Abstract
Background
Internalized weight stigma (Internalized‐WS) is prevalent among individuals with severe obesity, particularly women, and is associated with shame, disordered eating, and weight gain. Effective, accessible interventions that address both severe (Class‐III) obesity and Internalized‐WS are needed. This randomized pilot trial evaluated the feasibility, acceptability, and preliminary efficacy of a fully‐remote lifestyle modification intervention (LM) followed by mindful self‐compassion training (MSC) or control.
Methods
Twenty‐eight women with Class‐III obesity (46.6 ± 3.7 kg/m2) and elevated Internalized‐WS were randomized to a virtually‐delivered 4‐month LM followed by a 2‐month MSC or cooking/dietary education (CON). Psychosocial measures/weight were assessed at baseline, 4‐(post‐LM), 6‐(post‐MSC/CON), and 9‐month (follow‐up).
Results
Improvements in Internalized‐WS, shame, and self‐compassion were observed with LM. Mean 4‐month weight loss was 6.3 ± 3.7%. MSC had lower attendance and usefulness ratings versus CON. Post‐MSC/CON, MSC yielded significant and/or meaningful improvements in Internalized‐WS, self‐compassion, and intuitive eating relative to CON. Weight loss did not differ by group at 6‐month, and at 9‐month trended lower in MSC versus CON.
Conclusion
Virtual LM is feasible, acceptable, and leads to significant weight loss among women with severe obesity; MSC led to further improved Internalized‐WS, self‐compassion, and intuitive eating. Continued work is needed to elucidate effects of self‐compassion training on Internalized‐WS, its mechanisms, and linkages to cardiometabolic health and long‐term weight loss.
Keywords: extreme obesity, internalized weight stigma, lifestyle modification, self‐compassion
Weight stigma – prejudice toward people with overweight and obesity that can translate into discriminatory or unfair treatment – is an internationally‐recognized problem with adverse health impacts for those stigmatized. 1 Experiences of weight stigma can foster psychosocial processes shown to contribute to further weight gain and chronic disease risk. 2 , 3 , 4 Exposure to weight stigma can also lead to internalized weight stigma (WS), the self‐application of stereotypes associated with obesity. Amassing evidence has identified Internalized‐WS as a key factor linking weight stigma experiences to adverse health outcomes. 2 Internalized‐WS is prevalent among weight loss‐seeking individuals, is greater among those with higher BMI when a range of weights are represented, 2 and is associated with maladaptive eating behaviors such as dietary disinhibition, 2 eating to cope with negative emotions, 5 and less intuitive eating. 6 , 7 , 8 These and other findings suggest Internalized‐WS may impede sustainable eating behavior change 2 , 9 , 10 and ultimately weight management. In fact, prior work suggests that for every one‐unit increase in Internalized‐WS, the odds of weight loss maintenance are reduced by 28%. 11
While weight stigma and Internalized‐WS clearly have important health implications, there are two conflicting theories regarding how to best to address these factors in those with obesity: a weight‐inclusive or non‐dieting approach (i.e., de‐emphasizing body weight as a determinant of health, eschewing weight loss practices like dieting), 12 and a weight‐normative approach (i.e., emphasizing weight loss). Although these are commonly presented as mutually exclusive, both can lead to reductions in Internalized‐WS and improved health behaviors among people with obesity. 13 , 14 Prior research shows participation in lifestyle modification (LM) decreased Internalized‐WS. 13 , 15 , 16 Pearl et al. 17 built on this by integrating LM with a cognitive behavioral therapy (CBT) component that addressed Internalized‐WS and found that the targeted dialectical approach initially improved Internalized‐WS relative to LM alone, although 6‐month follow‐up showed no long‐term difference between groups.
Current weight‐inclusive interventions follow an early generation of research that attempted to improve overall behavioral health and weight through non‐dieting approaches that found beneficial effects on eating behavior, body image, negative affect, and weight stability, yet little effect on weight loss. 18 , 19 , 20 , 21 , 22 Although such interventions often addressed body image and self‐acceptance they did not specifically directly address self‐compassion, a stigma‐protective factor that refers to treating oneself as a loved one might during moments of distress or difficulty. More recently, using a weight‐inclusive approach for women with obesity that integrated self‐compassion, Palmeira et al. 14 found reductions in body mass index (BMI), Internalized‐WS, and emotional eating in a single‐group pilot trial. Changes in Internalized‐WS and emotional eating were mediated by increases in self‐compassion, suggesting that interventions that target self‐compassion could also concurrently improve weight loss and Internalized‐WS.
Self‐compassion has also been implicated in ameliorating the adverse effects of stigma, Internalized‐WS, and/or shame on distress and eating behaviors 23 , 24 , 25 , 26 , 27 including among people with obesity, 9 , 27 , 28 and is associated with less distress in response to dietary lapses and with improved eating behaviors such as intuitive eating. 29 , 30 , 31 , 32 Self‐compassion training is also linked to improvement in eating behaviors and perceived stress, 14 , 32 including via remotely‐delivered treatment, 33 with a recent review suggesting small if promising effects on weight loss. 32 However, a more rigorous recent RCT comparing video‐conference delivered LM to LM integrated with self‐compassion skills (LM + self‐compassion) training found LM + self‐compassion to yield increased self‐compassion but no difference in caloric intake, physical activity, maladaptive eating patterns, or weight loss compared to LM alone at post‐treatment. 34 Yet this study did not target individuals with elevated Internalized‐WS or examine the effects of LM + self‐compassion on long‐term weight loss, which may be of particular interest as greater self‐compassion may be associated with long‐term weight loss. 35 Delivery of self‐compassion training following LM may optimally target Internalized‐WS‐related processes (e.g., shame following dietary disinhibition) that may aid in maintaining healthy behaviors and weight loss long‐term. This may particularly be true for women, who often report lower levels of self‐compassion 36 and greater levels of Internalized‐WS. 37 , 38
The purpose of this randomized trial was to advance the literature by examining the feasibility and acceptability of a videoconferencing‐delivered (a) fully remote LM program for weight loss and (b) MSC intervention, delivered following LM, for individuals with Class III obesity and elevated Internalized‐WS. Prior research indicates that LM can produce significant WL among those with severe obesity (i.e., a similar percentage of weight loss observed among those with severe obesity and lesser degrees of obesity) 40 , 41 and that those with greater obesity have greater Internalized‐WS. 2 Thus, this study examined whether adding an MSC intervention following LM would further improve WL in this population, as MSC targets factors related to Internalized‐WS and it provides additional skills beyond those taught in traditional LM programs for weight loss. These additional skills may be particularly helpful for people with severe obesity given the potentially greater likelihood of internalizing WS and corresponding barriers to adaptive health behavior change in this population. This study also examined whether an MSC intervention leads to improvements in Internalized‐WS, shame, and eating behaviors, relative to a control condition. It is hypothesized that the implementation of MSC training following LM for weight loss will reduce Internalized‐WS, improve self‐compassion, shame, and eating behaviors, and ultimately lead to increased weight loss at follow‐up.
1. MATERIALS AND METHODS
1.1. Participants and procedures
1.1.1. Participants
Women eligible for this study were aged 18–65 years, with a BMI between 40 and 55 kg/m2 and elevated Internalized‐WS (determined by a score of ≥3 on the Weight Bias Internalization Scale [WBIS]). For this pilot project we opted for a less conservative cut‐point because individuals with greater obesity generally report greater Internalized‐WS relative to those with less. 2 Exclusion criteria included a history of bariatric surgery or recent weight loss (≥15 pounds within the past 6 months); conditions that would limit weight loss or exercise; present or recent (<1 year ago) participation in a weight loss program; or use of weight loss medication, pregnancy, or hospitalization for a psychiatric condition. Physician consent was required for those with a history of heart disease or diabetes.
