Abstract
Background
Positive psychological well‐being (PPWB) is generally associated with improved physical health, mental well‐being, and healthy behaviors. However, it is not clear how PPWB differs in women with obesity or if improving PPWB will improve their health. The objective of this study was to summarize the evidence on PPWB in women with obesity.
Method
A scoping review was conducted in APA PsycINFO, EMBASE, MEDLINE, Cochrane Central Register of Controlled Trials, CINAHL, SocINDEX, Family & Society Studies Worldwide, ProQuest Dissertations and Theses Global databases. Primary research studies, with an analysis of adult women with a BMI ≥30 kg/m2 with measures of PPWB are included.
Results
Thirty‐two studies encompassing >57,000 women with obesity, measured constructs of PPWB included: self‐esteem, life satisfaction, positive affect, social support, vitality, happiness, self‐acceptance, and optimism. Most studies showed that PPWB was lower in women with obesity although this association dissipated in studies when health and negative social factors were considered. Improvements in PPWB were associated with weight loss and with successful lifestyle changes with and without weight loss. Positive psychological interventions (PPIs) were used to bolster psychological well‐being. PPIs were associated with improved measures of self‐esteem and well‐being.
Conclusions
Prospective longitudinal and intervention studies are required to understand how evaluating and fostering PPWB might support gender‐informed obesity care.
Keywords: obesity, positive psychological wellbeing, women
1. INTRODUCTION
There is an association between positive psychological well‐being (PPWB) and improved health in general, yet the role of PPWB in improving health for women with obesity, is not clear. Positive psychological well‐being (PPWB) is associated with improved physical health, mental well‐being, and healthy behaviors. 1 While some researchers find women with obesity have lower psychological well‐being, 2 others dispute this association. 3 Women with obesity disproportionately face poorer health, 4 , 5 poorer mental well‐being, 6 weight discrimination, 7 and demotivated health behaviors. 8 , 9 , 10 , 11 Enhancing PPWB may improve positive health behaviors and buffer the effects of negative self‐beliefs and negative health outcomes in women with obesity 9 , 12 , 13 but the evidence to support this is limited. A systematic scoping review of the literature is needed to identify and describe the primary research on PPWB and women with obesity.
Positive psychology is the study of well‐being, and flourishing is the goal of therapy. 14 From this perspective, well‐being is not the absence of negative function (e.g., depression, loneliness) but rather the presence of positive functions. 15 Positive psychologists aim to support people to feel good about themselves, to feel fulfilled, and ultimately to flourish within their own unique circumstances. 14 The goal of interventions in positive psychology is to nurture strengths rather than repair weaknesses. 16
PPWB is a term used to describe positive psychological attributes studied in positive psychology. For the purpose of this scoping review, PPWB is defined as a multi‐dimensional construct that includes the domains of positive emotions, positive relationships, positive characteristics, and positive functions. 14 , 17 Specifically, the constructs included in this review are: gratitude, optimism, self‐compassion, positive relationships, engagement, self‐esteem, happiness, self‐love, self‐acceptance, accomplishment, vitality, resilience, body acceptance, body love, purpose, and meaning. 14 , 17
PPWB is associated with higher psychological functioning, 16 lower incidence of chronic diseases (e.g., gastrointestinal disease, arthritis), 18 lower risk of cardiovascular events, 19 and improved health behaviors such as regular exercise, restful sleep, and a decreased sedentary behavior. 1 In cardiovascular (CV) research, certain aspects of PPWB (e.g., optimism, purpose, happiness) are associated with decreased CV morbidity and mortality in those with and without CV disease. 20 , 21 The American Heart Association asserts that PPWB should be considered an independent factor as current data strongly suggest a causal role in better cardiovascular health. 20
PPWB is thought to improve health through three pathways: biological (e.g., increased endorphins decrease blood pressure), behavioral (e.g., increased ability to engage in health behaviors such as regular sleep, exercise, and/or nutritious eating), and psychosocial (e.g., increased engagement of social support and self‐regulation to buffer stress and reduce negative stress hormones). 2 It is speculated that there is a bidirectional relationship between healthy lifestyle behaviors and positive wellbeing (e.g., exercise makes you feel good and when you feel good its easier to exercise). 1
Although all people may benefit from higher elements of PPWB (e.g., self‐esteem, resilience, self‐compassion), women with obesity differ from men with obesity. In women, a higher BMI predicts lower general psychological well‐being but not in men. 2 Women's appraisal of their body image and quality of life are also negatively impacted by obesity. 11 , 22 , 23 Women with obesity are particularly at risk for having poorer overall health, socioeconomic status, education, and employment compared to non‐obese women or men. 9 , 24 These differences are thought to be related to gendered cultural norms as well as weight stigmatization and discrimination. 2 , 9 Women with obesity experience higher rates of weight discrimination than men. 7 Weight discrimination is associated with an increased risk of negative physical, mental, and social health and even morbidity. 9 , 25 With these notable differences in women and an awareness that sex and gender differences in general affect health outcomes, 26 research that focus on women with obesity is warranted.
A scoping review was undertaken to map the available research on PPWB and women with obesity to provide an overview of the current evidence. 27 The objective of this scoping review was to investigate what is known about PPWB in women classified as obese. More specifically, what constructs of PPWB were measured; how they were measured; what types of research methods were used to examine PPWB and what did they find; what positive psychological interventions (PPIs) were used to improve well‐being, health behaviors or general health; and lastly to identify what gaps exist in research that require further study.
2. METHODS
The Joanna Briggs Institute (JBI) guidelines for conducting scoping reviews informed the conduct of this review. PRISMA‐ScR reporting guidelines were used to report our findings. 27 , 28 , 29 , 30 The JBI scoping review guidelines outline the following as components of a scoping review: the review question articulated with the mnemonic PCC (population, concept, context), a protocol (available on request), a comprehensive and reproducible search strategy, a source of evidence selection, data extraction, an analysis of evidence, and the presentation of results. Three steps were used in the search strategy for this review. First, a discovery search of Google Scholar was conducted using key studies, which were then analyzed to identify key words and subject headings from titles and abstracts. Second, this analysis provided a foundation for the development of a comprehensive search in APA PscycInfo (OVID). Search development was led by a professional health sciences librarian (KAH). The full search strategies are available in the Appendix. The search was then adapted for the following databases: EMBASE (OVID), Medline and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations and Daily (OVID), Cochrane Central Register of Controlled Trials (OVID), CINAHL Plus with Full Text (Ebsco), SocINDEX with Full Text (Ebsco), Family & Society Studies Worldwide (Ebsco), and ProQuest Dissertations and Theses Global. Finally, all of the reference lists of the included studies were searched for additional studies. 27 The original search was conducted in August of 2019 and was updated December 2020. Another update followed in December 2021, when in addition to searching for any new studies from that year, the original search was re‐run adding the terms flourish, meaning and accomplishment.
2.1. Inclusion and exclusion criteria
Inclusion criteria were primary research using any method (i.e., quantitative, qualitative, mixed methods), written in English, and in which PPWB measures were used with adult females (≥18 years of age) with obesity (BMI ≥ 30 kg/m2). The term obesity is used to describe a weight category (BMI ≥ 30 kg/m2) not a disease. The context of the research was open to women with obesity in different geographical, health care, or sociocultural settings. Studies in which males were included had to present specific results for the female cohort. No date restrictions were specified, and all years included in each database were searched. Exclusion criteria were articles that were not academically peer reviewed (e.g., opinion, popular culture, self‐help materials), conference abstracts, books/book chapters, editorials texts, or studies that focused on pregnant women.
3. RESULTS
The original (August 2019) and updated (December 2020 and 2021) searches yielded 12,729 records; after duplicates were removed, 7284 records remained. Using the inclusion and exclusion criteria, two authors (HC, KKS) independently screened the records by title and abstract using CovidenceTM software. 31 This tool allowed each reviewer to track and ‘vote’ on each record. Any disagreement (n = 154, 98% agreement) on inclusion was resolved through discussion. Once this initial process was complete, the full text articles were uploaded (n = 139) to CovidenceTM and screened for inclusion. This resulted in 25 included studies. Then references from the 25 studies were reviewed and seven more studies that met the inclusion criteria were identified. Thirty‐two studies were thus included in this review (PRISMA‐ScR diagram 32 Figure 1). A data extraction form was prepared (by HC and KKS) to assist with summarizing relevant details from each article. Studies were read and reread to map and group evidence. Extraction was initially undertaken by HC then reviewed, edited, and verified by KKS. Study characteristics are illustrated in Table 1.
FIGURE 1.
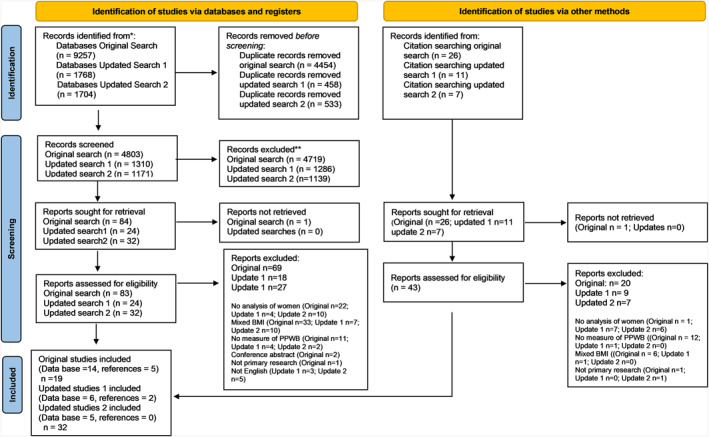
PRISMA‐SrR flow diagram
TABLE 1.
