Summary
Background
We aim to compare the effect of short versus long treatment duration in Gram-negative bacteremia on all-cause mortality in pre-specified sub-groups.
Methods
Individual participant data meta-analysis of randomized controlled trials (RCTs) comparing short (≤7) versus longer (>7 days) antibiotic treatment for Gram-negative bacteremia. Participants were adults (≥18 years), with Gram-negative bacteremia during hospital stay. We searched PubMed, Cochrane Central Register of Controlled Trials, and Web of Science to identify trials conducted up to May 2022. Primary outcome was 90-day all-cause mortality. Secondary outcomes were 30-day mortality, relapse of bacteremia, length of hospital stay, readmission, local or distant infection complications, adverse events, and resistance emergence.
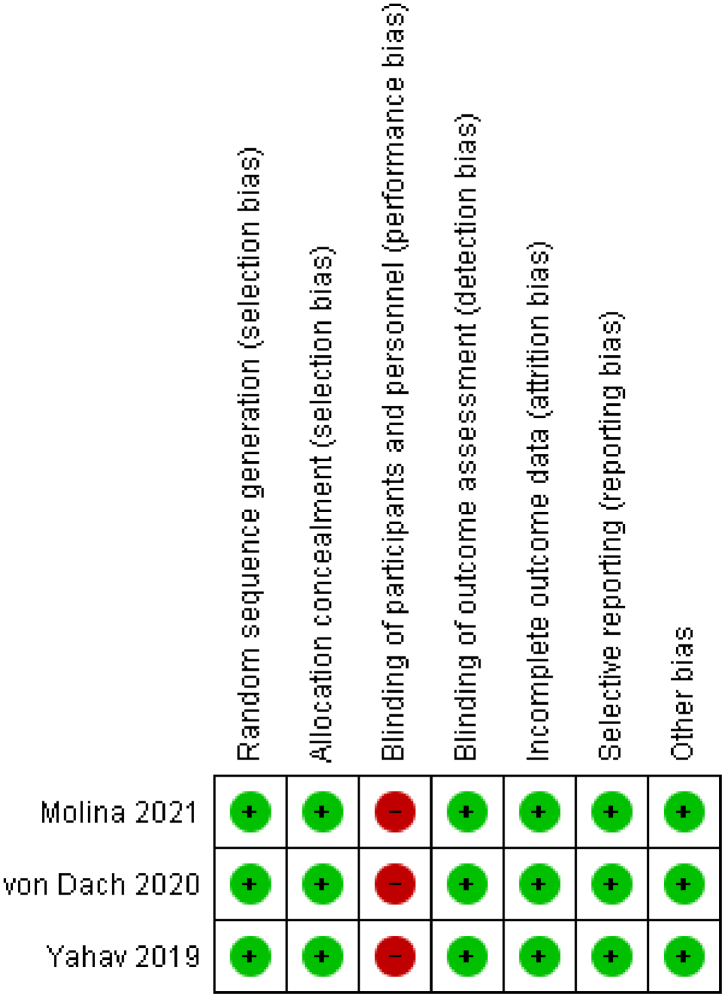
Outcomes were assessed in pre-specified subgroups: women vs men; non-urinary vs urinary source; presence vs absence of hypotension on initial presentation; immunocompromised patients versus non-immunocompromised patients, and age (above/below 65). Fixed-effect meta-analysis model was used to estimate pooled odds ratio (OR) and 95% confidence interval (CI). All three trials had low risk of bias for allocation generation and concealment.
Findings
Three RCTs (1186 patients) were included; 1121 with enterobacterales bacteremia. No significant difference in mortality was demonstrated between 7- and 14-days treatment (90-day mortality: OR 1.08, 95% CI 0.73–1.58; 30-day mortality: 1.08, 0.62–1.91). Relapse (1.00, 0.50–1.97); length of hospital stay (P = 0.78); readmission (0.96, 0.80–1.22); and infection complications (local: 1.62 0.76–3.47; distant: 2.00, 0.18–22.08), were without significant difference, and so were adverse events or resistance emergence.
No significant difference in clinical outcomes between 7 and 14 days of antibiotics was demonstrated in the subgroups of gender, age, hemodynamic status, immune status, and source of infection.
Interpretation
For patients hemodynamically stable and afebrile at 48 h prior to discontinuation, seven days of antibiotic therapy for enterobacterales bacteremia result in similar outcomes as 14 days, in terms of mortality, relapse, length of hospital stay, complications of infection, resistance emergence, and adverse events. These results apply for any adult age group, gender, source of infection, immune status, and hemodynamic status on presentation.
Funding
There was no funding source for this study.
Keywords: Individual patient data meta-analysis, Treatment duration, Gram-negative bacteremia, Antibiotics, Resistance
Research in context.
Evidence before this study
Previous retrospective data has shown inconclusive results regarding optimal treatment duration for Gram-negative bacteremia. We performed a systematic literature search for randomized controlled trials (RCTs) comparing treatment duration for Gram-negative bacteremia. We used three databases (PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), and Web of Science) and three clinical trial registries (ISRCTN registry, Clinicaltrials.gov and the European Union Clinical Trials Register) to search for RCTs conducted up to May 2022. No language or publication restrictions were applied. Search terms were 'duration OR days' and 'antibiotic' and 'bloodstream OR bacteremia OR bacteremia'.
We found three recent RCTs, that have all demonstrated non-inferiority for shorter antibiotic courses for Gram-negative bacteremia, but were underpowered for select subgroups such as: men vs women, non-urinary source of the infection, patients presenting with hemodynamic instability, immunocompromised patients, and the elderly.
Added value of this study
Our individual patient data meta-analysis has combined the largest comparison of shorter vs. longer duration of antibiotic treatment for Gram-negative bacteremia to date. It has reproduced the overall findings of each of the separated RCTs showing that a 7-day treatment is non-inferior to 14-days in terms of mortality and other clinical outcomes. Analyzing this large database for subgroup analysis, we did not find a significant difference in clinical outcomes between 7 and 14 days of antibiotics in the subgroups of women vs men; non urinary vs urinary source of bacteremia; presence vs absence of hypotension on initial presentation; immunosuppression; and age (above/below 65).
Implications of all available evidence
Shorter courses of antibiotic therapy may be encouraged in eligible patients and may shorten length of inpatient stay, decrease antibiotic exposure and reduce costs without impacting mortality or other adverse outcomes.