1.1.2. Study overview and procedures
Participants recruited from Internet sources completed an initial online screener (before the phone screen) that screened for age, BMI, gender, and WBIS. Participants who were eligible based upon the online screener were then contacted by phone. Participants referred from other studies or other individuals only completed the phone screen. Twenty‐eight women were then randomized to one of two interventions: 1) LM + MSC or 2) LM plus culinary and dietary education classes, which served as the contact‐matched control (CON). All participants received an identical 4‐month, group‐based LM program for weight loss, followed by either 2 months of MSC or 2 months of cooking/dietary education classes. Participants were randomized at baseline, but participants did not learn of their intervention assignment until the final week of the LM program. All intervention content was delivered using a securely‐encrypted, HIPAA‐compliant video‐conferencing software (i.e., Zoom). Assessments occurred at baseline, 4 months (end of LM program), 6 months (end of the MSC or CON), and 9 months (following a 3 months, no‐contact follow‐up period). Questionnaire measures were completed online prior to an in‐person visit, where weight was obtained. Individuals completing all 4‐ or 6‐month assessment measures were placed into a drawing to win one of two $75 Amazon gift cards at each time point. At 9 months, participants were compensated $25 in cash for completing assessment procedures. Informed consent was obtained prior to enrollment.
1.1.3. Lifestyle modification intervention
The 4‐month LM program was modeled after the Look AHEAD trial 41 with a mix of individual and group contact, and was designed to produce a 1–2 lb weight loss per week. Participants were given a calorie intake goal of 1500–2000 kcals/day (depending upon baseline weight) and were instructed to increase moderate‐to‐vigorous intensity physical activity, gradually progressing to 200 min/week. Participants were also given a personal weight loss goal of 10% of initial body weight. To facilitate achievement of this goal, participants were instructed to self‐monitor weight, dietary intake, and physical activity minutes daily and submitted their data electronically each week. Personalized feedback was provided by the interventionist and emailed to the participant weekly during weeks 1–4, and at least once per month thereafter. Intervention sessions included a combination of group‐based meetings (12 1‐h classes) and individual, one‐on‐one meetings with a study interventionist (during weeks 1, 5, 9 when group meetings were not held, approximately 15 min/session). Group sessions were designed to be interactive. Individual sessions with the interventionist discussed progress toward study goals, problem solving around barriers, and individual goal setting. Following the 4‐month program, participants were encouraged to continue the dietary, activity, and behavioral guidelines taught in the program, although these data were no longer reported to the intervention team.
1.1.4. Mindful self‐compassion intervention (MSC)
The 8‐week MSC program was a manualized, once‐weekly protocol designed to increase affect regulation and self‐compassion skills and improve psychological well‐being. 42 MSC was delivered in an adapted format comprising eight, 2‐hour sessions focused on guided meditations and reflections, psychoeducation, experiential exercises, group discussion, and recommended daily home practice meditations (10–20 min). Sessions were led by a postdoctoral fellow in clinical psychology also trained as a MSC teacher. Session themes included Discovering Mindful Self‐Compassion, Practicing Mindfulness, Practicing Loving‐Kindness, Discovering Your Compassionate Voice, Living Deeply, Meeting Difficult Emotions, Exploring Challenging Relationships, and Embracing Your Life. 43 To retain fidelity with the MSC protocol, sessions did not explicitly target weight loss or weight loss maintenance, although brief references were made to how MSC principles and practices could be applied in the context of health behavior change.
The decision was made to implement MSC following an initial LM program, and not in conjunction with LM, to minimize participant burden and allow individuals the time to learn and practice key self‐regulatory behaviors known to be associated with significant weight loss (e.g., self‐monitoring, daily self‐weighing, adhering to a calorie intake goal). Further, given that MSC is a time intensive standardized program (i.e., requires at least 2.5 h of content per session, adapted for 2 h in the present study), the duration of classes could have made it more difficult for participants to attend if implemented in conjunction with LM. Finally, it was hypothesized that skills taught within MSC classes would complement the self‐regulatory skills taught within LM and aid in further weight loss or improved weight loss maintenance, but that it was first important to learn those key weight loss skills and jump start weight loss.
1.1.5. Cooking and dietary education
Participants randomized to CON received 8 weeks of nutrition and cooking classes upon completion of the LM program. These group sessions were 1.5 h in length and were led once per week by a registered dietician. This group served as a contact‐matched control condition, in which participants were provided with intervention content relevant to weight loss (to promote attendance) yet unlikely to influence weight or psychological constructs targeted by MSC. No behavioral strategies for changing diet or inducing weight loss were discussed. Topics included nutrition (e.g., fruits and vegetables, grains, fluids, antioxidants, protein, sodium), culinary education (e.g., setting up a cooking workstation, safe food handling, knife skills, healthy dessert preparation), and healthy recipes.
1.2. Measures
1.2.1. Weight and height
Height was measured (baseline only) to the nearest millimeter using a stadiometer, and weight was measured at all assessments to the nearest 0.1 kg using a digital scale.
1.2.2. Assessment of feasibility and acceptability
Feasibility was measured by reviewing attendance and retention rates. Acceptability was assessed using program satisfaction questionnaires. Following the LM program and MSC/CON treatments, participants were asked to rate overall satisfaction with the program, program usefulness, and likeliness to recommend the program to family or friends. At 4 months, participants were also asked to rate level of enjoyment with the virtual format and preference for in‐person or virtual LM classes.
1.2.3. Psychosocial measures
All measures used in this study have been shown to be psychometrically validated and reliable. The primary outcome measure of Internalized‐WS was assessed using the WBIS, 44 , 45 which measures the degree to which an individual believes that negative weight‐related self‐appraisals are relevant and accurate and generates a total mean score. Higher scores indicate greater Internalized‐WS.
The 12‐item Weight‐Self Stigma Questionnaire (WSSQ) 46 was administered as a secondary measure of Internalized‐WS, consistent with prior work. 2 , 13 , 17 The WSSQ generates a total sum score, and self‐devaluation and fear of enacted stigma (also termed anticipated stigma) subscales, all reported here. Higher scores indicate greater Internalized‐WS.
Self‐compassion was assessed using the 26‐item Self‐Compassion Scale (SCS). 47 The current study reports an overall mean score of self‐compassion as well as two subscale scores comprising “warm” items (self‐warmth; comprising self‐kindness, common humanity, mindfulness) and “cold” items (self‐coldness; self‐judgment, isolation, and over‐identification), given recent controversy regarding the optimal structure of this scale. 48 , 49 , 50 [Correction added on 20 June 2022, after first online publication: References [48–50] have been cited in the preceding sentence.] Higher scores indicate greater self‐compassion.
Internalized shame, the extent to which people have internalized the painful effect of shame, was assessed using the sum score for the 30‐item Internalized Shame Scale (ISS). 51 , 52 Greater scores indicate greater shame.
Dietary disinhibition, referring to a tendency for people to experience loss of control over eating particularly during emotional distress, was assessed with the Three Factor Eating Questionnaire's 16‐item disinhibition subscale (TFEQ‐D). 53 Higher sum scores indicate greater disinhibition.
Intuitive eating was assessed using the 23‐item Intuitive Eating Scale‐2 (IES‐2). 54 , 55 The IES‐2 produces four subscale scores and an overall mean intuitive eating score, the latter reported here. Higher scores denote greater intuitive eating.
