Abstract
Different restorative techniques have been proposed for the treatment of posterior teeth affected by cracked tooth syndrome (CTS). However, the literature is scarce in protocols of how to solve CTS using ceramic restorations made by computer aided design–computer aided manufacturing (CAD-CAM) system. CAD-CAM provides a fast and efficient restorative treatment usually in a single visit, reducing the risk of contamination and micro-infiltration of the cracked line. The objective of this work was to describe 3 clinical cases of cracked teeth, which presented vertical fracture lines in different directions and extension through the pulp, restored by CAD-CAM system, with 5-year follow-up. Patients with short-term spontaneous masticatory pain, cold sensibility and restored teeth without cuspal coverage were selected. Digital radiographs (DR) were taken to confirm the pulp and periapical status. Periodontal probing depth, sensitivity, percussion, and occlusion tests were performed. The fracture lines with their direction and extension were identified under dental optical microscope (DOM). The treatment plan was performed in two stages: immediate treatment to stabilize the tooth and minimize pain, and final restorative treatment by CAD-CAM system to stabilize the crack. Patients were between the ages of 37 and 45 years. Most of the studied teeth presented extensive restorations without cuspal coverage. The presence of occlusal interference, in lateral movement, was a constant finding. Endodontic treatment was performed in cases of irreversible pulpitis or pulpal necrosis. In all three cases, cavity preparation was performed for full coverage restorations, as the fracture lines extended in several directions, requiring a re-enforcement of the cervical region of the teeth in question. The survival rate of the reported cases was 100% with 5-year clinical and radiographic follow-up, suggesting that CAD-CAM system may be a promising alternative treatment in the management of CTS, improving tooth longevity.
Key Words: CAD-CAM, Cracked Teeth, Cracked Tooth Syndrome, Incomplete Fracture, Prognosis
Introduction
According to the classification of cracks described by the American Association of Endodontists, there are 5 types of cracks: graze lines, fractured cusp, cracked tooth, split tooth and vertical root fracture [1].
Cracked tooth syndrome (CTS) also known as incomplete fracture is defined as a flat fracture that breaks the continuity of the enamel and dentine usually mesiodistally but where the segments do not completely separate, being held together by a portion of the structure. This fracture as it represents unknown depth and direction can extend to the pulp. CTS correspond to an intermediate stage of fracture, which if not diagnosed early, may progress to a complete fracture [2, 3]. All reviews state that the main signs and symptoms for CTS are chewing pain, sensitivity to cold and sweet food [3-6]. These symptoms may vary according to the position and extent of each cracked line. Some patients can precisely specify the tooth from which the symptoms may be arising, while others cannot [3-6]. The etiology of CTS is multifactorial, being described as "excessive forces applied to a healthy tooth such as parafunctional habits or physiological forces applied to a weakened tooth such as teeth with inadequate restorations resulting in loss of integrity of the coronary structure" [7]. The teeth most affected by CTS are the lower molars, followed by the maxillary molars. CTS is less likely in the premolars; however, the literature is not unanimous about this finding. It usually affects those between 30 and 60 years of age [3, 4, 8-10].
CTS diagnosis remains a challenge since there are various signs and symptoms which can be often confused with other pathologies. The success of the treatment plan and prognosis is directly related to early diagnosis, that should include patient's history, clinical periodontal, occlusal, radiographic, trans-illumination, methylene blue dye examinations, sensitivity tests and use of “dental operating microscopy” (DOM) [11-15]. Both the diagnosis and the treatment of CTS will depend on the location, periodontal probing depth (PPD) and direction of the crack line [7, 16]. Shallower cracks are treated more easily with restorations and crowns with cusp protection; however, the deepest cracks with pulp involvement, should be treated with root canal treatment and restoration with cusp/total crown coverage [16, 17]. In cases where PPD of cracked teeth extended more than 4 mm, the dental element should be removed and replaced with an implant [15, 17]. Griffin, in an article reporting a clinical case of CTS, suggested the use of ceramic restorations made by computer aided design–computer aided manufacturing (CAD-CAM) system that can be performed in a single visit, and reduce the chances of bacterial invasion and micro-infiltration [17, 18].
