Abstract
Background:
High-intensity drinking (HID; 8+ U.S. standard drinks for women, 10+ men) is initiated during adolescence/emerging adulthood, increasing risk for negative outcomes, including blackouts. We examined baseline data from a study of risky drinking youth to identify factors associated with HID.
Methods:
Risky drinkers (ages 16-24) were recruited online (positive 3-month AUDIT-C score) as part of a larger study to examine social media interventions for risky drinking. We used baseline survey data to examine HID in relation to demographics, substance use-related variables, and individual and social factors.
Results:
Among 931 risky drinkers, 29.8% reported past-month HID, and those with HID reported greater substance use and consequences. In multivariable analysis, HID was associated with male sex; greater social motives, impulsivity, and motivation; lower self-efficacy; and greater likelihood of not living with parents, drinking with important peers, and parental disapproval of posting drinking pictures. When examining age group interactions (16-20; 21-24), underage drinkers with high sensation seeking scores and lower parental disapproval of posting drinking pictures on social media reported greater HID.
Conclusions:
Among risky drinking youth, male sex, social motives, impulsivity, higher motivation to and lower-self-efficacy to reduce drinking, living away from parents, more frequent drinking with important peers, and lower parental disapproval of posting drinking pictures on social media were positively associated with HID. Further, HID was associated with greater health consequences, underscoring the need for HID interventions. Such interventions may benefit from enhancing motivation and self-efficacy, particularly in social contexts, as well as increasing positive peer and leisure activities to reduce HID.
Keywords: high-intensity drinking, prevention, adolescents, emerging adults
Introduction
Adolescents and emerging adults comprise a high-risk group for short- and long-term consequences of alcohol use.1 Although the risks of binge drinking (typically 4+ U.S. standard drinks for women and 5+ for men) are well-established, high-intensity drinking (HID) may intensify these risks. HID involves consumption of 8+ U.S. standard drinks for biological females and 10+ for biological males.2 One in nine emerging adults report at least one past 2-week HID episode3 with men having higher rates of HID versus women.4–7 Peak HID prevalence occurs around ages 21-223,5 with men peaking (ages 21-22) prior to women (ages 21-24). One in seven high school seniors sustain a HID pattern as emerging adults.8,9 Although HID is more common among underage college students away from home and amongst their peers (10+ drinks=12.4%, 15+ drinks=5.1%) compared to same-aged non-college students (10+ drinks=9.0%, 15+ drinks=3.5%) 10, the overall prevalence in youth remains concerning.11
HID is associated with other substance use12,13, academic/occupational problems, blackouts, impaired control and driving, injury, and altered brain functioning.9,14–17 Emerging adults with HID of 15+ drinks are likely to endorse continued drinking despite serious problems (e.g., blackouts, fighting, legal issues).18 Further, alcohol use disorder prevalence among those with HID is more than twice that of those who binge drink only,19 underscoring the need for targeted prevention interventions2,18 which should be tailored for young people.5
Greater understanding of HID-related individual (e.g., motives, negative affect, attitudes) and social influences (e.g., peers, parents) may be particularly useful when creating tailored interventions.20 For example, drinking motives are potential intervention targets.21 In college students, coping, social, and enhancement motives are greater among students with HID compared to those with lower drinking.16 For high school seniors, drinking motives involving coping, enjoying the taste, increasing other drug effects, and compulsion tend to distinguish those who report HID versus less risky drinking.22 In a treatment sample, 40-60% of adolescents reported HID at baseline, and youth meeting this threshold had more drinking days than binge drinkers and non-binge drinkers, greater cannabis and illicit drug use, and more pronounced alcohol consequences.23 Over time, high levels of social and enhancement alcohol motives differentiated those with HID versus those without HID, whereas decreasing coping motives were protective.
Internalizing factors (e.g., anxiety or depression symptoms), could also be related to HID, but are relatively unexplored. Instead, depression symptoms and heavy/binge drinking among youth are generally positively associated, with some variation by sex and across development.24–26 Findings for the relationship between anxiety and heavy/binge drinking are mixed depending on the anxiety disorder examined and contextual factors surrounding drinking.27–29 Externalizing factors (e.g., impulsivity, sensation seeking) could also be related to HID given their associations with binge drinking.30
Despite the robust role of social influences on youth drinking31–33, social factors are under-explored, but likely associated with HID. For example, HID is more common on holidays, special occasions, and during sporting events which commonly involve socializing with peers.17 Similarly, college students not residing with parents are more likely to report HID.10 Parent relationship quality is protective for heavy episodic drinking during the transition to emerging adulthood34; thus, it is plausible that parental factors may be protective against HID. For example, adolescents’ perceptions of parental disapproval of drinking are protective for consumption35, which remains true in the college years.36 Given social media’s ubiquity, youths’ perceptions of parental disapproval of posting alcohol pictures on social media could also be protective, as research shows that those engaging in this behavior have greater alcohol use.37,38
To inform future targeted prevention efforts, we examined individual and social factors associated with HID among adolescents and emerging adults who screened positive for past 3-month risky drinking in randomized controlled trial (RCT) of a social media-delivered alcohol intervention.39 We characterize differences between risky drinkers with and without past-month HID on demographics and substance use-related factors. We hypothesized that those with HID would have a more severe profile of substance use, consequences, and injury/legal involvement, and that men and older ages would be more likely to report HID than women and younger ages. Given prior research23, when examining individual and social influences, we hypothesized that enhancement and social motives would be positively correlated with HID. Although the literature is mixed regarding coping motives and HID, we expected coping motives and negative affect (depression, anxiety) would be positively related to HID. Similarly, we expected greater impulsivity and sensation seeking among those with HID, whereas we did not have directional hypotheses for motivation or self-efficacy to reduce drinking. We also hypothesized that HID would be positively associated with drinking with important peers and that parental factors would be protective. Finally, given developmental differences in adolescents and emerging adults, we conducted exploratory analyses examining interactions in individual and social factors by age group (16-20; 21-24), expecting parental influences would be stronger among underage drinkers.
