Abstract
Background
Body image concerns are prevalent among young adults, who may be vulnerable to developing body image concerns because of particular risk factors associated with this life period. With technological advancements, digital mobile health (mHealth) apps are cost-effective and scalable interventions. Thus, mHealth apps can be explored as a form of prevention effort to alleviate body image concerns in young adults.
Objective
In this randomized controlled trial, we examined the effectiveness of a self-guided mHealth app in improving body image and self-compassion in a sample of university students.
Methods
Participants (N=310) were randomized to a 9-day self-guided body image and self-compassion mHealth app (n=149) and to an active waitlist control group (n=161), where they completed a similarly structured 9-day program on cooperation. Both programs consisted of content learning and activities such as quizzes, with the number and length of activities matched for both programs. Measures were obtained at baseline, upon completion of the programs (after the intervention), and at 4-week follow-up.
Results
The intervention group for female participants reported significant reduction in body dissatisfaction (P<.001) and improvements in body appreciation (P<.001) and self-compassion (P=.001) compared with the active waitlist control group after the intervention. Similarly, for male participants after the intervention, a significant reduction was found in the intervention group in body dissatisfaction (P<.001) after the intervention as well as improvements in body appreciation (P=.02) and self-compassion (P=.047). The effects were maintained at 4-week follow-up for female participants on body dissatisfaction (P<.001), body appreciation (P<.001), and self-compassion (P=.02) but not for male participants. On body image risk factors, significant reductions were found for female participants after the intervention for thin-ideal internalization (P<.001), peer pressure (P=.002), and media pressure (P<.001) after the intervention, while the effects were only maintained for thin-ideal internalization (P=.008) and media pressure (P=.01) at 4-week follow-up, compared with the active waitlist control group. As for male participants, no intervention effects were found both after the intervention and at follow-up for all body image risk factors of muscularity internalization, peer pressure, and media pressure. Both apps were acceptable and participants engaged equally across the intervention and active waitlist control groups, as indicated on a measure of app engagement (P=.76).
Conclusions
This study provides preliminary evidence for a self-guided mHealth app in improving body image concerns and self-compassion in young adult university students. Future studies should include longer follow-ups, and examine its effects with the wider populations of young adults.
Trial Registration
ClinicalTrials.gov NCT04977973; https://clinicaltrials.gov/ct2/show/NCT04977973
Keywords: body image, body image program, mobile health app, mHealth app, mobile-based interventions, dissonance-based interventions, self-compassion
Introduction
Background
Body image problems are highly prevalent among adolescents and young adults and have been frequently implicated in the development and maintenance of problematic eating behaviors [1,2] and body dysmorphic disorder [3,4]. Young adults may be particularly vulnerable to developing body image problems because of particular risk factors associated with this life period [5,6]. As young people transition through this developmental period, their bodies change in height, weight, and proportion while being exposed to social pressures associated with physical appearances [7]. Sociocultural factors play an important role in the development of body image concerns. According to the tripartite influence model, media, peers, and parents are the main sources of social influence on an individual’s body image [8]. These influences largely take place through appearance-ideal internalization and appearance comparisons [9]. Research has shown that women tend to desire the thin-ideal, whereas men desire muscularity and weight [10]. Appearance-ideal internalization was found to mediate the relationship between sociocultural influences and body dissatisfaction [11,12], with greater internalization exacerbating body dissatisfaction [9]. This suggests that reducing the internalization of appearance ideals likely decreases body dissatisfaction.
Individuals tend to engage in upward appearance comparison, whereby they compare their appearance to others whom they perceive to be more attractive [13]. Consequently, they experience lower body esteem and higher body dissatisfaction, which perpetuate further appearance comparison [9,14].
Exposure to media contributes to appearance-ideal internalization and appearance comparison. Media and social networking platforms are filled with ideal-looking images of the self and others which are often skewed representations of reality [15,16]. Through social learning, individuals tend to normalize such content and internalize them as reality [15,17]. Moreover, individuals with vulnerability factors such as preexisting body image concerns, low self-esteem, depression, perfectionism, or overvalued appearance ideals are more likely to engage in appearance comparison to seek assurance and validation [18]. Altogether, appearance comparison on media platforms contributes to the development and maintenance of body dissatisfaction [9], highlighting the importance of addressing media literacy in reducing body image concerns.
Among peers, appearance-focused comparison and appearance-related conversations and activities may also increase body dissatisfaction as they increase individuals’ awareness of their bodies, strengthen the internalization of appearance ideals, and negatively alter personal attitudes and beliefs in relation to beauty standards [19].
Apart from sociocultural influences, ruminative cognitive styles have been associated with greater body dissatisfaction [20]. Rumination is a response style to distress wherein individuals focus on repetitive thoughts and feelings about the distress [21]. As such, distress arising from negative body image may elicit rumination about one’s appearance, which in turn contributes to body dissatisfaction [20].