Data extraction
| First Author setting discipline | Participants | Design and positive wellbeing outcomes | Positive wellbeing measures | Results | Comment |
|---|---|---|---|---|---|
|
Acmaz, G. (2013) Turkey Medicine |
N = 133 women (n = 47 control; n = 86 with polycystic ovary syndrome (PCOS) sub‐groups: n = 35 Hirsutism‐acne (HA), n = 22 infertility and, n = 26 obesity Age: Control 27.8 (SD 6.5), HA 26.1 years (SD 5.0), infertility 24.3 years (SD 5.0), obesity 26.0 years (SD 6.58) Mean BMI: Control 23.4 kg/m2 (SD 3.1), HA 24.5 kg/m2 (SD 2.8), infertility 24.4 kg/m2(SD 3.5), obesity 33.6 kg/m2 (SD 2.6) Recruited from a polyclinic and control from unknown group |
Design: Cross‐sectional survey comparing aspects of health in groups of women grouped by PCOS symptoms and women with no illness. Outcomes: Self‐esteem, vitality Attrition: N/A |
Rosenberg self‐esteem scale (RSES) SF‐36: vitality | Women with PCOS and obesity rated their self‐esteem lower than other women with PCOS only and the control group (p < 0.001). All women with PCOS had lower vitality compared to the control group (p < 0.001). | Women with PCOS, regardless of their sub‐group reported lower vitality when compared with a healthy control group. Women with PCOS and obesity were more likely to rate their self‐esteem low compared to others with PCOS only or controls. |
|
Ahmed, H. (2018) Iraq Medicine |
N = 40 women Age: 25–35 years Mean BMI: 43 kg/m2 (range 40–50 kg/m2) Recruited from surgical candidates having sleeve gastrectomy |
Design: Prospective longitudinal with 12‐month follow‐up Outcomes: Elements of QOL Attrition: none |
QOL five‐point Likert scale: Self‐esteem, happiness, time with friends |
All QOL measures were improved at 12‐month follow‐up including: Self‐esteem, spending time with friends, and feeling happy (p = 0.034). | One year after sleeve gastrectomy and subsequent weight loss, women reported improved self‐esteem, feeling happy and spending time with friends. |
|
Ahmed, H. (2019) Iraq Medicine |
N = 80 women Age: 20–39 years Mean BMI: 36 kg/m2 (range 31–39.9 kg/m2) Recruited from a private hospital and private clinic |
Design: Non‐randomized descriptive longitudinal study with 6‐month treatment of either n = 40 Atkins diet or n = 40 gastric balloon. 12‐month follow‐up Outcomes: Elements of QOL Attrition: None |
QOL five‐point Likert scale: Self‐esteem happiness, time with friends | All participants reported feeling happier, improved self‐esteem, spending time with friends. The gastric balloon group lost more weight than the Atkins diet group (p < 0.001) had greater improvements in feeling happy p = 0.005, improved self‐esteem p = 0.059 and spending more time with friends, p = 0.02. | PPWB measures including happiness, self‐esteem, and spending time with friends improved significantly in all women who lost weight with either gastric balloon insertion or Atkins. However, the gastric balloon group lost more weight than the Atkins group and had greater improvements in PPWB measurements. |
|
Bacon, L. (2005) USA Nutrition |
N = 78 women Age: 30–45 years Mean BMI: Health at Every size (HAES) group 35.9 kg/m2 (SD 4.6), Mean BMI: Diet group 36.7 kg/m2 (SD 4.2) Recruited from community |
Design: RCT* HAES versus diet program; treatment included 24, 90‐min, weekly sessions plus 6 monthly optional sessions. 2‐year follow‐up Outcomes: Self‐esteem Attrition: HAES 10/39 Diet group 16/39 |
RSES |
HAES group: Increased self‐esteem (p < 0.001). Diet group: Decreased self‐esteem (p = 0.028) |
With no significant weight loss in either group, women in the HAES group improved self‐esteem while the diet groups self‐esteem worsened. |
|
Ball, K. (2004) Australia Exercise and Nutrition |
N = 7865 women (n = 519 with obesity) who completed 1996 survey. Age: 18–23 years BMI: ≥ 30 kg/m2 Recruited from urban and rural communities |
Design: Cross‐sectional survey from the Women's health Australia longitudinal study. 1996 survey data. Outcomes: Life satisfaction Attrition: N/A |
Life satisfaction survey: Achievements in work/career/study; family relationships; partner/close relationships; friendships; social activities. | Women with obesity reported less satisfaction in work/career/study (Odds Ratio (OR) = 0.79, confidence interval (CI) 0.66‐0.94), family relationships (OR = 0.82, CI 0.68‐0.98), partner relationships (OR = 0.55, CI 0.46‐0.65), and social activities (OR = 0.69, CI 0.58‐0.83), relative to women in the healthy weight group. There was no difference in satisfaction with friendships (OR = 1.0, CI 0.83‐1.19). | Women with obesity reported lower life satisfaction scores in work/career/study, family and partner relationships, and social activities when compared to women in healthy weight category. Friendships did not differ. |
|
Berman, M. (2016) USA Psychiatric medicine |
N = 21 women, with major depressive disorder Age: 23–66 years Mean BMI: 37 kg/m2 (range 31–50 kg/m2) Recruited from community |
Design: Longitudinal study with a pre‐ post‐treatment and 3‐month follow‐up; 11 weekly 2‐h group sessions of self‐acceptance‐based treatment (participants broken up into 2 groups, n = 11 and n = 10). Outcomes: Well‐being, body image acceptance Attrition: 3/21 |
Obesity related well‐being (ORWELL‐97), body image acceptance and Action questionnaire (BIAAQ) | Self‐acceptance intervention improved: Obesity‐related well‐being (p < 0.001) and body image acceptance (p < 0.001) post‐treatment. Improvements were maintained at 3‐month follow‐up. | A self‐acceptance‐based treatment, accept Yourself, improved well‐being in women with obesity and major depressive disorder. |
|
Böckerman P. (2014) Finland Economics/Applied science and mental health |
N = 2245 (women = 1134 with obesity = unknown) Age: 30–54 years BMI ≥30 kg/m2 Recruited from health 2000 survey of Finish people |
Design: Cross‐sectional survey of subjective well‐being (SWB) with full time working people outcomes: SWB Attrition: N/A |
Single SWB question with a 11‐point Likert sale: “All things considered how satisfied have you been with your life as a whole during the past 30 days?” | Obesity was associated with a decrease in subjective well‐being (p < 0.05) and this association disappeared when health status and functional capacity were added to the model. | Lower SWB was associated with obesity yet when health and functional capacity were considered this association disappeared. |
|
Bookwala, J. (2008) USA Psychology |
N = 3251 (women = 1588 with obesity = 373) Age: 25‐74 BMI: ≥30 kg/m2 Recruited from the national survey of Midlife development in the USA (MIDUS I) |
Design: Cross‐sectional survey of sex differences BMI and PWB Outcomes: Measured six domains of well‐being and combined them for a single composite measure Attrition: N/A |
Ryff's scale. (Positive relations with others, self‐acceptance, autonomy, personal growth, mastery, and purpose in life) | Having a higher BMI was associated with lower psychological well‐being in women (p < 0.001) but not men p = 0.906. | Women classified as obese had lower psychological well‐being when compared to women in the normal weight category. Men psychological well‐being did not differ significantly between BMI groups. |
|
Borkoles, E. (2016) England Psychology/Exercise Physiology |
N = 62 women (non‐dieting lifestyle intervention n = 31, waitlist control n = 31) Age: 24–55 years BMI: >35.0 kg/m2 Recruited from community |
Design: RCT* examining 12‐week non‐dieting lifestyle intervention followed by 40‐week maintenance phase versus waitlist control; 1‐year follow‐up Outcomes: General well‐being, self‐perception, self‐esteem Attrition: 15/31 intervention, 15/31 wait‐list control |
General well‐being Schedule (GWB), self‐perception profile (SPP) measure of self‐esteem | Significant improvement in well‐being (29.9%, p < 0.001), and self‐perceptions (no data). | A non‐dieting lifestyle intervention improved well‐being and self‐perceptions from baseline to end of treatment, and over the 40‐week follow‐up |
|
Brown, W.J. (2000) Australia Human Movement/Gender and Health/Psychology/Population Health |
N = 14,762 women (n = 742 with obesity who completed 1996 surveys) Age: 18–23 years BMI: >30 kg/m2 Recruited from urban and rural communities |
Design: Cross‐sectional survey from the Womens health Australia longitudinal study. 1996 survey data Outcomes: Mental wellbeing. Attrition: N/A |
SF‐36: vitality | Women classified as overweight and obesity reported lower vitality when compared to women classified as normal or underweight. (p < 0.05). | Young Australian women with obesity reported lower vitality than peers classified as normal or underweight. |
|
Burns, D. (2021) USA Nursing |
N = 87 women with obesity Age: 30–44 years BMI: ≥30 kg/m2 Recruited from Facebook groups targeted 30–44‐year‐old Latino women |
Design: Cross‐sectional survey examining associations between self‐esteem, body dissatisfaction and the effect on internalized weight stigma (IWS). Outcomes: Self‐esteem Attrition: N/A |
RSES | When self‐esteem decreased by one unit (4‐point scale), body dissatisfaction increased by 0.270 (7‐point scale) (p < 0.001).Both self‐esteem (p < 0.001) and body dissatisfaction (p < 0.008) predicted IWS. | Lower self‐esteem is associated with a higher body dissatisfaction in Latino women with obesity. Self‐esteem and body dissatisfaction were predictors of IWS. |
|
Crerand, C. (2007) USA Medicine/Psychology |
N = 123 women (diet intervention n = 84, non‐dieting program n = 39) Mean age: 44.3 years diet intervention, 43.9 years non‐dieting program Mean BMI: 36.2 kg/m2 diet intervention, 35.5 kg/m2 non‐dieting group Recruited from community |
Design: RCT* Meal replacement or balanced deficit diet (LEARN program for weight control), versus non‐dieting program (Self‐Esteem Comes in all Sizes), with weekly meetings for the first 20 weeks lead by psychologist and RD) and biweekly for the following 20 weeks. Outcomes: Self‐esteem Attrition: Not reported |
RSES | There was an improvement in all participants' self‐esteem (p < 0.001) with no significant differences between groups at either the 20‐ or 40‐week follow‐up. | There was overall improvement in self‐esteem. Group assignment did not influence improvement. |
|
Godoy‐Izquierdo, D. (2020) Spain Psychology |
N = 100 (60 women, with 69 classified as overweight and 31 with obesity) Age: 19–57 years Mean BMI: Overweight 26.6 kg/m2 obese 33.5 kg/m2 Recruited from two primary care medical setting. |
Design: Cross‐sectional survey Outcomes: Positivity and SWB (reported with happiness scale) Attrition: N/A |
8‐Item positivity scale Single happiness question with a 11‐point Likert scale: “How happy are you at the present?” | No differences in positivity scores between overweight or obese participants. Obese individuals had significantly lower happiness scores (p = 0.014). BMI did not predict happiness after body satisfaction (p = 0.12 and positivity (p = 0.000) were considered. Self‐stigma explained variance in happiness (p < 0.001) but not when positivity included in model. | Women and men with obesity had significantly lower happiness scores compared to people who were overweigh. However, individuals with obesity who had higher positivity traits and higher body satisfaction were more likely to be happy. Authors suggest that positivity may supress the effects of self stigma. |
|
Groh, C. (2015) USA Nursing |
N = 106 African American women Age: 19–64 years Mean BMI: 41.2 kg/m2 (8.3) Recruited from a nurse managed center for underinsured and primary care clinic for uninsured in large urban center |
Design: Longitudinal study. Repeat measures intervention (24‐week) 12 weeks of exercise, educational sessions, scripture reading followed by 12 weeks with no intervention. 12 & 24‐week follow‐up Outcomes: Subscales of SF‐36: Vitality Attrition: 51/106 |
SF‐36v2: vitality | Improvements from base line to 24 weeks were found in vitality (p < 0.001) after interventions. | Improvement in vitality after the 12‐week program. Gains declined 12 weeks post‐intervention, yet improvements remained significant. |
|
Hill, A.J. (1998) England Psychiatry |
N = 179 women Age: 18–75 years BMI: >30.0 kg/m2 Recruited from subscribers to a magazine for women size 16+ |
Design: Cross‐sectional survey with women divided into three obesity categories assessing predictors of psychological distress Outcomes: Self‐esteem Attrition: N/A |
RSES with added questions on social life | Self‐ esteem decreased as weight increased (p < 0.001). Lower self‐esteem (p < 0.001) and peer relationships (p < 0.01) scores predicted lower mental health inventory scores regardless of weight category. | Self‐esteem decreased as weight increased. Yet, BMI alone did not predict mental health scores; low self‐esteem and social relationships predicted lower mental health scores. |
|
Jorm, A. (2003) Australia Medicine/Psychology |
N = 6919 (n = 574 women and n = 492 men with obesity) Age: Groups: 20–24 years n = 2280, 40–44 years n = 2334, 60–64 years n = 2305 BMI: >30.0 kg/m2 Recruitment from a random sample of participants from a longitudinal community study (PATH through life Project). |
