Abstract
Background:
Orthopedic treatment of flexed-knee gait consists of hamstring lengthening along with surgery at other levels. Transfer of the semitendinosus (hamstring transfer) was introduced to avoid increase of anterior pelvic tilt as well as reduce risk of recurrence.
Methods:
We retrospectively assessed children with spastic cerebral palsy and flexed-knee gait pre-operatively, 1 year post-operatively, and at a minimum of 7 years post-operatively.
Results:
The 39 patients were a mean 9.4 ± 3.4 years at the time of surgery, 20 subjects underwent hamstring transfer, and 19 subjects had hamstring lengthening with mean follow-up 9.1 years. Passive range of motion improved initially, but regressed at long term. Dynamic minimum knee flexion in stance decreased in both groups at the first post-operative study, and was maintained at final follow-up in 64-67% of patients. There was a small increase in anterior pelvic tilt at the 1-year follow-up which subsequently decreased to less than pre-operative in the hamstring lengthening group but remained mildly increased (5°) in the hamstring transfer group at final follow-up. Success in correcting stance knee flexion of the entire group was 69% of the Gross Motor Function Classification System grades I and II and 60% of the Gross Motor Function Classification System grade III subjects. Gait profile Score and sagittal knee Gait Variable Score both showed clinically important improvement after surgery and was mostly maintained long term for both groups. Lateral hamstring lengthening was beneficial in more severe patients, with minimal risk of adverse effects.
Conclusion:
Hamstring surgery as part of single event multi-level surgery (SEMLS) is effective in correcting flexed-knee gait in 60%–70% of patients with minimal effect on anterior pelvic tilt. There was no added advantage to hamstring transfer. Biceps Femoris lengthening may be beneficial and without significant additional risk.
Level of evidence:
level III.
Keywords: Spastic diplegia, cerebral palsy, hamstring lengthening, semitendinosus transfer, biceps femoris lengthening
Background
One of the most common gait abnormalities in children with cerebral palsy (CP) is excessive knee flexion during the stance phase of gait. 1 Dysphasic hamstring activity during mid-stance, a time where the hamstrings are inactive during normal gait, may be the most common initial cause of flexed-knee gait, and, along with other factors, contributes to the persistence and progression of flexed-knee gait. Walking in excessive knee flexion requires increased energy, places increased pressure on the knee articular surfaces, and is cosmetically unappealing. Gait deviations in the lower extremity joints can be observed visually and quantitated during walking with three-dimensional computerized motion analysis.
Treatments for excessive knee flexion may include physiotherapy, orthotics, injection of botulinum toxin into the hamstring muscle bellies, or surgery to the hamstring tendons,2–9 as well as distal femoral anterior hemiepiphysiodesis or distal femoral extension and shortening osteotomy, and frequently is associated with surgery at the adjacent joints that may contribute to the dynamic deformity. Tendon surgery involves lengthening or release of the hamstring tendons, thereby allowing these taut muscles, which have been overpowering their antagonists, to assume a shorter resting length which will weaken them as well as reduce the spasticity therein.2–8 Although hamstring surgery has been the standard for many decades and has been shown to improve knee extension in the short term, long-term studies, particularly in patients who have reached skeletal maturity, are limited.
In addition to flexing the knee, some of the hamstring muscles also contribute to hip extension, so there has been a concern that this important function will also be weakened when the hamstring tendons are elongated, leading to hip extensor weakness and increased anterior pelvic tilt. In order to minimize this consequence, Ma et al. 5 introduced the semitendinosus transfer to eliminate the semitendinosus as a knee flexor but preserve its hip extension function and reduce risk of recurrence by transferring the distal attachment of the semitendinosus above the knee. We have reported that significant correction of excessive knee flexion in gait may be gained with both hamstring lengthening (HSL) and hamstring transfer (HST) at the 1- and 4.4-year follow-up.6 ,10 Although this is useful information, it will be more beneficial to have a longer-term follow-up to determine if the corrections were maintained past skeletal maturity. The purposes of this study are to assess the long-term (7–14 years) outcomes of lengthening of the medial hamstrings with or without biceps femoris lengthening (HSL) and compare this to lengthening of the semimembranosus plus transfer of the semitendinosus and gracilis to a site proximal to the knee joint (HST), as well to assess the risks and benefits of the addition of lengthening of the biceps femoris.
Materials and methods
A retrospective review was conducted on all patients who had initial gait studies performed between April 1993 and November 2019 prior to having either HSL or HST in our institution, and at least a 1-year post-operative study. All surgical patients in our institution were offered pre-op as well as routine follow-up studies at no cost to them. In general, HSL was performed prior to 2004, while HST, including gracilis to reduce risk of recurrence, was introduced in 2004 and became the standard procedure by most surgeons at our hospital, based on the theoretical benefits of this modification. Surgical technique and post-operative management were similar to our previous studies.
Subjects were excluded from this study if they had selective dorsal rhizotomy or significant extrapyramidal involvement, and most had concomitant lower extremity surgeries as part of a single event multi-level surgery (SEMLS) approach, or had undergone prior surgery.
Thirty-nine children (29 males and 10 females) with bilateral spastic CP underwent a pre-operative gait study (pre-op), a follow-up study approximately 1 year post-operative (post-op), and a long-term study at a minimum of 7 years post-operative (long-term). Long-term studies were either done routinely as part of ongoing care (29 subjects) or collected from subjects meeting the qualifying timeline who were invited to return, with compensation for travel expenses (10 subjects). Shriners/Western Institutional Review Board (WIRB) approved the project POR1904, and all subjects returning at our request signed informed consent.
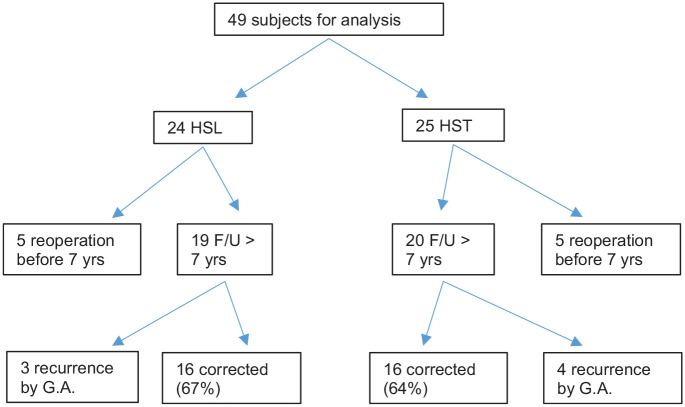
Subjects in failure rate analysis only
In addition to the 39 subjects with long-term studies, there were 10 subjects (5 in HST & HSL) who had pre-operative studies and 1 year post-operative studies, but then had recurrence of flexed-knee gait, and underwent subsequent femoral extension osteotomy or hamstring revision surgery. These 10 subjects were excluded from the comparison of HST versus HSL and evaluation of biceps femoris lengthening, but were included in the overall failure analysis of hamstring surgery. Figure 1 shows the subject selection flow chart.