In the last decades, great advances have been observed in ceramic restorative techniques and dentine adhesive systems, which allow faster restoration, and thus, reduce contamination and possible pulp complications, and thereby improve the longevity of the tooth [17, 19]. However, few studies describe the treatment of cracked teeth using CAD-CAM system, with long-term follow-ups [17, 19].
The objective of the current study was to demonstrate relevant results obtained in a series of three clinical cases of cracked teeth with vertical fracture lines in different directions and various extensions. It shows the importance of early diagnosis and appropriate methodology. The present study also highlighted the possibility of restoration of these cases using CAD-CAM system, which could provide fast and efficient restorative treatment, reduce the number of visits and consequently lower the risk of contamination, with clinical and radiographic follow-ups of 5 years.
Case Reports
Case 1:
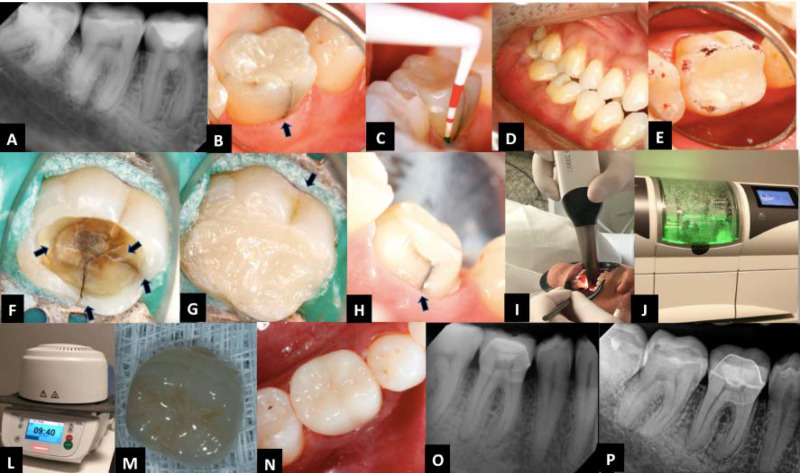
A 35-year-old man was clinically examined due to a complaint of pain when chewing hard food on the right side of the mouth and sensitivity whilst having cold drinks. He also claimed that he had a diet of constant consumption of oil seeds like nuts. Moreover, he showed symptoms of night clenching. Periapical radiographs to confirm the pulp and periapical status were taken. Presence of a deep restoration was observed (Figure 1A).
Figure 1.
Immediate treatment sequence: A) Initial digital radiography (DR) of tooth #46; B) Photo of the tooth, showing a vertical fracture line in the lingual surface of the tooth (BLUE ARROW); C) No periodontal probing depth was observed; D, E) Occlusal interferences in the working movements were investigated; F) Restoration in resin composite without cuspal coverage was removed, and several cracked lines in different directions under DOM (ARROWS) were identified; G) Temporary restoration in resin composite; H) Preparation of full crown of tooth #46; I) Intraoral CAD/CAM scanner; J) CEREC milling machine; L) The oven used for the preparation of the final restoration; M) Full crown in E-MAX; N) Definitive full crown restauration was placed; O) Periapical and bitewing radiography after 6 months; P) 5-year follow-up
Clinical examination showed the presence of a large composite resin restoration in tooth #46 without cuspal protection. A visible vertical fracture line, with lingual pigmentation, was also observed (Figure 1B). However, no abnormal probe depth was seen (Figure 1C). Pulp sensibility testing of the tooth was done with Endo-Ice (Frigi-Dent™ thermal pulp tester; Ellman International, Inc., Hicksville, NY, USA) and electronic pulp tester (EPT) (Digitest™ tooth vitality tester; Parkell, Inc., Edgewood, NY, USA), with exacerbation of pain to cold. Occlusal interference was identified in the lateral movement, in working motion on tooth #46 (Figure 1D, 1E).
Immediate treatment plan : Once the source of pain was identified, the patient was anaesthetised and restoration was removed. Under Dental operatory microscope (DOM), several cracked lines were identified in different directions; however, the crack did not involve the pulpal area (Figure 1F), which was confirmed by sensibility tests. Then, the cracked lines were cleaned with 2% chlorhexidine (Lenza Pharma, MG, Brazil) using ultrasonic tips (Helse, São Paulo, Brazil). The pulp cavity was protected with light-curing Ca(OH)2 (Ultradent, Indaiatuba, SP, Brazil). Then, the cavity was filled with Filtek Z 350 resin (3M ESPE, SP, Brazil) in small increments, covering the entire fracture line and protecting them from buccal fluids (Figure 1G). The tooth was left in infra-occlusion. All clinical findings on the prognosis, cost and especially need for long-term follow-up were explained to the patient and his consent was obtained.
