Abstract
Purpose
Adolescent and young adult (AYA) males historically have lower healthcare utilization than their female peers.
Methods
Electronic health record data from an Adolescent/Young Adult Medicine outpatient practice were reviewed to assess gender differences in routine health maintenance examinations before and during the COVID-19 pandemic.
Results
Routine health maintenance examinations decreased for both males and females during the pandemic. However, a two-proportion z-test demonstrated that established male patients were statistically less likely (p < .01) to have a routine health maintenance examination from December 2020 to December 2021 than their female counterparts.
Discussion
AYA males are at a higher risk for persistent disengagement in healthcare and exacerbates future gender gaps in healthcare utilization. Primary care providers need to focus efforts on re-engaging all young people in preventive care, with specific efforts tailored to AYA males.
Keywords: Adolescence, Young adults, Males, Health maintenance examination
Implications and Contribution.
The COVID-19 pandemic negatively affected routine health maintenance examinations among adolescent and young adults. However, this impact was more significant among adolescent and young adult males. This is concerning as once males are disengaged from healthcare, they are less likely to re-engage in the future.
The COVID-19 pandemic has impacted primary care access and utilization patterns, but research is still emerging regarding the distribution of these impacts. A recent retrospective study of four large academic institutions showed a significant decrease for routine pediatric healthcare visits and chronic condition follow-up between April 2019 and April 2020 [1]. Disruptions have also been noted among receipt of sexual and reproductive healthcare by adolescents in the primary care setting [[2], [3], [4], [5]]. These findings highlight the acute and potential long-term health implications surrounding missed care during the pandemic but do not address discrepancies due to gender.
Although young people face multiple barriers to care, masculinity norms may create an additional barrier for young males. Those with stronger masculine values are less likely to seek healthcare [6,7]. Historically, adolescent and young adult (AYA) males are less likely than females to have a usual source of healthcare or to have had a primary care visit within the last 12 months [8,9]. Thus, the decreases in healthcare utilization seen during the pandemic are particularly concerning for males as they already have a more tenuous connection to care [[10], [11], [12]].
In this report, we aim to describe gender differences of the COVID-19 pandemic's impact on AYAs' routine health maintenance examinations (HMEs). We use documented gender, which in the majority of cases is reflective of biological gender.
Methods
We retrospectively extracted electronic health record (EHR) data from a large academic center's Adolescent/Young Adult Medicine outpatient practice. The practice's primary care patients' demographics include age 12–26 years (primarily); insurance: 43% private and 53% public; ethnicity: 25% Latinx; and race: 38% Black, 37% unknown/declined, and 20% White. As the practice provides primary and specialty care, the primary care population was defined as AYAs with a routine HME within the three years prior to January 2019 through December 2021. A patient was considered to have an up-to-date routine HME if they had an HME within the last 18 months; time frame was established by our Accountable Care Organization. A patient was only counted once per 18-month period. Routine HMEs were identified via diagnostic codes. HMEs included physical examination, psychosocial screening, and immunizations. During the pandemic, some HMEs were offered via telehealth, with an in-person component offered as needed. Gender was defined in binary terms of male and female as documented in the EHR. Gender is reported at registration; it can subsequently be updated by patient or staff. Due to EHR limitations, “male” may include cisgender males, transgender males, nonbinary individuals who were assigned male gender at birth, and transgender females who may not have their gender updated in the EHR; “female” may also include a similar array of gender identities.
Descriptive analyses were conducted to determine the monthly number of males and females with up-to-date routine HMEs. Proportions of males and females with up-to-date routine HMEs were compared by month using Z-tests. A two-sided p value < .01 was considered statistically significant for analyses to be conservative for multiple comparisons.
The Boston Children's Hospital Institutional Review Board determined this study not to be human subjects’ research and thus was an Institutional Review Board exempt.