Positive Body Image and Self-compassion
Positive body image is characterized as being accepting, appreciating, and respecting of our bodies through attending to the body’s needs, protecting ourselves against unrealistic body ideals, having broader conceptualizations of beauty, and filtering information in a body-protective manner [22,23]. In qualitative studies, participants with positive body image actively rejected unrealistic media images to protect their body image [24,25]. Growing literature highlights that self-compassion contributes to a positive body image [26]. Self-compassion has been found to buffer the impact of media pressure on thin-ideal internalization in women [23], and to reduce body image distress and body dissatisfaction, reduce rumination, and increase body appreciation [23,27,28]. Homan and Tylka [29] highlighted that women who were high in self-compassion maintained high levels of body appreciation in the face of body-related comparisons. Thus, enhancing individuals’ self-compassion may reduce the effects of negative body image and promote positive body image.
Intervention programs targeting body image risk and protective factors have been developed in the last 2 decades. Psychoeducational and cognitive behavioral programs have been effective in improving body image concerns, reducing disordered eating behaviors and attitudes, thin-ideal internalization, and dieting in adolescents and young adults [30,31]. Dissonance-based interventions are also increasingly adopted to address health and social behaviors [32]. For example, the Body Project adopted dissonance-based approaches in a group setting by having participants voluntarily critique and take a counterattitudinal stance against the thin-ideal in verbal, written, and behavioral activities [33]. It was theorized that the discrepancy generated between participants’ personal beliefs (eg, thinner is better) and the counterattitudinal arguments made against pursuing thinness would elicit discomfort, and the discomfort would be alleviated by adjusting their personal beliefs to be more in line with the anti–thin-ideal statements [33]. Efficacy trials of the Body Project showed reduced eating disorder risk factors (eg, thin-ideal internalization and body dissatisfaction) and fewer eating disorder symptoms in female adolescents and young adults with body image concerns compared with assessment-only control conditions or alternative interventions, with numerous effects sustained up to 3-year follow-ups [34,35]. The Body Project M designed for male participants found that cognitive dissonance approach improved outcomes related to male participants’ dissatisfaction with body fat and muscularity, body appreciation, muscularity-enhancing behaviors, appearance comparison, and internalization after the intervention, with all outcomes except dissatisfaction with muscularity and internalization being sustained at 3-month follow-up [36]. Encouraging findings were also found for the Body Project: More Than Muscles, wherein significant reductions were observed for several eating disorder risk factors and muscularity and body fat dissatisfaction in male participants, with some outcomes maintained at the 4-week follow-up [37]. A further extension of the Body Project, the Body Project 4 All, evaluated the effectiveness of a mixed-sex program which found gains to be sustained over a 6-month follow-up [38]. Meta-analyses confirmed the effectiveness of dissonance-based programs [39,40]. Altogether, these studies suggest that dissonance-based interventions are promising in improving body image concerns in male and female participants.
The direct challenging of the thin-ideal within dissonance-based interventions differs somewhat from a self-compassion approach, which aims to promote greater awareness of adverse outcomes created by the thin-ideal. In response to this awareness, self-compassion interventions engender a mindset that promotes self-kindness and connection with others in the face of body image concerns. In other words, self-compassion approaches seek to alter the way in which individuals cope with the distress associated with negative body image [27,28] rather than changing body image itself.
Self-compassion interventions are gaining empirical support in alleviating body image concerns. Self-compassion meditation and single-session self-compassion writing tasks can reduce women’s body dissatisfaction and body shame and improve self-compassion and body appreciation [27,41]. A recent randomized controlled trial (RCT) by Toole et al [42] found self-compassion and dissonance-based interventions for young women with body image distress to be comparable with and more effective than waitlist control and suggested that integrating both self-compassion and dissonance-based approaches in interventions for body image may increase the acceptability of the interventions and reap more beneficial outcomes.
Self-guided, mobile-based body image programs have been developed and evaluated in light of technological advancements [43-45]. The 7-day mobile app study by Kosinski [44] led to a decrease in participants’ body dissatisfaction, drive for thinness, and increase in self-esteem. Cerea et al [43] adopted a cognitive behavioral training approach with short, daily, cognitive training exercises for 16 days and found that it reduced body dissatisfaction in female university students. Finally, BodiMojo, a 6-week program, which involves sending daily intervention messages on body image and self-compassion–related content, increased appearance esteem and self-compassion in adolescents [45]. In a sample of high school and college students, BodiMojo improved participants’ body image and self-compassion [45].
This Study
Emerging adulthood often marks the onset of body image concerns [35]. Presently, most intervention programs are designed for female participants and are conducted in Western populations. The Body Project was only recently modified to cater to male participants and mixed-sex groups [36-38]. However, these programs are conducted face-to-face and not on mobile platforms. Evidence is emerging that mobile apps can provide convenient, effective, and cost-friendly mental health interventions [46]. Therefore, this study evaluated the effectiveness of a self-guided mobile health (mHealth) body image app for both female and male participants. The app adopted both cognitive dissonance and self-compassion approaches, covering the following 3 topics: media literacy, appearance comparisons, and self-compassion. These topics were selected because of the robust empirical evidence that has been found for their role as risk and protective factors of body image concerns. The content was adapted from existing evidence-based interventions for body image, eating disorders, and self-compassion [47-51]. We predicted that the intervention would lead to significant improvements on measures of body image and self-compassion after the intervention and 4-week follow-up, compared with an active waitlist control group.