1.3. Statistical analysis
The primary study goal was the assessment of feasibility and acceptability as this research is in its earliest phases. This study was not powered to detect statistical between‐group differences although as an index of preliminary efficacy differences are reported where significant and effect sizes (ES) are emphasized to interpret substantive findings. Marginal between‐group findings (i.e., p‐value: 0.05 to <0.10) are noted. All available cases were analyzed, using listwise deletion. Baseline demographics, measures of feasibility and acceptability (program satisfaction), and percentage of participants achieving clinically significant weight loss were summarized and compared between treatment arms using t‐tests for continuous variables and chi‐squared tests for categorical variables. To accommodate the study design whereby participants learned of their randomization into MSC versus CON 4 months following baseline, a series of ANCOVAs were used to examine treatment effects on changes in psychosocial outcomes, eating behaviors, and weight from baseline to 4 months, and from 4‐ to 6‐month and 4‐ to 9‐month follow‐ups controlling for initial changes (baseline to 4 months). Analyses were run in SPSS 25 and significance level was set at 0.05 a priori. All analyses were based on a priori hypotheses, therefore adjustment for multiple comparisons was not made. Cohen's d was computed from partial eta squared for time by randomization group. 56
All study procedures were approved by The Miriam Hospital's Institutional Review Board.
2. RESULTS
2.1. Participants
See Figure 1 for CONSORT diagram characterizing recruitment flow and retention rates. Twenty‐eight participants began the LM program (n = 14 MSC and n = 14 CON) and 89.3% (n = 13 MSC and n = 12 CON) completed the 4‐month assessment and thus received their randomization assignment. Of those, 100% (n = 25) completed the 6‐month assessment and 96% (n = 24; missing one CON participant) completed the 9‐month assessment. At baseline, participants had an average BMI of 46.6 ± 3.7 kg/m2, were 48.8 ± 10.4 years of age, and were predominately White (92.9%) and non‐Hispanic (89.3%). The mean WBIS score for all participants at baseline was 5.1, similar to other work in this population. 13 Treatment groups did not differ on any demographic or baseline psychosocial measures (Table 1).
FIGURE 1.
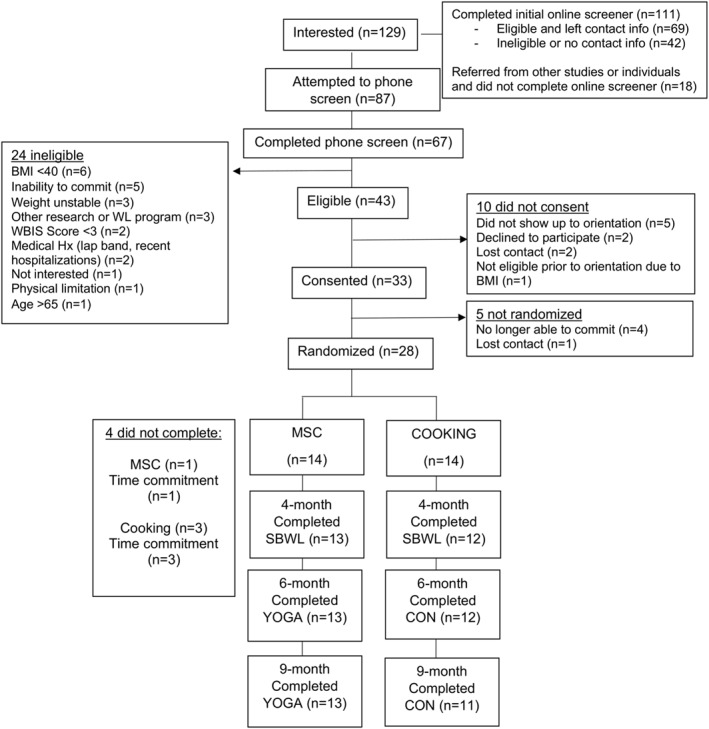
CONSORT diagram
TABLE 1.
Baseline demographics
| Likert scale range | Total (n = 28) | MSC (n = 14) | CON (n = 14) | p‐value for difference between groups | |
|---|---|---|---|---|---|
| Age (years) | 48.8 ± 10.4 | 48.4 ± 11.3 | 49.1 ± 9.7 | 0.86 | |
| Weight (kg) | 123.0 ± 12.7 | 124.8 ± 13.2 | 121.1 ± 12.5 | 0.46 | |
| BMI (kg/m2) | 46.6 ± 3.7 | 46.6 ± 3.6 | 46.6 ± 3.9 | 0.99 | |
| Internalized weight bias (WBIS) | 1–7 | 5.1 ± 1.1 | 5.0 ± 1.2 | 5.1 ± 1.1 | 0.68 |
| Weight self‐stigma (WSSQ – Total) | 12–60 | 42.3 ± 6.8 | 43.2 ± 7.9 | 41.5 ± 5.8 | 0.52 |
| Weight self‐stigma (WSSQ – Self‐devaluation) | 6–30 | 20.7 ± 4.5 | 21.6 ± 4.5 | 19.9 ± 4.5 | 0.32 |
| Weight self‐stigma (WSSQ – anticipated stigma) | 6–30 | 21.6 ± 3.6 | 21.6 ± 4.1 | 21.6 ± 3.2 | 0.98 |
| Internalized shame (ISS) | 0–96 | 44.6 ± 21.9 | 44.5 ± 22.3 | 44.7 ± 22.5 | 0.98 |
| Self‐compassion (SCS – Total) | 1–5 | 3.0 ± 0.9 | 2.9 ± 0.6 | 3.1 ± 1.0 | 0.46 |
| Dietary disinhibition (TFEQ‐D) | 2–15 | 10.7 ± 3.2 | 11.2 ± 3.4 | 10.3 ± 3.0 | 0.45 |
| Intuitive eating (IES‐2) | 1–5 | 2.8 ± 0.4 | 2.7 ± 0.4 | 2.9 ± 0.4 | 0.17 |
Abbreviations: IES‐2 (Intuitive Eating Scale‐2); ISS, Internalized Shame Scale; SCS, Self‐Compassion Scale; TFEQ, Three Factor Eating Questionnaire; WBIS, Weight Bias Internalization Scale; WSSQ, Weight Self‐Stigma Questionnaire.
2.2. Weight
Figure 2 shows the trajectory of weight change over time by treatment arm. On average, participants lost 7.5 ± 4.2 kg (6.3 ± 3.7% of their starting body weight) following the 4‐month LM program and 60% of individuals achieved a clinically significant weight loss (≥5%), with no difference by treatment arm (p's > 0.87). The MSC and cooking/dietary education programs produced little additional weight loss. Weight change did not differ between groups from 4 to 6 months, and from 4 to 9 months weight loss was marginally greater in CON versus MSC, with a small ES.
FIGURE 2.
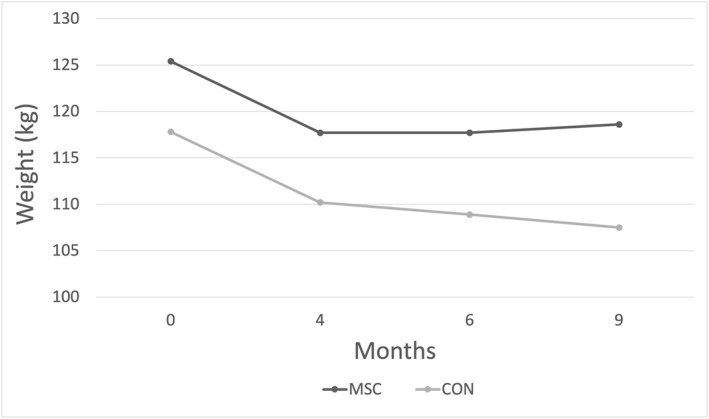
Weight change over time. Figure only includes those participants completing the 4‐month weight loss program (n = 25; MSC n = 13, CON n = 12) for all timepoints 0–6 months. Nine‐month timepoint for CON reflects all available data (n = 11)
2.3. Feasibility and acceptability
On average, participants attended 13.7 ± 2.9 out of 15 virtual behavioral weight loss sessions (group and individual combined). 89% of participants attended ≥80% of all group sessions and 89% attended all 3 individual sessions. Overall, participants reported high satisfaction to the LM program (5.7 ± 1.4 on 1–7 Likert scale; 88% reported satisfaction level ≥5) and indicated being highly likely to recommend the weight loss program to friends or family (6.0 ± 1.4 on 1–7 Likert scale; 88% rated ≥5). When queried regarding a preference for in‐person or virtual classes in the future, the responses were split, with 52% indicating in‐person classes and 48% indicating virtual classes.
