Abstract
Objectives:
To evaluate the available literature for postoperative fracture rates following implant removal in the pediatric population.
Methods:
A systematic review of articles in the PubMed and Embase computerized literature databases from January 2000 to June 2022 was performed using PRISMA guidelines. Randomized controlled trials, case-control studies, cohort studies (retrospective and prospective), and case series involving pediatric patients that included data on fracture rate following removal of orthopedic implants were eligible for review. Two authors independently extracted data from selected studies for predefined data fields for implant type, anatomic location of the implant, indication for implantation, fracture or refracture rate following implant removal, mean time to implant removal, and mean follow-up time.
Results:
Fifteen studies were included for qualitative synthesis. Reported fracture rates following implant removal vary based on several factors, with an overall reported incidence of 0%–14.9%. The available literature did not offer sufficient data for conduction of a meta-analysis.
Conclusion:
Our systematic review demonstrates that fracture following implant removal in pediatric patients is a relatively frequent complication. In children, the forearm and femur are the most commonly reported sites of fracture following removal of implants. Traumatic fractures treated definitively with external fixation have the highest reported aggregate rate of refracture. Knowledge of the incidence of this risk is important for orthopedic surgeons. There remains a need for well-designed studies and trials to further clarify the roles of the variables that contribute to this complication.
Keywords: Implant removal, fracture, refracture
Introduction
Pediatric orthopedic patients are treated with numerous implant types for fracture reduction or other indications, such as congenital musculoskeletal anomalies. Previous studies have estimated that 5%–6% of all orthopedic procedures are an implant removal (IR),1,2 and the estimated percentage of IR-only procedures is even higher among pediatric orthopedic surgeons at 6.2%–6.7%. 3 While practices may differ from surgeon to surgeon, many routinely preemptively plan for IR in certain patients. Implants are often removed from pediatric patients after a certain period of time to allow for continued growth of the skeleton.4–7 However, other indications for removal can include pain at the implant site, infection, implant migration, and allergies to the implant material.8–11 All-epiphyseal screws are frequently removed as their retention can lead to increased pressure on the articular cartilage surface. 12 Implants can also be removed to prevent long-term stress shielding of the bone and the consequences that arise from bone remodeling, mainly peri-implant fractures.13–15
As with any procedure, IR is associated with postoperative risks. While the risks may be low for these relatively routine procedures, the inherent risks of all surgeries (bleeding, infection, damage to surrounding structures, etc.) are still present. A unique consideration for IR is the risk of fracture at the implant site after removal. Recently, aggregate data for all orthopedic patient populations have been published on the complications of IR. 3 However, postoperative complications and fracture rates following orthopedic IR in the pediatric population are not well-defined. The purpose of this manuscript is to systematically review the current literature involving the postoperative fracture rates in the pediatric population following IR.
Materials and methods
Study selection
Our study follows the initial criteria of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P). 16 To identify relevant published manuscripts related to fractures following IR in pediatric patients, we conducted comprehensive searches using the PubMed and Embase search engine databases from 1 January 2000 to 24 June 2022. The initial search utilized the following Boolean operators: (hardware removal) AND (children); (hardware removal) AND (pediatric); (hardware removal) AND (children) AND (refracture); (hardware removal) AND (pediatric) AND (refracture).
Records identified through the searches were added to an Endnote X9 database and duplicates were removed. Two reviewers screened and reviewed the titles/abstracts for further selection by using the following inclusion criteria: (1) the article must be focused on procedures that are within the standard practice of orthopedic surgeons, (2) the article must assess outcomes following IR, and (3) the article must contain data for patients < 18 years of age.
When assessing full-text articles, the following exclusion criteria was then applied: (1) articles where initial implants were placed prior to 2000 were excluded to account for modern implant designs and protocols, (2) articles that defined fractures as periprosthetic fractures or implant breakages that occurred prior to IR, (3) articles where post-IR outcome measures were aggregated between both pediatric patients and patients > 18 years of age, and (4) case reports. After the exclusion process, 15 studies were left for in-depth review regarding fractures or refractures following IR in pediatric patients.
Results
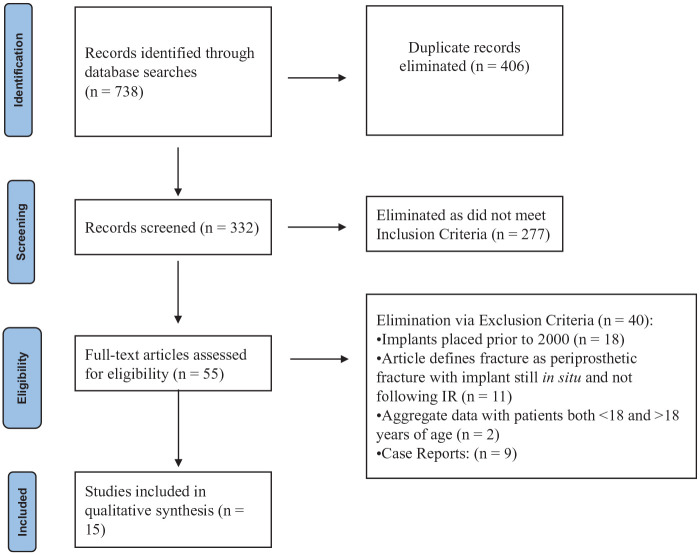
The initial database search yielded 738 articles. After eliminating duplicates and applying both inclusion and exclusion criteria, the screen yielded 15 articles to be included (Figure 1). The studies were conducted across 11 separate countries (Table 1).
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flowchart of studies.
Table 1.
