Abstract
Background
Depression is a common and important cause of morbidity and mortality worldwide. Depression is commonly treated with antidepressants and/or psychological therapy, but some people may prefer alternative approaches such as exercise. There are a number of theoretical reasons why exercise may improve depression. This is an update of an earlier review first published in 2009.
Objectives
To determine the effectiveness of exercise in the treatment of depression in adults compared with no treatment or a comparator intervention.
Search methods
We searched the Cochrane Depression, Anxiety and Neurosis Review Group’s Controlled Trials Register (CCDANCTR) to 13 July 2012. This register includes relevant randomised controlled trials from the following bibliographic databases: The Cochrane Library (all years); MEDLINE (1950 to date); EMBASE (1974 to date) and PsycINFO (1967 to date). We also searched www.controlled‐trials.com, ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform. No date or language restrictions were applied to the search.
We conducted an additional search of the CCDANCTR up to 1st March 2013 and any potentially eligible trials not already included are listed as 'awaiting classification.'
Selection criteria
Randomised controlled trials in which exercise (defined according to American College of Sports Medicine criteria) was compared to standard treatment, no treatment or a placebo treatment, pharmacological treatment, psychological treatment or other active treatment in adults (aged 18 and over) with depression, as defined by trial authors. We included cluster trials and those that randomised individuals. We excluded trials of postnatal depression.
Data collection and analysis
Two review authors extracted data on primary and secondary outcomes at the end of the trial and end of follow‐up (if available). We calculated effect sizes for each trial using Hedges' g method and a standardised mean difference (SMD) for the overall pooled effect, using a random‐effects model risk ratio for dichotomous data. Where trials used a number of different tools to assess depression, we included the main outcome measure only in the meta‐analysis. Where trials provided several 'doses' of exercise, we used data from the biggest 'dose' of exercise, and performed sensitivity analyses using the lower 'dose'. We performed subgroup analyses to explore the influence of method of diagnosis of depression (diagnostic interview or cut‐off point on scale), intensity of exercise and the number of sessions of exercise on effect sizes. Two authors performed the 'Risk of bias' assessments. Our sensitivity analyses explored the influence of study quality on outcome.
Main results
Thirty‐nine trials (2326 participants) fulfilled our inclusion criteria, of which 37 provided data for meta‐analyses. There were multiple sources of bias in many of the trials; randomisation was adequately concealed in 14 studies, 15 used intention‐to‐treat analyses and 12 used blinded outcome assessors.
For the 35 trials (1356 participants) comparing exercise with no treatment or a control intervention, the pooled SMD for the primary outcome of depression at the end of treatment was ‐0.62 (95% confidence interval (CI) ‐0.81 to ‐0.42), indicating a moderate clinical effect. There was moderate heterogeneity (I² = 63%).
When we included only the six trials (464 participants) with adequate allocation concealment, intention‐to‐treat analysis and blinded outcome assessment, the pooled SMD for this outcome was not statistically significant (‐0.18, 95% CI ‐0.47 to 0.11). Pooled data from the eight trials (377 participants) providing long‐term follow‐up data on mood found a small effect in favour of exercise (SMD ‐0.33, 95% CI ‐0.63 to ‐0.03).
Twenty‐nine trials reported acceptability of treatment, three trials reported quality of life, none reported cost, and six reported adverse events.
For acceptability of treatment (assessed by number of drop‐outs during the intervention), the risk ratio was 1.00 (95% CI 0.97 to 1.04).
Seven trials compared exercise with psychological therapy (189 participants), and found no significant difference (SMD ‐0.03, 95% CI ‐0.32 to 0.26). Four trials (n = 300) compared exercise with pharmacological treatment and found no significant difference (SMD ‐0.11, ‐0.34, 0.12). One trial (n = 18) reported that exercise was more effective than bright light therapy (MD ‐6.40, 95% CI ‐10.20 to ‐2.60).
For each trial that was included, two authors independently assessed for sources of bias in accordance with the Cochrane Collaboration 'Risk of bias' tool. In exercise trials, there are inherent difficulties in blinding both those receiving the intervention and those delivering the intervention. Many trials used participant self‐report rating scales as a method for post‐intervention analysis, which also has the potential to bias findings.
Authors' conclusions
Exercise is moderately more effective than a control intervention for reducing symptoms of depression, but analysis of methodologically robust trials only shows a smaller effect in favour of exercise. When compared to psychological or pharmacological therapies, exercise appears to be no more effective, though this conclusion is based on a few small trials.
Plain language summary
Exercise for depression
Why is this review important?
Depression is a common and disabling illness, affecting over 100 million people worldwide. Depression can have a significant impact on people’s physical health, as well as reducing their quality of life. Research has shown that both pharmacological and psychological therapies can be effective in treating depression. However, many people prefer to try alternative treatments. Some NHS guidelines suggest that exercise could be used as a different treatment choice. However, it is not clear if research actually shows that exercise is an effective treatment for depression.
Who may be interested in this review?
Patients and families affected by depression. General Practitioners. Mental health policy makers. Professionals working in mental health services.
What questions does this review aim to answer?
This review is an update of a previous Cochrane review from 2010 which suggested that exercise can reduce symptoms of depression, but the effect was small and did not seem to last after participants stopped exercising.
We wanted to find out if more trials of the effect of exercise as a treatment for depression have been conducted since our last review that allow us to answer the following questions:
Is exercise more effective than no therapy for reducing symptoms of depression? Is exercise more effective than antidepressant medication for reducing symptoms of depression? Is exercise more effective than psychological therapies or other non‐medical treatments for depression? How acceptable to patients is exercise as a treatment for depression?
Which studies were included in the review?
We used search databases to find all high‐quality randomised controlled trials of how effective exercise is for treating depression in adults over 18 years of age. We searched for studies published up until March 2013. We also searched for ongoing studies to March 2013. All studies had to include adults with a diagnosis of depression, and the physical activity carried out had to fit criteria to ensure that it met with a definition of ‘exercise’.
We included 39 studies with a total of 2326 participants in the review. The reviewers noted that the quality of some of the studies was low, which limits confidence in the findings. When only high‐quality trials were included, exercise had only a small effect on mood that was not statistically significant.
What does the evidence from the review tell us?
Exercise is moderately more effective than no therapy for reducing symptoms of depression. Exercise is no more effective than antidepressants for reducing symptoms of depression, although this conclusion is based on a small number of studies. Exercise is no more effective than psychological therapies for reducing symptoms of depression, although this conclusion is based on small number of studies. The reviewers also note that when only high‐quality studies were included, the difference between exercise and no therapy is less conclusive. Attendance rates for exercise treatments ranged from 50% to 100%. The evidence about whether exercise for depression improves quality of life is inconclusive.
What should happen next?
The reviewers recommend that future research should look in more detail at what types of exercise could most benefit people with depression, and the number and duration of sessions which are of most benefit. Further larger trials are needed to find out whether exercise is as effective as antidepressants or psychological treatments.
Summary of findings
Background
Description of the condition
Depression refers to a wide range of mental health problems characterised by the absence of a positive affect (a loss of interest and enjoyment in ordinary things and experiences), persistent low mood and a range of associated emotional, cognitive, physical and behavioural symptoms (NICE 2009).
Severity of depression is classified using the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM‐IV) criteria as mild (five or more symptoms with minor functional impairment), moderate (symptoms or functional impairment are between 'mild' and 'severe') and severe (most symptoms present and interfere with functioning, with or without psychotic symptoms) (NICE 2009). Depression is common, affecting 121 million adults worldwide, and rated as the fourth leading cause of disease burden in 2000 (Moussavi 2007). Depression is an important cause of morbidity and mortality and produces the greatest decrement in health compared with other chronic diseases such as angina or arthritis (Moussavi 2007).
Description of the intervention
Depression is commonly treated with antidepressants or psychological therapies or a combination of both. Antidepressants are effective for the treatment of depression in primary care (Arroll 2009). However antidepressants may have adverse side effects, adherence can be poor, and there is a lag time between starting antidepressants and improvements in mood. Psychological treatments are generally free from side effects and are recommended in the UK National Institute for Health and Clinical Excellence (NICE) guidelines (NICE 2009) but some people may not wish to receive psychological therapy due to low expectations of positive outcome or perceived stigma. Psychological therapy also requires sustained motivation and a degree of psychological mindedness in order to be effective. Depression is a well‐recognised reason for seeking alternative therapies (Astin 1998). Whilst this may reflect dissatisfaction with conventional treatments, another possibility is that alternative therapies may be more in line with people's own beliefs and philosophies (Astin 1998). There has been increasing interest in the potential role of alternative therapies such as music therapy, light therapy, acupuncture, family therapy, marital therapy, relaxation and exercise for the management of depression.
Exercise is defined as the "planned, structured and repetitive bodily movement done to improve or maintain one or more components of physical fitness" (ACSM 2001). The effect of exercise on depression has been the subject of research for several decades and is believed by a number of researchers and clinicians to be effective in the treatment of depression (Beesley 1997). This reflects an historic perspective on the role of aerobic exercise prescription for depression. For example, a report for the National Service Framework for Mental Health suggested that exercise should be included as a treatment option for people with depression (Donaghy 2000). The NICE guideline for depression recommended structured, supervised exercise programmes, three times a week (45 minutes to one hour) over 10 to 14 weeks, as a low‐intensity Step 2 intervention for mild to moderate depression (NICE 2009). A recent guideline published by the Scottish Intercollegiate Guidelines Network (SIGN) for non‐pharmaceutical management of depression in adults recommended that structured exercise may be considered as a treatment option for people with depression (graded 'B' relating to the strength of the evidence on which the recommendation was based) (SIGN 2010). Exercise programmes can be offered in the UK through Exercise Referral Systems (DOH 2001). These schemes direct someone to a service offering an assessment of need, development of a tailored physical activity programme, monitoring of progress and follow‐up. However, a systematic review of exercise on prescription schemes found limited evidence about their effectiveness and recommended further research (Sorensen 2006), and a further more recent review found that there was still considerable uncertainty about the effectiveness of exercise referral schemes for increasing physical activity, fitness, or health indicators, or whether they are an efficient use of resources for sedentary people (Pavey 2011). A second recent review noted that most trials in this area that have previously been included in systematic reviews recruit participants from outside of health services, making it difficult to assess whether prescribing exercise in a clinical setting (i.e. when a health professional has made a diagnosis of depression) is effective (Krogh 2011). In that review, studies were restricted only to those trials in which participants with a clinical diagnosis of depression were included, and the authors found no evidence of an effect of exercise in these trials (Krogh 2011). NICE concluded that there was insufficient evidence to recommend Exercise Referral Schemes other than as part of research studies to evaluate their effectiveness. Thus, whilst the published guidelines recommend exercise for depression, NICE recommends that Exercise Referral Schemes, to which people with depression are referred, need further evaluation.
This review focuses on exercise defined according to American College of Sports Medicine (ACSM) criteria. Whilst accepting that other forms of bodily movement may be effective, some of these are the subjects of other reviews.
How the intervention might work
Observational studies have shown that depression is associated with low levels of physical activity (Smith 2013). Whilst an association between two variables does not necessarily imply causality, there are plausible reasons why physical activity and exercise may improve mood. Exercise may act as a diversion from negative thoughts, and the mastery of a new skill may be important (LePore 1997). Social contact may be part of the mechanism. Craft 2005 found support for self efficacy as the mechanism by which exercise might have an antidepressant effect; people who experienced an improvement in mood following exercise showed higher self efficacy levels at three weeks and nine weeks post‐exercise. Self efficacy has been found to be intricately linked with self esteem, which in turn is considered to be one of the strongest predictors of overall, subjective well‐being (Diener 1984). Low self esteem is also considered to be closely related to mental illness (Fox 2000). Physical activity may have physiological effects such as changes in endorphin and monoamine levels, or reduction in the levels of the stress hormone cortisol (Chen 2013), all of which may improve mood. Exercise stimulates growth of new nerve cells and release of proteins known to improve health and survival of nerve cells, e.g. brain‐derived growth neurotrophic factor (Cotman 2002; Ernst 2005).
Why it is important to do this review
Several systematic reviews and meta‐analyses (Blake 2009; Carlson 1991; Craft 2013; Krogh 2011; Lawlor 2001; North 1990; Pinquart 2007; Rethorst 2009; Sjosten 2006; Stathopoulou 2006; Sorensen 2006) have looked at the effect of exercise on depression. However, five of these reviews pooled data from a range of study types that included uncontrolled studies and randomised as well as non‐randomised controlled trials, and pooled data from trials that compared exercise without treatment with data from trials that compared exercise and other forms of treatment (Blake 2009; Carlson 1991; Craft 2013; North 1990; Pinquart 2007). Two included trials predominantly of older people (Blake 2009; Sjosten 2006). One meta‐analysis (Stathopoulou 2006) included only publications from peer‐reviewed journals even though it is widely acknowledged that positive trials are more likely to be published than negative or inconclusive trials. The Cochrane Handbook for Systematic Reviews of Interventions recommends comprehensive searching for all trials, including unpublished ones, to avoid bias (Handbook 2011). Two meta‐analyses which included assessments of study quality both cautiously concluded that exercise may be effective, but recommended that further well‐designed trials are required (Lawlor 2001; Sjosten 2006). One meta‐analysis (Rethorst 2009) concluded that exercise is effective as a treatment for depression, but suggested that further conclusive results are necessary for exercise to become a recommended form of treatment. When only studies recruiting participants from a clinical setting were included (i.e. those diagnosed by a health professional as having depression), there is no evidence that exercise is of benefit (Krogh 2011). Another review of walking for depression suggested that walking might be a useful adjunct for depression treatment, and recommended further trials (Robertson 2012).
This review was published in 2001, in the British Medical Journal (Lawlor 2001). It was converted into a Cochrane review in 2009 (Mead 2009), and updated in 2012 (Rimer 2012). Since our last update, we had become aware of new trials that needed to be considered for inclusion, some of which had received considerable press coverage. Furthermore, several suggestions were made by the Cochrane Depression, Anxiety and Neurosis Review Group (CCDAN) editorial team about how to improve the review, e.g. inclusion of new subgroup analyses and summary of findings tables. The aim of this review is therefore to update the evidence in this area and to improve the methodology since the previous version (Rimer 2012). These changes are described below in Differences between protocol and review.
Objectives
To determine the effectiveness of exercise compared with no treatment (no intervention or control) for depression in adults.
To determine the effectiveness of exercise compared with other interventions (psychological therapies, alternative interventions such as light therapy, pharmacological treatment) for depression in adults.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) (including parallel, cluster, or individual, or the first phase of cross‐over trials).
We defined a trial as a 'randomised controlled trial' if the allocation of participants to intervention and comparison groups is described as randomised (including terms such as 'randomly', 'random' and 'randomisation').
Types of participants
Adult men and women aged 18 and over (with no upper age limit) in any setting, including inpatients.
Studies were included if the participants were defined by the author of the trial as having depression (by any method of diagnosis and with any severity of depression). We excluded trials that randomised people both with and without depression, even if results from the subgroups of participants with depression were reported separately, as we had done in previous versions of the review (Mead 2009; Rimer 2012).
The effects of exercise on depressive symptoms in participants with emotional distress (but not fulfilling a diagnosis of depression) or those who are healthy were not included in this review. We acknowledge that it can sometimes be difficult to distinguish between depression and dysthymia in the 'real world', as there needs to be only two weeks of decreased interest and enjoyment to define depression. However, we were primarily interested in the role of exercise in people with depression, for whom there is substantial morbidity, rather than people with mild, transient episodes of low mood.
Studies that investigated the effect of exercise on anxiety and neurotic disorders, dysthymia (i.e. low mood not fulfilling diagnostic criteria for depression) or postnatal depression were not included in the review.
Types of interventions
Exercise was defined as "planned, structured and repetitive bodily movement done to improve or maintain one or more components of physical fitness" (ACSM 2001). The reviews in 2001 (Lawlor 2001) and 2009 (Mead 2009) included any trial where the intervention was defined by the authors as exercise, irrespective of whether it fulfilled this standard definition. For subsequent updates, we agreed with the CCDAN Review Group editorial team that we would use the widely accepted and standardised definition instead (ACSM 2001). This meant that we excluded two trials (Chou 2004; Tsang 2006) that we had included in a previous review , and we also excluded studies that provided advice on how to increase physical activity, that did not fulfil the ACSM definition of exercise. We note however that studies are included irrespective of whether fitness gains were reported or not, and if they were reported, irrespective of whether fitness gains were achieved.
Experimental intervention
Any type of exercise (as defined above). We excluded studies that measured outcomes immediately before and after a single exercise session, and trials which provided less than a week of exercise.
Comparator intervention
A 'control' intervention. This included studies in which exercise was compared to no intervention; 'waiting list control', those in which it was compared to an intervention which the authors defined as a placebo; and those in which exercise was used as an adjunct to an established treatment which was received (in an identical way) by participants in both the exercising and non‐exercising group, e.g. exercise plus cognitive behavioural therapy (CBT) versus CBT alone.
Other type of active treatments, where the aim of the treatment was to improve mood. This includes pharmacological treatments, psychological therapies, or other alternative treatments.
Note that this strategy was the same as that included in the original review (Lawlor 2001).
We excluded studies comparing two different types of exercise with no non‐exercising comparison group.
We excluded trials described by the authors as 'combination treatments', where exercise was one component of the 'combination', because we could not disentangle the effect of exercise from the effect of the other components of the intervention.
Types of outcome measures
Primary outcomes
1. Our primary outcome was a measure of depression or mood at the outcome assessment, either as a continuous measure or as a dichotomous outcome.
Continuous measures of depression were reported using a variety of depression scales, the most common of which were the Beck Depression Inventory (Beck 1961) and the Hamilton Rating Scale for Depression (Hamilton 1960).
In previous versions of the review, where trials used a number of different tools to assess depression, we included the main outcome measure only in the meta‐analysis. The main outcome measure was defined using a hierarchy of criteria as follows: identified by the trial authors as the main outcome measure, outcome reported in the abstract, first outcome reported in the Results section.
Where trials used dichotomous data as primary outcomes, and also provided data on continuous outcome measures, we used the data provided in the trial reports for the continuous outcome measure in our meta‐analysis. This was because we knew from previous updates that trials generally reported only continuous outcomes.
Secondary outcomes
2. Acceptability of treatment, assessed by a) attendance at exercise interventions, and b) the number of participants completing the interventions; 3. Quality of life; 4. Cost; 5. Adverse events, e.g. musculoskeletal pain, fatigue.
In order to better understand the generalisability of exercise for depression, we also extracted data on the number of people screened for inclusion and the number recruited (Table 5).
1. Number screened; number still in trial and exercise intervention at end of trial.
| Trial ID | Screened | Randomised | Allocated exercise | Completed trial | Completed comparator group, e.g. control, other treatment (as a proportion of those allocated) | Completed exercise (as a proportion of those allocated) |
| Blumenthal 1999 | 604 underwent telephone screening | 156 | 55 | 133 | 41/48 (medication) | 44/55 (exercise plus medication) 39/53 (exercise alone) |
| Blumenthal 2007 | 457 | 202 | 51 (supervised), 53 home‐based | 183 | 42/49 (placebo) 45/49 (sertraline) |
45/51 (supervised), 51/53 home‐based |
| Blumenthal 2012b | 1680 enquired about the study | 101 | 37 | 95 | 23/24 completed 'placebo' and 36/40 completed the medication | 36/37 completed the exercise |
| Brenes 2007 | Not reported | 37 | 14 | Not reported | Not reported | Not reported |
| Bonnet 2005 | Not reported | 11 | 5 | 7 | 4/6 | 3/5 |
| Chu 2008 | 104 responded to adverts | 54 | 36 | 38 | 12/18 | 26/36 (both exercise arms combined) 15/18 in the high‐intensity arm |
| Dunn 2005 | 1664 assessed for eligibility | 80 | 17 | 45 | 9/13 | 11/17 (public health dose 3 times per week) |
| Doyne 1987 | 285 responded to adverts | 57 | Not reported | 40 completed treatment or control | 27 (denominator not known) | 13 (denominator not known) |
| Epstein 1986 | 250 telephone inquiries received | 33 | 7 | Not reported | Not reported | 7 |
| Fetsch 1979 | Not reported | 21 | 10 | 16 | 8/11 | 8/10 |
| Foley 2008 | 215 responded to adverts | 23 | 10 | 13 | 5/13 | 8/10 |
| Fremont 1987 | 72 initially expressed an interest | 61 | 21 | 49 | 31/40 | 18/21 |
| Gary 2010 | 982 referred, 242 had heart failure, 137 had a BDI > 10 and 74 eligible and consented | 74 | 20 | 68/74 completed post‐intervention assessments and 62 completed follow‐up assessments | usual care 15/17 | exercise only: 20/20 |
| Greist 1979 | Not reported | 28 | 10 | 22 | 15/18 | 8/10 |
| Hemat‐Far 2012 | 350 screened | 20 | 10 | 20 | not stated | not stated |
| Hess‐Homeier 1981 | Not reported | 17 | 5 | Not reported | Not reported | Not reported |
| Hoffman 2010 | 253 screened, 58 ineligible | 84 | 42 | 76 | 39/42 (2 were excluded by the trialists and 1 did not attend follow‐up) | 37/42 of exercise group provided data for analysis |
| Klein 1985 | 209 responded to an advertisement | 74 | 27 | 42 | 11/23 (meditation) 16/24 (group therapy) |
15/27 |
| Knubben 2007 | Not reported | 39 (note data on only 38 reported) | 20 | 35 | 16/18 | 19/20 |
| Krogh 2009 | 390 referred | 165 | 110 | 137 | 42/55 | 95/110 (both exercise arms combined) 47/55 (strength) 48/55 (aerobic) |
| Martinsen 1985 | Not reported | 43 | 24 | 37 | 17/19 | 20/24 |
| Mather 2002 | 1185 referred or screened | 86 | 43 | 86 | 42/43 | 43/43 |
| McCann 1984 | 250 completed BDI, 60 contacted | 47 | 16 | 43 | 14/15 completed placebo 14/16 completed 'no treatment' |
15/16 |
| McNeil 1991 | 82 | 30 | 10 | 30 | 10/10 (waiting list) 10/10 (social contact) |
10/10 |
| Mota‐Pereira 2011 | 150 | 33 | 22 | 29/33 | 10/11 | 19/22 |
| Mutrie 1988 | 36 | 24 | 9 | 24 | 7/7 | 9/9 |
| Nabkasorn 2005 | 266 volunteers screened | 59 | 28 | 49 | 28/31 | 21/28 |
| Orth 1979 | 17 | 11 | 3 | 7 | 2/2 | 3/3 |
| Pilu 2007 | Not reported | 30 | 10 | 30 | 20/20 | 10/10 |
| Pinchasov 2000 | Not reported | 18 | 9 | Not reported | Not reported | Not reported |
| Reuter 1984 | Not reported | Not reported | 9 | Not reported | Not reported | 9 |
| Schuch 2011 | 14/40 invited patients were not interested in participating | 26 | 15 | "no patient withdrew from intervention" | "no patient withdrew from intervention" | "no patient withdrew from intervention" |
| Setaro 1985 | 211 responses to advertisement | 180 | 30 | 150 | Not reported | 25/30 |
| Shahidi 2011 | 70 older depressed women chosen from 500 members of a district using the geriatric depression scale | 70 | 23 | 60/70 | 20/24 | 20/23 |
| Sims 2009 | 1550 invitations, 233 responded | 45 | 23 | 43 | 22/22 | 21/23 |
| Singh 1997 | Letters sent to 2953 people, 884 replied | 32 | 17 | 32 | 15/15 | 17/17 |
| Singh 2005 | 451 | 60 | 20 | 54 | 19/20 (GP standard care) | 18/20 (high‐intensity training) |
| Veale 1992 | Not reported | 83 | 48 | 57 | 29/35 | 36/48 |
| Williams 2008 | 96 in parent study | 43 | 33 | 34 | 8/10 | 26/33 (both exercise groups combined) 15/16 exercise 11/17 walking |
BDI: Beck Depression Inventory
Timing of outcome assessment
We extracted data at the end of treatment, and also at the end of any longer‐term follow‐up after the intervention had been stopped.
Search methods for identification of studies
Electronic searches
We carried out the following electronic searches (Appendix 1; Appendix 2)
The Cochrane Depression, Anxiety and Neurosis Review Group's Specialised Register (CCDANCTR) (all years to 1 March 2013);
The Cochrane Central Register of Controlled Trials (CENTRAL) (all years to 2010):
MEDLINE (1950 to February 2010);
EMBASE (1980 to February 2010);
PsycINFO (all years to February 2010);
Sports Discus (1975 to 2007).
We searched Current Controlled Trials (May 2008, November 2010 and March 2013) to identify any ongoing trials. We performed an electronic search of ClinicalTrials.gov and WHO International Clinical Trials Registry Platform (ICTRP) in March 2013.
Because the searches for the CDCANCTR register are up‐to‐date and comprehensive, we were advised by the CCDAN editorial team that it was not necessary to search the other databases.
For a previous version of this review (Mead 2009) we conducted a cited reference search in the Web of Science using the references to all included studies, excluded studies and studies awaiting assessment. This cited reference search was not repeated for subsequent updates.
In order to ensure that the review was as up‐to‐date as possible when it was submitted for editorial review, we searched the CCDANCTR (up to 1st March 2013) again on 2nd May 2013, , so that we could list potentially eligible studies as ‘Studies awaiting classification’.
Searching other resources
For the initial review (Lawlor 2001), the following journals were searched: BMJ, JAMA, Archives of Internal Medicine, New England Journal of Medicine, Journal of the Royal Society of Medicine, Comprehensive Psychiatry, British Journal of Psychiatry, Acta Psychiatrica Scandinavica and British Journal of Sports Medicine.
For the update in 2009 (Mead 2009), we contacted experts, including authors of all included studies and those with at least two publications amongst the excluded studies, to identify any additional unpublished or ongoing studies, authors of significant papers and other experts in the field to ensure identification of all randomised controlled trials (published, unpublished or ongoing).
Due to limitations in available resources for this current update, we did not repeat these handsearches. We limited our contact with authors to those whose trials had been 'ongoing' in the previous version, to enquire whether they had subsequently been published. We also contacted authors to obtain any missing information about trial details. We had planned to do this should any data be missing e.g. standard deviations, although this was not necessary.
We screened the bibliographies of all included articles for additional references.
Data collection and analysis
Selection of studies
Two review authors (GC and GM) independently screened the citations from the searches, and decided which full texts should be retrieved. They then independently applied inclusion and exclusion criteria, resolving any differences in opinion through discussion. If they could not reach agreement, a third author was available (CG) to decide whether a study should be included or excluded.
For the searches of the CCDANCTR up to 1st March 2013, the Trials Search Co‐ordinator checked abstracts, excluded obviously irrelevant ones, and then sent a list of the remaining citations to GM for scrutiny, to be included as 'studies awaiting classification'.
We created a PRISMA flow diagram to detail the study selection process.
Data extraction and management
We extracted data, when available, at the end of treatment and at the end of follow‐up.
For this update, two review authors (GC, FW) independently extracted data for our primary and secondary outcomes for each new trial identified. A third review author (GM) extracted data on type of exercise from all the included trials, to enable a fourth author (CG) to categorise intensity of exercise according to ACSM criteria.
Data extracted were participants, interventions, outcome measures, results, the number of people screened, the number randomised, the number allocated to exercise, the number who dropped out of the exercise arm (Table 5), secondary clinical outcomes, cost and adverse events, and main conclusions. All the review authors used the same structured paper extraction form that had been piloted on two studies. We resolved any discrepancies by referring to the original papers and by discussion.
Main comparisons
We undertook the following analyses.
Exercise versus 'control' (as defined above).
Exercise versus psychological therapies.
Exercise versus alternative treatments.
Exercise versus pharmacological treatments.
Assessment of risk of bias in included studies
The Cochrane Collaboration 'Risk of bias' tool was used to assess risks of bias, according to Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Handbook 2011). Two review authors independently extracted data on random sequence generation, allocation concealment, blinding of participants, blinding of those delivering the intervention, blinding of outcome assessors, incomplete outcome data, selective reporting and other potential biases. Each of these domains was categorised as being at high risk of bias, unclear risk of bias or low risk of bias. We resolved any disagreements through discussion.
For concealment of allocation we distinguished between trials that were adequately concealed (central randomisation at a site remote from the study; computerised allocation in which records are in a locked, unreadable file that can be assessed only after entering participant details; the drawing of non‐opaque envelopes), inadequately concealed (open lists or tables of random numbers; open computer systems; drawing of non‐opaque envelopes) and unclear (no information in report, and the authors either did not respond to requests for information or were unable to provide information).
Trials could only be defined as 'intention‐to‐treat' if participants were analysed according to the allocated treatment AND if all participants either completed allocated treatments or if missing outcome data were replaced using a recognised statistical method, e.g. last observation carried forward (LOCF).
For blinding we distinguished between trials in which the main outcome was measured by an assessor who was blind to treatment allocation (blind) and those in which the main outcome was measured either by the participants themselves (i.e. self report) or by a non‐blinded assessor (not blind).
Measures of treatment effect
We undertook a narrative review of all studies and a meta‐analysis of those studies with appropriate data. Where trials used a number of different tools to assess depression we included the main outcome measure only in the meta‐analysis. The main outcome measure was defined using a hierarchy of criteria as follows: identified by the authors as the main outcome measure; outcome reported in the abstract; first outcome reported in the Results section.
For continuous data where different scales were used, the standardised mean difference (SMD) was calculated and reported with a 95% confidence interval (CI). For dichotomous data the risk ratio was calculated and reported with a 95% CI.
We interpreted the SMDs using the following 'rule of thumb': 0.2 represents a small effect, 0.5 a moderate effect and 0.8 a large effect (Schünemann 2008).
We pooled long‐term follow‐up data from those trials that reassessed participants long after the interventions had been completed. 'Long after' could mean an assessment at any period of time after the intervention had been completed.
Unit of analysis issues
Studies with multiple treatment groups
Where trials included a control arm, an exercise arm and an 'established treatment' arm (e.g. CBT, antidepressants), we extracted data on control versus exercise, and exercise versus established treatment. This meant that data from the exercise arm were included in two separate comparisons, in separate univariate analyses.
Where trials compared an established treatment (e.g. CBT, antidepressants) versus exercise versus both the established treatment and exercise, we made two comparisons: (i) established treatment plus exercise versus established treatment alone, and included this in the meta‐analysis of treatment versus control; (ii) exercise versus established treatment (e.g. CBT, antidepressants). This means that data from the 'established treatment alone' arm were used in two separate comparisons.
In the review versions in 2001 (Lawlor 2001), 2009 (Mead 2009) and 2012 (Rimer 2012) , for trials which included more than one intensity of exercise, we used the exercise arm with the greatest clinical effect in the review. Similarly, when trials provided more than one type of exercise, we used the type of exercise with the greatest clinical effect. However, because this may overestimate the effect of exercise, we now use the exercise arm which provides the biggest 'dose' of exercise, and performed a sensitivity analysis to explore the effect of using the smallest 'dose'.
Cross‐over trials
For cross‐over trials, we intended to use the first phase of the trial only due to the potential 'carry‐over' effect of exercise. To date, we have not included any cross‐over trials.
Cluster‐randomised trials
If cluster‐randomised trials were identified and incorrectly analysed using individuals as the unit of analysis, we intended to make corrections using the intracluster correlation coefficient (ICC). If this had not been available, we would have imputed the ICC from similar studies. In fact, we did not find any cluster‐RCTs to include.
Dealing with missing data
For two previous versions of this review (Lawlor 2001; Mead 2009) we found current contact details of all authors through correspondence addresses in study reports and by searching websites. We contacted all authors by email or post (sending three reminders to non‐responders) to establish missing details in the methods and results sections of the written reports and to determine authors' knowledge of, or involvement in, any current work in the area. For the previous update (Rimer 2012) and this current update, we contacted authors only if there were missing data items, or if we needed more detail to decide on whether or not to include the study.
Some trials, in which participants dropped out, reported data from only the remaining participants, so we used these data in our meta‐analyses. For trials which attempted to impute data from missing participants (e.g. LOCF for continuous data) we used the imputed values and categorised the trial as 'intention‐to‐treat.' When we could not obtain information either from the publication or from the authors, we classified the trial as 'not intention‐to‐treat', and used the data from the available cases in the meta‐analysis.
Assessment of heterogeneity
We used the Chi² test, together with the I² statistic, to assess heterogeneity.
A P value of 0.1 or less indicates significant heterogeneity when considering Chi². The ranges for I² are:
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity.
Note that the importance of the observed value of I² depends on (i) the magnitude and direction of effects and (ii) the strength of evidence for heterogeneity (e.g. P value from the Chi² test, or a confidence interval for I²) (Handbook 2011).
Assessment of reporting biases
We used a funnel plot to explore reporting biases when 10 or more studies were included in the meta‐analysis. However, other reasons such as heterogeneity and small study effects also cause asymmetrical funnel plots.
Data synthesis
We used a random‐effects model based on DerSimonian and Laird's method to calculate the pooled effect size (DerSimonian 1986). We synthesised data from trials where outcome data were collected as soon as the intervention ended, and performed a separate synthesis of data collected weeks or months after the intervention ended, to explore whether any benefits were retained after the intervention had been completed. When performing meta‐analyses of complex interventions, decisions need to be made about whether the interventions are sufficiently similar to be combined into a meta‐analysis. We included trials that fulfilled the ACSM definition of exercise (ACSM 2001), and combined these data in a meta‐analysis.
We created 'Summary of findings' tables for outcomes and graded them accordingly using the GRADE approach (gradepro.org/aboutus.html).
Subgroup analysis and investigation of heterogeneity
We explored the effect of different types of exercise (aerobic, resistance exercise or mixed aerobic and resistance) for those trials comparing exercise versus control on outcome, by performing subgroup analyses for the different types of exercise.
This update has for the first time explored the impact of intensity of exercise on outcome, dividing intensity into hard/vigorous or moderate, using ACSM criteria(ACSM 1998).The combination (where possible) of authors' description, compendium of physical activities classification and the ACSM intensity/metabolic equations (MET) cut‐offs (in particular the most recent ones which take age into account) were used to categorise intensity (https://sites.google.com/site/compendiumofphysicalactivities/Activity).
This update has for the first time explored the effect of the number of exercise sessions, by extracting data on the length of the exercise programme and the frequency of exercise sessions. We categorised studies by the total number of sessions and then grouped the total number as 0 ‐ 12, 13 ‐ 24, 25 ‐ 36, at least 37.
This update has for the first time explored how the diagnosis of depression at baseline (using a cut‐point on a scale, or by psychiatric interview) influenced the effect of exercise on mood at the end of treatment.
Sensitivity analysis
We undertook sensitivity analyses to explore how much of the variation between studies comparing exercise to no exercise is explained by between‐study differences in:
publication type (peer‐reviewed journal, conference abstract/proceedings, doctoral dissertation).
allocation concealment.
intention‐to‐treat analysis (as defined above).
blinding.
We included only trials at low risk of bias for each of these outcomes in the sensitivity analysis. We then performed a sensitivity analysis, as we had done previously, including trials that were at low risk of bias for three key quality criteria: Allocation concealment, AND intention‐to‐treat AND blinding.
We also performed a sensitivity analysis using those trials that had several arms, for which we had included the arm with the biggest 'dose' of exercise in the initial analysis. Here we include the arm with the smallest 'dose'.
Results
Description of studies
Results of the search
The results of searches for the previous updates have already been described in detail (Lawlor 2001; Mead 2009; Rimer 2012).
The 2012 review update (Rimer 2012) included studies identified from searches performed in 2010 and 2011. In 2010 (Rimer 2012), we had identified three ongoing trials (Blumenthal 2012a; McClure 2008; Underwood 2013). Of these, one has been included (Blumenthal 2012a) in this update. One of these was excluded because the intervention was not exercise alone (McClure 2008). The other was excluded because participants did not have to have depression to enter the trial (Underwood 2013); although the trialists reported results from the subgroup with depression at entry, we had previously excluded trials reporting our main outcomes as subgroup analyses. In June 2011, our search of the Cochrane Depression, Anxiety and Neurosis Group Clinical Trials Register (CCDANCTR) identified 45 citations; of which we retrieved full texts for 10 studies. Of these 10 full‐text studies, we excluded five (Lolak 2008; Mailey 2010; Oeland 2010; Sneider 2008; Thomson 2010) and five studies (Annesi 2010; Ciocon 2003; Gary 2010; Shahidi 2011; Chalder 2012) were listed as 'awaiting classification' (Rimer 2012); in this current update, two of these have been included (Gary 2010; Shahidi 2011), one has been excluded because further scrutiny led us to conclude that the intervention did not fulfil the definition of 'exercise' (Ciocon 2003), one was excluded because it was a trial of advice to increase physical activity that did not fulfil the ACSM definition of exercise (Chalder 2012) and one was excluded because it was a subgroup analysis from a trial of people with obesity (Annesi 2010).
