Abstract
Background
In 2020, almost 20% of people living with HIV (PLHIV) in Morocco are still unaware of their HIV status. Under these circumstances, HIV self-test (HIVST) can be an efficient additional tool for improving the testing rates in Morocco and reaching the first objective of the UNAIDS 95–95-95 goal. ALCS, a Community-based organization, involved in HIV Testing since 1992, and the Ministry of Health of Morocco conducted, a study on the acceptability and usability of HIVST among Female sex workers (FSW) and MSM (men who have sex with men), using a salivary rapid test. To our knowledge, this is the first study in Morocco exploring these parameters.
Methods
We conducted a pilot study on the usability of the OraQuick HIV-1/2 salivary self-test among MSM and FSW visiting the ALCS centers for standard HIV rapid testing in five Moroccan cities.
Participants chose whether or not to be assisted by lay provider HIV testing. The counselors sampled them to perform a standard rapid test and then invited them to a private room to perform the HIV self-test simultaneously. In addition, a questionnaire was administered to collect socio-demographic data and to assess their opinion about the usability of the salivary HIVST.
Results
Our study was carried out for 5 months and included 492 participants (257 MSM and 233 FSW). The average age of the participants was 29 years among MSM vs 34 years among FSW. The FSW have a lower educational level, 28,8% of them are Illiterate vs. 6,1% of the MSM.
Only 18% of participants were aware of the existence of the HIVST, nevertheless, we recorded a very high rate of acceptability (90,6%) of the HIVST. Performing the HIVST was deemed very easy for 92,2% of MSM versus 80,6% of FSW. Although it was found very difficult for six participants, including five FSW, 4 of them could not read or write. Overall, the study registered a high HIV positivity rate (3,8%) and 100% of concordance between HIVST participants’ interpretation and standard HIV testing performed by ALCS lay provider HIV testing.
Conclusion
Our study shows very high acceptability of HIVST among FSWs and MSM in Morocco, HIV self-testing is still unknown by key populations in Morocco, and the low level of education of FSWs may be a barrier to the use of this test, but with the proposed assistance and adapted demonstration tools, the HIV self-testing will certainly improve access to testing in Morocco.
Keywords: HIV, Self-testing, Vulnerable populations, Acceptability, Feasibility, Usability, Morocco
Introduction
More than forty years after the discovery of the first case, HIV and Aids remain a global health crisis. In 2020, 37.7 million people were living with Human Immunodeficiency Virus (HIV) worldwide, with 1.5 million new HIV infections, and 680,000 AIDS-related deaths [1].
To reach the UNAIDS 95–95-95 target, meaning 95% of all seropositive people would know of their HIV status, 95% of them would receive antiretroviral therapy and 95% of those would suppress their viral load, in order to end the AIDS epidemic by 2030, HIV testing is the key and the first step of the HIV care cascade [2].
That target is a challenging goal for all countries worldwide [3], and particularly for HIV testing. In the world, there are nearly 6.1 million [4.9 million–7.3 million] people who still did not know their HIV serological status in 2020 [4].
The main barriers to HIV testing are stigma, discrimination, lack of confidentiality, access to testing sites, and poverty, particularly among key high-risk populations, such as female sex workers (FSW) and men who have sex with men (MSM) [5, 6].
HIV self-testing (HIVST) is an innovative tool. It’s an immunoassay test performed manually for the qualitative detection of antibodies to HIV-1 and HIV-2 in human oral fluid. An oral fluid specimen is collected using the flat pad on the test device, followed by the insertion of the test device into the vial of developer solution. A positive test result in the apparition of reddish-purple line indicating the presence of antibodies to HIV-1 and/or HIV-2 in the specimen. The test results are interpreted after 20 minutes but not more than 40 minutes after the introduction of the test device into the developer solution containing the test specimen.
HIVST and effective way, that can greatly increase the uptake of testing for people who are frequently at risk of HIV infection, especially those who have little or no access to testing due to barriers to access [7, 8]. Since 2016, the World Health Organization (WHO) has recommended the use of HIV self-testing as a safe, accurate to reach people who might not otherwise get tested, including people from key populations [9].
Internationally, and in response to WHO guidelines, in 2020, 78 countries have self-testing policies, and 41 have implemented self-testing. More and more countries are adopting HIV self-testing policies and introducing self-testing [10].
On a regional scale, UNITAID has set up two major projects, “ATLAS “and “STAR”, aiming to introduce, promote and expand HIV self-testing in Africa [11, 12]. Several recent studies conducted in sub-Saharan Africa have demonstrated high acceptability and uptake of HIVST such as in Benin [13], Uganda [14, 15], Nigeria [16], Malawi [17], Kenya [18], and Rwanda [19].