Definitive treatment plan : After one week, the patient returned for the reassessment, reporting complete disappearance of his painful symptoms. All sensibility tests were positive. Then, the patient was anaesthetised, and full crown preparation was immediately performed to promote the cervical splint for the cracks in tooth 46 (Figure 1H). Tooth preparation was scanned by an intraoral scanner compatible with the CAD-CAM system, and the obtained data were sent to the software (Figure 1I).
A computerised milling machine printed the crown in an E-MAX block (Ivoclar Vivadent Ltda, SP, Brazil). The adaptation of the crown was verified. Immediately afterwards, it was make-up and taken to the oven (Figure 1J, 1K). The full crown was fixed using a dual cure cement Variolink II (Ivoclar Vivadent Ltda, SP, Brazil) (Figure 1L, 1M). The occlusal contact was re-established.
Initially, the patient was followed after 6 months to observe some clinical and radiographic changes (Figure 1N). In the absence of signs and symptoms, the follow-up became annual. Currently, digital radiograph (DR) with 5 years follow-up (Figure 1O) has been taken.
Case 2:
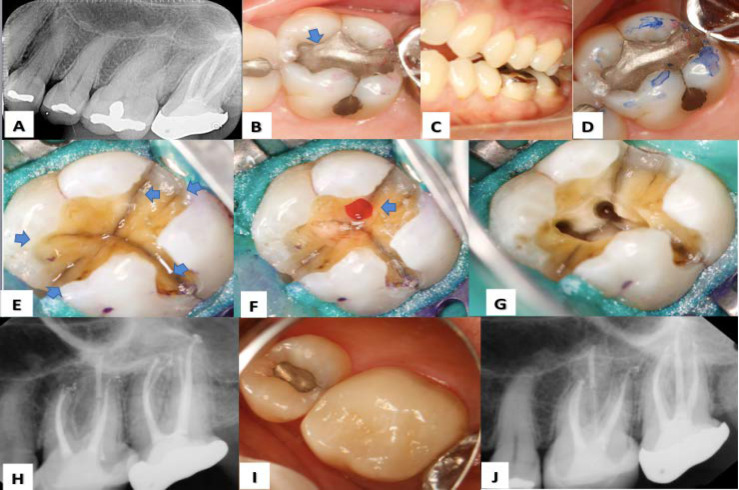
A 42-year-old female was clinically examined. She reported diffuse pain, which exacerbated with cold water and chewing, in the left region of maxilla. Radiographic examination showed no periapical pathology in any of the teeth (Figure 2A). However, tooth 26 responded to the cold and biting tests with prolonged pain and thus, irreversible pulpitis was considered as the diagnosis. Clinical examination revealed a class I dental amalgam restoration without cuspal coverage (Figure 2B). Furthermore, there were fracture lines visible to the naked eye, nevertheless without any abnormal periodontal probing. Occlusal evaluation exhibited lateral interferences during the working movement of the tooth 26 (Figure 2C, 2D).
Figure 2.
Treatment sequence: A) Diagnostic radiograph of tooth #26; B) Clinical evaluation; identifying the presence of a class I amalgam restoration (BLUE ARROW); C, D) Occlusion evaluation; showing occlusal interferences in the lateral movement; E) Identification of crack lines after the removal of amalgam (BLUE ARROWS); F) Small direct pulpal exposure (BLUE ARROW); G, H) Endodontic treatment and final restoration by CAD-CAM System; I, J) Clinical and radiographic follow-up at 5 years
Immediate treatment plan : After confirming the origin of the pain, the patient was anesthetised and restoration was removed under DOM. Cracked lines from mesial to distal, and palatine groove were identified. Several other microcracks were also observed (Figure 2E). A small pulpal exposure was seen (Figure 2F). Then, pulpectomy was performed for pain relief, and the depth and extension of the fracture lines were evaluated. The fracture lines did not extend inside the canals. Root canal treatment (RCT) was performed using Protaper Next System (Proglider, F1, F2 and F3; Dentsply-Maillefer, Ballaigues, Switzerland). The canals were dressed completely with Ca(OH)2 (Ultradent, SP, Brazil). Subsequently, a temporary restoration was placed on the tooth as case 1. The occlusion was checked and the tooth was left in infra-occlusion. The findings were presented and explained to the patient, and her consent was obtained.