Methods
Participants
The sample consisted of 310 female (age: mean 21.12, SD 2.07 years) and male (age: mean 22.68, SD 2.10 years) adults aged between 18 to 30 years, recruited from the department of psychology’s research participant pool and the research recruitment platform of the National University of Singapore. A poster advertisement was uploaded on the respective recruitment platforms, wherein interested students were able to directly access a web-based link to participate in the study. Participants received either course credits or a reimbursement of SGD $ 15 (US $10.63). A power analysis with G*power 3.1 [52] revealed a minimum number of 128 participants, using a moderate effect size as found in relevant mobile-based body image studies [45,53,54]. We aimed for a total of 308 participants to account for a potential attrition of 20% [45].
Intervention Conditions
Body Image Program
This 9-day program adopted cognitive dissonance and self-compassion approaches designed around the following 3 topics: media literacy, appearance comparison, and self-compassion. At the start of each 3-day period, the participants underwent a 5-minute content learning and dissonance-based or self-compassion activity related to the topic (Textbox 1). The dissonance-based activity involved participants challenging sociocultural influences regarding media messages, appearance ideals, and appearance comparison. Participants typed their answers to questions which guided them in challenging sociocultural ideals. Self-compassion interventions involved psychoeducation and experiential activities. Participants were also given a cognitive or behavioral task, which encouraged noticing and challenging sociocultural influences in their daily lives, or practicing self-compassion.
Overview of the body image program content.
Topics and content
-
Topic 1: appearance ideal and media literacy
Introduce the concepts of body image and appearance ideals
Highlight how the media influences our appearance ideals and raise awareness of media manipulations
Elicit discrepancies between participants’ existing beliefs and behaviors about media influences
Develop participants’ skills in identifying media influences on appearance ideals
-
Topic 2: appearance comparison
Introduce the concept of appearance comparison
Highlight areas of common appearance comparisons for female and male participants
Highlight disadvantages and consequences of appearance comparison
Elicit discrepancies between participants’ existing beliefs and behaviors about appearance ideals and comparison
Develop participants’ ability to manage situations when appearance comparison arises
-
Topic 3: self-compassion
Introduce the concepts of self-compassion and appearance rumination
Highlight the disadvantages and consequences of appearance rumination
Introduce skills to develop participants’ ability to engage in self-compassion to manage negative thoughts and feelings about their body
Daily body image and self-compassion–focused messages were sent through the app to participants thrice a day, messages modeled after the BodiMojo mobile app (Table 1) [45]. These intervention messages included psychoeducation, affirmations, behavioral tips, short activities, and quizzes to reinforce participants’ learning (Figure 1).
Table 1.
Body image and self-compassion–focused intervention messages.
| Intervention messages | Examples |
| Body image |
|
| Mindfulness |
|
| Common humanity |
|
| Self-kindness |
|
| Behavioral tips |
|
| Affirmations |
|
Figure 1.
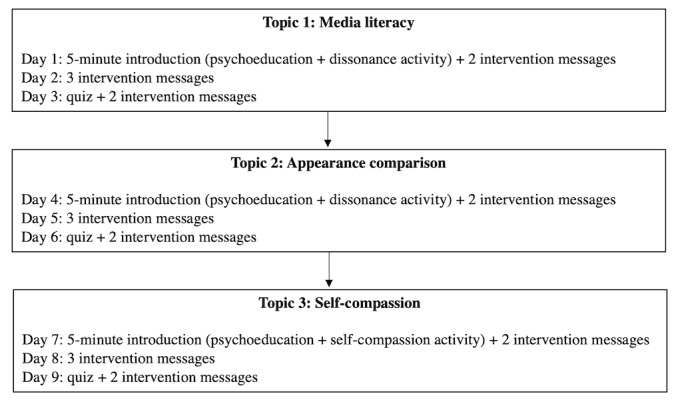
Flow of Body Image Program.
Cooperation Learning Program
Participants in the active waitlist control group engaged in a self-guided learning program on cooperation. The active waitlist control group was chosen instead of a waitlist control as it serves as an attention control to create similar experiences for participants in both groups to control for nonspecific factors that may influence the study outcomes [55]. This 9-day learning program develops participants’ skills to improve group morale and relationships. It consists of content learning once a day and activities such as quizzes, and the number and length of activities were matched to the body image app.
Ethics Approval
Ethics approval for this study was obtained from the National University of Singapore’s institutional review board (NUS-IRB-2021-85), and it was preregistered with ClinicalTrials.gov (registration number: NCT04977973). The methods and results described complied with the CONSORT (Consolidated Standards of Reporting Trials; 2010) guidelines for reporting RCTs (Figure 2) [56]. Data collection took place in Singapore in an entirely web-based setting.
Figure 2.
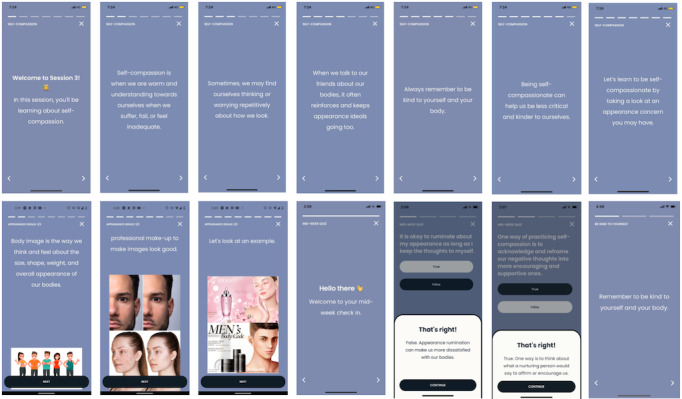
Screenshots of the body image program.