Figure 1.
Subject selection flow chart.
Data collection
Data collection included age, gender, and Gross Motor Function Classification System (GMFCS) level, age at surgery, physical exam, and three-dimensional (3D) computerized gait analysis. Methods used for physical examination, 3D gait analysis, surgical techniques, and rehabilitation and orthotic protocols were as previously reported.6 ,10 Operative notes from all surgeries were analyzed.
Statistical analysis
All statistical analyses of the data were done only for the right leg unless only the left leg had hamstring surgery (in patients with asymmetric diplegia) to meet the statistical requirement for independence. 11
Two-way mixed analysis of variance (ANOVA) was used to detect differences between the HSL and HST groups. There were two independent variables: (1) the between subject variable was surgery, which had two levels (HSL or HST) and (2) the within subject variable was time (pre-op, post-op, and long-term). The dependent variables were the physical examination and kinematic measures.
For each group (HSL or HST), a one-way repeated measures ANOVA was used to detect differences in the range of movement (ROM) or kinematics variables repeatedly measured in the same subjects at pre-op, post-op, and long-term. The independent variable was time (pre-op, post-op, and long-term). The dependent variables were the ROM and kinematics variables. The significace levels were set at 0.05.
The gait profile score (GPS) 12 and gait variable score (GVS) 12 were calculated for each subject, and minimal clinical important difference (MCID) 13 was used to determine whether there was a clinically significant difference. The MCID for the GPS score is 1.6°, which is the mean difference between adjacent levels of the Gillette Functional Assessment Questionnaire (FAQ) walking scale. 13 We also calculated the sagittal knee GVS from the GPS.12,14 The MCID for sagittal knee GVS is 3.4°.12,14
Results
In the initial survey, we found 39 subjects with pre-op and 1 year post-op studies, of whom 29 had 7 years, or longer, follow-up study (long-term). An additional 10 patients who had not had a 7-year follow-up were recruited for a final study making a total of 39 patients. A total of 28 subjects had biceps femoris fractional lengthening in addition to the medial hamstring surgery due to patient indications and surgeon preference.
Comparison of HSL and HST
The 39 children included for the comparison of HST to HSL, ranged in age from 4 to 19 years old (mean = 9.4 ± 3.4 years) at the time of surgery, and from 18 to 28 years (mean = 18.4 ± 3.6 years) at final follow-up. There were 20 subjects in the HST group and 19 subjects in the HSL group. The average long-term follow-up from pre-op to final assessment was 9.1 ± 1.9 years for the HSL group and 9.3 ± 2.2 years for the HST group. A detailed description of the subjects is shown in Table 1.
Table 1.
Subject characteristics.
| HSL | HST | |
|---|---|---|
| (n = 19) | (n = 20) | |
| Gender | ||
| Male | 16 | 13 |
| Female | 3 | 7 |
| Age at surgery (years) | 9.4 ± 3.8 | 9.4 ± 3.0 |
| First follow-up time from surgery (years) | 1.2 ± 0.3 | 1.3 ± 0.5 |
| Long-term follow-up time from surgery (years) | 9.1 ± 1.9 | 9.3 ± 2.2 |
| GMFCS level | ||
| I | 6 | 4 |
| II | 6 | 10 |
| III | 7 | 6 |
HSL: hamstring lengthening; HST: hamstring transfer; GMFCS: Gross Motor Function Classification System.
There were 9 subjects at GMFCS level I (23.1%), 15 subjects at level II (38.5%), and 15 subjects at level III (38.5%). Most subjects had concomitant multilevel surgical interventions (Table 2), and five had prior adductor lengthening and three had prior iliopsoas lengthening.
Table 2.
Concomitant surgeries.
| Concomitant procedure | Number |
|---|---|
| Rectus femoris transfer/transposition | 12 |
| Adductor lengthening | 11 |
| Gastroc lengthening (Strayer) | 3 |
| Psoas lengthening | 7 |
| Achilles tendon lengthening | 2 |
| Derotational osteotomy of the femur | 3 |
| Posterior tibialis lengthening | 1 |
| Subtalar fusion | 4 |
| Derotational osteotomy of the tibia | 4 |
| Total number of concomitant procedures | 47 |
| Total number of patients with concomitant procedures | 31 |
The results of the two-way mixed ANOVA which compares HSL to HST (Table 3 and Figure 2) showed that the only outcome difference between HSL and HST was anterior pelvic tilt, which was increased slightly over baseline by 5° at long term in HST, and was unchanged in HSL.
Table 3.
Results of the two-way mixed ANOVA.
| Test of within-subjects effects | Pairwise comparisons of time with Bonferroni’s adjustment | ||||||
|---|---|---|---|---|---|---|---|
| Time × surgery | Time | ||||||
| F(2,74) | Significance | F(2,74) | Significance | Pre-op vs Post-op | Pre-op vs long-term | Post-op vs long-term | |
| Physical exam | |||||||
| Knee extension | 0.09 | 0.913 | 17.9 | <0.001 | <0.001 | 0.003 | 0.199 |
| Straight leg raise | 1.14 | 0.325 | 14.4 | <0.001 | 0.004 | 0.199 | <0.001 |
| Popliteal angle | 1.84 | 0.167 | 20.7 | <0.001 | <0.001 | 1.000 | <0.001 |
| Dorsiflexion with knee flexed | 1.92 | 0.153 | 3.53 | 0.034 | 0.026 | 1.000 | 0.125 |
| Dorsiflexion with knee extended | 0.41 | 0.667 | 1.75 | 0.181 | 0.458 | 1.000 | 0.132 |
| Kinematics | |||||||
| Average pelvic tilt | 5.12 | 0.008 | 15.4 | <0.001 | <0.001 | 0.219 | 0.005 |
| Minimum hip flexion in stance | 2.68 | 0.075 | 0.421 | 0.658 | 1.000 | 1.000 | 1.000 |
| Minimum knee flexion in stance | 0.26 | 0.769 | 43.5 | <0.001 | <0.001 | <0.001 | 0.03 |
| Peak dorsiflexion in stance | 1.85 | 0.165 | 0.51 | 0.602 | 1.000 | 1.000 | 1.000 |
ANOVA: analysis of variance; pre-op: pre-operative; post-op: 1 year post-operative; long-term: long-term study at a minimum of 7 years post-operative.
