Abstract
Background and Aims.
Although high-resolution manometry (HR_ARM) is commonly used to diagnose defecatory disorders, its intraindividual day-to-day reproducibility is unknown. Since these measurements entail voluntary effort, this study aimed to evaluate the intraindividual day-to-day reproducibility of HR_ARM.
Methods.
In 22 healthy women (35 [14] y, mean [SD]) and 53 constipated patients (42[ 13] y, 46 women), the rectal balloon expulsion time (BET) and anorectal pressures were measured with HR_ARM on 2 days separated by a median (interquartile range) of 15 (11–53) days in healthy and 40 (8–75) days in constipated patients. Anorectal pressures were evaluated at rest (20s), during squeeze, and during evacuation. Rectal sensation was also evaluated in constipated patients. The agreement between both measurements was evaluated with Lin’s concordance correlation coefficient (CCC) and other tests.
Results.
Among constipated patients, the anal resting (mean CCC [95%CI] 0.62 [0.43–0.76]) and squeeze pressures (CCC 0.65 [0.47–0.79]), rectoanal gradient during evacuation (CCC 0.42 [0.17–0.62]), and rectal sensory thresholds (CCC for urgency 0.72 [0.52–0.84]) were concordant. Between days 1 and 2, one or more outcomes, characterized as normal or abnormal, differed in 79% of constipated patients, i.e., anal resting and squeeze pressures, the gradient, and the rectal BET differed in, respectively, 25%, 19%, 36%, and 10% of constipated patients. The rectal BET was prolonged in 3 healthy persons (both days) and either on one day (6 patients) or two days (33 patients) in constipated patients.
Conclusions.
While HR_ARM variables and the BET are reproducible within healthy and constipated persons, the outcome on repeat testing differed in 79% of constipated patients.
Graphical Abstract
Reliability refers to the degree to which test results are stable in measuring what they are intended to measure. Our understanding of the day-to-day reproducibility of anorectal high resolution anorectal manometry (HR_ARM) is limited. reports. In this study, anorectal pressures, rectal sensation, and the BET were reproducible within healthy and constipated persons. However, on repeat testing, the outcome, characterized as normal or abnormal, of one or more anorectal pressures or the balloon expulsion time, differed in 79% of constipated patients.
BACKGROUND
Anorectal manometry and the rectal balloon expulsion test are widely used to diagnose defecatory disorders (DD) in constipated patients and to identify anal weakness in fecal incontinence (1–3). This test can be conducted with non-high-resolution catheters, with high resolution anorectal manometry (HR_ARM) catheters, or with high-definition anorectal manometry (HD_ARM) catheters, which (4). HR_ARM and HD_ARM catheters measure circumferential pressures throughout the anal canal. HD_ARM catheters also measure circumferential pressure symmetry. The design of HR_ and HD_ARM catheters is manufacturer dependent. For the Manoscan HR_ARM and to a lesser extent HD_ARM catheters, normal values in healthy people are available (4).
Reliability refers to the degree to which test results are stable in measuring what they are intended to measure. Summarized elsewhere (5), anal resting and squeeze pressures measured with non-HR_ARM were reproducible as also when measured with a custom-built HR_ARM catheter (5), the Manoscan HD_ARM catheter (6), and the Manoscan HD_ARM catheter (7), respectively, in 80 healthy people, 16 healthy people, and 21 women with fecal incontinence. In the only study that also evaluated these variables, the pressures during evacuation were less reproducible than resting or squeeze pressure (7). More recently, among 28 patients who had a HR_ARM with the Manoscan HR_ARM catheter, “only a minority of patients who underwent repeat anorectal manometry as analyzed by the London Classification had stable manometric findings, raising questions regarding the validity of a single manometric measurement, as currently analyzed, for clinical decision-making” (8). Hence, our aims were to assess the day-to-day reproducibility of anorectal pressures and rectal sensation and rectal balloon expulsion time in healthy people and constipated patients.