Definitive treatment plan : The patient returned a week later, with complete remission of clinical symptoms. Ca(OH)2 (Ultradent, SP, Brazil) dressing was removed, and endodontic treatment was performed (Figure 2G, 2H). Then, a fiberglass pin (Angelus, SP, Brazil) was placed in the palatal root, and the pulp chamber was filled with Filtek Z 350 resin composite (3M ESPE, SP, Brazil). As the crack lines extended in several directions, a full coverage crown preparation was performed in an attempt to cover all fracture lines. The preparation was scanned as in the applied protocol in case 1. Once the full crown was obtained from CAD-CAM system, it was placed, and the occlusal contacts were re-established. The patient was followed every 6 months, and is currently completing 5 years of clinical and radiographic follow-up (Figure 2I, 2J).
Case 3:
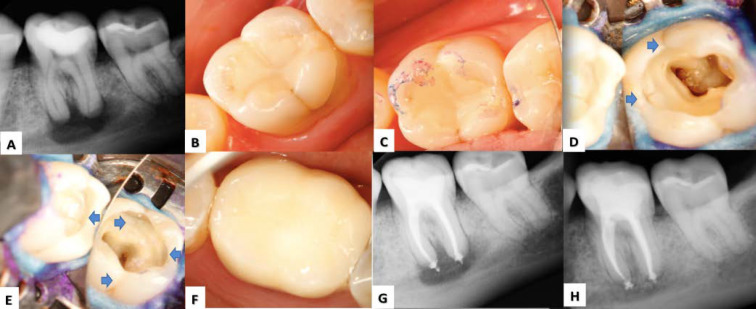
A 37-year-old female, with intermittent and exacerbated pain on tooth 36 when chewing, was referred for necessary consultation/treatment. Pulp necrosis was diagnosed. All sensibility tests were negative, and a large apical lesion was observed on the radiograph (Figure 3A). There was no periodontal probing depth. Clinical examinations showed presence of a composite class I restoration (Figure 3B) without cuspal coverage. Occlusal interference on tooth 36 was observed on the working side (Figure 3C).
Figure 3.
Treatment sequence: A) Initial radiograph of tooth #36; B) Class I resin composite restoration without cuspal coverage; C) Evaluation of occlusal interferences; D, E) Identification of fracture lines on the 4 walls (BLUE ARROWS); F) Scanning and preparation of the crown in E-MAX; the final restoration was placed; G) Digital radiography one-year follow-up; H) Digital radiography 5-year follow-up
Immediate treatment plan : The patient was anaesthetised and rubber dam was properly placed. Then, the resin restoration was immediately removed under DOM for thorough visual inspection so as to identify the position and extent of the cracks.
Isolated fracture lines were observed in the bucco-occlusal, disto-occlusal, mesio-occlusal and lingual directions, extending to the pulp chamber (Figure 3D, 3E). The endodontic access cavity was performed. Canals were prepared with Protaper Next system (Proglider, F1, F2 and F3; Dentsply-Maillefer, Ballaigues, Switzerland), followed by the application of Ca(OH)2 (Lenza Pharma, MG, Brazil) as the intracanal dressing. The tooth was restored with a Filtek Z 350 resin composite filling material (3M ESPE, SP, Brazil) and left in infra-occlusion in order to avoid any extra contact over the tooth.
Definitive treatment plan : In one week, clinical symptoms had disappeared. The intracanal dressing was then removed, and the radicular canals were hermetically sealed with thermo-plasticised gutta-percha. Once the treatment was finished, the pulp chamber was completely filled with Filtek Z 350 resin composite restorative material (3M ESPE, SP, Brazil). The cavity preparation option was a full crown since the crack lines were located in several directions, and had involved both marginal ridges. When preparing the tooth, it was attempted to remove as little of the dentine structure as possible to preserve the maximum
dental structure. The cavity preparation was scanned, and following the protocol of case 1, a total crown in E-MAX (Ivoclar Vivadent Ltda, SP, Brazil) prepared by CAD/CAM system was immediately installed (Figure 3F). The patient was initially monitored every 6 months. Radiographies were taken in the one-year follow-up appointment (Figure 3G). Currently, the patient has 5 years of clinical/radiographic follow-ups and has shown apical bone repair (Figure 3H).