Attendance at cooking and dietary education classes (7.7 ± 0.7 out of 8) was better than attendance at MSC classes (6.9 ± 0.8; p = 0.015). Similarly, CON participants were slightly more satisfied with the 2‐month program compared to MSC participants (5.7 ± 1.2 vs. 4.6 ± 1.6 out of 7; p = 0.07), with 83% of CON participants reporting a satisfaction level ≥5 versus 46% of MSC participants reporting this level of satisfaction. Cooking and dietary education participants also rated the program as being more useful than MSC participants (5.2 ± 1.4 vs. 3.9 ± 1.5 relatively; p = 0.03).
2.4. Psychosocial and behavioral outcomes, including Internalized‐WS
Table 2 displays the change in psychosocial measures over time across groups and by treatment arm. Figure 3 shows the trajectories of change in Internalized‐WS (primary outcome measure, WBIS) over time by treatment arm.
TABLE 2.
Change in psychosocial variables
| Mean difference (overall) | Time p‐value a | MSC | CON | Group × Time p‐value b | Cohen's d c | |
|---|---|---|---|---|---|---|
| WBIS | ||||||
| BL to 4 months | −0.7 ± 0.7 | <0.001 | −1.0 ± 0.6 | −0.3 ± 0.5 | 0.004 | 0.65 |
| 4–6 months d | −0.6 ± 0.9 | 0.004 | −0.8 ± 1.0 | −0.3 ± 0.7 | 0.082 | 0.26 |
| 4–9 months d | −0.2 ± 0.7 | 0.051 | −0.3 ± 0.7 | −0.2 ± 0.7 | 0.404 | 0.07 |
| WSSQ (total) | ||||||
| BL to 4 months | −3.8 ± 6.8 | 0.010 | −5.9 ± 5.0 | −1.5 ± 8.0 | 0.106 | 0.22 |
| 4–6 months d | −2.5 ± 4.6 | 0.039 | −3.8 ± 5.5 | −1.1 ± 3.1 | 0.194 | 0.15 |
| 4–9 months d | −2.3 ± 5.0 | 0.101 | −2.1 ± 5.7 | −2.6 ± 4.5 | 0.673 | 0.02 |
| WSSQ (self‐devaluation) | ||||||
| BL to 4 months | −1.4 ± 4.1 | 0.111 | −2.5 ± 3.0 | −0.1 ± 4.8 | 0.135 | 0.19 |
| 4–6 months d | −1.3 ± 2.6 | 0.056 | −1.8 ± −0.7 | −0.7 ± 1.6 | 0.413 | 0.06 |
| 4–9 months d | −1.6 ± 3.5 | 0.064 | −1.5 ± 3.9 | −1.7 ± 3.2 | 0.817 | 0.01 |
| WSSQ (anticipated stigma) | ||||||
| BL to 4 months | −2.4 ± 3.9 | 0.005 | −3.4 ± 2.9 | −1.4 ± 4.7 | 0.219 | 0.13 |
| 4–6 months d | −1.2 ± 2.8 | 0.021 | −2.0 ± 3.1 | −0.4 ± 2.4 | 0.106 | 0.23 |
| 4–9 months d | −0.8 ± 2.3 | 0.141 | −0.6 ± 2.5 | −0.9 ± 2.1 | 0.900 | 0.00 |
| Internalized shame | ||||||
| BL to 4 months | −7.5 ± 15.5 | 0.012 | −15.6 ± 13.7 | 1.3 ± 12.6 | 0.004 | 0.65 |
| 4–6 months d | −5.4 ± 10.0 | 0.018 | −5.7 ± 11.0 | −5.2 ± 9.2 | 0.693 | 0.01 |
| 4–9 months d | −1.6 ± 6.0 | 0.371 | −0.6 ± 7.1 | −2.7 ± 4.5 | 0.333 | 0.09 |
| Self‐compassion (total) | ||||||
| BL to 4 months | 0.3 ± 0.5 | 0.008 | 0.4 ± 0.6 | 0.2 ± 0.5 | 0.267 | 0.11 |
| 4–6 months d | 0.3 ± 0.6 | 0.006 | 0.6 ± 0.6 | −0.1 ± 0.4 | 0.002 | 0.79 |
| 4–9 months d | 0.1 ± 0.5 | 0.097 | 0.2 ± 0.5 | 0.02 ± 0.4 | 0.257 | 0.12 |
| Self‐compassion (self‐coldness) | ||||||
| BL to 4 months | −0.01 ± 1.4 | 0.992 | −0.3 ± 1.2 | −0.3 ± 1.5 | 0.370 | 0.04 |
| 4–6 months d | −0.5 ± 1.3 | 0.003 | −0.6 ± 1.4 | −0.5 ± 1.2 | 0.162 | 0.21 |
| 4–9 months d | −0.4 ± 0.9 | 0.003 | −0.5 ± 1.1 | −0.2 ± 0.8 | 0.223 | 0.15 |
| Self‐compassion (self‐warmth) | ||||||
| BL to 4 months | 0.2 ± 0.6 | 0.075 | 0.3 ± 0.6 | 0.1 ± 0.5 | 0.479 | 0.02 |
| 4–6 months d | 0.3 ± 06 | <0.001 | 0.6 ± 0.6 | 0.1 ± 0.4 | <0.001 | 0.80 |
| 4–9 months d | 0.1 ± 0.5 | 0.073 | 0.2 ± 0.1 | 0.001 ± 0.5 | 0.174 | 0.20 |
| TFEQ – Disinhibition | ||||||
| BL to 4 months | −1.3 ± 3.3 | 0.068 | −1.5 ± 3.7 | −1.1 ± 2.8 | 0.779 | 0.01 |
| 4–6 months d | −1.0 ± 2.7 | 0.048 | −0.8 ± 3.0 | −1.3 ± 2.4 | 0.645 | 0.02 |
| 4–9 months d | −0.6 ± 2.4 | 0.036 | −0.6 ± 2.9 | −0.5 ± 1.6 | 0.852 | 0.00 |
| Intuitive Eating | ||||||
| BL to 4 months | 0.2 ± 0.3 | 0.018 | 0.2 ± 0.3 | 0.1 ± 0.3 | 0.467 | 0.05 |
| 4–6 months d | 0.2 ± 0.4 | <0.001 | 0.3 ± 0.3 | 0.1 ± 0.3 | 0.020 | 0.46 |
| 4–9 months d | 0.1 ± 0.4 | 0.020 | 0.1 ± 0.4 | 0.01 ± 0.3 | 0.214 | 0.15 |
| Weight (kg) | ||||||
| BL to 4 months | −7.5 ± 4.2 | <0.001 | −7.7 ± 3.7 | −7.3 ± 4.9 | 0.820 | 0.00 |
| 4–6 months d | −0.6 ± 2.7 | 0.046 | 0.0 ± 2.9 | −1.2 ± 2.4 | 0.163 | 0.00 |
| 4–9 months d | −0.8 ± 5.3 | 0.142 | 0.9 ± 5.0 | −2.7 ± 5.2 | 0.075 | 0.33 |
Note: Bolded values denote statistical significance and/or a meaningful effect size.