Implant removal study characteristics.
| Author | Year | Country | Study design | Level of evidence |
|---|---|---|---|---|
| Ryan et al. 17 | 2022 | United States | Retrospective | IV |
| Guo et al. 18 | 2021 | China | Retrospective | IV |
| Del Balso et al. 19 | 2021 | Canada | Retrospective | IV |
| Ding et al. 20 | 2021 | China | Retrospective cohort | III |
| Scheider et al. 7 | 2020 | Austria | Retrospective | IV |
| Busch et al. 21 | 2019 | United States | Retrospective | IV |
| Chung et al. 22 | 2018 | South Korea | Retrospective cohort | III |
| Dey et al. 23 | 2018 | India | Prospective comparative | II |
| Li et al. 24 | 2018 | United States | Retrospective | IV |
| Donadio et al. 25 | 2016 | France | Retrospective | IV |
| Canavese et al. 26 | 2014 | France and Italy | Retrospective | IV |
| Kelly et al. 27 | 2014 | United States | Retrospective cohort | III |
| Makki et al. 28 | 2014 | United Kingdom | Retrospective cohort | III |
| Becker et al. 29 | 2012 | Israel | Retrospective | IV |
| Gorter et al. 30 | 2011 | Netherlands | Retrospective | IV |
There is one (6.7%) prospective comparative study included in this review. The remaining studies are retrospective in nature, with four (26.7%) studies being retrospective comparative cohort studies. In terms of level of evidence, studies in this review included the following: level II (6.7%), level III (26.7%), and level IV (66.7%).
All studies included in this review defined a fracture or refracture as occurring subsequent to IR. In terms of anatomic locations, six (40.0%) articles only examined IR from the upper extremity, seven (46.7%) only reviewed IR from the lower extremity, and two (13.3%) looked at IR in both the upper and lower extremities. Six (40.0%) articles looked at a single type of IR, while nine (60.0%) examined fractures or refractures following the removal of multiple different types of implants. Four (26.7%) articles reported aggregate data on fractures following IR for both fractures as well as for IR following other initial indications for implant placement, such as congenital deformities. Two articles (13.3%) reported data for specific non-traumatic anatomic pathologies. The other nine (60.0%) articles specifically limited the initial indication to traumatic fractures; thus, reporting data on refractures (Table 2).
Table 2.
Summary of the implant removal studies reviewed.
| Author | Year | Implant type | Anatomic location | Key results |
|---|---|---|---|---|
| Ryan et al. 17 | 2022 | Deep implants (no further specifications) (n = 227) | Humerus (n = 49); radius (n = 6); ulna (n = 11); hip/pelvis (n = 17); femur (n = 85); tibia (n = 46); fibula (n = 3); foot (n = 10) | There was a fracture rate of 0.44% (1/227) following deep IR. |
| Guo et al. 18 | 2021 | External fixator (n = 165) | Femur (n = 165) | In patients with traumatic femoral shaft fractures treated definitively with external fixation, there was a refracture rate of 14.5% (24/165) |
| Del Balso et al. 19 | 2021 | Rigid IM nail (n = 9); distal locking screw (n = 15) | Femur (n = 24) | No refractures occurred following rigid IM nail removal in traumatic diaphyseal femoral fractures. |
| Ding et al. 20 | 2021 | Blade plate and LCP (n = 101) | Proximal femur (hip) (n = 101) | There was a fracture rate of 14.9% (15/101) following IR initially placed during proximal femoral osteotomy for developmental dysplasia of the hip. |
| Scheider et al. 7 | 2020 | ESIN (n = 33); plate (n = 98); K-wire (n = 204); external fixator (n = 102); Steinmann pin (n = 1); cerclage (n = 4); screw (n = 6) | Clavicle (n = 7); humerus (n = 108); radius (n = 52); ulna (n = 44); BBFA (n = 56); carpal (n = 11); metacarpal (n = 42); phalanx (n = 36); other/unspecified (n = 92) | There was a fracture rate of 2.5% (11/448) following IR in upper extremity surgery. |
| Busch et al. 21 | 2019 | ESIN (n = 14) | Femur (n = 14) | No refractures occurred following ESIN removal in length-unstable diaphyseal or metaphyseal femoral fractures. |
| Chung et al. 22 | 2018 | Blade plate (n = 273); LCP (n = 144) | Proximal femur (hip) (n = 417) | There was a fracture rate of 0.48% (2/417) following IR initially placed during proximal femoral osteotomy. |
| Dey et al. 23 | 2018 | Blade plate (n = 17); ESIN with temporary external fixators (n = 16) | Femur (n = 33) | No refractures occurred following IR in comminuted femoral shaft fractures. |
| Li et al. 24 | 2018 | Plate (n = 15) | Clavicle (n = 15) | There was a refracture rate of 6.7% (1/15) following plate removal for displaced clavicle fractures. |
| Donadio et al. 25 | 2016 | Locking plate (n = 4) | Wrist (n = 4) | No fractures occurred following IR in patients with cerebral palsy undergoing wrist arthrodesis. |
| Canavese et al. 26 | 2014 | ESIN (n = 52) | Humerus (n = 52) | No refractures occurred following ESIN removal in displaced proximal humerus fractures. |
| Kelly et al. 27 | 2014 | ESIN (n = 159); K-wire (n = 170); ESIN/K-wire combination (n = 10) | Radius (n = 40); ulna (n = 108); BBFA (n = 191) | There was a refracture rate of 4.7% (16/339) following IR in displaced forearm fractures. |
| Makki et al. 28 | 2014 | ESIN (n = 24); plate (n = 82) | Radius (n = 52); ulna (n = 12); BBFA (n = 42) | There was a refracture rate of 10.4% (11/106) following IR in forearm fractures. |
| Becker et al. 29 | 2012 | LCP (n = 35) | Femur (n = 35) | 8.6% (3/35) of patients experienced a fracture or refracture following femoral LCP removal. |
| Gorter et al. 30 | 2011 | ESIN (n = 96); K-wire (n = 173); screw (n = 19) | Humerus (n = 89); forearm (radius vs ulna vs BBFA not specified) (n = 142); femur (n = 23); leg (tibia vs fibula vs tibia/fibula not specified) (n = 15) | There was a refracture rate of 1.3% (4/309) following IR for traumatic fractures. |
IR: implant removal; IM: intramedullary; LCP: locking compression plate; ESIN: elastic stable intramedullary nail; BBFA: both bone forearm.