The between subject variable is surgery (HSL or HST); the within subject variable is time (pre-op, post-op, and long-term). The dependent variables are the ROM and kinematics variables. Significant level is set at 0.05.
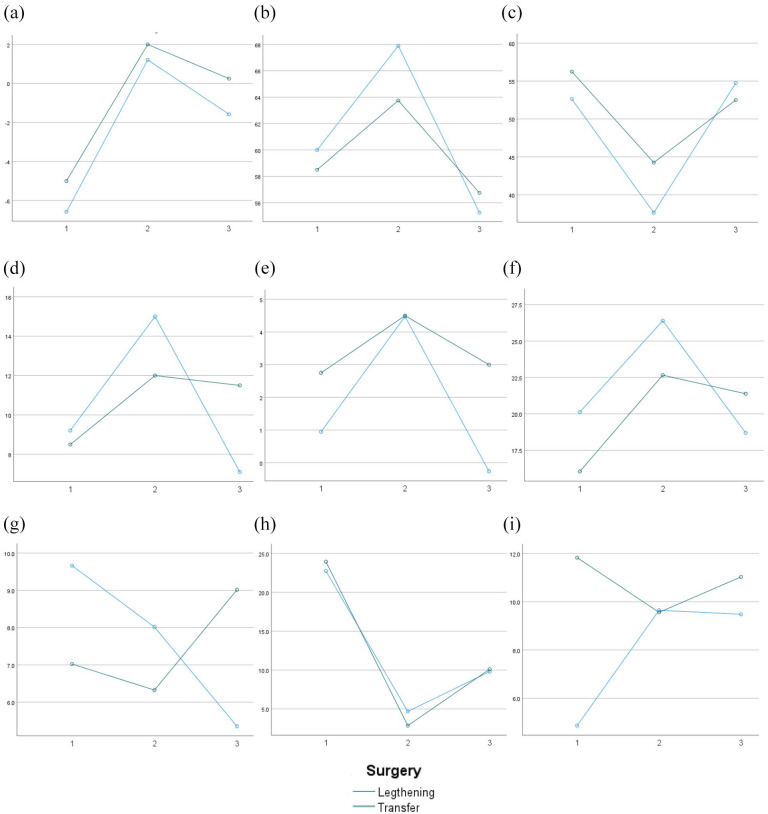
Figure 2.
Profile plots for the ROM and kinematics variables repeatedly measured for the HSL group (blue) and HST group (green). The horizontal axis is time (1. pre-op, 2. post-op, and 3. long-term). The vertical axis is estimated marginal means (unit: degree): (a) knee extension, (b) straight leg raise, (c) popliteal angle, (d) dorsiflexion with knee flexed, (e) dorsiflexion with knee extended, (f) pelvic tilt, (g) minimum hip flexion, (h) minimum knee flexion, and (i) peak dorsiflexion.
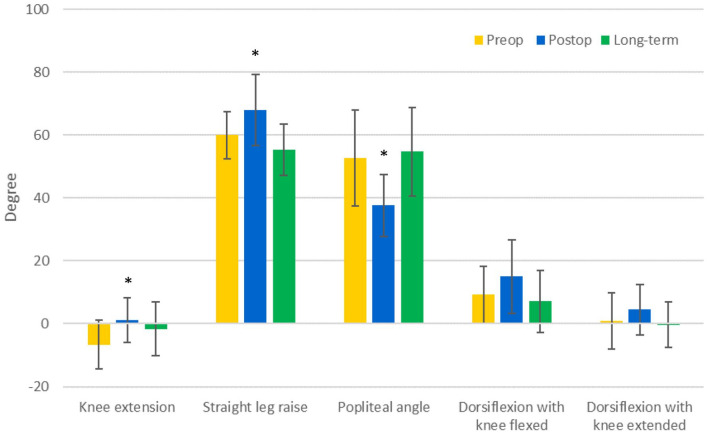
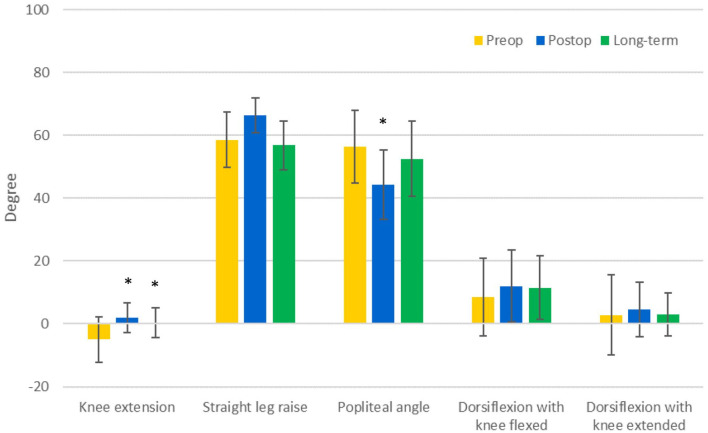
The results of one-way repeated measures ANOVA for each group are seen in Tables 4 and 5 and Figures 3–6. Passive knee extension was improved at post-op in both groups and at long-term only for the HST group, and final absolute contracture was small (<2°) for both groups. Straight leg raise and popliteal angle showed initial improvement at 1 year but returned close to pre-op values at the final follow-up for both groups. Static exam of dorsiflexion was unchanged for all conditions at both time points.
Table 4.