In September 2012, the searches of the CCDANCTR identified a further 290 citations. Of these, we retrieved full texts for 43 studies: 39 were excluded (Akandere 2011; Arcos‐Carmona 2011; Attia 2012; Aylin 2009; Bowden 2012; Chalder 2012; Chan 2011; Chow 2012; Christensen 2012; Clegg 2011; Demiralp 2011; Deslandes 2010; Gutierrez 2012; Hedayati 2012; Immink 2011; Jacobsen 2012; Johansson 2011; Lavretsky 2011; Leibold 2010; Levendoglu 2004; Levinger 2011; Littbrand 2011; Matthews 2011; Midtgaard 2011; Mudge 2008; O'Neil 2011; Ouzouni 2009; Penttinen 2011; Perna 2010; Piette 2011; Robledo Colonia 2012; Roshan 2011; Ruunsunen 2012; Schwarz 2012; Silveira 2010; Songoygard 2012; Trivedi 2011; Whitham 2011; Wipfli 2011); three were included (Hemat‐Far 2012; Mota‐Pereira 2011; Schuch 2011) and one trial is not yet complete (EFFORT D).
In March 2013, a search of the WHO Clinical Trials Registry Platform identified 188 citations. We sought full texts for 29; of these 29 studies, 23 are listed as ongoing trials (ACTRN12605000475640; ACTRN12612000094875; ACTRN12612000094875; CTR/2012/09/002985; EFFORT D; IRCT201205159763; IRCT2012061910003N1; ISRCTN05673017; NCT00103415; NCT00643695; NCT00931814; NCT01024790; NCT01383811; NCT01401569; NCT01464463; NCT01573130; NCT01573728; NCT01619930; NCT01696201; NCT01763983; NCT01787201; NCT01805479; UMIN000001488). One trial has been completed and is included (Hoffman 2010). Four trials were excluded (Bromby 2010; Lever‐van Milligen 2012; NCT00964054; NCT00416221) and one awaits assessment (DEMO II 2012)
Through correspondence with the authors of one study (Blumenthal 2012a), another study by the same group was identified (Blumenthal 2012b); however this reported data from a subgroup with depression and was excluded (as we did for previous trials reporting subgroups).
The search of CCDANCTR up to 1st March 2013 identified 151 records (titles and abstracts). The Trials Search Co‐ordinator excluded 89 obviously irrelevant citations. Of the remaining 62 studies, seven were already listed as included or excluded or awaiting assessment, one review author (GM) excluded 46 were excluded as they were obviously irrelevant, and the full text of nine articles were retrieved; one of these was a subsidiary publication for an included study (Hoffman 2010), one had already been excluded (Silveira 2010) and the other seven are listed as ‘awaiting classification' (Aghakhani 2011; DEMO II 2012; Gotta 2012; Murphy 2012; Pinniger 2012; Sturm 2012; Martiny 2012).
For this current update, we are therefore including seven new studies (Hemat‐Far 2012;Hoffman 2010; Gary 2010; Mota‐Pereira 2011; Shahidi 2011; Schuch 2011; Blumenthal 2012a), making a total of 39 included studies (Characteristics of included studies table). For this update, we have excluded a further 54 studies (Characteristics of excluded studies table), giving a total of 175 excluded, listed 23 as ongoing studies (Characteristics of ongoing studies table), and listed seven as awaiting classification (Characteristics of studies awaiting classification table).
See the PRISMA flow diagram for details of the study selection process for this current update (Figure 1).
1.
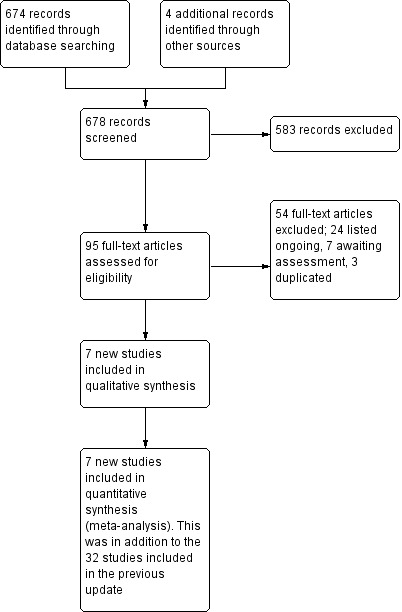
Study flow diagram, showing the results of the searches for this current update.
Included studies
In our previous update, we identified 32 completed trials.
For this update, we include seven additional trials, recruiting a total of 408 additional participants at randomisation. Of these, 374 participants remained in the trials by the time of outcome analysis (Blumenthal 2012a; Gary 2010; Hemat‐Far 2012; Hoffman 2010; Mota‐Pereira 2011; Shahidi 2011; Schuch 2011) (see Characteristics of included studies table).
Of the 39 included trials (recruiting 2326 people), 22 were from the USA (Blumenthal 1999; Blumenthal 2007; Blumenthal 2012a; Bonnet 2005; Brenes 2007; Chu 2008; Dunn 2005; Doyne 1987; Epstein 1986; Fetsch 1979; Fremont 1987; Gary 2010; Greist 1979; Hess‐Homeier 1981; Hoffman 2010; Klein 1985; McCann 1984; Orth 1979; Reuter 1984; Setaro 1985; Singh 1997; Williams 2008); one was from Canada (McNeil 1991), three from the UK (Mather 2002; Mutrie 1988; Veale 1992), two from Australia (Sims 2009; Singh 2005), two from Iran (Hemat‐Far 2012; Shahidi 2011), one from New Zealand (Foley 2008), one from Norway (Martinsen 1985), one from Denmark (Krogh 2009), one from Germany (Knubben 2007), one from Italy (Pilu 2007), one from Russia (Pinchasov 2000), one from Brazil (Schuch 2011), one from Portugal (Mota‐Pereira 2011) and one from Thailand (Nabkasorn 2005).
Of these 39 trials, 30 were peer‐reviewed papers (Blumenthal 1999; Blumenthal 2007; Blumenthal 2012a; Brenes 2007; Dunn 2005; Doyne 1987; Foley 2008; Fremont 1987; Gary 2010; Greist 1979; Hemat‐Far 2012; Hoffman 2010; Klein 1985; Krogh 2009; Knubben 2007; Martinsen 1985; Mather 2002; McCann 1984; McNeil 1991; Mota‐Pereira 2011; Nabkasorn 2005; Pilu 2007; Pinchasov 2000; Schuch 2011; Shahidi 2011; Sims 2009; Singh 1997; Singh 2005; Veale 1992; Williams 2008). Seven were doctoral dissertations (Bonnet 2005; Chu 2008; Epstein 1986; Fetsch 1979; Hess‐Homeier 1981; Orth 1979; Setaro 1985) and two were published in abstract form only (Mutrie 1988; Reuter 1984).
Of these 39 trials, data from two studies were unsuitable for statistical pooling because they were provided in graphical form only (McCann 1984) or provided no numerical data at all (Greist 1979). One trial (Nabkasorn 2005) provided data in graphical form only which we were able to include after manually converting the graph into mean and standard deviation (SD) values by drawing a horizontal line from the mean and SD on the graph to the vertical axis. Hence, we used data from 37 trials in the meta‐analyses.
Five trials (Blumenthal 1999; Blumenthal 2007; Blumenthal 2012a; Krogh 2009; Mather 2002) provided data on whether participants fulfilled diagnostic criteria for depression at the end of the study, as well as depression scales. We used the scale results described in the paper rather than using formulae to convert the dichotomous outcomes to continuous outcomes, to allow inclusion of these trials in the meta‐analysis.
Five authors provided further data on their studies (Blumenthal 2012a; Gary 2010; Hoffman 2010; Mota‐Pereira 2011; Sims 2009).
Design
All included studies were randomised controlled trials (RCTs); further details are provided in the Characteristics of included studies table. There were no cluster‐RCTs that fulfilled our inclusion criteria.
Seventeen studies had two arms (Bonnet 2005; Fetsch 1979; Foley 2008; Knubben 2007; Hemat‐Far 2012; Hoffman 2010; Martinsen 1985; Mather 2002; Mota‐Pereira 2011; Nabkasorn 2005; Pilu 2007; Pinchasov 2000; Reuter 1984; Schuch 2011; Sims 2009; Singh 1997; Veale 1992), 17 had three arms (Blumenthal 1999; Blumenthal 2012a; Brenes 2007; Chu 2008,; Doyne 1987; Epstein 1986; Fremont 1987; Greist 1979; Hess‐Homeier 1981; Klein 1985; Krogh 2009; McCann 1984; McNeil 1991; Mutrie 1988; Shahidi 2011; Singh 2005; Williams 2008), three had four arms (Blumenthal 2007; Gary 2010; Orth 1979), one had five arms (four intensities of exercise and control; (Dunn 2005) and one had six arms (cognitive behavioural therapy (CBT) plus aerobic exercise, aerobic exercise only, CBT only, CBT plus non‐aerobic exercise, non‐aerobic exercise only or no intervention; Setaro 1985).
Of the 17 trials with two arms, exercise was compared with waiting list or usual care in eight trials (Hemat‐Far 2012; Hoffman 2010; Mota‐Pereira 2011; Nabkasorn 2005; Pilu 2007; Schuch 2011; Sims 2009; Veale 1992), exercise was compared with a placebo intervention (e.g. social activity) in four trials (Knubben 2007; Martinsen 1985; Mather 2002; Singh 1997), exercise was compared with CBT in one trial (Fetsch 1979), two trials compared CBT plus exercise versus CBT alone (Bonnet 2005; Reuter 1984), one trial compared exercise with stretching (Foley 2008) and one trial compared exercise with bright light therapy (Pinchasov 2000).
Of the 17 trials with three arms, one trial compared exercise versus exercise plus sertraline versus sertraline (Blumenthal 1999), one compared exercise versus sertraline versus usual care (Brenes 2007), one compared exercise versus antidepressant (sertraline) versus placebo (Blumenthal 2012a), one compared exercise versus walking versus social conversation (Williams 2008) and three compared exercise versus waiting list versus a placebo intervention (e.g. social activity) (McCann 1984; McNeil 1991; Mutrie 1988). Two compared exercise versus usual care versus CBT (Epstein 1986; Hess‐Homeier 1981), one compared exercise versus CBT versus both exercise and CBT (Fremont 1987), one compared exercise versus low‐intensity CBT versus high‐intensity CBT (Greist 1979), and one compared exercise versus a placebo versus CBT (Klein 1985). One trial compared high‐intensity versus low‐intensity aerobic exercise versus stretching (Chu 2008), one compared strength versus aerobic versus relaxation training (Krogh 2009), one compared high‐intensity resistance training versus low‐intensity resistance training versus usual care (Singh 2005), one compared exercise versus yoga versus control (Shahidi 2011) and one compared running versus weight‐lifting versus waiting list (Doyne 1987).
Of the three trials with four arms, one compared exercise to three types of control (Orth 1979), one compared home‐based exercise versus supervised exercise versus sertraline versus placebo (Blumenthal 2007), and one compared exercise versus combined exercise and CBT versus CBT alone versus usual care (Gary 2010).
Participants
Twenty‐three trials recruited participants from non‐clinical populations (Blumenthal 1999; Blumenthal 2007; Bonnet 2005; Brenes 2007; Dunn 2005; Doyne 1987; Epstein 1986; Fetsch 1979; Fremont 1987; Greist 1979; Hemat‐Far 2012; Hess‐Homeier 1981; Klein 1985; McCann 1984; McNeil 1991; Nabkasorn 2005; Orth 1979; Pinchasov 2000; Setaro 1985; Shahidi 2011; Singh 1997; Singh 2005; Williams 2008) with most involving recruitment of participants through the media.
Nine trials recruited participants from clinical populations, i.e. hospital inpatients or outpatients (Gary 2010; Knubben 2007; Martinsen 1985; Mota‐Pereira 2011; ; Mutrie 1988; Pilu 2007; Reuter 1984; Schuch 2011; Veale 1992).
Seven trials recruited participants from both clinical and non‐clinical populations (Blumenthal 2012a; Chu 2008; Foley 2008; Hoffman 2010; Krogh 2009; Mather 2002; Sims 2009).
Of the 23 trials recruiting people from non‐clinical populations, diagnosis of depression was by a clinical interview in ten studies (Blumenthal 1999; Blumenthal 2007; Bonnet 2005; Doyne 1987; Dunn 2005; Hemat‐Far 2012; Klein 1985; Pinchasov 2000; Singh 1997; Singh 2005). The other 13 studies used a cut‐off point on one of several depression scales: Beck Depression Inventory: (Epstein 1986; Fremont 1987; Fetsch 1979; Hess‐Homeier 1981; McCann 1984; McNeil 1991); Centre for Epidemiologic Studies Depression Scale (Nabkasorn 2005); Cornell Scale for Depression in Dementia (Williams 2008); Depression Adjective Checklist (Orth 1979); Minnesota Multiple Personality Inventory (Setaro 1985); Patient Health Questionnaire‐9 (Brenes 2007); Geriatric Depression Scale (Shahidi 2011); or Symptom Checklist Score (Greist 1979).
There were more women than men (see Characteristics of included studies table) and mean age ranged from 22 years (Orth 1979) to 87.9 years (Williams 2008).
Interventions
Thirty‐three trials provided aerobic exercise, of which 16 trials provided running (Blumenthal 1999; Blumenthal 2012a; Doyne 1987; Epstein 1986; Fetsch 1979; Fremont 1987; Greist 1979; Hess‐Homeier 1981; Hemat‐Far 2012; Klein 1985; McCann 1984; Nabkasorn 2005; Orth 1979; Reuter 1984; Shahidi 2011; Veale 1992), three provided treadmill walking (Blumenthal 2007; Bonnet 2005; Dunn 2005), four provided walking (Gary 2010; Knubben 2007; McNeil 1991; Mota‐Pereira 2011), one provided aerobic training with an instructor (Martinsen 1985), one provided aerobic dance (Setaro 1985) and one provided cycling on a stationary bicycle (Pinchasov 2000).
Three studies provided aerobic exercises according to preference (Chu 2008; Hoffman 2010; Schuch 2011) and another provided mixed aerobic and resistance training (Brenes 2007). One study did not specify the type of aerobic exercise provided (Foley 2008).
Two trials compared two different exercise interventions versus control: Krogh 2009 compared resistance training with combination aerobic exercises (including cycling, running, stepping and rowing) and Williams 2008 compared combination walking and strength training and walking alone.
Two trials provided mixed exercise, i.e. endurance, muscle strengthening and stretching (Mather 2002; Mutrie 1988), and four provided resistance training (Pilu 2007; Sims 2009; Singh 1997; Singh 2005).
Seventeen trials (Blumenthal 2007; Blumenthal 2012a; Bonnet 2005; Brenes 2007; Doyne 1987; Dunn 2005; Fremont 1987; Hoffman 2010; Knubben 2007; Mather 2002; McCann 1984; Mutrie 1988; Schuch 2011; Setaro 1985; Sims 2009; Singh 1997; Singh 2005) provided indoor exercise, two trials provided outdoor exercise ( Gary 2010; McNeil 1991) and the remaining trials did not report whether the exercise was indoors or outdoors.
Only one trial stated that unsupervised exercise was provided (Orth 1979). Two trials included both supervised and home‐based exercise arms (Blumenthal 2007; Chu 2008). The other trials provided supervised exercise or did not report this information.
Twelve trials provided individual exercises (Blumenthal 2007; Chu 2008; Doyne 1987; Dunn 2005; Greist 1979; Klein 1985; McNeil 1991; Mota‐Pereira 2011; Mutrie 1988; Orth 1979; Schuch 2011; Williams 2008), 16 provided group exercises (Blumenthal 1999; Blumenthal 2012a; Brenes 2007; Fetsch 1979; Fremont 1987; Krogh 2009; Mather 2002; McCann 1984; Nabkasorn 2005; Pilu 2007; Setaro 1985; Shahidi 2011; Sims 2009; Singh 1997; Singh 2005; Veale 1992) and the remaining trials did not report this information.
The duration of the intervention ranged from 10 days (Knubben 2007) to 16 weeks (Blumenthal 1999; Blumenthal 2007). Two trials did not state duration: one performed assessments at the end of the intervention at eight months (Pilu 2007) and the other at time of discharge from hospital (Schuch 2011).
The 'control' groups of 'no treatment' or 'placebo' comprised heterogeneous interventions including social conversation, telephone conversations to discuss their general health and relaxation (avoiding muscular contraction). For exercise versus control, there were different types of comparator arm (see Analysis 5.5). Two compared with a placebo; 17 with no treatment, waiting list, usual care or self management; six compared exercise plus treatment vs treatment; six compared exercise with stretching, meditation or relaxation; and four with 'occupational intervention', health education or casual conversation.
5.5. Analysis.
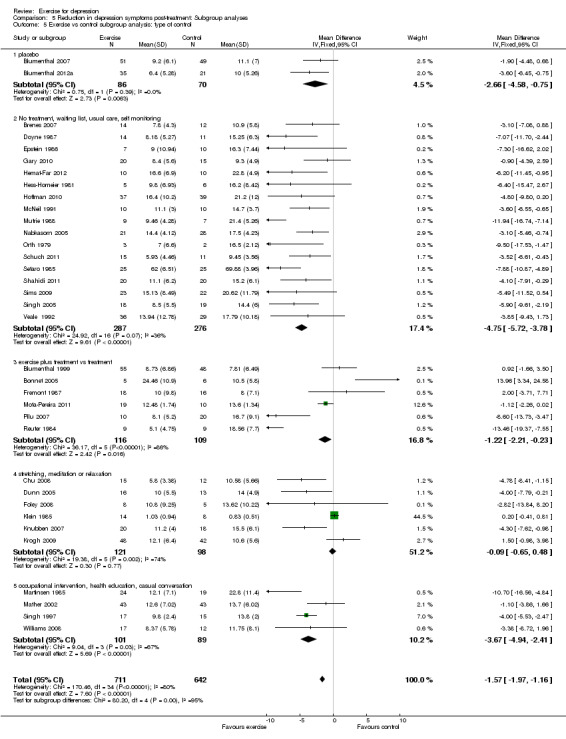
Comparison 5 Reduction in depression symptoms post‐treatment: Subgroup analyses, Outcome 5 Exercise vs control subgroup analysis: type of control.
Outcomes
Depression measurement
Of the 39 trials, 12 reported Beck Depression Inventory (BDI) scores, and 13 reported Hamilton Rating Scale for Depression (HAMD) scores. A variety of other scales were also used.
Other clinical endpoints and adverse effects
Several recorded clinical endpoints as well as mood: Blumenthal 2012a, Brenes 2007 and Gary 2010 (physical functioning); Chu 2008 (self efficacy), Foley 2008 (self efficacy, episodic memory and cortisol awakening response), Knubben 2007 (length of hospital stay), Krogh 2009 (absence from work and effect on cognitive ability), Mather 2002 (participant and clinical global impression), Pilu 2007 and Mota‐Pereira 2011 (clinical global impression and global assessment of functioning), Sims 2009 (quality of life, stroke impact scale, psychosocial health status and adverse events), Singh 1997 (sickness impact profile), Gary 2010, Hoffman 2010, Schuch 2011, Singh 2005, Pilu 2007 and Brenes 2007 (quality of life), Shahidi 2011 (Life satisfaction scale) and Blumenthal 2012a (cardiovascular biomarkers).
Seven trials systematically recorded and reported adverse events (Blumenthal 2007; Blumenthal 2012a; Dunn 2005; Knubben 2007; Singh 1997; Singh 2005; Sims 2009). No trial provided data on costs.
Timing of outcome measures
All our included trials reported mood as a continuous outcome at the end of treatment. Long‐term follow‐up data beyond the end of the interventions are described for eight trials (ranging from 4 months to 26 months). Fremont 1987 (follow‐up at four months), Sims 2009 (follow‐up at six months), Klein 1985 (follow‐up for nine months), Blumenthal 1999 (follow‐up at 10 months Babyak 2000), Krogh 2009 (follow‐up at 12 months), Singh 1997 (follow‐up at 26 months, reported in Singh 2001), Mather 2002 (follow‐up at 34 weeks) and Gary 2010 (follow‐up at six months). Hoffman 2010 reported long‐term follow‐up but we were unable to include this in the meta‐analysis due to the way it was reported. The author has been contacted for data.
Excluded studies
In this update, a further 54 studies were excluded following review of full text.
In this update, we decided not to list reviews as excluded studies. Additionally some references that were previously classified as excluded studies have been re‐classified as additional reports of included studies. As a result there are now a total of 174 excluded studies.
One hundred and twenty‐nine publications described randomised trials of exercise; the reasons for excluding these are listed in more detail below:
In 93 trials, participants did not have to have depression (as defined by the authors of the trial) to be eligible for the trial (Abascal 2008; Akandere 2011; Arcos‐Carmona 2011; Asbury 2009; Aylin 2009; Badger 2007; Baker 2006; Berke 2007; Blumenthal 2012b; Bosch 2009; Brittle 2009; Burton 2009; Carney 1987; Chen 2009; Christensen 2012; Clegg 2011; Courneya 2007; Demiralp 2011; Dalton 1980; Eby 1985; Elavsky 2007; Ersek 2008; Fox 2007; Gary 2007; Ghroubi 2009; Gottlieb 2009; Gusi 2008; Gutierrez 2012; Haffmans 2006; Hannaford 1988; Haugen 2007; Hembree 2000; Herrera 1994; Hughes 1986; Jacobsen 2012; Johansson 2011; Karlsson 2007; Kerr 2008; Kerse 2010; Kim 2004; Knapen 2006; Kulcu 2007; Kupecz 2001; Lai 2006; Latimer 2004; Lautenschlager 2008; Leppämäki 2002; Levendoglu 2004; Lever‐van Milligen 2012; Levinger 2011; Lin 2007; Littbrand 2011; Lolak 2008; Machado 2007; Mailey 2010; Martin 2009; Matthews 2011; Midtgaard 2011; Morey 2003; Motl 2004; Mudge 2008; Mutrie 2007; Neidig 1998; Neuberger 2007; Nguyen 2001; Oeland 2010; Ouzouni 2009; Pakkala 2008; Penttinen 2011; Perna 2010; Rhodes 1980; Robledo Colonia 2012; Ruunsunen 2012; Salminen 2005; Sarsan 2006; Sims 2006; Smith 2008; Songoygard 2012; Stein 1992; Stern 1983; Strömbeck 2007; Sung 2009; Tapps 2009; Thomson 2010; Tomas‐Carus 2008; Tsang 2003; Tenorio 1986; Underwood 2013; Weinstein 2007; White 2007; Wilbur 2009; Wipfli 2008; Wipfli 2011).
Ten trials compared two types of exercise with no non‐exercising control (Bosscher 1993; NCT00546221; NCT01152086; Legrand 2009; Passmore 2006; Sexton 1989; TREAD 2003; Trivedi 2011; Wieman 1980; Williams 1992).
Three trials reported subgroup analyses of depressed patients, one from a randomised trial of exercise for osteoarthritis (Penninx 2002), one from a cohort of participants enrolled in cardiac rehabilitation following major cardiac events (Milani 2007) and one from a cluster‐RCT of exercise in nursing homes (Underwood 2013).
Three trials included only a single bout of exercise (Bartholomew 2005; Bodin 2004; Gustafsson 2009) and one trial provided exercise for only four days (Berlin 2003).
Two trials that recruited women with postnatal depression were excluded (Armstrong 2003; Armstrong 2004).
Five trials provided exercise interventions that did not fulfil the ACSM definition of exercise (Tai‐Chi (Chou 2004); Qigong (Tsang 2006; Chow 2012); and yoga (Oretzky 2006; Immink 2011) to waiting list controls.
Seven trials involving adolescents (Beffert 1993; Brown 1992; NCT00964054; Hughes 2009; MacMahon 1988; Rofey 2008; Roshan 2011) were excluded.
Two trials were excluded as they provided exercise counselling, not exercise (Vickers 2009; Chalder 2012).
Three trials were excluded as the intervention was multifaceted (McClure 2008; O'Neil 2011; Sneider 2008).
Ongoing studies
There are 23 ongoing studies (IRCT201205159763; NCT01805479; CTR/2012/09/002985; NCT01787201; NCT01619930; NCT01573130; NCT01573728; EFFORT D; NCT01464463; ACTRN12605000475640; UMIN000001488; NCT01763983; ACTRN12612000094875; NCT00103415; ACTRN12609000150246; NCT01696201; ISRCTN05673017; NCT01401569; IRCT2012061910003N1; NCT01024790; NCT01383811; NCT00643695; NCT00931814). One trial (EFFORT D) was identified from the September 2012 search of the CCDANCTR and the remaining 23 were identified from the March 2013 search of the WHO Clinical Trials Registry Platform.
Studies awaiting classification
This is a fast‐moving field and our searches of CCDANCTR in March 2013 identified seven studies that are awaiting further assessment (Aghakhani 2011; DEMO II 2012; Martiny 2012; Murphy 2012; Pinniger 2012; Sturm 2012; Gotta 2012). Initial screening of these studies indicated three of these studies (Martiny 2012; Pinniger 2012; Sturm 2012) could be eligible for inclusion in this review. We plan to update the review, ideally within the year, to include the constantly growing number of relevant studies. See Characteristics of studies awaiting classification for full details.
New studies found for this update
We are including seven additional trials, recruiting a total of 408 participants at randomisation. Of these, 374 participants remained in the trials by the time of outcome analysis (Blumenthal 2012a; Hemat‐Far 2012; Hoffman 2010; Gary 2010; Mota‐Pereira 2011; Shahidi 2011; Schuch 2011). See Characteristics of included studies.
Risk of bias in included studies
Sequence generation
We categorised 11 trials as being at low risk of bias, one as being at high risk of bias (Hemat‐Far 2012), and the rest as being at unclear risk of bias. A graphical representation of the 'Risk of bias' assessment can be seen in Figure 2 and Figure 3. Please see the Characteristics of included studies for the full 'Risk of bias' assessment for each study.
2.
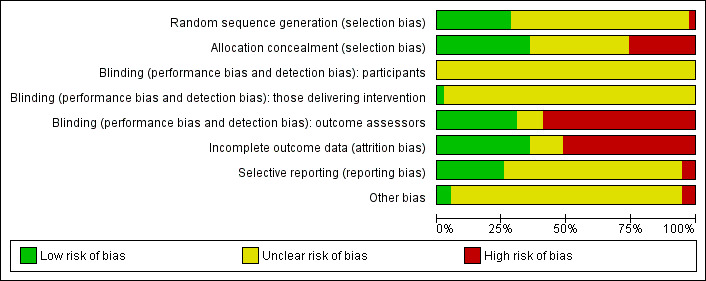
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
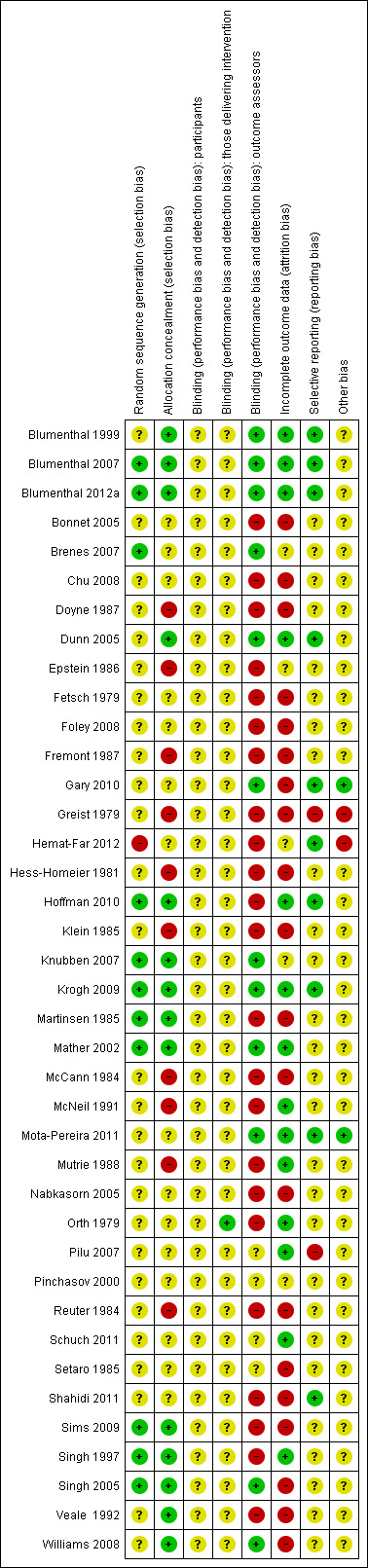
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Allocation concealment was adequate and therefore at low risk of bias in 14 trials (Blumenthal 2007; Blumenthal 2007; Blumenthal 2012a; Dunn 2005; Hoffman 2010; Knubben 2007; Krogh 2009; Martinsen 1985; Mather 2002; Sims 2009; Singh 1997; Singh 2005; Veale 1992; Williams 2008). For the remaining trials, the risk of bias was rated as unclear or high.
Blinding
Twelve trials included blinding of the outcome assessor so were rated as being at low risk of bias (Blumenthal 1999; Blumenthal 2007; Blumenthal 2012a; Brenes 2007; Dunn 2005; Gary 2010; Knubben 2007; Krogh 2009; Mather 2002; Mota‐Pereira 2011; Singh 2005; Williams 2008). The rest were categorised as being at unclear or high risk because they used self‐reported outcomes.
In exercise trials, participants cannot be blind to the treatment allocation. We were uncertain what effect this would have on bias, so we classified all trials as being at 'unclear' risk of bias. Similarly, for those trials where supervised exercise was provided, the person delivering the intervention could not be blind, so we classified all trials as being at 'unclear' risk of bias (note that not all reported whether exercise was performed with or without supervision).
Incomplete outcome data
Fifteen trials performed 'intention‐to‐treat' (ITT) analyses (Blumenthal 1999; Blumenthal 2007; Blumenthal 2012a; Dunn 2005; Hemat‐Far 2012; Hoffman 2010; Krogh 2009; Mather 2002; McNeil 1991; Mota‐Pereira 2011; Mutrie 1988; Orth 1979; Pilu 2007; Singh 1997; Schuch 2011), i.e. complete outcome data were reported or, if there were missing outcome data, these were replaced using a recognised statistical method, e.g. last observation carried forward, and participants remained in the group to which they had been allocated. One trial reported data for individual participants (Orth 1979), so by using last observation carried forward we replaced data from the participants who did not complete the trial and included these data in the meta‐analysis of ITT trials. One trial reported that the analysis was ITT, because it used a 'worse‐case' scenario assumption to replace data from participants who did not complete the trial, but only included 38 of the 39 randomised participants in the analyses, so we classified it as 'not ITT' (Knubben 2007). The remaining studies were classified as being at unclear or high risk of bias. Most trials did not report data from participants who dropped out.
Selective reporting
We attempted to identify whether a protocol was available by screening the reference list of the publications. We identified protocols for three trials and checked that all prespecified outcome events were reported, and rated these as being at low risk of bias (Blumenthal 2012a; Dunn 2005; Krogh 2009). We categorised four others trials (Hemat‐Far 2012; Hoffman 2010; Mota‐Pereira 2011; Shahidi 2011) as being at low risk of bias as we judged that there was sufficient information in the methods to be sure that the trials had reported all their planned outcomes.
Other potential sources of bias
On the basis of the first 50 participants, one study (Krogh 2009) changed their sample size calculation based on the observed standard deviation (they had initially calculated they needed a minimum of 186 participants (SD = 6), but for the first 50 participants the SD was 3.9 so they adjusted their sample size calculation to 135 participants). Hemat‐Far 2012 told the control group to reduce their activity.
We decided to include data on continuous depression scores in our meta‐analysis, rather than depression measured as a dichotomous outcome. This is because we knew from previous updates that very few trials had reported depression as a dichotomous outcome, and we wished to include as many trials as possible in our meta‐analysis. For future updates, we will consider whether to perform a separate meta‐analysis for trials that measured depression as a dichotomous outcome.
Publication bias
Visually our funnel plot appeared to be asymmetrical.
There is evidence of bias (Begg P value = 0.02, Egger P value = 0.002) (funnel plot for Analysis 1.1, exercise versus control, Figure 4) that might be due to publication bias, to outcome reporting bias or to heterogeneity.
1.1. Analysis.
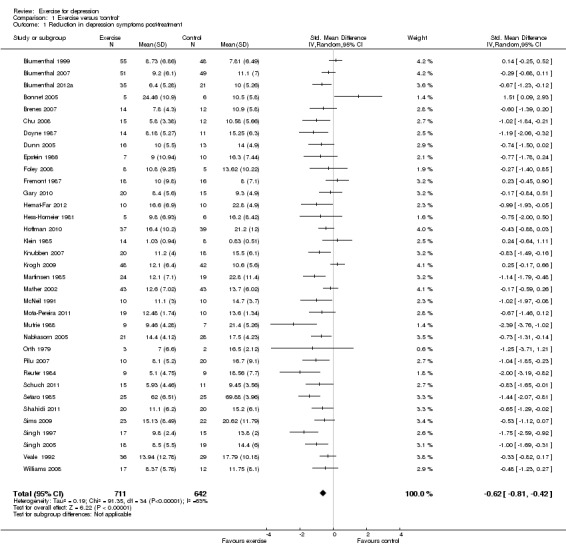
Comparison 1 Exercise versus 'control', Outcome 1 Reduction in depression symptoms post‐treatment.
4.
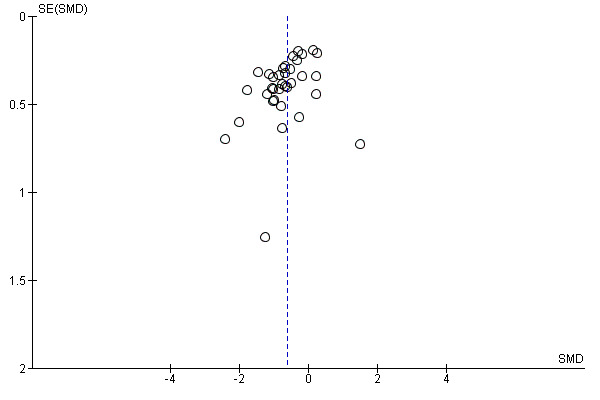
Funnel plot of comparison: 1 Exercise versus control, outcome: 1.1 Reduction in depression symptoms post‐treatment.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Summary of findings for the main comparison. Exercise compared to control for adults with depression.
| Exercise compared to no intervention or placebo for adults with depression | |||||
| Patient or population: adults with depression Settings: any setting Intervention: Exercise Comparison: no intervention or placebo | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| No intervention or placebo | Exercise | ||||
| Symptoms of depression Different scales Follow‐up: post‐treatment | The mean symptoms of depression in the control groups was 0 | The mean symptoms of depression in the intervention groups was 0.62 standard deviations lower (0.81 to 0.42 lower)1 | 1353 (35 studies) | ⊕⊕⊕⊝ moderate2,3,4 | SMD ‐0.62 (95% CI: ‐0.81 to ‐0.42). The effect size was interpreted as 'moderate' (using Cohen's rule of thumb) |
| Symptoms of depression (long‐term) different scales | The mean symptoms of depression (long‐term) in the control groups was 0 | The mean symptoms of depression (long‐term) in the intervention groups was 0.33 standard deviations lower (0.63 to 0.03 lower) | 377 (8 studies) | ⊕⊕⊝⊝ low4,5 | SMD ‐0.33 (95% CI: ‐0.63 to ‐0.03). The effect size was interpreted as 'small' (using Cohen's rule of thumb) |
| Adverse events | See comment | See comment | 0 (6 studies) | ⊕⊕⊕⊝ moderate | Seven trials reported no difference in adverse events between exercise and usual care groups. Dunn 2005 reported increased severity of depressive symptoms (n = 1), chest pain (n = 1) and joint pain/swelling (n = 1); all these participants discontinued exercise. Singh 1997 reported that 1 exerciser was referred to her psychologist at 6 weeks due to increasing suicidality; and musculoskeletal symptoms in 2 participants required adjustment of training regime. Singh 2005 reported adverse events in detail (visits to a health professional, minor illness, muscular pain, chest pain, injuries requiring training adjustment, falls, deaths and hospital days) and found no difference between the groups. Knubben 2007 reported "no negative effects of exercise (muscle pain, tightness or fatigue)"; after the training had finished, 1 person in the placebo group required gastric lavage and 1 person in the exercise group inflicted a superficial cut on her arm. Sims 2009 reported no adverse events or falls in either the exercise or control group. Blumenthal 2007 reported more side effects in the sertraline group (see comparison below) but there was no difference between the exercise and control group. Blumenthal 2012a reported more fatigue and sexual dysfunction in the sertraline group than the exercise group. |
| Acceptability of treatment | Study population | 1363 (29 studies) | ⊕⊕⊕⊝ moderate2 | RR 1 (95% CI: 0.97 to 1.04) | |
| 865 per 1000 | 865 per 1000 (839 to 900) | ||||
| Quality of life | The mean quality of life in the intervention groups was 0 higher (0 to 0 higher) | 0 (4 studies) | See comment | There was no statistically significant differences for the mental (SMD ‐0.24; 95% CI ‐0.76 to 0.29). psychological (SMD 0.28; 95% CI ‐0.29 to 0.86) and social domains (SMD 0.19; 95% CI ‐0.35 to 0.74). Two studies reported a statistically significant difference for the environment domain favouring exercise (SMD 0.62; 95% CI 0.06 to 1.18) and 4 studies reported a statistically significant difference for the physical domain favouring exercise (SMD 0.45; 95% CI 0.06 to 0.83). | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1 Effect estimate calculated by re‐expressing the SMD on the Hamilton Depression Rating Scale using the control group SD (7) from Blumenthal 2007 (study chosen for being most representative). The SD was multiplied by the pooled SMD to provide the effect estimate on the HDRS. 2 Lack of blinding of outcome assessors probably increased effect sizes and drop‐out rates were high. Also sequence generation was considered unclear in 23 studies. 3 I² = 63% and P < 0.00001, indicated moderate levels of heterogeneity 4 Population size is large, effect size is above 0.2 SD, and the 95% CI does not cross the line of no effect. 5 Lack of blinding of outcome assessors probably increased effect sizes and drop‐out rates were high. Also sequence generation was considered unclear in 4 studies.