However, there is a lack of data on the acceptability of HIV self-testing in the MENA (Middle East and North Africa) region which has the lowest HIV prevalence in the world (less than 0,1%), but the fastest growing epidemic due to the increase in the number of new infections and deaths related to AIDS. Indeed with With 20,000 new infections in 2019, the region had recorded a 25% increase compared to 2010 [20]. To date, HIV self-testing kits are available in Iran since 2018 and Morocco since 2019 [21]. In Mauritania, a pilot study on the distribution of HIV self-testing kits is underway [22]. Libya, Algeria, Somalia, and Sudan are in the process of developing self-diagnosis policies [20].
In Morocco HIVST was first introduced on September 2019. At the period of this study, it was not yet authorized to sale. It was only available in the frame of “Autotest-Maroc” a demonstration project on acceptability and feasibility of HIV self-testing among key populations carried out by Association de Lutte Contre le Sida (ALCS) in partnership with the Ministry of Health, with the support of Global Fund and UNAIDS.
At the end of 2020, Morocco had an estimated 22,000 People living with HIV (PLHIV), and HIV prevalence in the general population is estimated to be 0,08% but it’s 1.7 among FSW, and 4.9 among MSM [23]. The Kingdom has made significant progress in HIV testing, thanks to the expansion of testing centers and the diversification of the offer, however almost 20% of people living with HIV (PLHIV) in Morocco are still unaware of their HIV status [23]. HIV self-testing could be a good opportunity to help fill this gap.
This study aims to explore the acceptability, and usability of HIVST among FSW and MSM, using OraQuick Rapid HIV-1/2 Antibody self-test HIV and according to recent WHO recommendations [24].
Methods
The usability evaluation of the OraQuick Rapid HIV-1/2 Antibody Test is a multicenter study performed between September 2019 to January 2020 in five Moroccan cities: Agadir, Casablanca, Marrakech, Rabat, and Tangiers.
To assess the acceptability of oral HIVST, we considered the willing to buy and use of HIVST if it’s available. The usability was assessed by the degree of ease of use and interpret of the test. We also examined the key population’s knowledge about HIV self-testing and asking for the price that they can spend to buy it if authorized to sale in future.
Study population and design
A convenience sample of 500 participants, was planned and distributed according to each city’s active file.
The participants’ recruitment has occurred in ALCS centers. The suggestion to participate was done for each beneficiary meeting the followed eligibility criteria: to self-identify as a FSW or a MSM, aged 18 years or older, requesting HIV testing at the ALCS centers during the study period, and to be able to provide informed consent. PLHIV and Pre-Exposure Prophylaxis (PrEP) users were excluded from this study, since OraQuick Rapid HIV-1/2 Antibody Test is not suitable for people on ARVs because of the risk of false negatives.
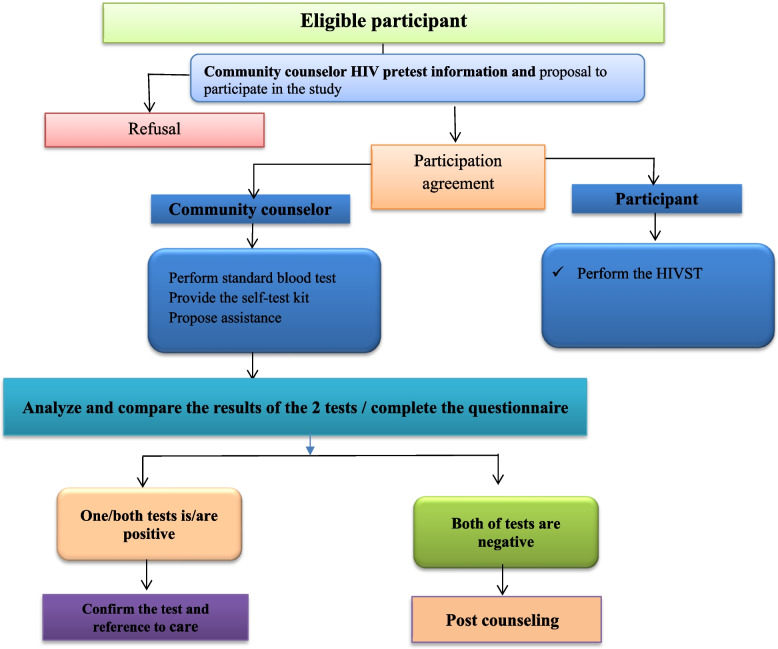
As shown in Fig. 1, all participants were provided with a salivary HIVST, OraQuick Rapid HIV-1/2 Antibody Test that they used on their own in a private room in the ALCS center and self-reported the result. In parallel, rapid standard blood testing was performed by one of the ALCS lay provider HIV testing. Instructions and assistance on using the oral HIV self-testing were also offered to participants. Lay provider HIV testing was requested to check the salivary test and report the result within 20 minutes after the participant performed it.
Fig. 1.
Participant flow
After completing the self-test, the lay provider HIV testing administrated a questionnaire to the participant and compared the results obtained by the two tests. When a participant has one or both tests positive, he was accompanied to a public care center by a Navigator to confirm the result and benefit from care and support service.