MATERIALS AND METHODS
Study Design and Participants
This retrospective cohort study was approved by the Mayo Clinic Institutional Review Board. Informed consent was waived for patients authorizing use of their health records for research. The data were gathered in participants who underwent HR_ARM as part of their clinical assessment and/or other research studies. In 22 healthy women (35 ± 14 y [Mean ± SD]) and 53 patients with constipation (42 ± 13 y, 46 women), HR_ARM and the rectal BET were performed on two occasions (HR_ARM1 and HR_ARM2), which were separated by a median of 15 (11–53) in healthy and 40 (8–75) days in constipated persons. Among the 53 constipated patients, 36 had functional constipation, and 17 had constipation-predominant irritable bowel syndrome. In 35 constipated patients, one examination was performed during the clinical evaluation. In the remaining participants, both assessments were performed for research studies, with no therapeutic intervention (i.e., changes in bowel regimen, anorectal biofeedback therapy or procedures, or use of a footstool to aid defecation) between HR_ARM1 and 2. Asymptomatic participants who had enrolled in previous clinical trials utilizing anorectal manometry were identified through public advertisements and constipated participants were identified from our clinical practice or from prior studies (9–13).
Anorectal Manometry and Balloon Expulsion Test
Anorectal pressures were evaluated in the left lateral position with the Manoscan HR_ARM catheter (Medtronic Inc) at rest (20 s), during contraction of anal sphincter (3 squeeze maneuvers, 20 s each), and evacuation (without rectal distention, 20s) (13, 14). In constipated patients, we also evaluated rectal sensation by stepwise rectal distention (10). During the balloon expulsion test, participants were asked to expel a water filled (50 ml) rectal balloon while seated on a commode; a balloon expulsion time (BET) greater than 60s was abnormal.
Statistical Analysis
The Lin’s concordance correlation coefficient (CCC), paired t tests, and Bland–Altman plots were compared HR_ARM1 and HR_ARM2. Coefficients of variation (CV) were calculated using a nested one-way ANOVA. The intraindividual CV (%) was computed by dividing the root mean square of the error by the overall mean. To estimate the inter-individual CV, the interindividual variance was obtained by computing 50% of the difference between the model mean square error and the residual mean square error, taking its square root, and dividing by the overall mean. On each day, all values were categorized as normal or abnormal with reference to sex-matched and, in women, also age-matched normal values (14).
RESULTS
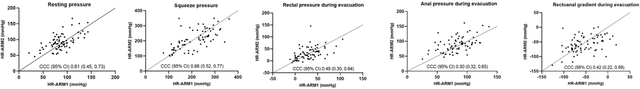
Most pressures were significantly correlated between HR_ARM1 and HR_ARM2 (Figure 1, Table 1). During evacuation, the rectoanal gradient was concordant in healthy and constipated persons; rectal and anal pressures were also concordant in patients. Measured in 32 constipated patients, rectal sensory thresholds were also concordant between HR_ARM1 and HR_ARM2. The Bland Altman’s test was not significant for any variable. Except for the anal resting pressure (p=0.018) and anal pressure during evacuation (0.014), which were greater in the second vs the first study in healthy participants, differences between HR_ARM1 and HR_ARM2 were not significant.
Figure 1. Comparison of anal pressures at rest, squeeze, and recto-anal pressures during evacuation.
Panel A depicts concordance correlation coefficient while Panel B depicts Bland-Altman plots.
Table 1.