The key results of each individual study are summarized in Table 2. Mean time to IR and mean follow-up time are reported in Table 3.
Table 3.
Mean time to IR and mean follow-up time.
| Author | Year | Mean time to implant removal (months) | Mean follow-up time (months) |
|---|---|---|---|
| Ryan et al. 17 | 2022 | 8.4 | 25.0 |
| Guo et al. 18 | 2021 | 6.8 | 19.7 |
| Del Balso et al. 19 | 2021 | Not specified | 27.4 |
| Ding et al. 20 | 2021 | Not specified | >2 years follow-up required |
| Scheider et al. 7 | 2020 | 6.3 | 27.6 |
| Busch et al. 21 | 2019 | 9.4 | 18.0 |
| Chung et al. 22 | 2018 | Blade plate: 14.4; LCP: 13.2 | Blade plate: 105.6; LCP: 42.0 |
| Dey et al. 23 | 2018 | Not specified | 26.0 |
| Li et al. 24 | 2018 | 16.8 | 15.6 |
| Donadio et al. 25 | 2016 | Not specified | 22.0 |
| Canavese et al. 26 | 2014 | Range: 5–8 months | 18.3 |
| Kelly et al. 27 | 2014 | Buried implants: 3.5; exposed implants: 1.2 | 5.2 |
| Makki et al. 28 | 2014 | ESIN: 4.8; plate: 12.6 | Not specified (at least 12 months) |
| Becker et al. 29 | 2012 | Fracture group: 13; osteotomy group: 17.6 | 31.7 |
| Gorter et al. 30 | 2011 | K-wire: 1.3; ESIN: 4.0; screw: 6.3 | K-wire: 2.5; ESIN: 2.0; screw: 2.5 |
LCP: locking compression plate; ESIN: elastic stable intramedullary nail.
Intramedullary nails
In a retrospective cohort study of 339 patients examining complications of displaced pediatric forearm fractures treated with exposed versus buried implants, 16 (4.7%) patients experienced refracture following IR. 27 Of the 159 patients treated with elastic stable intramedullary nails (ESINs), 5 (3.1%) experienced a refracture. Makki et al. 28 performed a retrospective cohort study to investigate refractures following the removal of compression plates versus ESIN in pediatric forearm fractures. Of the 106 patients in the study, 11 (10.4%) experienced a refracture. Four out of 24 (16.7%) patients experienced refracture after the removal of ESIN. All refractures in the ESIN group occurred when IR was performed within 6 months of the initial surgery, and the refracture rate demonstrated significance beginning at 9 years of age (p = 0.02). Thus, the authors discourage routine removal of ESIN within 6 months of implantation.
A study by Canavese et al. 26 followed 52 children after removal of ESIN for displaced proximal humerus fractures. The primary objective of the study was to assess functional outcomes via a Quick DASH questionnaire.31,32 With an average follow-up of 18.3 ± 8.3 months (range: 6–39.5), no patients sustained a refracture following IR.
In a single-surgeon retrospective study, Busch et al. 21 investigated the outcomes of 14 length-unstable pediatric metaphyseal and diaphyseal femoral fractures treated with four ESINs. No cases of refracture occurred following IR; however, 1 (7.1%) patient sustained a peri-implant fracture with the ESINs still in place. The authors advocate consideration of this technique as an alternative to rigid intramedullary (IM) nailing, submuscular bridge plating, external fixation, or the use of only two ESINs in the treatment of these fractures.
A recent retrospective case series investigated the rate of femoral head osteonecrosis following rigid IM nail placement with a trochanteric start point for traumatic femoral shaft fractures. 19 Mean patient age was 13.4 ± 1.4 years. Of the 65 fractures treated with this technique, 24 (36.9%) underwent subsequent IR: 9 cases where the entire IM nail was removed and 15 cases of distal interlocking screw removal only. No patients experienced a refracture after the IR surgery. The authors also report no cases of femoral head avascular necrosis, demonstrating that their technique is safe in select skeletally immature patients.
In a study of 309 cases of IR following traumatic fractures, 4 (1.3%) patients experienced refracture. 30 Of the 96 patients treated with ESIN, 2 (2.1%) experienced refracture.
Plating
A recent study by Li et al. 24 examined complications after plate fixation of displaced pediatric clavicle fractures. Of the 36 cases reported in the article, 15 patients underwent subsequent plate removal, and 1 (6.7%) patient experienced refracture following IR.
The retrospective study by Makki reports that 7 out of 82 (8.5%) patients sustained a refracture following compression plate removal in pediatric forearm fractures. 28 All refractures occurred in the compression plate group when IR was performed within 12 months of the index surgery, with the refracture rate shown to be significantly higher beginning at 12 years of age (p = 0.03). Thus, the authors advocate waiting at least 12 months after implantation before removing plates in this population.
A retrospective review examined the functional outcomes of patients with cerebral palsy who underwent wrist arthrodesis with proximal row carpectomy and dorsal locking plate implantation for correction of flexion contractures. 25 Of the 20 patients included in the study, 4 (20%) underwent subsequent IR due to painful and prominent fixed extension of the third metacarpal head. No cases of fracture following IR had occurred at the latest follow-up.
Becker et al. 29 performed a retrospective study examining fractures and refractures following locking compression plate (LCP) implantation in children. In all, 41 patients were included, of which 25 underwent surgery for acute fracture, and 16 were treated with osteotomy or limb lengthening. Thirty-five plates were removed after radiographic evidence of complete union. There were 3 (8.6%) cases of fracture or refracture after IR. The authors concluded that LCPs may create an overly stiff construct, similar to external fixators. They report an apparent increased risk of refracture in the early postoperative period following femoral LCP removal and advise for greater caution during this time. Following the results of this institutional study, the authors have changed patients’ weightbearing status from weightbearing as tolerated in the immediate postoperative period to partial weightbearing with the use of crutches for at least 1 month following LCP removal.