Procedure and Participant Flow
Participants first read the Participation Information Sheet on Qualtrics. After providing informed consent, participants completed measures on body image, body image risk factors, and self-compassion to obtain baseline ratings. Thereafter, participants were randomized to 1 of 2 conditions, intervention or active waitlist control, using simple randomization procedures. In this study, blinding of participants was marginally feasible as the content of the intervention programs that the participants engaged in were different in nature. However, participants were not outwardly informed of the real function of each intervention condition or of the real nature of the study being to evaluate the effectiveness of the body image program. The title of the study made known to participants was kept general (The effectiveness of a self-guided mobile phone application in improving the way we see ourselves and our bodies) to reduce the demand characteristics of the participants.
Next, the participants downloaded the mobile app and were guided on how to navigate the app. Participants in the intervention group underwent 9 days of body image training, while participants in the active waitlist control group underwent 9 days of the cooperation learning program. The anticipated time participants spent on each program was comparable (<5 minutes per day).
Participants filled out the same questionnaires upon program completion (postintervention measure) and after 4 weeks (follow-up measure). The feedback questionnaire was administered only after the intervention.
After the 6-week data collection period, participants were debriefed about the purpose and real intent of the study. Participants in the active waitlist control group were given access to the body image program.
Outcome Measures
Overview
Body Image Ideals Questionnaire (BIQ [57]) is a 22-item scale that assesses body image satisfaction-dissatisfaction by measuring the degree of congruence or discrepancy in one’s perceived and idealized physical attributes. On a scale ranging from 0 (exactly as I am) to 3 (very unlike me), participants rated the degree to which they resembled their physical ideal on 11 physical attributes. Next, participants rated the importance that they assigned to attaining their ideal on each physical attribute. The cross-products of the discrepancy and importance ratings for each physical attribute were obtained and a composite BIQ score was computed. Higher scores indicated greater disparity between one’s perceived and ideal physical attributes, suggesting higher levels of body dissatisfaction. The BIQ showed good internal consistency, with a Cronbach α of .81 for male participants and .76 for female participants.
The Body Appreciation Scale-2 [58] is a 10-item scale that assesses individuals’ positive attitudes toward their bodies. The items are scored on a scale from 1 (never) to 5 (always). Scores on all items are averaged with higher scores indicating greater body appreciation. The Body Appreciation Scale-2 has excellent internal consistency, with a Cronbach α of .96 for male participants and .97 for female participants.
The Sociocultural Attitudes Toward Appearance Questionnaire-4 Revised [59] measures internalization ideals and appearance-related sociocultural pressures. The 7 subscales consist of 31 items for female participants and 28 items for male participants on a scale ranging from 1 (definitely disagree) to 5 (definitely agree). Higher scores on each subscale indicate higher levels of internalization and sociocultural pressure. In this study, the subscales of Internalisation: Thin/Low Body Fat (for female participants), Internalisation: Muscularity (for male participants), and Pressures: Peers and Media were used. The internal consistencies of the subscales are good, with Cronbach α of ≥.82 in a sample of university female participants and Cronbach of ≥.75 in a sample of university male participants.
Self-Compassion Scale-Short Form [60] is a 12-item scale that measures self-compassion on 6 subscales. Each item is scored from 1 (almost never) to 5 (almost always). A total self-compassion score is the mean of all 6 subscales, with higher scores indicating higher levels of self-compassion. The internal consistency of the scale is excellent, with a Cronbach α of .86.
App Engagement
App Engagement Scale [61] is a 7-item scale that measures participants’ engagement on the phone app with scores ranging from 1 (definitely disagree) to 5 (definitely agree). A total score is derived by adding the scores from each item. Internal reliability of the scale is good, with a Cronbach α of .84.
Analytic Approach
Statistical analyses were conducted using SPSS (version 26.0; IBM Corp). As previous research has found that female and male participants’ body image are dissimilar and that they respond differently to intervention programs [62,63], analyses for this study were conducted separately for female and male participants. Intent-to-treat analyses were conducted to address loss of participant data because of participant withdrawal or technical difficulties, by carrying forward the participants’ last reported score. Independent 2-tailed t tests were also conducted to determine if participants who withdrew or could not continue because of technical difficulties differed significantly from those who remained in the study on any demographic and outcome measures. This informed of attrition-related bias, if any. Finally, missing scores on the App Engagement Scale (AES) were substituted using mean substitution [64].
An analysis of covariance (ANCOVA) examined if changes in outcome measures after intervention and at follow-up were significantly different in the intervention group compared with the active waitlist control group. ANCOVA is the recommended analysis for the inferential test of intervention effects [65]. By controlling for baseline scores, any baseline differences that may account for effects in the groups were removed, ensuring that the results after the intervention and at follow-up were because of intervention effects [66]. To compare the intervention and active waitlist control groups after the intervention, ANCOVA was conducted on postintervention scores, with baseline scores of the relevant outcome measures entered as the covariate. The α level was set at P<.05. Partial eta squared (ηp2) was the effect size reported for ANCOVA, while eta squared (η2) was the effect size reported for 2-tailed t tests and ANOVA.