Introduction
Gram-negative bacteremia is common in both community and health care settings, with a significant increase in incidence described for some Gram-negative bacteria in recent years.1,2 Prolonged duration of antibiotic therapy for such common infections may lead to increased resistance emergence; adverse events and secondary infections, including Clostridioides difficile infection; prolonged hospital-stay; and excess cost.3,4
tThough recent randomized controlled trials (RCTs) have demonstrated the non-inferiority of shorter antibiotic courses for Gram-negative bacteremia,5, 6, 7 prolonged courses are still commonly used and current guidelines still recommend the range of 7–14 days.4,8 In addition, it is unclear whether shorter courses of antibiotics are appropriate for specific sub-groups of patients, such as those with non-urinary source of bacteremia; intensive care patients, elderly, and others.
Observational design is a limited tool for evaluating duration of therapy due to confounding by indication and immortal time bias issues.9 Thus, RCTs are the preferred design to answer this question. Individual participant data (IPD) meta-analysis of RCTs is considered to be the gold standard of systematic review.10 IPD meta-analysis advantages (among others) are narrowing the confidence intervals, and increasing the power to evaluate treatment effect in specific sub-groups of patients.11
We performed an IPD meta-analysis of RCTs evaluating short (≤7 days) versus longer (>7 days) antibiotic treatment for Gram-negative bacteremia. We aimed to explore outcomes in several pre-specified sub-groups of patients. We hypothesized no significant difference between short and long antibiotic course for either of the sub-groups.
Methods
This IPD systematic review and meta-analysis was conducted and reported according to the PRISMA-IPD Statement,12 and Cochrane instructions for IPD-MA.13 Considering the priority of the results for decision-making, and taking into account expected new evidence from a large ongoing trial in the topic, we conduct this review as a living systematic review.14,15 For the living systematic review we will repeat the search every 12 months. Updates of the meta-analysis will be conducted when new evidence that is likely to influence the results will be identified.
We included RCTs comparing short (≤7 days) versus longer (>7 days) antibiotic treatment for Gram-negative bacteremia. Participants were hospitalized adults (≥18 years), with Gram-negative bacteremia, as defined in individual trials. We included only trials evaluating patients with Gram-negative bacteremia as their target population. Trials evaluating various infection types (e.g., pneumonia, urinary tract infection), and reporting bacteremic patients as a sub-group were not included. We excluded trials addressing source of bacteremia requiring prolonged treatment (endocarditis/endovascular infections; necrotizing fasciitis; osteomyelitis; abdominal abscesses and other unresolved abdominal sources requiring source control (surgery/drainage); central nervous system infections; empyema; any uncontrolled focus of infection (undrained abscess/deep seated intra-abdominal infection, undrained moderate to severe hydronephrosis). We also excluded patients with intracellular pathogens including Salmonella spp. and Brucella spp.
Interventions tested were antibiotics with in vitro activity against the pathogen for ≤7 vs > 7 days. Any choice and route of administration of antibiotics (oral or intravenous) were eligible for inclusion. Any source of bacteremia not requiring prolonged treatment (urinary tract infection, pneumonia, etc.) and any place of acquisition (community or hospital) were eligible for inclusion.
Primary outcome was 90-day all-cause mortality.16 Secondary outcomes included 30-day all-cause mortality; relapse of bacteremia; length of hospital stay; readmissions; local suppurative and distant complications; restarting of Gram-negative-directed antibiotic therapy; emergence of resistance to study antibiotics; functional capacity and time to return to baseline capacity; new clinically or microbiologically documented infection; and adverse events: any diarrhea, C. difficile associated diarrhea, acute kidney injury, and rash (for secondary outcomes definitions, see Appendix).
We pre-planned to extract data regarding the following sub-groups: men versus women; patients with a non-urinary source of infection vs patients with urinary tract infection (UTI); presence vs absence of hypotension on initial presentation (hypotension was defined as systolic blood pressure of less than 100 mmHg), immunocompromised patients versus non-immunocompromised patients, and elderly (age ≥65 years) versus younger patients.
Immunosuppression was defined as treatment with immunosuppressive drugs (including prednisone ≥20 mg/day or equivalent, biological agents) due to any reason, active chemotherapy, solid organ transplantation, and stem cell transplantation. The following immunosuppressive conditions were excluded: HIV infection with CD4 cell count ≤500/μl, and neutropenia (absolute neutrophil count ≤500/μl) in the 48 h prior to randomization.
Information sources and search strategy
We searched PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), and Web of Science to identify trials conducted up to May 2022. Search term combined the Cochrane filter for RCTs17 with the terms 'duration OR days' and 'antibiotic' and 'bloodstream OR bacteremia OR bacteraemia', restricted to adults by PubMed filter. We applied no language or publication restrictions. References of all included trials were searched for additional relevant trials. The investigators of eligible trials were contacted to ask for acquaintance with similar trials. We also searched relevant conference proceedings, as well as ongoing trial databases for unpublished trials.
Data collection and analysis
Studies were fully reviewed (titles, abstract and full texts) and appraised by two investigators independently. Conflicts were resolved by consultation with an independent third reviewer. First authors of the trials identified were invited to share their trials' data through email, and consenting authors were asked to participate and send their data anonymized in an encrypted table. Each participating site received the permission of the local ethics committee to transfer the data according to local regulations. Queries regarding data were resolved by communication with the authors of each trial and discrepancies between published and raw data were checked with them.
Risk of bias of included trials was assessed by two review authors independently using domain-based evaluation as recommended in the Cochrane Handbook for Systematic Reviews of Interventions.17
Statistical analysis
Baseline characteristic of included trials are presented as frequencies (percentages) for categorical variables, and interquartile range (IQR, 25–75 percentiles) for non-normally distributed continuous variables.
Difference in outcomes rate between 7 and 14 days of antibiotic therapy for Gram-negative bacteremia were examined. An analysis of outcomes by several pre-specified sub-groups of patients was also performed. Generalized linear models (GLM) were used for the comparison of continuous variables between trials. For categorical variables, the fixed-effect meta-analysis model (Mantel-Haenszel method) was used to estimate pooled odds ratio and associated 95% confidence interval. The Breslow–Day test for homogeneity of odds ratios was performed to test for between trials differences. The analysis was performed following the intention-to-treat principle, including all patients according to the treatment group assigned at the time of randomization. We also performed a per-protocol analysis for the primary outcome.
Statistical analyses were performed using IBM SPSS Statistics, version 27.
Role of the funding source
There was no funding source for this study.