A retrospective cohort study by Chung et al. 22 investigated the implant-related complications of LCPs versus blade plates (BPs) in patients undergoing proximal femoral osteotomy. The overall fracture rate following IR was 0.48% (2/417), with both cases occurring after LCP removal in patients with cerebral palsy. The authors also report 7 (2.6%) cases of loss of fixation with the BP still in place, and 1 (0.7%) periprosthetic fracture with a retained LCP. The overall risk of implant-related complications increased with age (p = 0.002).
In a retrospective case-control study, Ding et al. 20 investigated risk factors for implant-related fractures following proximal femoral osteotomy for developmental dysplasia of the hip. A total of 218 patients undergoing either BP or LCP were included in the study, of which 28 (12.8%) sustained an implant-related fracture. In all, 101 patients underwent IR, and 15 (14.9%) sustained a subsequent fracture. The remaining 13 fractures occurred in patients with retained implants.
K-wires
In the retrospective study by Kelly et al., 27 11 of 170 (6.5%) patients experienced forearm refracture after K-wire removal. There was no significant difference in refracture rate based on treatment with ESIN versus K-wires (p = 0.20). None of the 10 patients treated with an ESIN/K-wire combination experienced refracture. The authors demonstrated that there was no difference in refracture rate, infection rate, or overall complication rate based on whether implants were left exposed versus buried following surgery.
The study by Gorter et al. 30 reports that 2 of 173 (1.2%) patients sustained a refracture following K-wire removal. The authors found no difference in refracture or complication rate following IR based on fixation with ESIN, K-wires, or screws.
External fixation
A recent retrospective study investigated risk factors for refracture following external fixator removal in traumatic pediatric femoral shaft fractures. 18 Of the 165 patients treated in this study, 24 (14.5%) developed refracture. Statistical analysis showed that AO Pediatric Comprehensive Classification of Long Bone Fractures classification type 32-D/4.2 and L2/L3 ratio (L2, length of femur fixed by the two screws farthest from the fracture line; L3, the total length from the greater trochanter to the distal end of femur) were independent risk factors for refracture.
Multiple types of implants or hybrid fixation
A recent retrospective study examined complications of pediatric IR in the upper extremity. 7 Complications were graded according to classification systems established by Goslings and Gouma 33 and Sink et al. 34 IR was performed for both congenital and acquired malformations. In 448 cases of IR performed in 317 patients, there were 11 (2.5%) cases of fracture following removal of the implant. The authors found that the following variables were positively related to the severity of complications: more distal level of IR, external fixators, longer duration of surgery, and female sex.
Dey et al. 23 conducted a prospective study to compare the outcomes of blade plating versus a combination of elastic nailing with temporary external fixation in the treatment of comminuted pediatric femoral shaft fractures. No refractures occurred following the removal of either implant type. Both methods of fixation had comparable functional and radiographic outcomes. However, removal of the BP was noted to be more difficult compared to the temporary external fixation.
Ryan et al. 17 recently published a manuscript that reports data on complications following pediatric deep IR performed by graduate medical trainees (range, postgraduate year 2 to fellow). Of the 227 procedures performed, there was 1 (0.44%) refracture and 2 (0.88%) infections. All three complications occurred in procedures performed by resident physicians at the post-graduate year 3 (PGY3) level of training.
Discussion
The indications for orthopedic IR in the pediatric population remains a topic of debate.4,35–44 The procedure of IR encompasses a vast range of pathologies and fixation techniques. Exposed implants are routinely removed in the outpatient office setting 4–6 weeks postoperatively. Superficially buried implants are typically removed on an elective basis once complete fracture healing has occurred 6 months to a year after the initial operation. Buried implants should be removed in cases where skin breakdown results in exposure of the implant. 27 With respect to deep implants, peri-implant deep infections of plates or rigid IM nails is the only consensus indication for IR; in most other scenarios, IR is not a required procedure, and removal may be performed on a case-by-case basis through shared decision making between the patient and surgeon. 45 In 2005, Peterson described five general guidelines for which IR in the pediatric population may be considered. 46 (1) Implants with the potential to move in vivo, such as smooth K-wires and ESINs. These implants are prone to migrate causing irritation and damage to the surrounding soft tissues. (2) Plate fixation constructs that cause significant stress shielding of long bones which compromise the integrity of the bone should be removed. 11 (3) Social history including contact sports or high-impact activities may prompt IR upon healing due to high incidence of periprosthetic fractures. (4) When the implant will pose an increase in the difficulty or complicate a future procedure. (5) When there is potential for bony remodeling to completely embed the implant into the bone, hypothetically leading to significant difficulty with future removal. Other sources propose relative indications for IR including screw migration, implant failure, healed fractures, malunion or nonunion, and metal allergy.11,28,45,46 Patients under the age of 12 are at a significantly higher risk for refracture, and this complication must be considered when performing routine IR in this population. 28
Fractures following IR are one of the most feared complications of the operation. Numerous authors attribute these fractures to stress shielding.47–51 Conceptually, when the implant is in place, it reduces functional stress on the bone leading to weakening. Once removed, the weakened bone is at higher risk for injury until it remodels and strengthens. Busam et al. 11 concluded that implants should not be removed until 12 months after implantation to allow for osseous hypertrophy, and fluoroscopy should be utilized to ensure fracture did not occur during removal. In addition, stress risers cause a weakened cortical area where screws are removed. Studies have shown that these areas have a decreased energy absorbing capacity of up to 55%, and cadaveric models have shown a reduction in load to failure rates following drill hole placement.52,53 Protected weight bearing for 4 months following screw removal has been recommended as it is hypothesized that the bone mass at the removal site returns to near normal 18 weeks postoperatively. 54 In regard to plate fixation, Perren et al. 55 hypothesized that the construct contacting periosteum causes a temporary osteopenia resulting from decreased blood flow. This temporary vascular disruption may explain why multiple studies have shown lower rates of refracture when implants are retained longer.28,29,56