Anorectal pressures and rectal sensation in first and second studies
| Parameter | Healthy participants (N=22) | Constipated patients (N=53) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| First study Mean (SD) | Second study Mean (SD) | CCC (95% CI) | Coefficient of variation (%) | First study Mean (SD) | Second study Mean (SD) | CCC (95% CI) | Coefficient of variation (%) | |||
| Intraindividual | Interindividual | Intraindividual | Interindividual | |||||||
| Anal resting pressure, mmHg | 79 (19) a | 90 (28) | 0.55 (0.23, 0.75) | 20 | 21 | 91 (26) | 94 (23) | 0.62 (0.43, 0.76) | 16 | 21 |
| Anal squeeze pressure, mmHg | 225 (62) | 217 (58) | 0.67 (0.36, 0.85) | 15 | 24 | 204 (72) | 205 (70) | 0.65 (0.47, 0.79) | 20 | 28 |
| Squeeze c duration, s | 12 (7) | 14 (6) | 0.76 (0.45, 0.91) | 24 | 44 | 14 (5) | 13 (6) | 0.26 (0.01, 0.50) | 36 | 22 |
| Evacuation | ||||||||||
| Rectal pressure, mmHg | 36 (22) | 29 (18) | 0.39 (0 .01, 0.68) | 48 | 40 | 28 (25) | 33 (28) | 0.52 (0.30, 0.69) | 61 | 63 |
| Anal pressure, mmHg | 69 (18) b | 82 (20) | 0.16 (−0.18, 0.47) | 26 | 8 | 89 (21) | 92 (27) | 0.56 (0.36, 0.72) | 18 | 20 |
| Rectoanal gradient, mmHg | −33 (30) | −53 (21) | 0.34 (0.04, 0.59) | 55 | 34 | −61 (28) | −59 (30) | 0.42 (0.17, 0.62) | 36 | 32 |
| Rectal sensation thresholds (ml) d | ||||||||||
| First sensation, ml | NA | 50 (24) | 40 (51) | 0.43 (0.21, 0.61) | 66 | 58 | ||||
| Urgency, ml | NA | 88 (41) | 77 (54) | 0.72 (0.52, 0.84) | 31 | 49 | ||||
| Discomfort, ml | NA | 129 (49) | 122 (67) | 0.55 (0.29, 0.74) | 31 | 35 | ||||
CCC: Concordance correlation coefficient; CI: confidence interval; NA: not available.
P =0.018
P = 0.014 vs corresponding parameter in the second study
Data available for 50 constipated and 14 healthy participants;
Data available for 32 constipated patients
The intra- and inter-individual coefficients of variation for anal resting and squeeze pressures were less than 30% (Table 1). For the anal squeeze duration, these values were higher. During evacuation, the intra- and inter-individual coefficients of variation were greater for rectal pressure and rectoanal gradient than the anal pressure. In constipated patients, the intra-individual coefficient of variation for the rectal pressure and rectoanal gradient was 61% and 36%. Excluding 3 outliers (i.e., 2 healthy and 1 constipated participant), the intraindividual coefficient of variation for rectal pressure was lower i.e., 36% in healthy and 51% in patients. By comparison, excluding these outliers increased the interindividual coefficient of variation for rectal pressure in healthy (i.e., 47%) and constipated participants (65%).
In 12 healthy (55%) and 42 constipated participants (79%) the outcome, which was characterized as normal or abnormal, of one or more anorectal pressure variables or the BET differed between HR_ARM1 and HR_ARM2. For anal resting pressures, outcomes differed in 6 healthy (27%) and 13 constipated participants (25%) while squeeze pressure differed in 1 healthy (5%) and 10 constipated (19%) participants (Table 2).
Table 2.