Time p‐value refers to a dependent t‐test comparing BL to 4 months, 4–6 months, and 4–9 months across all participants.
Group * time p‐value refers to between‐groups ANCOVAs from BL to 4 months, and from 4 to 6 months and 4–9 months (controlling for change from BL to 4 months).
Effect size (ES) thresholds are standard for BL to 4 months; from 4 to 6 months and 4–9 months, small effect sizes (0.2–0.5) are considered meaningful for psychosocial measures, as the primary treatment target (Internalized‐WS; WBIS) for MSC reduced before the MSC intervention. 57 , 58 WBIS, Weight Bias Internalization Scale; WSSQ, Weight Self‐Stigma Questionnaire.
Models adjust for change from baseline to 4 months.
FIGURE 3.
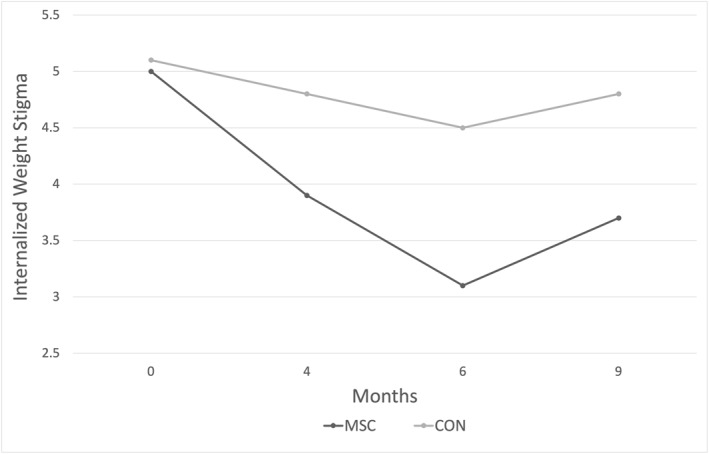
Internalized weight stigma (IWS) change over time as measured by primary IWS outcome metric, the Weight Bias Internalization Scale (WBIS). Figure only includes those participants completing the 4‐month weight loss program (n = 25; MSC n = 13, CON n = 12) for all timepoints 0–6 months. Nine‐month timepoint for CON reflects all available data (n = 11)
Interpretation of effect size (ES) thresholds are standard for BL to 4 months. However, small ES (0.2–0.5) are considered meaningful for the interpretation of psychosocial measure ES from 4 to 6 months and 4–9 months, because the primary treatment target (Internalized‐WS; WBIS) for MSC reduced before the MSC intervention. 57 , 58
Across both groups, the 4‐month virtual LM program yielded significant improvements in all outcomes except weight self‐stigma (self‐devaluation), self‐compassion (self‐coldness, self‐warmth), and dietary disinhibition. Although group assignment had not yet been revealed during LM, MSC experienced greater reductions in Internalized‐WS and shame than did CON, with medium ES.
Next, the short‐term effect of MSC versus control on each outcome was examined by assessing 4‐to‐6‐month changes (i.e., post‐LM to post‐MSC/CON). Across both groups, participants further statistically improved on all measures save self‐compassion (self‐coldness), with marginally greater improvements in weight self‐stigma (self‐devaluation). Compared to CON, MSC reported significantly greater gains in self‐compassion (total and self‐warmth, both large ES) and intuitive eating (medium ES), and marginally greater gains in WBIS. Meaningful improvements, as determined by small ES, were also observed in favor of MSC versus control for Internalized‐WS (WBIS), weight self‐stigma (anticipated stigma) and self‐compassion (self‐coldness).
Last, whether post‐LM changes were maintained following MSC/CON was examined by assessing 4‐to‐9‐month changes. Participants across groups reported further significant improvements in self‐compassion (self‐coldness), disinhibition, and intuitive eating, and marginally greater improvements in Internalized‐WS. There were no significant group × time interactions. There was a meaningful increase in self‐compassion (self‐warmth) in MSC versus CON (small ES).
3. DISCUSSION
This pilot RCT was the first to evaluate a remote‐based lifestyle modification (LM) program followed by mindful self‐compassion (MSC) training for individuals with Class III obesity reporting elevated levels of internalized weight stigma (Internalized‐WS). Intervention attendance throughout the 4‐month LM program was excellent and women were overall very satisfied with the LM program. Attendance and satisfaction lagged in MSC versus dietary education control (CON), although MSC evidenced statistically and/or meaningfully greater change in Internalized‐WS, self‐compassion, and intuitive eating from 4 to 6 months relative to CON. Clinically significant weight loss was also achieved across groups, with a mean 4‐month weight loss of 6.3%; however MSC did not produce any additional weight loss relative to CON.
Reduced Internalized‐WS in MSC versus CON from 4 to 6 months was only marginally significant with a small effect size (ES). Indeed, during LM treatment and prior to participants learning their randomization assignment, Internalized‐WS and internalized shame – key targets of the MSC intervention – evidenced medium‐to‐large declines in MSC relative to CON. This raises the possibility that MSC treatment may have led to greater improvements in Internalized‐WS had large reductions not been observed during LM. It is also possible that people randomized to MSC might have continued to improve on Internalized‐WS independent of their treatment assignment due to unmeasured characteristics, underscoring a need for continued investigation with larger sample sizes with attention to treatment moderators.
In our sample of women with Class III obesity, the magnitude of reduction in Internalized‐WS during LM among those subsequently randomized to MSC was similar to that observed in another LM trial of people with overweight/obesity and elevated Internalized‐WS, 13 and lower than seen in other samples with overweight/obesity that were not screened on Internalized‐WS. 15 , 16 Nonetheless, during LM in this study, individuals subsequently randomized to CON evidenced minimal reductions in Internalized‐WS, indicating variability in the effects of LM on Internalized‐WS and emphasizing a need for continued research to elucidate those for whom LM reduces Internalized‐WS and/or the longevity and correlates of such changes to inform treatment development.
The finding of increased self‐compassion from 4‐to‐6 months in MSC versus CON comports with those of prior RCTs on the MSC program. 59 , 60 , 61 These findings also align with those of the RCT that compared videoconference LM + self‐compassion training to LM alone. 34 The latter study also showed increased self‐compassion in the intervention group, no differences in weight between groups, and increased intuitive eating across groups. These findings extend this literature by showing that following an initial LM among women with Class III obesity and heightened Internalized‐WS, MSC training also yields greater increases in intuitive eating than does CON. Intuitive eating may emerge a novel and implicit outcome of self‐compassion training, consistent with prospective evidence linking changes in intuitive eating to reduced Internalized‐WS and increased self‐compassion. 62
Of note, most post‐LM changes in Internalized‐WS, shame, self‐compassion, disinhibition, and intuitive eating were maintained or further improved at 9‐month follow‐up irrespective of participation in subsequent MSC or CON. Participants were encouraged to continue everything learned in LM during participation in MSC or CON, although neither condition explicitly emphasized weight loss. This study's findings suggest the possibility that more explicit tailoring for weight management may be necessary for MSC training to have a stronger effect on Internalized‐WS, self‐compassion, eating behaviors, and/or weight. Indeed, most studies examining self‐compassion training for weight‐related outcomes in a recent review delivered such training integrated with weight loss principles. 32 While the latter review found small effects of self‐compassion training on weight loss, a more recent and rigorous study comparing LM to LM + self‐compassion found no differential effects by group. 34 A longer duration of self‐compassion training, and/or consistent practice in the form of self‐compassion meditation may be helpful in improving weight‐related outcomes; approaches that integrate booster sessions and/or ongoing group or home practice support may prove supportive in this regard.