Design: Cross‐sectional survey of three age groups and four weight categories (under weight, acceptable, overweight, & obese). Outcomes: positive affect measures. Attrition: N/A |
PANAS | Women with obesity had lower positive affect (p < 0.001). However, when physical health, vigorous activity, negative support from family, years of education, and financial problems were controlled the association was not significant. | Women with obesity had lower positive affect than women classified as acceptable weight. This association was gone after controlling for negative physical and social factors. |
|
Laferrere, B. (2002) USA Medicine |
N = 145 women Mean age: 46.3 ± 11.1 years Mean BMI: 35.2 ± 4.2 kg/m2 Recruited from middle class urban community |
Design: Cross‐sectional survey of pre and post menopausal African american (AA) n = 80 and white women (W) n = 65. Outcomes: Medical outcomes study Short (MOS‐SF‐36): Survey includes life satisfaction, self‐esteem, vitality, social activity. Attrition: N/A |
SWLS RSES SF‐36:Vitality | No difference between AA and W women self‐esteem or life satisfaction. Yet there were differences between pre and post menopausal women pre‐menopause women had less vitality (p = 0.001), life satisfaction (p < 0.01). | No difference in life satisfaction and self‐esteem were found between African american and white women with obesity. Post‐menopausal AA women had more vitality and life satisfaction compared to pre‐menopausal AA women. |
|
Latif, E. (2014) Economics Canada |
N = 28,952 (n = 6006 women, n = 5837 with obesity) Mean age: women 46.7 years, men 44 years BMI: Obesity ≥30.0 kg/m2 obesity Recruited from the Canadian national Public survey 1994‐2006 |
Design: Cross‐sectional survey Outcomes: Happiness Attrition: N/A |
Single happiness question with 5 ordered choices: So unhappy in life, very unhappy, somewhat unhappy, somewhat happy, and happy in life | Obesity is associated with a reduction in happiness in women between the ages of 25‐54 (p = 0.04). Obesity was not associated with happiness in men. Statistical model controlled for age, marital statis, education, income, urban location, own home, and provinces. | Obesity is associated with reduced happiness in women between the ages of 25‐54. Obesity is not associated with happiness in men. |
|
Mensinger, J. (2016) USA Psychology/Population health |
N = 80 women Age: 30–45 years BMI: 30–45 kg/m2 Recruited from community |
Design: RCT* comparing 6‐month group‐based weight ‐neutral (HUGS program) or weight‐loss interventions with 2‐year follow‐up Outcome: Self‐esteem Attrition: Weight‐loss: 6‐month 7/40 24‐ month 19/40, weight‐neutral: 6‐month 1/40 24‐month 21/40 |
RSES | Both groups increased self‐esteem (p < 0.001) | Women in both interventions significantly increased their self‐esteem. |
|
Pasco, J. (2013) Australia Medicine/Psychiatry |
N = 273 women (n = 68 with obesity) Age: 29‐84 BMI: ≥30 kg/m2 Recruited from the Geelong Osteoporosis study from general population |
Design: Cross‐sectional survey Outcomes: positive and negative affect Attrition: N/A |
PANAS | No association between BMI category and positive affect. Obesity was associated with high negative affect (OR 1.95 CI 0.57‐1.69) and physical illness explained this association. | Women's positive affect was not associated with their BMI category. |
|
Polat, H. (2020) Turkey Nursing |
N = 90 women Mean age: 32.98 ± 7.74 years Mean BMI: 40.10 ± 5.14 kg/m2 Recruited from a University hospital dietitian department |
Design: Cross‐sectional Outcome: Self‐esteem Attrition: N/A |
RSEM | Women with obesity had moderate levels of self‐esteem. Self‐esteem was higher in those who were physically active (p < 0.05). Positive association between self‐esteem and sexual quality of life (p < 0.01). | Obese women had moderate levels of self‐esteem. Exercise enhanced self‐esteem. High self esteem was associated with improved sexual quality of life in women with obesity. |
|
Ripsch, J. (2002) USA Social work PhD Thesis |
N = 13 women Age: 32–53 years Mean BMI: 37 kg/m2 Recruitment from a snowball sampling from a University and community. |
Design: Grounded theory Women with obesity who reported positive sense of self on the Orientation to life questionnaire) were interviewed. Outcomes: Theory development on how women maintained a positive sense of self Attrition: none |
Orientation to life questionnaire | Participants chose to have a positive sense of self irrespective of their weight. They shared supportive relationships with friends, family and/or mentors, developed skills and competencies, cared for others, and engaged in positive self talk. | Women with obesity attributed their positive sense of self to interpersonal connections, positive self‐talk as well as their skills and abilities. |
|
Rodino, I. (2016) Australia Psychology |
N = 403 women (n = 73 with obesity) Age: 34.5 years (SD = 4.8) BMI: >30 kg/m2 Recruited from an infertility clinic |
Design: Cross‐sectional survey examining wellbeing of women with and without polycystic ovary syndrome Outcomes: positive affect and self‐esteem Attrition: 445/1000 participants returned survey |
PANAS RSES | Women with obesity exhibited lower levels of self‐esteem as compared to their normal weight and overweight counterparts (p < 0.001). Higher self‐esteem was associated with a higher positive affect (p < 0.001). | Women with obesity scored lower in self‐esteem. Higher self‐esteem was associated with a higher level of positive affect. |
|
Sarwer, D (2013) USA Medicine/Psychiatry |
N = 390 women (n = 311) Mean age: 51.5 (SD = 11.5) BMI: 30.0–50.0 kg/m2 Recruited from six primary care practices |
Design: RCT* with three arms: usual care, brief lifestyle counseling (BLC) or enhanced LC (ELC). Women were followed for 2 years. Outcomes: Self‐esteem Attrition: 20/130 usual care, 19/130 B LC, 15/129 ELC |
Impact of weight on quality of life‐Lite (IWQOL) | A mean population weight loss of 3.7 kg ± 0.4% at 12 months and 3.0 ± 0.4% at 24 months was associated with improved self‐esteem (p < 0.001) in women. | Women's self‐esteem measures improved significantly with modest weight reduction regardless of treatment stream, |
|
Sato, K. (2020) Japan Political science |
N = 6359 women and men in China/USA (n = 1380/4979). Number of women with obesity not reported. Mean age: China/USA women 46.1/50.5 years, men 45.5/49.0 years BMI: ≥30 kg/m2 Recruited between 2009 and 2013 |
Design: Cross‐sectional survey subjective well‐being (happiness) Outcome: Happiness Attrition: N/A``` |
Single happiness question with 11‐point Likert scale: “ overall, how happy would you say you are currently?” | No significant association between obesity and happiness in women overall. Obese men in China were happier (p < 0.001) than obese men in USA. | There was no association with obesity and happiness in women from China and USA. |
|
Smith (2014) USA Nursing |
N = 68 women Age: 18–24 years Mean BMI: 35.6 (5.1) kg/m2 Recruited from a community healthcare center |
Design: Cross‐sectional survey of young women with obesity Outcomes: Self‐esteem Attrition: N/A |
RSES | Self‐esteem had a strong inverse association with stress (r = − 0.6, p < 0.001), and loneliness (r = −0.69, p < 0.001). Women who rated their health poor/fair had lower self‐esteem (p = 0.001) compared to those who rated their health good/very good. | Poor self‐esteem was associated with stress, and loneliness in women with obesity. Poor self‐esteem was also associated with personal assessment of poor/fair health. |
|
Toft B. (2020) Denmark Lifestyle Rehabilitation/Nursing |
N = 10 (n = 5 women, n = 5 men) Age: 30–69 years BMI: 40–48 kg/m2 Recruited from a lifestyle intervention hospital program |
Design: Qualitative Hermeneutic. Interviews were conducted 18 months after a 12‐month health promotion intervention by an interdisciplinary team Outcome: Barriers and facilitators of well‐being Attrition: one woman |
Well‐being defined by womens descriptions of elevated mood and vitality | Women participants appreciated how the process of vitality gave them the desire and courage to stay committed to healthy living. Vitality came from reducing self‐blame, strengthening confidence and a strong sense of self. | Women found increasing their pride, confidence and self‐acceptance improved their mood and vitality which enabled them to engage in an active everyday life. |
|
Ul‐Haq, Z. (2014) UK Public health |
N = 163,066 (54.5% women) n = 39,941 classified obese Age: 30–72 years BMI: > 30.0 kg/m2 Recruited form biobank participants |
Design: Cross‐sectional Outcomes: Happiness Attrition: N/A |
Single happiness question with a 6‐chocies: “In general, how happy are you?” | Women with obesity had greater odds of being unhappy when compared to normal weight women (OR: Obesity Class l ‐ 1.27 (CI 1.16‐1.40 p < 0.001), Class ll‐ 1.41 (CI 1.23‐1.61, p < 0.001), Class lll‐ 2.11 (1.79‐2.49, p < 0.001). There was no association between happiness and obesity when self‐reported health (SRH) was included in the model | Women with obesity reported more unhappiness compared to those of normal weight. When adjusted for self‐reported health, the association between women with obesity and lower ratings of happiness disappeared. Author suggested self‐reported health may be a mediator of happiness. |
|
Unlu, S. (2019) Turkey Nutrition and Dietetics |
N = 250 women (80 in each category normal, overweight, and obese) Age: 18–64 years BMI: Obese group ≥30 kg/m2 Recruited from a family healthcare center |
Design: Cross‐sectional Outcomes: Self‐esteem Attrition: N/A |
Self‐esteem Inventory | Women with obesity were 12.19 times more likely to have lower low self‐esteem (p < 0.001). and 91.22 times more likely to have body dissatisfaction (p < 0.001) compared to the normal weight group. | Obesity negatively effects self‐esteem and body satisfaction. |
|
Wadsworth, T. (2014) USA Sociology |
N = 1,319,340, n = 82,116 women (33% with obesity), n = 498,224 men (32% with obesity) Mean age: Female 46.78 years, men 44.67 years BMI: Obese class I 30–34.9 kg/m2, class II 35–39.9 kg/m2, Class III >40 kg/m2 Corrected self‐reported weight Recruited from telephone survey across communities in the USA |
Design: Cross‐sectional Behavior risk factor Surveillance System (BRFSS) survey data 2005‐2008 Outcome: Life satisfaction Attrition: N/A |
Single life satisfaction question with 3 choices: “In general, how satisfied are you with your life?” | Women with class I obesity or class II or III report lower levels of life satisfaction compared to non obese women (OR 0.78, 0.57, p < 0.001). Although men with obesity also report lower levels of satisfaction, women were statistically lower (p = 0.001). Good health, being employed, white, married, and having higher education improve life satisfaction scores for women. | People with obesity report lower life satisfaction and this association is stronger for women than men. |
|
Wee, C. (2014) USA Medicine |
N = 337 (women/men with BMI ≥35 n = 230/107) Mean age 48.1 years BMI: ≥35 kg/m2 Recruited from four primary care practices in greater Boston |
Design: Cross‐sectional interview/survey. Examined how specific QOL domains explained health Utility (overall well‐being) in African american, Caucasian, and Hispanic population. Outcomes: Self‐esteem Attrition: N/A |
Impact of weight on quality of life‐lite (IWQOL‐lite)‐subscale self‐esteem | Self‐esteem did not explain diminished well‐being in women with obesity. Social stigma(public distress) and impaired sexual function were associated with lower well‐being (p < 0.05) | Self‐esteem was not associated with well‐being in African american, Caucasian, or Hispanic women with obesity. |
|
van Zutven, K. (2015) Australia Psychology |
N = 2734 (women/men classified non‐obese n = 1220/769, obese n = 276/169) Age 20–44 years BMI: Obese ≥30 kg/m2 Non‐obese 20–29.9 kg/m2 Recruited from 2006 Australian community survey (Food, Drink, lifestyle and wellbeing survey) |
Design: Cross‐sectional survey Outcomes: Satisfaction with life Attrition: N/A |
SWLS | Women with obesity had lower satisfaction with life scores than non‐obese women (<0.001). This relationship was not significant after considering health, weight and shape concerns and binge eating (p = 0.23). | Women with obesity had lower satisfaction with life than non‐obese participants. However, this association dissipated after considering health, weight/shape concerns, and binge eating. |
3.1. Study characteristics
The 32 studies included an analysis of more than 57,000 women, ages 18–84 years, who had a BMI greater than or equal to 30 kg/m2. The studies were conducted in the United States (n = 11), 2 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 Australia (n = 5), 45 , 46 , 47 , 48 , 49 , 50 England (n = 2), 51 , 52 Iraq (n = 2), 53 , 54 Turkey (n = 3), 55 , 56 , 57 Canada (n = 1), 58 Denmark (n = 1), 59 Finland (n = 1), 60 Japan (n = 1), 61 Spain (n = 1), 62 and United Kingdom (n = 1). 3 The disciplines of lead authors were predominantly psychology and medicine. Participants were recruited from a variety of locations including health centers, universities, and both urban and rural communities.