Results of repeated measures ANOVA for the HSL group.
| Mean ± standard deviation | Test of within-subjects effects | Pairwise comparisons with Bonferroni’s adjustment | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Long-term | F(2,36) | Significance | Pre-op vs post-op | Pre-op vs long-term | Post-op vs long-term | |
| Physical exam | ||||||||
| Knee extension | −6.6 ± 7.8 | 1.2 ± 7.2 | −1.6 ± 8.5 | 7.3 | 0.002 | 0.002 | 0.144 | 0.560 |
| Straight leg raise | 60.0 ± 7.5 | 67.9 ± 11.3 | 55.3 ± 8.2 | 14.5 | <0.001 | 0.013 | 0.113 | <0.001 |
| Popliteal angle | 52.6 ± 15.2 | 37.6 ± 9.9 | 54.7 ± 14.0 | 13.7 | <0.001 | <0.001 | 1.000 | <0.001 |
| Dorsiflexion with knee flexed | 9.2 ± 9.0 | 15.0 ± 11.7 | 7.1 ± 9.8 | 4.1 | 0.026 | 0.085 | 1.000 | 0.065 |
| Dorsiflexion with knee extended | 0.9 ± 8.9 | 4.5 ± 8.0 | −0.3 ± 7.2 | 2.3 | 0.119 | 0.226 | 1.000 | 0.230 |
| Kinematics | ||||||||
| Average pelvic tilt | 20.1 ± 7.1 | 26.4 ± 6.7 | 18.7 ± 3.8 | 10.6 | <0.001 | 0.008 | 1.000 | 0.003 |
| Minimum hip flexion in stance | 9.7 ± 8.5 | 8.0 ± 9.4 | 5.4 ± 7.0 | 1.8 | 0.178 | 1.000 | 0.210 | 0.519 |
| Minimum knee flexion in stance | 22.7 ± 10.7 | 4.7 ± 10.8 | 9.8 ± 10.6 | 19.8 | <0.001 | <0.001 | <0.001 | 0.374 |
| Peak dorsiflexion in stance | 4.9 ± 14.4 | 9.6 ± 7.7 | 9.5 ± 8.2 | 1.6 | 0.223 | 0.416 | 0.674 | 0.416 |
ANOVA: analysis of variance; HSL: hamstring lengthening; pre-op: pre-operative; post-op: 1 year post-operative; long-term: long-term study at a minimum of 7 years post-operative.
The within-subjects variable is time (pre-op, post-op, and long-term). The dependent variables are the ROM and kinematics variables (units: degree).
The significant level is set at 0.05.
Table 5.
Results of repeated measures ANOVA for the HST group.
| Mean ± standard deviation | Test of within-subjects effects | Pairwise comparisons with Bonferroni’s adjustment | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Long-term | F(2,36) | Significance | Pre-op vs post-op | Pre-op vs long-term | Post-op vs long-term | |
| Physical exam | ||||||||
| Knee extension | −5.0 ± 7.3 | 2.0 ± 4.7 | 0.3 ± 4.7 | 11.8 | <0.001 | <0.001 | 0.014 | 0.604 |
| Straight leg raise | 58.5 ± 8.8 | 66.3 ± 5.5 | 56.8 ± 7.7 | 3.3 | 0.050 | 0.269 | 1.000 | 0.086 |
| Popliteal angle | 56.3 ± 11.5 | 44.3 ± 11.0 | 52.5 ± 12.0 | 7.9 | 0.001 | 0.005 | 0.644 | 0.045 |
| Dorsiflexion with knee flexed | 8.5 ± 12.3 | 12.0 ± 11.4 | 11.5 ± 10.1 | 1.1 | 0.355 | 0.446 | 0.958 | 1.000 |
| Dorsiflexion with knee extended | 2.8 ± 12.7 | 4.5 ± 8.7 | 3.0 ± 6.8 | 0.2 | 0.786 | 1.000 | 1.000 | 1.000 |
| Kinematics | ||||||||
| Average pelvic tilt | 16.0 ± 5.7 | 22.7 ± 5.7 | 21.4 ± 7.9 | 9.7 | <0.001 | <0.001 | 0.004 | 1.000 |
| Minimum hip flexion in stance | 7.0 ± 8.0 | 6.3 ± 11.1 | 9.0 ± 8.6 | 1.1 | 0.336 | 1.000 | 0.898 | 0.617 |
| Minimum knee flexion in stance | 23.9 ± 12.4 | 2.9 ± 9.7 | 10.1 ± 10.2 | 23.9 | <0.001 | <0.001 | 0.001 | 0.113 |
| Peak dorsiflexion in stance | 11.8 ± 12.3 | 9.6 ± 6.4 | 11.0 ± 7.1 | 0.5 | 0.622 | 1.000 | 1.000 | 1.000 |
ANOVA: analysis of variance; HSL: hamstring lengthening; pre-op: pre-operative; post-op: 1 year post-operative; long-term: long-term study at a minimum of 7 years post-operative.
The within-subjects variable is time (pre-op, post-op, and long-term). The dependent variables are the ROM and kinematic variables (units: degree). The significant level is set at 0.05.
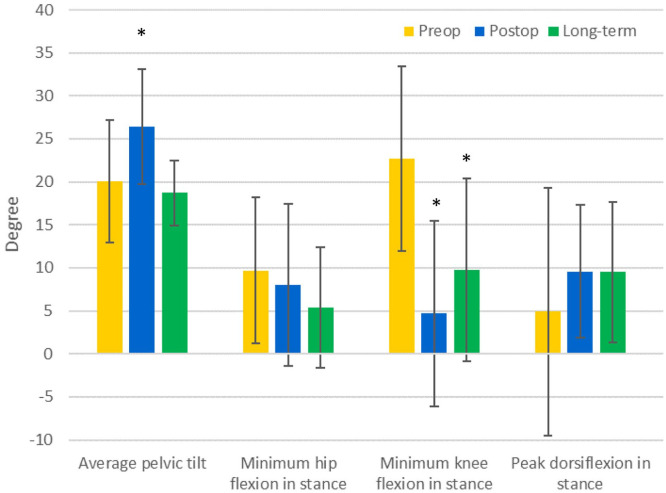
Figure 3.
Pre-op, 1 year post-op, and long-term follow-up range of motion measurements for the HSL group.
*Indicates p < 0.05 compared with the pre-op values (repeated measures ANOVA, pairwise comparisons with Bonferroni’s adjustment).
Figure 4.
Pre-op, 1-year post-op, and long-term follow-up range of motion measurements for the HST group.
*Indicates p < 0.05 compared with the pre-op values (repeated measures ANOVA, pairwise comparisons with Bonferroni’s adjustment).
Figure 5.
Pre-op, 1 year post-op, and long-term follow-up kinematics measurements for the HSL group.
*Indicates p < 0.05 compared with the pre-op values (repeated measures ANOVA, pairwise comparisons with Bonferroni’s adjustment).