Participant involvement
The participants and members of the communities MSM and FSW were involved at several stages of this study, including the formative research which allowed us to finalize the design, the questionnaire translation, validation, data collection and results dissemination.
Data collection tool
A questionnaire was administered face to face by trained interviewers to eligible participants. The interviewers were community counselors who are also HIV testing lay providers in ALCS. The data collected was around socio-demographic features including, sex, age, sexual orientation, relationship status, employment status, education level, and to assess participants’ knowledge of HIV self-testing and their opinion on the usability of the HIV self-testing.
HIV test used for self-testing
The OraQuick Rapid HIV-1/2 Antibody t self-test HIV (OraSure Technologies, USA) was used to assess the usability of oral HIV self-testing.
This qualitative test detects antibodies to the HIV types 1 and 2 (HIV-1/2) in human oral fluid. It is read visually and provides results in 20 minutes. Moreover, this assay has a concordance of more than 99% with Western blot confirmation.
Data analysis
The software EpiData was used to collect and manage data. Categorical variables are specified as proportions, with percent and confidence intervals (95%). Quantitative variables are represented by means with IQR.
Factors associated with having any difficulty to perform HIVST were assessed using binary logistic regression. Variables with a p-value lower than 0.20 in the univariable analysis were considered eligible to enter the multivariable model. In the multivariable analysis. A backward procedure based on the Likelihood Ratio Chi-2 test was used to select variables for the final model. Statistical analysis was carried out using Stata/SE 14.0 software (StataCorp LP, College Station, USA). Given the small number of transgender people (2 persons), they are not included in this analysis.
Results
Participant’s characteristics
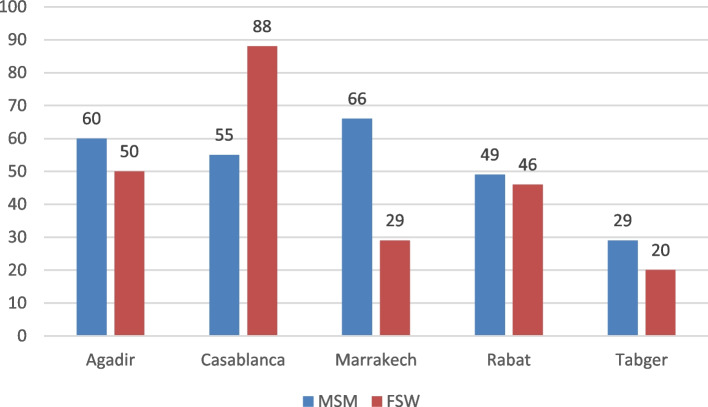
This pilot study was conducted in 5 major cities in Morocco, Agadir, Casablanca, Marrakech, Rabat, and Tangier, lasted 5 months. Eight of the 500 people to whom we suggest to participate to study refused. The included 492 participants, were 259 MSM and 233 FSW. “Fig. 2“.
Fig. 2.
Recruitment of participants in each city
The median age of participants was 27 years (IQR = 9) for MSM vs. 35 years (IQR = 13) for FSWs. The youngest and oldest participants were MSM at 18 and 76 years, respectively.
Regarding the sexual orientation of the population, we report that 73% of MSM self-identified as homosexual and 26,3% bisexual. Moreover, 90.6% of FSW self-identified as heterosexual.
The educational level and the professional situation in MSM were better compared to in FSW. Indeed, 28,8% of the FSW were illiterate vs. 6,1% of the MSM, and 79% of the FSW were unemployed or occasionally employed vs. 44% of the MSM.
We report that MSM were predominantly single and nearly half of FSW were divorced or separated. All data are summarized in Table 1.
Table 1.