Results
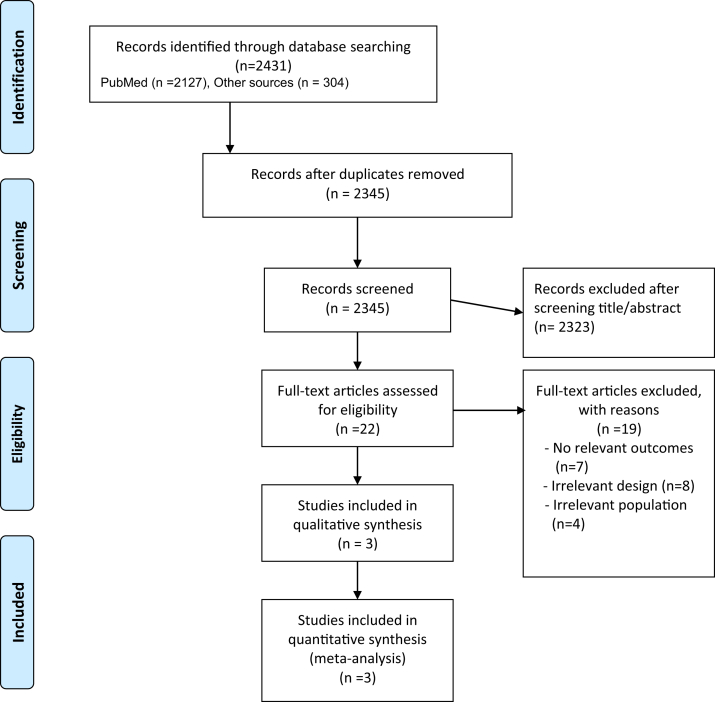
The study flow chart is presented in Fig. 1. Three trials met our inclusion criteria, all were investigator-initiated, and compared an antibiotic duration of seven versus fourteen days for Gram-negative bacteremia.5, 6, 7 One of these three trials included a C-reactive protein (CRP)-based duration arm that was excluded from the analysis,6 leaving overall 1186 randomized patients (1182 evaluable patients; Yahav et al. 604 patients5; von Dach et al. 334 patients6; and Molina et al. 248 patients7). Trials’ characteristics are detailed in Table 1. The most common source of bacteremia in the original trials was UTI (411/604, 68%; 213/334, 64%, and 136/248, 55% of patients in the different trials). Accordingly, the vast majority of causative bloodstream isolates were enterobacterales (95%, 1125/1186), with two trials including only patients with enterobacterales bacteremia,6,7 and a third trial allowing other Gram-negatives.5 In the three included trials, choice and route of administration of antibiotics was at the discretion of the treating physician. Risk of bias assessment of the included trials is detailed in Fig. 2. All three trials had low risk of bias for allocation generation and concealment; all three were open-label.
Fig. 1.
Study flowchart.
Table 1.
Baseline characteristic of included trials.
| Yahav et al. (2018) | von Dach et al. (2020) | Molina et al. (2021) | |
|---|---|---|---|
| Trial characteristics | |||
| Design | Investigator-initiated randomized controlled trial | Investigator-initiated randomized controlled trial | Investigator-initiated randomized controlled trial |
| Study period | 2013–2017 | 2017–2019 | 2014–2016 |
| Inclusion criteria | Adults with growth of Gram-negative bacteria in one or more blood cultures, hemodynamically stable and afebrile for at least 48 h. | Adults with growth of Gram-negative fermenters in at least one blood culture and treatment with a microbiologically efficacious antibiotic. | Adults with a diagnosis of enterobacterales bloodstream infections with appropriate source control. |
| Exclusion criteria | Sources of infection requiring prolonged treatment, fever or hemodynamic instability in the 48 h prior to randomization, uncontrolled focus of infection, polymicrobial growth involving Gram-positive bacteria, specific pathogens (Brucella, Salmonella), or specific immunosuppression (human immunodeficiency virus, neutropenia). | Fever or hemodynamic instability in the 24 h prior to recruitment, severe immunosuppression, bacteremia with nonfermenting bacilli or polymicrobial, gram-positive growth, recurrent bacteremia, or complicated Infections. |
Pregnancy, noncontrolled source of infection and no expectation of being controlled in the subsequent 24 h, patients undergoing chemotherapy with neutropenia <500 cells/mm3 expected for more than 7 days, infections requiring prolonged antibiotic treatment, infections caused by a carbapenemase producing member of the Enterobacterales, polymicrobial bacteraemia, and expectation of survival <48 h. |
| Timing of randomization | At least 48 h without fever and hemodynamically stable and until day 7 from positive culture | Day 5 from first positive culture | <48 h since pathogen identification |
| Number randomized | 604 | 504 | 248 |
| Primary outcome of the original study | Composite at 90 days of mortality, relapse, complications, and readmission or extended hospitalization | Composite at 30 days of mortality, relapse, distal complications, and the restarting of antibiotics for suspected relapse | Number of days of antibiotic treatment required at the end of follow-up. |
| Patient characteristics | |||
| Age (median, interquartile range) | 71 (61–80) | 79 (68–86) | 67 (53–77) |
| Gender- women | 319/604 (53%) | 306/504 (61%) | 118/248 (48%) |
| Immunocompromised patientsa | |||
| Malignancy | 159/604 (26%) | NR | 64/248 (26%) |
| Immunosuppressive drugs | 150/604 (25%) | None | 31/248 (12.5%) |
| Solid-organ transplant | 51/604 (8.5%) | None | 11/248 (4.5%) |
| Stem-cell transplant | 5/604 (0.8%) | None | NR |
| Infection characteristics | |||
| Source of infection | |||
| Urinary tract | 411/604 (68%) | 335/504 (66%) | 136/248 (55%) |
| Abdominal | 71/604 (12%) | 80/504 (16%) | 34/248 (14%) |
| Respiratory | 24/604 (4%) | 25/504 (5%) | 15/248 (6%) |
| Central venous catheter | 38/604 (6%) | 8/504 (2%) | 30/248 (12%) |
| Skin and soft tissue | 9/604 (2%) | 4/504 (1%) | 3/248 (1%) |
| Unknown | 51/604 (8%) | 52/504 (10%) | 29/248 (12%) |
| Presence of hypotension on initial presentation (SBP<100) | 186/604 (31%) | 169/504 (34%) | 63/244 (26%) |
| Hospital acquired | 176/604 (29%) | 135/504 (27%) | 81/247 (33%) |
| Bacteria type | |||
| Escherichia coli | 380/604 (63%) | 377/502 (74%) | 155/247 (63%) |
| Klebsiella spp | 80/604 (13%) | 68/502 (14%) | 46/247 (19%) |
| Other | 82/604 (14%) | 45/502 (9%) | 46/247 (19%) |
| Enterobacteriaceae | |||
| Non-fermenting bacilli | 61/604 (10%) | None | None |
| Otherb | 1/604 (∼0%) | 12/502 (2%) | None |
| Recurrent bacteremia (previous 60 days) | NR | None | NR |
| Multidrug resistant (MDR) bacteriac | 109/604 (18%) | 40/504 (8%) | 41/248 (16.5%) |
SBP – systolic blood pressure.