3.2. PPWB constructs and measures
Self‐esteem was the most frequently measured PPWB construct and was measured in 14 of the 32 studies. 33 , 35 , 37 , 38 , 40 , 41 , 43 , 44 , 48 , 51 , 52 , 55 , 56 , 57 Other constructs of PPWB included: life satisfaction 37 , 42 , 45 , 49 , 60 ; positive affect 47 , 50 , 51 , 62 ; social support 52 , 53 , 54 ; vitality 36 , 37 , 46 , 57 , 59 ; happiness 3 , 53 , 54 , 58 , 61 , 62 ; self‐acceptance 34 ; and optimism. 39 Various approaches were used to measure self‐esteem that included the Rosenberg Self Esteem Survey (RSES), 33 , 35 , 37 , 38 , 41 , 43 , 48 , 52 , 56 , 57 the Self Perception Profile (SPP), 51 Self‐esteem Inventory 55 and the self‐esteem subscale of the Impact of Weight on Quality of Life‐Lite (IWQOL) scale. 40 There was no indication of the source of the questions used to measure self‐esteem in two studies. 53 , 54
Satisfaction was measured using the Satisfaction with Life scale (SWLS) 37 , 49 and twice with different questions. In two cases, a single question rating life satisfaction was used (question source not identified). 42 , 60 In another case, a group of questions rating women's satisfaction with work/career/study, family relationships, partner/close relationships, friendships, and social activities (questionnaire source not referenced) was used. 37 Positive affect was measured using the Positive and Negative Affect Scale (PANAS) 47 , 50 , 51 and the positivity scale. 62 Social support was examined using questions about social life and friends in three studies 52 , 53 , 54 (questionnaire source not referenced). Vitality was measured with the sub‐scales from the SF 36. 36 , 37 , 46 , 57 Vitality was also a theme in one qualitative study. 59 There was no indication of the origin of the questions used to measure happiness in any studies. 3 , 53 , 54 , 58 , 61 , 62 Self‐acceptance was measured using the Body Image Acceptance and Action Questionnaire (BIAAQ). 34 Lastly, optimism was measured with the Orientation to Life Questionnaire. 39
Rather than measuring an individual construct, some researchers chose instruments that measured well‐being and included multiple constructs of PPWB. 2 , 34 , 51 The Obesity Related Well‐being questionnaire (ORWELL‐97) was used to measure the impact of obesity on positive affect, social activities, physical activity, self esteem, relationships, and perception of health. 34 The Ryff's Scale was used to measure positive relationships, self‐acceptance, autonomy, personal growth, mastery, and purpose in life. 2 Finally, the General Well‐being Schedule (GWB) was used to measures positive well‐being, vitality, general health, anxiety, depression, and self control. 51
3.3. Research methods and findings
Study types varied and included interventional studies (5 randomized controlled trials (RCT) 33 , 35 , 38 , 40 , 51 and 4 longitudinal studies 34 , 36 , 53 , 54 ), 21 cross‐sectional surveys, 3 , 10 , 37 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 52 , 55 , 56 , 57 , 58 , 60 , 61 , 62 and 2 qualitative studies. 39 , 59
3.4. Cross‐sectional surveys
Women's ratings of PPWB varied. Cross‐sectional study results are illustrated in Table 2. Most studies found women with obesity rated their self‐reported PPWB significantly lower than men or women without obesity. 2 , 42 , 45 , 46 , 48 , 52 , 55 , 57 , 58 While some researchers found the association between lower PPWB and obesity was attenuated when other variables (e.g., self‐health, body satisfaction, positivity, social factors) were included in the statistical model. 3 , 47 , 49 , 60 , 62 Still some researchers found no association between obesity and aspects of PPWB (positive affect, happiness, self‐esteem). 44 , 50 , 61 Though PPWB was significantly lower for women with obesity overall, women who were in a sub‐cohort of those who reported higher economic status, employment, education, health, relationships, sexual quality of life, exercise levels and body satisfaction were more likely to report higher PPWB than those who were not. 55 , 56 , 58 , 62
TABLE 2.
Summary of cross‐sectional studies' self‐ratings of PPWB outcomes in women with obesity
| Context | Comparators | PPWB measures | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | General population | Health care centers | BMI <18.5 kg/m2 | BMI 18.5–25 kg/m2 | BMI 25–29.9 kg/m2 | BMI ≥30 kg/m2 | Country | Healthy volunteer | Men | Menopause | PCOS | Race | 18–24 years of age | General well‐being | Happiness | Life satisfaction | Positive affect | Positive relationships | Self‐esteem | Vitality |
| Acmaz 2013 | x | x | x | x | x | ↓ | ↓ | |||||||||||||
| Ball 2004 | x | x | x | ↓ | ↓ | |||||||||||||||
| Böckerman 2014 | x | x | x | x | x | ↔ | ||||||||||||||
| Bookwala 2008 | x | x | X | ↓ | ||||||||||||||||
| Brown 2000 | x | x | x | x | x | ↓ | ||||||||||||||
| Burns 2021 | x | x | ↓a | |||||||||||||||||
| Godoy‐Izquierdo 2020 | x | x | x | X | ↓ | |||||||||||||||
| Hill 1998 | x | x | x | x | ↓ | |||||||||||||||
| Jorm 2003 | x | x | x | x | ↔ | |||||||||||||||
| Laferrere 2002 | x | x | x | ↔ | ↔ | ↑b | ||||||||||||||
| Latif 2014 | x | X | ↓ | |||||||||||||||||
| Pasco 2013 | x | x | ⊗ | |||||||||||||||||
| Polat 2020 | x | x | ⊕ | |||||||||||||||||
| Rodino 2016 | x | x | x | x | x | x | ↓ | |||||||||||||
| Sato 2020 | x | x | x | X | ⊗ | |||||||||||||||
| Smith 2014 | x | x | x | ↓c | ||||||||||||||||
| Ul‐Haq 2014 | x | x | ↔ | |||||||||||||||||
| Unlu 2019 | x | x | ↓ | |||||||||||||||||
| Wadsworth 2014 | x | x | X | ↓ | ||||||||||||||||
| Wee 2014 | x | x | ⊗ | |||||||||||||||||
| van Zutven 2015 | x | x | x | ↔ | ||||||||||||||||
Abbreviations: BMI, body mass index; PCOS‐Polycystic Ovary Syndrome. Symbols, ↓Low levels; ↓ a low Self‐esteem predicted internalized weight stigma; ↑b Vitality higher in post‐menopausal women compared to premenopausal African American women with obesity; ↓c lower self esteem associated with stress, loneliness, and poor health; ⊕ moderate level; ↔ negative association not significant after controlling variables; ⊗ no association.
3.5. Interventional studies
Aspects of PPWB were improved in all interventional studies. However, improving PPWB was not the primary focus of any study. Interventional studies are divided into two groups: RCTs and longitudinal studies. Interventional study results are shown in Table 3.
TABLE 3.
Summary of interventions with PPWB outcomes in women
| Reference | Population | Intervention | Control | PPWB and weight outcomes | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI ≥30 kg/m2 | BMI ≥35 kg/m2 | BMI ≥40 kg/m2 | Depression | Underserved AAW | Bariatric surgery | Lifestyle behavior | *PPI | Weight loss | Weight‐neutral | Usual care | Waitlist | General well‐being | Happiness | Healthy eating | Self‐esteem | Positive relationships | Vitality | Weight | |||||||||||||||
| RCT | |||||||||||||||||||||||||||||||||
| Bacon 2005* | x | x | x | x | x | ↑ | ↔ | ||||||||||||||||||||||||||
| Borkoles 2016 | x | x | x | x | ↑ | ↑ | ↔ | ||||||||||||||||||||||||||
| Crerand 2007* | x | x | x | x | ↑ | ↓↔ | |||||||||||||||||||||||||||
| Mensinger 2016* | x | x | x | x | ↑ | ↑ | ↓↔ | ||||||||||||||||||||||||||
| Sarwer 2013 | x | x | x | x | ↑ | ↓ | |||||||||||||||||||||||||||
| Longitudinal | |||||||||||||||||||||||||||||||||
| Ahmen 2018 | x | x | ↑ | ↑ | ↑ | ↓ | |||||||||||||||||||||||||||
| Ahmen 2019 | x | x | x | ↑ | ↑ | ↑ | ↓ | ||||||||||||||||||||||||||
| Berman 2016* | x | x | x | x | ↑ | ↔ | |||||||||||||||||||||||||||
| Groh 2015 | x | x | x | x | ↑ | ||||||||||||||||||||||||||||
Abbreviations: BMI, body mass index; RCT, randomized Controlled Trial; AAW, African American women; * PPI, positive psychology intervention. Symbols: ↓ Weight‐loss, ↔ weight neutral, ↓↔ weight‐PPWB outcomes with both weight loss and neutral groups.
3.6. Randomized controlled trials
The primary purpose of all five RCTs was to examine non‐diet and/or diet treatment outcomes. Self‐esteem was measured in all five RCTs and one also measured overall well‐being. Most women who participated in these lifestyle change program reported improved PPWB irrespective of weight loss. 33 , 35 , 38 , 40 , 51 Women in a non‐dieting lifestyle program arm of a RCT 33 and in both the non‐diet and the diet arms of randomized controlled lifestyle trials 35 , 38 reported improved self‐esteem, with and without weight loss. However, women in the diet treatment of a RCT 33 who did not sustain weight loss reported lower self‐esteem.