The rationale for IR and subsequent means of bone failure likely differs for various implant types. Smooth K-wire removal is routinely performed in the pediatric population to decrease the risk of physeal disruption. 57 Stress shielding is the most cited reason for refracture following plate removal. 54 Among traumatic fractures, the highest refracture rate (14.5%) from the aggregate data of the studies included in our review was seen following removal of external fixators. 18 This result substantiates previous literature that has shown significantly higher rates of complications, including refractures, following the removal of external fixators versus ESIN. 58 Likewise, there are likely differences in fracture rates for IR based on the bone from which the implant is removed, but this remains poorly documented in the literature. In contrast, previous studies have provided some evidence regarding the risk of refracture with nonoperative management. Pediatric forearm refracture rate following nonoperative management ranges between 4% and 8%,15,28,59,60 which is similar to the refracture rate of 4.7%–10.4% following IR in forearm fractures based on the results of our review.27,28 Clavicular refracture rates with nonoperative management are higher at 13%. 61 The results of our study demonstrate a clavicular refracture rate of 6.7% after IR, although this rate is based on the results of a single study. 24
While IR can result in subsequent fracture or other complications, implant retention is also associated with risks. Plate retention can accentuate angular deformities, most notably observed in the pediatric population with submuscular plate retention in the lateral distal femur leading to a valgus deformity. 47 Allergies to nickel or chromium, two common implant metals, have a reported prevalence of up to 15% in the population.62,63 Allergic reactions to metals can result in pruritic skin symptoms, or more severely in issues at the surgical site, such as poor wound healing or implant migration. 63 Implant corrosion may lead to the accumulation of toxic metal ions that oxidize and cause local tissue inflammation, fibrosis, or even necrosis.63,64 Some studies have suggested that the accumulation of very high levels of active ions may even lead to malignant growths.35,46,65–67 However, the available literature on both implant-related corrosion and carcinogenesis in orthopedic implants outside of those used in adult arthroplasty are largely confined to case reports. A recent review on implants used in fracture surgery affirmed that the risks of corrosion and carcinogenesis are exceedingly rare or even non-existent and are not a valid indication for IR. 64 Pain at the implant site is by far the most common adverse symptom of implant retention and remains the most common reason for IR.35,48
Retention of implants can also result in periprosthetic fractures or breakages of the implant itself. Implant retention increases stress concentration on the adjacent bone. This increased stress concentration, often termed a stress riser, helps explain why periprosthetic fractures can result from minor trauma.13,68 A study of forearm plate retention in the pediatric population reports a periprosthetic fracture incidence of 7.3%, 69 again similar to our reported refracture rate of 4.7%-10.4% following IR. In addition, Becker et al. 29 report a periprosthetic fracture rate of 4.9% with retained femoral LCPs, which is lower than their reported fracture rate of 8.6% following IR. Surgeons must weigh the risks of these periprosthetic fractures with the risks of postoperative fractures when contemplating IR.
The results of this systematic review show that the fracture rate ranges from 0% to 14.9% following IR. This review includes numerous different fracture types, anatomic locations, and types of implants. Some articles included in this review do not specify the type of implant removed prior to the fracture or refracture. Due to this heterogeneity, it is difficult to ascertain the underlying reasons for the observed differences in the rates of fracture or refracture following IR. The available literature also makes it difficult to adequately analyze the fracture rate following IR based on the initial indication for surgery. Broadly speaking, the articles included in this review report data on postoperative fractures for either trauma or congenital deformities for which reconstructive procedures were performed. Furthermore, there is little information on the bone quality or nutritional status of the patients at the time of IR. Unreported conditions such as relative osteopenia or low vitamin D levels may complicate the results of individual studies. There is also minimal discussion of the reduction techniques utilized in the individual studies, so it is difficult to discern whether closed versus open reduction has an impact on refracture rates. This information would be useful for implant types where either closed or open reduction can be employed, such as ESIN and K-wires. Each of these factors potentially limits the generalizability of the available data.
Despite the heterogeneity of the studies in this review, the results do allow for comparisons and analyses of the fracture rates for certain types of implants. Two studies examined the forearm refracture rate following the removal of ESIN.27,28 With the use of flexible nails in this population, Kelly et al. 27 report a refracture rate of 3.1%, while Makki et al. 28 found the rate to be higher at 16.7%, albeit with a much smaller sample size (n = 159 vs n = 24, respectively). Notably, the post-IR follow-up time was at least 12 months in the study by Makki et al., as opposed to a mean of 5.2 months follow-up in the study by Kelly et al. Thus, this may be a confounding variable, and a higher refracture rate may have been observed with longer follow-up time. This review also suggests that there are similar refracture rates with the use of plates in fracture surgery. The results demonstrate that the refracture rates range from 6.7% to 8.6% following LCP removal in the forearm, clavicle, and femur, respectively.24,28,29
The authors of this systematic review present the current state of the literature regarding fracture and refracture rates following orthopedic IR in the pediatric population. This review is limited by the relatively small number of studies and patients included. Furthermore, there is only 1 (6.7%) article with level II evidence, with the remaining studies having a level of evidence of either III or IV. Future studies could investigate differences in fracture or refracture rates based on different types of implants and different anatomic locations of IR. A randomized control trial or prospective study investigating the refracture rate for traumatic fractures treated nonoperatively versus with operative intervention would offer results without a potentially confounding retrospective clinical picture. Studies investigating rates of fractures following IR versus periprosthetic fractures that occur with retained implants would also be useful to better define the differences in incidence of these two complications.