Sociodemographic characteristics of study participants (MSM and FSW)
| Gender | ||||
|---|---|---|---|---|
| MSM N(%) |
MSM N(%) |
MSM N(%) |
||
| 259 (53) | 233 (47) | 492 | ||
| Mean age in years (min-max) | 29 (18–76) | 35 (19–60) | 32 (18–76) | |
| Age classes | ||||
|
18–25 CI 95 |
83 (33) 27,1%-39,1% |
43 (19) 13,8%-24,2% |
126 (26) 22,3%-30,1% |
|
|
> 25–50 CI95 |
161 (64) 57,6%-69,8% |
173 (75) 68,7%-80,3% |
334 (69) 64,8%-73,1% |
|
|
> 50–70 CI95 |
6 (2) 0,8%-5,1% |
15 (6) 3,6%-10,4% |
21 (4) 2,8%-6,5% |
|
|
> 70 CI 95 |
2 (1) 0,1%-2,8% |
0 |
2 (0.4) 0,1%-1,5% |
|
| Sexual Orientation |
Homosexual CI 95 |
188 (73.0) 67,2%-78,4% |
1 (0.4) 0,0%-2,3% |
189 (38.6) 34,3%-42,9% |
|
Bisexual CI 95 |
68 (26.3) 21,1%-32,3% |
9 (3.9) 1,7%-7,2% |
77 (15.7) 12,7%-19,2% |
|
|
Heterosexual IC 95 |
– |
211 (90.6) 86,0%-93,9% |
211 (43.1) 38,7%-47,4% |
|
|
Undefined CI 95 |
1 (0.4) 0,0%-2,1% |
12 (5.1) 2,6%-8,8% |
13 (2.6) 1,5%-4,4% |
|
| Educational level |
Illiterate CI 95 |
16 (6.1) 3,6%-9,9% |
67 (28.8) 23,0%-35,0% |
83 (16.9) 13,8%-20,5% |
|
Primary school CI 95 |
33 (12,8) 9,0%-17,5% |
56 (24) 18,7%-30,0% |
89 (18.2) 15,0%-21,8% |
|
|
Secondary CI 95 |
101 (39.3) 33,2%-45,5% |
80 (34.3) 28,2%-40,8% |
181 (37) 32,7%-41,3% |
|
|
University CI 95 |
107 (41.4) 35,5%-47,9% |
30 (12.9) 8,8%-17,8% |
137 (27.9) 24,1%-32,0% |
|
| Employment Status |
Unemployed CI 95 |
79 (30.9) 25,1%-36,7% |
123 (52.8) 46,1%-59,3% |
202 (41.2) 36,9%-45,6% |
| Nonformal employmentCI 95 |
35 (13.9) 9,6%-18,4% |
62 (26.6) 21,0%-32,7% |
97 (20) 16,5%-23,5% |
|
|
Civil servant CI 95 |
51 (19.7) 15,1%-25,2% |
15 (6.4) 3,6%-10,4% |
66 (13.4) 10,7%-16,7% |
|
|
Liberal profession CI 95 |
35 (13.5) 9,6%-18,4% |
20 (8.6) 5,3%-12,9% |
55 (11.2) 8,7%-14,3% |
|
|
Student CI 95 |
57 (22) 17,2%-27,7% |
13 (5.6) 3,0%-9,3% |
70 (14.2) 11,4%-17,6% |
|
| Relationship Status | Single |
239 (93) 89,1%-95,8% |
99 (42.4) 36,0%-49,1% |
338 (68.9) 64,7%-72,9% |
| Married |
10 (3,8) 1,8%-7,0% |
6 (2.5) 0,9%-5,5% |
16 (3.2) 2,0%-5,2% |
|
| In relationship with a stable partner |
7 (2,72) 1,1%-5,5% |
6 |
13 (2,65) 1,5%-4,4% |
|
| Divorced/separated |
1 (0,3) 0,0%-2,1% |
107 (45.9) 0,9%-5,5% |
108 (22,0) 18,6%-25,9% |
|
| widowed | 0 (0) |
15 (6.4) 3,6%-10,4% |
15 (3.0) 1,8%-4,9% |
|
Acceptability and usability of oral HIVST
We record a very high rate of acceptability of the HIVST, 90,6% of our population, both MSM and FSWs, would be ready to use it and buy it if the price was around 50 MAD (IQR = 50) which is equivalent to 5€.
We found that only 18,1% of participants were aware of the existence of the self-test before participating in this study (see Table 2).
Table 2.
Acceptability of HIVST key populations including MSM and FSW living in Morocco (n = 492)
| MSM N(%) |
FSW N(%) |
Total N(%) |
||
|---|---|---|---|---|
| Acceptability (Willing to buy and to use HIVST if available) |
Yes CI 95 |
233 (90,6) 86,4%-93,9% |
211 (90,5) 86,0%-93,9% |
444 (90,6) 87,7%-92,8% |
|
NO CI 95 |
24 (9,3) 6,0%-13,5% |
21 (9,0) 5,6%-13,4% |
45 (9,1) 6,9-12,0% |
|
| Knowledge of HIV self-testing |
Yes CI 95 |
76 (29.3) 24,0%-35,5% |
13 (5.6) 3,0%-9,3% |
89 (18,1) 15,0%-21,8% |
|
No CI 95 |
183 (70.7) 64,4%-75,9% |
220 (94.4) 90,6%-97,0% |
403 (81,8) 78,1%-85,0% |
|
| Performing the HIV self-diagnosis test | Very easy |
237 (92.2) 88,2%-95,1% |
188 (80.6) 75,0%-85,5% |
425 (86.7) 83,4%-89,4% |
| Rather easy |
15 (5.8) 3,3%-9,4% |
34 (14.5) 10,3%-19,7% |
49 (10) 7,6%-12,9% |
|
| Rather difficult |
4 (1.6) 0,4%-3,9% |
6 (2.5) 0,9%-5,5% |
10 (2,0) 1,1%-3,7% |
|
| very difficult |
1 (0.3) 0,0%-2,1% |
5 (2.1) 0,7%-4,9% |
6 (1.2) 0,5%-2,6% |
|
| Interpretation of the test results | Very easy |
231 (89,8) 85,5%-93,2% |
186 (79.8) 74,0%-84,7% |
417 (85.1) 81,6%-87,9% |
| Rather easy |
19 (7.3) 4,5%-11,3% |
37 (15.8) 11,4%-21,2% |
56 (11.4) 8,9%-14,5% |
|
| Rather difficult |
6 (2.3) 0,8%-5,0% |
6 (2.5) 0,9%-5,5% |
12 (2.4) 1,4%-4,2% |
|
| very difficult |
1 (0.3) 0,0%-2,1% |
4 (1.7) 0,4%-4,3% |
5 (1,2) 0,4%-2,3% |
Performing the salivary HIV self-test was considered very easy for 92,2% of MSM versus 80,6% of FSW. Of the 6 people who found it very difficult to perform the self-test, 5 were FSW, 4 of them could not read or write.