Number and proportion of constipated patients with normal and abnormal values in first and second studies 1
| Evacuation | ||||||
|---|---|---|---|---|---|---|
| Parameter | Anal resting pressure | Anal squeeze pressure | Rectal pressure | Anal pressure | Rectoanal gradient | Balloon expulsion time |
| Normal in both HR_ARMs | 34 (64%) | 40 (75%) | 46 (87%) | 41 (77%) | 26 (49%) | 14 (26%) |
| Abnormal in both ARMs | 6 (11%) | 3 (6%) | 2 (4%) | 3 (6%) | 8 (15%) | 33 (62%) |
| Normal (HR_ARM1) and abnormal (HR_ARM2) | 6 (11%) | 3 (6%) | 3 (6%) | 5 (9%) | 7 (13%) | 5 (9%) |
| Abnormal (HR_ARM1) and normal (HR_ARM2) | 7 (13%) | 7 (13%) | 2 (4%) | 4 (8%) | 12 (23%) | 1 (2%) |
Values are n (%) of participants in each category
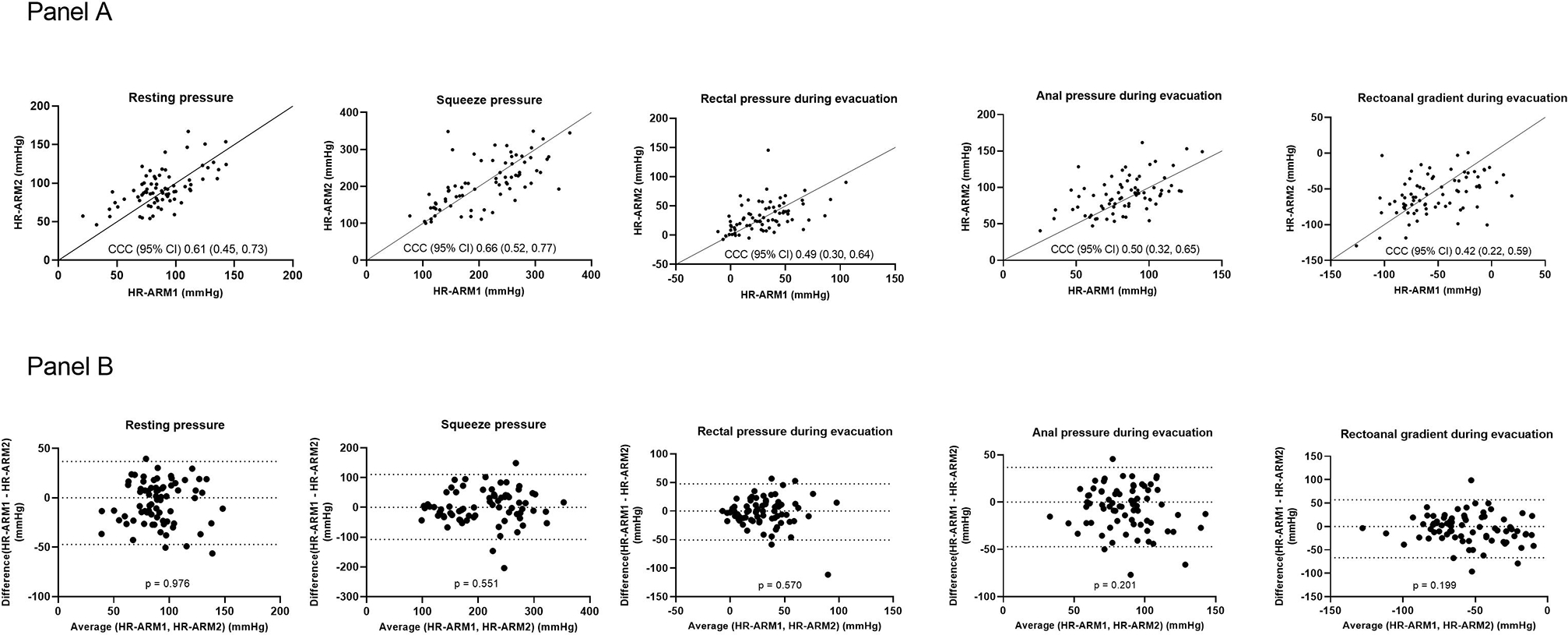
During evacuation, the rectal pressure, anal pressure, and rectoanal gradient were, respectively, different in 1 healthy (5%) and 5 constipated participants (9%), 4 healthy (18%) and 9 constipated participants (17%), and 5 healthy (23%) and 19 constipated participants (36%) (Figure 2). In 3 healthy participants (14%), the BET was prolonged in both studies. In 38 constipated patients (72%), the BET was prolonged on one (6 patients) or both days (33 patients).