Conclusion
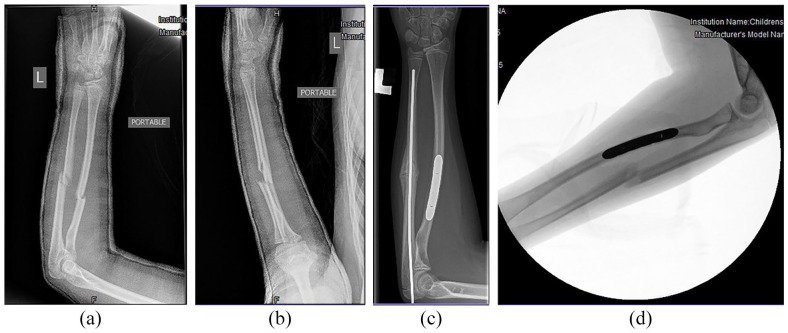
Overall, there is a paucity of literature addressing fracture rates following IR in the pediatric population. Based on our review, these complications occur frequently enough that patients, parents, and guardians should be counseled on the risk of this possibility prior to undergoing IR. The results of this review suggest that the forearm and femur are the anatomic sites most susceptible to fracture after IR, with reported incidences as high as 10.4% and 14.9%, respectively.20,28 With respect to traumatic fractures, definitive treatment with external fixation shows the highest aggregate rate of refracture, with a reported incidence of 14.5% in femoral shaft fractures.18,58 While the reported incidence of refracture following ESIN removal in pediatric forearm fractures is as high as 16.7%, this rate is drawn from a relatively small subset (n = 24) of patients in a study with a much larger total sample size (n = 106). 28 Other literature reports a much lower refracture rate of 3.1% with the removal of forearm flexible nails, 27 and even 0% when ESIN removal is performed in certain humerus and femur fractures, respectively.21,26 The results of this review show that the refracture rate following compression plate removal lies within a narrow range of 6.7%–8.6% across different anatomic sites.24,28,29 In certain instances, the fracture rate following IR might be greater than the rate of periprosthetic fractures that occur with retained implants. 29 Providers should carefully weigh the risks of these two complications when deliberating on removal or retention of the implant. Given that IR is one of the most common procedures performed by pediatric orthopedic surgeons, knowledge about postoperative fracture and its incidence is important in clinical decision making (Figure 2).
Figure 2.
AP (a) and lateral (b) radiographs following initial closed reduction and casting of a 12-year-old female who suffered a left bone forearm fracture. (c) Radiograph of the forearm at the time of ulnar ESIN removal. (d) Lateral fluoroscopic radiograph demonstrating refracture of the ulnar shaft 12 weeks after ESIN removal.
Footnotes
Author contributions: Anthony M Padgett: Study design; data acquisition; analysis and interpretation of data.
Cole M Howie: Study design; data acquisition; analysis and interpretation of data.
Thomas C Sanchez: Data acquisition; analysis and interpretation of data.
Addison Cimino: Analysis and interpretation of data.
Kevin A Williams: Data acquisition; analysis and interpretation of data.
Shawn R Gilbert: Study design; analysis and interpretation of data.
Michael J Conklin: Study design; analysis and interpretation of data.
All authors were actively involved in manuscript drafting, manuscript revision, and critical review of the manuscript for important intellectual content. All authors approve the manuscript submitted.
Compliance with ethical standards: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board. Informed consent was obtained from the parent/legal guardian for the publication of the details of any institutional cases and accompanying images presented in this manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Anthony M Padgett  https://orcid.org/0000-0003-1606-0641
https://orcid.org/0000-0003-1606-0641
References
- 1. Rutkow IM. Orthopaedic operations in the United States, 1979 through 1983. J Bone Joint Surg Am 1986; 68(5): 716–719. [PubMed] [Google Scholar]
- 2. Bostman O, Pihlajamaki H. Routine implant removal after fracture surgery: a potentially reducible consumer of hospital resources in trauma units. J Trauma 1996; 41(5): 846–849. [DOI] [PubMed] [Google Scholar]
- 3. Kellam PJ, Harrast J, Weinberg M, et al. Complications of hardware removal. J Bone Joint Surg Am 2021; 103(22): 2089–2095. [DOI] [PubMed] [Google Scholar]
- 4. Hanson B, van der Werken C, Stengel D. Surgeons’ beliefs and perceptions about removal of orthopaedic implants. BMC Musculoskelet Disord 2008; 9: 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stanitski CL. Metal removal in asymptomatic children and adolescents. J Pediatr Orthop 2005; 25(4): 557. [DOI] [PubMed] [Google Scholar]
- 6. Jamil W, Allami M, Choudhury MZ, et al. Do orthopaedic surgeons need a policy on the removal of metalwork? A descriptive national survey of practicing surgeons in the United Kingdom. Injury 2008; 39(3): 362–367. [DOI] [PubMed] [Google Scholar]
- 7. Scheider P, Ganger R, Farr S. Complications of hardware removal in pediatric upper limb surgery: a retrospective single-center study of 317 patients. Medicine 2020; 99(5): e19010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Highland TR, LaMont RL. Deep, late infections associated with internal fixation in children. J Pediatr Orthop 1985; 5(1): 59–64. [DOI] [PubMed] [Google Scholar]
- 9. Roberts TT, Haines CM, Uhl RL. Allergic or hypersensitivity reactions to orthopaedic implants. J Am Acad Orthop Surg 2017; 25(10): 693–702. [DOI] [PubMed] [Google Scholar]
- 10. Yoon PW, Kwon JE, Yoo JJ, et al. Femoral neck fracture after removal of the compression hip screw from healed intertrochanteric fractures. J Orthop Trauma 2013; 27(12): 696–701. [DOI] [PubMed] [Google Scholar]