3.7. Longitudinal studies
In the four longitudinal studies, women were followed for 24–52 weeks. PPWB was examined as an outcome in two studies focused on weight loss treatment outcomes. 53 , 54 Researchers found that when women lost weight, regardless of the weight loss treatment, the ratings of PPWB improved. Women who lost large amounts of weight (>10–35 kg) after sleeve gastrectomy procedure, 53 gastric balloon insertion, 54 or adhering to an Atkins diet, 54 reported higher self‐esteem, happiness and spending more time with friends. The greater the weight loss, the greater the gains in PPWB. PPWB was also examined as an outcome in two studies that focused on improving lifestyle behaviors and mental health outcomes. 34 , 36 In one instance, after a faith‐based lifestyle change program, underserved African American women reported increased vitality. 36 While in another study, women with a major depressive disorder reported improved over all well‐being after a weight neutral lifestyle behavior program with a positive physiological intervention (Accept Yourself). 34
3.8. Qualitative studies
Using a grounded theory approach, women who reported a positive sense of self, were asked how they maintained their PPWB. 39 The participants conveyed that having a positive sense of self required supportive relationships with friends, family and mentors, the ability to develop skills and competencies, involvement in caring for others, and the ability to engage in positive self‐talk. 39 Another researcher, using Hermeneutic inquiry, found women in a lifestyle intervention program, described improved vitality and mood came from reducing self‐blame, strengthening their confidence, and self acceptance. 59 Women appreciated how an increase in vitality gave them the desire and courage to stay committed to healthy living and engage in their activities of everyday life. 59
3.9. Positive psychological interventions (PPIs)
Positive psychological interventions (PPIs) were used to enhance psychological well‐being in four studies. 33 , 34 , 35 , 38 PPIs included a Health at Every Size (HAES) group intervention where the researchers taught women self‐acceptance, size diversity, and how healthy people come in all sizes. 33 Other researchers used self‐esteem boosting exercises from Johnson's book Self‐Esteem Comes in All Sizes. 35 While another research group used the HUGS (Health focused, Understanding lifestyle, Group supported, and Self‐esteem building) program to build self‐esteem. 38 Lastly, researchers used a self‐acceptance treatment model called Accept Yourself. 34 Although the types of PPIs varied, participants were seen weekly, for one to 2 hours, for a duration of 11–26 weeks and had follow‐up ranging from 6 months to 2 years.
Women who participated in PPIs reported improved self‐esteem or well‐being in all four‐studies. 33 , 34 , 35 , 38 Although in two studies, women who did not receive the PPI also improved their self‐esteem. 35 , 38 In addition to improving PPWB, women reported increased physical activity 33 , 38 and eating more fruit and vegetables. 38 Women's physical health measures of LDL cholesterol (bad cholesterol) 33 , 38 and blood pressure were lower. 33 , 34 Finally, women reported higher mental well‐being measures of quality of life, 34 , 38 and body image acceptance 34 , 35 as well as less depression 34 , 35 and weight self‐stigma. 34
4. DISCUSSION
This is the first scoping review to our knowledge that has a focus on PPWB in women with obesity. In studies that included over 57,000 women with obesity, many constructs of PPWB were measured using a variety of instruments. In the majority of studies, PPWB was lower in women with obesity. Improved PPWB was associated with weight loss and with successful lifestyle changes with and without weight loss. Although few in numbers, PPIs were associated with improved self‐esteem and well‐being. These findings offer glimpses into how PPWB may be associated with improved aspects of health, and healthy behaviors in women with obesity. Still, the causal relationships are not explained by the studies included in this scoping review. There are many knowledge gaps that need to be addressed before providers who work to support women with obesity can determine if and what role PPWB will play in their care.
There is a notable gap in the evidence of how women with obesity experience PPWB and what aspects they may or may not wish to address. For example, it is not known if women with obesity feel a need to improve aspects of their PPWB. There has been an acceleration of calls over the last decade for greater research participant engagement in the research process. 63 Using patient/person‐oriented research, which often includes creating early partnerships with potential research participants to ensure that research questions and the methods to gain answers are relevant and the findings are interpreted in a manner that resonates with those who will benefit most from the research, women with obesity would have much to contribute and gain.
Further, researchers were not able to illuminate what constructs of PPWB are most important to measure in women with obesity. Some constructs of PPWB may have greater importance in terms of health outcomes in general populations. Cardiovascular researchers have identified that optimism, positive psychological constructs, and subjective well‐being are linked to significantly better cardiovascular outcomes, decreased rehospitalization and reduced risk of mortality. 19 , 21 , 64 , 65 , 66 Prospective studies have yet to identify if certain constructs of PPWB are associated with better health outcomes in women with obesity specifically. Longitudinal prospective studies are needed to identify what constructs of PPWB, if any, are associated with the improved health outcomes in this particular population.
Using an instrument that measures multiple aspects of PPWB and reporting sub‐scale scores could provide a richer and more substantive understanding of the relationship between psychological well‐being and health in women with obesity. For example, the PERMA‐profiler measures five constructs of well‐being including positive emotion, engagement, relationships, meaning and accomplishment. 14 It also measures subjective health, loneliness, negative emotion, happiness and provides a composite score for overall PPWB. This is one of many tools that could be used to gain greater insights into multiple aspects of PPWB and possible inter‐related variables for women with obesity.
Future research is needed to explore if women who optimized PPWB feel more able to increase their activity and/or if increasing activity bolsters their PPWB. Not surprisingly, women who reported sustained improvements in exercise also reported improved PPWB. 33 , 38 , 51 , 59 PPWB and improved health behaviors are thought to have a reciprocal relationship. 1 As such, the interactions between exercise and PPWB in women with obesity should be investigated further.
In cross‐sectional studies, the relationship between health, PPWB and obesity in women is not clear. Health status was not measured 2 , 43 , 44 , 45 , 48 , 55 , 62 or adjusted for in multi‐variable analyses. 46 , 58 In studies where analyses were adjusted for subjective health ratings, the association between obesity and lower PPWB was attenuated. 3 , 42 , 49 , 60 It is possible that poor health supersedes BMI as a predictor of low PPWB. These findings suggest that when measuring PPWB it would be helpful to also measure physical health.
Further research is needed to understand the relationships between psychosocial health and PPWB in women with obesity. In this review, the particular psychosocial variables that were associated with PPWB included functional capacity, self‐stigma, social‐stigma, body image, body satisfaction, social determinates of health, and social support. 34 , 42 , 43 , 44 , 45 , 47 , 60 , 62 Additional mechanisms that contribute to lower PPWB in women with obesity may include lower socioeconomic status, level of education and employment status; internal weight stigmatization; societal prejudice; and weight discrimination; and body dissatisfaction and mental health concerns. 6 , 67
Race was not included as a variable in the majority of studies. 35 , 41 , 45 , 46 , 47 , 48 , 49 , 50 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 62 Still, in the few studies for which race was reported, women of color were not included in representative proportions. 2 , 3 , 33 , 34 , 38 , 39 , 51 In all but four 40 , 42 , 43 , 44 over 90% of the women were white. 2 , 3 , 33 , 34 , 38 , 39 , 51 The influence of race on PPWB in women with obesity was examined in three studies. 36 , 37 , 43 Research that includes race and provides representative data is needed.
With only a few studies in which PPIs were examined to improve PPWB, clinicians lack sufficient evidence to recommend them in treatment programs. Researchers suggest that positive emotions may improve negative self‐beliefs and health. 9 , 12 , 13 Although HAES, HUGS, Accept Your Self, and Self‐esteem Comes in All Sizes PPIs have demonstrated associations between improved PPWB and improved health behaviors (increased exercise, healthy eating) or other outcome measures (decreased depression, blood pressure and LDL cholesterol measures), the causal relationship between improved PPWB constructs and improved health is yet to be elucidated. More RCTs are needed to assess if indeed psychological well‐being promoting interventions can improve health outcomes in women with obesity.
Taken together, the role of PPWB in supporting women with obesity remains to be determined. Prospective longitudinal and intervention studies are required to understand how fostering PPWB and evaluating relevant outcomes might support gender‐informed obesity care.
5. STRENGTHS AND LIMITATIONS
Significant strengths of this study were that the search was conducted by a professional health science librarian (KAH) and the authors followed a rigorous methodological and reporting framework (JBI 28 , 29 and PRISMA‐ScR 32 ). Another strength is multiple databases were searched that encompassed a wide variety of disciplines and these databases are not often included in health reviews (i.e., SocINDEX with Full Text, Family & Society Studies Worldwide). A thoughtful preliminary literature review strategy was used to determined keywords. However, even with a comprehensive strategy, omission of potentially relevant keywords is a limitation inherent to researching multidimensional constructs. Lastly this study is limited by including English‐only language publications.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGMENTS
K. Alix Hayden conducted the systematic literature review. Heather E. Conradson and Kathryn King‐Shier reviewed all of the abstracts and full‐text articles. All authors were involved in writing the paper and had final approval of the submitted and published versions.
Final Search Strategies: Positive Psychological Well‐being in Women with Obesity
Changes to search:
Update #1: December 2020 did not limit searches by English
-
Update #2: December 2021 added in Search Concept A:
◦ (flourish* or accomplishment*)
◦ (meaning adj3 (life or making)
Database(s): APA PsycInfo 1806 to November Week 52,021 Search Strategy:
| # | Searches | Results |
|---|---|---|
| 1 | exp *Well being/ | 37,763 |
| 2 | exp Gratitude/ | 1497 |
| 3 | exp Optimism/ | 4619 |
| 4 | exp Self‐compassion/ | 1485 |
| 5 | exp *Self‐esteem/ | 20,260 |
| 6 | exp happiness/ | 8344 |
| 7 | (optimism or optimistic).tw,id. | 16,484 |
| 8 | gratitude.tw,id. | 3717 |
| 9 | self‐love.tw,id. | 423 |
| 10 | self‐compassion.tw,id. | 2520 |
| 11 | self‐esteem.tw,id. | 48,340 |
| 12 | self‐accept*.tw,id. | 2752 |
| 13 | vitality.tw,id. | 4744 |
| 14 | resilience.tw,id. | 30,283 |
| 15 | body acceptance.tw,id. | 150 |
| 16 | body love.tw,id. | 7 |
| 17 | happiness.tw,id. | 17,496 |
| 18 | (flourish* or accomplishment*).tw,id. | 15,832 |
| 19 | (meaning adj3 (life or making)).tw,id. | 10,748 |