Summary of findings 2. Exercise compared to psychological treatments for adults with depression.
| Exercise compared to cognitive therapy for adults with depression | |||||
| Patient or population: adults with depression Settings: Intervention: Exercise Comparison: cognitive therapy | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Cognitive therapy | Exercise | ||||
| Symptoms of depression | The mean symptoms of depression in the intervention groups was 0.03 standard deviations lower (0.32 lower to 0.26 higher) | 189 (7 studies) | ⊕⊕⊕⊝ moderate1,2,3 | SMD ‐0.03 (95% CI: ‐0.32 to 0.26) | |
| Acceptability of treatment | Study population | 172 (4 studies) | ⊕⊕⊕⊝ moderate1 | RR 1.08 (95% CI: 0.95 to 1.24) | |
| 766 per 1000 | 827 per 1000 (728 to 950) | ||||
| Quality of Life | The mean quality of life in the intervention groups was 0 higher (0 to 0 higher) | 0 (1 study) | ⊕⊕⊕⊝ moderate1 | One trial reported changes in the Minnesota Living with Heart Failure Questionnaire, a quality of life measure (Gary 2010). There was no statistically significant difference for the physical domain (MD 0.15; 95% CI: ‐7.40 to 7.70) or the mental domain (MD ‐0.09; 95% CI: ‐9.51 to 9.33). | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1 Lack of blinding of outcome assessors probably increased effect sizes and drop‐out rates were high. Also sequence generation was considered unclear in 7 studies. 2 I² = 0% and P = 0.62, indicated no heterogeneity 3 The studies included were all relevant to the review question, particularly given that all studies had to meet the criteria of the ACSM definition of exercise.
Summary of findings 3. Exercise compared to bright light therapy for adults with depression.
| Exercise compared to bright light therapy for adults with depression | |||||
| Patient or population: adults with depression Settings: Intervention: Exercise Comparison: bright light therapy | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Bright light therapy | Exercise | ||||
| Symptoms of depression | The mean symptoms of depression in the intervention groups was 6.4 lower (10.2 to 2.6 lower) | 18 (1 study) | ⊕⊝⊝⊝ very low1,2,3 | MD ‐6.40 (95% CI: ‐10.20 to ‐2.60). Although this trial suggests a benefit of exercise, it is too small to draw firm conclusions |
|
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1 Lack of blinding of outcome assessors probably increased effect sizes and drop‐out rates were not reported. Also sequence generation and concealment was considered unclear. 2 The study included was relevant to the review question, particularly given that all studies had to meet the criteria of the ACSM definition of exercise. 3 Based on 18 people
Summary of findings 4. Exercise compared to pharmacological treatments for adults with depression.
| Exercise compared to antidepressants for adults with depression | |||||
| Patient or population: adults with depression Settings: Intervention: Exercise Comparison: antidepressants | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Antidepressants | Exercise | ||||
| Symptoms of depression | The mean symptoms of depression in the intervention groups was 0.11 standard deviations lower (0.34 lower to 0.12 higher) | 300 (4 studies) | ⊕⊕⊕⊝ moderate1,2,3 | SMD ‐0.11 (95% CI: ‐0.34 to 0.12) | |
| Acceptability of treatment | Study population | 278 (3 studies) | ⊕⊕⊕⊝ moderate1 | RR 0.98 (95% CI: 0.86 to 1.12) | |
| 891 per 1000 | 873 per 1000 (766 to 997) | ||||
| Quality of life | The mean quality of life in the intervention groups was 0 higher (0 to 0 higher) | 0 (1 study) | ⊕⊕⊕⊝ moderate1 | One trial, Brenes 2007, reported no difference in change in SF‐36 mental health and physical health components between medication and exercise groups. | |
| Adverse events | See comment | See comment | 0 (3 studies) | ⊕⊕⊕⊝ moderate1 |
Blumenthal 1999 reported that 3/53 in exercise group suffered musculoskeletal injuries; injuries in the medication group were not reported. Blumenthal 2007 collected data on side effects by asking participants to rate a 36‐item somatic symptom checklist and reported that "a few patients reported worsening of symptoms"; of the 36 side effects assessed, only 1 showed a statistically significant group difference (P = 0.03), i.e. that the sertraline group reported worse post‐treatment diarrhoea and loose stools. Blumenthal 2012a assessed 36 side effects; only 2 showed a significant group difference: 20% of participants receiving sertraline reported worse post‐treatment fatigue compared with 2.4% in the exercise group and 26% reported increased sexual problems compared with 2.4% in the exercise group. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1 Lack of blinding of outcome assessors probably increased effect sizes and drop‐out rates were high. Also sequence generation was considered unclear in 1 study. 2 I² = 0% and P = 0.52, indicated no heterogeneity 3 The studies included were all relevant to the review question, particularly given that all studies had to meet the criteria of the ACSM definition of exercise.
We included 37 trials in our meta‐analyses. The remaining two trials could not be included for the reasons stated above (Greist 1979; McCann 1984).
Comparison 1: Exercise versus 'control'
Thirty‐five trials (1356 participants) included a comparison of exercise with a 'control' intervention.
Primary outcome measure
1.1 Reduction in depression symptom severity
Post‐treatment
The pooled standardised mean difference (SMD), for the 35 trials, calculated using the random‐effects model was ‐0.62 (95% confidence interval (CI) ‐0.81 to ‐0.42) (Analysis 1.1), indicating a moderate clinical effect in favour of exercise. There was substantial heterogeneity (I² = 63%).
End of long‐term follow‐up
The pooled SMD from the eight trials (Blumenthal 1999; Fremont 1987; Gary 2010; Klein 1985; Krogh 2009; Mather 2002; Sims 2009; Singh 1997) (377 participants) that provided long‐term follow‐up data found only a small effect in favour of exercise (SMD ‐0.33, 95% CI ‐0.63 to ‐0.03) (Analysis 1.2). The long‐term follow‐up data from Blumenthal 1999 were reported in a separate publication (Babyak 2000), and from Singh 1997 in a separate publication (Singh 2001). There was moderate statistical heterogeneity (I² = 49%). Follow‐up data from Blumenthal 2007 have been reported according to the proportion who had fully or partially remitted from depression, but continuous mood scores were not reported so we could not include these data in the meta‐analysis.
1.2. Analysis.
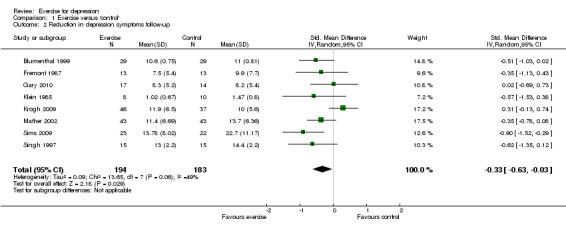
Comparison 1 Exercise versus 'control', Outcome 2 Reduction in depression symptoms follow‐up.
Secondary outcome measures
1.2a Acceptability of treatment: attendance at exercise
Fourteen trials reported attendance rates for exercise; these were 50.6% for aerobic and 56.2% for strength arm (Krogh 2009), 59% (Mather 2002), 70% (Doyne 1987), 72% (Dunn 2005), 78% (Nabkasorn 2005), 82% (Gary 2010), 91% (Mota‐Pereira 2011) 92% (Blumenthal 1999; Blumenthal 2007), 93% (Singh 1997), 94% (Blumenthal 2012a), 97.3% for high‐intensity and 99.1% for low‐intensity (Chu 2008) and 95% to 100% (Singh 2005). One trial reported the mean number of exercise sessions attended as 5.88 (Hoffman 2010). One trial rescheduled missed visits (McNeil 1991) so participants attended the full course of exercise. As with intensity of exercise, it is difficult to attribute any differences in outcome to differences in attendance rates, because there were other sources of variation in the type of interventions (e.g. duration of intervention, type of exercise) and differences in the methodological quality between trials which might account for differences in outcome.
1.2b Acceptability of treatment: completing the intervention or control
We extracted data on the number randomised and completing each trial (see Table 5). This ranged from 100% completion (Hemat‐Far 2012; Mather 2002; McNeil 1991; Mutrie 1988; Pilu 2007; Singh 1997; Schuch 2011) to 42% completion (Doyne 1987). For the exercise intervention, this ranged from 100% completion (Gary 2010; Hemat‐Far 2012; Mather 2002; McNeil 1991; Mutrie 1988; Pilu 2007; Singh 1997; Schuch 2011) to 55% completion (Klein 1985).
Twenty‐nine studies (1363 participants) reported how many completed the exercise and control arms (Analysis 1.3). The risk ratio (RR) was 1.00 (95% CI 0.97 to 1.04).
1.3. Analysis.
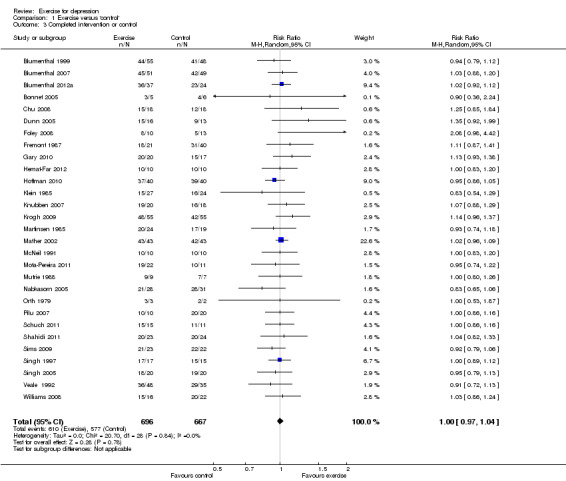
Comparison 1 Exercise versus 'control', Outcome 3 Completed intervention or control.
1.3. Quality of life
Five trials reported quality of life at the end of treatment (Gary 2010; Hoffman 2010; Schuch 2011; Singh 2005; Pilu 2007). One author provided data regarding the different domains (Gary 2010). One trial reported quality of life at baseline but not at follow‐up (Sims 2009).
There were no statistically significant differences for the mental (SMD ‐0.24; 95% CI ‐0.76 to 0.29), psychological (SMD 0.28; 95% CI ‐0.29 to 0.86) and social domains (SMD 0.19; 95% CI ‐0.35 to 0.74) (Analysis 1.4). Two studies reported a statistically significant difference for the environment domain favouring exercise (SMD 0.62; 95% CI 0.06 to 1.18) and four studies reported a statistically significant difference for the physical domain favouring exercise (SMD 0.45; 95% CI 0.06 to 0.83).
1.4. Analysis.
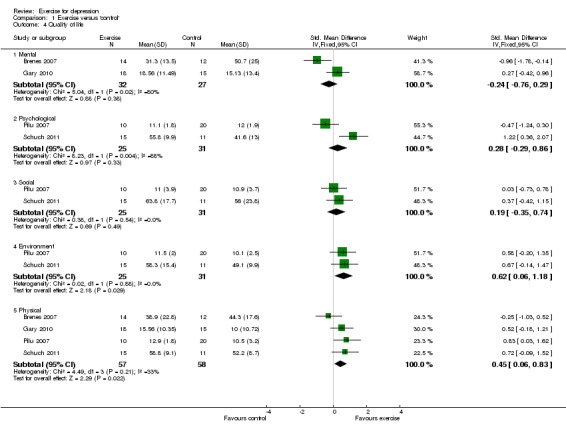
Comparison 1 Exercise versus 'control', Outcome 4 Quality of life.
1.4 Cost
No trial reported costs.
1.5 Adverse events
Seven trials reported no difference in adverse events between the exercise and usual care groups (Blumenthal 2007; Blumenthal 2012a; Dunn 2005; Knubben 2007; Singh 1997; Singh 2005; Sims 2009). Dunn 2005 reported increased severity of depressive symptoms (n = 1), chest pain (n = 1) and joint pain/swelling (n = 1); all these participants discontinued exercise. Singh 1997 reported that one exerciser was referred to her psychologist at six weeks due to increasing suicidality; and musculoskeletal symptoms in two participants required adjustment of training regime. Singh 2005 reported adverse events in detail (visits to a health professional, minor illness, muscular pain, chest pain, injuries requiring training adjustment, falls, deaths and hospital days) and found no difference between the groups. Knubben 2007 reported "no negative effects of exercise (muscle pain, tightness or fatigue)"; after the training had finished, one person in the placebo group required gastric lavage and one person in the exercise group inflicted a superficial cut in her arm. Sims 2009 reported no adverse events or falls in either the exercise or control groups. Blumenthal 2007 reported more side effects in the sertraline group (see comparison below) but there was no difference between the exercise and control group. Blumenthal 2012a reported more fatigue and sexual dysfunction in the sertraline group than in the exercise group.
Because of the diversity of different adverse events reported, we decided not to do a meta‐analysis of these data.
Comparison 2: Exercise versus psychological therapies
Primary outcome
2.1 Reduction in depression symptom severity
Post‐treatment
Seven trials (189 participants) provided data comparing exercise with psychological therapies; the SMD was ‐0.03 (95% CI ‐0.32 to 0.26) (Analysis 2.1) indicating no significant difference between the two interventions. No statistical heterogeneity was indicated.
2.1. Analysis.
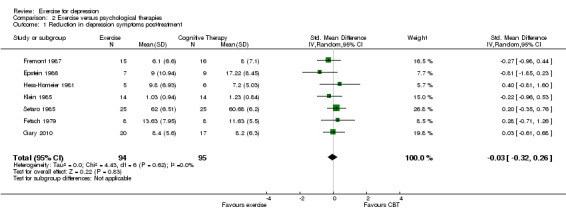
Comparison 2 Exercise versus psychological therapies, Outcome 1 Reduction in depression symptoms post‐treatment.
End of long‐term follow‐up
There were insufficient data available for long‐term follow‐up.
Secondary outcomes
2.2a Acceptability of treatment: attendance at exercise sessions
One trial reported adherence scores that were calculated based on the number of sessions attended of those prescribed. This trial reported that the adherence rates were 82% for exercise and 72% for CBT (Gary 2010).
2.2b Acceptability of treatment: completing the intervention or psychological therapies
For staying in the trial, there were data from four trials (172 participants) (Analysis 2.2). The risk ratio was 1.08 (95% CI 0.95 to 1.24).
2.2. Analysis.
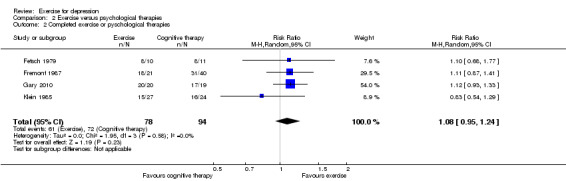
Comparison 2 Exercise versus psychological therapies, Outcome 2 Completed exercise or pyschological therapies.
2.3. Quality of life
One trial reported changes in the Minnesota Living with Heart Failure Questionnaire, a quality of life measure (Gary 2010). There was no statistically significant difference for the physical domain (MD 0.15; 95% CI: ‐7.40 to 7.70) or the mental domain (MD ‐0.09; 95% CI: ‐9.51 to 9.33) (Analysis 2.3).
2.3. Analysis.
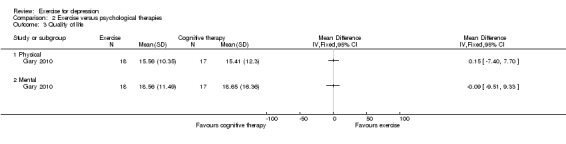
Comparison 2 Exercise versus psychological therapies, Outcome 3 Quality of life.
2.4 Cost
No trial reported costs.
2.5 Adverse events
No data available.
Comparison 3: Exercise versus alternative treatments
Primary outcome
3.1 Reduction in depression symptom severity
Post‐treatment
One trial found that exercise was superior to bright light therapy in reducing depression symptoms (Pinchasov 2000) (MD ‐6.40, 95% CI ‐10.20 to ‐2.60) (Analysis 3.1).
3.1. Analysis.
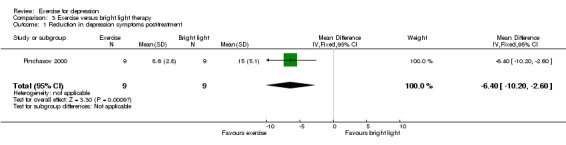
Comparison 3 Exercise versus bright light therapy, Outcome 1 Reduction in depression symptoms post‐treatment.
End of long‐term follow‐up
There were no data with regard to long‐term follow‐up.
Secondary outcomes
This trial did not report on any of the following outcomes.
3.2a Acceptability of treatment: attendance at exercise
3.2b Acceptability of treatment: completing the intervention or control
3.3. Quality of life
3.4 Cost
3.5 Adverse events
Comparison 4: Exercise versus pharmacological treatments
Primary outcome
4.1 Reduction in depression symptom severity
Post‐treatment
For the four trials (298 participants) that compared exercise with pharmacological treatments (Blumenthal 1999; Blumenthal 2007; Blumenthal 2012a; Brenes 2007) the SMD was ‐0.11 (95% CI ‐0.34 to 0.12) (Analysis 4.1), indicating no significant difference between the two interventions. No statistical heterogeneity was indicated.
4.1. Analysis.
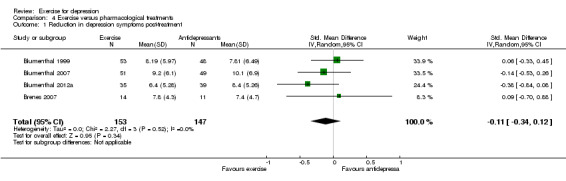
Comparison 4 Exercise versus pharmacological treatments, Outcome 1 Reduction in depression symptoms post‐treatment.
End of long‐term follow‐up
There were insufficient data available for long‐term follow‐up.
Secondary outcomes
4.2a Acceptability of treatment: attendance at exercise
Blumenthal 1999 reported that of those allocated exercise alone, the median number of sessions attended was 89.6%. Of those allocated medication, no participant deviated by more than 5% from the prescribed dose.
4.2b Acceptability of treatment: completing the intervention or pharmacological intervention
For remaining in the trial, there were data from three trials (278 participants). The risk ratio was 0.98 (95% CI 0.86 to 1.12) (Analysis 4.2).
4.2. Analysis.
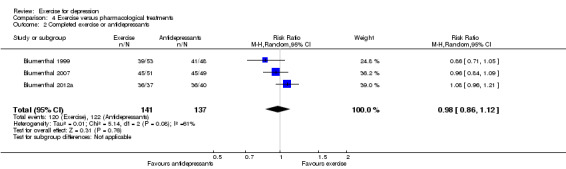
Comparison 4 Exercise versus pharmacological treatments, Outcome 2 Completed exercise or antidepressants.
4.3. Quality of life
One trial Brenes 2007 reported no difference in change in SF‐36 mental health and physical health components between medication and exercise groups (Analysis 4.3).
4.3. Analysis.
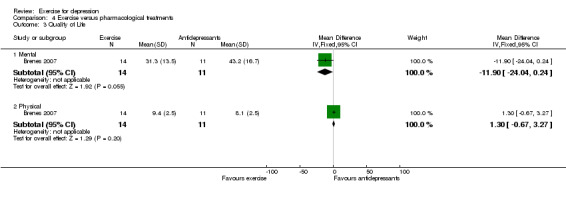
Comparison 4 Exercise versus pharmacological treatments, Outcome 3 Quality of Life.
4.4 Cost
No trial reported costs.
4.5 Adverse events
Blumenthal 1999 reported that 3/53 in the exercise group suffered musculoskeletal injuries; injuries in the medication group were not reported.
Blumenthal 2007 collected data on side effects by asking participants to rate a 36‐item somatic symptom checklist and reported that "a few patients reported worsening of symptoms"; of the 36 side effects assessed, only one showed a statistically significant group difference (P = 0.03), i.e. that the sertraline group reported worse post‐treatment diarrhoea and loose stools.
Blumenthal 2012a assessed 36 side effects; only two showed a significant group difference: 20% of participants receiving sertraline reported worse post‐treatment fatigue compared with 2.4% in the exercise group and 26% reported increased sexual problems compared with 2.4% in the exercise group.
Subgroup analyses
Type of exercise
We explored the influence of the type of exercise (aerobic, mixed or resistance) on outcomes for those trials comparing exercise versus control (Analysis 5.1). The SMD for aerobic exercise indicated a moderate clinical effect (SMD ‐0.55, 95% CI ‐0.77 to ‐0.34), whilst the SMDs for both mixed exercise (SMD ‐0.85, 95% CI ‐1.85 to 0.15) and resistance exercise (SMD ‐1.03, 95% CI ‐1.52 to ‐0.53) indicated large effect sizes, but with wide confidence intervals.
5.1. Analysis.
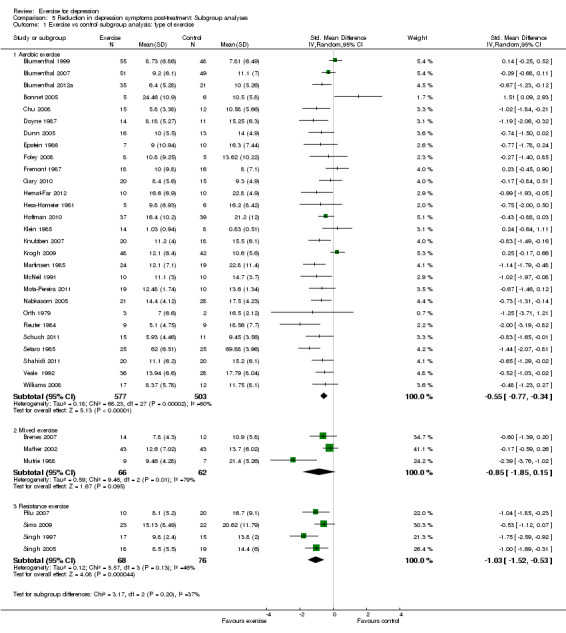
Comparison 5 Reduction in depression symptoms post‐treatment: Subgroup analyses, Outcome 1 Exercise vs control subgroup analysis: type of exercise.
Intensity of exercise
We explored the influence of intensity (light/moderate, moderate, moderate/hard, hard, moderate/vigorous, vigorous) on the reduction of depression for those trials comparing exercise versus control (Analysis 5.2). The SMD for moderate/vigorous intensity (SMD ‐0.38, 95% CI ‐1.61 to 0.85) indicated a small effect size, whilst for moderate (SMD ‐0.64, 95% CI ‐1.01 to ‐0.28), moderate/hard (SMD ‐0.63, 95% CI ‐1.13 to ‐0.13) and hard intensity (SMD ‐0.56, 95% CI ‐0.93 to ‐0.20) there was a moderate clinical effect. A large effect size was indicated for vigorous intensity (SMD ‐0.77, 95% CI ‐1.30 to ‐0.24) and light/moderate intensity (SMD ‐0.83, 95% CI ‐1.32 to ‐0.34).
5.2. Analysis.
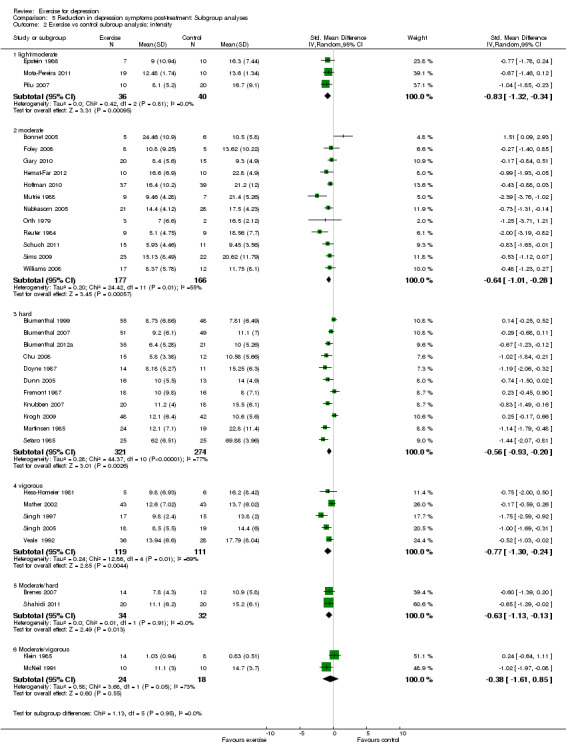
Comparison 5 Reduction in depression symptoms post‐treatment: Subgroup analyses, Outcome 2 Exercise vs control subroup analysis: intensity.
Duration and frequency of exercise
We explored the influence of the total number of prescribed exercise sessions (0 ‐ 12, 13 ‐ 24, 25 ‐ 36, 37+ sessions) on the reduction of depression for those trials comparing exercise versus control (Analysis 5.3). A moderate effect size was observed for 0 ‐ 12 sessions (SMD ‐0.42, 95% CI ‐1.26 to 0.43), and 37+ sessions (SMD ‐0.46, 95% CI ‐0.69 to ‐0.23). A large effect size was observed for 13 ‐ 24 sessions (SMD ‐0.70, 95% CI ‐1.09 to ‐0.31) and 25 ‐ 36 sessions (SMD ‐0.80, 95% CI ‐1.30 to ‐0.29).
5.3. Analysis.
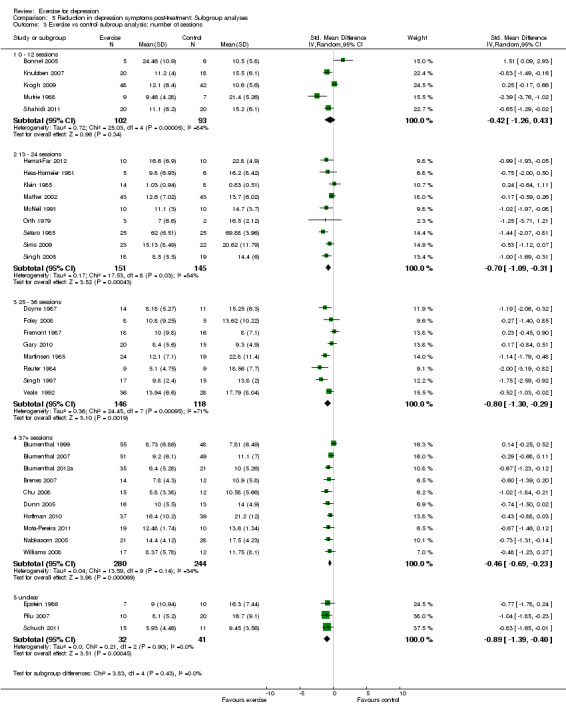
Comparison 5 Reduction in depression symptoms post‐treatment: Subgroup analyses, Outcome 3 Exercise vs control subroup analysis: number of sessions.
Type of diagnosis
We performed subgroup analyses according to how the diagnosis of depression was made (cut‐point on a scale, or clinical interview and proper psychiatric diagnosis) (Analysis 5.4). There was a moderate effect size for clinical diagnosis of depression (SMD ‐0.57, 95% CI ‐0.81 to ‐0.32) and a cut‐point on a scale (SMD ‐0.67, 95% CI ‐0.95 to ‐0.39).
5.4. Analysis.
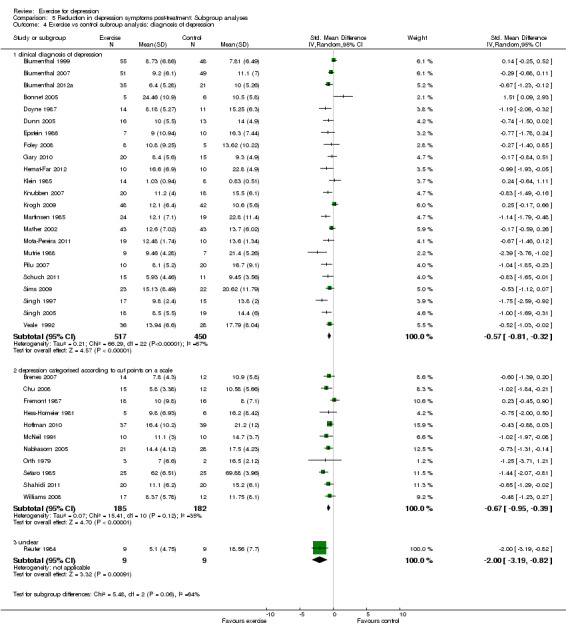
Comparison 5 Reduction in depression symptoms post‐treatment: Subgroup analyses, Outcome 4 Exercise vs control subroup analysis: diagnosis of depression.
Type of control
We categorised controls as a) placebo; b) no treatment (including waiting list); c) exercise plus treatment versus treatment alone; d) stretching, meditation or relaxation; e) 'occupational', including education, occupational therapy. These categorisations were made by one author (KD) on the basis of data extracted at the initial stage of data extraction, and were checked by a second author (GM) (Analysis 5.5). The largest effect size was when exercise was compared with 'occupational' (SMD ‐3.67, 95% CI ‐4.94 to ‐2.41), and there was no statistically significant effect of exercise when it was compared with 'stretching, meditation or relaxation' (SMD ‐0.09 (95% CI ‐0.65 to 0.48).
We considered whether to perform additional subgroup analyses according to supervised versus unsupervised, indoor versus outdoor and individual versus group, and according to the type of control group (in the no‐treatment comparison) but we wanted to focus on the main subgroups of interest. Multiple subgroup analyses are generally considered inadvisable.
Sensitivity analyses
We conducted sensitivity analyses for the first comparison of exercise versus control to explore the impact of study quality on effect sizes. We have commented on how these sensitivity analyses influence pooled SMD, compared with the pooled SMD for the 35 trials comparing exercise with control (‐0.62 (95% CI) ‐0.81 to ‐0.42) (Analysis 1.1).
Peer‐reviewed journal publications
For the 34 trials (1335 participants) that were reported in peer‐reviewed journal publications or doctoral theses, the SMD was ‐0.59 (95% CI ‐0.78 to ‐0.40) (Analysis 6.1), showing a moderate clinical effect in favour of exercise, which is similar to the pooled SMD for all 35 trials.
6.1. Analysis.
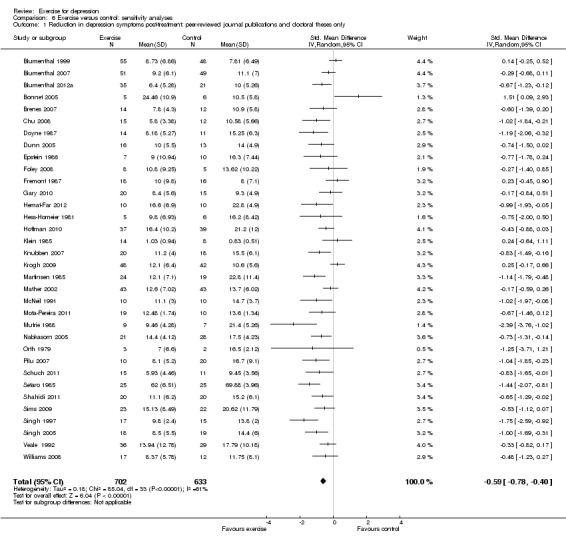
Comparison 6 Exercise versus control: sensitivity analyses, Outcome 1 Reduction in depression symptoms post‐treatment: peer‐reviewed journal publications and doctoral theses only.
Published as abstracts/conference proceedings only
The pooled SMD for the one study published as conference abstracts only was ‐2.00 (95% CI ‐3.19 to ‐0.82) (Analysis 6.2), showing a large effect size in favour of exercise i.e. larger than the pooled SMD for all 35 trials.
6.2. Analysis.
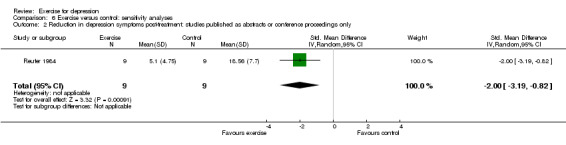
Comparison 6 Exercise versus control: sensitivity analyses, Outcome 2 Reduction in depression symptoms post‐treatment: studies published as abstracts or conference proceedings only.
Allocation concealment
For the 14 trials (829 participants) with adequate allocation concealment and therefore at low risk of bias, the SMD was ‐0.49 (95% CI ‐0.75 to ‐0.24) (Analysis 6.3), showing a moderate clinical effect in favour of exercise, similar to the pooled SMD for all 35 trials.
6.3. Analysis.
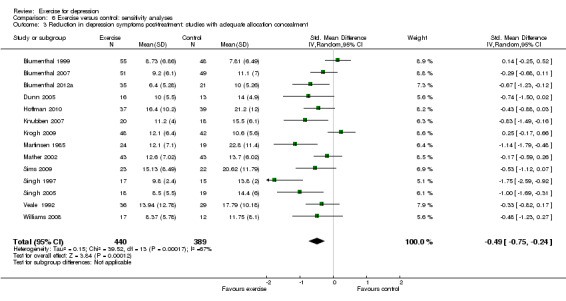
Comparison 6 Exercise versus control: sensitivity analyses, Outcome 3 Reduction in depression symptoms post‐treatment: studies with adequate allocation concealment.
Use of intention‐to‐treat analysis
For the 11 trials (567 participants) with intention‐to‐treat analyses, the SMD was ‐0.61 (95% CI ‐1.00 to ‐0.22) (Analysis 6.4), showing a moderate clinical effect in favour of exercise, similar to the pooled SMD for all 35 trials.
6.4. Analysis.
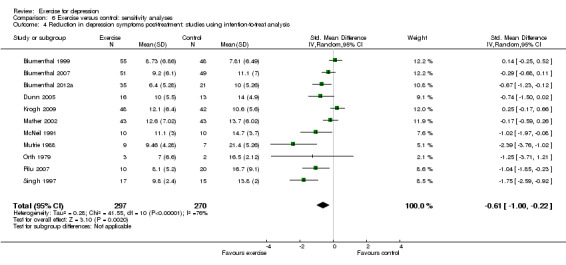
Comparison 6 Exercise versus control: sensitivity analyses, Outcome 4 Reduction in depression symptoms post‐treatment: studies using intention‐to‐treat analysis.
Blinded outcome assessment
For the 12 trials (658 participants) with blinded outcome assessments and therefore at low risk of bias, the SMD was ‐0.36 (95% CI ‐0.60 to ‐0.12) (Analysis 6.5), showing a small clinical effect in favour of exercise,which is smaller than the pooled SMD for all 35 trials.
6.5. Analysis.
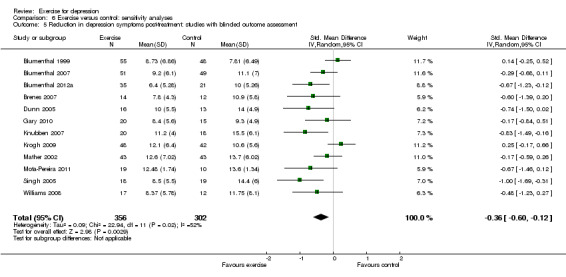
Comparison 6 Exercise versus control: sensitivity analyses, Outcome 5 Reduction in depression symptoms post‐treatment: studies with blinded outcome assessment.
Allocation concealment and intention‐to‐treat analysis and blinded outcome assessment
For the six trials (Blumenthal 1999; Blumenthal 2007; Blumenthal 2012a; Dunn 2005; Krogh 2009; Mather 2002) (464 participants) with adequate allocation concealment and intention‐to‐treat analyses and blinded outcome assessment and therefore at low risk of bias, the SMD was ‐0.18 (95% CI ‐0.47 to 0.11) (Analysis 6.6), i.e. there was a small clinical effect in favour of exercise, which did not reach statistical significance. This is smaller than the pooled SMD for all 35 trials.
6.6. Analysis.
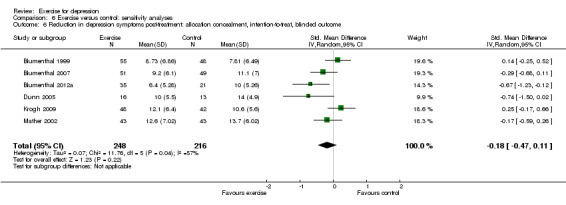
Comparison 6 Exercise versus control: sensitivity analyses, Outcome 6 Reduction in depression symptoms post‐treatment: allocation concealment, intention‐to‐treat, blinded outcome.