Method
Procedures
Procedures received approval from our Institutional Review Board. Details regarding online study procedures were previously published.39 Over 10 recruitment waves (2017-2019) we placed Facebook/Instagram ads for our study, which directed viewers to an online consent and screening survey. Trial eligibility included: age 16-24, U.S. residence, and a positive past 3-month AUDIT-C score (ages 16-17 years: ≥3 females and ≥4 males; ages 18-24 years: ≥4 females and ≥5 males).40–44 To promote sample diversity, we recruited using ethnic affinity targeting and diverse ads depicting individuals with varying racial and ethnic characteristics.
Of 11,914 individuals who self-administered our screening survey, we invited 1,541 who screened positive on the AUDIT-C and passed verification processes45,Bauermeister, Pingel, Zimmerman, Couper, Carballo-Dieguez, Strecher 46 to complete a baseline assessment ($30 gift card compensation) and submit a selfie for identity confirmation. Of 1,015 participants completing the baseline, 46 did not send a selfie, 8 did not pass the selfie verification, 4 were too busy for the study, and 2 timed out. We enrolled 955 participants in the RCT with randomization to three 8-week social media conditions: Social Media Intervention with Incentives, Social Media Intervention without Incentives, and Control. Comparison of those who completed enrollment to those who did not revealed that enrolled participants were older (M=20.4 years, SD=2.6 vs. M=20.1 years, SD=2.5; p<.05), more likely to be female (54.5% vs. 39.2%, p<.001), and had slightly lower AUDIT-C scores (M=6.6, SD=1.9 vs. M=7.0, SD=2.0; p<.001), but these two groups did not differ on racial or ethnic distribution.
The 8-week intervention conditions are detailed elsewhere.47 Briefly, interventions involved electronic coaches posting and replying to pre-determined content consistent with Motivational Interviewing and cognitive behavioral approaches to address risky drinking. The control condition included entertaining social media content as an attention-placebo. Participants completed a 3-, 6-, and 12-month online follow-up assessment.
Measures
Demographics
Demographics (e.g., age, race, ethnicity) were measured based on prior work48 and national studies.49,50
Alcohol and Other Drug Consumption
Participants completed a 30-day online Timeline Follow Back calendar51–53 and were coded as having past 30-day HID at least once (8+ drinks for women, 10+ for men) or not at all. We also calculated total number of alcohol use and HID days. To characterize other drug use, we queried past 3-month use with response options54 of 0 (never/none) to 7 (more than once a day) for: cannabis; cocaine, crack, or methamphetamine; ecstasy or molly, other illegal or recreational drug; misuse of prescription opioid pain relievers; misuse of prescription medications for sleep or anxiety; or, misuse of prescription medications for ADHD. We summed these items for a total drug use score.
Substance Use Consequences, Injury/Legal factors, and Prior Treatment
For past 3-month alcohol consequences, we modified the Brief Young Adult Alcohol Consequences Questionnaire (see39 for details) by removing two rarely endorsed items and substituting two original items reflecting property damage and fighting.55–57 We used a total consequences score among 24 items (alpha=0.93).
Driving under the influence was measured using a 3-month version of the Young Adult Driving Questionnaire’s give drinking and driving items.58 Responses (e.g., “In the past 3 months, how many times did you drive within one hour after drinking one or two beers or other alcoholic beverages?”) ranged from 0 (never) to 4 (10+ times) and we computed total scores (alpha=0.85).
Lifetime non-fatal overdose experience was queried59: “In your lifetime, how many times have you lost consciousness or taken too much drugs, alcohol, or medications/pills, or more than your body could handle?”
Past 3-month intentional injuries due to a physical fight or being physically attacked was queried (yes/no) with an item adapted from the Adolescent Injury Checklist.60 Frequency of lifetime arrests (none, once, more than once) was based on Add Health.61
Lifetime mental health and substance use treatment were queried with separate yes/no options: “Have you ever received psychological or emotional counseling?” and “Have you ever attended an alcohol or drug treatment center, including outpatient or inpatient counseling?”61
Individual and Social Factors
Past 2-week depression and anxiety symptom severity were assessed with the Patient Health Questionnaire-862 and Generalized Anxiety Disorder-7.63 Responses used a 4-point Likert scale (“not at all” to “nearly every day”); clinical cut-offs ≥10 indicated a positive screen.
Five motives items were abbreviated based on the Drinking Motives Questionnaire-Revised64 similar to prior research.65 We calculated a mean of two coping items (“because it helps you when you feel depressed or nervous” and “to cheer you up when you’re in a bad mood”; alpha=0.83). One item each queried social (“because it makes social gatherings more fun”) and enhancement (“because you like the feeling”) motives. Items were selected based on prior subscale factor loadings64,66, relevance to the population, and reading ease. Participants rated how often their drinking was motivated by each domain (response options: 1=almost never/never to 5=almost always/always).
Current motivation (i.e., importance of cutting back drinking) and self-efficacy (i.e., confidence to do so “if you wanted to”) were assessed using Motivational Interviewing-based rulers67 ranging from 1 (not at all) to 10 (very).
Impulsivity used the total score for the 8-item Barrett Impulsivity Scale68 (alpha=0.83). Sensation seeking was measured with the 4-item brief sensation seeking scale (alpha=0.78).
Based on prior work48, we quantified past 3-month frequency of drinking with important peers (“people with whom you have had contact during the past 3 months who are most important to you”). For each of five nominated individuals, participants reported frequency of alcohol use (1 = almost never/never to 5 = almost always/always) with that person, and we derived a mean score from these items.
Living with parents was assessed with a checklist of who participants lived with (yes/no).61 Parental disapproval of regular drinking69 was queried by asking: “How wrong do your parent(s) (or the people who raised you) feel it would be for you to drink regularly?”; response options included a 4-point Likert scale (“very wrong” to “not at all wrong”). Parental attitudes regarding their child posting drinking pictures on social media was assessed with an item70 asking how much they agree or disagree with the statement that their parents (or the other people who raised me) “would be upset if they found online pictures of me drinking.” Five-point Likert responses ranged from “strongly disagree” to “strongly agree.”