| 20 | (emotional adj2 stability).tw,id. | 2970 |
| 21 | ((hedonic* or eudaimonia*) adj2 (well‐being or wellbeing)).tw,id. | 270 |
| 22 | ((positive* or psycholog* or optimal) adj4 (well‐being or wellbeing)).tw,id. | 23,487 |
| 23 | ((positive* or social) adj4 (relationships or engagement)).tw,id. | 38,113 |
| 24 | or/1‐23 | 222,451 |
| 25 | exp *Obesity/ | 21,295 |
| 26 | exp *Overweight/ | 22,786 |
| 27 | exp *Body Weight/ | 47,599 |
| 28 | exp *Weight Loss/ | 2864 |
| 29 | exp *Body mass Index/ | 4442 |
| 30 | exp *Weight Control/ | 4217 |
| 31 | (obese or obesity).tw,id. | 43,792 |
| 32 | (overweight or over‐weight).tw,id. | 16,519 |
| 33 | (weight adj2 (excessive or management or loss)).tw,id. | 14,842 |
| 34 | (bmi or body mass index).tw,id. | 30,301 |
| 35 | or/25‐34 | 86,885 |
| 36 | exp Human Females/ | 151,783 |
| 37 | wom?n*.mp. | 334,308 |
| 38 | female*.mp. | 1,125,130 |
| 39 | or/36‐38 | 1,275,335 |
| 40 | 24 and 35 and 39 | 2509 |
| 41 | (child* or adolescen* or teen*).ti. | 474,138 |
| 42 | 40 not 41 | 1980 |
| 43 | limit 42 to peer reviewed journal | 1627 |
Database(s): Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process, In‐Data‐Review & Other Non‐Indexed Citations and Daily 1946 to 14 December 2021 Search Strategy:
| # | Searches | Results |
|---|---|---|
| 1 | exp Optimism/ | 898 |
| 2 | *Self Concept/ | 26,726 |
| 3 | exp Happiness/ | 4902 |
| 4 | (optimism or optimistic).tw,kf. | 16,327 |
| 5 | gratitude.tw,kf. | 1886 |
| 6 | self‐love.tw,kf. | 63 |
| 7 | self‐compassion.tw,kf. | 1484 |
| 8 | self‐esteem.tw,kf. | 22,818 |
| 9 | self‐accept*.tw,kf. | 851 |
| 10 | vitality.tw,kf. | 13,645 |
| 11 | resilience.tw,kf. | 34,152 |
| 12 | body acceptance.tw,kf. | 119 |
| 13 | body love.tw,kf. | 3 |
| 14 | happiness.tw,kf. | 8066 |
| 15 | (flourish* or accomplishment*).tw,kf. | 13,892 |
| 16 | (meaning adj3 (life or making)).tw,kf. | 3348 |
| 17 | (emotional adj2 stability).tw,kf. | 1102 |
| 18 | ((hedonic* or eudaimonia*) adj2 (well‐being or wellbeing)).tw,kf. | 139 |
| 19 | ((positive* or psycholog* or optimal) adj4 (well‐being or wellbeing)).tw,kf. | 18,299 |
| 20 | ((positive* or social) adj4 (relationships or engagement)).tw,kf. | 22,108 |
| 21 | or/1‐20 | 170,497 |
| 22 | *Obesity/or *obesity, morbid/ | 153,057 |
| 23 | *Overweight/ | 16,722 |
| 24 | *Body weight/ | 30,407 |
| 25 | *Weight loss/ | 16,920 |
| 26 | *body mass index/ | 23,060 |
| 27 | (obese or obesity).tw,kf. | 342,038 |
| 28 | (overweight or over‐weight).tw,kf. | 78,878 |
| 29 | (weight adj2 (excessive or management or loss)).tw,kf. | 107,283 |
| 30 | (bmi or body mass index).tw,kf. | 280,154 |
| 31 | or/22‐30 | 631,956 |
| 32 | wom?n*.mp. | 1,300,606 |
| 33 | female*.mp. | 9,486,632 |
| 34 | Female/ | 9,280,090 |
| 35 | or/32‐34 | 9,661,543 |
| 36 | 21 and 31 and 35 | 4521 |
| 37 | Limit 36 to English language | 4300 |
| 38 | (Child* or adolescen* or teen*).ti. | 952,106 |
| 39 | 37 not 38 | 3290 |
| 40 | Limit 39 to (address or autobiography or bibliography or biography or clinical trial, veterinary or clinical trials, veterinary as topic or comment or dataset or dictionary or directory or editorial or “expression of concern” or government document or interactive tutorial or interview or lecture or legal case or legislation or letter or news or newspaper article or observational study, veterinary or patient education handout or periodical index or personal narrative or portrait or video‐audio media or webcast) | 20 |
| 41 | 39 not 40 | 3270 |
Database(s): Embase 1974 to 2021 December 14 Search Strategy:
| # | Searches | Results |
|---|---|---|
| 1 | *wellbeing/ | 11,724 |
| 2 | exp *optimism/ | 1203 |
| 3 | exp *self esteem/ | 4379 |
| 4 | exp *happiness/ | 2697 |
| 5 | (optimism or optimistic).tw,kw. | 20,376 |
| 6 | gratitude.tw,kw. | 2379 |
| 7 | self‐love.tw,kw. | 90 |
| 8 | self‐compassion.tw,kw. | 1617 |
| 9 | self‐esteem.tw,kw. | 29,082 |
| 10 | self‐accept*.tw,kw. | 1054 |
| 11 | vitality.tw,kw. | 18,653 |
| 12 | resilience.tw,kw. | 38,196 |
| 13 | body acceptance.tw,kw. | 128 |
| 14 | body love.tw,kw. | 2 |
| 15 | happiness.tw,kw. | 9485 |
| 16 | (flourish* or accomplishment*).tw,kw. | 16,185 |
| 17 | (meaning adj3 (life or making)).tw,kw. | 3850 |
| 18 | (emotional adj2 stability).tw,kw. | 1381 |
| 19 | ((hedonic* or eudaimonia*) adj2 (well‐being or wellbeing)).tw,kw. | 131 |
| 20 | ((positive* or psycholog* or optimal) adj4 (well‐being or wellbeing)).tw,kw. | 22,718 |
| 21 | ((positive* or social) adj4 (relationships or engagement)).tw,kw. | 26,088 |
| 22 | or/1‐21 | 189,895 |
| 23 | *obesity/or *morbid obesity/ | 202,407 |
| 24 | *body weight/ | 33,088 |
| 25 | *body weight loss/ | 7821 |
| 26 | *body mass/ | 36,120 |
| 27 | (obese or obesity).tw,kw. | 503,836 |
| 28 | (overweight or over‐weight).tw,kw. | 118,812 |
| 29 | (weight adj2 (excessive or management or loss)).tw,kw. | 170,887 |
| 30 | (bmi or body mass index).tw,kw. | 505,017 |
| 31 | or/23‐30 | 989,459 |
| 32 | wom?n*.mp. | 1,777,395 |
| 33 | female*.mp. | 10,443,381 |
| 34 | female/ | 10,162,538 |
| 35 | or/32‐34 | 10,643,932 |
| 36 | 22 and 31 and 35 | 5897 |
| 37 | (child* or adolescen* or teen*).ti. | 1,092,546 |
| 38 | 36 not 37 | 4754 |
| 39 | limit 38 to conference abstracts | 1491 |
| 40 | 38 not 39 | 3263 |
| 41 | limit 40 to (book or book series or major reference work or trade journal) | 3 |
| 42 | 40 not 41 | 3260 |
Database(s): EBM Reviews ‐ Cochrane Central Register of Controlled Trials November 2021 Search Strategy:
| # | Searches | Results |
|---|---|---|
| 1 | exp Optimism/ | 0 |
| 2 | self concept/ | 2504 |
| 3 | exp Happiness/ | 226 |
| 4 | (optimism or optimistic).tw,kw. | 1221 |
| 5 | gratitude.tw,kw. | 329 |
| 6 | self‐love.tw,kw. | 8 |
| 7 | self‐compassion.tw,kw. | 691 |
| 8 | self‐esteem.tw,kw. | 3738 |
| 9 | self‐accept*.tw,kw. | 104 |
| 10 | vitality.tw,kw. | 2666 |
| 11 | resilience.tw,kw. | 2313 |
| 12 | body acceptance.tw,kw. | 21 |
| 13 | body love.tw,kw. | 0 |
| 14 | happiness.tw,kw. | 1166 |
| 15 | (flourish* or accomplishment*).tw,kw. | 520 |
| 16 | (meaning adj3 (life or making)).tw,kw. | 310 |
| 17 | (emotional adj2 stability).tw,kw. | 247 |
| 18 | ((hedonic* or eudaimonia*) adj2 (well‐being or wellbeing)).tw,kw. | 18 |
| 19 | ((positive* or psycholog* or optimal) adj4 (well‐being or wellbeing)).tw,kw. | 7692 |
| 20 | ((positive* or social) adj4 (relationships or engagement)).tw,kw. | 2045 |
| 21 | Or/1‐20 | 22,678 |
| 22 | obesity/or obesity, morbid/ | 13,728 |
| 23 | Overweight/ | 5623 |
| 24 | Body weight/ | 8747 |
| 25 | Weight loss/ | 6566 |
| 26 | body mass index/ | 10,861 |
| 27 | (obese or obesity).tw,kw. | 46,798 |
| 28 | (overweight or over‐weight).tw,kw. | 18,310 |
| 29 | (weight adj2 (excessive or management or loss)).tw,kw. | 24,227 |
| 30 | (bmi or body mass index).tw,kw. | 66,465 |
| 31 | or/22‐30 | 111,332 |
| 32 | wom?n*.mp. | 172,398 |
| 33 | female*.mp. | 865,885 |
| 34 | female/ | 479,414 |
| 35 | or/32‐34 | 910,661 |
| 36 | 21 and 31 and 35 | 1233 |
| 37 | (child* or adolescen* or teen*).ti. | 92,605 |
| 38 | 36 not 37 | 1049 |
Database(s): CINAHL Plus with Full Text
| # | Query | Limiters/Expanders | Results |
|---|---|---|---|
| S1 | (MM “Psychological Well‐Being”) | Search modes ‐ find all my search terms | 13,748 |
| S2 | (MM “Optimism”) | Search modes ‐ find all my search terms | 1160 |
| S3 | (MM “Self Concept”) | Search modes ‐ find all my search terms | 14,631 |
| S4 | (MM “Happiness”) | Search modes ‐ find all my search terms | 2296 |
| S5 | TI ((meaning N3 (life or making)) OR AB ((meaning N3 (life or making)) | Search modes ‐ find all my search terms | 3723 |
| S6 | TI ((gratitude or self‐love or self‐compassion or self‐esteem or self‐accept* or optimism or optimistic)) OR AB ((gratitude or self‐love or self‐compassion or self‐esteem or self‐accept* or optimism or optimistic)) | Search modes ‐ find all my search terms | 23,720 |
| S7 | TI ((vitality or resilience or “body acceptance” or “body love” or happiness or flourish* or accomplishment*)) OR AB ((vitality or resilience or “body acceptance” or “body love” or happiness or flourish* or accomplishment*)) | Search modes ‐ find all my search terms | 29,513 |
| S8 | TI (emotional N2 stability) OR AB (emotional N2 stability) | Search modes ‐ find all my search terms | 476 |
| S9 | TI (((hedonic* or eudaimonia*) N2 (well‐being or wellbeing))) OR AB (((hedonic* or eudaimonia*) N2 (well‐being or wellbeing))) | Search modes ‐ find all my search terms | 83 |
| S10 | TI (((positive* or psycholog* or optimal) N4 (well‐being or wellbeing))) OR AB (((positive* or psycholog* or optimal) N4 (well‐being or wellbeing))) | Search modes ‐ find all my search terms | 11,446 |
| S11 | TI (((positive* or social) N4 (relationships or engagement))) OR AB (((positive* or social) N4 (relationships or engagement))) | Search modes ‐ find all my search terms | 26,839 |
| S12 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 | Search modes ‐ find all my search terms | 108,830 |
| S13 | (MM “Obesity”) OR (MM “Obesity, Morbid”) | Search modes ‐ find all my search terms | 60,158 |
| S14 | (MM “Body Weight”) | Search modes ‐ find all my search terms | 8589 |
| S15 | (MM “Weight Loss”) | Search modes ‐ find all my search terms | 10,766 |
| S16 | (MM “Body Mass Index”) | Search modes ‐ find all my search terms | 13,517 |
| S17 | (MM “Weight Control”) | Search modes ‐ find all my search terms | 4607 |
| S18 | TI ((obese or obesity)) OR AB ((obese or obesity)) | Search modes ‐ find all my search terms | 112,718 |
| S19 | TI ((overweight or over‐weight)) OR AB ((overweight or over‐weight)) | Search modes ‐ find all my search terms | 35,331 |
| S20 | TI ((weight N2 (excessive or management or loss))) OR AB ((weight N2 (excessive or management or loss))) | Search modes ‐ find all my search terms | 34,484 |
| S21 | TI ((bmi or “body mass index”)) OR AB ((bmi or “body mass index”)) | Search modes ‐ find all my search terms | 100,154 |
| S22 | S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 | Search modes ‐ find all my search terms | 220,164 |
| S23 | (MH “female”) | Search modes ‐ find all my search terms | 2,113,616 |
| S24 | TI (women or woman or female*) OR AB (women or woman or female*) | Search modes ‐ find all my search terms | 652,525 |
| S25 | S23 OR S24 | Search modes ‐ find all my search terms | 2,250,278 |
| S26 | S12 AND S22 AND S25 | Search modes ‐ find all my search terms | 2707 |
| S27 | S12 AND S22 AND S25 | Search modes ‐ find all my search terms | 2707 |
| S28 | S12 AND S22 AND S25 | Limiters ‐ Scholarly (peer reviewed) Journals Search modes ‐ find all my search terms | 2598 |
| S29 | TI (child* or adolescen* or teen*) | Search modes ‐ find all my search terms | 396,398 |
| S30 | S28 NOT S29 | Search modes ‐ find all my search terms | 1985 |
Database(s): SocIndex with Full Text
| # | Query | Limiters/Expanders | Results |
|---|---|---|---|
| S1 | TI ((meaning N3 (life or making)) OR AB ((meaning N3 (life or making)) OR KW ((meaning N3 (life or making)) | Search modes ‐ find all my search terms | 3380 |
| S2 | TI ((gratitude or self‐love or self‐compassion or self‐esteem or self‐accept* or optimism or optimistic)) OR AB ((gratitude or self‐love or self‐compassion or self‐esteem or self‐accept* or optimism or optimistic)) OR KW ((gratitude or self‐love or self‐compassion or self‐esteem or self‐accept* or optimism or optimistic)) | Search modes ‐ find all my search terms | 19,044 |
| S3 | TI ((vitality or resilience or "body acceptance" or "body love" or happiness or flourish* or accomplishment*)) OR AB ((vitality or resilience or "body acceptance" or "body love" or happiness or flourish* or accomplishment*)) OR KW ((vitality or resilience or "body acceptance" or "body love" or happiness or flourish* or accomplishment*)) | Search modes ‐ find all my search terms | 23,365 |
| S4 | TI (emotional N2 stability) OR AB (emotional N2 stability) OR KW (emotional N2 stability) | Search modes ‐ find all my search terms | 556 |