Sensitivity analyses: including the arm with the smallest dose of exercise for those trials for which we used the arm with the largest dose of exercise in comparison 1
We included the arm with the smallest dose of exercise for 10 trials (Blumenthal 2007; Chu 2008; Doyne 1987; Dunn 2005; Krogh 2009; Mutrie 1988; Orth 1979; Setaro 1985; Singh 2005; Williams 2008) for which we had used the arm with the largest clinical effect in comparison 1 (Analysis 1.1). The SMD was ‐0.44 (95% CI ‐0.55 to ‐0.33) (Analysis 6.7), showing a moderate clinical effect in favour of exercise. This is similar to the pooled SMD for all 35 trials.
6.7. Analysis.
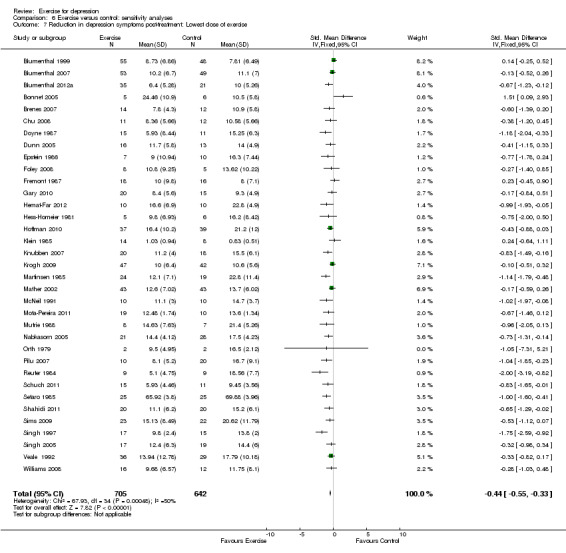
Comparison 6 Exercise versus control: sensitivity analyses, Outcome 7 Reduction in depression symptoms post‐treatment: Lowest dose of exercise.
Recruitment and retention of participants
Table 5 presents data about the feasibility of recruiting and retaining participants both in the trial as a whole and in the exercise intervention in particular. We extracted data, when available, about the number of participants who were considered for inclusion in each trial, although this information was not available for all trials. The trials that did provide these data used different recruitment techniques (ranging from screening of people responding to advertisements to inclusion of those patients who were considered eligible by a referring doctor).
Discussion
Summary of main results
This updated review includes seven additional trials (384 additional participants); conclusions are similar to our previous review (Rimer 2012). The pooled standardised mean difference (SMD), for depression (measured by continuous variable), at the end of treatment, represented a moderate clinical effect. The 'Summary of findings' table suggests that the quality of the evidence is moderate.
There was some variation between studies with respect to attendance rates for exercise as an intervention, suggesting that there may be factors that influence acceptability of exercise among participants.
There was no difference between exercise and psychological therapy or pharmacological treatment on the primary outcome. There are too few data to draw conclusions about the effect of exercise on our secondary outcomes, including risk of harm.
Uncertainties
Uncertainties remain regarding how effective exercise is for improving mood in people with depression, primarily due to methodological shortcomings (please see below). Furthermore, if exercise does improve mood in people with depression, we cannot determine the optimum type, frequency and duration of exercise, whether it should be performed supervised or unsupervised, indoors or outdoors, or in a group or alone. There was, however, a suggestion that more sessions have a larger effect on mood than a smaller number of sessions, and that resistance and mixed training were more effective than aerobic training. Adverse events in those allocated to exercise were uncommon, but only a small number of trials reported this outcome. Ideally both the risks and benefits of exercise for depression should be evaluated in future trials. There were no data on costs, so we cannot comment on the cost‐effectiveness of exercise for depression. The type of control intervention may influence effect sizes. There was a paucity of data comparing exercise with psychological and pharmacological treatments; the available evidence suggests that exercise is no more effective than either psychological or pharmacological treatments.
Overall completeness and applicability of evidence
For this current update, we searched the CCDAN Group's trial register in September 2012, which is an up‐to‐date and comprehensive source of trials. We also searched the WHO trials portal in March 2013 in order to identify new ongoing trials. We scrutinised reference lists of the new trials identified. Ideally, we would have performed citation reference searches of all included studies, but with the large number of trials now in this review, this was no longer practical. Thus, it is possible that we may have missed some relevant trials. We updated our search of the CCDAN trials register up to 1st March 2013 and identified several studies that may need to be included in our next update. It is notable that in a seven‐month period (September 2012 to March 2013), several more potentially eligible completed trials have been published (Characteristics of studies awaiting classification). This demonstrates that exercise for depression is a topic of considerable interest to researchers, and that further updates of this review will be needed, ideally once a year, to ensure that the review is kept as up‐to‐date as possible.
The results of this review are applicable to adults classified by the trialists as having depression (either by a cut‐off score on a depression scale or by having a clinical diagnosis of depression) who were willing to participate in a programme of regular physical exercise, fulfilling the American College of Sports Medicine (ACSM) definition of exercise, within the context of a randomised controlled clinical trial. The trials we included are relevant to the review question. It is possible that only the most motivated of individuals were included in this type of research.
The data we extracted on aspects of feasibility (see Table 5) suggest that a large number of people need to be screened to identify suitable participants, unless recruiting from a clinical population, e.g. inpatients with depression. Note, though, that there was a wide range in the proportion of those screened who were subsequently randomised; this may be a function of the sampling frame (which may include a range of specifically screened or non‐screened potential participants), and interest in being a research participant at a time of low mood, as much as whether potential participants are interested in exercise as a therapy. A substantial number of people dropped out from both the exercise and control programmes, and even those who remained in the trial until the outcome assessments were not able to attend all exercise sessions.
We did not include trials in which advice was given to increase activity. Thus, we excluded a large, high‐quality trial (n = 361) in which people with depression in primary care were randomised to usual care or to usual care plus advice from a physical activity facilitator to increase activity (Chalder 2012), which showed no effect of the intervention on mood.
We had previously decided to exclude trials which included people both with and without depression, even if they reported data from a subgroup with depression. Thus, for this update, we excluded a large, high‐quality, cluster‐randomised trial recruiting 891 residents from 78 nursing homes (Underwood 2013), of whom 375 had baseline Geriatric Depression Scores suggesting depression. At the end of the treatment, there was no difference between the intervention and control group, for people both with and without depression at baseline. For future updates, we will include data from trials that reported subgroups with depression.
If this review had had broader inclusion criteria in relation to the type of intervention, we would have included additional studies, e.g. trials which provide advice to increase activity (e.g. Chalder 2012) and trials of other types of physical activity interventions that do not fulfil the ACSM definition for exercise (e.g. Tai Chi or Qigong, where mental processes are practiced alongside physical activity and may exert an additional or synergistic effect). Arguably, the review could be broader, but we have elected to keep the it more focused, partly to ensure that it remains feasible to update the review on a regular basis, with the resources we have available. The original review questions were conceived more than 10 years ago (Lawlor 2001), and although they are still relevant today, it would be of value to broaden the research questions to include evidence for other modes of physical activity. This could be through a series of related Cochrane reviews. There are already separate reviews of Tai Chi for depression, and we suggest that a review of advice to increase physical activity would be of value.
This review did not attempt to take into account the effects of exercise when the experience is pleasurable and self‐determined, though this would have been difficult as such data were not reported in the trials.
There were more women than men in the studies that we included, and there was a wide range in mean ages. We cannot currently make any new recommendations for the effectiveness of exercise referral schemes for depression (DOH 2001; Pavey 2011; Sorensen 2006). One study of the Welsh exercise referral scheme is 'awaiting assessment'. Nor can we be certain about the effect of exercise on other relevant outcomes e.g. quality of life, adverse events or its cost‐effectiveness because the majority of trials did not systematically report this information, although our meta‐analysis of quality of life suggested that exercise did not significantly improve quality of life compared to control.
We cannot comment about the effect of exercise in people with dysthymia (or sub‐clinical depression) and in those without mood disorders, as we explicitly excluded these trials from the review. Future systematic reviews and meta‐analyses might include these people, although new reviews would need to ensure that the search strategy was sufficiently comprehensive to identify all relevant trials. We excluded trials of exercise for postnatal depression (as we had done for our previous update).
Quality of the evidence
The majority of the trials we included were small and many had methodological weaknesses. We explicitly aimed to determine the influence of study quality, in particular allocation concealment, blinding and intention‐to‐treat analyses on effect sizes, as we had done in previous review versions (Lawlor 2001; Mead 2009, Rimer 2012). When only those trials with adequate allocation concealment and intention‐to‐treat analysis and blinded outcome assessors were included, the effect size was clinically small and not statistically significant (Analysis 6.6).
There was substantial heterogeneity; this might be explained by a number of factors including variation in the control intervention. However, when only high‐quality trials were included, the effect size was small and not statistically significant. Of the eight trials (377 participants) that provided long‐term follow‐up data, there was only a small effect in favour of exercise (SMD ‐0.33, 95% CI ‐0.63 to ‐0.03) at the end of long‐term follow‐up, This suggests that any benefits of exercise at the end of treatment may be lost over time. Thus, exercise may need to be continued in the longer term to maintain any early benefits. Our summary of findings tables indicate that the quality of evidence is low ('Summary of findings' table 5).
Our subgroup analyses showed that effect sizes were higher for mixed exercise and resistance exercise than for aerobic exercise alone, but confidence intervals were wide (Analysis 5.1). There were no apparent differences in effect sizes according to intensity of exercise (Analysis 5.2). Effect sizes were smaller in trials which provided fewer than 12 sessions of exercise (Analysis 5.3). Effect sizes were not statistically significant when compared with stretching, meditation or relaxation (Analysis 5.5). Our sensitivity analysis for 'dose' of exercise suggested that a lower dose of exercise was less effective than a higher dose (Analysis 6.7). Although our subgroup analyses, are simply observational in nature, they are not inconsistent with the current recommendations by NICE (NICE 2009).
We extracted information from the trials about other potential sources of biases, in line with the Cochrane Collaboration 'Risk of bias' tool. In exercise trials, it is generally not possible to blind participants or those delivering the intervention to the treatment allocation. Thus, if the primary outcome is measured by self report, this is an important potential source of bias. When we performed sensitivity analysis by including only those trials with blinded outcome assessors, the effect size was smaller than when these trials were included. This suggests that self report may lead to an overestimate of treatment effect sizes. It is important to note, however, that clinician‐rated outcomes (e.g. Hamilton Rating Scale for Depression) may also be subject to clinical interpretation and therefore are not free from bias. For random sequence generation, the risk of bias was unclear for most of the trials. For selective reporting, we categorised risk of bias as unclear for most of the trials, although we did not have the study protocols.
Furthermore, the funnel plot was asymmetrical suggesting small study bias, heterogeneity or outcome reporting bias.
Potential biases in the review process
We attempted to avoid bias by ensuring that we had identified all relevant studies through comprehensive systematic searching of the literature and contact with authors of the trials to identify other trials, both published and unpublished. However, we accept that some publication bias is inevitable and this is indicated by the asymmetrical funnel plot. This is likely to lead to an overestimate of effect sizes, because positive trials are more likely to be published than negative trials. The searches for this current update were less extensive than for the initial review in 2001 (Lawlor 2001), but because the CCDAN register of trials is updated regularly from many different sources, we think it is unlikely that we have missed relevant trials.
As noted above, there is considerable interest in the continued development of a robust and accurate evidence base in this field to guide practice and healthcare investment. We are already aware of three recent additional studies that were identified through extensive searches of CCDANCTR. Initial scrutiny of these studies suggests that they would not overturn our conclusions, but they highlight the need to maintain regular updates of this review.
For a previous version of this review (Mead 2009), we made post hoc decisions to exclude trials defined as a 'combination' intervention, a trial in which the exercise intervention lasted only four days (Berlin 2003), and trials of postnatal depression (Armstrong 2003; Armstrong 2004). For the update in 2012, (Rimer 2012), we specified in advance that we would exclude trials that did not fulfil the ACSM criteria (ACSM 2001) for exercise; this meant that we excluded two studies (Chou 2004; Tsang 2006) that had previously been included.
In previous versions of the review, we used data from the arm with the largest clinical effect; this approach could have biased the results in favour of exercise. For this update, we used the largest 'dose' of exercise and performed a sensitivity analyses to determine the effect of using the smaller 'dose' (Analysis 6.7). This showed that the effect size was slightly smaller for the lower dose than the higher dose (‐0.44 for the lower dose and ‐0.62 for the higher dose). This is consistent with one of the subgroup analyses which showed that fewer than 12 sessions was less effective than a larger number of sessions.
We performed several subgroup analyses, which, by their nature, are simply observational. A variety of control interventions were used. We explored the influence of the type of control intervention (Analysis 5.5); this suggests that exercise may be no more effective than stretching/meditation or relaxation on mood. When we performed subgroup analysis of high‐quality trials only, we categorised the comparator (relaxation) in one of the trials as a control intervention (Krogh 2009), rather than as an active treatment. Had we categorised relaxation as an active treatment,(e.g.Analysis 6.6), exercise would have had a larger clinical effect in the meta‐analysis.
Agreements and disagreements with other studies or reviews
Previous systematic reviews which found that exercise improved depression included uncontrolled trials (Blake 2009; Carlson 1991; Craft 2013; North 1990; Pinquart 2007), so the results of these reviews are probably biased in favour of exercise. Another systematic review (Stathopoulou 2006) which identified trials in peer‐reviewed journals only included only eight of the trials which we identified for our review (Doyne 1987; Dunn 2005; Klein 1985; McNeil 1991; Pinchasov 2000; Singh 1997; Singh 2005; Veale 1992), and also included two trials which we had excluded (Bosscher 1993; Sexton 1989). This review (Stathopoulou 2006) found a larger effect size than we did. A further two reviews included mainly older people (Blake 2009; Sjosten 2006), whereas we included participants of all ages (aged 18 and over). Another meta‐analysis (Rethorst 2009) concluded that exercise is effective as a treatment for depression, and also found a larger effect size than we did. A narrative review of existing systematic reviews suggested that it would seem appropriate that exercise is recommended in addition to other treatments pending further high‐quality trial data (Daley 2008). However, a systematic review that included only studies where participants had a clinical diagnosis of depression according to a healthcare professional found no benefit of exercise (Krogh 2011). Another review of walking for depression suggested that walking might be a useful adjunct for depression treatment, and recommended further trials (Robertson 2012).
Authors' conclusions
Implications for practice.
Our review suggested that exercise might have a moderate‐sized effect on depression, but because of the risks of bias in many of the trials, the effect of exercise may only be small. We cannot be certain what type and intensity of exercise may be effective, and the optimum duration and frequency of a programme of exercise. There are few data on whether any benefits persist after exercise has stopped.
The evidence also suggests that exercise may be as effective as psychological or pharmacological treatments, but the number of trials reporting these comparisons and the number of participants randomised, were both small.
Implications for research.
A future update of the current review, including results from ongoing trials and those 'awaiting classification', may increase the precision of estimates of effect sizes. Future systematic reviews and meta‐analyses could be performed to investigate the effect of exercise on people with dysthymia.
This review would be strengthened by additional large‐scale high‐quality studies where all participants at the time of recruitment were diagnosed through clinical interview as having depression, adhered closely to an exercise regimen as a sole intervention and were further assessed through diagnostic clinical interview post‐intervention.
It would also be worth considering whether any long‐lasting effects of exercise correlated with sustained increases in physical activity over time. Now that we can measure physical activity directly using accelerometers, this would be a feasible piece of research to perform.
There is a paucity of data comparing exercise with psychological treatments and pharmacological treatments. Further trials are needed in this area.
Feedback
Concerning the DOSE 2002 trial, 3 November 2009
Summary
I recently read [the] review entitled "Exercise for Depression" and would like to point out some errors in your review. First, you stated the following in your review, "We attempted to extract data on intensity of exercise but this was reported for only a few trials, and there was too much variation in other aspects of the trial methodologies to attribute differences in outcomes to differences exercise intensities. One of the included trials compared four different 'doses' of aerobic exercise (DOSE 2002) and found that high intensity exercise was more effective than low intensity exercise."
In actuality, participants were allowed to self‐select intensity and the two factors that were manipulated were frequency of exercise and total energy expenditure. It was the total energy expenditure that seemed to have a great effect on reduction of symptoms when the low dose was compared with the higher dose. Second, the study is not cited correctly throughout the article and finally I am not sure why the main results paper was not included in this review because it was published in 2005. What was included was our baseline design paper that had no results. I would like to see this error corrected in the review.
Andrea L. Dunn, PhD
Reply
Reply of Dr Gillian Mead, 10 November 2009
The 2005 paper is now cited as well as the 2002 paper.
The purpose of our review was to determine the effectiveness of exercise for depression. Thus we included trials which compared exercise with 'no treatment' and trials which compared exercise to other treatments for depression e.g. CBT. Our conclusions were that 'It is reasonable to recommend exercise to people with depressive symptoms and to those who fulfil diagnostic criteria for depression....'
I agree... that it would be misleading if people with depression and researchers were given the impression that exercise had to be intense to bring about benefits. Based on our subgroup analyses, we have stated that 'we cannot give people accurate information about how effective exercise might be, nor can recommendations be made about the relative benefits of aerobic exercise, resistance exercise or mixed exercise, whether group or individual exercises are better, nor about the optimum duration of exercise'. We then go on to say that further research is required.
[Concerning intensity within the DOSE study] ‐ text has been added for clarification in both the 'Description of studies' and the 'Discussion'.
Contributors
Andrea L. Dunn, PhD Senior Research Scientist Klein Buendel, Inc. 1667 Cole Boulevard, Suite 225 Golden, CO 80401 (303)‐565‐4321 (main line) (303) 565‐4320 (fax) www.kleinbuendel.com
What's new
| Date | Event | Description |
|---|---|---|
| 2 May 2013 | New citation required but conclusions have not changed | New studies incorporated |
| 2 May 2013 | New search has been performed | Review updated |
History
Protocol first published: Issue 3, 2003 Review first published: Issue 4, 2008
| Date | Event | Description |
|---|---|---|
| 12 November 2009 | Feedback has been incorporated | Feedback received from a trialist received 3 November 2009 concerning the DOSE 2002 study was addressed on 10 November 2009 |
| 13 May 2009 | New citation required but conclusions have not changed | Incorrect 'date assessed as up to date' changed from February 2000 to March 2007 (date of last electronic searches). Abstract corrected to reflect true history of searches |
| 13 August 2008 | New search has been performed | This is an updated version of a previous review published in the BMJ in 2001 and includes several new trials |
| 30 July 2008 | Amended | Converted to new review format |
| 21 February 2000 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
An initial review of the effects of exercise in the treatment of depression, in which Professor Debbie Lawlor was the principal investigator, began as part of a training course at the NHS Centre for Reviews and Dissemination, University of York. Dr Stephen Hopker, consultant psychiatrist at Bradford Community Trust, was an investigator in the earlier review and Mr Alan Lui, audit nurse Airedale General Hospital, helped with the protocol development and retrieval of articles. Dr Domenico Scala, Senior House Officer in psychiatry and Lynfield Mount Hospital, Bradford, translated one Italian paper that was excluded from the review. We are grateful to Mr Paul Campbell for contributing to the previous update by providing expertise on depression. Dr Maria Corretge, Specialty Registrar in Geriatric Medicine at St. John's Hospital, West Lothian, translated two papers in Spanish and Portuguese which were subsequently excluded from the 2010 updated review.
We are very grateful to Ms Maureen Harding, Geriatric Medicine, University of Edinburgh, who retrieved articles and provided administrative support. We are also grateful to the Cochrane Depression, Anxiety and Neurosis Group editorial base team for assistance with searches and for advice on the review.
We are also grateful to several authors for providing more information or data for their studies (Elizabeth Wise ‐ Hoffman 2010; Jorge Mota Pereira ‐ Mota‐Pereira 2011; Jane Sims ‐ Sims 2009; James Blumenthal ‐ Blumenthal 2012a; Rebecca Gary ‐ Gary 2010).
We are grateful for the support of an NIHR incentive award to help support the update of this review.
CRG Funding Acknowledgement: The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Depression, Anxiety and Neurosis Group.
Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Appendices
Appendix 1. CCDAN searches all years to 1 March 2013
The Cochrane Depression, Anxiety and Neurosis Review Group's Specialised Register (CCDANCTR)
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintain two clinical trials registers at their editorial base in Bristol, UK: a references register and a studies based register. The CCDANCTR‐References Register contains over 31,500 reports of trials in depression, anxiety and neurosis. Approximately 65% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual. Please contact the CCDAN Trials Search Coordinator for further details. Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950‐), EMBASE (1974‐) and PsycINFO (1967‐); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and review specific searches of additional databases. Reports of trials are also sourced from international trials registers c/o the World Health Organization's trials portal (ICTRP), drug companies, the handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCDAN's generic search strategies (used to identify RCTs) can be found on the Group's website.
The CCDANCTR was searched all years to 31 March 2013.
The CCDANCTR‐Studies Register was searched using the following terms: Diagnosis =Depressi* or Dysthymi* and Intervention = Exercise
The CCDANCTR‐References Register was searched using a more sensitive set of terms to identify additional untagged/uncoded references: Title/Abstract/Keywords = (depressi* or dysthymi*) AND Free‐text = (sport* or exercis* or aerobic* or running or jogging or walk* or hiking or swim* or aquatic* or cycling or bicycl* or ((physical or strength*) and (activit* or educat* or fitness or train*)) or “physical medicine” or ((resistance or weight*) and (train* or lift*)))
Additional searches were conducted on MEDLINE, EMBASE, PsycINFO and CENTRAL (2007 to 2010) by CCDAN’s Trials Search Co‐ordinator (TSC) when the CCDANCTR was out of date due to relocation of the Group’s editorial base and a changeover of staff .
MEDLINE
OVID MEDLINE (2007 to 2010) was searched using the following terms: 1. exp Exercise/ 2. exp Exercise Therapy/ 3. exp "Physical Education and Training"/ 4. Physical Fitness/ 5. Physical Exertion/ 6. exp Walking/ 7. Running/ or Jogging/ 8. Swimming/ 9. (cycling or bicycling).tw. 10. (exercise$ or exercising).tw. 11. (physical adj3 (education or training)).tw. 12. or/1‐11 13. Depression/ 14. exp Depressive Disorder/ 15. or/13‐14 16. randomized controlled trial.pt. 17. controlled clinical trial.pt. 18. randomly.ab. 19. trial.ab. 20. groups.ab. 21. (control$ adj3 (trial$ or study or studies)).tw. 22. randomi#ed.ab. 23. placebo$.ab. 24. or/16‐23 25. 12 and 15 and 24 26. (2007$ or 2008$ or 2009$ or 2010$).ed,yr. 27. 25 and 26
EMBASE
OVID EMBASE (2007 to 2010) was searched using the following terms: 1. exp exercise/ 2. exp physical activity/ 3. exp sport/ 4. (exercise$ or exercising).tw. 5. or/1‐4 6. exp depression/ 7. randomized controlled trial/ 8. controlled clinical trial/ 9. major clinical study/ 10. randomization/ 11. placebo/ 12. randomi#ed.ti,ab. 13. placebo$.tw. 14. trial.ti,ab. 15. randomly.ab. 16. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 17. (control$ adj3 (trial$ or study or studies$)).tw. 18. or/6‐16 19. (2007$ or 2008$ or 2009$ or 2010$).em,yr. 20. 5 and 6 and 18 and 19
PsycINFO
OVID PsycINFO (2007 to 2010) was searched using the following terms: 1. exp major depression/ 2. atypical depression/ 3. seasonal affective disorder/ 4. (depress$ adj3 (patient$ or symptom$ or disorder$)).ti,ab. 5. or/1‐4 6. exp physical activity/ 7. exp sports/ 8. running/ or walking/ 9. (cycling or bicycling).tw. 10. (exercise$ or exercising).tw. 11. (physical adj3 (education or training)).tw. 12. or/6‐11 13. treatment effectiveness evaluation/ 14. clinical trials/ 15. mental health program evaluation/ 16. placebo/ 17. placebo$.tw. 18. randomly.ab. 19. randomi#ed.tw. 20. trial$.tw. 21. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).tw. 22. (control* adj3 (trial* or study or studies)).tw. 23. "2000".md. 24. or/13‐23 25. 5 and 12 and 24 26. (2007$ or 2008$ or 2009$ or 2010$).an,up,yr. 27. 25 and 26
Cochrane Central Register of Controlled Trials (CENTRAL)
CENTRAL was searched using the following terms: #1 MeSH descriptor Exercise explode all trees #2 MeSH descriptor Exercise Therapy explode all trees #3 MeSH descriptor Physical Education and Training explode all trees #4 MeSH descriptor Physical Fitness, this term only #5 MeSH descriptor Physical Exertion, this term only #6 MeSH descriptor Walking explode all trees #7 MeSH descriptor Running explode all trees #8 MeSH descriptor Swimming, this term only #9 (cycling or bicycling) #10 (exercise* or exercising) #11 (physical NEAR/5 (education or training)) #12 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11) #13 MeSH descriptor Depressive Disorder explode all trees #14 MeSH descriptor Depression, this term only #15 (#13 OR #14) #16 (#12 AND #15) #17 (#16), from 2007 to 2010 #18 SR‐DEPRESSN #19 HS‐DEPRESSN #20 (#17 AND NOT ( #18 OR #19 ))
Appendix 2. Previous search to 2007
The authors searched Ovid MEDLINE and EMBASE, PsycINFO and Sports Discus on the Silver Platter platform, the Cochrane Controlled Trials Register and the Cochrane Database of Systematic Reviews. Details of the search strategy used in MEDLINE are provided below (Lawlor 2001); this search was modified as appropriate for other databases. Appropriate filters were applied to identify randomised controlled trials.
MEDLINE search strategy: 1. exp EXERCISE/ 2. exp Exercise Therapy/ 3. exp Exertion/ 4. exp Physical Fitness/ 5. exp Walking/ 6. exp Running/ 7. exp Swimming/ 8. exp Jogging/ 9. exp "Physical Education and Training"/ 10. exercise$ near aerobic$.tw. 11. train$ near aerobic$.tw. 12. exercise$ near strength$.tw. 13. train$ near strength$.tw. 14. bicycling$.tw. 15. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 16. exp DEPRESSION/ 17. exp Depressive Disorder/ 18. exp Dysthymic Disorder/ 19. 16 or 17 or 18 20 15 and 19
Data and analyses
Comparison 1. Exercise versus 'control'.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Reduction in depression symptoms post‐treatment | 35 | 1353 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐0.81, ‐0.42] |
| 2 Reduction in depression symptoms follow‐up | 8 | 377 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.63, ‐0.03] |
| 3 Completed intervention or control | 29 | 1363 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.97, 1.04] |
| 4 Quality of life | 4 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Mental | 2 | 59 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.24 [‐0.76, 0.29] |
| 4.2 Psychological | 2 | 56 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.29, 0.86] |
| 4.3 Social | 2 | 56 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.35, 0.74] |
| 4.4 Environment | 2 | 56 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.62 [0.06, 1.18] |
| 4.5 Physical | 4 | 115 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.45 [0.06, 0.83] |
Comparison 2. Exercise versus psychological therapies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Reduction in depression symptoms post‐treatment | 7 | 189 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.32, 0.26] |
| 2 Completed exercise or pyschological therapies | 4 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.95, 1.24] |
| 3 Quality of life | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Physical | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Mental | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. Exercise versus bright light therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Reduction in depression symptoms post‐treatment | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐6.4 [‐10.20, ‐2.60] |
Comparison 4. Exercise versus pharmacological treatments.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Reduction in depression symptoms post‐treatment | 4 | 300 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.34, 0.12] |
| 2 Completed exercise or antidepressants | 3 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.86, 1.12] |
| 3 Quality of Life | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Mental | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | ‐11.90 [‐24.04, 0.24] |
| 3.2 Physical | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [‐0.67, 3.27] |
Comparison 5. Reduction in depression symptoms post‐treatment: Subgroup analyses.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Exercise vs control subgroup analysis: type of exercise | 35 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Aerobic exercise | 28 | 1080 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.77, ‐0.34] |
| 1.2 Mixed exercise | 3 | 128 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.85 [‐1.85, 0.15] |
| 1.3 Resistance exercise | 4 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.03 [‐1.52, ‐0.53] |
| 2 Exercise vs control subroup analysis: intensity | 35 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 light/moderate | 3 | 76 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐1.32, ‐0.34] |
| 2.2 moderate | 12 | 343 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.01, ‐0.28] |
| 2.3 hard | 11 | 595 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.93, ‐0.20] |
| 2.4 vigorous | 5 | 230 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐1.30, ‐0.24] |
| 2.5 Moderate/hard | 2 | 66 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.13, ‐0.13] |
| 2.6 Moderate/vigorous | 2 | 42 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐1.61, 0.85] |
| 3 Exercise vs control subroup analysis: number of sessions | 35 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 0 ‐ 12 sessions | 5 | 195 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐1.26, 0.43] |
| 3.2 13 ‐ 24 sessions | 9 | 296 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.09, ‐0.31] |
| 3.3 25 ‐ 36 sessions | 8 | 264 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.30, ‐0.29] |
| 3.4 37+ sessions | 10 | 524 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.69, ‐0.23] |
| 3.5 unclear | 3 | 73 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐1.39, ‐0.40] |
| 4 Exercise vs control subroup analysis: diagnosis of depression | 35 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 clinical diagnosis of depression | 23 | 967 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐0.81, ‐0.32] |
| 4.2 depression categorised according to cut points on a scale | 11 | 367 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐0.95, ‐0.39] |
| 4.3 unclear | 1 | 18 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.00 [‐3.19, ‐0.82] |
| 5 Exercise vs control subgroup analysis: type of control | 35 | 1353 | Mean Difference (IV, Fixed, 95% CI) | ‐1.57 [‐1.97, ‐1.16] |
| 5.1 placebo | 2 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐2.66 [‐4.58, ‐0.75] |
| 5.2 No treatment, waiting list, usual care, self monitoring | 17 | 563 | Mean Difference (IV, Fixed, 95% CI) | ‐4.75 [‐5.72, ‐3.78] |
| 5.3 exercise plus treatment vs treatment | 6 | 225 | Mean Difference (IV, Fixed, 95% CI) | ‐1.22 [‐2.21, ‐0.23] |
| 5.4 stretching, meditation or relaxation | 6 | 219 | Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.65, 0.48] |
| 5.5 occupational intervention, health education, casual conversation | 4 | 190 | Mean Difference (IV, Fixed, 95% CI) | ‐3.67 [‐4.94, ‐2.41] |
Comparison 6. Exercise versus control: sensitivity analyses.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Blumenthal 1999.
| Methods | RCT, parallel groups | |
| Participants | Community volunteers recruited via media. Eligible if had DSM‐IV major depressive disorder Mean age 70 (range 61 to 88) 63% women N = 156 | |
| Interventions | 1. Group walking or jogging 3 times per week (n = 53 randomised)
2. Sertraline (SSRI) at standard dose (n = 48 randomised)
3. Combined walking or jogging and sertraline (n = 55 randomised) Duration of interventions: 16 weeks Exercise intensity was 70% to 85% of target heart rate |
|
| Outcomes | 1. Clinical diagnosis of depression using DSM‐IV 2. Hamilton Rating Scale for Depression 3. Beck Depression Inventory | |
| Notes | Analysis intention‐to‐treat, using last observation carried forward for missing data. Review authors used group 2 and group 3 in the meta‐analysis Outcome assessor blind | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of randomisation is not described in the paper |
| Allocation concealment (selection bias) | Low risk | This was categorised as inadequate in the first version of this review, published in the BMJ, after Debbie Lawlor had contacted authors to obtain data on allocation concealment. Further information from the author has enabled us to change this to low risk |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants were aware of the treatment group to which they were allocated |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the interventions were aware of treatment group. It is not clear whether this would have introduced bias. |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | Used HAM‐D as an outcome measure. This is rated by clinicians. Every effort was made to ensure that clinical raters were unaware of participants' treatments groups after allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Although not all participants completed the interventions, the authors used last observation carried forward to impute missing values |
| Selective reporting (reporting bias) | Low risk | From the study report, it appears that all the prespecified outcome measures have been reported, |
| Other bias | Unclear risk | Unclear |
Blumenthal 2007.
| Methods | RCT | |
| Participants | People with major depression recruited through television, radio and newspaper. Mean age 52 (SD 8), 76% women, N = 202 | |
| Interventions | 1. Home‐based aerobic exercise (same 'exercise prescription' as the supervised aerobic group, but performed it on their own (n = 53) 2. Supervised group aerobic exercise (walking and jogging) (n = 51) 3. Sertraline (n = 49) 4. Placebo (n = 49) Intervention 16 weeks | |
| Outcomes | Primary endpoint was remission (no MDD) and a HAM score of < 8, and also a continuous severity score on the HAM‐D | |
| Notes | Analysis intention‐to‐treat using last observation carried forward Blinded outcome assessment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Conditional randomisation, stratified by age, gender and depression severity |
| Allocation concealment (selection bias) | Low risk | Central allocation by a computer |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants were aware of whether they received exercise or not. It is unclear whether this introduced bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those personnel delivering exercise were aware of group allocation. It is unclear whether this introduced bias |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | The outcome assessors were unaware of treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Imputed missing outcome assessment results by last observation carried forward |
| Selective reporting (reporting bias) | Low risk | From the study report, it appears that all the prespecified outcome measures have been reported. Authors report protocol on clinicaltrials.gov |
| Other bias | Unclear risk | Unclear |
Blumenthal 2012a.
| Methods | RCT | |
| Participants | 35 years or older with documented coronary artery disease and depressive symptoms (n=101) | |
| Interventions | 1. Exercise (group walking, running or jogging on treadmill (n = 37; 65% men) 2. Sertraline (n = 40; 63% men) 3. Placebo (n = 24; 83% men) |
|
| Outcomes | Depression as diagnosed by DSM‐IV and severity of depression as rated on HAM‐D; heart disease biomarkers | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based randomisation |
| Allocation concealment (selection bias) | Low risk | Allocation through distribution of sealed envelopes |
| Blinding (performance bias and detection bias) participants | Unclear risk | Not possible to blind participants receiving exercise; unclear effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | No detail given |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | Telephone surveys (HAMD) by psychologists blinded to arm of trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 95 out of 101 completed protocol and outcome assessment |
| Selective reporting (reporting bias) | Low risk | Prespecified outcomes reported in results. There is a study protocol |
| Other bias | Unclear risk | Unclear |
Bonnet 2005.
| Methods | RCT | |
| Participants | University counselling service Mean age 23.3 years 82% women N = 11 | |
| Interventions | 1. CBT plus exercise (n = 5)
2. CBT alone (n = 6) Exercise was walking on a treadmill for 20 minutes, twice a week for 6 weeks Cognitive therapy: met counsellors once a week for 9 weeks |
|
| Outcomes | 1. DSM‐IV MDD, dysthymia or depressive disorder 2. Above cut‐off depression on BDI and CES‐D | |
| Notes | Self report Randomisation method not stated 7/11 randomised participants completed the interventions Data provided for each participant. Mean and SD calculated by us carrying forward baseline data for those who dropped out | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Method of randomisation not described |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants were not blind to treatment allocation, but it is unclear whether this introduced bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blinded; the effect of this on bias is unclear |
| Blinding (performance bias and detection bias) outcome assessors | High risk | The primary outcome was the BDI, which is a self report measure |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4/11 dropped out (2/5 in the exercise and CBT; 2/6 in the CBT only group) |
| Selective reporting (reporting bias) | Unclear risk | On the basis of the report, all the prespecified outcomes have been reported. No protocol |
| Other bias | Unclear risk | Unclear |
Brenes 2007.
| Methods | RCT | |
| Participants | Community‐dwelling and nursing home people over 65 with mild depression, recruited through newsletters, newspaper advertisements, distributing flyers at local nursing homes and public presentations Mean age 73.5 (SD 7.8) in exercise, 76.4 (6.4) in medication and 73.9 (5.8) in control group 62% women N = 37 |
|
| Interventions | 1. Faculty‐based group aerobic and resistance training for 60 minutes 3 days a week for 16 weeks (n = 14) 2. Once daily sertraline titrated to response (evaluated at weeks 2, 6, 10 and 14) (n = 11) 3. Control group: contacted at weeks 2, 6, 10, 14 to discuss general health status (n = 12) |
|
| Outcomes | HAM‐D | |
| Notes | Method of randomisation not stated, states intention‐to‐treat analysis, however data unclear on how many participants dropped out of each group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random allocation list |
| Allocation concealment (selection bias) | Unclear risk | Method not described in the paper |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants were not blinded to treatment allocation |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind, but it is not clear what influence this had on bias |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | Used HDRS as an outcome, assessors were blind to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The authors of the trial state that it is intention‐to‐treat, but no data are provided on the number who dropped out of the trial |
| Selective reporting (reporting bias) | Unclear risk | It appears that all the prespecified outcomes are reported, but no protocol |
| Other bias | Unclear risk | unclear |
Chu 2008.
| Methods | RCT | |
| Participants | Volunteers aged 18 to 45 recruited via flyers and word of mouth from University and local physician referral. Depression severity mild to moderate, if severe required written permission from physician. Mean age 26.4 (18 to 43). 100% women. |
|
| Interventions | For 10 weeks: 1. Up to 5 high‐intensity aerobic exercise sessions per week (1 supervised) to expend 1000 Kcal per week (n = 15) 2. Up to 5 low‐intensity aerobic exercise sessions per week (1 supervised) to expend 1000 Kcal per week (n = 11) 3. Met with investigator once per week for 30 minutes of group stretching exercises (n = 12) |
|
| Outcomes | Beck Depression Inventory‐II | |
| Notes | Analysis not intention‐to‐treat BDI‐II self‐rated depression score |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Unclear; not described |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind to treatment allocation |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind |
| Blinding (performance bias and detection bias) outcome assessors | High risk | BDI‐II self report was used as the primary outcome |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 16/54 dropped out (3/18 in high dose, 7/18 in low dose and 6/18 in control) |
| Selective reporting (reporting bias) | Unclear risk | It appears that all prespecified outcomes are reported, but no protocol |
| Other bias | Unclear risk | Unclear |
Doyne 1987.
| Methods | RCT | |
| Participants | Community volunteers recruited via media Mean age 28.5 (SD 4.36) 100% women N = 40. The number randomised into each group not stated. | |
| Interventions | 1. Supervised running or walking 4 times a week for 8 weeks 2. Supervised strength training 4 times a week 3. Waiting list control | |
| Outcomes | 1. Beck Depression Inventory 2. Lubin's Depression Adjective List 3. Hamilton Rating Scale for Depression | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Report states random assignment after matching participants on baseline BDI scores of intervals of < 19, 20 ‐ 29 and > 30 |
| Allocation concealment (selection bias) | High risk | Inadequate (as assessed by Lawlor and Hopker in BMJ review in 2001) |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind to treatment allocation, but unclear risk of bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind |
| Blinding (performance bias and detection bias) outcome assessors | High risk | BDI was the primary outcome |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of the 57 women who met criteria for inclusion, 40 completed treatment, and 32 completed follow‐up. Drop‐out rates were 40% in 'track', 29% in 'universal' and 13% in waiting list control |
| Selective reporting (reporting bias) | Unclear risk | It appears that all the prespecified outcome measures are reported, but no protocol |
| Other bias | Unclear risk | Unclear |
Dunn 2005.
| Methods | RCT | |
| Participants | Community volunteers recruited via media. Men or women aged 20 to 45 with mild to moderate depression Mean age 35.9 75% women N = 80 | |
| Interventions | 4 different aerobic exercise programmes, that varied in total energy expenditure (7.0 kcal/kg/week or 17.5 kcal/kg/week) and frequency (3 days per week or 5 days per week). The 17.5 kcal/kg/week is consistent with public health recommendations for physical activity and is termed 'public health dose'.