Figure 2. Comparison of rectoanal gradient and balloon expulsion test in HR_ARM1 vs HR_ARM2 among 23 patients in whom the rectoanal gradient and/or balloon expulsion time differed between HR_ARM1 and HR_ARM2.
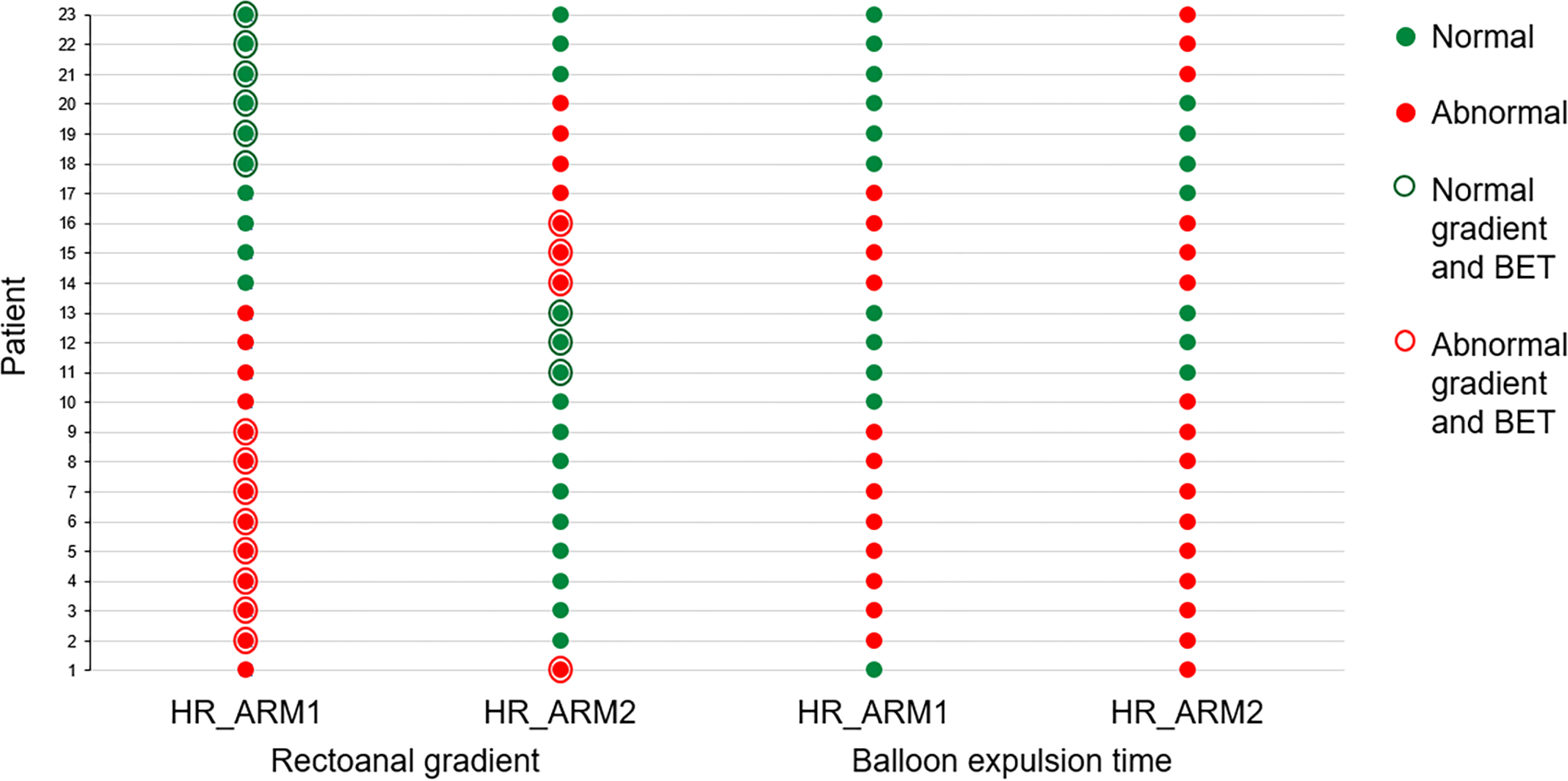
Filled green and red circles represent normal and abnormal results for individual tests (ie, HR_ARM or BET). In 19 and 6 patients, the gradient and BET result differed between HR_ARM1 and HR_ARM2. The open circles represent a combined assessment of the gradient and BET; patients in whom results of both tests were normal or abnormal are respectively indicated as green or red circles. The gradient and BET findings were both normal (green open circles) or abnormal (red open circles) during HR_ARM1 and HR_ARM2, respectively in 14 and 7 patients. By contrast, discordant results (eg, normal gradient and prolonged BET) are not surrounded by an open circle. No patients had the same concurrent findings i.e., normal in HR_ARM1 and HR_ARM2 or abnormal in HR_ARM1 and HR_ARM2.