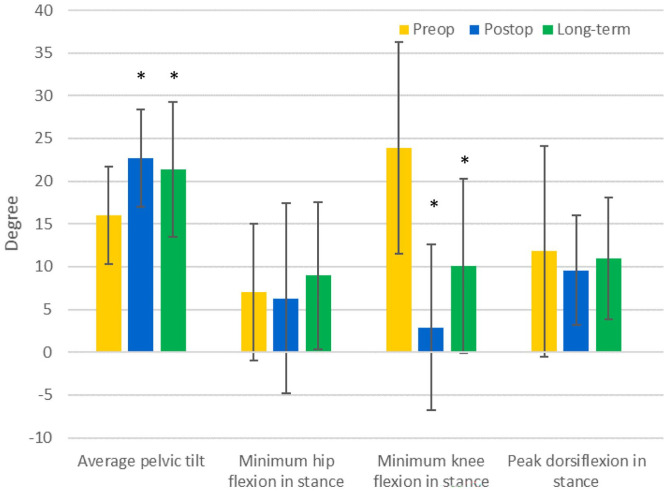
Figure 6.
Pre-op, 1 year post-op, and long-term follow-up kinematics measurements for the HST group.
*Indicates p < 0.05 compared with the pre-op values (repeated measures ANOVA, pairwise comparisons with Bonferroni’s adjustment).
As far as kinematics (Tables 4 and 5 and Figures 3–6), anterior pelvic tilt increased by about 6° in both groups at 1 year post-op, but subsequently decreased to less than pre-operative in the HSL group but remained mildly increased (by 5°) in the HST group at final follow-up. Minimum hip flexion (indicating no deficit in hip extension) and peak dorsiflexion in stance did not show statistically significant change after surgery for both groups.
Most importantly, mean dynamic minimum knee flexion in stance decreased significantly in both groups at the first post-operative study, and this was maintained at final follow-up (Tables 4 and 5 and Figures 3–6). Ten of the 39 subjects had knee recurvatum at 1 year post-op, but only 2 of the 10 still had recurvatum (−2.2° and −8.2°) at long-term follow-up.
GPS and sagittal knee GVS both showed clinically important improvement after surgery and was mostly maintained long term for both groups (Table 6). The change in GPS after surgery correlates with one level increase on the FAQ and was maintained long term for both groups (Table 6).
Table 6.
Pre-operative (pre-op), 1 year post-operative (post-op), and long-term follow-up (long-term) measurements (unit: degree) for the HSL and the HST groups.
| HSL (n = 19) | HST (n = 20) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Change | Long-term | Change | Pre-op | Post-op | Change | Long-term | Change | |
| GPS | 16.5 | 14.1 | 2.4 | 12.0 | 4.5 | 13.9 | 11.0 | 2.9 | 11.8 | 2.0 |
| Sagittal knee GVS | 22.5 | 14.2 | 8.3 | 13.2 | 9.3 | 22.6 | 13.1 | 9.5 | 14.6 | 8.0 |
HSL: hamstring lengthening; HST: transfer of the semitendinosus; GPS: gait profile score; GVS: gait variable score; pre-op: pre-operative; post-op: 1 year post-operative; long-term: long-term study at a minimum of 7 years post-operative.
Changes compared with pre-operative values are presented. The minimal clinical important difference for GPS and GVS are 1.6° and 3.4°, respectively.
Overall outcome of hamstring surgery
In addition to the 39 subjects who were analyzed to compare HSL with HST, there were five HSL subjects and five HST subjects who had been excluded from this analysis because they had either hamstring revision surgery or distal femoral extension osteotomy (DFEO) before a 7-year period. These subjects were included along with the others for analysis of overall outcome of hamstring surgery and had a mean popliteal angle of 53.5° ± 10.6° and an average minimum knee flexion of 27.6° ± 9.5° in stance before their second hamstring surgery or subsequent DFEO surgery. None of these subjects had Achilles tendon lengthening (Zone 3), and only two subjects had lengthening in Zone 1 or 2. In addition to these failures who underwent repeat knee surgery, three HSL subjects and four HST subjects had increased knee flexion in mid-stance at the long-term study compared to pre-operative values (Table 7). These patients had a mean knee flexion of 10.5° pre-op, which increased to 16.4° at final follow-up. This was not due to excessive second rocker dorsiflexion (i.e. crouch) since the failures do not show a statically significant increase of second rocker at their final study (p = 0.30) (Table 7). These 17 subjects (10 with revision surgery at the knee before long-term follow-up and 7 with higher dynamic knee extension values than pre-op values) were classified as failures. Thus, in the total group of 49 patients who underwent hamstring surgery, there were 32/49 (65.3%) subjects who had successful outcomes, and 17/49 (34.6%) subjects who were failures. The success rate by GMFCS levels were 9/13 (69.2%) of the GMFCS I subjects, 11/16 (68.8%) of the GMFCS II subjects, and 12/20 (60.0%) of the GMFCS III subjects.
Table 7.
Results of repeated measures ANOVA for the seven subjects who had increased knee flexion in stance at long-term follow-up from pre-operative values.
| Mean ± standard deviation | Test of within-subjects effects | Pairwise comparisons with Bonferroni’s adjustment | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Long-term | F(2,10) | Significance | Pre-op vs post-op | Pre-op vs long-term | Post-op vs long-term | |
| Physical exam | ||||||||
| Knee extension | −2.1 ± 6.4 | 2.9 ± 4.9 | −3.5 ± 9.0 | 2.2 | 0.163 | 0.098 | 1.000 | 0.392 |
| Straight leg raise | 59.3 ± 8.9 | 67.1 ± 4.9 | 48.6 ± 6.9 | 14.7 | 0.001 | 0.124 | 0.212 | 0.002 |
| Popliteal angle | 52.9 ± 11.5 | 39.3 ± 11.3 | 66.4 ± 16.0 | 11.9 | 0.002 | 0.262 | 0.053 | 0.020 |
| Dorsiflexion with knee flexed | 10.0 ± 13.5 | 7.9 ± 18.5 | 8.6 ± 13.1 | 0.15 | 0.863 | 1.000 | 1.000 | 1.000 |
| Dorsiflexion with knee extended | 2.9 ± 7.0 | 1.4 ± 12.8 | −2.1 ± 8.1 | 1.5 | 0.271 | 1.000 | 0.677 | 0.473 |
| Kinematics | ||||||||
| Average pelvic tilt | 18.6 ± 8.5 | 28.1 ± 8.3 | 19.4 ± 5.9 | 5.6 | 0.023 | 0.039 | 1.000 | 0.082 |
| Minimum hip flexion in stance | 1.7 ± 6.9 | 4.1 ± 7.9 | 9.8 ± 6.2 | 4.7 | 0.035 | 1.000 | 0.107 | 0.207 |
| Minimum knee flexion in stance | 10.5 ± 6.8 | −5.9 ± 8.8 | 16.4 ± 9.1 | 18.3 | <0.001 | 0.031 | 0.019 | 0.020 |
| Peak dorsiflexion in stance | 1.8 ± 14.8 | 7.2 ± 9.7 | 4.7 ± 9.5 | 0.6 | 0.571 | 1.000 | 1.000 | 1.000 |
pre-op: pre-operative; post-op: 1 year post-operative; long-term: long-term study at a minimum of 7 years post-operative.