1. Public health dose 3/week (n = 17)
2. Public health dose 5/week (n = 16)
3. Low dose 3/week.(n = 16)
4. Low dose 5/week (n = 18)
5. Control, (flexibility exercise) 3 sessions per week (n = 13) Exercise was on a treadmill or stationary bike, individually and monitored by laboratory staff. Duration 12 weeks. |
|
| Outcomes | Change in HRSD from baseline to 12 weeks. | |
| Notes | Intention‐to‐treat (though data from the last available exercise session rather than data collected at 12 weeks were used in the analysis) Outcome assessors blind | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation not stated |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind to treatment allocation, but unclear effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those supervising delivery of the intervention were not blind, but it is unclear what effect this had on bias |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | Trained research assistants applied the HRSD blind to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analyses |
| Selective reporting (reporting bias) | Low risk | There is a published protocol (Dunn 2002) |
| Other bias | Unclear risk | Unclear |
Epstein 1986.
| Methods | RCT | |
| Participants | Community volunteers recruited via media Mean age 39.4 (range 24 to 60) 92% women | |
| Interventions | 1. Group walking or jogging for 30 minutes 3 to 5 times a week for 8 weeks (n = 7) 2. Cognitive therapy 1 session of 1.5 hours per week (n = 9) 3. Waiting list control (n = 10) | |
| Outcomes | 1. Beck Depression Inventory 2. Zung Self Rating Depression Scale | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information not available |
| Allocation concealment (selection bias) | High risk | Assessed by Lawlor and Hopker for BMJ review |
| Blinding (performance bias and detection bias) participants | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Information not available |
| Blinding (performance bias and detection bias) outcome assessors | High risk | BDI: self report |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information not available |
| Selective reporting (reporting bias) | Unclear risk | From the information available, it appears that all prespecified outcomes were reported |
| Other bias | Unclear risk | Unclear |
Fetsch 1979.
| Methods | RCT. n = 21 | |
| Participants | Depressed people (reactive depression) referred from a University counselling service and recruited via advertisements | |
| Interventions | 1. Running 4 sessions over 4 weeks (n = 10). Age range 18 ‐ 51 2. Stroking therapy (a type of 'talking' therapy), 4 sessions over 4 weeks (n = 11) (age range 20 ‐ 35) | |
| Outcomes | Beck Depression inventory | |
| Notes | Outcome assessment not blind (self report) Analysis not intention‐to‐treat (only 16/21 randomised participants completed trial and were included in the analysis) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Method not described |
| Blinding (performance bias and detection bias) participants | Unclear risk | Not blind to treatment allocation, but unclear effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Not blind, but unclear risk on bias |
| Blinding (performance bias and detection bias) outcome assessors | High risk | BDI; self report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only included the scores for the 16 people who completed 2 or more sessions |
| Selective reporting (reporting bias) | Unclear risk | It appears from the information available that all prespecified outcomes were reported, but no protocol |
| Other bias | Unclear risk | Unclear |
Foley 2008.
| Methods | RCT (parallel group) | |
| Participants | Recruited from media advertisements, pamphlet and poster displays and psychiatric referrals with major depressive episode. Age range 18 ‐ 55, mean age and gender data not stated N = 23 |
|
| Interventions | 1. Moderate‐intensity aerobic exercise. Each session lasted 30 ‐ 40 minutes (n = 10) 2. Mild‐intensity stretching (n = 13) 12‐week programme of 3 supervised sessions per week |
|
| Outcomes | Beck Depression Inventory Montgomery‐Asberg Depression Rating scale |
|
| Notes | Intention‐to‐treat analysis Small sample size with insufficient power to detect small differences |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants were not blind to treatment allocation, but it is unclear what effect this has had on bias. |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention were not blind, but it is unclear what effect this had on bias |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report BDI |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 10/23 dropped out (2/10 in exercise arm and 8/13 in stretching) |
| Selective reporting (reporting bias) | Unclear risk | From the study report, it appears that all prespecified outcome measures have been reported; no protocol |
| Other bias | Unclear risk | Unclear |
Fremont 1987.
| Methods | RCT | |
| Participants | Community volunteers recruited via media Data on age and gender not available N = 61 | |
| Interventions | 1. Group running (3 times a week, for 10 weeks, with a running coach in small groups of 6 ‐ 8 subjects) (n = 15)
2. Cognitive therapy (10 individual 1 hour sessions with a therapist) (n = 16)
3. Combined running and cognitive therapy (n = 18) 10 weeks |
|
| Outcomes | Beck Depression Inventory | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information available |
| Allocation concealment (selection bias) | High risk | Inadequate (as assessed by Lawlor and Hopker in the 2001 BMJ review) |
| Blinding (performance bias and detection bias) participants | Unclear risk | Not stated |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Not stated |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report BDI |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Categorised as not intention‐to‐treat for the BMJ review (Lawlor and Hopkins). Data on drop‐outs not available to lead author |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available for scrutiny. From the study report, it appears that all prespecified outcome measures have been reported |
| Other bias | Unclear risk | Unclear |
Gary 2010.
| Methods | RCT | |
| Participants | Depressed people with heart failure (NYHA Class II to III) 42% men Age 30 ‐ 70 |
|
| Interventions | 1. Home exercise programme: 12 weekly face‐to‐face home visits to monitor walking and to tailor the exercise prescription. Participants were advised to walk for 3 days per week for 12 weeks, and to increase duration to a maximum of 1 hour for 3 days per week at moderate intensity (n = 20). 2. Home exercise programme plus CBT (n = 18) 3. CBT alone, based on Beck's CBT model. Each session lasted 1 hour. Total number of sessions not stated, but we assume this was 12 because in the combined group they were delivered at the same time as the home exercise programme visits (n = 18) 4. Usual care (n = 17) |
|
| Outcomes | HAM‐D, 6‐minute walk | |
| Notes | Small sample size | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Reported as randomised, but no details given |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants were not blinded to treatment allocation; unclear effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering treatment were not blinded; unclear effect on bias |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | "Data collectors were blind to group assessment" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 68/74 provided outcome data post‐intervention. Classified as high risk, as more than 5% did not provide outcome data |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported. |
| Other bias | Low risk | No other source of bias identified |
Greist 1979.
| Methods | RCT | |
| Participants | Community volunteers Age range 18 ‐ 30 53.4% women N = 28 | |
| Interventions | 1. Supervised running (n = 10). running leader met individually with his participants 3 ‐ 4 times per week for 1 hour, then in the 5th week, only 2 sessions were scheduled with the leader, and in the 7th and 8th weeks, only 1 was scheduled. 2. Time‐limited psychotherapy (n = 6) 3. Time‐unlimited psychotherapy (n = 12) | |
| Outcomes | Symptom checklist score | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information in report |
| Allocation concealment (selection bias) | High risk | Categorised in BMJ review (Lawlor and Hopker) as inadequate |
| Blinding (performance bias and detection bias) participants | Unclear risk | Not blinded to treatment allocation |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering exercise not blinded, effect on bias unclear |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report symptom checklist score |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6/28 dropped out (2/10 in the running group and 4/18 in the psychological groups) |
| Selective reporting (reporting bias) | High risk | Outcome measures were not prespecified. There was no methods section in the paper; after an introduction, the entry criteria were stated and the interventions were described. The first time the outcome measures were described was in the results section. |
| Other bias | High risk | The authors conclude the paper by saying that "our bias (and we purposely label it as bias that requires additional evaluation) is that running may prove to have antidepressant properties for many individuals with moderate depression". It is possible that this author bias was present before the trial was completed, and so may have influenced results. |
Hemat‐Far 2012.
| Methods | RCT | |
| Participants | University students aged 18 ‐ 25 with depression 100% women |
|
| Interventions | 1. 40 ‐ 60 minutes of running, 3 times a week, supervised. (n = 10) 2. Control group with no active intervention (n = 10) |
|
| Outcomes | Beck Depression Inventory score | |
| Notes | Small sample size (10 participants in each arm); specific population under study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Clinician judgement used at recruitment. After reviewing questionnaires psychiatrists "selected" 20 women |
| Allocation concealment (selection bias) | Unclear risk | No information given |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blinded to intervention; unclear effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | No information given |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report BDI |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No discussion on attrition rate |
| Selective reporting (reporting bias) | Low risk | BDI specified at outset and completed in results |
| Other bias | High risk | The control group were told not to do so much exercise. |
Hess‐Homeier 1981.
| Methods | RCT | |
| Participants | Community volunteers recruited via media Data on age and gender distribution not available N = 17 | |
| Interventions | 1. Running or walking with the instructor for 30 minutes 4 times a week for 8 weeks (n = 5) 2. Cognitive therapy: 1 session of 1 hour and 2 of ½ hour per week (n = 6) 3. Waiting list control (n = 6) | |
| Outcomes | Beck Depression Inventory | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated that "random assignment" was performed |
| Allocation concealment (selection bias) | High risk | Categorised as inadequate in BMJ review (Lawlor and Hopker) |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blinded to treatment allocation |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report BDI |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Previously categorised by Lawlor and Hopker as not intention‐to‐treat, but data on drop‐outs are not reported |
| Selective reporting (reporting bias) | Unclear risk | The BDI was listed as the first outcome measure and data on BDI were reported. The authors also mentioned the Zung Self rating Depression Scale, but data were not reported in the abstract. No protocol was available |
| Other bias | Unclear risk | Unclear |
Hoffman 2010.
| Methods | RCT | |
| Participants | People with a history of traumatic brain injury occurring between 6 months and 5 years prior to trial with at least mild depression (n = 80) | |
| Interventions | 1. Aerobic exercise of participant's choosing. 60 minutes of gym‐based supervised exercise per week and 4 x 30‐minute home exercise sessions per week (n = 40; 38% men) 2. No intervention in control group (n = 40; 50% men) |
|
| Outcomes | Beck Depression Inventory Score | |
| Notes | The control group were informed they could participate in exercise programme post‐trial intervention period. Authors report that both intervention and control groups showed a substantial increase in exercise. SDs received from author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participation open to anyone who met inclusion criteria. Random distribution of sealed envelopes. |
| Allocation concealment (selection bias) | Low risk | Use of sealed envelopes |
| Blinding (performance bias and detection bias) participants | Unclear risk | All participants informed of nature of the study and both groups increased total amount of exercise over study period |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | No detail provided |
| Blinding (performance bias and detection bias) outcome assessors | High risk | BDI self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evidence of missing data |
| Selective reporting (reporting bias) | Low risk | All findings reported |
| Other bias | Unclear risk | Unclear |
Klein 1985.
| Methods | RCT (parallel group) | |
| Participants | Community volunteers recruited via media Mean age 30.1 (SD 6.72) 72% women N = 74 | |
| Interventions | 1. Supervised running twice a week for 12 weeks (n = 27) 2. Group cognitive therapy for 2 hours once a week (n = 24) 3. Control group: meditation for 1 hour twice weekly (n = 23) | |
| Outcomes | 1. Symptom checklist 2. Target symptoms 3. Structural Analysis of Social Behaviour 4. Social Adjustment Self reported Questionnaire 5. Cornell Medical Index 6. Role Rating Questionnaire 7. Hamilton Rating Scale 8. Global Assessment Scale | |
| Notes | Main outcome assessment not blind. Hamilton Rating Scale administered by interviewer blind to allocation. Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated |
| Allocation concealment (selection bias) | High risk | Inadequate. Categorised by Lawlor and Hopker for BMJ review |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind but unclear whether this had an effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report for main outcome |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of the 74 randomised, 32 dropped out or never started treatment (12/27 in the running group; 12/23 in the meditation group and 8/24 in the group therapy group) |
| Selective reporting (reporting bias) | Unclear risk | It appears that all outcomes specified in methods are reported. No protocol |
| Other bias | Unclear risk | Unclear |
Knubben 2007.
| Methods | RCT (parallel group) | |
| Participants | Inpatients with major depression Mean age 49 55% women N = 38 | |
| Interventions | 1. Walking training on a treadmill for 10 days (n = 10) 2. Placebo (low‐intensity stretching and relaxation) light stretching exercises for the calves, thighs, back, shoulders and pectoral muscles, as well as relaxation exercises, daily for 30 minutes (n = 18) | |
| Outcomes | 1. Bech‐Rafaelsen Scale (BRMS) 2. Center for Epidemiologic Studies Depression Scale (CES‐D) | |
| Notes | Authors state intention‐to‐treat, but of the 39 recruited only 38 were used in the analysis. Outcome assessor for BRMS blinded to treatment allocation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block list |
| Allocation concealment (selection bias) | Low risk | Central randomisation |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants aware of treatment allocation, unclear effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention aware of allocation, unclear effect on bias |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | A single psychologist (blinded to treatment allocation) assessed outcome using the BRMS |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The report states 39 were randomised, but the outcome data relate to only 38. Three participants dropped out. Missing data were imputed, but authors have not accounted for the 1 participant who seems to have been randomised but was not reported in the tables of results. |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes seem to have been reported, but no protocol |
| Other bias | Unclear risk | Unclear |
Krogh 2009.
| Methods | RCT (parallel group) | |
| Participants | Referred from general practitioners, private psychiatrists, psychologists and psychiatric wards institutions. Included if met criteria for major depression Mean age 38.9 73.9% women N = 165 |
|
| Interventions | 1. Strength circuit training (n = 55) 2. Aerobic (machine‐based) training (n = 55) 3. Relaxation control (n = 55 Twice‐weekly intervention for 32 sessions delivered over a 4‐month period |
|
| Outcomes | Hamilton Rating Scale for Depression | |
| Notes | Intention‐to‐treat analysis Significant drop‐outs in each group Changed sample size calculation after first 50 participants on basis of observed standard deviation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised restricted randomisation with a block size of 8 |
| Allocation concealment (selection bias) | Low risk | The block size and allocation sequence were unknown to the DEMO trial staff |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, but unclear what influence this had on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Physiotherapists delivering the intervention were not blind. Unclear how this influenced risk of bias |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | The assessor was blind to intervention group. The investigators asked the outcome assessors to guess intervention group. The kappa values for agreement between the right allocation and the guessed allocation were 0.15 and 0.05 for the assessments at 4 and 12 months respectively |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 137/165 were available for follow‐up at the end of the intervention. Eighteen were lost to follow‐up and 10 refused to participate (8/55 in strength group, 7/55 in aerobic group and 13/55 in the relaxation group). The authors used a likelihood‐based mixed‐effect model with an unstructured variance matrix available in SPSS, which is able to handle missing data with higher precision and power than last observation carried forward. The authors reported no significant difference between missing participants and participants included in the analyses at either 4 or 12 months, and concluded that it was reasonable to assume that the missing data were 'missing at random' |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes seem to have been reported. Protocol was published in advance of the trial |
| Other bias | Unclear risk | The authors repeated power calculations part‐way through the trial, and reduced the sample size as the standard deviation was lower than anticipated |
Martinsen 1985.
| Methods | RCT (parallel group) | |
| Participants | Psychiatric hospital inpatients Mean age 40 (range 17 ‐ 60) Data on sex distribution not available N = 49 | |
| Interventions | 1. Aerobic exercise with instructor for 1 hour 3 times a week for 9 weeks at 50 ‐ 70% of maximum aerobic capacity (n = 28 randomised) 2. Control group attended occupational therapy whilst intervention group exercised (n = 21 randomised) | |
| Outcomes | Beck Depression Inventory | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation with respect to age |
| Allocation concealment (selection bias) | Low risk | Categorised by Lawlor and Hopker as low risk |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report BDI |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6 participants dropped out, leaving 43 who completed the study |
| Selective reporting (reporting bias) | Unclear risk | Prespecified outcome measures were reported, but no protocol |
| Other bias | Unclear risk | unclear |
Mather 2002.
| Methods | RCT (parallel group) | |
| Participants | Primary care, psychiatric services, advertisement in paper and radio. N = 86 (59 women and 27 men). Mean age 63.7 (range 53 ‐ 78) in exercise and 66.2 (56 ‐ 91) in control group. | |
| Interventions | 1. Endurance, muscle strengthening and stretching, in a group exercise class, lasting 45 minutes. An instructress ran the class from a podium in the centre of a hall (n = 43). Twice weekly for 10 weeks 2. Health education classes (n = 43), twice weekly for 10 weeks |
|
| Outcomes | 1. Hamilton Rating Scale for Depression 2. Geriatric Depression Scale 3. Clinical Global Impression 4. Patient Global Impression | |
| Notes | Outcome assessor blind Intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number list |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, unclear effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention aware of allocation, unclear effect on bias |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | Primary outcome was HRSD delivered by one of 2 psychiatrists who were blinded to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcome measures reported, but no protocol |
| Other bias | Unclear risk | Unclear |
McCann 1984.
| Methods | RCT (parallel group) | |
| Participants | Undergraduate psychology students with a requirement to participate in a research project No details of age 100% women N = 47 | |
| Interventions | 1. Aerobic exercise: group running, jogging or dancing for 1 hour twice weekly for 10 weeks (n = 16 randomised) 2. Placebo control group ‐ muscle relaxation for 15 ‐ 20 minutes 4 times a week (n = 15 randomised) 3. Waiting list control (n = 16 randomised) | |
| Outcomes | Beck Depression Inventory | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | High risk | Classified as inadequate by Lawlor and Hopker |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention not blind |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report depression scores |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4/47 withdrew (1 from the aerobic exercise, 1 from the placebo condition and 2 from the 'no treatment' condition). 43 remained |
| Selective reporting (reporting bias) | Unclear risk | No prespecified outcomes. Reported depression scores before and after the intervention. No protocol |
| Other bias | Unclear risk | Unclear |
McNeil 1991.
| Methods | RCT | |
| Participants | Community volunteers from religious and community organisations Mean age 72.5 Details of gender distribution not provided N = 30. number randomised into each group not stated, we assume this is 10 in each group) | |
| Interventions | 1. Walking accompanied by investigator for 20 minutes 3 times a week for 6 weeks 2. Social contact control group (visit by investigator for a "chat" avoiding any discussion of depression or health, twice a week) 3. Waiting list control group | |
| Outcomes | Beck Depression Inventory | |
| Notes | Outcome assessment not blind All completed intervention so classified as intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | High risk | Inadequate (as assessed by Lawlor and Hopker for BMJ review) |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, but this on its own does not necessary imply bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Investigator delivering intervention was not blind |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report BDI |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcome measures were reported, but no protocol |
| Other bias | Unclear risk | Note Lawlor and Hopker categorised this study as "not intention‐to‐treat" |
Mota‐Pereira 2011.
| Methods | RCT | |
| Participants | 18 ‐ 60 year‐olds with treatment resistant major depressive disorder selected from outpatient setting (n = 33) | |
| Interventions | 1. Five sessions a week of 30 ‐ 45 minutes moderate intensity walking. Four of these were unsupervised and one was supervised on a hospital gym treadmill (n = 22, 57.9% women) 2. Control group, receiving no exercise (n = 11 : 80% women) |
|
| Outcomes | Hamilton Depression Scale Global Assessment of Functioning Scale Clinical Global Impression Scale. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants were not blinded to intervention, but were not provided with information on how the intervention might benefit them. |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention not blinded to treatment group |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | Investigators carrying out rating tests post‐intervention were blinded to treatment group |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data |
| Selective reporting (reporting bias) | Low risk | Prespecified outcomes all reported |
| Other bias | Low risk | Appears to be free of other bias |
Mutrie 1988.
| Methods | RCT | |
| Participants | Depressed people referred to study by general practitioner (primary care physician) Mean age 42.1 83% women N = 36 | |
| Interventions | 1. Aerobic exercise ‐ conducted on an individual basis and without group contact, 29 minutes 3 times a week for 4 weeks (n = 9) 2. Strength and stretching exercise completed on an individual basis and without group contact, 20 minutes 3 times a week (n = 8) 3. Waiting list control (n = 7) i.e. delayed treatment | |
| Outcomes | 1. Beck Depression Inventory 2. Profile of Mood States | |
| Notes | Outcome assessment not blind All completed intervention so analysis intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No data in report |
| Allocation concealment (selection bias) | High risk | Inadequate (classified by Lawlor and Hopker in BMJ review) |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind |
| Blinding (performance bias and detection bias) outcome assessors | High risk | BDI self report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the intervention |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes are reported, but no protocol |
| Other bias | Unclear risk | Unclear |
Nabkasorn 2005.
| Methods | RCT | |
| Participants | Student nurses with mild to moderate depressive symptoms Aged 18 to 20 All women N = 59 | |
| Interventions | 1. Group jogging 50 minutes a day 5 days a week for 8 weeks (n = 28) 2. Usual care (n = 31) | |
| Outcomes | 1. CES‐D scores (data from means and SD at end of treatment not available so obtained from published graph) | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information in the paper; wrote to authors but no response |
| Allocation concealment (selection bias) | Unclear risk | No information in the paper |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, unclear effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention not blind, unclear effect on bias |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report using CES‐D score, so not blind |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 59 randomised, 7/28 in jogging group not available at follow‐up, 3/31 in control group not available for follow‐up; leaving data from 49 to be analysed |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcome measures seem to have been reported, but no protocol |
| Other bias | Unclear risk | Unclear |
Orth 1979.
| Methods | RCT | |
| Participants | College students with dysphoria or depression Mean age 22 27% women N = 11 | |
| Interventions | 1. Jogging 5 times a week for 30 minutes over 4 weeks (n = 3) 2. Meditation (n = 3) 3. Self‐chosen activity (n = 3) 4. Self monitoring (control) (n = 2) | |
| Outcomes | 1. Depression Adjective Checklist 2. Minnesota Multiphasic Personality Inventory | |
| Notes | Not stated whether intention‐to‐treat though all participants allocated control and running provided data at baseline and post‐intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear, not specified. Too old a study to contact authors |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) participants | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) those delivering intervention | Low risk | Not relevant as activities done on own |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self‐report outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the study, data from all reported |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported, but no protocol |
| Other bias | Unclear risk | Unclear |
Pilu 2007.
| Methods | RCT | |
| Participants | Recruited from clinical activity registries of the University psychiatric unit if diagnosed with major depression. Data on age not stated (inclusion criteria range 40 ‐ 60) 100% women N = 30 |
|
| Interventions | 1. Physiological strengthening exercises plus pharmacological treatment (n=10). The physical activity programme included 2 60‐minute lessons per week, held by skilled an instructor, with ISEF (Physical Education) diploma, Psychology degree and post‐degree diploma in sport Psychopathology (MS). Each session was set in three steps:
Step I: welcome and warming up (about 5 minutes)
Step II: physiological strengthening (about 50 minutes)
Step III: stretching, cooling down, goodbye (about 5 minutes). 2. Pharmacological treatment only (n = 20) Intervention delivered twice per week for 8 months |
|
| Outcomes | Hamilton Rating Scale for Depression | |
| Notes | Not stated if intention‐to‐treat analysis No information given regarding drop‐out rates |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, unclear risk of bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention were not blind, unclear risk of bias |
| Blinding (performance bias and detection bias) outcome assessors | Unclear risk | Unclear. Two different trained psychiatrists rated outcomes, including the HAM‐D, but authors did not report whether these psychiatrists were blind to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All those starting the intervention had outcome data reported |
| Selective reporting (reporting bias) | High risk | The authors stated that a structured diagnostic interview was performed to make a diagnosis of depression at 8 months (follow‐up), but these data were not reported |
| Other bias | Unclear risk | Unclear |
Pinchasov 2000.
| Methods | RCT | |
| Participants | Several groups including one with depression in the absence of seasonal affective disorder. Also 1 group of depressed people fulfilling criteria for seasonal affective disorder mean age 35.2. 100% women N = 63 | |
| Interventions | 1. 54 minutes per day of cycling on stationary bicycle for 1 week
2. Bright light therapy 7 groups, 9 participants in each We are using data from the cycling and bright light therapy |
|
| Outcomes | 1. HDRS score 2. Body weight 3. Oxygen consumption | |
| Notes | Randomisation method unclear Unclear if outcome assessment was blind | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information given |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | The authors did not state how the intervention was delivered |
| Blinding (performance bias and detection bias) outcome assessors | Unclear risk | HDRS, but not stated whether outcome assessor blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 63 participants were recruited, and were included in 7 groups, 9 per group. Data not provided on number still in the trial at the end of the interventions |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information provided to make this judgement |
| Other bias | Unclear risk | Unclear |
Reuter 1984.
| Methods | RCT | |
| Participants | University students presenting to mental health clinic with depression Details of age and gender distribution not provided N = 18 | |
| Interventions | 1. Supervised running for at least 20 minutes 3 times a week for 10 weeks plus counselling 2. Counselling only | |
| Outcomes | Beck Depression Inventory | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information to make this judgement |
| Allocation concealment (selection bias) | High risk | Not used |
| Blinding (performance bias and detection bias) participants | Unclear risk | No information |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind, but the effect on bias is uncertain |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Judged by Lawlor and Hopker in BMJ review as not blind |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Judged by Lawlor and Hopker as not intention‐to‐treat |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information; no protocol |
| Other bias | Unclear risk | Unclear |
Schuch 2011.
| Methods | RCT | |
| Participants | Hospital inpatients being treated for severe depression with conventional therapy (n = 26) Gender not specified |
|
| Interventions | 1. 3 sessions per week of participant‐selected aerobic exercise (n = 15) 2. Control group receiving conventional therapy (i.e. pharmacotherapy/ECT only) (n = 11) |
|
| Outcomes | Depressive symptom rating by psychiatrist using HAM‐D scoring | |
| Notes | Intervention continued 'until discharge' but no further information on length of intervention. No detail on exercise compliance rates. Of 40 originally invited to take part, 14 declined at outset. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation stated but details not given |
| Allocation concealment (selection bias) | Unclear risk | No details on how participants were allocated |
| Blinding (performance bias and detection bias) participants | Unclear risk | No details given on to what extent participants were aware of the theoretical effects of exercise on depression. Participants not blinded to intervention but unclear of the effect of this on bias. |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering exercise not blinded to group; effect of this on bias is unclear |
| Blinding (performance bias and detection bias) outcome assessors | Unclear risk | No detail given on whether those assessing outcome measures were blinded to group |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants remained in trial throughout intervention |
| Selective reporting (reporting bias) | Unclear risk | Reported on all measures outlined at start of trial |
| Other bias | Unclear risk | Unclear |
Setaro 1985.
| Methods | RCT (parallel group) | |
| Participants | Community volunteers recruited via the media Age range 18 ‐ 35 (mean age not stated) 26% women N = 150 | |
| Interventions | 1. Cognitive therapy and aerobic dance classes (n = 30)
2. Aerobic dance classes only (n = 30)
3. Cognitive therapy only using the principles of A Beck (n = 30)
4. Cognitive therapy and non‐aerobic exercise classes (n = 30)
5. Non‐aerobic exercise only (arts and crafts) (n = 30)
6. No intervention (n =30) Duration of interventions was 10 weeks |
|
| Outcomes | Minnesota Multiphasic Personality Inventory | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants blocked by gender; male‐female ratios kept constant |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, unclear risk on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Group intervention, unclear if those delivering the intervention were blind |
| Blinding (performance bias and detection bias) outcome assessors | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 180 randomised, 150 completed trial |
| Selective reporting (reporting bias) | Unclear risk | Reported prespecified outcomes; no protocol |
| Other bias | Unclear risk | Unclear |
Shahidi 2011.
| Methods | RCT | |
| Participants | Older members of a local cultural community Age 60 ‐ 80 100% women all with geriatric depression score greater than 10 (n = 70) |
|
| Interventions | 1. 10 sessions of aerobic group exercise, each 30 minutes in duration, including jogging and stretching (n = 23) 2 "Laughter yoga" ‐ 10 sessions of structured group activity which includes laughing, clapping, chanting and positive discussion (n = 23) 3. Control (n = 24) |
|
| Outcomes | Depression scoring on Geriatric Depression Scale, Life Satisfaction scale | |
| Notes | Overall drop‐out of 10 participants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail given |
| Allocation concealment (selection bias) | Unclear risk | No detail given |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blinded to intervention; unclear what effect this may have on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Not blinded; unclear effect on bias |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Geriatric depression scale; self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 14% attrition rate |
| Selective reporting (reporting bias) | Low risk | All measures listed at outset reported in results |
| Other bias | Unclear risk | Unclear |
Sims 2009.
| Methods | RCT | |
| Participants | Recruited from hospital databases of stroke patients discharged in last year, general practitioners and newspaper articles. Had to be over 6 months post‐stroke and have depression confirmed by a psychiatrist. Mean age 67.13 (range 21 to 93) 40% women N = 45 |
|
| Interventions | 1. Group‐based moderate‐intensity strengthening exercises twice a week for 10 weeks.The PRT programme included 2 high‐intensity sessions/week for 10 weeks at a community‐based gymnasium. (n = 23). 2. Usual care (n = 22) |
|
| Outcomes | Centre for Epidemiologic Studies for Depression scale | |
| Notes | Intention‐to‐treat analysis Outcome was self‐rated symptoms of depression by CES‐D scale |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomised list |
| Allocation concealment (selection bias) | Low risk | Randomisation was conducted centrally by an independent person |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, unclear risk of bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention were not blind, unclear risk of bias |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self report outcome (depressive symptoms by CES‐D scale) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Baseline assessment was performed in 45 people; complete data were available for 43 people at 6 months (23/23 in intervention group and 20/22 in the control) |
| Selective reporting (reporting bias) | Unclear risk | Reported all prespecified outcome (though we do not have access to the protocol) |
| Other bias | Unclear risk | Unclear |
Singh 1997.
| Methods | RCT | |
| Participants | Community volunteers from 2 registers of individuals interested in participation in research Mean age 70 (range 61 ‐ 88) 63% women N = 32 | |
| Interventions | 1. Supervised non‐aerobic progressive resistance training 3 times a week for 10 weeks (n = 17) 2. Control group received health seminars twice a week in which depression and mental health were not discussed (n = 15) | |
| Outcomes | 1. Beck Depression Inventory 2. Hamilton Rating Scale of Depression | |
| Notes | Outcome assessment not blind Intention‐to‐treat analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of blocks of 5 |
| Allocation concealment (selection bias) | Low risk | Assessed by Lawlor and Hopker as adequate |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention were not blind |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self‐rated BDI |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All completed the study |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported, though no protocol |
| Other bias | Unclear risk | Unclear |
Singh 2005.
| Methods | RCT | |
| Participants | People responding to a postal questionnaire who had DSM‐IV depression or dysthymia Mean age 69 55% women N = 60 | |
| Interventions | 1. Progressive resistance training at 80% of 1 repetition max (n = 20)
2. Resistance training at 20% of 1 repetition max (n = 20)
3. Usual care (n = 20) Each intervention group held 3 times a week for 8 weeks |
|
| Outcomes | 1. Hamilton Rating Scale for depression 2. Geriatric Depression score | |
| Notes | Not intention‐to‐treat (50/60 completed the study and were available for assessment) Outcome assessment blind | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Adequate. Sealed opaque envelopes open after baseline assessment |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, unclear effect on bias |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind to treatment allocation, unclear effect on bias |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | HRSD performed by blinded outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6/60 dropped out (2 from the high‐dose, 3 from the low‐dose and 1 from the usual care group) |
| Selective reporting (reporting bias) | Unclear risk | Prespecified outcomes in paper were reported, but no protocol |
| Other bias | Unclear risk | Unclear |
Veale 1992.
| Methods | RCT | |
| Participants | Psychiatric hospital outpatients and hospital day‐patients Mean age 35.5 (range 19 ‐ 58) 64% women N = 83 | |
| Interventions | 1. Group running 3 times a week for 12 weeks, plus routine care (n = 48) 2. Control group: routine care only (n = 35) | |
| Outcomes | 1. Beck Depression Inventory 2. State‐Trait Anxiety Inventory | |
| Notes | Outcome assessment not blind Analysis not intention‐to‐treat | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Low risk | Adequate (categorised by Lawlor and Hopker) |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, unclear risk |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering the intervention were not blind, but the influence on bias is unclear |
| Blinding (performance bias and detection bias) outcome assessors | High risk | Self‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | A total of 18 dropped out, leaving 65 for analyses |
| Selective reporting (reporting bias) | Unclear risk | All the prespecified outcomes stated in the paper were reported, but no protocol |
| Other bias | Unclear risk | unclear |
Williams 2008.