The followings were excluded: HIV infection with CD4 cell count ≤500/μl, hematopoietic stem-cell transplantation in the first month after transplantation and at any time before engraftment, neutropenia in the 48 h prior to randomization, receipt of high-dose steroids [>40 mg prednisone or its equivalent] daily for >2 weeks, in the two weeks prior to randomization.
Bacteroides fragilis, Haemophilus influenza.
Multidrug resistance (MDR) was defined as: • Extended spectrum beta-lactamase (ESBL)-positive Enterobacteriaceae (Enterobacteriaceae demonstrating resistance to oxyimino-beta-lactam substrates (cefotaxime and ceftazidime) were defined as ESBL positive). • Pseudomonas spp. resistant to three or more of the following antimicrobial agents: antipseudomonal penicillins (e.g., piperacillin), antipseudomonal cephalosporins (e.g., ceftazidime), fluoroquinolones (e.g., ciprofloxacin), carbapenems (imipenem, meropenem), and aminoglycosides. • Acinetobacter spp. resistant to three or more of the following agents: imipenem (or meropenem), levofloxacin (or other fluoroquinolones), ceftazidime, colistin, tobramycin (or other aminoglycosides), and piperacillin–tazobactam.
Fig. 2.
Risk of bias assessment.
Overall, 592 patients were included for evaluation in the short (7 days) arm and 590 in the long (14 days) arm. The Breslow–Day test showed no heterogeneity of odds ratios between trials. For the outcome of mortality, no significant difference was demonstrated for either 90- or 30-day mortality between arms (90 days mortality 7 days: 60/592 (10.1%), 14 days: 56/590 (9.5%) - OR 1.08, 95% CI 0.73–1.58; 30d mortality 7 days: 26/592 (4.4%), 14 days: 24/590 (4.1%) - OR 1.08, 95% CI 0.62–1.91 (with OR > 1 favoring 14 days).
Overall, 1041 patients (88%) were included in the per-protocol analysis. For the primary outcome of 90-day mortality, no significant difference was demonstrated between arms (OR 1.26, 95% CI 0.81–1.95).
Other components of the primary outcomes from the trials were without significant difference between arms (Table 2). These included relapse of bacteremia, length of hospital stay, readmissions at 30 days; and distal complications and local suppurative complications at 90 days (Table 2). Other components of the primary outcomes were reported by individual trials, including restart of targeted antibiotics until 90 days by von Dach et al., without difference between arms (7-days: 9/169, 56% vs 14-days: 9/165, 56%)6; and absence of clinical cure (i.e. no resolution of signs and symptoms) by Molina et al., with no significant difference between arms (7-days: 8/110, 7.3% vs 14-days: 12/122, 9.8%).7
Table 2.
The association between study arm and outcomes, stratified by trial (For categorical variables, fixed-effect meta-analysis model, Mantel-Haenszel method. Homogeneity of odds ratios between trials was evaluated with the Breslow–Day test).
| Variable | Yahav et al. |
von Dach et al. |
Molina et al. |
Mantel-Haenszel OR (95% CI) | Breslow–Day P value | |||
|---|---|---|---|---|---|---|---|---|
| 7 days (n = 306) | 14 days (n = 298) | 7 days (n = 169) | 14 days (n = 165) | 7 days (n = 117) | 14 days (n = 127) | |||
| 90-d mortality | 36 (11.8) | 32 (10.7) | 14 (8.3) | 9 (5.5) | 10 (8.5) | 15 (11.8) | 1.08 (0.73–1.58) | 0.41 |
| 30-d mortality | 16 (5.2) | 12 (4.0) | 6 (3.6) | 4 (2.4) | 4 (3.4) | 8 (6.3) | 1.08 (0.62–1.91) | 0.40 |
| Relapse of bacteremia −30d | 8 (2.6) | 8 (2.7) | 2 (1.2) | 3 (1.8) | 7 (5.9) | 6 (4.7) | 1.00 (0.50–1.97) | 0.82 |
| Readmissions - 30d | 74 (24.2) | 79 (26.5) | 14 (8.3) | 9 (5.5) | 11 (9.2) | 12 (9.3) | 0.98 (0.73–1.33) | 0.49 |
| Hospital length of stay, Median (IQR) | 1 (0–4) | 1 (0–4) | 4 (1.3–10) | 4 (1–11) | 4 (0–9) | 3 (0–8) | – | 0.71∗ |
| Duration of antibiotic therapy, Median (IQR) | 5 (4–13) | 12 (10–16) | 7 (6–9) | 13 (9–14) | 7 (7–14) | 14 (14–16) | – | 0.39∗ |
| Local suppurative complications 90d | 16 (5.2) | 10 (3.4) | 2 (1.2) | 1 (0.6) | – | – | 1.62 (0.76–3.47) | 0.87 |
| Distal complications 90d | 2 (0.7) | 1 (0.3) | 0 (0.0) | 0 (0.0) | – | – | 2.00 (0.18–22.08) | – |
| Emergence of resistance to study antibiotic −90d | 33 (10.8) | 29 (9.7) | 3 (1.8) | 0 (0.0) | – | – | 1.23 (0.74–2.04) | 0.11 |
| Diarrhea | 18 (5.9) | 24 (8.1) | – | 2 (1.7) | 3 (2.3) | 0.73 (0.40–1.33) | 1.00 | |
| Clostridioides difficile infection | 2 (0.7) | 2 (0.7) | 2 (1.2) | 4 (2.4) | – | – | 0.65 (0.18–2.31) | 0.60 |
| Rash | 2 (0.7) | 4 (1.3) | – | – | 1 (0.8) | 4 (3.1) | 0.37 (0.10–1.41) | 0.67 |
| Acute kidney injury | 14 (4.6) | 12 (4.0) | – | – | 3 (2.5) | 1 (0.8) | 1.33 (0.64–2.77) | 0.37 |
Data are presented as no. (%).
OR – odds ration; CI – confidence interval; IQR - interquartile range.