Discussion
Teeth with cracks, which involve both marginal ridges, extend vertically through the pulp or involve subpulpal floor, have a poor prognosis. Generally, the treatment of cracked teeth owing to their unpredictable prognosis presents a restorative dilemma for dentists. To treat and restore teeth with CTS, the clinical decision involves a) negotiation on prognosis and cost with patients, and b) need for long-term follow-up [6, 15-18].
The causes of CTS are multifactorial. Abrupt changes in temperature, age of the patient, parafunctional habits such as bruxism (Case 1, 2 and 3), and consumption of hard food such as oil seeds (Case 2) tend to generate forces with high values [6, 9, 20]. In 1997, Diangelis studied two clinical cases where patients reported chewing pain and sensitivity to cold. The patients had pierced their tongue and created a habit of biting/playing with it between the posterior teeth, which had led to the development of cracked tooth syndrome [21].
Another factor which contributes to the occurrence and propagation of cracks is occlusal interferences, both in closing and centric/eccentric movements. In these circumstances, there are no incisal and canine guides, which could finally generate harmful eccentric forces [22-24]. Balancing-side interferences may also increase the possibility of fractures in a mesiodistal direction, especially in teeth with extensive restorations. However, excessive contacts on the working side might contribute to the fractures of nonfunctional cusps. Canine wear is a strong indication that posterior teeth are in eccentric contacts and is a significant indication of teeth predisposed to fracture [6, 25-27]. Clinical cases 1, 2 and 3 corroborate these findings.
In literature, there is a great divergence regarding the teeth affected by CTS/the age group. Some authors argue that mandibular molars are the most affected teeth, followed by the maxillary premolars, maxillary molars and mandibular premolars [3, 15]. Other authors believe that the lower second molars are the most affected, followed by the lower first molars [8, 28, 29]. Yang [15] argued that the lower first molars would be the most affected, followed by the upper first molars, the lower second molars and finally the upper second molars. In contrast, Seo [9] stated that the most affected tooth was the upper first molars, followed by the lower first molars, the lower second molars sequence and finally the upper second molars [9, 28]. The present article was in agreement with Yang’s findings (Cases 1 and 3). Moreover, literature states that the highest incidence of cracks occurs predominantly between the ages of 30 and 60. Several authors believe that this phenomenon could be explained by the common wear the teeth suffer with age, which adds to the loss of the dentine elasticity that occurs over the years, in addition to other factors such as deleterious habits [3, 10, 15, 28]. All the presented case reports in this study are in agreement with these findings.
The prognosis of a tooth affected by CTS is determined by a) the extent and location of the fracture, b) the time at which restorative intervention is initiated and c) the type of restoration applied to splint the fracture [5, 17]. Generally, when several lines of fracture are present, it is believed that the involved teeth are structurally weaker than those with a single fracture line. However, what will condemn a cracked tooth is the presence of a probing depth [15]. Therefore, teeth which introduce cracks without pulpal involvement (Case 1), present a more favourable prognosis [15, 27].
It is believed that fracture lines can be colonized by bacterial biofilms [15, 30, 31]. If the cracks result in pulpal involvement, an endodontic treatment will be necessary. In this study, Case 2 was diagnosed with irreversible pulpitis whilst Case 3 suffered from pulp necrosis with absence of caries.
Some authors suggest that cracked teeth, requiring endodontic treatment, will present a worse prognosis in long time [32, 33]. This is predictable since there is loss of internal structure, due to the need for direct access along the canal. However, Cases 1, 2 and 3 contradict such concept. Once the fracture line was splinted in the proper time and with the correct restoration, it obtained good clinical and radiographic results. Corroborating these findings, recent studies on minimally invasive endodontics have demonstrated that there is no difference amongst the cases where conventional access was made [34].
Therefore, if the assertive diagnosis is made and the correct treatment is implemented, the prognosis becomes favorable in long term, regardless of whether or not the tooth is treated endodontically [35].