Results
Participant Characteristics
A total of 313 participants completed questionnaires at baseline, 296 (94.57%) participants completed questionnaires after the intervention, and 291 (92.97%) participants completed questionnaires at follow-up (Figure 3).
Figure 3.
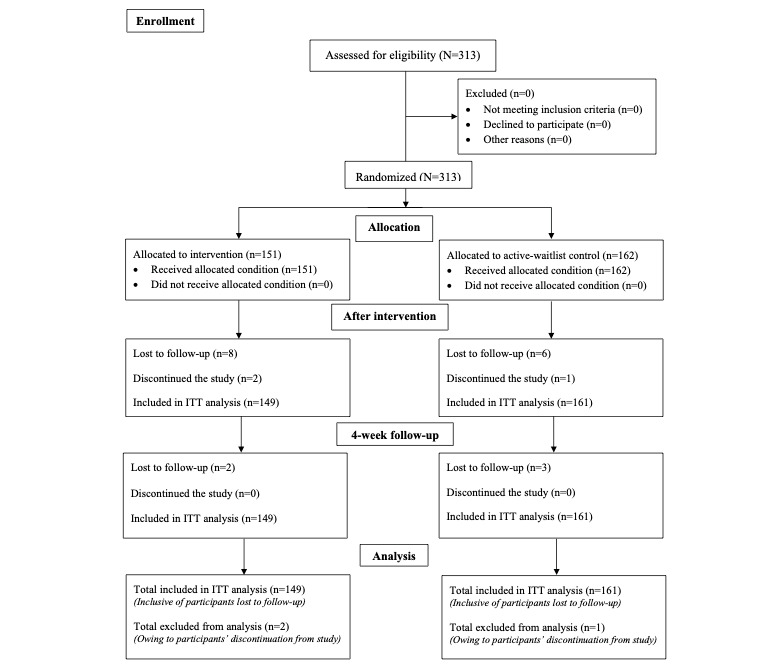
CONSORT (Consolidated Standards of Reporting Trials) flow diagram. ITT: intention-to-treat.
Preliminary Analyses
The intervention and active waitlist control groups did not differ significantly on demographic variables and most outcome measures at baseline (Tables 2, 3, and 4). The only outcome measure with a significant baseline difference was BIQ for male participants (P=.03). AES rated after the intervention did not differ significantly between female and male participants (P=.51) and between the intervention and active waitlist control groups (P=.76).
Table 2.
Descriptive statistics for demographic variable of sex by condition.
| Demographic variable | Intervention condition (n=149), n (%) | Active waitlist control condition (n=161), n (%) | P value | ||
| Sex | .32 | ||||
|
|
Female | 98 (65.8) | 115 (71) |
|
|
|
|
Male | 51 (34.2) | 46 (29) |
|
|
Table 3.
Descriptive statistics of baseline demographic and outcome variables by condition for female participants (N=213).
| Variable | Intervention condition | Active waitlist control condition | P value | ||
| Age (years), mean (SD) | 21.05 (1.96) | 21.18 (2.17) | .65 | ||
| BMI (kg/m2), mean (SD) | 20.20 (2.59) | 20.85 (3.32) | .14 | ||
| Race, n (%) | .13 | ||||
|
|
Chinese | 94 (95.9) | 102 (88.7) |
|
|
|
|
Malay | 0 (0) | 1 (0.9) |
|
|
|
|
Indian | 1 (1) | 8 (7) |
|
|
|
|
Others | 3 (3.1) | 4 (3.5) |
|
|
| BIQa score, mean (SD) | 2.14 (1.21) | 2.10 (1.17) | .80 | ||
| BASb score, mean (SD) | 3.44 (0.77) | 3.50 (0.75) | .54 | ||
| SCS-SFc score, mean (SD) | 2.88 (0.63) | 2.98 (0.55) | .23 | ||
| SATAQ-4Rd: Internalisation Thin/Low Body Fat score, mean (SD) | 3.15 (0.86) | 3.03 (0.89) | .32 | ||
| SATAQ-4R: peer pressure score, mean (SD) | 2.23 (1.00) | 2.14 (0.98) | .50 | ||
| SATAQ-4R: media pressure score, mean (SD) | 3.26 (1.04) | 3.18 (1.23) | .61 | ||
aBIQ: Body Image Ideals Questionnaire.
bBAS-2: Body Appreciation Scale-2.
cSCS-SF: Self-Compassion Scale-Short Form.
dSATAQ-4R: Sociocultural Attitudes Toward Appearance Questionnaire-4 Revised.
Table 4.