Results
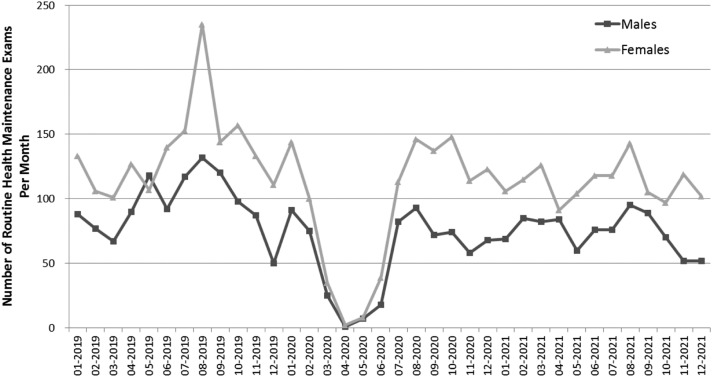
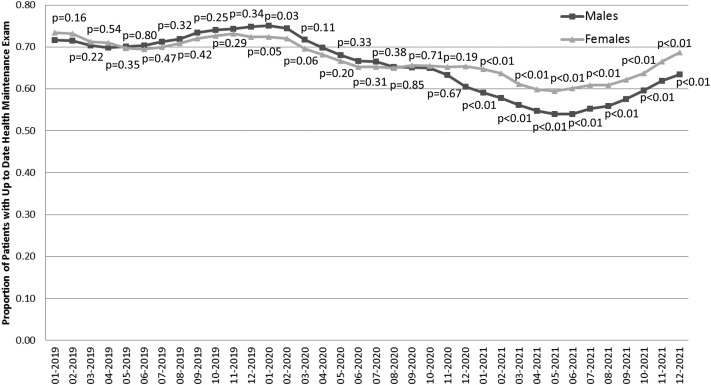
During January 2019 to December 2021, there were 6,853 routine HMEs performed. During this span, females accounted for a larger proportion of patients with an up-to-date HME (59.2% females). Following the onset of the COVID-19 pandemic in March 2020, the absolute number of routine HMEs declined for both female and male patients (Figure 1 ). The proportion of patients with an up-to-date HME also decreased for both females and males (Figure 2 ). Pre-pandemic young males engaged in care were not statistically different from females to have a routine HME. During the 13-month period of December 2020 (60.5% vs. 65.4%) to December 2021 (63.5% vs. 68.7%), AYA females were more likely to have an up-to-date HME than AYA males. There was a statistically significant (p < .01) widening of the gap between males and females from December 2020 to December 2021.
Figure 1.
Routine health maintenance examinations by gender. Monthly number of males and females with an up-to-date routine health maintenance examination (i.e., within the prior 18 months) during 2019–2021.
Figure 2.
Proportion of patients with an up-to-date health maintenance examination by gender. Comparison of proportion of males and females attending an adolescent and young adult practice with an up-to-date routine health maintenance examination (i.e., within the prior 18 months) during 2019–2021. p values shown for Z-tests comparing proportions of routine health maintenance examinations by documented gender in electronic health record.
Discussion
Our data highlight a general decrease in routine HMEs during the COVID-19 pandemic for males and females. This general decrease is consistent with other findings regarding health visits and preventive services during the pandemic [[1], [2], [3], [4], [5]]. Routine HMEs are associated with higher rates of preventive services for adolescents and young adults, such as anticipatory guidance, blood pressure checks, and influenza immunization [13]. This reduction in HMEs demonstrates a loss of these services at an age when many chronic conditions are first diagnosed [13].
In addition, our study highlights gender differences in healthcare utilization that predated the pandemic. Males have lower healthcare utilization than their female peers [[10], [11], [12]]. As of December 2020, male patients who had previously been engaged in primary care were statistically less likely than their female counterparts to have an up-to-date HME. From a health equity lens, any difference in care is concerning, especially as these young men are at risk to remain disengaged in care in the future. A recent study of well-care use patterns from childhood through adolescence found that nearly half (48%) of males were persistently disengaged in healthcare with only 18% gradually re-engaging [14]. COVID-19 may serve as the initial rupture in care which exacerbates future gender gaps in healthcare utilization and health outcomes without steps to re-engage those AYA male patients back into healthcare.
Our results have limitations. The definition of gender was limited due to EHR constraints. We also defined an up-to-date HME as 18-months rather than the 12-month ideal, due to an accountable care organization-defined measure and recognizing several potential barriers to care, especially in the setting of the pandemic. We were unable to assess whether patients had a routine HME elsewhere. Urgent care or problem-based follow-up visits were not examined. Based on prior literature, it is likely gender disparities would be exacerbated including these other visit types as AYA females have higher healthcare utilization overall. Finally, our data include patients in Massachusetts and may limit generalizability.
