Abstract
Mitral transcatheter edge-to-edge repair (MTEER) is the first transcatheter technique for mitral valve repair (MVR) in patients with severe mitral regurgitation (MR) who are considered at high risk for surgical intervention. Mitral valve prolapse with subsequent MR is a common manifestation of Marfan syndrome. MTEER has never been reported as a treatment option in such kind of patients. We describe the case of a 30-year-old patient who was known to have Marfan syndrome which was complicated with severe symptomatic MR. The surgical risk was high, and he preferred transcatheter intervention. MTEER was complicated with an immediate single-leaflet detachment of the first deployed MitraClip XTR. Bail-out edge-to-edge MVR with two additional MitraClip XTR was performed successfully to stabilize the detached clip. The patient's symptoms and quality of life improved significantly after 10 months of follow-up.
Keywords: Marfan Syndrome, MitraClip, mitral regurgitation, mitral transcatheter edge-to-edge repair, mitral valve repair
INTRODUCTION
Marfan syndrome is an autosomal dominant inherited connective tissue disease that results from a mutation of the gene that encodes for fibrillin-1 protein.[1] Wide variety of clinical presentations, of which problems in the cardiac, ocular, and musculoskeletal systems predominate.[2]
Cardiovascular manifestations of Marfan syndrome are responsible for most of the morbidity and mortality related to this disease. Aortic dilation, aneurysm, and dissection are the most worrisome findings.[3]
Mitral valve prolapse (MVP) with subsequent various degrees of mitral regurgitation (MR) is also common in Marfan syndrome and contributes, sometimes significantly, to clinical presentation and disease burden.[4]
Transcatheter percutaneous mitral valve repair (MVR) is a newly introduced method for the management of severe MR in patients with high perioperative surgical risk.[5] However, it has not been reported yet in patients with Marfan syndrome which can be related to the concept that mitral leaflets in Marfan syndrome are likely more prone to leaflet injury or partial clip detachment as the leaflets are thinner and have more elastic tissue alternation when compared to other types of degenerative MR.[6] This is the first reported case of the use ofMitral transcatheter edge-to-edge repair in Marfan patients with severe MR.
CASE PRESENTATION
A 30-year-old male patient with a known case of Marfan syndrome complicated with lens subluxation, refractory myopia, and severe kyphoscoliosis that required surgical intervention a long time ago. He presented to the emergency department complaining of progressing shortness of breath over a few weeks associated with cough and orthopnea. It was complicated with a gradual decline in his usual daily activities which got worse 10 days before presentation when he started to have dyspnea on minimal exertion like going to the bathroom and starting to use a wheelchair for ambulating. There was no chest pain, palpitation, fever, chills, rigors, or upper respiratory symptoms.
Apart from tachypnea, he was vitally stable during the initial evaluation. Upon physical examination, in addition to marfanoid features (tall stature, arachnodactyly, and high-arched palate), he was conscious and oriented, and his cardiovascular examination revealed a holosystolic murmur with the highest intensity in the apex of the heart and the murmur was radiating to the axilla. Auscultation of the lung demonstrated minimal bibasilar crackles.
Complete blood count and renal and liver function tests were within normal range. Pro Beta-type natriuretic peptide was 2858 pg/ml (normal range <125 pg/ml). Two sets of cardiac enzymes (troponin) were 19 and 17, respectively (normal range between 3 and 15 ng/L). Coronavirus (COVID-19) polymerase chain reaction test was negative.
Chest X-ray showed cardiomegaly and mild pulmonary congestion. Electrocardiogram demonstrated normal sinus rhythm. Transthoracic echocardiography (TTE) showed a normal ejection fraction = 54% with no regional wall motion abnormalities, but it revealed that the left atrium was severely dilated with moderate myxomatous changes on mitral leaflets and severe MVP. The MVP affects mainly the posterior leaflet with subsequent moderate-to-severe MR. The mitral valve regurgitation is directed anteriorly.