Descriptive statistics of baseline demographic and outcome variables by condition for male participants (N=97).
| Variable | Intervention condition | Active waitlist condition | P value | ||
| Age (years), mean (SD) | 23.06 (2.33) | 22.26 (1.76) | .06 | ||
| BMI (kg/m2), mean (SD) | 22.19 (3.59) | 22.79 (3.17) | .39 | ||
| Race, n (%) | .07 | ||||
|
|
Chinese | 50 (98) | 39 (84.8) |
|
|
|
|
Malay | 0 (0) | 1 (2.2) |
|
|
|
|
Indian | 0 (0) | 5 (10.9) |
|
|
|
|
Others | 1 (2) | 1 (2.2) |
|
|
| BIQa score, mean (SD) | 2.12 (1.17) | 1.59 (1.12) | .03b | ||
| BASc score, mean (SD) | 3.45 (0.73) | 3.55 (0.68) | .48 | ||
| SCS-SFd score, mean (SD) | 3.01 (0.52) | 3.05 (0.49) | .67 | ||
| SATAQ-4Re: muscularity internalization score, mean (SD) | 3.44 (0.74) | 3.17 (0.82) | .32 | ||
| SATAQ-4R: peer pressure score, mean (SD) | 2.79 (1.14) | 2.78 (1.10) | .94 | ||
| SATAQ-4R: media pressure score, mean (SD) | 2.70 (1.10) | 2.71 (1.05) | .96 | ||
aBIQ: Body Image Ideals Questionnaire.
bP<.05.
cBAS-2: Body Appreciation Scale-2.
dSCS-SF: Self-Compassion Scale-Short Form.
eSATAQ-4R: Sociocultural Attitudes Toward Appearance Questionnaire-4 Revised.
Intent-to-treat analyses were conducted for participants who were lost to follow-up by carrying forward their last reported scores. Missing scores for AES were substituted with the mean score. Independent 2-tailed t tests did not reveal any attrition-related biases across demographic and outcome variables (P>.10).
Main Analyses
Overview
Most outcome variables met the assumption tests for ANCOVA. The homogeneity of variance assumption was violated for a small number of outcome measures. However, because of the robustness of ANCOVA when sample sizes in each group are relatively equal [67], analysis using ANCOVA proceeded. The assumption of independence between independent variable and covariate was met for all outcome measures (P>.20), except BIQ for male participants. The assumption of homogeneity of regression slopes were violated in 2 variables for female participants (postintervention BIQ; postintervention SATAQ-4R Internalisation: Thin/Low Body Fat). For these variables, 1-way ANOVA was conducted using differences in scores between baseline and after the intervention and baseline and follow-up, respectively.
Female Participants
On body image measures, the intervention group reported significantly lower body dissatisfaction, and significantly higher body appreciation, after the intervention and at follow-up, compared with the active waitlist control group. The effect sizes were between moderate to large at both postintervention and follow-up. On thin-ideal internalization, the intervention group reported significantly lower internalization of thin-ideal scores after the intervention and at follow-up, compared with the active waitlist control group, with small to moderate effect sizes after the intervention and at follow-up. Significant score reductions were found on measures of peer and media pressure after the intervention in the intervention group, compared with the active waitlist control group, with small to moderate effect sizes. At follow-up, a significant difference was only found for reduction in media pressure, and no significant difference was found for peer pressure. Finally, significant differences were found for the self-compassion measure after the intervention and at follow-up, compared with the active waitlist control group (Table 5).
Table 5.
Means (SDs), univariate F test values, and effect sizes for outcome variables in female participants.
| Variable | Scale range | Baseline, mean (SD) | After the intervention | Follow-up | ||||||||||
|
|
|
Intervention | Control | Intervention, mean (SD) | Control, mean (SD) | F test (df) | P value | Effect sizea | Intervention, mean (SD) | Control, mean (SD) | F test (df) | P value | Effect sizea | |
| Body Image Ideals Questionnairescoreb | −3 to 9 | 2.14 (1.21) | 2.10 (1.17) | 1.30 (0.99) | 1.94 (1.20) | 26.02c (1) | <.001d | 0.11 | 1.42 (0.09) | 1.91 (0.087) | 17.48c (1) | <.001 | 0.077 | |
| Body Appreciation Scale-2 scoree | 1 to 5 | 3.44 (0.77) | 3.50 (0.75) | 3.79 (0.48) | 3.57 (0.44) | 37.80c (1) | <.001 | 0.27 | 3.73 (0.05) | 3.60 (0.045) | 38.00c (1) | <.001 | 0.27 | |
| Self-Compassion Scale-Short Form scoree | 1 to 5 | 2.88 (0.63) | 2.98 (0.55) | 3.28 (0.04) | 3.09 (0.041) | 10.82f (1) | .001 | 0.049 | 3.20 (0.47) | 3.05 (0.043) | 5.92g (1) | .02 | 0.027 | |
| SATAQ-4Rh: Internalisation Thin/Low Body Fatb score | 1 to 5 | 3.15 (0.86) | 3.03 (0.89) | 2.77 (0.85) | 3.03 (0.92) | 18.49c (1) | <.001 | 0.081 | 2.79 (0.06) | 3.00 (0.053) | 7.21f (1) | .008 | 0.033 | |
| SATAQ-4R: peer pressureb score | 1 to 5 | 2.23 (1.00) | 2.14 (0.98) | 2.00 (0.07) | 2.28 (0.065) | 9.73f (1) | .002 | 0.044 | 2.12 (0.08) | 2.30 (0.073) | 2.93 (1) | .09 | 0.014 | |
| SATAQ-4R: Media pressureb score | 1 to 5 | 3.26 (1.04) | 3.18 (1.23) | 2.77 (0.09) | 3.27 (0.080) | 18.08c (1) | <.001 | 0.079 | 2.80 (0.09) | 3.12 (0.085) | 6.49a (1) | .01 | 0.031 | |
aEffect sizes of 0.01=small, 0.06=moderate, and 0.14=large [68].
bLower scores are more desirable.
cP<.001.
dItalicized values indicate a significant P value at .05.
eHigher scores are more desirable.
fP<.01.
gP<.05.
hSATAQ-4R: Sociocultural Attitudes Toward Appearance Questionnaire-4 Revised.