Analyses
We calculated descriptive statistics for the total sample and by group: risky drinkers who did or did not report past 30-day HID. Using independent samples t-tests and chi-squared analyses, we compared those with and without recent HID on the individual and social variables above. We then used logistic regression to evaluate the simultaneous relationships between demographics and individual and social variables significant in bivariate comparisons in relation to the presence or absence of past 30-day HID. Variables included in the model were correlated |<.50|. Finally, interactions by age group (underage drinkers ages 16-20 vs. legal drinkers 21-24) with individual and social factors were tested individually in the model.
Results
Participant Characteristics
Table 1 displays demographics based on HID status. Participants were M=20.4 years old (SD=2.6 years) and 54.5% were female. They were mostly White (69.9%) with representation from Black/African American persons (19.1%) and Hispanic or Latino persons individuals (20.1%). Risky drinkers with HID were significantly older and were more likely to be men and to have higher levels of education than those without HID.
Table 1.
Background Characteristics of Risky Drinkers by HID status.
| Total Sample N = 931 M (SD) or % (n) |
HID N = 285 (30.6%) M (SD) or % (n) |
No HID N = 646 (69.4%) M (SD) or % (n) |
|
|---|---|---|---|
| Demographics | |||
| Age*** | 20.4 (2.6) | 21.0 (2.3) | 20.2 (2.7) |
| Age Group** | |||
| 16-20 | 45.2% (421) | 37.9% (108) | 48.5% (313) |
| 21-24 | 54.8% (510) | 62.1% (177) | 51.6% (333) |
| Male sex*** | 45.5% (424) | 54.0% (154) | 41.8% (270) |
| Race | |||
| Black/African American | 19.1% (178) | 16.8% (48) | 20.1% (130) |
| White | 69.9% (651) | 73.3% (209) | 68.4% (442) |
| Other races | 11.0% (102) | 9.8% (28) | 11.5% (74) |
| Hispanic/Latinx | 20.1% (187) | 16.8% (48) | 21.5% (139) |
| Substance Use | |||
| Alcohol use days (past 30 days)*** | 7.8 (7.0) | 10.5 (7.4) | 6.8 (6.5) |
| Cannabis use | 62.7% (584) | 66.3% (189) | 61.2% (395) |
| Cannabis use frequency | 2.1 (2.4) | 2.2 (2.4) | 2.0 (2.4) |
| Prescription opioid misuse | 9.6% (89) | 11.6% (33) | 8.7% (56) |
| Prescription sedative misuse | 10.7% (100) | 13.0% (37) | 9.8% (63) |
| Prescription stimulant misuse* | 13.2% (123) | 17.3% (49) | 11.5% (74) |
| Ecstasy use** | 7.7% (72) | 11.9% (34) | 5.9% (38) |
| Cocaine/methamphetamine*** | 7.5% (70) | 15.4% (44) | 4.0% (26) |
| Other drugs (not cannabis)** | 35.9% (334) | 43.5% (124) | 32.5% (210) |
| Total drug use index* | 4.3 (3.4) | 4.8 (3.9) | 4.1 (3.1) |
| Consequences a | |||
| Alcohol consequences*** | 13.2 (11.4) | 19.3 (13.4) | 10.6 (9.4) |
| Driving under the influence*** | 1.6 (2.7) | 2.4 (3.7) | 1.2 (2.1) |
| Had lifetime overdose*** | 63.2% (588) | 77.2% (220) | 57.0% (368) |
| Intentional injury* | 5.4% (50) | 8.1% (23) | 4.2% (27) |
| Lifetime arrests*** | |||
| None | 86.1% (802) | 79.7% (227) | 89.0% (575) |
| Once | 10.5% (98) | 13.7% (39) | 9.1% (59) |
| More than once | 3.2% (30) | 6.3% (18) | 1.9% (12) |
| Lifetime mental health treatment | 53.5% (498) | 51.9% (148) | 54.2% (350) |
| Lifetime substance use treatment* | 6.3% (59) | 9.1% (26) | 5.1% (33) |
p < .05
p < .01
p < .001.
Time frame is last 3 months unless otherwise indicated.
Substance Use, Consequences, Injury/Legal Factors, and Treatment
The mean number of HID days for the 29.8% of participants reporting past-month HID, was 2.7 (SD=3.1, range = 1-29). Individuals with HID had a higher likelihood of most substance use-related risk factors (Table 2), including significantly more drinking days, higher total drug use, and greater use of illicit drugs than those without HID. When examining misuse of prescription drugs, only stimulants were more likely to be used by those with HID. Risky drinkers with HID reported almost twice as many recent alcohol consequences, more frequent impaired driving, and more frequent lifetime non-fatal overdose than participants without HID. Those with HID were also more likely to have a recent intentional injury and at least one lifetime arrest. Mental health treatment did not differ significantly by HID status, but substance use treatment was significantly greater among those with HID than those without.
Table 2.
Individual and Social Factors by HID status.
| Total Sample N = 931 M (SD) or % (n) |
HID N = 285 (30.6%) M (SD) or % (n) |
No HID N = 646 (69.4%) M (SD) or % (n) |
|
|---|---|---|---|
| Individual Factors | |||
| Positive anxiety screen (>=10) | 40.1% (373) | 38.6% (110) | 40.7% (263) |
| Positive depression screen (>=10) | 39.1% (364) | 37.5% (107) | 39.8% (257) |
| Coping motives | 2.6 (1.2) | 2.7 (1.3) | 2.5 (1.2) |
| Enhancement motives* | 3.7 (1.0) | 3.8 (1.0) | 3.6 (1.1) |
| Social motives*** | 4.0 (1.0) | 4.2 (0.8) | 3.9 (1.0) |
| Impulsivity ** | 17.1 (4.6) | 17.7 (4.6) | 16.8 (4.5) |
| Sensation Seeking* | 14.5 (3.3) | 14.8 (3.3) | 14.4 (3.3) |
| Motivation to reduce drinking*** | 2.9 (2.4) | 3.3 (2.5) | 2.7 (2.3) |
| Self-efficacy to reduce drinking*** | 8.5 (2.2) | 7.9 (2.4) | 8.7 (2.1) |
| Social Factors | |||
| Lives with parents*** | 39.1% (364) | 28.4% (81) | 43.8% (283) |
| Drinking with important peers*** | 2.4 (0.8) | 2.7 (0.8) | 2.3 (0.8) |
| Parent disapproval regular drinking | 2.8 (1.1) | 2.8 (1.)) | 2.8 (1.1) |
| Parent disapproval of posting drinking pictures*** | 3.4 (1.4) | 3.1 (1.4) | 3.5 (1.4) |
p < .05
p < .01
p < .001
Individual and Social Factors
Table 3 shows differences in individual and social factors by HID status. Those with HID reported significantly higher enhancement and social motives for alcohol consumption versus those without HID. Also, HID was associated with higher scores on impulsivity and sensation seeking. While participants with HID rated their motivation to reduce alcohol use significantly higher than those without HID, their self-efficacy to do so was significantly lower.