Bivariate analysis for level of ease in performing performing HIVST
In the univariable analysis, age, being a female sex worker, heterosexual orientation, being illiterate or having primary school level, not knowing about HIVST before and having difficulty to interpret HIVST were associated with having difficulty to perform HIVST. Being student or having a liberal profession were negatively associated with having this difficulty (Table 3).
Table 3.
Bivariate analysis for performing HIVST
| Variable | Odd ratio | Lower 95% C.I.for EXP(B) |
Upper 95% C.I.for EXP(B) |
P value |
|---|---|---|---|---|
| AGE | 1,0 | 1,0 | 1,0 | 0,010 |
| Key population | ||||
| MSM | 1,0 | |||
| FSW | 2,8 | 1,6 | 4,9 | 0,000 |
| Sexual orientation | ||||
| Homosexual | 1,0 | |||
| Bisexual | 1,2 | 0,4 | 3,2 | 0,645 |
| Heterosexual | 3,1 | 1,6 | 5,8 | 0,001 |
| Undefined | 2,2 | 0,4 | 11,2 | 0,315 |
| Education | ||||
| Illetriate or primary school | 4,2 | 1,4 | 12,52 | 0,008 |
| Secondaryor University | 1,0 | |||
| Profession | ||||
| Unemployed | 1,0 | |||
| Nonformal employment | 1,3 | 0,7 | 2,4 | 0,371 |
| Civil servant | 0,0 | 0,0 | 0,997 | |
| Liberal profession | 0,4 | 0,1 | 1,2 | 0,142 |
| Student | 0,2 | 0,0 | 0,8 | 0,023 |
| Knowledge of HIVST | ||||
| Yes | 1,0 | |||
| No | 1,6 | 0,7 | 3,6 | 0,193 |
Multivariate analysis for level of ease in performing performing HIVST
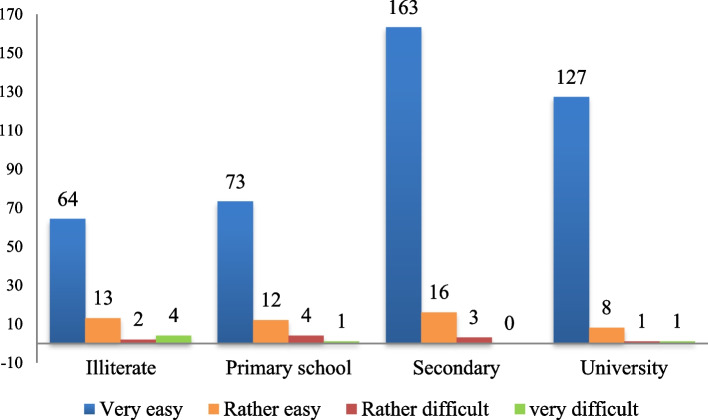
In the multivariate analysis only a low education level was significantly associated with having difficulty to perform HIVST (Table 4). What can explain that the interpretation of the OraQuick HIV Saliva Self-Test was more difficult among FSW with primary education or illiteracy. (Fig. 3).
Table 4.
Multivariate analysis for performing HIVST
| Variable | Odd ratio | Lower 95% C.I.for EXP(B) |
Upper 95% C.I.for EXP(B) |
P value |
|---|---|---|---|---|
| Key population | ||||
| MSM | 1,0 | |||
| FSW | 1,5 | 0,5 | 4,9 | 0,436 |
| Education | ||||
| Illetriate or primary school | 3,6 | 1,1 | 11,4 | 0,027 |
| Secondaryor University | 1000 | |||
Fig. 3.
Usability of HIV Self-Testing by Education level
Positive rate and concordance between HIVST and conventional blood test results
Based on participants’ interpretation of the HIVST, 18 participants were tested positive among the 492 participants, 6 FSW and 12 MSM. The results of the standard rapid blood test performed by ALCS lay provider HIV testing confirmed these results resulting in 100% concordance between the 2 tests and a global HIV-positive rate of 3.7, 4.6% in MSM, and 2.6% in FSW.