The patient was admitted to the cardiology team and was started on intravenous (IV) furosemide 40 mg once daily, then changed to oral after 2 days, valsartan 40 mg twice daily, and bisoprolol 2.5 mg once daily. Transesophageal echocardiography (TEE) showed a flail posterior (P2) segment causing torrential mitral valve regurgitation (MR). Computed tomography aortography revealed normal thoracic and abdominal aorta.
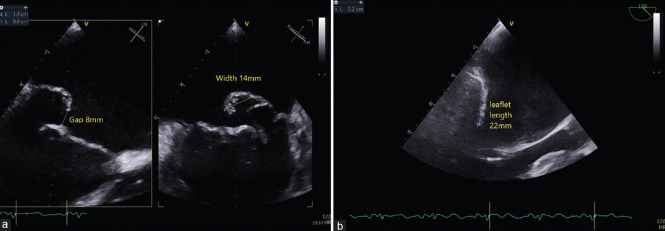
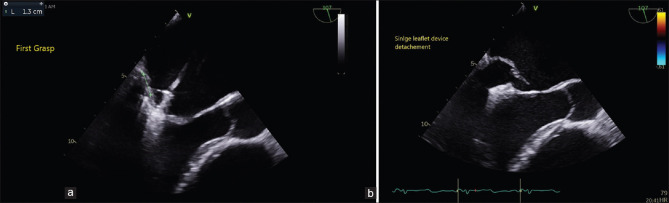
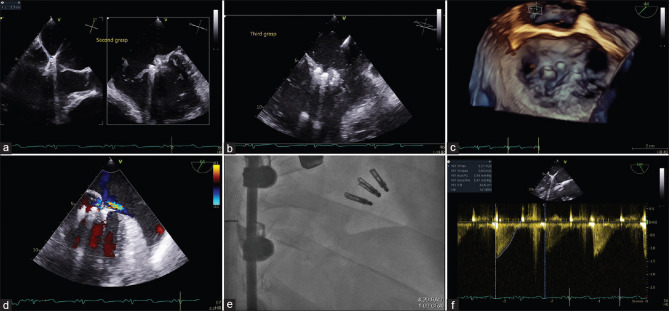
Due to his high risk for surgical morbidity, which was secondary to severe musculoskeletal deformities on the chest, obesity, decompensated heart failure, and patient preference, he was referred for mitral transcatheter edge-to-edge repair using MitraClip system which was done under TEE and fluoroscopy guidance. During the procedure, TEE revealed a wide P2 flail at 14 mm with a large gap at 8 mm and adequate posterior leaflet length at 22 mm [Figure 1]. Given this anatomy, the third-generation MitraClip XTR was utilized for the management of his prolapse. Despite the adequate grasp with the first XTR device [Figure 2a and Video 1], there was immediate single-leaflet device detachment (SLDA) from the posterior leaflet [Figure 2b and Video 2]. The partially detached device was stabilized with a second XTR lateral to its position [Figure 3a]. A third XTR clip was placed medially to treat residual medial regurgitation and to further stabilize the initial partially detached device [Figure 3b–f and Videos 3, 4].
Figure 1.
Transesophageal echocardiogram images showing wide P2 flail at 14 mm with a large gap at 8 mm. (a) with adequate posterior leaflet measured at 22 mm for MitraClip XTR device (b)
Figure 2.
Transthoracic echocardiogram image at grasping view showing an adequate grasp of 9 mm with the first MitraClip XTR device. (a) Despite the adequate grasp immediate SLDA from the posterior leaflet occurred after device release (b)
Figure 3.