Table 3.
Logistic regression model evaluating individual and social factors in relation to HID status.
| AOR | 95% (CI) | |
|---|---|---|
| Age group (21-24 vs. 16-20 referent) | 1.11 | (0.78-1.58) |
| Male (vs. female)** | 1.52 | (1.11-2.07) |
| Total drug index | 1.03 | (0.99 -1.08) |
| Enhancement motives | 1.04 | (0.88-1.22) |
| Social motives** | 1.26 | (1.05-1.52) |
| Impulsivity* | 1.04 | (1.00-1.07) |
| Sensation-seeking | 1.01 | (0.96-1.06) |
| Motivation* | 1.08 | (1.01-1.15) |
| Self-efficacy** | 0.91 | (0.84-0.97) |
| Drinking with important peers*** | 1.52 | (1.26-1.88) |
| Lives with parents (vs. not)* | 0.60 | (0.43-0.83) |
| Parental disapproval of post drinking pictures* | 0.87 | (0.78-0.99) |
AOR= Adjusted Odds Ratios.
p < .05
p < .01
p < .001
Frequency of drinking with important peers was higher among those with HID than those without. Regarding parental influences, participants with HID were significantly less likely to live with parents. Although perceptions of parental disapproval of posting alcohol pictures was lower for those with HID versus those without, parental disapproval of regular drinking was not related to HID.
Multivariable Logistic Regression Analyses
The initial model focused on main effects of demographics, individual and social factors in relation to HID status (Table 4). Risky drinking individuals with HID were significantly more likely to be male and not live with parents; they had greater social motives, impulsivity, and motivation to reduce drinking along with lower self-efficacy. They had greater frequency of recent drinking with peers and lower parental disapproval of posting drinking pictures. In this model, total drug use, enhancement motives, and sensation seeking did not significantly differentiate risky drinkers with HID.
Subsequently, we tested interaction terms based on age group (16-20; 21-24) with individual and social factors in the model. Age-group interaction terms for sensation seeking (p<.05) and parental disapproval of posting drinking pictures (p<.01) were significant. For underage drinkers, more sensation seeking increased their probability of HID whereas sensation seeking did not affect HID risk for older drinkers; similarly, for underage drinkers, perceptions that parents would be upset if they posted drinking pictures online was protective whereas it was non-significant for legal drinkers (Figures 1–2).
Figure 1.
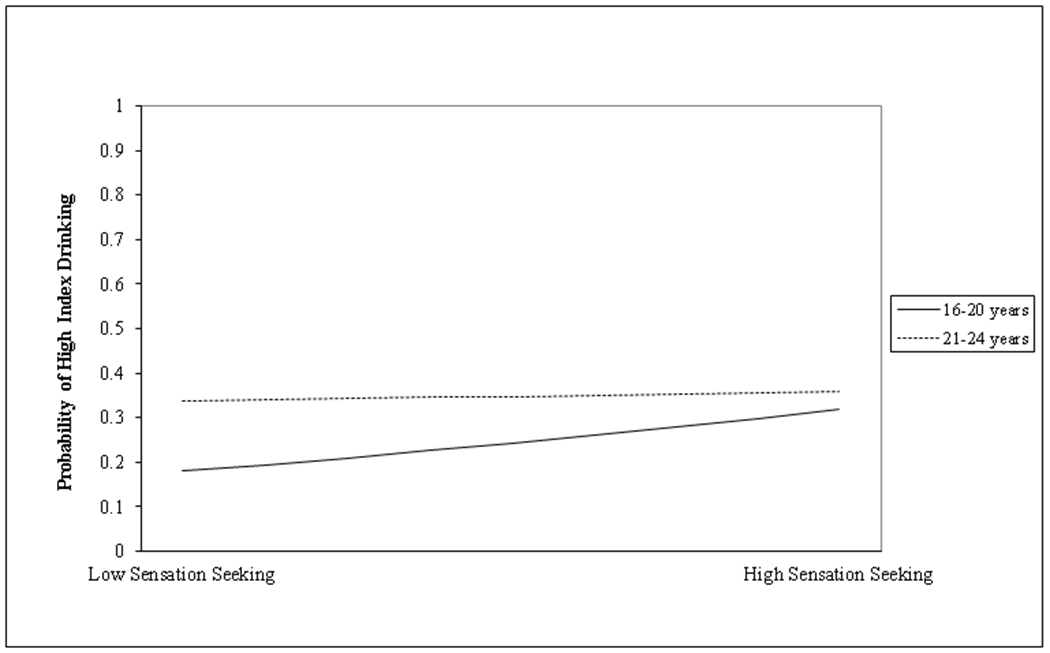
Interaction between age group and sensation seeking for HID.
Figure 2.