- 11. Busam ML, Esther RJ, Obremskey WT. Hardware removal: indications and expectations. J Am Acad Orthop Surg 2006; 14(2): 113–120. [DOI] [PubMed] [Google Scholar]
- 12. Heldt B, Roepe I, Guo R, et al. All-epiphyseal versus trans-epiphyseal screw fixation for tillaux fractures: does it matter? World J Orthop 2022; 13(2): 131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Labosky DA, Cermak MB, Waggy CA. Forearm fracture plates: to remove or not to remove. J Hand Surg Am 1990; 15(2): 294–301. [DOI] [PubMed] [Google Scholar]
- 14. Lascombes P, Prevot J, Ligier JN, et al. Elastic stable intramedullary nailing in forearm shaft fractures in children: 85 cases. J Pediatr Orthop 1990; 10(2): 167–171. [PubMed] [Google Scholar]
- 15. Bould M, Bannister GC. Refractures of the radius and ulna in children. Injury 1999; 30(9): 583–586. [DOI] [PubMed] [Google Scholar]
- 16. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ryan C, Dunleavy ML, Burton A, et al. Outcomes of hardware removal surgery for children. Orthopedics 2022; 45(2): e91–e95. [DOI] [PubMed] [Google Scholar]
- 18. Guo M, Su Y. Risk factors for refracture of the femoral shaft in children after removal of external fixation. J Orthop Traumatol 2021; 22(1): 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Del Balso C, Bartley D, Cashin M, et al. Rigid intramedullary nail fixation of traumatic femoral fractures in the skeletally immature. OTA Int 2021; 4(2): e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ding J, Dai ZZ, Liu Z, et al. Risk factors for implant-related fractures after proximal femoral osteotomy in children with developmental dysplasia of the hip: a case-control study. Acta Orthop 2021; 92(2): 228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Busch MT, Perkins CA, Nickel BT, et al. A quartet of elastic stable intramedullary nails for more challenging pediatric femur fractures. J Pediatr Orthop 2019; 39(1): e12–e17. [DOI] [PubMed] [Google Scholar]
- 22. Chung MK, Kwon SS, Cho BC, et al. Incidence and risk factors of hardware-related complications after proximal femoral osteotomy in children and adolescents. J Pediatr Orthop B 2018; 27(3): 264–270. [DOI] [PubMed] [Google Scholar]
- 23. Dey S, Mishra K, Nagda TV, et al. Titanium elastic nailing with temporary external fixator versus bridge plating in comminuted pediatric femoral shaft fractures: a comparative study. Indian J Orthop 2018; 52(5): 507–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li Y, Helvie P, Farley FA, et al. Complications after plate fixation of displaced pediatric midshaft clavicle fractures. J Pediatr Orthop 2018; 38(7): 350–353. [DOI] [PubMed] [Google Scholar]
- 25. Donadio J, Upex P, Bachy M, et al. Wrist arthrodesis in adolescents with cerebral palsy. J Hand Surg Eur Vol 2016; 41(7): 758–762. [DOI] [PubMed] [Google Scholar]
- 26. Canavese F, Athlani L, Marengo L, et al. Evaluation of upper-extremity function following surgical treatment of displaced proximal humerus fractures in children. J Pediatr Orthop B 2014; 23(2): 144–149. [DOI] [PubMed] [Google Scholar]
- 27. Kelly BA, Miller P, Shore BJ, et al. Exposed versus buried intramedullary implants for pediatric forearm fractures: a comparison of complications. J Pediatr Orthop 2014; 34(8): 749–755. [DOI] [PubMed] [Google Scholar]
- 28. Makki D, Kheiran A, Gadiyar R, et al. Refractures following removal of plates and elastic nails from paediatric forearms. J Pediatr Orthop B 2014; 23(3): 221–226. [DOI] [PubMed] [Google Scholar]
- 29. Becker T, Weigl D, Mercado E, et al. Fractures and refractures after femoral locking compression plate fixation in children and adolescents. J Pediatr Orthop 2012; 32(7): e40–e46. [DOI] [PubMed] [Google Scholar]
- 30. Gorter EA, Vos DI, Sier CF, et al. Implant removal associated complications in children with limb fractures due to trauma. Eur J Trauma Emerg Surg 2011; 37(6): 623–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand). Am J Ind Med 1996; 29(6): 602–608. [DOI] [PubMed] [Google Scholar]
- 32. Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord 2003; 4: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Goslings JC, Gouma DJ. What is a surgical complication? World J Surg 2008; 32(6): 952. [DOI] [PubMed] [Google Scholar]
- 34. Sink EL, Leunig M, Zaltz I, et al. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res 2012; 470(8): 2220–2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Raney EM, Freccero DM, Dolan LA, et al. Evidence-based analysis of removal of orthopaedic implants in the pediatric population. J Pediatr Orthop 2008; 28(7): 701–704. [DOI] [PubMed] [Google Scholar]
- 36. Kahle WK. The case against routine metal removal. J Pediatr Orthop 1994; 14(2): 229–237. [DOI] [PubMed] [Google Scholar]
- 37. Morshed S, Humphrey M, Corrales LA, et al. Retention of flexible intramedullary nails following treatment of pediatric femur fractures. Arch Orthop Trauma Surg 2007; 127(7): 509–514. [DOI] [PubMed] [Google Scholar]
- 38. Simanovsky N, Tair MA, Simanovsky N, et al. Removal of flexible titanium nails in children. J Pediatr Orthop 2006; 26(2): 188–192. [DOI] [PubMed] [Google Scholar]
- 39. Sanderson PL, Ryan W, Turner PG. Complications of metalwork removal. Injury 1992; 23(1): 29–30. [DOI] [PubMed] [Google Scholar]