According to Banerji, the management of CTS can be divided into a) immediate treatments (IMTR) and b) intermediate or definitive treatments (DFTR). IMTRs are performed in an emergency situation in order to stabilize the tooth and minimize the pain [17]. Some authors suggest use of orthodontic band, direct restoration with or without protection of the cusp and occlusal adjustments as IMTR options. Others use IMTRs as definitive treatments; due to their practicality and affordable cost [36, 37]. However, it is already known that IMTRs are not effective because they do not protect the cracked tooth from inter-occlusal pressure during chewing. Therefore, it is believed that the importance of performing a treatment with onlays, in which the cusps are covered, or the use of a full crown despite doubtful prognosis is indisputable [16, 17]. The preparation and placement of temporary crowns in acrylic resin or direct restoration with photo-activated composite resins with cusp coverage (Cases 1, 2, and 3) has been described as a predictable option of immediate splinting for CTS [33, 35]. IMTRs are considered a necessary step, but only for short time, so as to assess whether or not the symptoms will subside. IMTRs are used to stabilize the cracks and relieve symptoms of pain, preventing the propagation of the crack. Long-used temporary crowns as IMTR options have been questioned because they a) increases the risk of recontamination of the crack, b) may fracture, and c) leak or be displaced leading to pulp complications [17-19].
DFTRs include direct and indirect restorations with or without cuspal coverage, onlays and full crowns [13, 16]. In literature, there is evidence that the success rates of using adhesive restorations, to restore cracked teeth, can be improved by including cuspal coverage in the design of the restoration [17]. The use of full crowns is also an indicated procedure, as it offers resistance and distribution of the occlusal loads throughout the tooth axis, and stress reduction which could lead to the crack [20, 22, 36].
Crown onlays can be made in either metal or ceramics, and involve reducing the height of the cusps from 1.0 mm to 1.5 mm (metal)/2.0 mm (ceramic), and creating a circumferential shoulder or chamfer margin. Currently, this form of full-crown preparation is questioned since it could promote loss of dental tissues and pulp vitality [17]. However, the treatment plan is very diverse, and may vary according to the classification of the crack (Cases 1, 2 and 3) [17, 19]. The most important factor towards success in the restorative treatment of CTS is directly related to possible full-splint of cracked lines, so as to prevent its progression.
Currently, with advances in dentine adhesive technology as well as ceramic restorations, and preparations produced by CAD-CAM system such as CEREC (Sirona Dental Systems, Charlotte, North Carolina, USA) a faster approach is allowed. Such advancements have given the opportunity for the treatments to be performed in a single visit, which could avoid using temporary acrylic crowns. Furthermore, through these enhancements, favourable improvements like decreasing the chance of bacterial invasion, lowering cusp flexure caused by occlusal load stress during mastication, reducing the risk of pulp complications and improving the longevity of the tooth could be achievable [17, 18].
Conclusion
Regardless of the direction and extension through the pulp, early diagnosis of CTS should be the priority of treatment, aiming to stabilize and protect the affected tooth. The definitive treatment plan would depend on the location and depth of the fracture lines. In the present study, the cavity preparations were performed with full coverage restorations by CAD-CAM system. Occlusal interferences were presented in almost all cases. The survival rate of cases 1, 2, and 3 was 100% over a 5-year follow-up. However, there is still much to be investigated on the subject and clinical studies of more cases are needed, which may have constituted a limitation for this study.
Acknowledgment
This study was supported by grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico-CNPq, Fundacão de Amparo à Pesquisa do Estado de Minas Gerais-FAPEMIG.
Conflict of Interest:
‘None declared’.