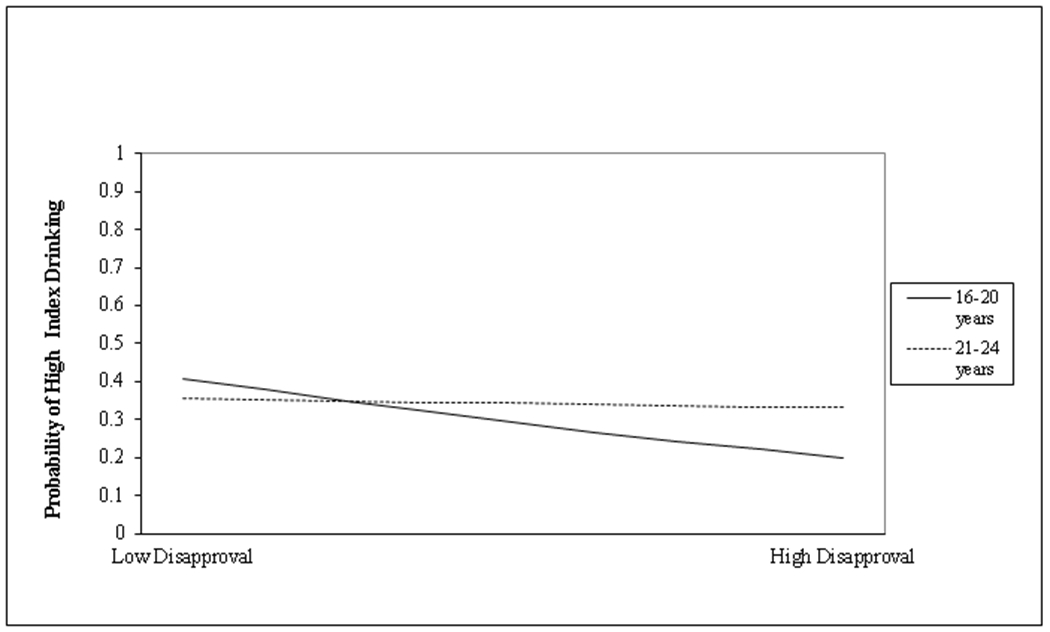
Interaction of age group by parental disapproval of posting drinking pictures online for HID.
Discussion
About a third of risky drinkers reported HID, whereas nearly two-thirds did not, underscoring a severity spectrum that should be considered when developing interventions to reduce consequences, such as blackouts. In addition to including a selective prevention sample, this research is novel in differentiating individual and social factors that set high-intensity drinkers apart from other risky drinkers.
Findings replicate and extend studies showing greater problem severity among youth with HID. Like others12,13, our data indicated that risky drinkers with HID drank more frequently, had more alcohol-related consequences, and were more likely to report impaired driving than their risky drinking counterparts who did not report past-month HID. We add novel findings that young people with HID were more likely to have a prior overdose, a past arrest, a recent intentional injury, and prior substance use treatment. Finally, data suggest that the relationship between HID and drug use is nuanced, showing no significant association with cannabis use frequency, and a positive association with illicit drug use, prescription stimulant misuse (not prescription opioids or sedatives), and total drug use involvement. These findings raise concern regarding consequences of concurrent or simultaneous of stimulants/other illicit drugs. Ecological momentary assessment studies are needed to understand the timing of co-use and associated consequences. Regardless, given our data showing substance use consequences, and legal/health consequences among risky drinkers with HID, and prior research suggesting that adolescents and emerging adults with higher alcohol consumption are less likely to respond to interventions71,72, our findings underscore the importance of identifying novel intervention approaches for HID.
To this end, we found key individual and social factors that could be addressed in interventions for those reporting HID. Specifically, although coping motives are often associated with more problematic drinking patterns73, coping motives, anxiety, and depression measures were unrelated to HID status among these risky drinkers. These findings mirror literature showing inconsistent associations between these factors and heavy drinking.27,29 Risky drinkers with HID reported greater motivation to change their drinking, potentially reflecting their experience of alcohol-related consequences, overdose, injury and legal involvement. However, motivation to reduce drinking was relatively low (~3 out of 10), suggesting that many of these individuals are likely contemplative about reducing drinking. Moreover, the negative relationship between self-efficacy to reduce drinking and HID suggests a more entrenched pattern or set of circumstances surrounding drinking that may inhibit one’s perceived ability to change, potentially reflecting their awareness of impulsivity and/or the role of social influences. Motivational interviewing74 can be used to engage and bolster the self-efficacy of pre-contemplative drinkers, and could be studied among those with HID.
Social motives and influences distinguished those with HID. Specifically, drinking for social reasons was higher amongst those with HID versus risky drinkers without HID. Therefore, HID may reflect social activities (e.g., partying) and/or a propensity for risk-taking (i.e., consistent with findings for impulsivity and sensation seeking herein). In a parallel manner, frequency of drinking with “important” peers was positively associated with HID, highlighting peer relationships as prominent intervention targets for this unique subgroup. Although we do not have data about peers’ HID, peers are amongst the most robust influences on adolescent and emerging adult drinking.31–33 Further, because living with parents was protective, it may be that individuals with greater independence have greater exposure to opportunities for heavy drinking with peers. Next, perceptions that parents disapprove of posting drinking pictures on social media were protective for HID and amplified among underage drinkers. This perception may reflect anticipated regret, which could result in less risky drinking89, and may be malleable with intervention, however, only if parents convey such disapproval, which could be beneficial public health messaging for parents. Those with HID could also benefit from emphasis on increasing motivation, confidence, and skills for identifying cognitive and behavioral strategies to reduce drinking in social situations, encouraging interaction with peers who drink at or below recommended levels, and/or by assisting youth in cultivating and sustaining non-drinking enjoyable peer-based activities. Strategies that address social network factors or capitalize on identification of opinion leaders75 or strategic players embedded proximally in one’s social network76 should be considered.
Consistent with prior research4–7, we found that male sex and older age were associated with increased HID risk, despite the lower HID threshold among females. However, among younger, underage risky drinkers, risk for HID was amplified among those with greater sensation seeking and lower perceptions of parental disapproval of posting drinking pictures, suggesting that early interventions are needed. While school or university-based interventions capture some younger-aged individuals, it is a challenge for the field to identify novel ways of reaching this at-risk population in healthcare or other community settings.77–80 In current times (i.e., coronavirus pandemic), no-contact, virtual and scalable approaches to preventing substance use problems are urgently needed81 and these could include approaches using telemedicine or social media82, given our identification of this sample via social media recruitment.
Regarding limitations, recall bias is a concern of self-report data, yet our use of a Timeline Follow-Back with event prompts aids recall and is a strength relative to surveys. We were limited to a 30-day HID measure, leaving more sporadic or seasonal HID patterns undetected. Although under-reporting may be a concern83, research supports the validity of self-reported alcohol data.84 Demand characteristics were likely lessened because surveys were confidential, participants knew that data would be separate from their names, and because there were no existing relationships between researchers and participants wherein a power differential could influence reporting. Some measures were limited to single items, potentially limiting variation. Further, the cross-sectional nature of these data preclude causality (e.g., consequences may not have occurred due to HID episodes). Additionally, factors across socio-ecological levels (e.g., alcohol policy, alcohol outlet density, parent/peer drinking behaviors) were not measured, but can influence alcohol use. We recommend that such constructs be incorporated into future HID work. Finally, results may not be generalizable at a nationally representative level to all young risky drinkers.