- 40. Kim WY, Zenios M, Kumar A, et al. The removal of forearm plates in children. Injury 2005; 36(12): 1427–1430. [DOI] [PubMed] [Google Scholar]
- 41. Langkamer VG, Ackroyd CE. Removal of forearm plates. A review of the complications. J Bone Joint Surg Br 1990; 72(4): 601–604. [DOI] [PubMed] [Google Scholar]
- 42. Loder RT, Feinberg JR. Orthopaedic implants in children: survey results regarding routine removal by the pediatric and nonpediatric specialists. J Pediatr Orthop 2006; 26(4): 510–519. [DOI] [PubMed] [Google Scholar]
- 43. Jevsevar DS, Shea KG, Murray JN, et al. AAOS clinical practice guideline on the treatment of pediatric diaphyseal femur fractures. J Am Acad Orthop Surg 2015; 23(12): e101. [DOI] [PubMed] [Google Scholar]
- 44. Howard A, Mulpuri K, Abel MF, et al. The treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg 2012; 20(5): 320–327. [DOI] [PubMed] [Google Scholar]
- 45. Montgomery BK, Gamble JG, Kha ST, et al. Indications for and risks associated with implant removal after pediatric trauma. J Am Acad Orthop Surg Glob Res Rev 2022; 6(4): 155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Peterson HA. Metallic implant removal in children. J Pediatr Orthop 2005; 25(1): 107–115. [DOI] [PubMed] [Google Scholar]
- 47. Kelly B, Heyworth B, Yen YM, et al. Adverse sequelae due to plate retention following submuscular plating for pediatric femur fractures. J Orthop Trauma 2013; 27(12): 726–729. [DOI] [PubMed] [Google Scholar]
- 48. Blasier RD, Aronson J, Tursky EA. External fixation of pediatric femur fractures. J Pediatr Orthop 1997; 17(3): 342–346. [PubMed] [Google Scholar]
- 49. Skaggs DL, Leet AI, Money MD, et al. Secondary fractures associated with external fixation in pediatric femur fractures. J Pediatr Orthop 1999; 19(5): 582–586. [PubMed] [Google Scholar]
- 50. Zhao X, Jing W, Yun Z, et al. An experimental study on stress-shielding effects of locked compression plates in fixing intact dog femur. J Orthop Surg Res 2021; 16(1): 97. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 51. Bostman OM. Refracture after removal of a condylar plate from the distal third of the femur. J Bone Joint Surg Am 1990; 72(7): 1013–1018. [PubMed] [Google Scholar]
- 52. Brooks DB, Burstein AH, Frankel VH. The biomechanics of torsional fractures. The stress concentration effect of a drill hole. J Bone Joint Surg Am 1970; 52(3): 507–514. [PubMed] [Google Scholar]
- 53. Juliano PJ, Yu JR, Schneider DJ, et al. Evaluation of fracture predilection in the calcaneus after external fixator pin removal. J Orthop Trauma 1997; 11(6): 430–434. [DOI] [PubMed] [Google Scholar]
- 54. Rosson J, Murphy W, Tonge C, et al. Healing of residual screw holes after plate removal. Injury 1991; 22(5): 383–384. [DOI] [PubMed] [Google Scholar]
- 55. Perren SM, Cordey J, Rahn BA, et al. Early temporary porosis of bone induced by internal fixation implants. Clin Orthop Relat Res 1988; 232: 139–151. [PubMed] [Google Scholar]
- 56. Schaaf AC, Weiner DS, Steiner RP, et al. Fracture incidence following plate removal in Legg-Calve-Perthes disease: a 32-year study. J Child Orthop 2008; 2(5): 381–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dahl WJ, Silva S, Vanderhave KL. Distal femoral physeal fixation: are smooth pins really safe. J Pediatr Orthop 2014; 34(2): 134–138. [DOI] [PubMed] [Google Scholar]
- 58. Guo YC, Feng GM, Xing GW, et al. A meta-analysis of flexible intramedullary nailing versus external fixation for pediatric femoral shaft fractures. J Pediatr Orthop B 2016; 25(5): 466–470. [DOI] [PubMed] [Google Scholar]
- 59. Litton LO, Adler F. Refracture of the forearm in children: a frequent complication. J Trauma 1963; 3: 41–51. [DOI] [PubMed] [Google Scholar]
- 60. Tischer W. Forearm fractures in childhood. Zentralbl Chir 1982; 107(3): 138–148. [PubMed] [Google Scholar]
- 61. Masnovi ME, Mehlman CT, Eismann EA, et al. Pediatric refracture rates after angulated and completely displaced clavicle shaft fractures. J Orthop Trauma 2014; 28(11): 648–652. [DOI] [PubMed] [Google Scholar]
- 62. Swiontkowski MF, Agel J, Schwappach J, et al. Cutaneous metal sensitivity in patients with orthopaedic injuries. J Orthop Trauma 2001; 15(2): 86–89. [DOI] [PubMed] [Google Scholar]
- 63. Black J. Does corrosion matter? J Bone Joint Surg Br 1988; 70(4): 517–520. [DOI] [PubMed] [Google Scholar]
- 64. Vos DI, Verhofstad MH. Indications for implant removal after fracture healing: a review of the literature. Eur J Trauma Emerg Surg 2013; 39(4): 327–337. [DOI] [PubMed] [Google Scholar]
- 65. Jacobs JJ, Gilbert JL, Urban RM. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am 1998; 80(2): 268–282. [DOI] [PubMed] [Google Scholar]
- 66. Keel SB, Jaffe KA, Petur Nielsen G, et al. Orthopaedic implant-related sarcoma: a study of twelve cases. Mod Pathol 2001; 14(10): 969–977. [DOI] [PubMed] [Google Scholar]
- 67. Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J Bone Joint Surg Am 2001; 83(3): 428–436. [DOI] [PubMed] [Google Scholar]
- 68. Yoo J, Ma X, Lee J, et al. Research update on stress riser fractures. Indian J Orthop 2021; 55(3): 560–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Clement ND, Yousif F, Duckworth AD, et al. Retention of forearm plates: risks and benefits in a paediatric population. J Bone Joint Surg Br 2012; 94(1): 134–137. [DOI] [PubMed] [Google Scholar]