| Methods | RCT | |
| Participants | Residents recruited from 8 long‐term care facilities if clinical evidence of Alzheimer's Disease dementia and depression Mean age 87.9 (range 71 to 101) 89% women N = 45 |
|
| Interventions | 1. Comprehensive exercise ‐ strength, balance, flexibility and walking (n = 16) 2. Supervised walking at pace of individual (n = 17) 3. Control group of casual conversation (n = 12) Intervention delivered individually 5 days per week for 16 weeks |
|
| Outcomes | Cornell Scale for Depression in Dementia | |
| Notes | Analysis intention‐to‐treat Substantial drop‐out rate |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of random sequence generation not stated |
| Allocation concealment (selection bias) | Low risk | Adequate. Participants were assigned a code number, which was drawn by a research assistant who had no access to pretest results |
| Blinding (performance bias and detection bias) participants | Unclear risk | Participants not blind, though effect on bias unclear |
| Blinding (performance bias and detection bias) those delivering intervention | Unclear risk | Those delivering intervention were not blind, unclear risk on bias |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | Observational assessment by raters blind to treatment group allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 9/45 dropped out (1/16 in comprehensive exercise group, 6/17 in walking group, 2/12 in conversation) |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcome seem to be reported (although we do not have the trial protocol) |
| Other bias | Unclear risk | Unclear |
BDI: Beck Depression Inventory; BRMS: Bech‐Rafaelsen Scale; CBT: cognitive behavioural therapy; CES‐D: Center for Epidemiologic Studies Depression Scale; DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, fourth edition; HRSD/HAM‐D: Hamilton Rating Scale for Depression; RCT: randomised controlled trial; SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abascal 2008 | Did not have to have depression to enter trial |
| Akandere 2011 | Did not have to have depression to enter trial |
| Annesi 2010 | subgroup analysis from a trial in people with obesity |
| Arcos‐Carmona 2011 | Did not have to have depression to enter trial |
| Armstrong 2003 | Postnatal depression |
| Armstrong 2004 | Postnatal depression |
| Asbury 2009 | Did not have to have depression to enter trial |
| Attia 2012 | Not RCT for exercise in depression |
| Aylin 2009 | Did not have to have depression to enter trial |
| Badger 2007 | Did not have to have depression to enter trial |
| Baker 2006 | Did not have to have depression to enter trial |
| Bartholomew 2005 | Single bout of exercise |
| Beffert 1993 | Trial involving adolescents |
| Berke 2007 | Did not have to have depression to enter trial |
| Berlin 2003 | Duration of exercise was only 4 days |
| Biddle 1989 | Non‐systematic review |
| Blumenthal 2012b | Did not have to have depression to enter trial |
| Bodin 2004 | Single bout of either martial arts or stationary bike |
| Bosch 2009 | Did not have to have depression to enter trial |
| Bosscher 1993 | Comparing different types of exercise with no non‐exercising control group |
| Bowden 2012 | Not exercise according to ACSM; all arms received an intervention |
| Boyll 1986 | College students, did not have to have depression |
| Brittle 2009 | Did not have to have depression to enter trial |
| Bromby 2010 | Non‐randomised study |
| Broocks 1997 | Non‐systematic review |
| Brown 1992 | Trial involving adolescents with diagnoses of dysthymia and conduct disorder |
| Burbach 1997 | Non‐systematic review |
| Burton 2009 | Did not have to have depression to enter trial and multimodal intervention |
| Carney 1987 | Participants were those undergoing haemodialysis and did not have to have depression to be included |
| Chalder 2012 | Intervention not exercise; multimodal intervention including motivational interviewing, life coaching, support |
| Chan 2011 | Intervention is Dejian mind‐body intervention, not exercise. |
| Chen 2009 | Did not have to have depression to enter trial and intervention was yoga |
| Chou 2004 | Exercise intervention was Tai Chi |
| Chow 2012 | Exercise intervention was Qigong |
| Christensen 2012 | Did not have to have a depression to enter trial |
| Ciocon 2003 | Published in abstract form only, intervention appeared not to be exercise according to ACSM definition, and no further information available from the authors |
| Clegg 2011 | Did not have to have depression to enter trial |
| Courneya 2007 | Did not have to have depression to enter trial |
| Dalton 1980 | Trial in a "wheelchair bound population" with diverse aetiologies |
| Demiralp 2011 | Did not have to have depression to enter trial |
| Deslandes 2010 | Not randomized; participants chose their intervention |
| DeVaney 1991 | A trial of reducing exercise in those exercising more than 6 hours per week |
| DiLorenzo 1999 | People with depression were excluded |
| Eby 1985 | Trial of exercise in students who did not have to have depression to enter trial |
| Elavsky 2007 | Did not have to have depression to enter trial |
| Emery 1990a | Participants did not have to have depression |
| Emery 1990b | Participants did not have to have depression |
| Ersek 2008 | Did not have to have depression to enter trial |
| Fitzsimmons 2001 | Not exercise (the participant was placed in wheelchair adapted for connection to the front of a bicycle, the carer pedaled and steered the bicycle) |
| Fox 2007 | Did not have to have depression to enter trial |
| Gary 2007 | Did not have to have depression to enter trial |
| Ghroubi 2009 | Did not have to have depression to enter trial |
| Gottlieb 2009 | Did not have to have depression to enter trial |
| Gusi 2008 | Did not all have to have depression to enter trial |
| Gustafsson 2009 | Single bout of exercise with no non‐exercising control group |
| Gutierrez 2012 | Did not have to have depression to enter trial |
| Haffmans 2006 | Did not have to have depression to enter trial (mixed population of people with affective disorders) |
| Hannaford 1988 | General mental health patients with no separation of those with depression |
| Haugen 2007 | Did not have to have depression to enter trial |
| Hedayati 2012 | Not a trial |
| Hembree 2000 | Participants were ageing female population residing in a retirement home environment who did not have diagnosis of depression to enter the trial |
| Herrera 1994 | Participants did not have to have depression to enter the trial |
| Hughes 1986 | Effect of exercise on mood in people free from psychopathology |
| Hughes 2009 | Outline trial involving adolescents |
| Immink 2011 | Yoga as intervention |
| Jacobsen 2012 | Participants did not have to have depression to enter the trial |
| Johansson 2011 | Did not have to have depression to enter trial; intervention Qigong |
| Karlsson 2007 | Did not have to have depression to enter trial |
| Kerr 2008 | Did not have to have depression to enter trial |
| Kerse 2010 | Did not all have diagnosis of depression to enter trial |
| Kim 2004 | Effect of exercise on mental distress in healthy participants |
| Knapen 2003 | Non‐psychotic psychiatric patients with no separation of those with depression |
| Knapen 2006 | Did not have to have depression to enter trial (mixed depression and/or anxiety and/or personality disorders) |
| Kubesh 2003 | Outcome was executive function; Mood was measured using a subjective mental state scale. People with depression and some controls underwent neuropyschological testing prior to, or after exercise. Participants were randomly allocated to 2 doses of exercise. Thus, people with depression were not randomly allocated to exercise or control |
| Kulcu 2007 | Did not have to have depression to enter trial |
| Kupecz 2001 | Participants were veterans and did not have diagnosis of depression to enter the trial |
| Labbe 1988 | Comparison of exercise with exercise and instructions about how to improve compliance to exercise |
| Lacombe 1988 | Three types of exercise, no non‐exercising control |
| Lai 2006 | Trial in stroke patients. Did not have to have depression to be eligible |
| Latimer 2004 | Did not have to have depression to enter trial |
| Lautenschlager 2008 | Did not have to have depression to enter trial |
| Lavretsky 2011 | Control is health education, an active intervention |
| Legrand 2009 | Comparing 2 exercise regimens (of walking intensity) with no non‐exercising control group |
| Leibold 2010 | Qualitative analysis |
| Leppämäki 2002 | Effects of exercise on symptoms of mental distress in healthy participants |
| Levendoglu 2004 | Did not have to have depression to enter trial |
| Lever‐van Milligen 2012 | Did not have to have depression to be included in trial |
| Levinger 2011 | Did not have to have depression to enter trial |
| Lin 2007 | Did not have to have depression to enter trial |
| Littbrand 2011 | Did not have to have depression; control group undertake activity as intervention |
| Lolak 2008 | Did not have to have depression to enter the trial |
| Machado 2007 | Did not have to have depression to enter trial |
| MacMahon 1988 | Trial involving adolescents |
| Mailey 2010 | Participants were having mental health counselling, but there is no statement that they had to have depression to enter the study |
| Martin 2009 | Did not have to have depression to enter trial |
| Martinsen 1988a | Non‐systematic review |
| Martinsen 1988b | RCT (block randomisation with respect to sex) but compared different types of exercise without including a non‐exercising control group. |
| Martinsen 1989c | Non‐systematic review |
| Martinsen 1993 | Non‐systematic review |
| Matthews 2011 | Educational intervention and stretching exercises in control; did not have to be depressed to enter trial |
| McClure 2008 | intervention included a combination of interventions including a pedometer, Step Up program workbook, and a series of counselling calls from a study counsellor |
| Midtgaard 2011 | Did not have to have depression to enter trial |
| Milani 2007 | Retrospective evaluation of patients with depressive symptoms who participated in cardiac rehabilitation programme post major cardiac event |
| Morey 2003 | Older sedentary adults who did not have a diagnosis of depression to enter the trial |
| Motl 2004 | Older adults who did not have to be depressed to be included in the trial |
| Mudge 2008 | Did not have to have depression to enter trial |
| Munro 1997 | Cost‐effectiveness analysis of the likely public health benefits of purchasing exercise for over 65s |
| Mutrie 2007 | Did not have to have depression to enter trial |
| NCT00416221 | Study not randomised |
| NCT00546221 | Comparing 2 different exercise interventions with no non‐exercising control arm |
| NCT00964054 | Trial in adolescents |
| NCT01152086 | Comparing 2 exercise regimens (of hiking programme) with no non‐exercising control group, in participants with chronic suicidality, not depression |
| Neidig 1998 | Participants had HIV infection and did not have diagnosis of depression to enter trial |
| Netz 1994 | General mental health patients with no separation of those with depression |
| Neuberger 2007 | Did not have to have depression to enter trial |
| Nguyen 2001 | Trial in people with chronic obstructive pulmonary disease who did not have to have depression to enter trial |
| O'Neil 2011 | Multimodal intervention ‐ telephone based lifestyle advice as well as exercise |
| Oeland 2010 | Combination of people with depression and/or anxiety disorders |
| Oretzky 2006 | Exercise intervention was yoga |
| Ouzouni 2009 | Did not have to have depression to enter trial |
| Pakkala 2008 | Did not have to have depression to enter trial |
| Palmer 2005 | Participants were recovering from substance abuse |
| Passmore 2006 | Aerobic exercise versus aerobic and resistance exercise; no non‐exercising control |
| Peacock 2006 | The methodology fulfilled criteria but the study was not completed due to staff sickness |
| Pelham 1993 | General mental health patients with no separation of those with depression |
| Penninx 2002 | Retrospective subgroup analysis of patients who participated in a randomised trial of exercise for knee osteoarthritis who also had depression |
| Penttinen 2011 | A study in survivors of breast cancer, not depression |
| Perna 2010 | A study in breast cancer, not depression |
| Perri 1984 | No outcome measure of depression. This must have been excluded by Debbie Lawlor. |
| Piette 2011 | Does not fulfill ACSM criteria for exercise; intervention largely psychological |
| Raglin 1990 | Non‐systematic review |
| Rhodes 1980 | Not randomised, participants not depressed |
| Robledo Colonia 2012 | Did not have to have depression to enter trial |
| Rofey 2008 | Trial involving adolescents |
| Roshan 2011 | Trial in adolescents |
| Roth 1987 | No outcome measure of depression. This must have been excluded by Debbie Lawlor |
| Ruunsunen 2012 | Did not have to have depression to enter trial; intervention multimodal |
| Salminen 2005 | Coronary heart disease patients with no separation of those with depressive symptoms Intervention described by authors as health advocacy, counselling and activation programme |
| Salmon 2001 | Non‐systematic review |
| Sarsan 2006 | Did not have to have depression to enter trial |
| Schwarz 2012 | Unable to get access to full text of study; attempts made to contact authors were unsuccessful |
| Sexton 1989 | Comparing different types of exercise with no non‐exercising group |
| Silveira 2010 | Unable to assess if randomized; attempts made to contact authors unsuccessful, assumed to be non‐random |
| Sims 2006 | Did not all have diagnosis of depression to enter trial |
| Skrinar 2005 | DSM‐IV or psychotic disorders; no separation of those with depression |
| Smith 2008 | Did not have to have depression to enter trial |
| Sneider 2008 | intervention was combined diet and exercise |
| Songoygard 2012 | Did not have to have depression to be included in trial |
| Stein 1992 | Not described as randomised. Did not have to be depressed to participate |
| Stern 1983 | Trial in patients with myocardial infarction who did not have to be depressed to enter trial |
| Strömbeck 2007 | Did not have to have depression to enter trial |
| Sung 2009 | Did not have to have depression to enter trial |
| Tapps 2009 | Did not have to have depression to enter trial |
| Taylor 1986 | Trial in patients with myocardial infarction (no diagnosis of depression to enter trial) |
| Tenorio 1986 | Trial in subclinical depression |
| Thomson 2010 | Did not have to have depression to enter the trial |
| Tomas‐Carus 2008 | Did not have to have depression to enter trial |
| TREAD 2003 | Ongoing trial comparing 2 intensities of exercise |
| Trivedi 2011 | No true control group; both arms of trial receive exercise |
| Tsang 2003 | Participants had chronic physical disease not depression |
| Tsang 2006 | Exercise intervention was Qigong |
| Underwood 2013 | Did not have to have depression to enter trial |
| Van de Vliet 2003 | Single study design |
| Van der Merwe 2004 | Intervention was a manual‐based therapy programme not exercise |
| Vickers 2009 | Intervention was not exercise (exercise counselling) |
| Weinstein 2007 | Did not have to have depression to enter trial |
| Weiss 1989 | Not randomised controlled trial |
| White 2007 | Did not have to have depression to enter trial |
| Whitham 2011 | Trial in bipolar affective disorder |
| Wieman 1980 | Jogging versus racket ball so no non‐exercising control |
| Wilbur 2009 | Did not have to have depression to enter trial |
| Williams 1992 | Aerobic versus low‐intensity exercise. No control group |
| Wipfli 2008 | Did not have to have depression to enter trial |
| Wipfli 2011 | Participants did not have to be depressed to enter trial; control arm had intervention of yoga and stretching |
Characteristics of studies awaiting assessment [ordered by study ID]
Aghakhani 2011.
| Methods | Randomised trial |
| Participants | People with MI in selected hospitals in Iran |
| Interventions | Education programme, including 'exercises' |
| Outcomes | Hospital anxiety and depression score |
| Notes | Unlikely to fulfil inclusion criteria, as participants did not have to have depression and the intervention was multimodal |
DEMO II 2012.
| Methods | Randomised Controlled Trial |
| Participants | Outpatients with major depressive disorder (DSM‐IV) |
| Interventions | Supervised stretching or supervised aerobic fitness programme |
| Outcomes | Hamilton depression rating Scale |
| Notes | Unlikely to fulfil inclusion criteria, as the control arm also received exercise |
Gotta 2012.
| Methods | Clinical trial |
| Participants | People > 65 years with a recent decline in memory or thinking |
| Interventions | Aerobic or stretching exercise group, 60 minutes 3 times a week for 12 weeks |
| Outcomes | Depression included as an outcome measure |
| Notes | unlikely to be eligible for inclusion as it appears that people did not have to have depression to enter the trial |
Martiny 2012.
| Methods | Randomised trial, 75 adults |
| Participants | Major depression |
| Interventions | 9‐week 'chronotherapeutic intervention' or 9 weeks of daily exercise. Both groups received duloxetine |
| Outcomes | 17‐item Hamilton depression rating scale |
| Notes | Likely to be eligible for inclusion N=75 Study unlikely to contribute to current review comparisons. Further scrutiny required. |
Murphy 2012.
| Methods | Randomised clinical trial |
| Participants | People with 1 of several conditions (e.g. mental health problems, coronary heart disease) |
| Interventions | Welsh exercise referral scheme or usual care, Euroquol 5D, Hospital anxiety and depression score, Client Service Receipt Inventory questionnaire, |
| Outcomes | Total minutes of physical activity per week |
| Notes | Unlikely to be eligible for inclusion as the 'mental health' subgroup included people with depression, anxiety and stress, and because we have previously excluded trials that reported subgroups with depression |
Pinniger 2012.
| Methods | Randomised trial; three groups. (n = 97) |
| Participants | people with "self‐declared" depression |
| Interventions | 6‐week programme of Argentine tango dance, mindfulness meditation, waiting list control |
| Outcomes | Depression, anxiety and stress scale, self esteem scale, satisfaction with life scale, and mindful attention awareness scale |
| Notes | Likely to be eligible for inclusion N=66 Study could contribute data to two comparisons, although three‐arm trial with small sample size. Results positive for intervention involving exercise. Unlikely to affect review conclusions. |
Sturm 2012.
| Methods | Randomised trial (n = 20) |
| Participants | People with previous suicidal attempts and clinically diagnosed with "hopelessness" |
| Interventions | 9‐week hiking, 9‐week control |
| Outcomes | Hopelessness, depression, physical endurance, suicidal ideation |
| Notes | Likely to be eligible for inclusion N=20 Study could contribute data for one comparison, although very small sample size. Results positive for intervention involving exercise. Unlikely to affect review conclusions. |
CBT: cognitive behavioural therapy; HAM‐D: Hamilton Rating Scale for Depression
Characteristics of ongoing studies [ordered by study ID]
ACTRN12605000475640.
| Trial name or title | Does a home‐based physical activity programme improve function and depressive symptomatology in older primary care patients: a randomised controlled trial |
| Methods | Randomised controlled trial |
| Participants | Those aged 75 or older with depression |
| Interventions | Home‐based physical activity programme |
| Outcomes | Change in geriatric depression score |
| Starting date | 2006 |
| Contact information | Karen Hayman k.hayman@auckland.ac.nz |
| Notes |
ACTRN12609000150246.
| Trial name or title | Promoting physical activity to improve the outcome of depression in later life (ACTIVEDEP) |
| Methods | Randomised controlled trial ‐ parallel |
| Participants | Age 50 or over with DSM‐IV diagnosis of depression |
| Interventions | Mixed aerobic and strength training programme |
| Outcomes | Montgomery‐Asperg Depression Rating Scale; remission of symptoms |
| Starting date | 2009 |
| Contact information | Osvaldo Ameida osvaldo.almeida@uwa.edu.au |
| Notes |
ACTRN12612000094875.
| Trial name or title | A randomised controlled trial to improve depression in family carers through a physical activity intervention IMPACCT Study |
| Methods | Randomised controlled trial |
| Participants | Depressed carers over 60 and their care recipients |
| Interventions | 6‐month physical activity programme |
| Outcomes | Rating on Geriatric Depression Scale |
| Starting date | 2012 |
| Contact information | Ms Kirsten Moore k.moore@nari.unimelb.edu.au |
| Notes | Completed, unreported study |
CTR/2012/09/002985.
| Trial name or title | Effect of sprint interval training on depression: a randomised controlled trial |
| Methods | Randomisation, blinding |
| Participants | Age 20 35, male, diagnosis of depression |
| Interventions | Sprint training exercise or aerobic exercise |
| Outcomes | Depression scale |
| Starting date | September 2012 |
| Contact information | Dr Khaled Badaam khalid_badaam@yahoo.com |
| Notes | Completed, unreported study |
EFFORT D.
| Trial name or title | Effect of running therapy on depression (EFFORT‐D). Design of a randomised controlled trial in adult patients [ISCRCTN 1894] |
| Methods | Randomised controlled trial |
| Participants | People with a depressive disorder |
| Interventions | Group‐based 1‐hour exercise sessions of increased intensity over 6 months |
| Outcomes | Reduction in depressive symptoms as measured by HAM‐D |
| Starting date | 2012 |
| Contact information | Frank Kruisdijk f.kruisdijk@ggzcentraal.nl |
| Notes |
IRCT201205159763.
| Trial name or title | The effect of regular exercise on the depression of haemodialysis patients |
| Methods | |
| Participants | Age 15 ‐ 65, chronic kidney disease receiving haemodialysis |
| Interventions | Exercise |
| Outcomes | Beck Depression Inventory Score |
| Starting date | June 2012 |
| Contact information | Alireza Abdi alireza_abdi61@yahoo.com |
| Notes | Depression not specified in inclusion criteria Completed, unreported study |
IRCT2012061910003N1.
| Trial name or title | A comparative study of the efficiency of group cognitive‐behavioural therapy with aerobic exercise in treating major depression |
| Methods | Randomised |
| Participants | 18 ‐ 25 with depressive symptoms |
| Interventions | Either exercise or CBT or no intervention as control |
| Outcomes | Beck Depression Inventory score |
| Starting date | July 2012 |
| Contact information | Kheirollah Sadeghi khsadeghi@kums.ac.ir |
| Notes | Completed, unreported study |
ISRCTN05673017.
| Trial name or title | Psycho‐education physical exercise effects: does treating subsyndromal depression improve depression‐ and diabetes‐related outcomes? PEPEE |
| Methods | Randomised controlled three‐arm study |
| Participants | 18 ‐ 60 years with depression and Type II diabetes |
| Interventions | Psycho‐education or exercise intervention or control |
| Outcomes | Depressive symptoms |
| Starting date | 2010 |
| Contact information | Mirjana Pibernik‐Okanovic mirjana.pibernik@idb.hr |
| Notes |
NCT00103415.
| Trial name or title | Randomized clinical trial Investigating the effect of different exercise forms on depression |
| Methods | Randomised interventional model |
| Participants | 18 ‐ 55 with depression |
| Interventions | Strength endurance training |
| Outcomes | Hamilton Depression Scoring Scale |
| Starting date | 2006 |
| Contact information | Merete Nordentoft Bispebjerg Hospital |
| Notes |
NCT00643695.
| Trial name or title | Efficacy of an exercise intervention to decrease depressive symptoms in veterans with hepatitis C |
| Methods | Randomised interventional model |
| Participants | Adults positive for hepatitis C with depression |
| Interventions | Home‐based walking programme |
| Outcomes | Reduction in Beck Depression Scale |
| Starting date | 2008 |
| Contact information | Patricia Taylor‐Young Portland VA Medical Centre |
| Notes |
NCT00931814.
| Trial name or title | Effects of exercise on depression symptoms, physical function, and quality of life in community‐dwelling elderly |
| Methods | Randomised interventional model |
| Participants | Community‐dwelling participants age 65 or older |
| Interventions | Group exercise 3 times per week |
| Outcomes | Taiwanese Geriatric Depression Scale |
| Starting date | 2009 |
| Contact information | Ying‐Tai Wu National Taiwan University |
| Notes |
NCT01024790.
| Trial name or title | Exercise study to help patients who have type 2 diabetes and depression |
| Methods | Randomised interventional model |
| Participants | Eomen 21 ‐ 65, with depression and diabetes |
| Interventions | Exercise group |
| Outcomes | Depression symptoms |
| Starting date | 2009 |
| Contact information | Kristin Schneider University of Massachusetts, Worcester |
| Notes |
NCT01383811.
| Trial name or title | Clinical and neuroendocrine/metabolic benefits of exercise in treatment resistant depression (TRD): a feasibility study |
| Methods | Randomised controlled trial |
| Participants | Sedentary adults with depression |
| Interventions | Moderate intensity aerobic exercise |
| Outcomes | Change from baseline depression score on Hamilton Scale |
| Starting date | 2011 |
| Contact information | Ravi Singareddy Penn State University College of Medicine |
| Notes |
NCT01401569.
| Trial name or title | Efficacy of exercise and counselling Intervention on relapse in smokers with depressive disorders STOB‐ACTIV |
| Methods | Randomised, intervention model |
| Participants | 18‐65 with depression |
| Interventions | Exercise |
| Outcomes | Evaluation of depression |
| Starting date | 2010 |
| Contact information | Xavier Quantin x‐quantin@chu‐montpellier.fr |
| Notes | May be multimodal with counselling for smoking cessation |
NCT01464463.
| Trial name or title | The impact of psychological interventions (with and without exercise) on psychometric and immunological measures in patients with major depression |
| Methods | Randomised controlled trial |
| Participants | 18 ‐ 65 year‐olds with depression diagnosed according to DSM‐IV |
| Interventions | Exercise and psychological input |
| Outcomes | Change in depression symptomology |
| Starting date | 2011 |
| Contact information | Frank Euteneuer frank.euteneuer@staff.uni‐marburg.de |
| Notes | Intervention may be multimodal |
NCT01573130.
| Trial name or title | An internet‐administered, therapist‐supported physical exercise program for the treatment of depression |
| Methods | Randomised intervention model |
| Participants | Adults with DSM‐IV diagnosis of depression |
| Interventions | Physical exercise programme |
| Outcomes | Change in MADRS rating scale for depression |
| Starting date | March 2012 |
| Contact information | Prof Per Carlbing per.carlbring@psy.umu.se |
| Notes |
NCT01573728.
| Trial name or title | Role of exercise in depression in middle aged and older adults |
| Methods | Randomised, double‐blind |
| Participants | Age 46 or older; diagnosis of depression |
| Interventions | Low‐dose exercise |
| Outcomes | PHQ 9 depression score |
| Starting date | May 2012 |
| Contact information | Daniel O Clark Indiana University School of Medicine |
| Notes |
NCT01619930.
| Trial name or title | The effects of behavioral activation and physical exercise on depression |
| Methods | Randomised, Intervention Model |
| Participants | Participants with depression |
| Interventions | Behavioural activation, motivational interviewing, physical activity |
| Outcomes | Change from baseline in Patient Health Questionnaire |
| Starting date | August 2012 |
| Contact information | Professor Per Carlbring per.carlbring@psy.umu.se |
| Notes |
NCT01696201.
| Trial name or title | Effect of a supervised exercise program during whole pregnancy on outcomes and level of depression. A randomized controlled trial |
| Methods | Randomised, intervention |
| Participants | Pregnant women |
| Interventions | Exercise group |
| Outcomes | Change in level of depression |
| Starting date | 2009 |
| Contact information | Maria Perales m.perales.santaella@gmail.com |
| Notes |
NCT01763983.
| Trial name or title | Effects of Cognitive Behavioural Therapy and exercise on depression and cognitive deficits in Multiple Sclerosis |
| Methods | Randomised, single‐blind, intervention model |
| Participants | 18 ‐ 50 years‐old with multiple sclerosis and depression |
| Interventions | Exercise, CBT |
| Outcomes | Change in Hamilton Depression rating, cognitive scoring |
| Starting date | January 2013 |
| Contact information | Bethany Lerman bethany.lerman@sunnybrook.ca |
| Notes |
NCT01787201.
| Trial name or title | The effects of exercise in depression symptoms using levels of neurotransmitters and EEG as markers |
| Methods | Randomised, intervention model |
| Participants | 18 ‐ 65 years old with depression |
| Interventions | Exercise |
| Outcomes | Beck Depression Inventory score, serum levels serotonin and catecholamines |
| Starting date | March 2013 |
| Contact information | Dr Timothy Barclay thbarclay@liberty.edu |
| Notes |
NCT01805479.
| Trial name or title | Exercise training in depressed traumatic brain injury survivors |
| Methods | Randomised, single‐blind intervention model |
| Participants | Depressed, sedentary survivors of traumatic brain injury |
| Interventions | Aerobic exercise |
| Outcomes | Mood assessment, MRI, neuropsychology testing, biochemical assays, suicide severity rating |
| Starting date | February 2013 |
| Contact information | Justin Alicea joalicea@vcu.edu |
| Notes |
UMIN000001488.
| Trial name or title | A randomised controlled trial of exercise class for older persons with mild depression |
| Methods | Parallel randomised trial |
| Participants | 60 ‐ 86 year‐olds with mild depression |
| Interventions | Low‐intensity exercise programme |
| Outcomes | Hamilton Depression Rating Scale |
| Starting date | 2009 |
| Contact information | Kazushige Ihara ihara1@med.toho‐u.ac.jp |
| Notes |
BDI: Beck Depression Inventory; RCT: randomised controlled trial; MDD: major depressive disorder
Differences between protocol and review
For this update, we defined exercise according to the American College of Sports Medicine (ACSM) definition of exercise, rather than the trialist's own definition of exercise. We performed an additional sensitivity analysis to explore the effect of excluding those trials for which we used the arm with the largest clinical effect, rather than the largest 'dose' of exercise.
Changes for this update: we added subgroups, performed a sensitivity analysis for low/high 'dose' of exercise, included more detail in 'included study' table; we decided to include cluster‐RCTs, we produced a PRISMA diagram for the results of the searches for update; and we produced a 'Summary of findings' tables.
Contributions of authors
This review is based on a previously published BMJ review by Debbie Lawlor and Stephen Hopker. For this update, Dr Cooney and Professor Mead scrutinised studies and selected studies for inclusion. Dr Waugh and Dr Cooney performed data extraction, Dr Dwan performed the analysis, Dr Greig categorised intensity of exercise, and assisted with study selection. Professor Mead, Dr Cooney and Dr Dwan wrote the text. The text was read by all authors.
Sources of support
Internal sources
NHS Lothian, University of Edinburgh, UK.
External sources
National Institute for Health Research, Cochrane Review Incentive Scheme 2012, UK.
Declarations of interest
Marion McMurdo is co‐director of D.D. Developments, a University of Dundee not‐for‐profit organisation which provides exercise classes for older people.
Gillian E Mead developed a course on exercise after stroke which is licensed to Later Life Training. She receives royalty payments from Later Life Training, which are paid into an account at University of Edinburgh to support further research. She personally receives royalties from a book about Exercise and Fitness Training after Stroke. She receives expenses for speaking at conferences on exercise and fatigue after stroke.
Kerry Dwan: none known.
Carolyn A Greig: none known.
Debbie A Lawlor: none known.
Gary Cooney: None known
Jane Rimer: none known.
Fiona Waugh: none known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Blumenthal 1999 {published data only}
- Babyak M, Blumenthal JA, Herman S, Khatri P, Doraiswamy M, Moore K, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosomatic Medicine 2000;62(5):633‐8. [DOI] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, Moore KA, Craighead WE, Herman S, Khatri P, et al. Effects of exercise training on older patients with major depression. Archives of Internal Medicine 1999;159(19):2349‐56. [DOI] [PubMed] [Google Scholar]
- Herman S, Blumenthal JA, Babyak M, Khatri P, Craighead WE, Krishnan KR, et al. Exercise therapy for depression in middle‐aged and older adults: predictors of early dropout and treatment failure. Health Psychology 2002;21(6):533‐63. [PubMed] [Google Scholar]
- Khatri P, Blumenthal JA, Babyak MA, Craighead WE, Herman S, Baldewitz T, et al. Effects of exercise training on cognitive functioning among depressed older men and women. Journal of Aging and Physical Activity 2001;9:43‐57. [Google Scholar]
Blumenthal 2007 {published data only}
- Blumenthal JA, Babyak MA, Doraiswamy PM, Watkins L, Hoffman BM, Barbour KA, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosomatic Medicine 2007;69(7):587‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman BM, Babyak MA, Craighead WE, Sherwood A, Doraiswamy PM, Coons MJ, et al. Exercise and pharmacotherapy in patients with major depression: one‐year follow‐up of the SMILE study. Psychosomatic Medicine 2011;73(2):127‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blumenthal 2012a {published data only}
- Blumenthal J, Sherwood A, Babyak M, Watkins L, Smith PJ, Hoffman B, et al. Exercise and pharmacological treatment of depressive symptoms in patients with coronary heart disease. Journal of the American College of Cardiology 2012;60(12):1053‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal JA, Sherwood A, Rogers SD, Babyak MA, Doraiswamy M, Watkins L, et al. Understanding prognostic benefits of exercise and antidepressant therapy for persons with depression and heart disease: the UPBEAT study‐rationale, design, and methodological issues. Clinical Trials 2007;4:548. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bonnet 2005 {published data only}
- Bonnet LH. Effects of Aerobic Exercise in Combination with Cognitive Therapy on Self Reported Depression [dissertation]. Hempstead, NY: Hofstra University, 2005. [Google Scholar]
Brenes 2007 {published data only}
- Brenes GA, Williamson JD, Messier SP, Rejeski WJ, Pahor M, Ip E, et al. Treatment of minor depression in older adults: a pilot study comparing sertraline and exercise. Aging and Mental Health 2007;11(1):61‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chu 2008 {published data only}
- Chu IH. Effect of Exercise Intensity During Aerobic Training on Depressive Symptoms in Initially Sedentary Depressed Women [dissertation]. Columbus, OH: The Ohio State University, 2008. [Google Scholar]
- Chu IH, Buckworth J, Kirby TE, Emery CF. Effect of exercise intensity on depressive symptoms in women. Mental Health and Physical Activity 2009;2(1):37‐43. [Google Scholar]
Doyne 1987 {published data only}
- Doyne EJ, Ossip‐Klein DJ, Bowman ED, Osborn KM, McDougall‐Wilson IB, Neimeyer RA. Running versus weight lifting in the treatment of depression. Journal of Consulting and Clinical Psychology 1987;55(5):748‐54. [DOI] [PubMed] [Google Scholar]
- Ossip‐Klein DJ, Doyne EJ, Bowman ED, Osborn KM, McDougall‐Wilson IB, Neimeyer RA. Effects of running or weight lifting on self‐concept in clinically depressed women. Journal of Consulting and Clinical Psychology 1989;7(1):158‐61. [DOI] [PubMed] [Google Scholar]
Dunn 2005 {published data only}
- Dunn AL, Trivedi MH. Exercise and depression: meeting standards to establish treatment efficacy. Proceedings of the 63rd Annual Meeting of the American Psychosomatic Society, 2005 March 2‐5, Vancouver, Canada. McLean, VA: American Psychosomatic Society, 2005:A19.
- Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. American Journal of Preventive Medicine 2005;28(1):1‐8. [DOI] [PubMed] [Google Scholar]
- Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. The DOSE study: a clinical trial to examine efficacy and dose response of exercise as a treatment for depression. Controlled Clinical Trials 2002;23:584‐603. [DOI] [PubMed] [Google Scholar]
- Kitzman HE, Trivedi MH, Dunn AL, Galper DI, Kampert JB, Greer TL. The effect of exercise dose on quality of life in depressed adults. Proceedings of the 63rd Annual Meeting of the American Psychosomatic Society, 2005 March 2‐5, Vancouver, Canada. McLean, VA: American Psychosomatic Society, 2005:A110.
Epstein 1986 {published data only}
- Epstein D. Aerobic Activity Versus Group Cognitive Therapy: an Evaluative Study of Contrasting Interventions for the Alleviation of Clinical Depression [dissertation]. Reno: University of Nevada, 1986. [Google Scholar]
Fetsch 1979 {published data only}
- Fetsch RJ. A comparison of the psychological effects of running and transactional analysis stroking for the relief of reactive depression in adults [thesis]. Dissertation Abstracts International 1980;40(10‐B):4999. [Google Scholar]
Foley 2008 {published data only}
- Foley LS, Prapavessis H, Osuch EA, Pace JA, Murphy BA, Podolinsky NJ. An examination of potential mechanisms for exercise as a treatment for depression: a pilot study. Mental Health and Physical Activity 2008;1(2):69‐73. [Google Scholar]
Fremont 1987 {published data only}
- Fremont J. The Separate and Combined Effects of Cognitively Based Counseling and Aerobic Exercise for the Treatment of Mild and Moderate Depression [dissertation]. PA, USA: Pennsylvania State University, 1983. [Google Scholar]
- Fremont J, Wilcoxon Craighead L. Aerobic exercise and cognitive therapy in the treatment of dysphoric moods. Cognitive Therapy and Research 1987;11:241‐51. [Google Scholar]
Gary 2010 {published data only}
- Gary RA, Dunbar SB, Higgins MK, Musselman DL, Smith AL. Combined exercise and cognitive behavioral therapy improves outcomes in patients with heart failure. Journal of Psychosomatic Research 2010;69(2):119‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Greist 1979 {published data only}
- Greist JH, Klein MH, Eischens RR, Faris J, Gurman AS, Morgan WP. Running as a treatment for depression. Proceedings of the 131st Annual Meeting of the American Psychiatric Association; 1978 May 8‐12; Atlanta, GA. 1978.
- Greist JH, Klein MH, Eischens RR, Faris J, Gurman AS, Morgan WP. Running as treatment for depression. Comprehensive Psychiatry 1979;20(1):41‐54. [DOI] [PubMed] [Google Scholar]
- Greist JH, Klein MH, Eischens RR, Faris J, Gurman AS, Morgan WP. Running through your mind. Journal of Psychosomatic Research 1978;22(4):259‐94. [DOI] [PubMed] [Google Scholar]
Hemat‐Far 2012 {published data only}
- Hemat‐Far A, Shahsavari A, Mousavi SR. Effects of selected aerobic exercises on the depression and concentrations of plasma serotonin in the depressed female students aged 18 to 25. Journal of Applied Research 2012;12(1):47‐52. [Google Scholar]
Hess‐Homeier 1981 {published data only}
- Hess‐Homeier MJ. A Comparison of Beck's Cognitive Therapy and Jogging as Treatments for Depression [dissertation]. Missoula: University of Montana, 1981. [Google Scholar]
Hoffman 2010 {published data only}
- Hoffman JM, Bell KR, Powell JM, Behr J, Dunn EC, Dikmen S, et al. A randomized controlled trial of exercise to improve mood after traumatic brain injury. American Academy of Physical Medicine and Rehabilitation 2010;2:911‐9. [DOI] [PubMed] [Google Scholar]
- Wise ER, Hoffman JM, Powell JM, Bombadier CH, Bell KR. Benefits of exercise maintenance after traumatic brain injury. Archives of Physical Medicine and Rehabilitation 2012;93(8):1319‐23. [DOI] [PubMed] [Google Scholar]
Klein 1985 {published data only}
- Klein MH, Greist JH, Gurman RA, Neimeyer RA, Lesser DP, Bushnell NJ. A comparative outcome study of group psychotherapy vs. exercise treatments for depression. International Journal of Mental Health 1985;13:148‐77. [Google Scholar]
Knubben 2007 {published data only}
- Knubben K, Reischies FM, Adli M, Schlattmann P, Bauer M, Dimeo F. A randomised controlled study on the effects of a short‐term endurance training programme in patients with major depression. British Journal of Sports Medicine 2007;41:29‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Krogh 2009 {published data only}
- Krogh J, Nordentoft M, Mohammad‐Nezhad M, Westrin A. Growth hormone, prolactin and cortisol response to exercise in patients with depression. Journal of Affective Disorders 2010;125:189‐97. [DOI] [PubMed] [Google Scholar]
- Krogh J, Petersen L, Timmermann M, Saltin B, Nordentoft M. Design paper: The DEMO trial: a randomized, parallel‐group, observer‐blinded clinical trial of aerobic versus non‐aerobic versus relaxation training for patients with light to moderate depression [NCT00103415]. Contemporary Clinical Trials 2007;28(1):79‐89. [DOI] [PubMed] [Google Scholar]
- Krogh J, Saltin B, Gluud C, Nordentoft M. The DEMO Trial: a randomized, parallel‐group, observer‐blinded clinical trial of strength versus aerobic versus relaxation training for patients with mild to moderate depression. Journal of Clinical Psychiatry 2009;70(6):790‐800. [DOI] [PubMed] [Google Scholar]
Martinsen 1985 {published data only}
- Martinsen EW, Medhus A, Sandvik L. Effects of aerobic exercise on depression: a controlled study. British Medical Journal 1985;291(6488):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mather 2002 {published data only}
- Mather AS, Rodrigues C, Guthrie MF, McHarg AM, Reid IC, McMurdo MET. Effects of exercise on depressive symptoms in older adults with poorly responsive depressive disorder. British Journal of Psychiatry 2002;180:411‐5. [DOI] [PubMed] [Google Scholar]
McCann 1984 {published data only}
- McCann IL, Holmes DS. Influence of aerobic exercise on depression. Journal of Personality and Social Psychology 1984;46(5):1142‐7. [DOI] [PubMed] [Google Scholar]
McNeil 1991 {published data only}
- McNeil JK, LeBlanc EM, Joyner M. The effect of exercise on depressive symptoms in the moderately depressed elderly. Psychology and Aging 1991;6(3):487‐8. [DOI] [PubMed] [Google Scholar]
Mota‐Pereira 2011 {published data only}
- Mota‐Pereira J, Silverio J, Carvalho S, Ribiero JC, Fonte D, Ramos J. Moderate exercise improves depression parameters in treatment‐resistant patients with major depressive disorder. Journal of Psychiatric Research 2011;45:1005‐11. [DOI] [PubMed] [Google Scholar]
Mutrie 1988 {published data only}
- Mutrie N. Exercise as a Treatment for Depression within a National Health Service [dissertation]. PA, USA: Pennsylvania State University, 1986. [Google Scholar]
- Mutrie N. Exercise as a treatment for moderate depression in the UK National Health Service [abstract]. Proceedings of Sport, Health Psychology and Exercise Symposium, Sports Council and Health Education Authority, London 1988:96‐105.