There were 23 patients in whom the gradient and/or BET findings changed between HR_ARM1 and HR_ARM2. Of these 23 patients, the findings of both tests (ie, gradient and BET) were concurrent (ie, normal or abnormal) in 14 patients (HR_ARM1) and 7 patients (HR_ARM2) (Figure 2). However, no patients had the same concurrent findings in both HR_ARM1 and HR_ARM2.
DISCUSSION
In this study, anal resting and squeeze pressures were reproducible on different days in healthy and constipated persons. In constipated patients, the intra- and inter-individual coefficients of variation of anal resting pressure were 16% and 21%, which is lower than corresponding values with non-HR_ARM in healthy persons (i.e., 26 and 39%). For squeeze pressure, the intra- and interindividual coefficients of variation measured with HR_ARM were 20% and 28%, vs respectively 24% and 35% with non-HR_ARM in healthy persons. Assuming an intra-individual coefficient of variation of 30%, a two-sample parallel group study with a type 1 error of 5% and a power of 80% would require 12 and 29 participants per group to detect a change in means of respectively 30 and 20%.
Among constipated patients, the intra- and inter-individual variation in anal pressure during evacuation were approximately 20%. However, the rectal pressure, hence the rectoanal gradient, during evacuation were more variable among and between patients. Assuming an intra-individual variation of 40%, which is greater than the observed variation of 36%, a trial comparing 2 groups (eg, pelvic floor biofeedback therapy vs placebo) would require 32 and 81 participants per group to detect a percent change in the mean gradient of 30 and 20% with a type 1 error of 5% and a power of 80%. The rectal pressure during evacuation is generated by a voluntary effort (12), which probably explains why the rectal pressure and the rectoanal gradient were more variable among and within patients. Arguably, coaching patients prior to the maneuver may reduce the variability in these pressures (15). But, in doing so, the test may not approximate the patient’s evacuation process.
Similar to our findings, another study observed that the categorization of variables (i.e., normal vs abnormal) differed between HRM_1 and HRM_2 in 79% of 28 patients (8). That study also included patients with fecal incontinence and the average interval between the HR_ARMs was longer (i.e., mean of 32 months) longer than in our study. Taken together, these studies suggest that diagnostic circumspection may be prudent when interpreting anorectal manometry findings (2), especially when the values are at the borderline between normal and abnormal. In our study, while the intraindividual coefficient of variation for rectal pressure during evacuation in constipated patients was 61%, the categorization, as normal or abnormal, differed in only 9% of patients, probably because the normal value range for this variable is wide. In constipated patients, the desire to defecate threshold was more reproducible than the first sensation threshold perhaps because participants find it difficult to distinguish between the perception of an undistended rectal balloon and the first sensation threshold. Since the instructions to participants during HR_ARM are standardized, the extent to which these findings are explained by differences among operators is unclear (16). A prospective study designed to understand this and other factors that affect day-to-day reproducibility of HR-ARM is necessary.