The within-subjects variable is time (pre-op, post-op, and long-term). The dependent variables are the ROM and kinematic variables (units: degree).
The significant level is set at 0.05.
We also assessed the role of the addition of biceps femoris intramuscular lengthening to the medial hamstring surgery, and since the outcomes of the HSL and HST groups were similar regarding correction of dynamic knee flexion, we grouped them together for this analysis. There were 11 patients who had medial hamstring surgery only (M), and 28 patients who had M plus lateral hamstring intramuscular lengthening (M + L). At final follow-up, correction of knee flexion contracture and popliteal angle were slightly greater in the M + L group, while dynamic maximum hip extension was better in the M + L after being more limited in the pre-op study. Pelvic tilt was similar to the pre-op level in both groups (increased by only 2.8° over baseline in the M + L group), and of greatest interest, the M group had 39% correction of stance knee flexion as compared to 62% correction in the M + L group. With regard to dynamic stance knee hyperextension, we found in the 1-year study, there were six patients with knee extension >5° in the M + L, and three in the M group, but all resolved except one in the M + L group of 8.2° at the final follow-up.
Discussion
Hamstring tightness or over-activity in ambulatory children with spastic diplegic CP is probably the initiating factor in the development of flexed-knee gait, particularly in children with competent calf muscle function, although other factors such as decreased hip extension and decreased ground reaction force at the ankle (leading to crouch) are likely contributors to the perpetuation and increase of knee flexion over time. Lengthening of the hamstrings is widely considered to be the standard surgical procedure for the correction of increased knee flexion, along with orthotics, and surgery at other joints as part of an SEMLS approach,2–5,7,15 Mid-term surgical outcomes of 3–5 years post-surgery have shown that the majority of children with CP benefit from hamstring lengthening or transfer surgeries.16,17 However, there are only a limited number of studies assessing the long-term outcome of hamstring surgeries, and the results are mixed.18,19 This study addressed the following three main outcome parameters as:
The overall success of hamstring surgery in spastic diplegia.
The role of hamstring lengthening alone as compared to the addition of semitendinosus and gracilis transfer proximal to the knee joint along with hamstring lengthening.
The effect of including the biceps femoris in the lengthening procedure.
In terms of the first issue, the overall efficacy of hamstring surgery, this study of 49 original subjects, showed improvement in passive and dynamic measures at the sagittal plane knee at 1 year post-op, and most importantly, improvement in dynamic knee extension in stance, which was maintained in 60%–70% of patients over a long-term follow-up period (7–15 years), although there was return to baseline of many of the passive measures. The findings are consistent with the study published by Õunpuu et al. 18 and Morais Filho et al. 20 who reported slight decrease in dynamic knee extension at the long-term follow-up compared to values measured at 1 year post-op, but they felt this could be due to natural progression of gait in children with CP which has been shown to decline over time.
It should be noted that our patient group had relatively small mean knee flexion contracture pre-operatively of 7° ± 8° but mean dynamic knee flexion in gait of 23° ± 12° prior to surgery. Thus, we did not wait for more severe knee flexion contracture to develop to do corrective surgery, as did other groups reporting their outcomes,19,21 but intervened early to treat the dynamic deformity. We think an important concept in the treatment of children with spastic diplegia is that we should treat dynamic deformities when they manifest and not wait for contractures to develop and worsen over time.
We found that in 69.2% of GMFCS I and 68.8% of GMFCS II the dynamic gains in stance knee flexion found at the 1 year post-op study were sustained at the longer-term follow-up, while only 60% of GMFCS III maintained the improvements found at year post-op at the long-term follow-up study. This indicates that GMFCS III patients are at higher risk of recurrence over time.
The regression in popliteal angle and straight leg raise at the final follow-up, following initial improvement at 1 year, is consistent with what others have previously reported.18,20 The disparity between passive range of motion and dynamic knee kinematics at the long-term follow-up showed that passive range of knee extension and popliteal angle do not directly correlate with dynamic function in the older and heavier patients.
Dreher et al. 19 found a decline in dynamic knee extension in stance in many patients at long-term follow-up which differed from the finding of Õunpuu et al. 18 and the findings of this study. The subjects in the study by Dreher et al. 19 had considerably more concomitant surgery than the subjects in this study, which may suggest the subjects in their study were more severely involved, which may explain the difference.
Regarding the second major issue, the comparison of HSL with HST, we found no advantage of the more complex and time-consuming approach of HST in comparison to the simpler HSL. This study showed similar improvement of knee extension in stance for both the HST and HSL groups and no difference between groups at either post-operative interval, similar to what has been reported at 4.4 years. 11 This is the first study evaluating HST surgery at long-term follow-up (7–15 years), and the improvements in HST are similar to HSL. A major concern regarding HSL has been that it was erroneously thought to result in an increase in anterior pelvic tilt, and one of the theoretical advantages of HST was prevention of this by retention of the semitendinosus as a hip extensor. Although there was an initial increase in anterior pelvic tilt in both HSL and HST patients, despite many of them having lateral as well as medial hamstrings lengthening, there was a decrease in anterior pelvic tilt of 1.4° to below pre-op levels at the final follow-up in the HSL group, while the HST group showed a 5° increase over the pre-op levels at final follow-up. Whether this 5° increase is clinically significant is unknown. Wijesekera et al. 22 similarly found no change in pelvic tilt following HSL except in GMFCS III patients; however, this study did not stratify anterior pelvic tilt changes by GMFCS levels. In a recent study by Bell et al., 21 they showed patients who underwent HST exhibited more improvement of passive knee extension as well as dynamic knee extension in gait than those who underwent HSL; however, HST was not effective in preventing the increase of anterior pelvic tilt.
The change found in GPS at 1 year post-op and long-term follow-up shows that there was improvement this measure at 1 year post-op, and it was maintained at long-term follow-up for both groups. These findings are similar to the findings of a mid-term outcome study published by Thomason et al. 16 As far as we are aware, there has been no long-term study examining GPS of subjects with primary hamstring surgery.