Nabkasorn 2005 {published data only}
- Nabkasorn C, Miyai N, Sootmongkol A, Junprasert S, Yamamoto H, Arita M, et al. Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms. European Journal of Public Health 2005;16:179‐84. [DOI] [PubMed] [Google Scholar]
Orth 1979 {published data only}
- Orth DK. Clinical Treatments for Depression [dissertation]. Morgantown, WV: West Virginia University, 1979. [Google Scholar]
Pilu 2007 {published data only}
- Carta MG, Hardoy MC, Pilu A, Sorba M, Floris AL, Mannu FA, et al. Improving physical quality of life with group physical activity in the adjunctive treatment of major depressive disorder. Clinical Practice and Epidemiology in Mental Health 2008;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilu A, Sorba M, Hardoy MC, Floris AL, Mannu F, Seruis ML, et al. Efficacy of physical activity in the adjunctive treatment of major depressive disorders: preliminary results. Clinical Practice and Epidemiology in Mental Health 2007;3(8):doi:10.1186/1745‐0179‐3‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinchasov 2000 {published data only}
- Pinchasov BB, Shurgaja AM, Grischin OV, Putilov AA. Mood and energy regulation in seasonal and non‐seasonal depression before and after midday treatment with physical exercise or bright light. Psychiatry Research 2000;94:29‐42. [DOI] [PubMed] [Google Scholar]
Reuter 1984 {published data only}
- Reuter M, Mutrie N, Harris DV. Running as an adjunct to counseling in the treatment of depression [unpublished manuscript]. Pennsylvania State University, 1984. [Google Scholar]
Schuch 2011 {published data only}
- Schuch FB, Vasconcelos‐Moreno MP, Borowsky C, Fleck MP. Exercise and severe depression: preliminary results of an add‐on study. Journal of Affective Disorders 2011;133:615‐8. [DOI] [PubMed] [Google Scholar]
Setaro 1985 {published data only}
- Setaro JL. Aerobic Exercise and Group Counseling in the Treatment of Anxiety and Depression [dissertation]. Maryland: University of Baltimore, 1985. [Google Scholar]
Shahidi 2011 {published data only}
- Shahidi M. Reply to the letter to the editor re Shahidi M, Mojtahed A, Modabbernia a, et al. 2011. Laughter yoga versus group exercise program in elderly depressed women: A randomized controlled trial. Int j geriatr psychiatr 26: 322‐327. First things first! Caveats in research on "laughter yoga". International Journal of Geriatric Psychiatry 2012;27(8):875‐6. [DOI] [PubMed] [Google Scholar]
- Shahidi M, Mojtahed A, Modabbernia A, Mojtahed M, Shafiabady A, Delavar A, et al. Laughter yoga versus group exercise program in elderly depressed women: a randomized controlled trial. International Journal of Geriatric Psychiatry 2011;26(3):322‐7. [DOI] [PubMed] [Google Scholar]
Sims 2009 {published data only}
- Sims J, Galea M, Taylor N, Dodd K, Jespersen S, Joubert L, et al. Regenerate: assessing the feasibility of a strength‐training program to enhance the physical and mental health of chronic post stroke patients with depression. International Journal of Geriatric Psychiatry 2009;24(1):76‐83. [DOI] [PubMed] [Google Scholar]
- Teoh V, Sims J, Milgrom J. Psychosocial predictors of quality of life following a stroke. Topics in Stroke Rehabilitation 2009;16(2):157‐66. [DOI] [PubMed] [Google Scholar]
Singh 1997 {published data only}
- Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of progressive resistance training in depressed elders. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 1997;52(1):M27‐35. [DOI] [PubMed] [Google Scholar]
- Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of the effect of exercise on sleep. Sleep 1997;20(2):95‐100. [DOI] [PubMed] [Google Scholar]
Singh 2005 {published data only}
- Singh NA, Stavrions TM, Scarbek Y, Galambos G, Liber C, Fiatorone Singh MA. A randomised controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2005;60A:768‐76. [DOI] [PubMed] [Google Scholar]
Veale 1992 {published data only}
- Veale D, Fevre K, Pantelis C, Souza V, Mann A, Sargeant A. Aerobic exercise in the adjunctive treatment of depression: a randomized controlled trial. Journal of the Royal Society of Medicine 1992;85(9):541‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2008 {published data only}
- Williams CL, Tappen RM. Exercise training for depressed older adults with Alzheimer's disease. Aging and Mental Health 2008;12(1):72‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Abascal 2008 {published data only}
- Abascal L. The Effect of Depression and Adherence in a Dietary and Physical Activity Intervention for Overweight and Obese Adults [dissertation]. University of California, San Diego and San Diego State University 2008.
Akandere 2011 {published data only}
- Ankandere M, Demir B. The effect of dance over depression. Collegium Antropologicum 2011;35(3):651‐6. [PubMed] [Google Scholar]
Annesi 2010 {published data only}
- Annesi JJ, Gorjala S. Association of reduction in waist circumference with normalization of mood in obese women initiating exercise supported by the Coach Approach protocol. Southern Medical Journal 2010;103(6):517‐21. [DOI] [PubMed] [Google Scholar]
Arcos‐Carmona 2011 {published data only}
- Arcos‐Carmona IM, Castro‐Sanchez AM, Mataran‐Penarrocha GA, Gutierrez‐Rubio AB, Ramos‐Gonzalez E, Moreno‐Lorenzo C. Effects of aerobic exericise program and relaxation techniques on anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia: A randomised controlled trial. Medicina Clinica 2011;137(9):398‐401. [DOI] [PubMed] [Google Scholar]
Armstrong 2003 {published data only}
- Armstrong K, Edwards H. The effects of exercise and social support on mothers reporting depressive symptoms: a pilot randomised controlled trial. International Journal of Mental Health Nursing 2003;12:130‐8. [DOI] [PubMed] [Google Scholar]
Armstrong 2004 {published data only}
- Armstrong K, Edwards H. The effectiveness of a pram‐walking exercise programme in reducing depressive symptomatology for postnatal women. International Journal of Nursing Practice 2004;10:177‐94. [DOI] [PubMed] [Google Scholar]
Asbury 2009 {published data only}
- Asbury EA, Kanji N, Ernst E, Barbir M, Collins P. Autogenic training to manage symptomology in women with chest pain and normal coronary arteries. Menopause 2009;16(1):60‐5. [DOI] [PubMed] [Google Scholar]
Attia 2012 {published data only}
- Attia E. In the clinic eating disorders. Annals of Internal Medicine 2012;156(7):1‐16. [DOI] [PubMed] [Google Scholar]
Aylin 2009 {published data only}
- Aylin K, Arzu D, Sabri S, Handan TE, Ridvan A. The effect of combined resistance and home‐based walking exercises in type 2 diabetes patients. International Journal of Diabetes in Developing Countries 2009;29(4):159‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Badger 2007 {published data only}
- Badger T, Segrin C, Dorros SM, Meek P, Lopez AM. Depression with anxiety in women with breast cancer and their partners. Nursing Research 2007;56(1):44‐53. [DOI] [PubMed] [Google Scholar]
Baker 2006 {published data only}
- Baker MK, Kennedy DJ, Bohle PL, Campbell DS, Knapman L, Grady J, et al. Efficacy and feasibility of a novel tri‐modal robust exercise prescription in a retirement community: a randomised, controlled trial. Journal of the American Geriatrics Society 2007;55:1‐10. [DOI] [PubMed] [Google Scholar]
Bartholomew 2005 {published data only}
- Bartholomew JB, Morrison D, Ciccolo JT. Effects of acute exercise on mood and well‐being in patients with major depressive disorder. Medicine and Science in Sports and Exercise 2005;37:2032‐7. [DOI] [PubMed] [Google Scholar]
Beffert 1993 {published data only}
- Beffert JW. Aerobic Exercise as Treatment of Depressive Symptoms in Early Adolescents [dissertation]. University of Northern Colorado 1993.
Berke 2007 {published data only}
- Berke EM, Gottlieb LM, Moudon AV, Larson EB. Protective association between neighborhood walkability and depression in older men. Journal of the American Geriatrics Society 2007;55:526‐33. [DOI] [PubMed] [Google Scholar]
Berlin 2003 {published data only}
- Berlin B, Moul DE, LePage JP, Mogge NL, Sellers DG. The effect of aquatic therapy interventions on patients with depression: a comparison study. Annual in Therapeutic Recreation 2003;12:7‐13. [Google Scholar]
Biddle 1989 {published data only}
- Biddle S. Exercise and the treatment of depression. British Journal of Hospital Medicine 1989;42(4):267. [PubMed] [Google Scholar]
Blumenthal 2012b {published data only}
- Blumenthal JA, Babyak MA, O'Connor C, Keteyian S, Landzberg J, Howlett J, et al. Effects of exercise training on depressive symptoms in patients with chronic heart failure. JAMA 2012;308(5):465‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bodin 2004 {published data only}
- Bodin T, Martinensen EW. Mood and self‐efficacy during acute exercise in clinical depression. A randomised controlled study. Journal of Sport and Exercise Psychology 2004;26:623‐33. [Google Scholar]
Bosch 2009 {published data only}
- Bosch PR, Traustadóttir T, Howard P, Matt KS. Functional and physiological effects of yoga in women with rheumatoid arthritis: a pilot study. Alternative Therapies in Health and Medicine 2009;15(4):24‐31. [PubMed] [Google Scholar]
Bosscher 1993 {published data only}
- Bosscher RJ. Running and mixed physical exercises with depressed psychiatric patients. International Journal of Sport Psychology 1993;24:170‐84. [Google Scholar]
Bowden 2012 {published data only}
- Bowden D, Gaudry C, An SC, Gruzelier J. A comparative randomised controlled trial of the effects of brain wave vibration training, Iyengar yoga, and mindfulness on mood, well‐being, and salivary cortisol. Evidence‐based Complementary and Alternative Medicine 2012 Dec 15 [Epub ahead of print]. [DOI: 10.1155/2012/234713] [DOI] [PMC free article] [PubMed]
Boyll 1986 {published data only}
- Boyll JF. The Effects of Active and Passive Electronic Muscle Stimulation on Self‐concept, Anxiety and Depression [dissertation]. Flagstaff: Northern Arizona University, 1986. [Google Scholar]
Brittle 2009 {published data only}
- Brittle N, Patel S, Wright C, Baral S, Versfeld P, Sackley C. An exploratory cluster randomised controlled trial of group exercise on mobility and depression in care home residents. Clinical Rehabilitation 2009;23:146‐54. [DOI] [PubMed] [Google Scholar]
Bromby 2010 {published data only}
- Bromby S, Chandrasekara A. Study of the effect of physical activity on obese/overweight farm men and women on their psychological health and obesity related clinical co‐morbidities. Available from http://www.anzctr.org.au/ACTRN12610000827033.aspx (accessed May 2013). [ACTRN12610000827033]
Broocks 1997 {published data only}
- Broocks A, Meyer TF, George A, Pekrun G, Hillmer‐Vogel U, Hajak G, et al. Value of sports in treatment of psychiatric illness. Psychotherapie, Psychosomatik, Medizinische Psychologie 1997;47(11):379‐93. [PubMed] [Google Scholar]
Brown 1992 {published data only}
- Brown SW, Welsh MC, Labbé EE, Vitulli WE, Kulkarni P. Aerobic exercise in the psychological treatment of adolescents. Perceptual and Motor Skills 1992;74:555‐60. [DOI] [PubMed] [Google Scholar]
Burbach 1997 {published data only}
- Burbach FR. The efficacy of physical activity interventions within mental health services: anxiety and depressive disorders. Journal of Mental Health 1997;6:543‐66. [Google Scholar]
Burton 2009 {published data only}
- Burton NW, Pakenham KI, Brown WJ. Evaluating the effectiveness of psychosocial resilience training for heart health, and the added value of promoting physical activity: a cluster randomized trial of the READY program. BMC Public Health 2009;9:427. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carney 1987 {published data only}
- Carney RM, Templeton B, Hong BA, Harter HR, Hagberg JM, Schechtman KB, et al. Exercise training reduces depression and increases the performance of pleasant activities in haemodialysis patients. Nephron 1987;47:194‐8. [DOI] [PubMed] [Google Scholar]
Chalder 2012 {published data only}
- Baxter H, Winder R, Chalder M, Wright C, Sherlock S, Haase A, et al. Physical activity as a treatment for depression: the TREAD randomised trial protocol. Trials 2010;11:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalder M, Wiles NJ, Campbell J, Hollinghurst SP, Haase AM, Taylor AH, et al. et al. Facilitated physical activity as a treatment for depressed adults: a randomised controlled clinical trial. BMJ 2012;344:e2758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalder M, Wiles NJ, Campbell J, Hollinghurst SP, Searle A, Haase AM, et al. A pragmatic randomised controlled trial to evaluate the cost‐effectiveness of a physical activity intervention as a treatment for depression: The treating depression with physical activity (TREAD) trial. Health Technology Assessment 2012;16(10):1‐164. [DOI] [PubMed] [Google Scholar]
- Haase AM, Taylor AH, Fox KR, Thorp H, Lewis G. Rationale and development of the physical activity counselling intervention for a pragmatic TRial of Exercise and Depression in the UK (TREAD‐UK). Mental Health and Physical Activity 2010;3(2):85‐91. [Google Scholar]
- Searle A, Calnan M, Lewis G, Campbell J, Taylor A, Turner K. Patients' views of physical activity as treatment for depression: a qualitative study. British Journal of General Practice 2011;61(585):149‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Searle A, Calnan M, Turner KM, Lawlor DA, Campbell J, Chalder M, et al. General Practitioners' beliefs about physical activity for managing depression in primary care [ISRCTN16900744;TREAD UK]. Mental Health and Physical Activity 2012;5(1):13‐19. [Google Scholar]
Chan 2011 {published data only}
- Chan AS, Cheung M‐C, Tsui WJ, Sze SL, Shi D. Dejian mind‐body intervention on depressive mood of community‐dwelling adults: A randomised controlled trial. Evidence‐based Complementary and Alternative Medicine 2011:473961. [DOI] [PMC free article] [PubMed]
Chen 2009 {published data only}
- Chen KM, Chen MH, Chao HC, Hung HM, Lin HS, Li CH. Sleep quality, depression state, and health status of older adults after silver yoga exercises: cluster randomized trial. International Journal of Nursing Studies 2009;46(2):154‐63. [DOI] [PubMed] [Google Scholar]
Chou 2004 {published data only}
- Chou K‐L, Lee PWH, Yu ECS, MacFarlane D, Cheng Y‐H, Chan SSC, et al. Effect of Tai Chi on depressive symptoms amongst Chinese older patients with depressive disorders: a randomised clinical trial. International Journal of Geriatric Psychiatry 2004;19:1105‐7. [DOI] [PubMed] [Google Scholar]
Chow 2012 {published data only}
- Chow YWY, Dorcas A, Siu AMH. The effects of qigong on reducing stress and anxiety and enhancing body‐mind well‐being. Mindfulness 2012;3(1):51‐59. [Google Scholar]
Christensen 2012 {published data only}
- Christensen SB, Dall CH, Prescott E, Pedersen SS, Gustafsson F. A high‐intensity exercise program improves exercise capacity, self‐perceived health, anxiety and depression in heart transplant recipients: A randomised, controlled trial. Journal of Heart and Lung Transplantation 2012;31(1):106‐7. [DOI] [PubMed] [Google Scholar]
Ciocon 2003 {published data only}
- Ciocon JO, Galindo‐Ciocon D. Loneliness and depression in nursing home setting: the effect of a restorative program. International Psychogeriatrics [abstracts from The International Psychogeriatric Association 11th International Congress, Chicago, United States. 17‐22 August 2003]. 2003; Vol. 15:S027‐04.
Clegg 2011 {published data only}
- Clegg A, Barber S, Young J, Forster A, Iliffe S. The home‐based older people's exercise (HOPE) trial: study protocol for a randomised controlled trial. Trials (Electronic Resource) 2011; Vol. 12, issue 143. [DOI] [PMC free article] [PubMed]
Courneya 2007 {published data only}
- Courneya KS, Segal RJ, Gelmon K, Reid RD, Mackey JR, Friedenreich CM, et al. Six‐month follow‐up of patient‐related outcomes in a randomized controlled trial of exercise training during breast cancer chemotherapy. Cancer Epidemiology, Biomarkers and Prevention 2007;16(12):2572‐8. [DOI] [PubMed] [Google Scholar]
Dalton 1980 {published data only}
- Dalton RB. Effects of Exercise and Vitamin B12 Supplementation on the Depression Scale Scores of a Wheelchair Confined Population [dissertation]. Columbia, MO: University of Missouri, 1981. [Google Scholar]
Demiralp 2011 {published data only}
- Demiralp M, Oflaz F. The effect of relaxation training on symptoms of anxiety and depression in patients with breast cancer. TAF Preventive Medicine Bulletin 2011;10(2):165‐74. [Google Scholar]
Deslandes 2010 {published data only}
- Deslandes AC, Morales H, Alves H, Pompeu FAMS, Silveira, H, Mouta, R, et al. Effect of aerobic training on EEG alpha asymmetry and depressive symptoms in the elderly: A 1‐year follow‐up study. Brazilian Journal of Medical and Biological Research 2010;43(6):585‐92. [DOI] [PubMed] [Google Scholar]
DeVaney 1991 {published data only}
- DeVaney SB. Comparative Effects of Exercise Reduction and Relaxation Training on Type A Behaviour and Dysphoric Mood States in Habitual Aerobic Exercisers [dissertation]. Greensboro: University of North Carolina, 1991. [Google Scholar]
DiLorenzo 1999 {published data only}
- DiLorenzo TM, Bargman EP, Stucky‐Ropp R, Brassington GS, Frensch PA, LaFontaine T. Long‐term effects of aerobic exercise on psychological outcomes. Preventive Medicine 1999;28(1):75‐85. [DOI] [PubMed] [Google Scholar]
Eby 1985 {published data only}
- Eby JM. An Investigation into the Effects of Aerobic Exercise on Anxiety and Depression [dissertation]. Toronto, ON: University of Toronto, 1985. [Google Scholar]
Elavsky 2007 {published data only}
- Elavsky S, McAuley E. Lack of perceived sleep improvement after 4‐month structured exercise programs. Menopause 2007;14(3):535‐40. [DOI] [PubMed] [Google Scholar]
Emery 1990a {published data only}
- Emery CF, Blumenthal JA. Perceived change among participants in an exercise program for older adults. Gerontologist 1990;30(4):516‐21. [DOI] [PubMed] [Google Scholar]
Emery 1990b {published data only}
- Emery CF, Gatz M. Psychological and cognitive effects of an exercise program for community‐residing older adults. Gerontologist 1990;30(2):184‐8. [DOI] [PubMed] [Google Scholar]
Ersek 2008 {published data only}
- Ersek M, Turner JA, Cain KC, Kemp CA. Results of a randomized controlled trial to examine the efficacy of a chronic pain self‐management group for older adults. Pain 2009;138(1):29‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fitzsimmons 2001 {published data only}
- Fitzsimmons S. Easy rider wheelchair biking: a nursing‐recreation therapy clinical trial for the treatment of depression. Journal of Gerontological Nursing 2001;27:14‐23. [DOI] [PubMed] [Google Scholar]
Fox 2007 {published data only}
- Fox KR, Stathi A, McKenna J, Davis MG. Physical activity and mental well‐being in older people participating in the better ageing project. European Journal of Applied Physiology 2007;100:591‐602. [DOI] [PubMed] [Google Scholar]
Gary 2007 {published data only}
- Gary R, Lee SY. Physical function and quality of life in older women with diastolic heart failure: effects of a progressive walking program on sleep patterns. Progress in Cardiovascular Nursing 2007;22:72‐80. [DOI] [PubMed] [Google Scholar]
Ghroubi 2009 {published data only}
- Ghroubi S, Elleuch H, Chikh T, Kaffel N, Abid M, Elleuch MH. Physical training combined with dietary measures in the treatment of adult obesity. A comparison of two protocols. Annals of Physical and Rehabilitation Medicine 2009;52:394‐413. [DOI] [PubMed] [Google Scholar]
Gottlieb 2009 {published data only}
- Gottlieb SS, Kop WJ, Ellis SJ, Binkley P, Howlett J, O'Connor C, et al. Relation of depression to severity of illness in heart failure (from heart failure and a controlled trial investigating outcomes of exercise training [HF‐ACTION]). American Journal of Cardiology 2009;103:1285‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gusi 2008 {published data only}
- Gusi N, Reyes MC, Gonzalez‐Guerrero JL, Herrera E, Garcia JM. Cost‐utility of a walking programme for moderately depressed, obese, or overweight elderly women in primary care: a randomised controlled trial. BMC Public Health 2008;8:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gustafsson 2009 {published data only}
- Gustafsson G, Lira CM, Johansson J, Wisén A, Wohlfart, Ekman R, et al. The acute response of plasma brain‐derived neurotrophic factor as a result of exercise in major depressive disorder. Psychiatry Research 2009;169:244‐8. [DOI] [PubMed] [Google Scholar]
Gutierrez 2012 {published data only}
- Villaverde Gutierrez C, Torres Luque G, Medina, Ábalos Medina GM, Argente del Castillo MJ, Guisado IM, Guisado Barrilao R, et al. Influence of exercise on mood in postmenopausal women. Journal of Clinical Nursing 2012;21(7‐8):923‐28. [DOI] [PubMed] [Google Scholar]
Haffmans 2006 {published data only}
- Haffmans PMJ, Kleinsman ACM, Weelden C, Huijbrechts IPAM, Hoencamp E. Comparing running therapy with physiotraining therapy in the treatment of mood disorders. Acta Neuropsychiatrica 2006;18:173‐6. [DOI] [PubMed] [Google Scholar]
Hannaford 1988 {published data only}
- Hannaford CP, Harrell EH, Cox K. Psychophysiological effects of a running program on depression and anxiety in a psychiatric population. Psychological Record 1988;38:37‐48. [Google Scholar]
Haugen 2007 {published data only}
- Haugen TS, Stavem K. Rehabilitation in a warm versus a colder climate in chronic obstructive pulmonary disease. Journal of Cardiopulmonary Rehabilitation and Prevention 2007;27:50‐6. [DOI] [PubMed] [Google Scholar]
Hedayati 2012 {published data only}
- Hedayati SS, Yalamanchili, Finkelstein FO. A practical approach to the treatment of depression in patients with chronic kidney disease and end‐stage renal disease. Kidney International 2012;81(3):247‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hembree 2000 {published data only}
- Hembree LD. Exercise and its Effect on Hopelessness and Depression in an Aging Female Population in Eastern Oklahoma [dissertation]. Fayetteville: University of Arkansas, 2001. [Google Scholar]
Herrera 1994 {published data only}
- Herrera F. Efficacy of a psychological intervention for depression in patients on haemodialysis [Eficacia de la intervención psicológica en la depresión del paciente en hemodiálisis]. Psiquis 1994;15(4):175‐8. [Google Scholar]
Hughes 1986 {published data only}
- Hughes JR, Casal DC, Leon AS. Psychological effects of exercise: a randomised cross‐over trial. Journal of Psychosomatic Research 1986;30:355‐60. [DOI] [PubMed] [Google Scholar]
Hughes 2009 {published data only}
- Hughes CW, Trivedi MH, Cleaver J, Greer TL, Emslie GJ, Kennard B, et al. DATE: Depressed adolescents treated with exercise: study rationale and design for a pilot study. Mental Health and Physical Activity 2009;2:76‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Immink 2011 {published data only}
- Immink MA, Hillier SL. Yoga for chronic post‐stroke hemiparesis: A pilot randomised controlled trial. International Journal of stroke. 2011; Vol. Abstract of the 22nd Stroke Society of Australasia Annual Scientific Meeting.
Jacobsen 2012 {published data only}
- Jacobsen P, Phillips K, Jim H, Faul LA, Small B, Meade C, et al. Self‐directed stress management and exercise training for cancer chemotherapy patients. Psycho‐Oncology (abstracts of the 9th Annual Conference of the American Psychosocial Oncology Society). 2012; Vol. 21:17.
Johansson 2011 {published data only}
- Johansson M, Hassmen P, Jouper J. Acute effects of Qigong exercise on mood and anxiety. Sport, Exercise and Performance Psychology 2011;15(2):199‐207. [Google Scholar]
Karlsson 2007 {published data only}
- Karlsson MR, Edström‐Plüss C, Held C, Henriksson P, Billing E, Wallén NH. Effects of expanded cardiac rehabilitation on psychosocial status in coronary artery disease with focus on type D characteristics. Journal of Behavioral Medicine 2007;30:253‐61. [DOI] [PubMed] [Google Scholar]
Kerr 2008 {published data only}
- Kerr J, Patrick K, Norman G, Stein MB, Calfas K, Zabinski M, et al. Randomized control trial of a behavioral intervention for overweight women: impact on depressive symptoms. Depression and Anxiety 2008;25:555‐8. [DOI] [PubMed] [Google Scholar]
Kerse 2010 {published data only}
- Kerse N, Hayman KJ, Moyes SA, Peri K, Robinson E, Dowell A, et al. Home‐based activity program for older people with depressive symptoms: DeLLITE ‐ a randomized controlled trial. Annals of Family Medicine 2010;8:214‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2004 {published data only}
- Kim KB, Cohen SM, Oh HK, Sok SR. The effects of meridian exercise on anxiety, depression and self‐esteem of female college students in Korea. Holistic Nursing Practice 2004;18:230‐4. [DOI] [PubMed] [Google Scholar]
Knapen 2003 {published data only}
- Knapen J, Vliet P, Coppenolle H, David A, Peuskens J, Knapen K, et al. The effectiveness of two psychomotor therapy programmes on physical fitness and physical concept in nonpsychotic psychiatric patients: a randomised controlled trial. Clinical Rehabilitation 2003;17:637‐47. [DOI] [PubMed] [Google Scholar]
Knapen 2006 {published data only}
- Knapen J, Coppenolle H, Peuskens J, Pieters G, Knapen K. Comparison of changes in physical fitness, physical self‐concept, global self‐esteem, depression and anxiety following two different psychomotor therapy programs in non‐psychotic psychiatric inpatients. The Concept of Self in Education, Family and Sports. Nova, 2006:Chapter 4. [Google Scholar]
Kubesh 2003 {published data only}
- Kubesch S, Bretschneider V, Freudenmann R, Weiderhammer N, Lehmann M, Spitzer M, et al. Aerobic endurance exercise improves executive function in depressed patients. Journal of Clinical Psychiatry 2003;64:1005‐12. [DOI] [PubMed] [Google Scholar]
Kulcu 2007 {published data only}
- Kulcu DG, Kurtais Y, Tur BS, Gülec S, Seckin B. The effect of cardiac rehabilitation on quality of life, anxiety and depression in patients with congestive heart failure. A randomized controlled trial, short‐term results. Europa Medicophysica 2007;43:489‐97. [PubMed] [Google Scholar]
Kupecz 2001 {published data only}
- Kupecz DB. Effects of a Structured Exercise Program in Older Veteran Patients [dissertation]. Greely, CO: University of Northern Colorado, 2001. [Google Scholar]
Labbe 1988 {published data only}
- Labbe EE, Welsh MC, Delaney D. Effects of consistent aerobic exercise on the psychological functioning of women. Perceptual and Motor Skills 1988;67(3):919‐25. [DOI] [PubMed] [Google Scholar]
Lacombe 1988 {published data only}
- Lacombe JB. The Role of Aerobic Conditioning and Psychosocial Factors in Mediating the Effect of Exercise on Depression [dissertation]. Hempstead, NY: Hofstra University, 1987. [Google Scholar]
Lai 2006 {published data only}
- Lai SM, Studenski S, Richards L, Perera S, Reker D, Rigler S, et al. Therapeutic exercise and depressive symptoms after stroke. Journal of the American Geriatrics Society 2006;54(2):240‐7. [DOI] [PubMed] [Google Scholar]
Latimer 2004 {published data only}
- Latimer AE, Martin Ginis KA, Hicks AL, McCartney N. An examination of the mechanisms of exercise‐induced change in psychological well‐being among people with spinal cord injury. Journal of Rehabilitation Research and Development 2004;41(5):643‐51. [DOI] [PubMed] [Google Scholar]
Lautenschlager 2008 {published data only}
- Lautenschlager NT, Cox KL, Flicker L, Foster JK, Bockxmeer FM, Xiao J, et al. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease. JAMA 2008;300(9):1027‐37. [DOI] [PubMed] [Google Scholar]
Lavretsky 2011 {published data only}
- Lavretsky H, Alstein LL, Olmstead RE, Ercoli LM, Riparetti‐Brown M, Cyr NS, et al. Complementary use of tai chi chih augments escitalopram treatment of geriatric depression: A randomized controlled trial. American Journal of Geriatric Psychiatry 2011;19(10):839‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Legrand 2009 {published data only}
- Legrand FD, Mille CR. The effects of 60 minutes of supervised weekly walking (in a single vs. 3‐5 session format) on depressive symptoms among older women: findings from a pilot randomized trial. Mental Health and Physical Activity 2009;2:71‐5. [Google Scholar]
Leibold 2010 {published data only}
- Leibold ML. Activites and adaptive strategies in late life depression: A qualitative study [thesis]. Dissertation Abstracts International: Section B: The Sciences and Engineering 2011; Vol. 71, issue 9‐B:5425.
Leppämäki 2002 {published data only}
- Leppämäki S, Haukka J, Lönnqvist J, Partonen T. Drop‐out and mood improvement: a randomised controlled trial with light exposure and physical exercise. BMC Psychiatry 2004;4:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppämäki SJ, Partonen TT, Hurme J, Haukka JK, Lonnqvist JK. Randomised trial of the efficacy of bright‐light exposure and aerobic exercise on depressive symptoms and serum lipids. Journal of Clinical Psychiatry 2002;63(4):316‐21. [PubMed] [Google Scholar]
Levendoglu 2004 {published data only}
- Levendoğlu F, Altintepe L, Okudan N, Uğurlu H, Gökbel H, Tonbul Z, et al. A twelve exercise program improves the psychological status, quality of life and work capcity in hemodialysis patients. Journal of Nephrology 2004;17:826‐32. [PubMed] [Google Scholar]
Lever‐van Milligen 2012 {published data only}
- Lever‐van Milligen B. Mood treatment with antidepressants or running (MOTAR). http://www.trialregister.nl/admin/rctview.asp?TC=3460 June 2012. [NTR 3460] [DOI] [PMC free article] [PubMed]
Levinger 2011 {published data only}
- Levinger I, Selig S, Goodman C, Jerums G, Stewart A, Hare DL. Resistance training improves depressive symptoms in individuals at high risk for type 2 diabetes. Journal of Strength and Conditioning Research 2011;25(8):2328‐33. [DOI] [PubMed] [Google Scholar]
Lin 2007 {published data only}
- Lin MR, Wolf SL, Hwang HF, Gong SY, Chen CY. A randomized, controlled trial of fall prevention programs and quality of life in older fallers. Journal of the American Geriatrics Society 2007;55:499‐506. [DOI] [PubMed] [Google Scholar]
Littbrand 2011 {published data only}
- Littbrand H, Carlsson M, Lundin‐Olsson L, Lindelof N, Haglin L, Gustafson Y, et al. Effect of a high‐intensity functional exercise program on functional balance: Preplanned subgroup analyses of a randomized controlled trial in residential care facilities. Journal of the American Geriatrics Society 2011;59(7):1274‐82. [DOI] [PubMed] [Google Scholar]
Lolak 2008 {published data only}
- Lolak S, Conors GL, Sherican MJ, Wise TN. Effects of progressive muscle relaxation training on anxiety and depression in patients enrolled in an outpatient pulmonary rehabilitation program. Psychotherapy and Pyschosomatics 2008;77(2):119‐25. [DOI] [PubMed] [Google Scholar]
Machado 2007 {published data only}
- Machado LAC, Azevedo DC, Capanema MB, Neto TN, Cerceau DM. Client‐centered therapy vs exercise therapy for chronic low back pain: a pilot randomized controlled trial in Brazil. Pain Medicine 2007;8(3):251‐8. [DOI] [PubMed] [Google Scholar]
MacMahon 1988 {published data only}
- MacMahon JR, Gross RT. Physical and psychological effects of aerobic exercise in delinquent adolescent males. American Journal of Diseases of Children 1988;142:1361‐6. [DOI] [PubMed] [Google Scholar]
Mailey 2010 {published data only}
- Mailey EL, Wojcicki TR, Moti RW, Hu L, Strauser DR, Collins KD, et al. Internet‐delivered physical activity intervention for college students with mental health disorders: a randomised pilot trial. Psychology Health and Medicine 2010;15(6):646‐59. [DOI] [PubMed] [Google Scholar]
Martin 2009 {published data only}
- Martin JK, Church TS, Thompson AM, Earnest CP, Blair SN. Exercise dose and quality of life. Archives of Internal Medicine 2009;169(3):269‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martinsen 1988a {published data only}
- Martinsen EW. Exercise intervention studies in patients with anxiety and depressive disorders. Proceedings of Sport, Health Psychology and Exercise Symposium. London: Sports Council and Health Education Authority, 1988:77‐83.
Martinsen 1988b {published data only}
- Martinsen EW. Comparing aerobic and non‐aerobic forms of exercise in the treatment of clinical depression: a randomised trial. Proceedings of Sport, Health Psychology and Exercise Symposium. London: Sports Council and Health Education Authority, 1988:84‐95.
Martinsen 1989c {published data only}
- Martinsen EW. Aerobic exercise in the treatment of nonpsychotic mental disorders: an exploratory study. Nordic Journal of Psychiatry 1989;43:521‐9. [Google Scholar]
Martinsen 1993 {published data only}
- Martinsen EW. Therapeutic implications of exercise for clinically anxious and depressed patients. International Journal of Sport Psychology 1993;24:185‐99. [Google Scholar]
Matthews 2011 {published data only}
- Matthews MM, Hsu FC, Walkup MP, Barry LC, Patel KV, Blair SN. Depressive symptoms and physical performance in the lifestyle interventions and independence for elders pilot study. Journal of the American Geriatrics Society 2011;59(3):495‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
McClure 2008 {published data only}
- McClure JB, Catz SL, Ludman EJ, Richards J, Riggs K, Grothaus L. Feasibility and acceptability of a multiple risk factor intervention: the Step Up randomized pilot trial. BMC Public Health 2011;11(167):doi:10.1186/1471‐2458‐11‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT00644995. Step up wellness program for depression, physical inactivity, and smoking. ClinicalTrials.gov (http//www.clinicaltrials.gov) (accessed 2008). [NCT00644995]
Midtgaard 2011 {published data only}
- Midtgaard J, Stage M, Moller T, Andersen C, Quist M, Rorth M, et al. Exercise may reduce depression but not anxiety in self‐referred cancer patients undergoing chemotherapy. Post‐hoc analysis of data from the 'Body & Cancer' trial. Acta Oncologia 2011;50(5):660‐9. [DOI] [PubMed] [Google Scholar]
Milani 2007 {published data only}
- Milani RV, Lavie CJ. Impact of cardiac rehabilitation on depression and its associated mortality. American Journal of Medicine 2007;120:799‐806. [DOI] [PubMed] [Google Scholar]
Morey 2003 {published data only}
- Morey MC, Dubbert PM, Doyle ME, MacAller H, Crowley GM, Kuchibhatla M, et al. From supervised to unsupervised exercise: factors associated with exercise adherence. Journal of Aging and Physical Activity 2003;11(3):351‐68. [Google Scholar]
Motl 2004 {published data only}
- Motl RW, Konopack JF, McAuley E, Elavasky S, Jerome GJ, Marquez DX. Depressive symptoms among older adults: long‐term reduction after a physical activity intervention. Journal of Behavioral Medicine 2005;28(4):384‐94. [DOI] [PubMed] [Google Scholar]
Mudge 2008 {published data only}
- Mudge A. The impact of a disease management programme including a supervised exercise programme versus disease management alone on death, readmissions, depression and functional status on patients with a recent hospitalisation for heart failure. Australian New Zealand Clinical Trials Registry 2008.