Generally reproducible (17), the BET outcome differed between days 1 and 2 in only 11% of patients. Hence, one BET test is probably sufficient. The test need be repeated only in specific circumstances (e.g., if there is concern that patients misunderstood instructions during the first test). The BET was prolonged in 14% of asymptomatic healthy participants, and on both study days, which suggests that they had asymptomatic pelvic floor dysfunction (14). Moreover, the rectoanal gradient was lower, suggestive of pelvic floor dysfunction, in asymptomatic participants with a prolonged vs normal BET (14).
In 19 constipated patients (36%), the rectoanal gradient during defecation, which is the most useful HR_ARM variable for diagnosing DD (4), differed between HR_ARM1 and HR_ARM2. The consequence of this difference depends on (1) if only 1 criterion is required, which variable (ie, gradient or BET) is deemed more robust for diagnosing DD and (2) whether one or, as suggested by the Rome IV criteria, two abnormal tests are required to diagnose DD (18).
If one test is deemed sufficient and the BET is deemed more robust than the gradient (4), then the different gradients between HR_ARM1 and HR_ARM2 arguably have relatively modest consequences on the clinical diagnosis because the BET was either normal or abnormal on both study days in 17 of 19 patients who had a different gradient (ie, normal vs abnormal) between HR_ARM1 and HR_ARM2. (However, a recent study suggests that a reduced rectoanal gradient and a prolonged BET have comparable diagnostic utility vs defecography for diagnosing DD (19)).
On the other hand, if two abnormal tests (i.e., gradient and BET) are deemed necessary to diagnose DD, then the differences between HR_ARM1 and HR_ARM2 have a considerable impact because the overall diagnosis based on a combined assessment of the gradient and the BET differed between HR_ARM1 and HR_ARM2 in all 23 patients.
In conclusion, HR_ARM is a reproducible test. However, in 79% of constipated patients, the outcome (i.e., normal or abnormal) of one or more tests is different between the first and second studies.
KEY MESSAGES.
Anorectal pressures were measured with high-resolution manometry on two days in healthy persons and constipated patients.
Anal resting and squeeze pressures and the rectoanal gradient during evacuation were reproducible in healthy and constipated participants. Rectal sensory thresholds were also reproducible in constipated participants. However, in 79% of constipated patients the outcome for one or more variables was different on day 1 vs 2.
These findings suggest that HR_ARM is a reproducible test. However, repeated testing may reveal a different outcome, even absent an intervention between the first and second tests.
ACKNOWLEDGEMENTS, FUNDING, AND DISCLOSURES
Grant Support: This study was supported by US Public Health Service National Institutes of Health grant R01DK78924 to Dr. Bharucha.
Disclosures: Dr. Bharucha jointly holds patents for an anorectal catheter fixation device, anorectal manometry probe, and an anorectal device for fecal incontinence respectively with Medtronic Inc, Medspira Inc, and Minnesota Medical Technologies, receives royalties from Medspira Inc, and an honorarium from GI Supply Inc
ABBREVIATIONS
- BET
balloon expulsion time
- HR_ARM
High resolution anorectal manometry
- CCC
concordance correlation coefficient
- CI
confidence interval
- DD
defecatory disorders
- SD
standard deviation
REFERENCES
- 1.Bharucha AE, Lacy BE. Mechanisms, Evaluation, and Management of Chronic Constipation. Gastroenterology 2020; 158: 1232–1249.e1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carrington EV, Heinrich H, Knowles CH, et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil 2020; 32: e13679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wald A, Bharucha AE, Limketkai B, et al. ACG Clinical Guidelines: Management of Benign Anorectal Disorders. Am J Gastroenterol 2021; 116: 1987–2008. [DOI] [PubMed] [Google Scholar]