This study's findings complement Palmeira et al.’s 14 weight‐inclusive approach integrating acceptance and commitment therapy with compassion‐focused therapy to address Internalized‐WS, which found self‐compassion to mediate reductions in Internalized‐WS and emotional eating alongside reductions in BMI. 14 Indeed, self‐compassion is a common component in weight‐inclusive interventions such as intuitive eating given its affect regulation and stigma protective properties. 63 Given evidence suggesting self‐compassion interventions are most consistently linked to improved eating behaviors, 32 such training may be particularly helpful for individuals with obesity who eat to regulate negative affect (e.g., binge eating). 64 , 65 Future research would benefit from examining whether such training delivered in the context of LM or in a weight‐neutral context similar to Palmeira et al's 14 study beneficially influences weight and other parameters long‐term, as well as moderators of treatment response.
The magnitude of weight loss achieved during the 4‐month virtual LM program is in the range of that reported with more traditional face‐to‐face LM programs (7%–9%) for those with Class III obesity, some of which included additional elements, such as meal replacement products. 39 , 66 , 67 These comparable weight losses suggest that LM programs delivered via video‐conferencing platforms are effective for individuals with this magnitude of obesity, and thus have potential to expand treatment access to hard‐to‐reach populations and to reduce patient travel time and expenses. Indeed, half of study participants stated a preference for a virtual format over in‐person sessions. More direct comparisons of face‐to‐face and virtual LM formats are needed.
Despite these promising LM findings, the MSC program had no impact on weight relative to CON either at six or 9 months – indeed, weight loss was 3% higher in CON versus MSC at 9 months, with a small effect size. Such findings align with those of earlier‐generation non‐dieting approaches, which often found improved benefit of non‐dieting relative to LM pertaining to psychological health and eating behaviors, but not weight loss. 19 , 20 , 21 , 22 Nonetheless, this may in part relate to the use of a strong control group that led to continued weight loss. While weight loss was not discussed during CON, participants learned of the health benefits of fruits, vegetables, and other healthy foods while taking cooking classes. Moreover, the clear relevance of CON to weight loss and the preceding LM program likely contributed to the high program satisfaction ratings of CON when compared to MSC, which only nominally discussed application of self‐compassion to weight‐related behaviors.
Regarding future directions, although post‐LM reductions in Internalized‐WS were maintained in this study alongside weight loss across groups at follow‐up, some research suggests that such improvements may remit upon weight regain. 68 Reductions in Internalized‐WS during LM may be primarily driven by reductions in body size, which may decrease exposure to weight stigma experiences and self‐application of weight‐based stereotypes. This may be a feasible approach to reducing Internalized‐WS for those who successfully maintain weight loss following LM, yet for the majority who do not, a more sustainable approach may be needed. Self‐compassion training is theorized to improve Internalized‐WS through the weight‐neutral pathway of promoting self‐compassion to reduce self‐application of negative stereotypes. This weight‐neutral approach may take more time to achieve outside the context of reducing body size given the deep entrenchment of Internalized‐WS and the cultural pervasiveness of weight stigma, yet may also lead to longer‐term health behavior change and improved cardiometabolic health for some individuals relative to LM. Continued work is needed to ascertain whether an approach eschewing an explicit emphasis on weight loss, or one integrating LM with self‐compassion and/or Internalized‐WS‐reduction techniques, will more effectively promote cardiometabolic health in the long term and the behavioral phenotypes that may differentially respond to such treatments.
3.1. Strengths and limitations
While this study had many strengths including a randomized design, high retention rates, fully remote intervention delivery, and the novel application of MSC following LM for those with severe obesity, it is not without limitations. First, given that this was a preliminary investigation in this area, the sample size was relatively small and the study was not sufficiently powered to answer the proposed research questions. Second, given that the LM program for both treatment conditions was delivered via video conferencing software, it was not possible to properly evaluate whether the change in weight loss and psychosocial factors would be similar to an in‐person LM program. This study was also limited to predominately white women with severe obesity who endorsed some degree of weight bias internalization; thus, findings may not be generalizable to other populations, including those with lesser degrees of obesity. Given widespread population health disparities among ethno‐racial and sexual and gender minorities, future research would benefit from over‐sampling these groups and tailoring the intervention to specific minority stressors that may intersect with Internalized‐WS in these populations.
4. CONCLUSION
Study findings offer promise for the delivery of LM treatment for individuals with severe obesity using a virtual platform. The use of video conferencing software allows for more individuals, especially those in remote areas, to participate in these types of programs. More direct comparisons of face‐to‐face and virtual LM treatment are needed. MSC yielded meaningful improvement in Internalized‐WS, self‐compassion, and intuitive eating but no significant improvement in weight loss relative to CON. Future work is needed to elucidate the effects and longevity of self‐compassion training on Internalized‐WS and energy balance behaviors using both weight‐normative (e.g., LM) and weight‐inclusive (e.g., intuitive eating) approaches, as well as the behavioral phenotypes that may benefit from each respective approach.
AUTHOR CONTRIBUTIONS
Jessica L. Unick and Tosca D. Braun conceived the study and guided study design with the input of Kayloni Olson, Emily Panza, and Jason Lillis, and acquired, analyzed the data (with Zachary Kunicki's consultation), and interpreted data for the work, drafted the work, and revised it critically for important intellectual content. Kayloni Olson, Emily Panza, Jason Lillis, Leah Schumacher, Ana M. Abrantes, and Zachary Kunicki were involved in revising the work critically for important intellectual content. All authors provided final approval of the version to be published.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ACKNOWLEDGMENTS
This work was supported by training grants to Dr. Tosca Braun (NCCIH, U01 AT010863‐02S1; NHLBI, T32 HL076134), Dr. Leah Schumacher (NHLBI, T32 HL076134), Dr. KayLoni Olson (NIDDK, K23 DK124578), and Dr. Emily Panza (NIMHD, K23 MD015092).