By examining individual and social characteristics addressable in interventions, this study illuminates important differences that distinguish high-intensity drinkers from other risky drinkers. Findings suggest that behavioral interventions address individual characteristics, like sensation seeking, impulsivity, motivation, and self-efficacy, while considering social motives for use, harnessing positive peer influences, and potentially parents (at least for underage drinkers). Future research should test interventions for this population and determine individualized content and dose required to reduce HID.
Funding:
Supported by a grant from the NIAAA #024175. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
COIs: The authors do not have any personal financial interests related to the subject matters discussed in this manuscript, with 2 exceptions. MW is a minor shareholder in Facebook and has a conflict of interest plan approved by the University of Michigan. SY has received an unrestricted gift from Facebook, on file with the University of California, Los Angeles (his prior academic appointment).
Registration: Data are from the baseline (pre-intervention) phase of a RCT. ClinicalTrials.gov Identifier: NCT02809586
References
- 1.Merrill JE, Carey KB. Drinking over the lifespan: Focus on college ages. Alcohol Res. 2016. [PMC free article] [PubMed] [Google Scholar]
- 2.Patrick ME. A Call for Research on High-Intensity Alcohol Use. Alcohol Clin Exp Res. 2016;40(2):256–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future national survey results on drug use, 1975-2015: Volume 2, College students and adults ages 19-55. Ann Arbor: Institute for Social Research, The University of Michigan;2016. [Google Scholar]
- 4.Dash GF, Davis CN, Martin NG, Statham DJ, Lynskey MT, Slutske WS. High-Intensity Drinking in Adult Australian Twins. Alcoholism: clinical and experimental research. 2020;44(2):522–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patrick ME, Terry-McElrath YM. Prevalence of High-Intensity Drinking from Adolescence through Young Adulthood: National Data from 2016–2017. Subst Abuse. 2019;13:1178221818822976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fish JN. Sexual Orientation-Related Disparities in High-Intensity Binge Drinking: Findings from a Nationally Representative Sample. LGBT Health. 2019;6(5):242–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fish JN, Schulenberg JE, Russell ST. Sexual Minority Youth Report High-Intensity Binge Drinking: The Critical Role of School Victimization. J Adolesc Health. 2019;64(2):186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patrick ME, Terry-McElrath YM, Schulenberg JE, Bray BC. Patterns of high-intensity drinking among young adults in the United States: A repeated measures latent class analysis. Addict Behav. 2017;74:134–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hingson RW, Zha W, White AM. Drinking Beyond the Binge Threshold: Predictors, Consequences, and Changes in the U.S. Am J Prev Med. 2017;52(6):717–727. [DOI] [PubMed] [Google Scholar]
- 10.Patrick ME, Terry-McElrath YM. High-intensity drinking by underage young adults in the United States. Addiction. 2017;112(1):82–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Linden-Carmichael AN, Lanza ST. Drinking Patterns of College- and Non-College-Attending Young Adults: Is High-Intensity Drinking Only a College Phenomenon? Subst Use Misuse. 2018;53(13):2157–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patrick ME, Veliz PT, Terry-McElrath YM. High-intensity and simultaneous alcohol and marijuana use among high school seniors in the United States. Substance abuse. 2017;38(4):498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCabe SE, Veliz P, Patrick ME. High-intensity drinking and nonmedical use of prescription drugs: Results from a national survey of 12th grade students. Drug Alcohol Depend. 2017;178:372–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allen HK, Calhoun BH, Maggs JL. High-risk alcohol use behavior and daily academic effort among college students. J Am Coll Health. 2020:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cox MJ, Egan KL, Suerken CK, et al. Social and situational party characteristics associated with high-intensity alcohol use among youth and young adults. Alcoholism: clinical and experimental research. 2019;43(9):1957–1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White HR, Anderson KG, Ray AE, Mun EY. Do drinking motives distinguish extreme drinking college students from their peers? Addict Behav. 2016;60:213–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patrick ME, Azar B. High-Intensity Drinking. Alcohol research : current reviews. 2018;39(1):49–55. [PMC free article] [PubMed] [Google Scholar]
- 18.Hingson RW, White A. Trends in extreme binge drinking among US high school seniors. JAMA pediatrics. 2013;167(11):996–998. [DOI] [PubMed] [Google Scholar]
- 19.Linden-Carmichael AN, Vasilenko SA, Lanza ST, Maggs JL. High-Intensity Drinking Versus Heavy Episodic Drinking: Prevalence Rates and Relative Odds of Alcohol Use Disorder Across Adulthood. Alcohol Clin Exp Res. 2017;41(10):1754–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sudhinaraset M, Wigglesworth C, Takeuchi DT. Social and cultural contexts of alcohol use: Influences in a social-ecological framework. Alcohol Res. 2016;38(1):35–45. [PMC free article] [PubMed] [Google Scholar]
- 21.Patrick ME, Evans-Polce R, Kloska DD, Maggs JL, Lanza ST. Age-Related Changes in Associations Between Reasons for Alcohol Use and High-Intensity Drinking Across Young Adulthood. Journal of studies on alcohol and drugs. 2017;78(4):558–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Terry-McElrath YM, Stern SA, Patrick ME. Do alcohol use reasons and contexts differentiate adolescent high-intensity drinking? Data from U.S. high school seniors, 2005–2016. Psychol Addict Behav. 2017;31(7):775–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Creswell KG, Chung T, Skrzynski CJ, et al. Drinking beyond the binge threshold in a clinical sample of adolescents. Addiction. 2020;115(8):1472–1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Geisner IM, Mallett K, Kilmer JR. An examination of depressive symptoms and drinking patterns in first year college students. Issues Ment Health Nurs. 2012;33(5):280–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilkinson AL, Halpern CT, Herring AH, et al. Testing Longitudinal Relationships Between Binge Drinking, Marijuana Use, and Depressive Symptoms and Moderation by Sex. J Adolesc Health. 2016;59(6):681–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pedersen DE. Gender differences in college binge drinking: Examining the role of depression and school stress. The Social Science Journal. 2013;50(4):521–529. [Google Scholar]