Transthoracic echocardiogram image at grasping view showing placement of second MitraClip XTR lateral to first partially detached clip. (a) And the third Mitraclip XTR medial to the first partially detached clip. (b) 3D transthoracic echocardiogram image without. (c) And with (d) color Doppler and RAO Caudal fluoroscopic view (e) showing the final results with stable MitraClip devices. Continuous wave Doppler showing a mean gradient of 4 mmHg at the end of the procedure (f). RAO: Right anterior oblique
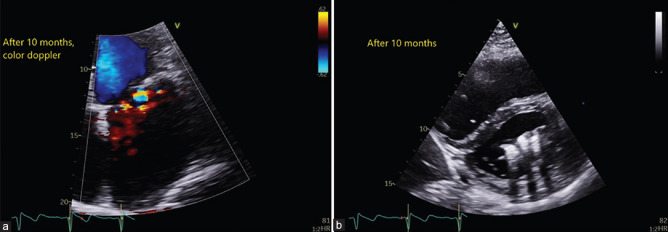
The patient was successfully discharged on the second day with residual mild MR. At the 10-month follow-up, the patient was free from heart failure rehospitalization, his lower extremity edema improved, and he was no longer using a wheelchair for mobility. His transthoracic echocardiogram revealed stable 3 × TR devices with mild residual MR and 4.5 mmHg diastolic mitral gradient [Figure 4a and b].
Figure 4.
Transthoracic echocardiogram at 10-month follow up showing mild residual mitral regurgitation (a), with stable MitraClip XTR devices (b)
DISCUSSION
Mitral valve pathology in Marfan syndrome shares some features of myxomatous degenerative mitral valve disease, such as leaflet prolapse, chordal elongation or rupture, and excess leaflet tissue.[7] However, there are some differences. According to an observational study published in 2005 that compared valve pathophysiology and morphometrics between both entities; patients with Marfan syndrome have less common posterior leaflet prolapse and more bileaflet and anterior leaflet prolapse compared with primary MVP. Both leaflets are thinner and longer in Marfan patients who usually presented earlier and are less likely to be men as compared with MVP patients.[8] These findings have raised concerns and suspicions about the efficacy and durability of MVR in patients with Marfan syndrome.
A retrospective study to evaluate the efficacy of surgical MVR of 12 patients with Marfan syndrome showed excellent survival benefits and a low rate of complications or treatment failure after a median follow-up of 60 months. Mild MR was documented in one patient (8.3%) only on the last follow-up visit, whereas others had no MR.[9] These findings were augmented by another retrospective study that compared the results of surgical MVR versus replacement in Marfan's patients, and it matched them with MVR in primary MVP patients. It exhibited that MVR is associated with better survival benefits than replacement in Marfan's patients. Survival and risk of reoperation were the same in both groups of patients treated with MVR.[10]
MTEER, using the MitraClip device, is a minimally invasive technique for MVR in patients with high surgical risk.[11] The most recent American College of Cardiology and American Heart Association guidelines of the management of valvular heart diseases gave class 2A recommendation for MTEER in patients with severe primary MR who have high or prohibitive surgical risk if mitral valve anatomy is considered appropriate for the procedure by TEE and the patient life expectancy is at least 1 year.[12]
MTEER has never been reported as a treatment option for severe MR in Marfan's patients. Our patient has severe musculoskeletal deformities that make surgical options technically difficult and at high risk. Due to the surgical risk and patient preference, he was referred for MTEER using the MitraClip system
(Abbott, Santa Clara, CA) which was done successfully. At the 10-month follow-up, the patient was free from heart failure rehospitalization, his shortness of breath and lower limbs edema improved; he was no longer using a wheelchair for mobility, and TTE revealed mild residual MR with well-grasped clips; the mitral diastolic gradient was around 4.5 mmHg.