There are little data, but much opinion, published on the outcomes of adding biceps femoris lengthening in combination with lengthening of the medial hamstrings.23,24 Excessive knee extension in mid-stance (recurvatum) has been shown to be a complication following hamstring surgery, 25 and there is concern that lengthening of the biceps femoris may contribute to this, as well as increasing anterior pelvic tilt. We cannot draw solid conclusions from our data, since the groups were somewhat dissimilar due to the surgeons choosing to address the lateral hamstrings in more severe cases, so that the M + L group had more severe involvement at baseline. We found that the addition of biceps lengthening added no clinically significant increase in adverse outcomes including no significant change in anterior pelvic tilt, no loss of hip extension in early stance, and a greater proportional improvement in stance knee flexion of 62% in M + L versus 39% of those who had medial lengthening only. Regarding the risk of genu recurvatum, there was only one patient who developed a recurvatum of >5° in the M + L group (8.2°). Thus, we feel that consideration should be given to adding intramuscular lengthening of the biceps femoris for patients with more severe involvement, and further study of this issue is warranted.
Since all patients in our institution undergoing surgery for dynamic gait abnormalities have pre-operative studies, and are invited for routine follow-up studies at 1 year post operative, this minimizes selection bias. Furthermore, this study protocol included patients invited to return for the long-term follow-up who had not received this study as part of their routine clinical follow-up, so fewer subjects were lost compared to other retrospective studies; thus, this also minimized bias in subject selection. However, there are still some limitations with this study. Some subjects who were called to be in the study declined to participate in the long-term follow-up, but only one family reported that their child was no longer ambulatory.
Long-term outcomes in the pediatric population are important because continued growth and weight gain associated with puberty may lessen the effect of initial benefits of pre-pubescent surgery. This study helps pediatric orthopedic surgeons choose between HSL and HST as well as other interventions to treat flexed-knee gait in patients with CP by presenting a longer follow-up assessment of gait for both hamstring surgical interventions. Although both were effective, there was no distinct advantage of HST, which is a more time-consuming and complex procedure as compared with traditional HSL. In addition, at the long-term study, anterior pelvic tilt returned to below pre-op values following HSL, while it remained increased in the HST group. Furthermore, biceps femoris lengthening led to improved correction of more severely involved subjects, with minimal increase in risk.
As an alternative to hamstring surgery, some surgeons now advocate DFEO with or without patellar tendon advancement as the primary procedure for treatment of flexed-knee gait, 26 although Erdal et al. 27 have shown that, while effective, this procedure is more complex and may lead to an increase in pelvic tilt, especially when patellar tendon advancement is included, and also has a risk of neurological injury. 28 Another approach for the skeletally immature patient is anterior distal femoral hemiepiphysiodesis with or without patellar tendon shortening for which positive short-term outcomes have been reported, but this procedure does not address hamstring spasticity, and is only recommended for those with moderate knee flexion contracture. 29
Our findings show that both HSL and HST result in a high degree of long-term control of flexed-knee gait. Attention must be paid to adjacent joint dysfunction which will contribute to dynamic increased stance phase knee flexion, such as decreased hip extension in late stance due to excessive hip flexor activity or contracture which can be treated by iliopsoas lengthening or release, as well as at the ankle, where over-lengthening of the triceps surae may lead to development of a crouch pattern. We have avoided Achilles lengthening and thereby avoided crouch gait by maintaining the plantar flexion-knee extension couple in our patient population, thus supporting other data showing the importance of avoiding this procedure in spastic diplegic patients. 29 We found no major long-term problems with knee recurvatum, as has also been demonstrated by Vuillermin et al. 29 At our institution, we emphasized the importance of post-op rehabilitation in our patients following hamstring surgery, with attention to controlling the foot and ankle in either well-molded below knee casts or ankle foot orthoses (AFOs) to maintain a proper shank-floor angle both in the post-operative period, as well as long-term use of AFOs, as needed.
Conclusion
These findings may have an impact on future surgical decision-making in pediatric spastic diplegic CP patients, and lead to more satisfactory long-term outcomes. The long-term findings of this study demonstrate that HSL surgery is an important part of the surgical treatment program to treat dynamic knee flexion and improve gait for children with spastic diplegia. The fact that we did not wait for knee flexion contracture to develop but treated dynamic deformity before contractures could develop, likely contributed to the successful outcome at a mean of 9.2 years following surgery. Recurrence rates in this study population increased as GMFCS level increased with the correction being maintained in 70% of the GMFCS I and II patients, and 60% of GMFCS III patients. Furthermore, we found no advantage of HST over the simpler HSL, and surprisingly, we found better control of anterior pelvic tilt with HSL than with HST; therefore, we see no advantage of HST over HSL. We also found that addition of biceps femoris lengthening in selected patients can provide increased correction with little risk of knee recurvatum.
Acknowledgments
The authors thank Susan Sienko, Director of Clinical Research, Shriner Children’s Portland, for her helpful comments on all aspects of this paper and suggestions regarding the statistical analysis.
Footnotes
Author contributions: P.D. involved in data design, acquisition, interpretation, and all aspects of manuscript preparation. J.F. involved in data design, interpretation, and all aspects of manuscript preparation. M.D.S. involved in data design, interpretation, and all aspects of manuscript preparation.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M.D.S. is a member of the Editorial Board of the Journal of Pediatric Orthopaedics and the Journal of Childrens’ Orthopaedics. Otherwise, there are no conflicting interests.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported, in part, by funding from the St. Giles Foundation Arthur H. Huene award to Michael Sussman, 2000, through the POSNA.
Informed consent: Patient consent was obtained for those patients who returned for studies at our request and was waived for those in retrospective review only.
Institutional review board/ethics committee approval: The study was in compliance with Helsinki Declaration, and approved by Shriners/WIRB (POR1904).