- 27.Dyer ML, Easey KE, Heron J, Hickman M, Munafò MR. Associations of child and adolescent anxiety with later alcohol use and disorders: a systematic review and meta-analysis of prospective cohort studies. Addiction. 2019;114(6):968–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Terlecki MA, Ecker AH, Buckner JD. College drinking problems and social anxiety: The importance of drinking context. Psychol Addict Behav. 2014;28(2):545–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Essau CA, Lewinsohn PM, Olaya B, Seeley JR. Anxiety disorders in adolescents and psychosocial outcomes at age 30. J Affect Disord. 2014;163:125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adan A, Forero DA, Navarro JF. Personality Traits Related to Binge Drinking: A Systematic Review. Frontiers in psychiatry. 2017;8:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abadi MH, Shamblen SR, Thompson K, Collins DA, Johnson K. Influence of risk and protective factors on substance use outcomes across developmental periods: A comparison of youth and young adults. Subst Use Misuse. 2011;46(13):1604–1612. [DOI] [PubMed] [Google Scholar]
- 32.Brechwald WA, Prinstein MJ. Beyond homophily: A decade of advances in understanding peer influence processes. Journal of Research on Adolescence. 2011;21(1):166–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burk WJ, Van Der Vorst H, Kerr M, Stattin H. Alcohol use and friendship dynamics: Selection and socialization in early-, middle-, and late-adolescent peer networks. J Stud Alcohol Drugs. 2012;73(1):89–98. [DOI] [PubMed] [Google Scholar]
- 34.Madkour AS, Clum G, Miles TT, et al. Parental Influences on Heavy Episodic Drinking Development in the Transition to Early Adulthood. J Adolesc Health. 2017;61(2):147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mrug S, McCay R. Parental and peer disapproval of alcohol use and its relationship to adolescent drinking: age, gender, and racial differences. Psychol Addict Behav. 2013;27(3):604–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abar CC, Morgan NR, Small ML, Maggs JL. Investigating associations between perceived parental alcohol-related messages and college student drinking. Journal of studies on alcohol and drugs. 2012;73(1):71–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moreno MA, Cox ED, Young HN, Haaland W. Underage college students’ alcohol displays on Facebook and real-time alcohol behaviors. J Adolesc Health. 2015;56(6):646–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Geusens F, Beullens K. The reciprocal associations between sharing alcohol references on social networking sites and binge drinking: A longitudinal study among late adolescents. Comput Human Behav. 2017;73:499–506. [Google Scholar]
- 39.Bonar EE, Schneeberger DM, Bourque C, et al. Social Media Interventions for Risky Drinking Among Adolescents and Emerging Adults: Protocol for a Randomized Controlled Trial. JMIR Res Protoc. 2020;9(5):e16688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chung T, Colby SM, Barnett NP, Rohsenow DJ, Spirito A, Monti PM. Screening adolescents for problem drinking: performance of brief screens against DSM-IV alcohol diagnoses. J Stud Alcohol. 2000;61(4):579–587. [DOI] [PubMed] [Google Scholar]
- 41.Chung T, Colby SM, Barnett NP, Monti PM. Alcohol use disorders identification test: factor structure in an adolescent emergency department sample. Alcoholism: Clinical and Experimental Research. 2002;26(2):223–231. [PubMed] [Google Scholar]
- 42.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Arch Intern Med. 1998;158(16):1789–1795. [DOI] [PubMed] [Google Scholar]
- 43.Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcoholism: Clinical and Experimental Research. 2005;29(5):844–854. [DOI] [PubMed] [Google Scholar]
- 44.Reinert DF, Allen JP. The alcohol use disorders identification test: an update of research findings. Alcoholism: Clinical and Experimental Research. 2007;31(2):185–199. [DOI] [PubMed] [Google Scholar]
- 45.Teitcher JE, Bockting WO, Bauermeister JA, Hoefer CJ, Miner MH, Klitzman RL. Detecting, preventing, and responding to “fraudsters” in internet research: Ethics and tradeoffs. J Law Med Ethics. 2015;43(1):116–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bauermeister JA, Pingel E, Zimmerman M, Couper M, Carballo-Dieguez A, Strecher VJ. Data quality in HIV/AIDS web-based surveys: Handling invalid and suspicious data. Field methods. 2012;24(3):272–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bonar EE, Kidwell KM, Bohnert ASB, et al. Optimizing scalable, technology-supported behavioral interventions to prevent opioid misuse among adolescents and young adults in the emergency department: A randomized controlled trial protocol. Contemp Clin Trials. 2021;108:106523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bauermeister JA, Zimmerman MA, Johns MM, Glowacki P, Stoddard S, Volz E. Innovative recruitment using online networks: Lessons learned from an online study of alcohol and other drug use utilizing a web-based, respondent-driven sampling (webRDS) strategy. J Stud Alcohol Drugs. 2012;73(5):834–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health. 2002;31(4):336–342. [DOI] [PubMed] [Google Scholar]
- 50.Bachman JG, Johnston LD, O’Malley PM, Schulenberg JE. The Monitoring the Future Project After Thirty-Seven Years: Design and Procedures. Ann Arbor, MI: Institute for Social Research;2011. [Google Scholar]
- 51.Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behav Res Ther. 1979;17(2):157–160. [DOI] [PubMed] [Google Scholar]
- 52.Hjorthøj CR, Hjorthøj AR, Nordentoft M. Validity of timeline follow-back for self-reported use of cannabis and other illicit substances—systematic review and meta-analysis. Addict Behav. 2012;37(3):225–233. [DOI] [PubMed] [Google Scholar]
- 53.Pedersen ER, Grow J, Duncan S, Neighbors C, Larimer ME. Concurrent validity of an online version of the Timeline Followback assessment. Psychol Addict Behav. 2012;26(3):672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grant B, Amsbary M, Chu A, et al. Source and accuracy statement: national epidemiologic survey on alcohol and related conditions-III (NESARC-III). https://www.niaaa.nih.gov/sites/default/files/NESARC_Final_Report_FINAL_1_8_15.pdf. Published January 2015. Accessed May 9, 2020.