Male Participants
Male participants in the intervention group reported significantly lower scores on body dissatisfaction after the intervention, compared with the active waitlist control group, with a large effect size. Male participants in the intervention group also reported significantly higher scores for body appreciation and self-compassion after the intervention, compared with the active waitlist control group, with effect sizes ranging from small to moderate. No intervention effects were found after the intervention for muscularity internalization, peer pressure, and media pressure, and at follow-up for all measures (Table 6).
Table 6.
Means (SDs), univariate F values, and effect sizes for outcome variables in male participants.
| Variable | Scale range | Baseline, mean (SD) | After the intervention | Follow-up | ||||||||||
|
|
|
Intervention | Control | Intervention, mean (SD) | Control, mean (SD) | F test (df) | P value | Effect sizea | Intervention, mean (SD) | Control, mean (SD) | F test (df) | P value | Effect sizea | |
| Body Image Ideals Questionnaireb | −3 to 9 | 2.12 (1.17) | 1.59 (1.12) | 1.24 (0.95) | 1.53 (1.20) | 16.07c (1) | <.001d | 0.15 | 1.69 (1.23) | 1.32 (1.24) | 0.69 (1) | .41 | 0.007 | |
| Body Appreciation Scale-2e | 1 to 5 | 3.45 (0.73) | 3.55 (0.68) | 3.83 (0.065) | 3.61 (0.068) | 5.71f (1) | .02 | 0.057 | 3.75 (0.07) | 3.60 (0.073) | 20.32 (1) | .13 | 0.024 | |
| Self-Compassion Scale-Short Forme | 1 to 5 | 3.00 (0.60) | 3.15 (0.64) | 3.33 (0.054) | 3.17 (0.057) | 4.039f (1) | .047 | 0.041 | 3.24 (0.06) | 3.12 (0.060) | 10.79 (1) | .18 | 0.019 | |
| SATAQ-4Rg: Muscularity internalisationb | 1 to 5 | 3.44 (0.74) | 3.28 (0.81) | 3.17 (0.092) | 3.20 (0.097) | .070 (1) | .79 | 0.001 | 3.27 (0.09) | 3.25 (0.093) | 0.018 (1) | .89 | 0.000 | |
| SATAQ-4R: Peer pressureb | 1 to 5 | 2.79 (1.14) | 2.78 (1.10) | 2.57 (0.12) | 2.85 (0.12) | 2.72 (1) | .10 | 0.028 | 2.48 (0.10) | 2.63 (0.11) | 0.99 (1) | .32 | 0.01 | |
| SATAQ-4R: Media pressureb | 1 to 5 | 2.70 (1.10) | 2.71 (1.05) | 2.54 (0.13) | 2.62 (0.13) | 0.17 (1) | .68 | 0.002 | 2.78 (0.12) | 2.65 (0.12) | 0.61 (1) | .44 | 0.006 | |
aEffect sizes of 0.01=small, 0.06=moderate, and 0.14=large [68].
bLower scores are more desirable.
cP<.001.
dItalicized values indicate a significant P value at .05.
eHigher scores are more desirable.
fP<.05.
gSATAQ-4R: Sociocultural Attitudes Toward Appearance Questionnaire-4 Revised.
Discussion
Principal Findings
This RCT evaluated the effectiveness of a self-guided mHealth app in improving body image and self-compassion in a sample of Asian university students. Our study extended the findings of previous studies by showing that cognitive dissonance and self-compassion approaches delivered on a mobile-based platform can be beneficial in improving body image and self-compassion in young adults.
Our hypotheses for female participants were largely supported. Except for peer pressure whereby intervention effects were not found at follow-up, the intervention group reported significant improvements on body image, body image risk factors, and self-compassion at both postintervention and follow-up, compared with the active waitlist control group. Consistent with past research on longer web-based or face-to-face interventions, our findings showed that a 9-day mobile-based program using cognitive dissonance and self-compassion approaches can reduce body dissatisfaction and its risk factors, improve body appreciation, and improve self-compassion after the intervention and at follow-up in female adults [33,34,42,43,44,51,69]. The moderate to large effect sizes for improvements found on body image and risk factor measures in our body image program are comparable with the average effect sizes found in eBody Project after the intervention [54]. Furthermore, our study extended the study by Toole et al [42] by demonstrating that integrating dissonance-based and self-compassion approaches and conducting the intervention on a mobile-based app can be beneficial for body image interventions. Comparable with the study by Toole et al [42], the effect sizes for female participants in our study were also moderate to large for body dissatisfaction, body appreciation, and thin-ideal internalization after the intervention.