Discussion
In this pilot study, we aimed to assess the acceptability and feasibility of HIVST for FSWs and MSM and we evaluated the usability of a salivary HIVST, the OraQuick Rapid HIV-1/2 Antibody HIV self-test, in Morocco, according to WHO recommendations for the usability assessment of self-testing tools [25].
We report a high level of HIVST acceptability (90,6%) within the key populations, all the participants showed interest in using HIVST if it was available, and they would be ready to buy it if the price was around 50 MAD on average, which is equivalent to 5€.
Our findings are on acceptability are similar to recent results of pilot studies conducted in Kenya and the Democratic Republic of the Congo, with acceptability rates of 94 and 98% respectively [18, 26], showing high acceptability and uptake of HIVST in key populations.
Only 18,1% of participants were aware of the existence of the HIVST before participating in this study, 5,6% in FSW Vs 29,3% in MSM. Participants’ low level of knowledge was expected since HIVST is a relatively new screening method that is not yet available in the country. That low awareness of HIVST is also consistent with results from other studies conducted in low and middle-income countries [13].
Most participants (86.7%) deemed performing HIVST was very easy, and the vast majority (96.5%) have found that the interpretation of HIVST was rather easy or very easy. Our findings are similar to other studies such as in Benin, in sub-Saharan Africa [32], in the Democratic Republic of the Congo. [33].
However, performing OraQuick HIV Saliva Self-Test was more difficult among FSW. Indeed among the 6 people who found it very difficult to perform, 5 were FSW and it is noteworthy to stress that 4 out of the 5 could not read or write.
Our findings are consistent with many studies conducted in several contexts, which have shown that difficulties in performing HIV testing are particularly related to low levels of education [13, 26–28], particularly among FSW [29, 30].
Furthermore, we report that 18 participants were tested HIV positive, 12 are MSM (4.6%), and 6 are FSWs (2.6%). This high seropositivity among MSM is in agreement with national HIV prevalence among MSM is 4.9 [23].
Following the positive results of this study confirming the usability of this test, two other pilot studies were launched by the ALCS in collaboration with the Ministry of Health to assess the relevance of two different distribution approaches:1- peer-led distribution and, 2-Online request, and recovery in partner pharmacies. (Results not yet published).
In 2021 OraQuick HIV-1/2 rapid antibody test obtained authorization for sale and currently HIVST is available in some pharmacies in addition to remaining still available for ALCS beneficiaries belonging to key populations for free.
Limitations
This study is subject to 2 limitations. First, the re-reading of the HIVST result by the lay provider HIV testing could lead to errors in the interpretation of the tests, because it has been reported that delayed re-reading of used OraQuick HIV-1/2 rapid antibody tests is not currently a valid methodological approach to quality assurance and may overestimate true HIV-positivity [31]. The reason why all the participants had another blood test performed simultaneously by the lay provider HIV testing is to ensure the validity of the results. We also made sure that the rereading did not exceed 20 min.
The second limitation that we acknowledge is that we have used only the oral HIV self-tests, and hence, unfortunately, our results do not encompass all forms of HIV self-testing, such as blood-based HIVST.
Conclusion
In conclusion, our study shows very high acceptability for HIVST among FSWs and MSM in Morocco. HIV self-testing is still largely unknown by key populations in Morocco, and the low level of education of FSWs may be a barrier to the use of this test, but with the proposed assistance and adapted demonstration tools, the HIV self-testing will certainly improve access to testing in Morocco. Moreover, HIVST offer should be integrated with prevention services and programs that promote safer sex practices.
Acknowledgments
We would like to thank all the respondents for their time, contribution, and participation in this study. We additionally like to thank the interviewers, the National AIDS Program, the UNAIDS Country Office, The Moroccan unit of the Global Fund to fight Aids, Tuberculosis, and Malaria, and all others who were instrumental in carrying out this study.
Abbreviations
- ALCS
Association de Lutte Contre le Sida
- FSW
Female Sex Workers
- HIV
Human Immunodeficiency Virus
- HIVST
HIV self-testing
- MAD
Dirham Marocain
- MENA
the Middle East and North African
- MSM
Men who have Sex with Men
- PLHIV
People living with HIV
- PrEP
Pre-Exposure Prophylaxis
- UNAIDS
The Joint United Nations Programme on HIV and AIDS UNITAID: Global Health Agency
- WHO
The World Health Organisation
Authors’ contributions
AB led the research and led the writing of the paper. OB contributed to drafting the paper, FH, LO contributed to the interpretation of the data and the development of the idea. AE, KA, MY and BE provided critical feedback and helped shape the research, analysis, and manuscript. MK supervised the research and successive drafts of the paper. All authors read and approved the final manuscript.