References
- 1.Rivera E, Walton R. Cracking the cracked tooth code: detection and treatment of various longitudinal tooth fractures. Am Assoc Endodontists Colleagues for Excellence News Lett. 2008:2:1–19. [Google Scholar]
- 2.Abou-Rass M. Crack lines: the precursors of tooth fractures - their diagnosis and treatment. Quintessence Int Dent Dig. 1983;14(4):437–47. [PubMed] [Google Scholar]
- 3.Ellis SG, Macfarlane TV, McCord JF. Influence of patient age on the nature of tooth fracture. J Prosthet Dent. 1999;82(2):226–30. doi: 10.1016/s0022-3913(99)70161-7. [DOI] [PubMed] [Google Scholar]
- 4.Cameron CE. CRACKED-TOOTH SYNDROME. J Am Dent Assoc. 1964;68:405–11. doi: 10.14219/jada.archive.1964.0108. [DOI] [PubMed] [Google Scholar]
- 5.Kahler W. The cracked tooth conundrum: terminology, classification, diagnosis, and management. Am J Dent. 2008;21(5):275–82. [PubMed] [Google Scholar]
- 6.Banerji S, Mehta SB, Millar BJ. Cracked tooth syndrome Part 1: aetiology and diagnosis. Br Dent J. 2010;208(10):459–63. doi: 10.1038/sj.bdj.2010.449. [DOI] [PubMed] [Google Scholar]
- 7.Geurtsen W. The cracked-tooth syndrome: clinical features and case reports. International Journal of Periodontics & Restorative Dentistry. 1992;12(5) [PubMed] [Google Scholar]
- 8.Lynch CD, McConnell RJ. The cracked tooth syndrome. J Can Dent Assoc. 2002;68(8):470–5. [PubMed] [Google Scholar]
- 9.Seo DG, Yi YA, Shin SJ, Park JW. Analysis of factors associated with cracked teeth. J Endod. 2012;38(3):288–92. doi: 10.1016/j.joen.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 10.Kim SY, Kim SH, Cho SB, Lee GO, Yang SE. Different treatment protocols for different pulpal and periapical diagnoses of 72 cracked teeth. J Endod. 2013;39(4):449–52. doi: 10.1016/j.joen.2012.11.052. [DOI] [PubMed] [Google Scholar]
- 11.Clark DJ, Sheets CG, Paquette JM. Definitive diagnosis of early enamel and dentin cracks based on microscopic evaluation. J Esthet Restor Dent. 2003;15(7):391–401. doi: 10.1111/j.1708-8240.2003.tb00963.x. discussion . [DOI] [PubMed] [Google Scholar]
- 12.de Toubes KMS, de Oliveira PAD, Machado SN, Pelosi V, Nunes E, Silveira FF. Clinical Approach to Pulp Canal Obliteration: A Case Series. Iran Endod J. 2017;12(4):527–33. doi: 10.22037/iej.v12i4.18006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang SH, Kim BS, Kim Y. Cracked Teeth: Distribution, Characteristics, and Survival after Root Canal Treatment. J Endod. 2016;42(4):557–62. doi: 10.1016/j.joen.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 14.de Toubes KM, Cortes MI, Valadares MA, Fonseca LC, Nunes E, Silveira FF. Comparative analysis of accessory mesial canal identification in mandibular first molars by using four different diagnostic methods. J Endod. 2012;38(4):436–41. doi: 10.1016/j.joen.2011.12.035. [DOI] [PubMed] [Google Scholar]
- 15.Yang SE, Jo AR, Lee HJ, Kim SY. Analysis of the characteristics of cracked teeth and evaluation of pulp status according to periodontal probing depth. BMC Oral Health. 2017;17(1):135. doi: 10.1186/s12903-017-0434-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mamoun JS, Napoletano D. Cracked tooth diagnosis and treatment: An alternative paradigm. Eur J Dent. 2015;9(2):293–303. doi: 10.4103/1305-7456.156840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Banerji S, Mehta SB, Millar BJ. Cracked tooth syndrome Part 2: restorative options for the management of cracked tooth syndrome. Br Dent J. 2010;208(11):503–14. doi: 10.1038/sj.bdj.2010.496. [DOI] [PubMed] [Google Scholar]
- 18.Griffin JD, Jr Efficient, conservative treatment of symptomatic cracked teeth. Compend Contin Educ Dent. 2006;27(2):93–102; quiz 3, 12. [PubMed] [Google Scholar]