| S5 | TI (((hedonic* or eudaimonia*) N2 (well‐being or wellbeing))) OR AB (((hedonic* or eudaimonia*) N2 (well‐being or wellbeing))) OR KW (((hedonic* or eudaimonia*) N2 (well‐being or wellbeing))) | Search modes ‐ find all my search terms | 98 |
| S6 | TI (((positive* or psycholog* or optimal) N4 (well‐being or wellbeing))) OR AB (((positive* or psycholog* or optimal) N4 (well‐being or wellbeing))) KW (((positive* or psycholog* or optimal) N4 (well‐being or wellbeing))) | Search modes ‐ find all my search terms | 1294 |
| S7 | TI (((positive* or social) N4 (relationships or engagement))) OR AB (((positive* or social) N4 (relationships or engagement))) OR KW (((positive* or social) N4 (relationships or engagement))) | Search modes ‐ find all my search terms | 27,824 |
| S8 | TI ((obese or obesity)) OR AB ((obese or obesity)) OR KW ((obese or obesity)) | Search modes ‐ find all my search terms | 6233 |
| S9 | TI ((overweight or over‐weight)) OR AB ((overweight or over‐weight)) OR KW ((overweight or over‐weight)) | Search modes ‐ find all my search terms | 2420 |
| S10 | TI ((weight N2 (excessive or management or loss))) OR AB ((weight N2 (excessive or management or loss))) OR KW ((weight N2 (excessive or management or loss))) | Search modes ‐ find all my search terms | 1342 |
| S11 | TI ((bmi or “body mass index”)) OR AB ((bmi or “body mass index”)) OR KW ((bmi or “body mass index”)) | Search modes ‐ find all my search terms | 3734 |
| S12 | TI (women or woman or female*) OR AB (women or woman or female*) OR KW (women or woman or female*) | Search modes ‐ find all my search terms | 260,073 |
| S13 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 | Search modes ‐ find all my search terms | 72,303 |
| S14 | S8 OR S9 OR S10 OR S11 | Search modes ‐ find all my search terms | 9756 |
| S15 | S12 AND S13 AND S14 | Search modes ‐ find all my search terms | 195 |
| S16 | TI (child* or adolescen* or teen*) | Search modes ‐ find all my search terms | 146,392 |
| S17 | S15 NOT S16 | Search modes ‐ find all my search terms | 158 |
| S18 | S15 NOT S16 | Limiters ‐ Scholarly (peer reviewed) Journals Search modes ‐ find all my search terms | 145 |
Database(s): Family & Society Studies Worldwide
| # | Query | Limiters/Expanders | Results |
|---|---|---|---|
| S1 | TI ((meaning N3 (life or making)) OR AB ((meaning N3 (life or making)) OR KW ((meaning N3 (life or making)) | Search modes ‐ find all my search terms | 1772 |
| S2 | TI ((gratitude or self‐love or self‐compassion or self‐esteem or self‐accept* or optimism or optimistic)) OR AB ((gratitude or self‐love or self‐compassion or self‐esteem or self‐accept* or optimism or optimistic)) OR KW ((gratitude or self‐love or self‐compassion or self‐esteem or self‐accept* or optimism or optimistic)) | Search modes ‐ find all my search terms | 17,917 |
| S3 | TI ((vitality or resilience or "body acceptance" or "body love" or happiness or flourish* or accomplishment*)) OR AB ((vitality or resilience or "body acceptance" or "body love" or happiness or flourish* or accomplishment*)) OR KW ((vitality or resilience or "body acceptance" or "body love" or happiness or flourish* or accomplishment*)) | Search modes ‐ find all my search terms | 14,276 |
| S4 | TI (emotional N2 stability) OR AB (emotional N2 stability) OR KW (emotional N2 stability) | Search modes ‐ find all my search terms | 383 |
| S5 | TI (((hedonic* or eudaimonia*) N2 (well‐being or wellbeing))) OR AB (((hedonic* or eudaimonia*) N2 (well‐being or wellbeing))) OR KW (((hedonic* or eudaimonia*) N2 (well‐being or wellbeing))) | Search modes ‐ find all my search terms | 28 |
| S6 | TI (((positive* or psycholog* or optimal) N4 (well‐being or wellbeing))) OR AB (((positive* or psycholog* or optimal) N4 (well‐being or wellbeing))) KW (((positive* or psycholog* or optimal) N4 (well‐being or wellbeing))) | Search modes ‐ find all my search terms | 1346 |
| S7 | TI (((positive* or social) N4 (relationships or engagement))) OR AB (((positive* or social) N4 (relationships or engagement))) OR KW (((positive* or social) N4 (relationships or engagement))) | Search modes ‐ find all my search terms | 17,765 |
| S8 | TI ((obese or obesity)) OR AB ((obese or obesity)) OR KW ((obese or obesity)) | Search modes ‐ find all my search terms | 34,659 |
| S9 | TI ((overweight or over‐weight)) OR AB ((overweight or over‐weight)) OR KW ((overweight or over‐weight)) | Search modes ‐ find all my search terms | 14,494 |
| S10 | TI ((weight N2 (excessive or management or loss))) OR AB ((weight N2 (excessive or management or loss))) OR KW ((weight N2 (excessive or management or loss))) | Search modes ‐ find all my search terms | 9381 |
| S11 | TI ((bmi or “body mass index”)) OR AB ((bmi or “body mass index”)) OR KW ((bmi or “body mass index”)) | Search modes ‐ find all my search terms | 27,191 |
| S12 | TI (women or woman or female*) OR AB (women or woman or female*) OR KW (women or woman or female*) | Search modes ‐ find all my search terms | 283,222 |
| S13 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 | Search modes ‐ find all my search terms | 50,753 |
| S14 | S8 OR S9 OR S10 OR S11 | Search modes ‐ find all my search terms | 56,046 |
| S15 | S12 AND S13 AND S14 | Search modes ‐ find all my search terms | 552 |
| S16 | TI (child* or adolescen* or teen*) | Search modes ‐ find all my search terms | 326,804 |
| S17 | S15 NOT S16 | Search modes ‐ find all my search terms | 469 |
| S18 | S15 NOT S16 | Limiters ‐ Scholarly (peer reviewed) Journals Search modes ‐ find all my search terms | 425 |
Database(s): PROQUEST DISSERTATIONS
((noft(optimism OR optimistic OR gratitude OR self‐love OR self‐compassion OR self‐esteem OR self‐accept* OR vitality OR resilience OR "body acceptance" OR "body love" OR happiness or flourish* or accomplishment*) OR noft(meaning WITHIN‐3 (life or making)) OR noft(emotional WITHIN‐2 stability) OR (noft(hedonic* WITHIN‐2 well‐being) OR noft(hedonic* WITHIN‐2 wellbeing) OR noft(eudaimonia* WITHIN‐2 well‐being) OR noft(eudaimonia* WITHIN‐2 wellbeing)) OR (noft(positive* WITHIN‐2 well‐being) OR noft(positive* WITHIN‐2 wellbeing) OR noft(psycholog* WITHIN‐2 well‐being) OR noft(psycholog* WITHIN‐2 wellbeing) OR noft(optiimal WITHIN‐2 well‐being) OR noft(optimal WITHIN‐2 wellbeing)) OR (noft(positive* WITHIN‐2 relationships) OR noft(positive* WITHIN‐2 engagement) OR noft(social WITHIN‐2 relationships) OR noft(social WITHIN‐2 engagement))) AND noft(obese OR obesity OR overweight OR over‐weight OR bmi OR "body mass index") AND noft(women OR woman OR female*)) NOT ti((child* OR adolescen* OR teen*))
Conradson HE, Hayden KA, Russell‐Mayhew S, Raffin Bouchal S, King‐Shier K. Positive psychological well‐being in women with obesity: a scoping review of qualitative and quantitative primary research. Obes Sci Pract. 2022;8(6):691‐714. 10.1002/osp4.605
REFERENCES
- 1. Prendergast KB, Schofield GM, Mackay LM. Associations between lifestyle behaviours and optimal well‐being in a diverse sample of New Zealand adults. BMC Publ Health. 2015;16(1):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bookwala J, Boyar J. Gender, excessive body weight, and psychological well‐being in adulthood. Psychol Women Q. 2008;32(2):188‐195. [Google Scholar]
- 3. Ul‐Haq Z, Mackay DF, Martin D, et al. Heaviness, health and happiness: a cross‐sectional study of 163066 UK Biobank participants. J Epidemiol Commun Health. 2014;68(4):340‐348. [DOI] [PubMed] [Google Scholar]
- 4. Pi‐Sunyer X. The medical risks of obesity. PGM (Postgrad Med). 2009;121(6):21‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Khan SS, Ning H, Wilkin Obes Sci Practs JT, et al. Association of body mass index with lifetime risk of cardiovascular disease and Compression of morbidity. JAMA Cardiol. 2018;3(4):280‐287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Taylor V, Sockalingam S, Hawa R, Hahn M. Canadian Adult Obesity Clinical Practice Guidelines: The Role of Mental Health in Obesity Management; 2020. https://obesitycanada.ca/guidelines/mentalhealth [Google Scholar]
- 7. Puhl RM, Andreyeva T, Brownell KD. Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America. Int J Obes. 2008;32(6):992‐1000. [DOI] [PubMed] [Google Scholar]
- 8. Bacon L, Aphramor L. Weight science: evaluating the evidence for a paradigm shift. Nutr J. 2011;10(1):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17(5):941‐964. [DOI] [PubMed] [Google Scholar]
- 10. Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obes Rev. 2018;19(8):1141‐1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Puhl RM, Himmelstein MS, Pearl RL. Weight stigma as a psychosocial contributor to obesity. Am Psychol. 2020;75(2):274‐289. [DOI] [PubMed] [Google Scholar]
- 12. Hilbert A, Braehler E, Schmidt R, Löwe B, Häuser W, Zenger M. Self‐compassion as a resource in the self‐stigma process of overweight and obese individuals. Obes Facts. 2015;8(5):293‐301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jackson SE, Beeken RJ, Wardle J. Obesity, perceived weight discrimination, and psychological well‐being in older adults in England: obesity, Discrimination, and Well‐being. Obesity. 2015;23(5):1105‐1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Seligman MEP. Flourish: A Visionary New Understanding of Happiness and Wellbeing: Simon and Schuster; 2011. [Google Scholar]
- 15. Butler J, Kern ML. The PERMA‐Profiler: a brief multidimensional measure of flourishing. Int J Wellbeing. 2016;6(3):1‐48. [Google Scholar]
- 16. Seligman MEP, Csikszentmihalyi M. Positive psychology: an introduction. Am Psychol. 2000;55(1):5‐14. [DOI] [PubMed] [Google Scholar]
- 17. Huppert FA, So TTC. Flourishing across Europe: application of a new conceptual framework for defining well‐being. Soc Indic Res. 2013;110(3):837‐861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keyes CLM. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am Psychol. 2007;62(2):95‐108. [DOI] [PubMed] [Google Scholar]
- 19. Kubzansky LD, Huffman JC, Boehm JK, et al. Positive psychological well‐being and cardiovascular disease. J Am Coll Cardiol. 2018;72(12):1382‐1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Levine GN, Cohen BE, Commodore‐Mensah Y, et al. Psychological health, well‐being, and the mind‐heart‐body connection: a scientific statement from the american heart association. Circulation. 2021;143(10):e763‐e783. [DOI] [PubMed] [Google Scholar]
- 21. DuBois CM, Lopez OV, Beale EE, Healy BC, Boehm JK, Huffman JC. Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: a systematic review. Int J Cardiol. 2015;195:265‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sarwer DB, Heinberg LJ. A review of the psychosocial aspects of clinically severe obesity and bariatric surgery. Am Psychol. 2020;75(2):252‐264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sarwer DB, Thompson JK, Cash TF. Body image and obesity in adulthood. Psychiatr Clin. 2005;28(1):69‐87. [DOI] [PubMed] [Google Scholar]
- 24. Fikkan J, Rothblum E. Is fat a feminist issue? Exploring the gendered nature of weight bias. Sex Roles. 2012;66(9‐10):575‐592. [Google Scholar]
- 25. Sutin AR, Stephan Y, Terracciano A. Weight discrimination and risk of mortality. Psychol Sci. 2015;26(11):1803‐1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Clayton JA, Tannenbaum C. Reporting sex, gender, or both in clinical research. JAMA. 2016;316(18):1863‐1864. [DOI] [PubMed] [Google Scholar]
- 27. Peters MDJ, Godfrey CM, Mclnerney P, Munn Z, Trico A, Khalil H. Chapter 11: Scoping reviews (2020 version). In: JBI Manual for Evidence Synthesis, JBI; 2020. https://synthesismanual.jbi.global [Google Scholar]
- 28. Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Base Healthc. 2015;13(3):141‐146. [DOI] [PubMed] [Google Scholar]
- 29. Peters MDJ, Godfrey CM, McInerney P, Soares CB, Khalil H, Parker D. Methodology for JBI Scoping Reviews. The Joanna Briggs Institute Reviewers Manual 2015; 2015. https://nursing.lsuhsc.edu/JBI/docs/ReviewersManuals/Scoping‐.pdf [Google Scholar]
- 30. Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119‐2126. [DOI] [PubMed] [Google Scholar]
- 31. Covidence . Veritas Health Innovations Ltd. Computer Software; 2020.