Funding
This research was supported by Global Fund to fight Aids, Tuberculosis, and Malaria.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the inclusion of potentially identifying and sensitive information but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was reviewed and granted approval by Casablanca Biomedical Research Ethics Committee (IRB00002504) in the Faculty of Medicine and Pharmacy of Casablanca at the Hassan II University in Casablanca. as a study that involves no greater than minimal risk. All study methods and data collection procedures were conducted in accordance with the guidelines and recommendations of the approving IRBs. All participants provided written informed consent prior to participation in this research.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have not competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.2021 UNAIDS Global AIDS Update — Confronting inequalities — Lessons for pandemic responses from 40 years of AIDS [Internet]. [cité 16 déc 2021]. Disponible sur: https://www.unaids.org/en/resources/documents/2021/2021-global-aids-update
- 2.90–90–90 - An ambitious treatment target to help end the AIDS epidemic [Internet]. [cité 19 déc 2021]. Disponible sur: https://www.unaids.org/en/resources/documents/2017/90-90-90
- 3.2021 UNAIDS Global AIDS Update — Confronting inequalities — Lessons for pandemic responses from 40 years of AIDS | UNAIDS [Internet]. [cité 21 déc 2021]. Disponible sur: https://www.unaids.org/en/resources/documents/2021/2021-global-aids-update
- 4.Global HIV & AIDS statistics — Fact sheet [Internet]. [cité 30 déc 2021]. Disponible sur: https://www.unaids.org/en/resources/fact-sheet
- 5.Khan MNM, Sarwar G, Irfan SD, Gourab G, Rana AKMM, Khan SI. Understanding the barriers of HIV testing services for men who have sex with men and transgender women in Bangladesh: a qualitative study. Int Q Community Health Educ. 2021:272684X21995672. 10.1177/0272684X21995672. [DOI] [PubMed]
- 6.Hamilton A, Shin S, Taggart T, Whembolua G-L, Martin I, Budhwani H, et al. HIV testing barriers and intervention strategies among men, transgender women, female sex workers and incarcerated persons in the Caribbean: a systematic review. Sex Transm Infect. 2020;96:189–196. doi: 10.1136/sextrans-2018-053932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Njau B, Damian DJ, Abdullahi L, Boulle A, Mathews C. The effects of HIV self-testing on the uptake of HIV testing, linkage to antiretroviral treatment and social harms among adults in Africa: a systematic review and meta-analysis. Plos one. 2021;16(1):e0245498. doi: 10.1371/journal.pone.0245498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katz DA, Golden MR, Hughes JP, Farquhar C, Stekler JD. HIV self-testing increases HIV testing frequency in high-risk men who have sex with men: a randomized controlled trial. J Acquir Immune Defic Syndr. 2018;78(5):505–512. doi: 10.1097/QAI.0000000000001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO recommends HIV self-testing – evidence update and considerations for success [Internet]. [cité 19 déc 2021]. Disponible sur: https://www.who.int/publications-detail-redirect/WHO-CDS-HIV-19.36
- 10.WHO and partners urge countries to fast-track implementation and scale-up of HIV self-testing and other innovative HIV testing approaches in Asia and the Pacific [Internet]. [cité 16 févr 2022]. Disponible sur: https://www.who.int/news/item/16-03-2021-who-and-partners-urge-countries-to-fast-track-implementation-and-scale-up-of-hiv-self-testing-and-other-innovative-hiv-testing-approaches-in-asia-and-the-pacific
- 11.Introducing and promoting HIV self-testing in West Africa [Internet]. Unitaid. [cité 23 déc 2021]. Disponible sur: https://unitaid.org/project/introducing-and-promoting-hiv-self-testing-in-west-africa/
- 12.Expanding HIV self-testing in Africa [Internet]. Unitaid. [cité 23 déc 2021]. Disponible sur: https://unitaid.org/project/self-testing-africa-star/
- 13.Boisvert Moreau M, Kintin FD, Atchekpe S, Batona G, Béhanzin L, Guédou FA, Gagnon MP, Alary M. HIV selftesting implementation, distribution and use among female sex workers in Cotonou, Benin: a qualitative evaluation of acceptability and feasibility. BMC Public Health. 2022;22(1):589. 10.1186/s12889-022-12917-3. [DOI] [PMC free article] [PubMed]
- 14.Asiimwe S, Oloya J, Song X, Whalen CC. Accuracy of un-supervised versus provider-supervised self-administered HIV testing in Uganda: a randomized implementation trial. AIDS Behav. 2014;18:2477–2484. doi: 10.1007/s10461-014-0765-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ortblad KF, Kibuuka Musoke D, Ngabirano T, Nakitende A, Taasi G, Barresi LG, et al. HIV self-test performance among female sex workers in Kampala, Uganda: a cross-sectional study. BMJ Open. 2018;8:e022652. doi: 10.1136/bmjopen-2018-022652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown B, Folayan MO, Imosili A, Durueke F, Amuamuziam A. HIV self-testing in Nigeria: public opinions and perspectives. Glob Public Health. 2015;10:354–365. doi: 10.1080/17441692.2014.947303. [DOI] [PubMed] [Google Scholar]