- 19.Opdam NJ, Roeters JJ, Loomans BA, Bronkhorst EM. Seven-year clinical evaluation of painful cracked teeth restored with a direct composite restoration. J Endod. 2008;34(7):808–11. doi: 10.1016/j.joen.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 20.Udoye CI, Jafarzadeh H. Cracked tooth syndrome: characteristics and distribution among adults in a Nigerian teaching hospital. J Endod. 2009;35(3):334–6. doi: 10.1016/j.joen.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 21.DiAngelis AJ. The lingual barbell: a new etiology for the cracked-tooth syndrome. J Am Dent Assoc. 1997;128(10):1438–9. doi: 10.14219/jada.archive.1997.0065. [DOI] [PubMed] [Google Scholar]
- 22.Geurtsen W, Schwarze T, Gunay H. Diagnosis, therapy, and prevention of the cracked tooth syndrome. Quintessence Int. 2003;34(6):409–17. [PubMed] [Google Scholar]
- 23.Moule AJ, Kahler B. Diagnosis and management of teeth with vertical root fractures. Aust Dent J. 1999;44(2):75–87. doi: 10.1111/j.1834-7819.1999.tb00205.x. [DOI] [PubMed] [Google Scholar]
- 24.Qian Y, Zhou X, Yang J. Correlation between cuspal inclination and tooth cracked syndrome: a three‐dimensional reconstruction measurement and finite element analysis. Dental Traumatology. 2013;29(3):226–33. doi: 10.1111/j.1600-9657.2012.01160.x. [DOI] [PubMed] [Google Scholar]
- 25.Swepston JH, Miller AW. The incompletely fractured tooth. J Prosthet Dent. 1986;55(4):413–6. doi: 10.1016/0022-3913(86)90165-4. [DOI] [PubMed] [Google Scholar]
- 26.Trushkowsky R. Restoration of a cracked tooth with a bonded amalgam. Quintessence Int. 1991;22(5):397–400. [PubMed] [Google Scholar]
- 27.Ratcliff S, Becker IM, Quinn L. Type and incidence of cracks in posterior teeth. J Prosthet Dent. 2001;86(2):168–72. doi: 10.1067/mpr.2001.116578. [DOI] [PubMed] [Google Scholar]
- 28.Hasan S, Singh K, Salati N. Cracked tooth syndrome: Overview of literature. Int J Appl Basic Med Res. 2015;5(3):164–8. doi: 10.4103/2229-516X.165376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krell KV, Caplan DJ. 12-month Success of Cracked Teeth Treated with Orthograde Root Canal Treatment. J Endod. 2018;44(4):543–8. doi: 10.1016/j.joen.2017.12.025. [DOI] [PubMed] [Google Scholar]
- 30.Berman LH, Kuttler S. Fracture necrosis: diagnosis, prognosis assessment, and treatment recommendations. J Endod. 2010;36(3):442–6. doi: 10.1016/j.joen.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 31.Ricucci D, Siqueira JF Jr, Loghin S, Berman LH. The cracked tooth: histopathologic and histobacteriologic aspects. J Endod. 2015;41(3):343–52. doi: 10.1016/j.joen.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 32.Tan L, Chen NN, Poon CY, Wong HB. Survival of root filled cracked teeth in a tertiary institution. Int Endod J. 2006;39(11):886–9. doi: 10.1111/j.1365-2591.2006.01165.x. [DOI] [PubMed] [Google Scholar]
- 33.Tang W, Wu Y, Smales RJ. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010;36(4):609–17. doi: 10.1016/j.joen.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 34.Sabeti M, Kazem M, Dianat O, Bahrololumi N, Beglou A, Rahimipour K, Dehnavi F. Impact of Access Cavity Design and Root Canal Taper on Fracture Resistance of Endodontically Treated Teeth: An Ex Vivo Investigation. J Endod. 2018;44(9):1402–6. doi: 10.1016/j.joen.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 35.Corsentino G, Pedulla E, Castelli L, Liguori M, Spicciarelli V, Martignoni M, Ferrari M, Grandini S. Influence of Access Cavity Preparation and Remaining Tooth Substance on Fracture Strength of Endodontically Treated Teeth. J Endod. 2018;44(9):1416–21. doi: 10.1016/j.joen.2018.05.012. [DOI] [PubMed] [Google Scholar]
- 36.Agar JR, Weller RN. Occlusal adjustment for initial treatment and prevention of the cracked tooth syndrome. J Prosthet Dent. 1988;60(2):145–7. doi: 10.1016/0022-3913(88)90303-4. [DOI] [PubMed] [Google Scholar]
- 37.Opdam NJ, Roeters JM. The effectiveness of bonded composite restorations in the treatment of painful, cracked teeth: six-month clinical evaluation. Oper Dent. 2003;28(4):327–33. [PubMed] [Google Scholar]