- 32. Page MJ, McKenzie J, Bossuyt P, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2020;372(n71). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bacon L, Stern JS, Van Loan MD, Keirn NL. Size acceptance and intuitive eating improve health for obese, female chronic dieters. J Am Diet Assoc. 2005;105(6):929‐936. [DOI] [PubMed] [Google Scholar]
- 34. Berman MI, Morton SN, Hegel MT. Uncontrolled pilot study of an acceptance and commitment therapy and health at every size intervention for obese, depressed women: accept Yourself. Psychother Theor Res Pract Train. 2016;53(4):462‐467. [DOI] [PubMed] [Google Scholar]
- 35. Crerand CE, Wadden TA, Foster GD, Sarwer DB, Paster LM, Berkowitz RI. Changes in obesity‐related attitudes in women seeking weight reduction. Obesity. 2007;15(3):740‐747. [DOI] [PubMed] [Google Scholar]
- 36. Groh CJ, Urbancic JC. The impact of a lifestyle change program on the mental health of obese under‐served African American women. Arch Psychiatr Nurs. 2015;29(2):76‐82. [DOI] [PubMed] [Google Scholar]
- 37. Laferrère B, Zhu S, Clarkson JR, et al. Race, menopause, health‐related quality of life, and psychological well‐being in obese women. Obes Res. 2002;10(12):1270‐1275. [DOI] [PubMed] [Google Scholar]
- 38. Mensinger JL, Meadows A. Internalized weight stigma mediates and moderates physical activity outcomes during a healthy living program for women with high body mass index. Psychol Sport Exerc. 2017;30:64‐72. [Google Scholar]
- 39. Ripsch J. Development and Maintenance of Positive Sense of Self in Successful Obese Women. Loyola University, Proquest Dissertations Publishing; 2002. [Google Scholar]
- 40. Sarwer DB, Moore RH, Diewald LK, et al. The impact of a primary care‐based weight loss intervention on the quality of life. Int J Obes. 2013;37(S1):S25‐S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Smith MJ, Theeke L, Culp S, Clark K, Pinto S. Psychosocial variables and self‐rated health in young adult obese women. Appl Nurs Res. 2014;27(1):67‐71. [DOI] [PubMed] [Google Scholar]
- 42. Wadsworth T, Pendergast PM. Obesity (sometimes) matters: the importance of context in the relationship between obesity and life satisfaction. J Health Soc Behav. 2014;55(2):196‐214. [DOI] [PubMed] [Google Scholar]
- 43. Burns DM. The Impact of Self‐Esteem and Body Dissatisfaction on Internalized Stigma in Obese, Hispanic Women. Walden University: ProQuest Dissertations Publishing; 2021. [Google Scholar]
- 44. Wee CC, Davis RB, Chiodi S, Huskey KW, Hamel MB. Sex, race, and the adverse effects of social stigma vs. other quality of life factors among primary care patients with moderate to severe obesity. J Gen Intern Med. 2015;30(2):229‐235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ball K, Crawford D, Kenardy J. Longitudinal relationships among overweight, life satisfaction, and aspirations in young women. Obes Res. 2004;12(6):1019‐1030. [DOI] [PubMed] [Google Scholar]
- 46. Brown W, Mishra G, Kenardy J, Dobson A. Relationships between body mass index and well‐being in young Australian women. Int J Obes. 2000;24(10):1360‐1368. [DOI] [PubMed] [Google Scholar]
- 47. Jorm AF, Korten AE, Christensen H, Jacomb PA, Rodgers B, Parslow RA. Association of obesity with anxiety, depression and emotional well‐being: a community survey. Aust N Z J Publ Health. 2003;27(4):434‐440. [DOI] [PubMed] [Google Scholar]
- 48. Rodino IS, Byrne S, Sanders KA. Obesity and psychological wellbeing in patients undergoing fertility treatment. Reprod Biomed Online. 2016;32(1):104‐112. [DOI] [PubMed] [Google Scholar]
- 49. van Zutven K, Mond J, Latner J, Rodgers B. Obesity and psychosocial impairment: mediating roles of health status, weight/shape concerns and binge eating in a community sample of women and men. Int J Obes. 2015;39(2):346‐352. [DOI] [PubMed] [Google Scholar]
- 50. Pasco JA, Williams LJ, Jacka FN, Brennan SL, Berk M. Obesity and the relationship with positive and negative affect. Aust N Z J Psychiatry. 2013;47(5):477‐482. [DOI] [PubMed] [Google Scholar]
- 51. Borkoles E, Carroll S, Clough P, Polman RCJ. Effect of a non‐dieting lifestyle randomised control trial on psychological well‐being and weight management in morbidly obese pre‐menopausal women. Maturitas. 2016;83:51‐58. [DOI] [PubMed] [Google Scholar]
- 52. Hill A, Williams J. Psychological health in a non‐clinical sample of obese women. Int J Obes. 1998;22(6):578‐583. [DOI] [PubMed] [Google Scholar]
- 53. Ahmed HO. Pattern of changes in quality of life of obese patients after sleeve gastrectomy in Sulaimani provence –Kurdistan‐Iraq, based on 4 years experience in two bariatric centers. Ann Med Surg. 2018;26:9‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ahmed HO, Ezzat RF. Quality of life of obese patients after treatment with the insertion of intra‐gastric balloon versus Atkins diet in Sulaimani Governorate, Kurdistan Region, Iraq. Ann Med Surg. 2019;37:42‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Unlu S, Aykut M, Borlu A, Kaner G. Are low self‐esteem and body image dissatisfaction related with body mass index? Prog Nutr. 2019:94‐103. [Google Scholar]
- 56. Polat HT, Serin EK. Self‐esteem and sexual quality of life among obese women. Psychiatr Care. 2020:1‐5. [DOI] [PubMed] [Google Scholar]
- 57. Acmaz G, Albayrak B, Acmaz M, Baser M, Soyok M, Zararsiz G. Level of anxiety, depression, self‐esteem, social anxiety, and quality of life among the women with polycystic ovary syndrome. Sci World J. 2013:851815‐851817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Latif E. Obesity and happiness: does gender matter? Econ Bus Lett. 2014;3(1):59‐67. [Google Scholar]
- 59. Toft BS, Nielsen CV, Uhrenfeldt L. Balancing one's mood: experiences of physical activity in adults with severe obesity 18 months after lifestyle intervention. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen. 2020;153‐154:23‐31. [DOI] [PubMed] [Google Scholar]
- 60. Böckerman P, Johansson E, Saarni SI, Saarni SE. The negative association of obesity with subjective well‐being: is it all about health? J Happiness Stud. 2014;15(4):857‐867. [Google Scholar]
- 61. Sato K. Unhappy and happy obesity: a comparative study on the United States and China. J Happiness Stud. 2020;22(3):1259‐1285. [Google Scholar]
- 62. Godoy‐Izquierdo D, González‐Hernández J, Rodríguez‐Tadeo A, et al. Body satisfaction, weight stigma, positivity, and happiness among Spanish adults with overweight and obesity. Int J Environ Res Publ Health. 2020;17(4186):1‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Canadian Institutes of Health Research . Foundations of SPOR; 2019. https://cihr‐irsc.gc.ca/e/51039.html [Google Scholar]
- 64. Tindle HA, Chang YF, Kuller L, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the women’s health initiative. Circulation. 2009;120(8):656‐662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Boehm JK, Kubzansky LD. The heart's content: the association between positive psychological well‐being and cardiovascular health. Psychol Bull. 2012;138(4):655‐691. [DOI] [PubMed] [Google Scholar]
- 66. Giltay EJ, Geleijnse JM, Zitman FG, Hoekstra T, Schouten EG. Dispositional optimism and all‐cause and cardiovascular mortality in a prospective cohort of elderly Dutch men and women. Arch Gen Psychiatr. 2004;61(11):1126‐1135. [DOI] [PubMed] [Google Scholar]
- 67. Kirk S, Salas XR, Alberga A, Russell‐Mayhew S. Canadian Adult Obesity Clinical Practice Guidelines: Reducing Weight Bias, Stigma and Discrimination in Obesity Management, Practice, and Policy. 2020. https://obesitycanada.ca/guidelines/weightbias [Google Scholar]