- 17.Choko AT, MacPherson P, Webb EL, Willey BA, Feasy H, Sambakunsi R, et al. Uptake, accuracy, safety, and linkage into care over two years of promoting annual self-testing for HIV in Blantyre, Malawi: a community-based prospective study. PLoS Med. 2015;12:e1001873. doi: 10.1371/journal.pmed.1001873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thirumurthy H, Masters SH, Mavedzenge SN, Maman S, Omanga E, Agot K. Promoting male partner HIV testing and safer sexual decision making through secondary distribution of self-tests by HIV-negative female sex workers and women receiving antenatal and post-partum care in Kenya: a cohort study. Lancet HIV. 2016;3:e266–e274. doi: 10.1016/S2352-3018(16)00041-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dzinamarira T, Muvunyi CM, Kamanzi C, Mashamba-Thompson TP. HIV self-testing in Rwanda: awareness and acceptability among male clinic attendees in Kigali, Rwanda: a cross-sectional survey. Heliyon. 2020;6:e03515. doi: 10.1016/j.heliyon.2020.e03515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moyen-Orient et Afrique du Nord [Internet]. [cité 19 déc 2021]. Disponible sur: https://www.unaids.org/fr/regionscountries/middleeastandnorthafrica
- 21.HIV and AIDS in the Middle East & North Africa (MENA) [Internet]. Avert. 2015 [cité 23 déc 2021]. Disponible sur: https://www.avert.org/professionals/hiv-around-world/middle-east-north-africa-mena
- 22.Community outreach fills the gap in Mauritania [Internet]. [cité 4 janv 2022]. Disponible sur: https://www.unaids.org/en/resources/presscentre/featurestories/2021/november/20211125_community-outreach-mauritania
- 23.Maroc | ONUSIDA [Internet]. [cité 16 déc 2021]. Disponible sur: https://www.unaids.org/fr/regionscountries/countries/morocco
- 24.World Health Organization. Guidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services [internet]. World health Organization; 2016 [cité 19 déc 2021]. Disponible sur: https://apps.who.int/iris/handle/10665/251655 [PubMed]
- 25.WHO Prequalification of In Vitro Diagnostics PUBLIC REPORT Product: OraQuick HIV Self-Test WHO reference number: PQDx 0159-055-0 [Internet]. [cité 19 déc 2021]. Disponible sur: https://webcache.googleusercontent.com/search?q=cache:jZ6U-wsbp0sJ:https://www.who.int/diagnostics_laboratory/evaluations/pq-list/200124_amended_pqpr_0159_055_01_oraquick_hiv_self_test.pdf+&cd=3&hl=fr&ct=clnk&gl=ma
- 26.Tonen-Wolyec S, Kayembe Tshilumba C, Batina-Agasa S, Marini Djang'eing'a R, Hayette MP, Belec L. Comparison of practicability and effectiveness between unassisted HIV self-testing and directly assisted HIV self-testing in the Democratic Republic of the Congo: a randomized feasibility trial. BMC Infect Dis. 2020;20(1):830. 10.1186/s12879-020-05554-x. [DOI] [PMC free article] [PubMed]
- 27.Figueroa C, Johnson C, Dalal S, Sands A, Baggaley R. Insufficient education is a challenge for HIV self-testing – authors’ reply. Lancet HIV Elsevier. 2018;5:e341–e342. doi: 10.1016/S2352-3018(18)30142-5. [DOI] [PubMed] [Google Scholar]
- 28.Grésenguet G, Longo JD, Tonen-Wolyec S, Mboumba Bouassa RS, Belec L. Acceptability and usability evaluation of finger-stick whole blood HIV self-test as an HIV screening tool adapted to the general public in the Central African Republic. Open AIDS J. 2017;11:101-118. 10.2174/1874613601711010101. [DOI] [PMC free article] [PubMed]
- 29.Ortblad KF, Musoke DK, Ngabirano T, Nakitende A, Haberer JE, McConnell M, et al. Female sex workers often incorrectly interpret HIV self-test results in Uganda. J Acquir Immune Defic Syndr. 1999;2018(79):e42–e45. doi: 10.1097/QAI.0000000000001765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ortblad KF, Kibuuka Musoke D, Ngabirano T, Nakitende A, Taasi G, Barresi LG, et al. HIV self-test performance among female sex workers in Kampala, Uganda: a cross-sectional study. BMJ Open. 2018;8:e022652. doi: 10.1136/bmjopen-2018-022652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Watson V, Dacombe RJ, Williams C, Edwards T, Adams ER, Johnson CC, et al. Re-reading of OraQuick HIV-1/2 rapid antibody test results: quality assurance implications for HIV self-testing programmes. J Int AIDS Soc. 2019;22:e25234. doi: 10.1002/jia2.25234. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the inclusion of potentially identifying and sensitive information but are available from the corresponding author on reasonable request.