In conclusion, there was a decline in routine HMEs following the onset of the COVID-19 pandemic. This has disproportionately affected AYA males and may lead to future disengagement in an already vulnerable population. Thus, it is imperative that primary care providers and community stakeholders work to re-engage all young people in preventive care, with specific efforts focused on AYA males.
Acknowledgments
The authors thank Elizabeth R. Woods, M.D., for her guidance.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding Sources
This article was supported in part by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an MCHB T71MC00009 LEAH training grant. The contents are those of the authors and do not necessarily represent the official views of nor an endorsement, by HRSA, HHS, or the U.S. Government (HRSA.gov). The funders/sponsors did not participate in the work.
References
- 1.Brown C.L., Montez K., Amati J.B., et al. Impact of COVID-19 on pediatric primary care visits at four academic institutions in the Carolinas. Int J Environ Res Public Health. 2021;18:5734. doi: 10.3390/ijerph18115734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steiner R.J., Zapata L.B., Curtis K.M., et al. COVID-19 and sexual and reproductive health care: Findings from primary care providers who serve adolescents. J Adolesc Health. 2021;69:375–382. doi: 10.1016/j.jadohealth.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ott M.A., Bernard C., Wilkinson T.A. Clinician perspectives on ethics and COVID-19: Minding the gap in sexual and reproductive health. Perspect Sex Reprod Health. 2020;52:145–149. doi: 10.1363/psrh.12156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lindberg L.D., Bell D.L., Kantor L.M. The sexual and reproductive health of adolescents and young adults during the COVID-19 pandemic. Perspect Sex Reprod Health. 2020;52:75–79. doi: 10.1363/psrh.12151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mmeje O.O., Coleman J.S., Chang T. Unintended consequences of the COVID-19 pandemic on the sexual and reproductive health of youth. J Adolesc Health. 2020;67:326–327. doi: 10.1016/j.jadohealth.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcell A.V., Ford C.A., Pleck J.H., Sonenstein F.L. Masculine beliefs, parental communication and male adolescents’ health care use. Pediatrics. 2007;119:e966–e975. doi: 10.1542/peds.2006-1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tyler R.E., Williams S. Masculinity in young men’s health: Exploring health, help-seeking and health service use in an online environment. J Health Psychol. 2014;19:457–470. doi: 10.1177/1359105312473784. [DOI] [PubMed] [Google Scholar]
- 8.Adams S.H., Newacheck P.W., Park M.J., et al. Health insurance across vulnerable ages: Patterns and disparities from adolescence to the early 30s. Pediatrics. 2007;119:e1033–e1039. doi: 10.1542/peds.2006-1730. [DOI] [PubMed] [Google Scholar]
- 9.Kirzinger W.K., Cohen R.A., Gindi R.M. Health care access and utilization among young adults aged 19–25: Early release of estimates from the National Health Interview Survey, January -September 2011. Natl Cent Health Stat. 2012 www.cdc.gov/nchs/nhis/releases.htm Available at: [Google Scholar]
- 10.Lau J.S., Adams S.H., Boscardin W.J., et al. Young adults’ health care utilization and expenditures prior to the affordable care act. J Adolesc Health. 2014;54:663–671. doi: 10.1016/j.jadohealth.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Callahan S.T., Cooper W.O. Gender and uninsurance among young adults in the United States. Pediatrics. 2004;113:291–297. doi: 10.1542/peds.113.2.291. [DOI] [PubMed] [Google Scholar]
- 12.Fortuna R.J., Robbins B.W., Haterman J.S. Ambulatory care among young adults in the United States. Ann Intern Med. 2009;151:379–385. doi: 10.7326/0003-4819-151-6-200909150-00002. [DOI] [PubMed] [Google Scholar]
- 13.Adams S.H., Park M.J., Twietmeyer L., et al. Increasing delivery of preventive services to adolescents and young adults: Does the preventive visit help? J Adolesc Health. 2018;63:166–171. doi: 10.1016/j.jadohealth.2018.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Van Eck K., Thakkar M., Matson P.A., et al. Adolescents' patterns of well-care use over time: Who stays connected. Am J Prev Med. 2021;60:e221–e229. doi: 10.1016/j.amepre.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]