∗P value by General linear models.
Emergence of resistance to study antibiotic was reported from two trials for a follow up of up to 90 days, reporting 36/592 cases (6%) in the short arm and 29/590 cases (5%) in the long arm, without significant difference (OR 1.23, 95% CI 0.74–2.04). New clinically or microbiologically documented infection and functional capacity were reported from only one trial. This trial reported no difference in new infections between arms, and significantly shorter time to return to baseline functional capacity in the 7 days arm.5 As expected, duration of antibiotic therapy for the index bacteremia was significantly shorter in the seven-day arm. Adverse events that were reported from at least two trials included diarrhea, C. difficile associated diarrhea, rash and acute kidney injury. All were without significant difference between short and long therapy (Table 2).
An analysis of outcomes by subgroups, including gender, source of infection (UTI vs non-UTI), blood pressure at presentation (Systolic blood pressure ≥100 mmHg or <100 mmHg), immune status, and age (≥65 years vs < 65) is presented in Table 3. Overall, 1182 (100%) patients were included in the subgroup analysis according to gender, infection source, and age; 1180 (∼100%) patients were included in the subgroup analysis according to hemodynamic status; and 850 (72%) patients were included in the subgroup analysis according to immune status. For the outcomes of 90- or 30-day mortality, relapse of bacteremia, and readmissions at 30 days, no significant difference was demonstrated between 7 and 14 days among any of the subgroups (gender, source of infection, hemodynamic status, immune status, and age).
Table 3.
The association between study arm and outcomes from included studies, stratified by age group, gender, hemodynamic status, immune status, and source of infection.
| Yahav et al. |
Von Dach et al. |
Molina et al. |
Mantel-Haenszel OR (95% CI) | Breslow–Day P value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 7 days (n = 306) | 14 days (n = 298) | 7 days (n = 169) | 14 days (n = 165) | 7 days (n = 117) | 14 days (n = 127) | |||||
| 90-d mortality | All patients | 36/306 (11.8) | 32/298 (10.7) | 14/169 (8.3) | 9/165 (5.5) | 10/117 (8.5) | 15/127 (11.8) | 1.08 (0.73–1.58) | 0.41 | |
| Gender | Women | 16/156 (10.3) | 14/163 (8.6) | 10/107 (9.3) | 5/94 (5.3) | 6/59 (10.2) | 5/59 (8.5) | 1.34 (0.77–2.34) | 0.64 | |
| Men | 20/150 (13.3) | 18/135 (13.3) | 4/62 (6.5) | 4/71 (5.6) | 4/58 (6.9) | 10/68 (14.7) | 0.88 (0.51–1.50) | |||
| Source of infection | Non UTI | 11/86 (12.8) | 6/107 (5.6) | 5/68 (7.4) | 5/53 (9.4) | 8/48 (16.7) | 9/63 (14.3) | 1.37 (0.73–2.56) | 0.12 | |
| UTI | 25/220 (11.4) | 26/191 (13.6) | 9/101 (8.9) | 4/112 (3.6) | 2/69 (2.9) | 6/64 (9.4) | 0.94 (0.58–1.52) | |||
| SBP | SBP≥100 | 22/215 (10.2) | 18/202 (8.9) | 5/106 (4.7) | 5/117 (4.3) | 8/88 (9.1) | 8/93 (8.6) | 1.15 (0.70–1.90) | 0.64 | |
| SBP<100 | 14/91 (15.4) | 14/95 (14.7) | 9/63 (14.3) | 4/47 (8.5) | 2/29 (6.9) | 7/34 (20.6 | 0.96 (0.53–1.74) | |||
| Age | Age<65 | 5/98 (5.1) | 12/102 (11.8) | 0/28 (0.0) | 1/39 (2.6) | 4/57 (7.0) | 5/57 (8.8) | 0.52 (0.23–1.18) | 0.20 | |
| Age≥65 | 31/208 (14.9) | 20/196 (10.2) | 14/141 (9.9) | 8/126 (6.3) | 6/60 (10.0) | 10/70 (14.3) | 1.33 (0.85–2.07) | |||
| Immunosuppression | No | 27/237 (11.4) | 22/217 (10.1) | / | / | 6/100 (6.0) | 12/113 (10.6) | 0.95 (0.57–1.57) | 0.64 | |
| Yes | 9/69 (13.0) | 10/81 (12.3) | / | / | 4/17 (23.5) | 3/14 (21.4) | 1.12 (0.49–2.58) | |||
| 30-d mortality | All patients | 16/306 (5.2) | 12/298 (4.0) | 6/169 (3.6) | 4/165 (2.4) | 4/117 (3.4) | 8/127 (6.3) | 1.08 (0.62–1.91) | 0.40 | |
| Gender | Women | 7/156 | 7/163 (4.3) | 4/107 (3.7) | 2/94 (2.1) | 3/59 (5.1) | 2/59 (3.4) | 1.26 (0.56–2.82) | 0.49 | |
| Men | 9/150 (6.0) | 5/135 (3.7) | 2/62 (3.2) | 2/71 (2.8) | 1/58 (1.7) | 6/68 (8.8) | 0.93 (0.42–2.09) | |||
| Source of infection | Non UTI | 7/86 (8.1) | 5/107 (4.7) | 2/68 (2.9) | 2/53 (3.8) | 3/48 (6.3) | 3/63 (4.8) | 1.35 (0.57–3.18) | 0.40 | |
| UTI | 9/220 (4.1) | 7/191 (3.7) | 4/101 (4.0) | 2/112 (1.9) | 1/69 (1.4) | 5/64 (7.8) | 0.94 (0.44–2.00) | |||
| SBP | SBP≥100 | 13/215 (6.0) | 11/202 (5.4) | 3/106 (2.8) | 2/117 (1.7) | 2/88 (2.3) | 3/93 (3.2) | 1.14 (0.57–2.27) | 0.76 | |
| SBP<100 | 3/91 (3.3) | 1/95 (1.1) | 3/63 (4.8) | 2/47 (4.3) | 2/29 (6.9) | 5/34 (14.7) | 0.96 (0.35–2.62) | |||
