed] [Google Scholar]
- 12.National Center for Health Statistics, Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) Questionnaire and Exam Protocol <http://www.cdc.gov/nchs/about/major/nhanes/questexam.%20U.S>
- 13.Department of Health and Human Services. Poverty Guidelines, Research, and Measurement <https://aspe.hhs.gov/poverty-research>
- 14.Dinkler JM, Sugar CA, Escarce JJ, Ong MK, Mangione CM. Does age matter? Association between usual source of care and hypertension control in the us population: data from NHANES 2007–2012. Am J Hypertens 2016; 29:934–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ostchega Y, Hughes JP, Wright JD, McDowell MA, Louis T. Are demographic characteristics, health care access and utilization, and comorbid conditions associated with hypertension among US adults? Am J Hypertens 2008; 21:159–165. [DOI] [PubMed] [Google Scholar]
- 16.Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S. Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc 2007; 55:1056–1065. [DOI] [PubMed] [Google Scholar]
- 17.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150:604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Office of Disease Prevention and Health Promotion (ODPHP). Physical Activity Guidelines <https://health.gov/paguidelines/guide-lines/adults.aspx>. Accessed 4 April 2018.
- 19.National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res 1998; 6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 20.National Center for Health Statistics. NHANES Physical Activity Questionnaire <https://www.cdc.gov/Nchs/Nhanes/2015–2016/PAQ_I.htm>
- 21.Ogden CL, Carroll MD, Lawman HG, Cheryl D, Fryar CD, Kruszon-Moran D, Kit KD, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016; 315:2292–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crim MT, Yoon SS, Ortiz E, Wall HK, Schober S, Gillespie C, Sorlie P, Keenan N, Labarthe D, Hong Y. National surveillance definitions for hypertension prevalence and control among adults. Circ Cardiovasc Qual Outcomes 2012; 5:343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tamhane AR, Westfall AO, Burkholder GA, Cutter GR. Prevalence odds ratio versus prevalence ratio: choice comes with consequences. Stat Med 2016; 35:5730–5735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Stat Notes 2001; 20:1–10. [PubMed] [Google Scholar]
- 25.Gu Q1, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health and Nutrition Examination Survey, 2001 to 2010. Circulation 2012; 126:2105–2114. [DOI] [PubMed] [Google Scholar]
- 26.Egan BM, Li J, Shatat IF, Fuller JM, Sinopoli A. Closing the gap in hypertension control between younger and older adults: National Health and Nutrition Examination Survey (NHANES) 1988 to 2010. Circulation 2014; 129:2052–2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang Y, Moran EM. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension 2017; 70:736–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paulose-Ram R, Gu Q, Kit BK. Characteristics of U.S. adults with hypertension who are unaware of their hypertension, 2011–2014 NCHS data brief, no 278. [PubMed]
- 29.The Office of Disease Prevention and Health Promotion (ODPHP). Reduce the proportion of persons in the population with hypertension. Healthy People 2020. <https://www.healthypeople.gov/2020/topics-objectives/topic/heart-disease-and-stroke/objectives>
- 30.O’Brien E First Thomas Pickering memorial lecture*: ambulatory blood pressure measurement is essential for the management of hypertension. J Clin Hypertens (Greenwich) 2012; 14:836–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997; 336:1117–1124. [DOI] [PubMed] [Google Scholar]
- 32.Burke V, Beilin LJ, Cutt HE, Mansour J, Wilson A, Mori TA. Effects of a lifestyle programme on ambulatory blood pressure and drug dosage in treated hypertensive patients: a randomized controlled trial. J Hypertens 2005; 23:1241–1249. [DOI] [PubMed] [Google Scholar]
- 33.Ohta Y, Tsuchihashi T, Kiyohara K. Relationship between blood pressure control status and lifestyle in hypertensive outpatients. Intern Med 2011; 50:2107–2112. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