- 4.Bharucha AE, Basilisco G, Malcolm A, et al. Review of the indications, methods, and clinical utility of anorectal manometry and the rectal balloon expulsion test. Neurogastroenterol Motil 2022: e14335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gosling J, Plumb A, Taylor SA, Cohen R, Emmanuel AV. High-resolution anal manometry: Repeatability, validation, and comparison with conventional manometry. Neurogastroenterology & Motility 2019; 31: e13591. [DOI] [PubMed] [Google Scholar]
- 6.Coss-Adame E, Rao SS, Valestin J, Ali-Azamar A, Remes-Troche JM. Accuracy and Reproducibility of High-definition Anorectal Manometry and Pressure Topography Analyses in Healthy Subjects. Clinical Gastroenterology and Hepatology : the official clinical practice journal of the American Gastroenterological Association 2015; 13: 1143–1150 e1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chakraborty S, Feuerhak KJ, Zinsmeister AR, Bharucha AE. Reproducibility of high-definition (3D) manometry and its agreement with high-resolution (2D) manometry in women with fecal incontinence. Neurogastroenterol Motil 2017; 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Triadafilopoulos G, Clarke JO, Kamal A, Neshatian L. Intra-subject Variability in High Resolution Anorectal Manometry Using the London Classification: Diagnostic and Therapeutic Implications. Dig Dis Sci 2022; 22: 22. [DOI] [PubMed] [Google Scholar]
- 9.Chakraborty S, Feuerhak K, Muthyala A, Harmsen WS, Bailey KR, Bharucha AE. Effects of Alfuzosin, an alpha1-Adrenergic Antagonist, on Anal Pressures and Bowel Habits in Women With and Without Defecatory Disorders. Clin Gastroenterol Hepatol 2019; 17: 1138–1147, e1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma M, Muthyala A, Feuerhak K, Puthanmadhom Narayanan S, Bailey KR, Bharucha AE. Improving the Utility of High Resolution Manometry for the Diagnosis of Defecatory Disorders in Women with Chronic Constipation. Neurogastroenterol and Motility 2020. Jul 01; 32: e13910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srinivasan SG, Muthyala A, Sharma M, et al. Abdomino-anal Dyscoordination in Defecatory Disorders. Clinical Gastroenterology & Hepatology 2021; 08: 08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deb B, Sharma M, Fletcher JG, et al. Inadequate Rectal Pressure and Insufficient Relaxation and Abdominopelvic Coordination in Defecatory Disorders. Gastroenterology 2022; 162: 1111–1122.e1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oblizajek NR, Deb B, Kathavarayan Ramu S, et al. Optimizing techniques for measuring anal resting and squeeze pressures with high-resolution manometry. Neurogastroenterology & Motility 2022; n/a: e14383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oblizajek NR, Gandhi S, Sharma M, et al. Anorectal pressures measured with high-resolution manometry in healthy people—Normal values and asymptomatic pelvic floor dysfunction. Neurogastroenterology and Motility : the official journal of the European Gastrointestinal Motility Society 2019: e13597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heinrich H, Fruehauf H, Sauter M, et al. The effect of standard compared to enhanced instruction and verbal feedback on anorectal manometry measurements. Neurogastroenterology and Motility 2013; 25: e163. [DOI] [PubMed] [Google Scholar]
- 16.Prichard DO, Fetzer JR. Retrospective evaluation of operator bias in the performance of high-resolution anorectal manometry. Neurogastroenterology & Motility 2022: e14341. [DOI] [PubMed] [Google Scholar]
- 17.Chiarioni G, Kim SM, Vantini I, Whitehead WE. Validation of the Balloon Evacuation Test: Reproducibility and Agreement With Findings From Anorectal Manometry and Electromyography. Clinical Gastroenterology and Hepatology 2014; 12: 2049–2054. [DOI] [PubMed] [Google Scholar]
- 18.Rao S, Bharucha AE, Chiarioni G, et al. Functional anorectal disorders. Gastroenterology 2016; 150: 1430–1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blackett JW, Kathavarayan Ramu S, Gautam M, et al. Anorectal Manometry Predictors of Abnormal Balloon Expulsion Test and Reduced Evacuation on Defecography Gastroenterology 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]