- 55.Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research. 2005;29(7):1180–1189. [DOI] [PubMed] [Google Scholar]
- 56.Read JP, Kahler CW, Strong DR, Colder CR. Development and preliminary validation of the young adult alcohol consequences questionnaire. J Stud Alcohol. 2006;67(1):169–177. [DOI] [PubMed] [Google Scholar]
- 57.Read JP, Merrill JE, Kahler CW, Strong DR. Predicting functional outcomes among college drinkers: Reliability and predictive validity of the Young Adult Alcohol Consequences Questionnaire. Addict Behav. 2007;32(11):2597–2610. [DOI] [PubMed] [Google Scholar]
- 58.Donovan JE. Young adult drinking-driving: behavioral and psychosocial correlates. J Stud Alcohol. 1993;54(5):600–613. [DOI] [PubMed] [Google Scholar]
- 59.Bohnert ASB, Walton MA, Cunningham RM, et al. Overdose and adverse drug event experiences among adult patients in the emergency department. Addict Behav. 2018;86:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jelalian E, Spirito A, Rasile D, Vinick L, Rohrbeck C, Arrigan M. Risk Taking, Reported Injiry, and Perception of Future Injury Among Adolesecents. J Pediatr Psychol. 1997;22(4):513–531. [DOI] [PubMed] [Google Scholar]
- 61.Bearman PS, Jones J, Udry JR. The National Longitudinal Study of Adolescent Health: Research Design. Carolina Population Center, University of North Carolina. http://www.cpc.unc.edu/projects/addhealth. Published 1997. Accessed May 30, 2020. [Google Scholar]
- 62.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1):163–173. [DOI] [PubMed] [Google Scholar]
- 63.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 64.Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychol Assess. 1994;6(2):117. [Google Scholar]
- 65.Bonar EE, Cunningham RM, Collins RL, et al. Feasibility and Acceptability of Text Messaging to Assess Daily Substance Use and Sexual Behaviors among Urban Emerging Adults. Addiction Research & Theory 2017;26(2):103–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Grant VV, Stewart SH, O’Connor RM, Blackwell E, Conrod PJ. Psychometric evaluation of the five-factor Modified Drinking Motives Questionnaire—Revised in undergraduates. Addict Behav. 2007;32(11):2611–2632. [DOI] [PubMed] [Google Scholar]
- 67.Butler CC, Rollnick S, Cohen D, Bachmann M, Russell I, Stott N. Motivational consulting versus brief advice for smokers in general practice: a randomized trial. The British Journal of General Practice. 1999;49(445):611. [Google Scholar]
- 68.Steinberg L, Sharp C, Stanford MS, Tharp AT. New tricks for an old measure: the development of the Barratt Impulsiveness Scale-Brief (BIS-Brief). Psychol Assess. 2013;25(1):216–226. [DOI] [PubMed] [Google Scholar]
- 69.Arthur MW, Hawkins JD, Pollard JA, Catalano RF, Baglioni A Jr. Measuring risk and protective factors for use, delinquency, and other adolescent problem behaviors: The Communities That Care Youth Survey. Evaluation review. 2002;26(6):575–601. [DOI] [PubMed] [Google Scholar]
- 70.Stoddard SA, Bauermeister JA, Gordon-Messer D, Johns M, Zimmerman MA. Permissive norms and young adults’ alcohol and marijuana use: the role of online communities. J Stud Alcohol Drugs. 2012;73(6):968–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Davis AK, Arterberry BJ, Bonar EE, et al. Predictors of positive drinking outcomes among youth receiving an alcohol brief intervention in the emergency department. Drug Alcohol Depend. 2018;188:102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Becker SJ, Spirito A, Hernandez L, et al. Trajectories of adolescent alcohol use after brief treatment in an Emergency Department. Drug Alcohol Depend. 2012;125(1–2):103–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clin Psychol Rev. 2005;25(7):841–861. [DOI] [PubMed] [Google Scholar]
- 74.Miller WR, Rollnick S. Motivational Interviewing: Helping people change. 3rd ed. New York: Guilford Press; 2013. [Google Scholar]
- 75.Valente TW. Network interventions. Science. 2012;337(6090):49–53. [DOI] [PubMed] [Google Scholar]
- 76.Ott MQ, Light JM, Clark MA, Barnett NP. Strategic Players for Identifying Optimal Social Network Intervention Subjects. Soc Networks. 2018;55:97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fernandez AC, Waller R, Walton MA, et al. Alcohol use severity and age moderate the effects of brief interventions in an emergency department randomized controlled trial. Drug Alcohol Depend. 2019;194:386–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cunningham RM, Chermack ST, Ehrlich PF, et al. Alcohol Interventions Among Underage Drinkers in the ED: A Randomized Controlled Trial. Pediatrics. 2015;136(4):e783–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Levy S, Wiseblatt A, Straus JH, Strother H, Fluet C, Harris SK. Adolescent SBIRT Practices Among Pediatricians in Massachusetts. J Addict Med. 2020;14(2):145–149. [DOI] [PubMed] [Google Scholar]
- 80.Martino S, Ondersma SJ, Forray A, et al. A randomized controlled trial of screening and brief interventions for substance misuse in reproductive health. Am J Obstet Gynecol. 2018;218(3):322.e321–322.e312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lin LA, Fernandez AC, Bonar EE. Telehealth for Substance-Using Populations in the Age of Coronavirus Disease 2019: Recommendations to Enhance Adoption. JAMA psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Merchant RM. Evaluating the Potential Role of Social Media in Preventive Health Care. JAMA. 2020;323(5):411–412. [DOI] [PubMed] [Google Scholar]
- 83.Northcote J, Livingston M. Accuracy of self-reported drinking: observational verification of ‘last occasion’ drink estimates of young adults. Alcohol Alcohol. 2011;46(6):709–713. [DOI] [PubMed] [Google Scholar]
- 84.Simons JS, Wills TA, Emery NN, Marks RM. Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addict Behav. 2015;50:205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]