| Age | Age<65 | 7/98 (7.1) | 2/102 (2.0) | 0/28 (0.0) | 0/39 (0.0) | 2/57 (3.5) | 2/57 (3.5) | 2.51 (0.76–8.29) | 0.29 | |
| Age≥65 | 9/208 (4.3) | 10/196 (5.1) | 6/141 (4.3) | 4/126 (3.2) | 2/60 (3.3) | 6/70 (8.6) | 0.81 (0.42–1.56) | |||
| Immunosuppression | No | 11/237 (4.6) | 12/217 (5.5) | / | / | 3/100 (3.0) | 7/113 (6.2) | 0.71 (0.35–1.44) | 0.06 | |
| Yes | 5/69 (7.2) | 0/81 (0.0) | / | / | 1/17 (5.9) | 1/14 (7.1) | 7.05 (0.83–59.80) | |||
| Relapse of bacteremia -30d | All patients | 8/306 (2.6) | 8/298 (2.7) | 2/169 (1.2) | 3/165 (1.8) | 7/117 (5.9) | 6/127 (4.7) | 1.00 (0.50–1.97) | 0.82 | |
| Gender | Women | 2/156 (1.3) | 6/163 (3.7) | 2/107 (1.9) | 3/94 (3.2) | 4/59 (6.8) | 2/59 (3.4) | 0.71 (0.28–1.78) | 0.33 | |
| Men | 6/150 (4.0) | 2/135 (1.5) | 0/62 (0.0) | 0/71 (0.0) | 3/59 (5.1) | 4/68 (5.9) | 1.53 (0.54–4.37) | |||
| Source of infection | Non UTI | 1/86 (1.2) | 3/107 (2.8) | 1/68 (1.5) | 2/53 (3.8) | 2/48 (4.2) | 3/63 (4.8) | 0.54 (0.16–1.83) | 0.88 | |
| UTI | 7/220 (3.2) | 5/191 (2.6) | 1/101 (1.0) | 1/112 (0.9) | 5/70 (7.1) | 3/64 (4.7) | 1.37 (0.58–3.24) | |||
| SBP | SBP≥100 | 6/215 (2.8) | 8/202 (4.0) | 1/106 (0.9) | 2/117 (1.7) | 5/88 (5.7) | 3/93 (3.2) | 0.93 (0.42–2.06) | 0.61 | |
| SBP<100 | 2/91 (2.2) | 0/95 (0.0) | 1/63 (1.6) | 1/47 (2.1) | 2/29 (6.9) | 3/34 (8.8) | 1.21 (0.32–4.57) | |||
| Age | Age<65 | 3/98 (3.1) | 2/102 (2.0) | 0/28 (0.0) | 1/39 (2.6) | 4/57 (7.0) | 4/57 (7.0) | 1.09 (0.37–3.16) | 0.91 | |
| Age≥65 | 5/208 (2.4) | 6/196 (3.1) | 2/141 (1.4) | 2/126 (1.6) | 3/61 (4.9) | 2/70 (2.9) | 0.96 (0.39–2.32) | |||
| Immunosuppression | No | 7/237 (3.0) | 7/217 (3.2) | / | / | 7/101 (6.9) | 3/113 (2.7) | 1.38 (0.61–3.16) | 0.10 | |
| Yes | 1/69 (1.4) | 1/81 (1.2) | / | / | 0/17 (0.0) | 3/14 (21.4) | 0.27 (0.03–2.44) | |||
| Readmissions −30d | All patients | 74/306 (24.2) | 79/298 (26.5) | 14/169 (8.3) | 9/165 (5.5) | 11/117 (9.2) | 12/127 (9.3) | 0.98 (0.73–1.33) | 0.49 | |
| Gender | Women | 39/156 (25.0) | 38/163 (23.3) | 6/107 (5.6) | 5/94 (5.3) | 4/59 (6.8) | 5/59 (8.5) | 1.00 (0.65–1.54) | 0.51 | |
| Men | 35/150 (23.3) | 41/135 (30.4) | 8/62 (12.9) | 4/71 (5.6) | 7/59 (11.9) | 7/70 (10.0) | 0.98 (0.63–1.50) | |||
| Source of infection | Non UTI | 23/86 (26.7) | 23/107 (21.5) | 9/68 (13.2) | 4/53 (7.5) | 4/48 (8.3) | 3/63 (4.8) | 1.40 (0.82–2.36) | 0.46 | |
| UTI | 51/220 (23.2) | 56/191 (29.3) | 5/101 (5.0) | 5/112 (4.5) | 7/70 (10.0) | 9/66 (13.6) | 0.82 (0.56–1.19) | |||
| SBP | SBP≥100 | 50/215 (23.3) | 50/202 (24.8) | 8/106 (7.5) | 7/117 (6.0) | 9/88 (10.2) | 7/93 (7.5) | 1.07 (0.73–1.55) | 0.67 | |
| SBP<100 | 24/91 (26.4) | 29/95 (30.5) | 6/63 (9.5) | 2/47 (4.3) | 2/29 (6.9) | 5/34 (14.7) | 0.82 (0.49–1.40) | |||
| Age | Age<65 | 28/98 (28.6) | 27/102 (26.5) | 1/28 (3.6) | 1/39 (2.6) | 3/58 (5.2) | 4/59 (6.8) | 1.11 (0.65–1.89) | 0.82 | |
| Age≥65 | 46/208 (22.1) | 52/196 (26.5) | 13/141 (9.2) | 8/126 (6.3) | 8/61 (13.1) | 8/70 (11.4) | 0.93 (0.64–1.35) | |||
| Immunosuppression | No | 53/237 (22.4) | 51/217 (23.5) | / | / | 9/102 (8.8) | 10/115 (8.7) | 0.99 (0.67–1.47) | 0.98 | |
| Yes | 21/69 (30.4) | 28/81 (34.6) | / | / | 2/17 (11.8) | 2/14 (14.3) | 0.79 (0.42–1.51) | |||
OR – odds ration; CI – confidence interval; SBP – systolic blood pressure; UTI – urinary tract infection.
Discussion
In this individual patient data meta-analysis of three RCTs, evaluating overall 1182 patients, we found no significant difference in 90- or 30-day mortality between 7 and 14 days of antibiotic therapy for Gram-negative bacteremia. Other patient related outcomes, such as relapse of bacteremia, length of hospital stay, readmission, and local or distant complications, were also demonstrated to be without significant difference. No difference in emergence of resistance or adverse events was either demonstrated between short and long therapy arms, though the number of events was low and the follow up duration limited to 90 days.
Analyzing this large database for subgroup analysis, we also did not find a significant difference in clinical outcomes between 7 and 14 days of antibiotics in the subgroups of women vs men; non urinary vs urinary source of bacteremia; presence vs absence of hypotension on initial presentation; immunocompromised patients vs non-immunocompromised patients; and age (above/below 65).