References
- 1. Rodda J, Graham HK. Classification of gait patterns in spastic hemiplegia and spastic diplegia: a basis for a management algorithm. Eur J Neurol 2001; 8(Suppl. 5): 98–108. [DOI] [PubMed] [Google Scholar]
- 2. Baumann JU, Ruetsch H, Schürmann K. Distal hamstring lengthening in cerebral palsy: an evaluation by gait analysis. Int Orthop 1980; 3(4): 305–309. [DOI] [PubMed] [Google Scholar]
- 3. Westwell M, DeLuca P, Ounpuu S. Effect of repeat hamstring lengthenings in individuals with cerebral palsy. Dev Med Child Neurol 2004; 46(Suppl. 99): 14–15. [Google Scholar]
- 4. Thometz J, Simon S, Rosenthal R. The effect on gait on lengthening of the medial hamstrings in cerebral palsy. J Bone Joint Surg 1989; 71(3): 345–353. [PubMed] [Google Scholar]
- 5. Ma FY, Selber P, Nattrass GR, et al. Lengthening and transfer of hamstrings for a flexion deformity of the knee in children with bilateral cerebral palsy: technique and preliminary results. J Bone Joint Surg Br 2006; 88(2): 248–254. [DOI] [PubMed] [Google Scholar]
- 6. Feng L, Patrick Do, Aiona M, et al. Comparison of hamstring lengthening with hamstring lengthening plus transfer for the treatment of flexed knee gait in ambulatory patients with cerebral palsy. J Child Orthop 2012; 6(3): 229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Carney BT, Oeffinger D, Meo AM. Sagittal knee kinematics after hamstring lengthening. J Pediatr Orthop B 2006; 15: 348–350. [DOI] [PubMed] [Google Scholar]
- 8. Vlachou M, Pierce R, Davis RM, et al. Does tendon lengthening surgery affect muscle tone in children with cerebral palsy? Acta Orthop Belg 2009; 75(6): 808–814. [PubMed] [Google Scholar]
- 9. Kim SK, Rha DW, Park ES. Botulinum toxin type A injections impact hamstring muscles and gait parameters in children with flexed knee gait. Toxins 2020; 12: 145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. De Mattos C, Do KP, Pierce R, et al. Comparison of hamstring transfer with hamstring lengthening in ambulatory children with cerebral palsy: further follow-up. J Child Orthop 2014; 8: 513–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Menz HB. Analysis of paired data in physical therapy research: time to stop double dipping? J Orthop Sports Phys Ther 2005; 35(8): 477–478. [DOI] [PubMed] [Google Scholar]
- 12. Baker R, McGinley J, Schwartz M, et al. The gait profile score and movement analysis profile. Gait Posture 2009; 30: 265–269. [DOI] [PubMed] [Google Scholar]
- 13. Baker R, McGinley J, Schwartz M, et al. The minimal clinically important difference for the Gait Profile Score. Gait Posture 2012; 35: 612–615. [DOI] [PubMed] [Google Scholar]
- 14. Ries AJ, Novacheck TF, Schwartz MH. The efficacy of ankle-foot orthoses on improving the gait of children with diplegic cerebral palsy: a multiple outcome analysis. PM R 2015; 7(9): 922–929. [DOI] [PubMed] [Google Scholar]
- 15. Galey SA, Lerner ZF, Bulea TC, et al. Effectiveness of surgical and non-surgical management of crouch gait in cerebral palsy: a systematic review. Gait Posture 2017; 54: 93–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Thomason P, Baker R, Dodd K, et al. Single-event multilevel surgery in children with spastic diplegia. J Bone Joint Surg Am 2011; 93: 451–460. [DOI] [PubMed] [Google Scholar]
- 17. Salami F, Brosa J, van Drongelen S, et al. Long-term muscle changes after hamstring lengthening in children with bilateral cerebral palsy. Dev Med Child Neurol 2019; 61: 791–797. [DOI] [PubMed] [Google Scholar]
- 18. Õunpuu S, Solomito M, Bell K, et al. Long-term outcomes after multilevel surgery including rectus femoris, hamstring and gastrocnemius procedures in children with cerebral palsy. Gait Posture 2015; 42(3): 365–372. [DOI] [PubMed] [Google Scholar]
- 19. Dreher T, Vegvari D, Wolf SI, et al. Development of knee function after hamstring lengthening as a part of multilevel surgery in children with spastic diplegia: a long-term outcome study. J Bone Joint Surg Am 2012; 94(2): 121–130. [DOI] [PubMed] [Google Scholar]
- 20. Morais Filho MC, Blumetti FC, Kawamura CM, et al. Comparison of the results of primary versus repeat hamstring surgical lengthening in cerebral palsy. J Pediatr Orthop 2020; 40(5): e380–e384. [DOI] [PubMed] [Google Scholar]
- 21. Bell KJ, Õunpuu S, DeLuca PA, et al. Natural progression of gait in children with cerebral palsy. J Pediatr Orthop 2002; 22(5): 677–682. [PubMed] [Google Scholar]
- 22. Wijesekera MPC, Wilson NC, Trinca D, et al. Pelvic tilt changes after hamstring lengthening in children with cerebral palsy. J Pediatr Orthop 2019; 39: e380–e385. [DOI] [PubMed] [Google Scholar]
- 23. Kay RM, McCarthy J, Narayanan U, et al. Finding consensus for hamstring surgery in ambulatory children with cerebral palsy using the Delphi method. J Child Orthop 2022; 16(1): 55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sutherland DH, Schottstaedt ER, Larsen LJ, et al. Clinical and electromyographic study of seven spastic children with internal rotation gait. J Bone Joint Surg Am 1969; 51(6): 1070–1082. [PubMed] [Google Scholar]
- 25. Boyer ER, Stout J, Laine J, et al. Long-term outcomes after distal femoral extension osteotomy and patellar tendon advancement in young adults with cerebral palsy. J Bone Joint Surg 2018; 100: 31–41. [DOI] [PubMed] [Google Scholar]
- 26. Klotz MCM, Hirsch K, Heitzmann D, et al. Distal femoral extension and shortening osteotomy as a part of multilevel surgery in children with cerebral palsy. World J Pediatr 2017; 13(4): 353–359. [DOI] [PubMed] [Google Scholar]
- 27. Erdal OA, Gorgun B, Sarikaya IA, et al. Intraoperative neuromonitoring during distal femoral extension osteotomy in children with cerebral palsy. J Pediatr Orthop B 2022; 31(2): 194–201. [DOI] [PubMed] [Google Scholar]
- 28. Rethlefsen SA, Hanson AM, Wren T, et al. Anterior distal femoral hemiepiphysiodesis with and without patellar tendon shortening for fixed knee flexion contractures in children with cerebral palsy. J Child Orthop 2020; 14: 415–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vuillermin C, Rodda J, Rutz E, et al. Severe crouch gait in spastic diplegia can be prevented: a population-based study. J Bone Joint Surg Br 2011; 93(12): 1670–1675. [DOI] [PubMed] [Google Scholar]