CONCLUSION
This is the first reported case that illustrates the feasibility of MTEER in a patient with Marfan syndrome who is otherwise not suitable for surgical repair due to high surgical risk. However, there is a risk of device detachment which could be related to the thinner and more elastic tissue alternation in mitral leaflets of Marfan's patients when compared to other types of degenerative MR.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initial s will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on: www.heartviews.org
REFERENCES
- 1.Robinson PN, Arteaga-Solis E, Baldock C, Collod-Béroud G, Booms P, De Paepe A, et al. The molecular genetics of Marfan syndrome and related disorders. J Med Genet. 2006;43:769–87. doi: 10.1136/jmg.2005.039669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dietz HC, Cutting GR, Pyeritz RE, Maslen CL, Sakai LY, Corson GM, et al. Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature. 1991;352:337–9. doi: 10.1038/352337a0. [DOI] [PubMed] [Google Scholar]
- 3.McKusick VA. The cardiovascular aspects of Marfan's syndrome: A heritable disorder of connective tissue. Circulation. 1955;11:321–42. doi: 10.1161/01.cir.11.3.321. [DOI] [PubMed] [Google Scholar]
- 4.Rybczynski M, Treede H, Sheikhzadeh S, Groene EF, Bernhardt AM, Hillebrand M, et al. Predictors of outcome of mitral valve prolapse in patients with the Marfan syndrome. Am J Cardiol. 2011;107:268–74. doi: 10.1016/j.amjcard.2010.08.070. [DOI] [PubMed] [Google Scholar]
- 5.Lim DS, Reynolds MR, Feldman T, Kar S, Herrmann HC, Wang A, et al. Improved functional status and quality of life in prohibitive surgical risk patients with degenerative mitral regurgitation after transcatheter mitral valve repair. J Am Coll Cardiol. 2014;64:182–92. doi: 10.1016/j.jacc.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 6.Fleischer KJ, Nousari HC, Anhalt GJ, Stone CD, Laschinger JC. Immunohistochemical abnormalities of fibrillin in cardiovascular tissues in Marfan's syndrome. Ann Thorac Surg. 1997;63:1012–7. doi: 10.1016/s0003-4975(97)00061-1. [DOI] [PubMed] [Google Scholar]
- 7.Taub CC, Stoler JM, Perez-Sanz T, Chu J, Isselbacher EM, Picard MH, et al. Mitral valve prolapse in Marfan syndrome: An old topic revisited. Echocardiography. 2009;26:357–64. doi: 10.1111/j.1540-8175.2008.00825.x. [DOI] [PubMed] [Google Scholar]
- 8.Bhudia SK, Troughton R, Lam BK, Rajeswaran J, Mills WR, Gillinov AM, et al. Mitral valve surgery in the adult Marfan syndrome patient. Ann Thorac Surg. 2006;81:843–8. doi: 10.1016/j.athoracsur.2005.08.055. [DOI] [PubMed] [Google Scholar]
- 9.Bernhardt AM, Treede H, Detter C, Rybczynski M, Sheikhzadeh S, Wagner FM, et al. Results of modern mitral valve repair in patients with Marfan syndrome. Thorac Cardiovasc Surg. 2014;62:35–41. doi: 10.1055/s-0033-1348919. [DOI] [PubMed] [Google Scholar]
- 10.Helder MR, Schaff HV, Dearani JA, Li Z, Stulak JM, Suri RM, et al. Management of mitral regurgitation in Marfan syndrome: Outcomes of valve repair versus replacement and comparison with myxomatous mitral valve disease. J Thorac Cardiovasc Surg. 2014;148:1020–4. doi: 10.1016/j.jtcvs.2014.06.046. [DOI] [PubMed] [Google Scholar]
- 11.Maisano F, La Canna G, Colombo A, Alfieri O. The evolution from surgery to percutaneous mitral valve interventions: The role of the edge-to-edge technique. J Am Coll Cardiol. 2011;58:2174–82. doi: 10.1016/j.jacc.2011.07.046. [DOI] [PubMed] [Google Scholar]
- 12.Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, 3rd, Gentile F, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: Executive summary: A report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021;143:e35–71. doi: 10.1161/CIR.0000000000000932. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.