Braun TD, Olson K, Panza E, et al. Internalized weight stigma in women with Class III obesity: a randomized controlled trial of a virtual lifestyle modification intervention followed by a mindful self‐compassion intervention. Obes Sci Pract. 2022;8(6):816‐827. 10.1002/osp4.616
REFERENCES
- 1. Rubino F, Puhl RM, Cummings DE, et al. Joint international consensus statement for ending stigma of obesity. Nat Med. 2020;26:485–497. 10.1038/s41591-020-0803-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obes Rev. 2018;19(8):1141‐1163. 10.1111/obr.12701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tomiyama AJ, Carr D, Granberg EM, et al. How and why weight stigma drives the obesity “epidemic” and harms health. BMC Med. 2018;16(1):1‐6. 10.1186/s12916-018-1116-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Puhl RM, Himmelstein MS, Pearl RL. Weight stigma as a psychosocial contributor to obesity. Am Psychol. 2020;75(2):274‐289. 10.1037/amp0000538 [DOI] [PubMed] [Google Scholar]
- 5. Himmelstein MS, Puhl RM, Quinn DM. Intersectionality: an understudied framework for addressing weight stigma. Am J Prev Med. 2017;53(4):421‐431. 10.1016/j.amepre.2017.04.003 [DOI] [PubMed] [Google Scholar]
- 6. Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutr Res Rev. 2017;30(2):272‐283. 10.1017/S0954422417000154 [DOI] [PubMed] [Google Scholar]
- 7. Linardon J, Tylka TL, Fuller‐Tyszkiewicz M. Intuitive eating and its psychological correlates: a meta‐analysis. Int J Eat Disord. 2021;54(7):1073‐1098. 10.1080/10640266.2019.1580126 [DOI] [PubMed] [Google Scholar]
- 8. Tylka TL, Calogero RM, Daníelsdóttir S. Intuitive eating is connected to self‐reported weight stability in community women and men. Eat Disord. 2020;28(3):256‐264. 10.1080/10640266.2019.1580126 [DOI] [PubMed] [Google Scholar]
- 9. Braun TD, Gorin AA, Puhl RM, et al. Shame and self‐compassion as risk and protective mechanisms of the internalized weight bias and emotional eating link in individuals seeking bariatric surgery. Obes Surg. 2021;31(7):3177–3187. 10.1007/s11695-021-05392-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee MS, Gonzalez BD, Small BJ, Thompson JK. Internalized weight bias and psychological wellbeing: an exploratory investigation of a preliminary model. PLoS One. 2019;14(5):1‐12. 10.1371/journal.pone.0216324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Puhl RM, Quinn DM, Weisz BM, Suh YJ. The role of stigma in weight loss maintenance among U.S. adults. Ann Behav Med. 2017;51(5):754‐763. 10.1007/s12160-017-9898-9 [DOI] [PubMed] [Google Scholar]
- 12. Tylka TL, Annunziato RA, Burgard D, et al. The weight inclusive versus the weight normative approach to health: evaluating the evidence for prioritising wellbeing over weight loss. J Obes. 2014;18. 10.1155/2014/983495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pearl RL, Wadden TA, Bach C, et al. Effects of a cognitive‐behavioral intervention targeting weight stigma: a randomized controlled trial. J Consult Clin Psychol. 2020;88(5):470‐480. 10.1037/ccp0000480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Palmeira L, Cunha M, Pinto‐Gouveia J. Processes of change in quality of life, weight self‐stigma, body mass index and emotional eating after an acceptance‐, mindfulness‐ and compassion‐based group intervention (Kg‐Free) for women with overweight and obesity. J Health Psychol. 2017;24(8):1‐14. 10.1177/1359105316686668 [DOI] [PubMed] [Google Scholar]
- 15. Mensinger JL, Calogero RM, Stranges S, Tylka TL. A weight‐neutral versus weight‐loss approach for health promotion in women with high BMI: a randomized‐controlled trial. Appetite. 2016;105:364‐374. 10.1016/j.appet.2016.06.006 [DOI] [PubMed] [Google Scholar]
- 16. Pearl RL, Wadden TA, Chao AM, et al. Weight bias internalization and long‐term weight loss in patients with obesity. Ann Behav Med. 2018;53(8):782‐787. 10.1093/abm/kay084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pearl RL, Wadden TA, Bach C, Tronieri JS, Berkowitz RI. Six‐month follow‐up from a randomized controlled trial of the weight BIAS Program. Obesity. 2020;28(10):1878‐1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Foreyt JP, Goodrick KG. Weight management without dieting. Nutr Today. 1993;28(2):4‐9. 10.1002/oby.22931 [DOI] [Google Scholar]
- 19. Goodrick GK, Poston WS, Kimball KT, Reeves RS, Foreyt JP. Nondieting versus dieting treatment for overweight binge‐eating women. J Consult Clin Psychol. 1998;66(2):363‐368. 10.1037/0022-006X.66.2.363 [DOI] [PubMed] [Google Scholar]
- 20. Higgins L, Gray W. What do anti‐dieting programs achieve? A review of research. Aust J Nutr Diet. 1999;56(3):128‐136. [Google Scholar]
- 21. Rosen JC, Reiter J. Cognitive behavior therapy for negative body image in obese women. Behav Ther. 1995;26(1):25‐42. 10.1016/S0005-7894(05)80081-4 [DOI] [Google Scholar]
- 22. Nauta H, Hospers H, Jansen A. One‐year follow‐up effects of two obesity treatments on psychological well‐being and weight. Br J Health Psychol. 2001;6(3):271‐284. 10.1348/135910701169205 [DOI] [PubMed] [Google Scholar]
- 23. Potts SK, Weidler DJ. The virtual destruction of self‐compassion: cyberbullying’s damage to young adults. Psi Chi J Psychol Res. 2015;20(4):217‐227. 10.24839/2164-8204.JN20.4.217 [DOI] [Google Scholar]
- 24. Vigna AJ, Poehlmann‐Tynan J, Koenig BW. Is self‐compassion protective among sexual‐ and gender‐minority adolescents across racial groups? Mindfulness. 2020;11(3):800‐815. 10.1007/s12671-019-01294-5 [DOI] [Google Scholar]
- 25. Wong CCY, Knee CR, Neighbors C, Zvolensky MJ. Hacking stigma by loving yourself: a mediated‐moderation model of self‐compassion and stigma. Mindfulness. 2019;10(3):415‐433. 10.1007/s12671-018-0984-2 [DOI] [Google Scholar]
- 26. Goss K, Allan S. Shame, pride and eating disorders. Clin Psychol Psychother. 2009;16(4):303‐316. 10.1002/cpp.627 [DOI] [PubMed] [Google Scholar]
- 27. Hilbert A, Braehler E, Schmidt R, Löwe B, Häuser W, Zenger M. Self‐compassion as a resource in the self‐stigma process of overweight and obese individuals. Obes Facts [Internet]; 2015;8(5):293‐301. 10.1159/000438681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gilbert J, Stubbs RJ, Gale C, Gilbert P, Dunk L, Thomson L. A qualitative study of the understanding and use of ‘compassion focused coping strategies’ in people who suffer from serious weight difficulties. J Compassionate Heal Care. 2014;(1):9. 10.1186/s40639-014-0009-5 [DOI] [Google Scholar]
- 29. Thøgersen‐Ntoumani C, Dodos LA, Stenling A, Ntoumanis N. Does self‐compassion help to deal with dietary lapses among overweight and obese adults who pursue weight‐loss goals? Br J Health Psychol. 2021;26(3):767‐788. 10.1111/bjhp.12499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rahimi‐Ardabili H, Reynolds R, Vartanian LR. A systematic review of the efficacy of interventions that aim to Increase self‐compassion on nutrition habits, eating behaviours, body weight and body image. Mindfulness. 2018;9:388‐400. 10.1007/s12671-017-0804-0 [DOI] [Google Scholar]
- 31. Dunne S, Sheffield D, Chilcot J. Brief report: self‐compassion, physical health and the mediating role of health‐promoting behaviours. J Health Psychol. 2016;23(7):993‐999. 10.1177/1359105316643377 [DOI] [PubMed] [Google Scholar]
- 32. Brenton‐Peters J, Consedine NS, Boggiss A, Wallace‐Boyd K, Roy R, Serlachius A. Self‐compassion in weight management: a systematic review. J Psychosom Res. 2021;150:110617. 10.1016/j.jpsychores.2021.110617 [DOI] [PubMed] [Google Scholar]