Shorter antibiotic therapy for Gram-negative bacteremia has been demonstrated to have similar outcomes to longer duration in several observational studies, mostly comparing 5–10 days to longer regimens.18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30 Mortality, relapse/recurrence, clinical success, and superinfection rates were similar between longer and shorter therapy in most studies, though some demonstrated higher rates of superinfection18,27 or resistance emergence23 with longer therapy; while others reported higher rates of re-initiation of antibiotics and C. difficile with shorter regimen.28
Concomitantly, three RCTs demonstrated non-inferiority of 7 vs 14 days of antibiotic therapy for hemodynamically stable patients with mainly enterobacterales bacteremia. The strength of this individual patient data meta-analysis is by allowing a larger sample size to test the effect of duration of therapy for specific subgroups of patients. In this meta-analysis, short versus long therapy had similar outcomes among 425 patients with non-urinary source of infection, 801 elderly patients (aged ≥65) and 359 patients with low systolic blood pressure. Nevertheless, sample size of each sub-group may not be sufficient to draw conclusions. Moreover, findings from subgroup analyses are at risk of bias given loss of randomization when considering only subgroups.
Additional limitations of this meta-analysis stem mainly from the inherent limitations of included trials and their external validity. These trials included patients that had ‘uncomplicated bacteremia’ – these were mainly immunocompetent patients, hemodynamically stable and afebrile at time of antibiotic discontinuation, with a controlled infection. For these patients our results are valid. Regarding non-fermenters Gram-negative uncomplicated bacteremia, the number of patients included was limited. Two retrospective studies evaluating therapy duration for uncomplicated Pseudomonas aeruginosa bacteremia demonstrated no significant difference in mortality or relapse between short and long courses,29,30 however in a recent RCT, 8 versus 15 days of antibiotics for P. aeruginosa ventilator associated pneumonia resulted in higher recurrence rate.31 Further studies are needed in order to define optimal duration of therapy for P. aeruginosa and other non-fermenters bacteremia.
Von-Dach et al. included in their trial a CRP-based duration arm. For patients included in this arm it was allowed to discontinue antibiotics when CRP declined by 75% from peak. Median antibiotic duration in this arm was 7 days (interquartile range, 6–10 days), and all outcomes were non-inferior compared to the 14 days arm.6 Future studies should examine biomarker-guided strategy for defining antibiotic duration.
We planned this systematic review as a living systematic review and meta-analysis in light of a large ongoing trial that may provide important additional data on the topic. This trial is currently recruiting patients; and includes patients any bacteremia for the comparison of 7 versus 14 days of antibiotic therapy.15 Two pilot RCTs were performed to evaluate the feasibility of this trial in ICU and ward patients. These were not included in our meta-analysis, since no relevant outcomes per study arm were reported.32,33
In conclusion, for patients with uncomplicated and controlled Gram-negative bacteremia, 7 days of antibiotic therapy for enterobacterales bacteremia result in similar outcomes as 14 days, in terms of mortality, relapse, complications of infection, resistance emergence, and adverse events. These results apply for any adult age group, gender, source of infection, immune status, and hemodynamic status on presentation. Future RCTs should address the duration of therapy for Gram-negative non-fermenters bacteremia.
Contributors
AT, MP, LL and DY conceived the study idea and wrote the protocol for the study. All authors contributed to the review of the final manuscript. EvD, JM, EF, FK, DY, YDB, CM, JRB, JMC, and AH contributed to the data collection and organization. AT, MP, LL and DY had full access to all the information for the paper and have verified all data included in the review. AT, MP, LL and DY performed the data analysis. AT and DY wrote the draft for the manuscript. All authors reviewed and supervised the manuscript. All authors have read and agreed to the published version of the manuscript.
Data sharing statement
The data that support the findings of this study are not publicly available due to privacy and ethical restrictions. All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Declaration of interests
We declare no competing interests.
Acknowledgments
There was no funding source for this study.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2022.101750.
Appendix A. Supplementary data
References
- 1.de Kraker M.E.A., Jarlier V., Monen J.C.M., Heuer O.E., van de Sande N., Grundmann H. The changing epidemiology of bacteraemias in Europe: trends from the European antimicrobial resistance surveillance system. Clin Microbiol Infect. 2013;19:860–868. doi: 10.1111/1469-0691.12028. [DOI] [PubMed] [Google Scholar]
- 2.Deen J., von Seidlein L., Andersen F., Elle N., White N.J., Lubell Y. Community-acquired bacterial bloodstream infections in developing countries in south and southeast Asia: a systematic review. Lancet Infect Dis. 2012;12:480–487. doi: 10.1016/S1473-3099(12)70028-2. [DOI] [PubMed] [Google Scholar]
- 3.Vaughn V.M., Flanders S.A., Snyder A., et al. Excess antibiotic treatment duration and adverse events in patients hospitalized with pneumonia: a multihospital cohort study. Ann Intern Med. 2019;171:153–163. doi: 10.7326/M18-3640. [DOI] [PubMed] [Google Scholar]
- 4.Spellberg B., Rice L.B. Duration of antibiotic therapy: shorter is better. Ann Intern Med. 2019;171:210–211. doi: 10.7326/M19-1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yahav D., Franceschini E., Koppel F., et al. Seven versus 14 Days of antibiotic therapy for uncomplicated gram-negative bacteremia: a noninferiority randomized controlled trial. Clin Infect Dis. 2019;69:1091–1098. doi: 10.1093/cid/ciy1054. [DOI] [PubMed] [Google Scholar]
- 6.von Dach E., Albrich W.C., Brunel A.-S., et al. Effect of C-reactive protein-guided antibiotic treatment duration, 7-day treatment, or 14-day treatment on 30-day clinical failure rate in patients with uncomplicated gram-negative bacteremia: a randomized clinical trial. JAMA. 2020;323:2160–2169. doi: 10.1001/jama.2020.6348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Molina J., Montero-Mateos E., Praena-Segovia J., et al. Seven-versus 14-day course of antibiotics for the treatment of bloodstream infections by Enterobacterales: a randomized, controlled trial. Clin Microbiol Infect. 2022;28:550–557. doi: 10.1016/j.cmi.2021.09.001. [DOI] [PubMed] [Google Scholar]