Munro 1997 {published data only}
- Munro J, Brazier J, Davey R, Nicholl J. Physical activity for the over‐65s: could it be a cost‐effective exercise for the NHS?. Journal of Public Health Medicine 1997;19(4):397‐402. [DOI] [PubMed] [Google Scholar]
Mutrie 2007 {published data only}
- Mutrie N, Campbell AM, Whyte F, McConnachie A, Emslie C, Lee L, et al. Benefits of supervised group exercise programme for women being treated for early stage breast cancer: pragmatic randomised controlled trial. BMJ 2007;334(7592):517. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT00416221 {published data only}
- NCT00416221. Development and a pilot study of the PACEPRO exercise and mood management program in depressed patients on escitalopram oxalate (Lexapro). http://clinicaltrials.gov/show/NCT00416221 (accessed 2008). [NCT 00416221]
NCT00546221 {published data only}
- NCT00546221. Pragmatic randomised controlled trial of a preferred intensity exercise programme to improve physiological and associated psychological, social, and wellbeing outcomes of women living with depression. ClinicalTrials.gov (http://www.clinicaltrials.gov) 2007. [NCT00546221]
NCT00964054 {published data only}
- NCT00964054. Adapting exercise treatment for depression to adolescents: a pilot study [NCT00964054]. http://clinicaltrials.gov/show/NCT00964054 (accessed 1 March 2013). [NCT00964054]
NCT01152086 {published data only}
- NCT01152086. The effects of regular mountain hiking on hopelessness in chronically suicidal patients. ClinicalTrials.gov (http://www.clinicaltrials.gov) (accessed 1st March 2013). [NCT01152086]
Neidig 1998 {published data only}
- Neidig JL. Aerobic Exercise Training: Effects on Depressive Symptoms in HIV Infected Adults (Immune Deficiency, Exercise Training) [dissertation]. Columbus, OH: The Ohio State University, 1998. [Google Scholar]
- Neidig JL, Smith BA, Brashers DE. Aerobic exercise training for depressive symptom management in adults living with HIV infection. Journal of Association of Nurses in AIDS Care 2003;14(2):30‐40. [DOI] [PubMed] [Google Scholar]
- Smith BA, Neidig JL, Nickel JT, Mitchell GL, Para MF, Fass RJ. Aerobic exercise: effects on parameters related to fatigue, dyspnea, weight and body composition in HIV‐infected adults. AIDS 2001;15(6):693‐701. [DOI] [PubMed] [Google Scholar]
Netz 1994 {published data only}
- Netz Y, Yaretzki A, Salganik I, Jacob T, Finkeltov B, Argov E. The effect of supervised physical activity on cognitive and affective state of geriatric and psychogeriatric in‐patients. Clinical Gerontologist 1994;15(1):47‐56. [Google Scholar]
Neuberger 2007 {published data only}
- Neuberger GB, Aaronson LS, Gajewski B, Embretson SE, Cagle PE, Loudon JK, et al. Predictors of exercise and effects of exercise on symptoms, function, aerobic fitness, and disease outcomes of rheumatoid arthritis. Arthritis and Rheumatism 2007;57(6):943‐52. [DOI] [PubMed] [Google Scholar]
Nguyen 2001 {published data only}
- Nguyen HQ, Carrieri‐Kohlman V, Demir‐Deviren S, Stulbarg MS. Are the improvements in fatigue, vigor and depression sustained with a home walking programme?. Proceedings of the American Thoracic Society 2001 International Conference; May 18‐23; San Francisco, California. 2001.
O'Neil 2011 {published data only}
- O'Neil A, Hawkes AL, Chan B, Sanderson K, Forbes A, Hollingsworth B, et al. A randomised, feasibility trial of a tele‐health intervention for Acute Coronary Syndrome patients with depression ('Moodcare') : Study protocol. BMC Cardiovascular Disorders 2011 25th Feb [Epub ahead of print]; Vol. 11, issue 8. [DOI: 10.1186/1471-2261-11-8] [DOI] [PMC free article] [PubMed]
Oeland 2010 {published data only}
- Oeland AM, Laessoe U, Olesen AV, Munk‐Jorgensen P. Impact of exercise on patients with depression and anxiety. Nordic Journal of Pyschiatry 2010;64(3):210‐7. [DOI] [PubMed] [Google Scholar]
Oretzky 2006 {published data only}
- Oretzky S. The Effects of Yoga on Elevated Depressive and Somatic Symptoms in Young Adults [dissertation]. California School of Professional Psychology, Alliant International University 2006.
Ouzouni 2009 {published data only}
- Ouzouni S, Kouidi E, Grekas D, Deligiannis A. Effect of intradialytic exercise training on health‐related quality of life indices in haemodialysis patient. Clinical Rehabilitation 2009;23:53‐63. [DOI] [PubMed] [Google Scholar]
Pakkala 2008 {published data only}
- Pakkala I, Read S, Leinonen R, Hirvensalo M, Lintunen T, Rantanen T. The effects of physical activity counseling on mood among 75‐ to 81‐year‐old people: a randomized controlled trial. Preventive Medicine 2008;46:412‐8. [DOI] [PubMed] [Google Scholar]
Palmer 2005 {published data only}
- Palmer JA, Michiels K, Thigpen B. Effects of type of exercise on depression in recovering substance abusers. Perceptual and Motor Skills 1995;80(2):523‐30. [DOI] [PubMed] [Google Scholar]
Passmore 2006 {published data only}
- Passmore T, Lane S. Exercise as a treatment for depression: a therapeutic recreation intervention. American Journal of Recreation Therapy 2006;5(3):31‐41. [Google Scholar]
Peacock 2006 {published data only}
- Peacock J. A feasibility study to analyse the psychosocial benefits of green exercise (GE) in comparison with cognitive behavioural therapy (CBT) with patients with mild to moderate depression. www.controlled‐trials.com 2007.
Pelham 1993 {published data only}
- Pelham TW, Compagna PD, Ritvo PG, Birnnie WA. The effects of exercise therapy on clients in a psychiatric rehabilitation program. Psychosocial Rehabilitation Journal 1993;16(4):75‐83. [Google Scholar]
Penninx 2002 {published data only}
- Ettinger WH Jr, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA 1997;277(1):25‐31. [PubMed] [Google Scholar]
- Penninx BWJH, Rejeski WJ, Pandya J, Miller ME, Bari MD, Applegate WB, et al. Exercise and depressive symptoms: a comparison on aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 2002;57(2):124‐32. [DOI] [PubMed] [Google Scholar]
Penttinen 2011 {published data only}
- Pentinnen HM, Saarto T, Kellokumpu‐Lehtinen P, Blomqvist C, Huovinen R, Kautiainen H, et al. Quality of life and physical performance and activity of breast cancer patients after adjuvant treatments. Psycho‐Oncology 2011;20(11):1211‐20. [DOI] [PubMed] [Google Scholar]
Perna 2010 {published data only}
- Perna FM, Craft L, Freund KM, Skrinar G, Stone M, Kachnic L, et al. The effect of a cognitive behavioral exercise intervention on clinical depression in a multiethnic sample of women with breast cancer: A randomized controlled trial. International Journal of Sport and Exercise Psychology 2010;8(1):36‐47. [Google Scholar]
Perri 1984 {published data only}
- Perri S 2nd, Temper DL. The effects of an aerobic exercise programme on psychological variables in older adults. International Journal of Aging and Human Development 1984;20(3):1984‐5. [DOI] [PubMed] [Google Scholar]
Piette 2011 {published data only}
- Piette JD, Valenstein M, Himle J, Duffy S, Torres T, Vogel M, et al. Clinical complexity and the effectiveness of an intervention for depressed diabetes patients. Chronic Illness 2011;7(4):267‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Raglin 1990 {published data only}
- Raglin JS. Exercise and mental health. Beneficial and detrimental effects. Sports Medicine 1990;9(6):323‐9. [DOI] [PubMed] [Google Scholar]
Rhodes 1980 {published data only}
- Rhodes DL. Mens Sana Corpore Sano: A Study of the Effect of Jogging on Depression Anxiety and Self Concept [dissertation]. Durham, NC: Duke University, 1980. [Google Scholar]
Robledo Colonia 2012 {published data only}
- Robledo Colonia AF, Sandoval Restrepo N, Mosquera Valderrama YF, Escobar Hurtado C, Ramirez Velez R. Aerobic exercise training during pregnancy reduces depressive symptoms in nulliparous women: a randomised trial. Journal of Physiotherapy 2012;58(1):9‐15. [DOI] [PubMed] [Google Scholar]
Rofey 2008 {published data only}
- Rofey DL, Szigethy EM, Noll RB, Dahl RE, Lobst E, Arslanian SA. Cognitive‐behavioral therapy for physical and emotional disturbances in adolescents with polycystic ovary syndrome: a pilot study. Journal of Pediatric Psychology 2009;34(2):156‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roshan 2011 {published data only}
- Roshan VD, Pourasghar M, Mohammadian Z. The efficacy of intermittent walking in water on the rate of MHPG sulfate and the severity of depression. Iranian Journal of Psychiatry 2011;5(2):26‐31. [PMC free article] [PubMed] [Google Scholar]
Roth 1987 {published data only}
- Roth DL, Holmes DS. Influence of aerobic exercise training and relaxation training on physical and psychologic health following stressful life events. Psychosomatic Medicine 1987;49(4):355‐65. [DOI] [PubMed] [Google Scholar]
Ruunsunen 2012 {published data only}
- Ruunsunen A, Voutilainen S, Karhunen L, Lehto SM, Tolmunen T, Keinanen‐Kiukaanniemi S, et al. How does lifestyle intervention affect depressive symptoms? Results from the Finnish Diabetes Prevention Study. Diabetic Medicine 2012;29(7):e126‐e132. [DOI] [PubMed] [Google Scholar]
Salminen 2005 {published data only}
- Salminen M, Isoaho R, Vahlberg T, Ojanlatva A, Kivela SL. Effects of a health advocacy, counselling, and activation programme on depressive symptoms in older coronary heart disease patients. International Journal of Geriatric Psychiatry 2005;20(6):552‐8. [DOI] [PubMed] [Google Scholar]
Salmon 2001 {published data only}
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clinical Psychology Review 2001;21(1):33‐61. [DOI] [PubMed] [Google Scholar]
Sarsan 2006 {published data only}
- Sarsan A, Ardiç F, Özgen M, Topuz O. The effects of aerobic and resistance exercises in obese women. Clinical Rehabilitation 2006;20:773‐82. [DOI] [PubMed] [Google Scholar]
Schwarz 2012 {published data only}
- Schwarz MJ, Hennings A, Riemer S, Stapf T, Selberdinger V, Gil FP, et al. Effect of physical exercise on psychoneuruoimmunological parameters in patients with depression and patients with somatoform disorder. Neurology Psychiatry and Brain Research [abstracts of the 11th Psychoimmunology Expert Meeting]. 2012.
Sexton 1989 {published data only}
- Sexton H, Maere A, Dahl NH. Exercise intensity and reduction in neurotic symptoms. A controlled follow‐up study. Acta Psychiatrica Scandinavica 1989;80(3):231‐5. [DOI] [PubMed] [Google Scholar]
Silveira 2010 {published data only}
- Silveira H, Deslandes AC, Moraes H, Mouta R, Ribeiro P, Piedade R, et al. Effects of exercise on electrocencephalographic mean frequency in depressed elderly subjects. Neuropsychobiology 2010;61(3):141‐7. [DOI] [PubMed] [Google Scholar]
Sims 2006 {published data only}
- Sims J, Hill K, Davidson S, Gunn J, Huang N. Exploring the feasibility of a community‐based strength training program for older people with depressive symptoms and its impact on depressive symptoms. BMC Geriatrics 2006;6:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Skrinar 2005 {published data only}
- Skrinar GS, Huxley NA, Hutchinson DS, Menninger E, Glew P. The role of a fitness intervention on people with serious psychiatric disabilities. Psychiatric Rehabilitation Journal 2005;29(2):122‐7. [DOI] [PubMed] [Google Scholar]
Smith 2008 {published data only}
- Smith PS, Thompson M. Treadmill training post stroke: are there any secondary benefits? A pilot study. Clinical Rehabilitation 2008;22:997‐1002. [DOI] [PubMed] [Google Scholar]
Sneider 2008 {published data only}
- Sneider KL, Bodenlos JS, Ma Y, Olendzki B, Oleski J, Merriam P, et al. Design and methods for a randomised clinical trial treating comorbid obesity and major depressive disorder. BMC Pyschiatry 2008;8:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Songoygard 2012 {published data only}
- Songoygard KM, Stafne SN, Evensen KAI, Salvesen KA, Vik T, Morkved S. Does exercise during pregnancy prevent postnatal depression?: A randomized controlled trial. Acta Obstetricia et Gynecologica Scandinavica 2012;91(1):62‐7. [DOI] [PubMed] [Google Scholar]
Stein 1992 {published data only}
- Stein PN, Motta RW. Effects of aerobic and nonaerobic exercise on depression and self‐concept. Perceptual and Motor Skills 1992;74(1):79‐89. [DOI] [PubMed] [Google Scholar]
Stern 1983 {published data only}
- Stern MJ, Gorman PA, Kaslow L. The group counseling v exercise therapy study. A controlled intervention with subjects following myocardial infarction. Archives of Internal Medicine 1983;143(9):1719‐25. [PubMed] [Google Scholar]
- Stern MJ, Plionis E, Kaslow L. Group process expectations and outcome with post‐myocardial infarction patients. General Hospital Psychiatry 1984;6(2):101‐8. [DOI] [PubMed] [Google Scholar]
Strömbeck 2007 {published data only}
- Strömbeck BE, Theander E, Jacobsson LTH. Effects of exercise on aerobic capacity and fatigue in women with primary Sjögren's syndrome. Rheumatology 2007;46:868‐71. [DOI] [PubMed] [Google Scholar]
Sung 2009 {published data only}
- Sung K. The effects of 16‐week group exercise program on physical function and mental health of elderly Korean women in long‐term assisted living facility. Journal of Cardiovascular Nursing 2009;24(5):344‐51. [DOI] [PubMed] [Google Scholar]
Tapps 2009 {published data only}
- Tapps T. An Investigation into the Effects of Resistance Exercise Participation on the Perceived Depression Levels of Older Adults Residing in a Long‐Term Care Facility Over Time [dissertation]. Oklahoma State University, 2009. [Google Scholar]
Taylor 1986 {published data only}
- Taylor CB, Houston Miller N, Ahn DK, Haskell W, DeBusk RF. The effects of exercise training programmes on psychosocial improvement in uncomplicated postmyocardial infarction patients. Journal of Psychosomatic Research 1986;30(5):581‐7. [DOI] [PubMed] [Google Scholar]
Tenorio 1986 {published data only}
- Tenorio LM. Effects of Aerobic Exercise on Symptoms of Depression in Women [dissertation]. Denton, TX: Texas Woman's University, 1986. [Google Scholar]
Thomson 2010 {published data only}
- Thomson RL, Buckley JD, Lim SS, Noakes M, Clifton PM, Norman RJ, et al. Lifestyle management improves quality of life and depression in overweight and obese women with polycystic ovary syndrome. Fertility and Sterility 2010;94(5):1812‐6. [DOI] [PubMed] [Google Scholar]
Tomas‐Carus 2008 {published data only}
- Tomas‐Carus P, Gusi N, Häkkinen A, Häkkinen K, Leal A, Ortega‐Alonso A. Eight months of physical training in warm water improves physical and mental health in women with fibromyalgia: a randomized controlled trial. Journal of Rehabilitation Medicine 2008;40:248‐52. [DOI] [PubMed] [Google Scholar]
TREAD 2003 {published data only}
- National Institute of Mental Health (NIMH). Treatment With Exercise Augmentation for Depression (TREAD). ClinicalTrials.gov (http://www.clinicaltrials.gov) 2003. [NCT00076258]
- Trivedi MH, Greer TL, Grannemann BD, Church TS, Galper DI, Sunderajan P, et al. TREAD: TReatment with Exercise Augmentation for Depression: study rationale and design. Clinical Trials 2006;3(3):291‐305. [DOI] [PubMed] [Google Scholar]
Trivedi 2011 {published data only}
- Trivedi MH, Greer TL, Church TS, Carmody TJ, Grannemann BD, Galper DI, et al. Exercise as an augmentation treatment for nonremitted major depressive disorder: a randomized, parallel dose comparison. Journal of Clinical Psychiatry 2011;72(5):677‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsang 2003 {published data only}
- Tsang HWH, Mok CK, Au Yeung YT, Chan SYC. The effect of Qigong on general and psychosocial health of elderly with chronic physical illnesses: a randomised clinical trial. International Journal of Geriatric Psychiatry 2003;18(5):441‐9. [DOI] [PubMed] [Google Scholar]
Tsang 2006 {published data only}
- Tsang HWH, Fung KMT, Chan ASM, Lee G, Chan F. Effect of qigong exercise programme on elderly with depression. International Journal of Geriatric Psychiatry 2006;21:890‐7. [DOI] [PubMed] [Google Scholar]
Underwood 2013 {published data only}
- Ellard DR, Taylor SJ, Parsons S, Thorogood M. The OPERA trial: a protocol for the process evaluation of a randomised trial of an exercise intervention for older people in residential and nursing accommodation. Trials 2011;12:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Underwood M, Lamb SE, Eldridge S, Sheehan B, Slowther A, Spencer A, et al. Exercise for depression in care home residents: a randomised controlled trial with cost effectiveness analysis (OPERA). Health Technology Assessment May 2013;17(18):1‐281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Underwood M, Lamb SE, Eldridge S, Sheehan B, Slowther A‐M, Spencer A, et al. Exercise for depression in elderly residents of care homes: a cluster‐randomised controlled trial. Lancet 2013;382(9886):41‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Underwood M, Eldridge S, Lamb S, Potter R, Sheehan B, Slowther AM, et al. The OPERA trial: protocol for a randomised trial of an exercise intervention for older people in residential and nursing accommodation. Trials 2011;12:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van der Merwe 2004 {published data only}
- Merwe I, Naude S. Exercise and depression: a treatment manual. Health SA Gesondheid 2004;9(4):28‐41. [Google Scholar]
Van de Vliet 2003 {published data only}
- Vliet P, Onghena P, Knapen J, Fox KR, Probst M, Coppenolle H, et al. Assessing the additional impact of fitness training in depressed psychiatric patients receiving multifaceted treatment: a replicated single‐subject design. Disability and Rehabilitation 2003;25(24):1344‐53. [DOI] [PubMed] [Google Scholar]
Vickers 2009 {published data only}
- Vickers KS, Patten CA, Lewis BA, Clark MM, Ussher M, Ebbert JO, et al. Feasibility of an exercise counseling intervention for depressed women smokers. Nicotine & Tobacco Research 2009;11(8):985‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weinstein 2007 {published data only}
- Weinstein AA, Deuster PA, Kop WJ. Heart rate variability as a predictor of negative mood symptoms induced by exercise withdrawal. Medicine and Science in Sports and Exercise 2007;39(4):735‐41. [DOI] [PubMed] [Google Scholar]
Weiss 1989 {published data only}
- Weiss CR, Jamieson NB. Women, subjective depression, and water exercise. Health Care for Women International 1989;10(1):75‐88. [DOI] [PubMed] [Google Scholar]
White 2007 {published data only}
- White PD, Sharpe MC, Chalder T, DeCesare JC, Walwyn R, PACE trial group. Protocol for the PACE trial: a randomised controlled trial of adaptive pacing, cognitive behaviour therapy, and graded exercise as supplements to standardised specialist medical care versus standardised specialist medical care alone for patients with the chronic fatigue syndrome/myalgic encephalomyelitis or encephalopathy. BMC Neurology 2007;7:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whitham 2011 {published data only}
- Whitham EA, Thommi SB, Holtzman NS, Ostacher MM, El‐Mallakh RS, Baldassano CF, et al. Rapid cycling and antidepressants: Data from a STEP‐BD randomized clinical trial. Bipolar Disorders [abstracts from the 9th International Conference on Bipolar Disorder]. 2011; Vol. 13:s1.
Wieman 1980 {published data only}
- Wieman JB. Running as a Treatment for Depression: A Theoretical Basis [dissertation]. Fresno, CA: California School of Professional Psychology, 1980. [Google Scholar]
Wilbur 2009 {published data only}
- Wilbur J, Zenk S, Wang E, Oh A, McDevitt J, Block D, et al. Neighborhood characteristics, adherence to walking, and depressive symptoms in midlife African American women. Journal of Women's Health 2009;18(8):1201‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 1992 {published data only}
- Williams VL. Acute Mood and EEG Effects of Aerobic Exercise in Depressed and Non‐Depressed Adults [dissertation]. Birmingham, AL: The University of Alabama, 1992. [Google Scholar]
Wipfli 2008 {published data only}
- Wipfli BM. Serotonin and Psychological Variables in the Relationship Between Exercise and Mental Health [dissertation]. Arizona State University, 2008. [DOI] [PubMed] [Google Scholar]
Wipfli 2011 {published data only}
- Wipfli B, Landers D, Nagoshi C, Ringenbach S. An examination of serotonin and psychological variables in the relationship between exercise and mental health. Scandinavian Journal of Medicine & Science in Sports 2011;21(3):474‐81. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Aghakhani 2011 {published data only}
- Aghakhani N, Sharif F, Khademvatan K, Rahbar N, Eghtedar S, Shojaei Motlagh V. The reduction in anxiety and depression by education of patients with myocardial infarction. International Cardiovascular Research Journal 2011;5(2):66‐8. [Google Scholar]
DEMO II 2012 {published data only}
- Krogh J, Videbech P, Thomsen C, Gluud C, Nordentoft M. DEMO‐II Trial. Aerobic exercise versus stretching exercise in patients with major depression ‐ a randomised clinical trial. PLoS ONE 2012;7(10):e48316. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gotta 2012 {published data only}
- Gotta G. Sex differences and the effects of exercise on depression and executive dysfunctioning in older adults (thesis). Dissertation Abstracts International: Section B: The Sciences and Engineering 2012;72(10‐B):6385. [Google Scholar]
Martiny 2012 {published data only}
- Martiny K, Refsgaard E, Lund V, Lunde M, Sorensen L, Thougaard B, et al. A 9‐week randomised trial comparing a chronotherapeutic intervention (wake and light therapy) to exercise in major depressive disorder patients treated with duloxetine. Journal of Clinical Pyschiatry 2012;73(9):1234‐42. [DOI] [PubMed] [Google Scholar]
Murphy 2012 {published data only}
- Murphy SM, Edwards RT, Williams N, Raisanen L, Moore G, Linck P, et al. An evaluation of the effectiveness and cost effectiveness of the National Exercise Referral Scheme in Wales, UK: a randomised controlled trial of a public health policy initiative. Journal of Epidemiology and Community Health 2012;66(8):745‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinniger 2012 {published data only}
- Pinniger R, Brown RF, Thorsteinssona EB, McKinley P. Argentine tango dance compared to mindfulness meditation and a waiting‐list control: a randomised trial for treating depression. Complementary Therapies in Medicine 2012;20(6):377‐84. [DOI] [PubMed] [Google Scholar]
Sturm 2012 {published data only}
- Sturm J, Ploderl M, Fartacek C, Kralovec K, Neunhauserer D, Niederseer D, et al. Physical exercise through mountain hiking in high‐risk suicide patients. A randomized crossover trial. Acta Psychiatrica Scandinavica 2012;126(6):467‐75. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12605000475640 {published data only}
- ACTRN12605000475640. Does a home‐based physical activity programme improve function and depressive symptomatology in older primary care patients: a randomised controlled trial. [Australian New Zealand Clinical Trials Registry] www.anzctr.org.au/ACTRN12605000475640.aspx (accessed 1 March 2013).
ACTRN12609000150246 {published data only}
- ACTRN12609000150246. Promoting physical activity to improve the outcome of depression in later life (ACTIVEDEP). www.anzctr.org.au/ACTRN12609000150246.aspx ) (accessed 1 March 2013.
ACTRN12612000094875 {published data only}
- ACTRN12612000094875. A randomised controlled trial to improve depression in family carers through a physical activity intervention: IMPACCT Study. www.anzctr.org.au/ACTRN12612000094875.aspx (accessed 1 March 2013).
CTR/2012/09/002985 {published data only}
- CTR/2012/09/002985. Effect of sprint interval training on depression: a randomized controlled trial [Clinical Trials Registry ‐ India]. www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=5224 (accessed 1 March 2013).
EFFORT D {published data only}
- Kruisdijk FR, Hendriksen IJM, Tak ECPM, Beekman ATF, Hopman‐Rock M. Effect of running therapy on depression (EFFORT‐D). Design of a randomised controlled trial in adult patients. BMC Public Health 2012;12:50. [NTR1894] [DOI] [PMC free article] [PubMed] [Google Scholar]
IRCT201205159763 {published data only}
- IRCT201205159763N1. The effect of regular exercise on the depression of hemodialysis patients. www.irct.ir/searchresult.php?id=9763&number=1 (accessed 1 March 2013). [IRCT201205159763N1]
IRCT2012061910003N1 {published data only}
- IRCT2012061910003N1. A comparative study of the efficiency of group cognitive‐ behavioral therapy with aerobic exercise in treating of major depression. www/irct.ir/searchresult.php?id=10065&number=1 (accessed 1 March 2013).
ISRCTN05673017 {published data only}
- ISRCTN05673017. Psycho‐education physical exercise effects: does treating subsyndromal depression improve depression‐ and diabetes‐related outcomes? [PEPEE]. isrctn.org/ISRCTN05673017 (accessed 1 March 2013).
NCT00103415 {published data only}
- NCT00103415. Trial investigating the effect of different exercise forms on depression. ClinicalTrials.gov/show/NCT00103415 (accessed 1 March 2013).
NCT00643695 {published data only}
- NCT00643695. Efficacy of an Exercise Intervention to Decrease Depressive Symptoms in Veterans With Hepatitis C. ClinicalTrials.gov/show/NCT00643695 (accessed 1 March 2013).
NCT00931814 {published data only}
- NCT00931814. Effects of exercise on depression symptoms, physical function, and quality of life in community‐dwelling elderly. ClinicalTrials.gov/show/NCT00931814 (accessed 1 March 2013).
NCT01024790 {published data only}
- NCT01024790. Exercise study to help patients who have type 2 diabetes and depression. ClinicalTrials.gov/show/NCT01024790 (accessed 1 March 2013).
NCT01383811 {published data only}
- NCT01383811. Clinical and neuroendocrine/metabolic benefits of exercise in treatment resistant depression (TRD): a feasibility study. ClinicalTrials.gov/ct2/show/NCT01383811 (accessed 1 March 2013).
NCT01401569 {published data only}
- NCT01401569. Efficacy of exercise and counseling intervention on relapse in smokers with depressive disorders STOB‐ACTIV [NXR 01401569]. http://clinicaltrials.gov/show/NCT01401569.
NCT01464463 {published data only}
- NCT01464463. The impact of psychological interventions (with and without wxercise) on psychometric and immunological measures in patients With major depression. ClinicalTrials.gov/show/NCT01464463 (accessed 1 March 2013).
NCT01573130 {published data only}
- NCT01573130. An internet‐administered, therapist‐supported physical exercise program for the treatment of depression. ClinicalTrials.gov/show/NCT01573130 (accessed 1 March 2013).
NCT01573728 {published data only}
- NCT01573728. Role of exercise in depression in middle aged and older adults. ClinicalTrials.gov/slow/NCT01573728 (accessed 1 March 2013).
NCT01619930 {published data only}
- NCT01619930. The effects of behavioural activation and physical exercise on depression. ClinicalTrials.gov/show/NCT01619930 (accessed 1 March 2013).
NCT01696201 {published data only}
- NCT01696201. Effect of a supervised exercise program during whole pregnancy on outcomes and level of depression. ClinicalTrials.gov/show/NCT01696201 (accessed 1 March 2013).
NCT01763983 {published data only}
- NCT01763983. Effects of cognitive behaviour therapy and exercise on depression and cognitive deficits in multiple sclerosis. ClinicalTrials.gov/show/NCT01763983 (accessed 1 March 2013).
NCT01787201 {published data only}
- NCT01787201. The effects of exercise on depression symptoms using levels of neurotransmitters and EEG as markers. ClinicalTrials.gov/show/NCT01787201 (accessed 1 March 2013).
NCT01805479 {published data only}
- NCT01805479. Exercise therapy in depressed traumatic brain injury survivors. ClinicalTrials.gov/show/NCT01805479 (accessed 1 March 2013).
UMIN000001488 {published data only}
- UMIN000001488. A randomised controlled trial of exercise class for older persons with mild depression. www.umin.ac.jp/ctr/index.htm (accessed 1 March 2013).
Additional references
ACSM 1998
- ACSM. ACSM position stand on the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in adults. Medicine and Science in Sports and Exercise 1998;30:975‐91. [DOI] [PubMed] [Google Scholar]
ACSM 2001
- American College of Sports Medicine. ACSM's Resource Manual for Guidelines for Exercise Testing and Prescription. 4th Edition. Lippincott, Williams and Wilkins, 2001. [Google Scholar]
Arroll 2009
- Arroll B, Elley CR, Fishman T, Goodyear‐Smith FA, Kenealy T, Blashki G, et al. Antidepressants versus placebo for depression in primary care. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007954] [DOI] [PMC free article] [PubMed] [Google Scholar]
Astin 1998
- Astin JA. Why patients use alternative medicine: results of a study. JAMA 1998;279(19):1548‐53. [DOI] [PubMed] [Google Scholar]
Babyak 2000
- Babyak M, Blumenthal JA, Herman S, Khatri P, Doraiswamy M, Moore K, et al. Exercise treatment for major depression. Maintenance of therapeutic benefits at 10 months. Psychosomatic Medicine 2000;62(5):633‐8. [DOI] [PubMed] [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4(6):561‐71. [DOI] [PubMed] [Google Scholar]
Beesley 1997
- Beesley S, Mutrie N. Exercise is beneficial adjunctive treatment in depression. BMJ 1997;315(7121):1542‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blake 2009
- Blake H. How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clinical Rehabilitation 2009;23:873‐87. [DOI] [PubMed] [Google Scholar]
Carlson 1991
- Carlson DL. The Effects of Exercise on Depression: A Review and Meta‐Regression Analysis [dissertation]. Milwaukee: University of Wisconsin, 1991. [Google Scholar]
Chen 2013
- Chen MJ. The neurobiology of depression and physical exercise. Handbook of Physical Activity and Mental Health. London: Routledge, 2013:169‐84. [Google Scholar]
Cotman 2002
- Cotman CW, Berchtold NC. Exercise: a behavioural intervention to enhance brain health and plasticity. Trends in Neurosciences 2002;25(6):295‐301. [DOI] [PubMed] [Google Scholar]
Craft 2005
- Craft LL. Exercise and clinical depression: examining two psychological mechanisms. Psychology of Sport and Exercise 2005;6:151‐71. [Google Scholar]
Craft 2013
- Craft LL. Potential psychological mechanisms underlying the exercise and depression relationship.. Handbook of Physical Activity and Mental Health. London: Routledge, 2013. [Google Scholar]
Daley 2008
- Daley A. Exercise and depression: a review of reviews. Journal of Clinical Psychology in Medical Settings 2008;15:140‐7. [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
Diener 1984
- Diener E. Subjective well‐being. Psychological Bulletin 1984;95:542‐75. [PubMed] [Google Scholar]
DOH 2001
- Department of Health. Exercise referral systems: a national quality assurance framework. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4009671 2001.
Donaghy 2000
- Donaghy M, Durward B. A report on the clinical effectiveness of physiotherapy in mental health. Research and Clinical Effectiveness Unit, Chartered Society of Physiotherapy 2000.
Ernst 2005
- Ernst C, Olson AK, Pinel JPJ, Lam RW, Christie BR. Antidepressant effects of exercise: evidence for an adult neurogenesis hypothesis?. Journal of Psychiatry and Neurosciences 2006;31(2):84‐92. [PMC free article] [PubMed] [Google Scholar]
Fox 2000
- Fox KR. The effects of exercise on self‐perceptions and self‐esteem. In: Biddle SJH, Fox KR editor(s). Physical Activity and Psychological Well‐Being. London: Routledge, 2000:88‐117. [Google Scholar]
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry 1960;23:56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Handbook 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Krogh 2011
- Krogh J, Nordentoft M, Sterne J, Lawlor DA. The effect of exercise in clinical depressed adults: systematic review and meta‐analysis of randomised controlled trials. Journal of Clinical Psychiatry 2011;72(4):529‐38. [DOI] [PubMed] [Google Scholar]
Lawlor 2001
- Lawlor DA, Hopker SW. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta‐regression analysis of randomised controlled trials. BMJ 2001;322(7289):763‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
LePore 1997
- LePore SJ. Expressive writing moderates the relation between intrusive thoughts and depressive symptoms. Journal of Personality and Social Psychology 1997;73(5):1030‐7. [DOI] [PubMed] [Google Scholar]
Moussavi 2007
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007;370(9590):808‐9. [DOI] [PubMed] [Google Scholar]
NICE 2009
- National Institute for Health and Clinical Excellence. Depression: the treatment and management of depression in adults (update). http://www.nice.org.uk/guidance/CG90 2009.
North 1990
- North TC, McCullagh P, Tran ZV. Effect of exercise on depression. Exercise and Sport Sciences Reviews 1990;18:379‐415. [PubMed] [Google Scholar]
Pavey 2011
- Pavey TG, Taylor AH, Fox KR, Hillsdon M, Anoyke N, Campbell L, et al. Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: systematic review and meta‐analysis. BMJ 2011;343:d6462. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinquart 2007
- Pinquart M, Duberstein PR, Lyness JM. Effects of psychotherapy and other behavioral interventions on clinical depressed older adults: a meta‐analysis. Aging and Mental Health 2007;11(6):645‐57. [DOI] [PubMed] [Google Scholar]
Rethorst 2009
- Rethorst CD, Wipfli BM, Landers DM. The antidepressive effects of exercise. Sports Medicine 2009;39(6):491‐511. [DOI] [PubMed] [Google Scholar]
Robertson 2012
- Robertson R, Robertson A, Jepson R, Maxwell M. Walking for depression or depressive symptoms: a systematic review and meta‐analysis. Mental Health and Physical Activity 2012;5:66‐75. [Google Scholar]
Schünemann 2008
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.o (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
SIGN 2010
- Scottish Intercollegiate Guidelines Network. Non‐pharmaceutical management of depression in adults. http://www.sign.ac.uk/pdf/sign114.pdf January 2010.
Singh 2001
- Singh NA, Clements KM, Singh MAF. The efficacy of exercise as a long‐term anti‐depressant ‐ elderly subjects. A randomised controlled trial. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2001;56(8):M497‐504. [DOI] [PubMed] [Google Scholar]
Sjosten 2006
- Sjosten N, Kivela SL. The effects of physical exercise on depressive symptoms among the aged: a systematic review. International Journal of Geriatric Psychiatry 2006;21(5):410‐8. [DOI] [PubMed] [Google Scholar]
Smith 2013
- Smith PJ, Blumenthal JA. Exercise and physical activity in the prevention and treatment of depression. Handbook of Physical Activity and Mental Health. London: Routledge, 2013:145‐160. [Google Scholar]
Sorensen 2006
- Sorensen JB, Skovgaard T, Puggaard L. Exercise on prescription in general practice: a systematic review. Scandinavian Journal of Primary Health Care 2006;24(2):69‐74. [DOI] [PubMed] [Google Scholar]
Stathopoulou 2006
- Stathopoulou G, Powers MB, Berry AC, Smits JAJ, Otto MW. Exercise interventions for mental health: a quantitative and qualitative review. Clinical Psychology: Science and Practice 2006;13:179‐93. [Google Scholar]
References to other published versions of this review
Mead 2009
- Mead GE, Morley W, Campbell P, Greig CA, McMurdo M, Lawlor DA. Exercise for depression. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD004366.pub4] [DOI] [PubMed] [Google Scholar]
Rimer 2012
- Rimer J, Dwan K, Lawlor DA, Greig CA, McMurdo M, Morley W, et al. Exercise for depression. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD004366.pub5] [DOI] [PubMed] [Google Scholar]