- 33. Schnepper R, Reichenberger J, Blechert J. Being my own companion in times of social isolation – a 14‐day mobile self‐compassion intervention improves stress levels and eating behavior. Front Psychol. 2020;11(10):1‐9. 10.3389/fpsyg.2020.595806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Carels RA, Miller JC, Shonrock AT, Byrd JR, Haley E. Exploring the addition of self‐compassion skills training to a behavioral weight loss program delivered using video conferencing software. J Context Behav Sci. 2021;21(July):196‐202. 10.1016/j.jcbs.2021.07.005 [DOI] [Google Scholar]
- 35. Phelan S, Halfman T, Pinto AM, Foster GD. Behavioral and psychological strategies of long‐term weight loss maintainers in a widely available weight management program. Obesity. 2020;28(2):421‐428. 10.1002/oby.22685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Yarnell LM, Neff KD, Davidson OA, Mullarkey M. Gender differences in self‐compassion: examining the role of gender role orientation. Mindfulness. 2019;10(6):1136‐1152. 10.1007/s12671-018-1066-1 [DOI] [Google Scholar]
- 37. Barber JA, Palmese L, Reutenauer EL, Grilo CM, Tek C. Implications of weight‐based stigma and self‐bias on quality of life among individuals with schizophrenia. J Nerv Ment Dis. 2011;199(7):431‐435. 10.1097/NMD.0b013e318221403d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Boswell RG, White MA. Gender differences in weight bias internalisation and eating pathology in overweight individuals. Adv Eat Disord. 2015;3(3):259‐268. 10.1080/21662630.2015.1047881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Unick JL, Beavers D, Jakicic JM, et al. Effectiveness of lifestyle interventions for individuals with severe obesity and type 2 diabetes: results from the look AHEAD trial. Diabetes Care. 2011;34(10):2152‐2157. 10.2337/dc11-0874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Unick JL, Beavers D, Bond DS, et al. The long‐term effectiveness of a lifestyle intervention in severely obese individuals. Am J Med. 2013;126(3):236‐242. 10.1016/j.amjmed.2012.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pi‐Sunyer X, Blackburn G, Brancati FL, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes. Diabetes Care. 2007;30:1374‐1383. 10.2337/dc07-0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Germer C, Neff K. Teaching the Mindful Self‐Compassion Program: A Guide for Professionals. Guilford Press; 2019. [Google Scholar]
- 43. Germer C, Neff K, Mi B, Hickman S. Mindful Self‐Compassion Teacher Guide. Center for Mindful Self‐Compassion; 2015:283. [Google Scholar]
- 44. Durso LE, Latner JD. Understanding self‐directed stigma: development of the weight bias internalization scale. Obesity. 2008;16(Suppl 2):S80–S86. 10.1038/oby.2008.448 [DOI] [PubMed] [Google Scholar]
- 45. Hilbert A, Baldofski S, Zenger M, Lowe B, Kersting A, Braehler E. Weight bias internalization scale: psychometric properties and population norms. PLoS One. 2014;9(1):1‐7. 10.1371/journal.pone.0086303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lillis J, Luoma JB, Levin ME, Hayes SC. Measuring weight self‐stigma: the weight self‐stigma questionnaire. Obesity. 2010;18(5):971‐976. 10.1038/oby.2009.353 [DOI] [PubMed] [Google Scholar]
- 47. Neff KD. The development and validation of a scale to measure self‐compassion. Self Identity. 2003;2:223‐250. 10.1080/15298860309027 [DOI] [Google Scholar]
- 48. Neff KD. The differential effects fallacy in the study of self‐compassion: misunderstanding the nature of bipolar continuums. Mindfulness. 2022;13(3):572‐576. 10.1007/s12671-022-01832-8 [DOI] [Google Scholar]
- 49. Finaulahi KP, Sumich A, Heym N, Medvedev ON. Investigating psychometric properties of the self‐compassion scale using rasch methodology. Mindfulness. 2021;12(3):730‐740. 10.1007/s12671-020-01539-8 [DOI] [Google Scholar]
- 50. Kotera Y, Sheffield D. Revisiting the self‐compassion scale‐short form: stronger associations with self‐inadequacy and resilience. SN Compr Clin Med. 2020;2(6):761‐769. 10.1007/s42399-020-00309-w [DOI] [Google Scholar]
- 51. Cook DR. Measuring shame: the internalized shame scale. Alcohol Treat Q. 1987;4(2):197‐215. [Google Scholar]
- 52. Cook DR. The Internalized Shame Scale: Technical Manual. Multi‐Health Systems, Inc; 1994. [Google Scholar]
- 53. Stunkard AJ, Messick S. The three‐factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71‐83. 10.1016/0022-3999(85)90010-8 [DOI] [PubMed] [Google Scholar]
- 54. Tylka TL, Kroon Van Diest AM. The Intuitive Eating Scale‐2: item refinement and psychometric evaluation with college women and men. J Couns Psychol. 2013;60(1):137‐153. 10.1037/a0030893 [DOI] [PubMed] [Google Scholar]
- 55. Tylka TL, Kroon Van Dienst AM. Protective factors. In: Smolak L, Levine MP, eds. The Wiley Handbook of Eating Disorders. 1st ed. John Wiley & Sons, Ltd; 2015:430‐444. [Google Scholar]
- 56. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Routledge; 1988. [Google Scholar]
- 57. Prentice M. When small effects are impressive. Psychol Bull. 1992;112(1):160‐164. 10.1037/0033-2909.112.1.160 [DOI] [Google Scholar]
- 58. Bakker A, Cai J, English L, Kaiser G, Mesa V, Van Dooren W. Beyond small, medium, or large: points of consideration when interpreting effect sizes. Educ Stud Math. 2019;102(1):1‐8. 10.1007/s10649-019-09908-4 [DOI] [Google Scholar]
- 59. Neff KD, Germer CK. A pilot study and randomized controlled trial of the Mindful Self‐Compassion program. J Clin Psychol. 2012;69(1):28‐44. 10.1002/jclp.21923 [DOI] [PubMed] [Google Scholar]
- 60. Haukaas RB, Gjerde IB, Varting G, Hallan HE, Solem S. A randomized controlled trial comparing the attention training technique and mindful self‐compassion for students with symptoms of depression and anxiety. Front Psychol. 2018;9(5). 10.3389/fpsyg.2018.00827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Quist Møller SA, Sami S, Shapiro SL. Health benefits of (mindful) self‐compassion meditation and the potential complementarity to mindfulness‐based interventions: a review of randomized controlled trials. OBM Integr Complement Med. 2018;4(1):1. 10.21926/obm.icm.1901002 [DOI] [Google Scholar]
- 62. Braun TD, Riley KE, Kunicki ZJ, et al. Internalized weight stigma and intuitive eating among stressed adults during a mindful yoga intervention: associations with changes in mindfulness and self‐compassion. Heal Psychol Behav Med. 2021;9(1):933‐950. 10.1080/21642850.2021.1992282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Tribole E, Resch E. Intuitive Eating. 3rd ed. St. Martin’s Press; 2012. [Google Scholar]
- 64. Braun TD, Park CL, Gorin A. Self‐compassion, body image, and disordered eating: a review of the literature. Body Image. 2016;17:117‐131. 10.1016/j.bodyim.2016.03.003 [DOI] [PubMed] [Google Scholar]
- 65. Turk F, Waller G. Is self‐compassion relevant to the pathology and treatment of eating and body image concerns? A systematic review and meta‐analysis. Clin Psychol Rev [Internet]. 2020;79(Dec):101856. 10.1016/j.cpr.2020.101856 [DOI] [PubMed] [Google Scholar]
- 66. Unick JL, O’Leary KC, Bond DS, Wing RR. Physical activity enhancement to a behavioral weight loss program for severely obese individuals: a preliminary investigation. ISRN Obes. 2012;2012:1‐4. https://www.hindawi.com/journals/isrn/2012/465158/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Goodpaster BH, DeLany JP, Otto AD, et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA, J Am Med Assoc. 2010;304(16):1795‐1802. 10.1001/jama.2010.1505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Cummins L, Olson K, Lillis J, et al. Examining long‐term changes in internalized weight bias in women following a group yoga intervention. Obesity Society Virtual Convention; 2021. [Google Scholar]