- 8.Mermel L.A., Allon M., Bouza E., et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 update by the infectious diseases society of America. Clin Infect Dis. 2009;49:1–45. doi: 10.1086/599376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shariff S.Z., Cuerden M.S., Jain A.K., Garg A.X. The secret of immortal time bias in epidemiologic studies. J Am Soc Nephrol. 2008;19:841–843. doi: 10.1681/ASN.2007121354. [DOI] [PubMed] [Google Scholar]
- 10.About IPD meta-analyses/ipdma/about-ipd-meta-analyses. 2020. [Google Scholar]
- 11.Riley R.D., Lambert P.C., Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ. 2010;340:c221. doi: 10.1136/bmj.c221. [DOI] [PubMed] [Google Scholar]
- 12.Stewart L.A., Clarke M., Rovers M., et al. Preferred reporting items for systematic review and meta-analyses of individual participant data: the PRISMA-IPD statement. JAMA. 2015;313:1657–1665. doi: 10.1001/jama.2015.3656. [DOI] [PubMed] [Google Scholar]
- 13.Frequently asked questions/ipdma/frequently-asked-questions. 2020. [Google Scholar]
- 14.Living systematic reviews. 2020. https://community.cochrane.org/review-production/production-resources/living-systematic-reviews [Google Scholar]
- 15.Sunnybrook Health Sciences Centre . 2019. Bacteremia Antibiotic Length Actually Needed for Clinical Effectiveness: Randomized Controlled Trial. clinicaltrials.gov.https://clinicaltrials.gov/ct2/show/NCT03005145 [Google Scholar]
- 16.Harris P.N.A., McNamara J.F., Lye D.C., et al. Proposed primary endpoints for use in clinical trials that compare treatment options for bloodstream infection in adults: a consensus definition. Clin Microbiol Infect. 2017;23:533–541. doi: 10.1016/j.cmi.2016.10.023. [DOI] [PubMed] [Google Scholar]
- 17.Cochrane Handbook for Systematic Reviews of Interventions./handbook. 2020. [Google Scholar]
- 18.Lee C.-C., Hsieh C.-C., Yang C.-Y., et al. Short versus long duration antimicrobial treatment for community-onset bacteraemia: a propensity score matching study. Int J Antimicrob Agents. 2019;54:176–183. doi: 10.1016/j.ijantimicag.2019.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Sousa A., Pérez-Rodríguez M.T., Suárez M., et al. Short- versus long-course therapy in gram-negative bacilli bloodstream infections. Eur J Clin Microbiol Infect Dis. 2019;38:851–857. doi: 10.1007/s10096-019-03467-5. [DOI] [PubMed] [Google Scholar]
- 20.Giannella M., Pascale R., Toschi A., et al. Treatment duration for Escherichia coli bloodstream infection and outcomes: retrospective single-centre study. Clin Microbiol Infect. 2018;24:1077–1083. doi: 10.1016/j.cmi.2018.01.013. [DOI] [PubMed] [Google Scholar]
- 21.Doi A., Morimoto T., Iwata K. Shorter duration of antibiotic treatment for acute bacteraemic cholangitis with successful biliary drainage: a retrospective cohort study. Clin Microbiol Infect. 2018;24:1184–1189. doi: 10.1016/j.cmi.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 22.Mercuro N.J., Stogsdill P., Wungwattana M. Retrospective analysis comparing oral stepdown therapy for enterobacteriaceae bloodstream infections: fluoroquinolones versus β-lactams. Int J Antimicrob Agents. 2018;51:687–692. doi: 10.1016/j.ijantimicag.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 23.Chotiprasitsakul D., Han J.H., Cosgrove S.E., et al. Comparing the outcomes of adults with enterobacteriaceae bacteremia receiving short-course versus prolonged-course antibiotic therapy in a multicenter, propensity score-matched cohort. Clin Infect Dis. 2018;66:172–177. doi: 10.1093/cid/cix767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nelson A.N., Justo J.A., Bookstaver P.B., Kohn J., Albrecht H., Al-Hasan M.N. Optimal duration of antimicrobial therapy for uncomplicated Gram-negative bloodstream infections. Infection. 2017;45:613–620. doi: 10.1007/s15010-017-1020-5. [DOI] [PubMed] [Google Scholar]
- 25.Swamy S., Sharma R. 714Gram negative bacteremia: are shorter courses of antimicrobial therapy feasible? Open Forum Infect Dis. 2014;1:S201–S202. [Google Scholar]
- 26.Uno S., Hase R., Kobayashi M., et al. Short-course antimicrobial treatment for acute cholangitis with Gram-negative bacillary bacteremia. Int J Infect Dis. 2017;55:81–85. doi: 10.1016/j.ijid.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 27.Park S.H., Milstone A.M., Diener-West M., Nussenblatt V., Cosgrove S.E., Tamma P.D. Short versus prolonged courses of antibiotic therapy for children with uncomplicated Gram-negative bacteraemia. J Antimicrob Chemother. 2014;69:779–785. doi: 10.1093/jac/dkt424. [DOI] [PubMed] [Google Scholar]
- 28.Hojat L.S., Bessesen M.T., Huang M., et al. Effectiveness of shorter versus longer durations of therapy for common inpatient infections associated with bacteremia: a multicenter, propensity-weighted cohort study. Clin Infect Dis. 2020;71:3071–3078. doi: 10.1093/cid/ciz1197. [DOI] [PubMed] [Google Scholar]
- 29.Babich T., Naucler P., Valik J.K., et al. Duration of treatment for Pseudomonas aeruginosa bacteremia: a retrospective study. Infect Dis Ther. 2022 doi: 10.1007/s40121-022-00657-1. published online May 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fabre V., Amoah J., Cosgrove S.E., Tamma P.D. Antibiotic therapy for Pseudomonas aeruginosa bloodstream infections: how long is long enough? Clin Infect Dis. 2019 doi: 10.1093/cid/ciz223. published online March 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bouglé A., Tuffet S., Federici L., et al. Comparison of 8 versus 15 days of antibiotic therapy for Pseudomonas aeruginosa ventilator-associated pneumonia in adults: a randomized, controlled, open-label trial. Intensive Care Med. 2022 doi: 10.1007/s00134-022-06690-5. published online May 13. [DOI] [PubMed] [Google Scholar]
- 32.Daneman N., Rishu A.H., Pinto R., et al. 7 versus 14 days of antibiotic treatment for critically ill patients with bloodstream infection: a pilot randomized clinical trial. Trials. 2018;19:111. doi: 10.1186/s13063-018-2474-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Daneman N., Rishu A.H., Pinto R., et al. A pilot randomized controlled trial of 7 versus 14 days of antibiotic treatment for bloodstream infection on non-intensive care versus intensive care wards. Trials. 2020;21:92. doi: 10.1186/s13063-019-4033-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.