Our hypotheses for male participants were partially supported. Unlike findings from Body 4 All and Body Project M, which found significant improvements in male participants on body satisfaction, body appreciation, dissatisfaction with fat and muscularity, appearance comparison, and internalization of cultural appearance ideals, with some effects sustained at their respective follow-ups [37,38], our study only revealed significantly lower body dissatisfaction, higher body appreciation, and higher self-compassion in the intervention group after the intervention relative to the active waitlist control group. In particular, the effect size for body dissatisfaction was large. Although the results for internalization of muscularity (P=.79 and P=.89), peer pressure (P=.10 and P=.32), and media pressure (P=.68 and P=.44) did not reach statistical significance after intervention and at follow-up, there was a trend observed toward male participants in the intervention group reporting lower scores of muscularity internalization and media and peer pressure after the intervention.
Overall, our findings provide preliminary support for the use of cognitive dissonance and self-compassion approaches on an mHealth app to reduce body image concerns and improve self-compassion in students. On the basis of the cognitive dissonance theory and the dual pathway model [33,70], guiding participants to challenge ideal appearances likely led to the participants’ reduced subscription to appearance ideals, which decreased body dissatisfaction. The 4-week follow-up effects found in female participants for all measures except for peer pressure were encouraging. In particular, the large effect sizes maintained for female participants on the improvements on both body dissatisfaction and body appreciation both after the intervention and at the 4-week follow-up are noteworthy. In addition to the use of cognitive dissonance techniques in our body image program to challenge appearance ideals directly, the integration of self-compassion components may have contributed to female participants’ enhanced self-awareness of appearance ideals, elicited a compassionate view of themselves and their bodies, and helped them to cope with the body image distress by fostering self-kindness and connection with others. Altogether, these may have translated to greater intrinsic self-worth and enhanced acceptance and appreciation of their bodies [27,42]. In addition, a self-compassion approach for the body image program may have been more appealing for young female adults, and increased their acceptance of the program [42].
Consistent with BodiMojo’s 6-week mobile-based intervention, our 9-day mobile-based intervention revealed comparable small to moderate effect sizes in self-compassion after the intervention for female and male participants. Compared with BodiMojo and the face-to-face programs of the Body Project, our study found similar or larger effect sizes for body image in both sexes after the intervention [36,45,71]. These suggest that beneficial effects for body image and self-compassion can be obtained much faster than through longer web-based or face-to-face programs in reducing body image concerns and improving self-compassion in young adults. Although longer programs may provide more opportunities for users to learn and practice skills to elicit behavior change [72], briefer interventions could also be of value in sustaining users’ engagement and reducing attrition rates.
Although significant improvements in self-compassion were found for male participants after the intervention, the effect was weaker, and not significant at follow-up. As self-compassion has been identified as a crucial factor in reducing body dissatisfaction and enhancing body appreciation in female and male participants [29,73,74], the weaker effects observed for self-compassion in male participants may have had a downstream effect and explained the lack of follow-up effects for male participants’ body dissatisfaction and body appreciation.
Sex differences in self-compassion may explain the lack of follow-up effects for self-compassion in male participants. A meta-analysis conducted by Yarnell et al [75] suggested that self-compassion approaches may be more effective for women than men, as feminine gender role norms associated with nurturance, self-sacrifice, and caregiving may facilitate the fostering of compassion toward the self. On the contrary, masculine gender norms, which tend to be associated with being strong, unemotional, pragmatic, and independent may form barriers to men being tender and caring toward themselves in times of need [76,77]. Hence, men with higher masculine norm conformity may find it challenging to acquire self-compassion [78]. Nonetheless, individuals may not necessarily conform to traditional gender role orientations [78], and our study did not explore participants’ conformity to gender norms. As literature in this area remains relatively new, further research is required to improve our understanding of gender role norms in self-compassion, to effectively tailor self-compassion approaches for female and male participants.
Several reasons are conceivable why peer pressure did not reveal differential effects for male participants and for female participants at follow-up. During this developmental phase as a young adult, interpersonal relationships are crucial for female and male participants [79,80]. Female participants tend to experience greater sensitivity and stress because of interpersonal rejection [81,82]. Coupled with female participants’ tendency to associate body image with the perception of peer acceptance and the lack of effective coping strategies, female participants may have found it challenging to manage peer pressures [83,84]. Thus, equipping female participants with stress and communication management skills may be a more targeted approach for enhancing female participants’ capacity to reduce peer pressures [84]. The lack of significant findings for peer pressure in female participants at follow-up may also be because of a floor effect, as participants in both intervention and active waitlist control groups had low ratings on the measure at baseline, thus limiting intervention effects at follow-up. As for male participants, studies found that greater body dissatisfaction was related to peer stressors focused on personality characteristics or achievements [81,84]. Thus, targeting body image and its risk factors may be less effective in reducing peer pressures for male participants.
The lack of significant reduction in the internalization of muscularity after the intervention and at follow-up may be accounted for by at least 2 possible reasons. First, adaptations made to our mixed-sex body image program to incorporate male body image concerns may be insufficient in addressing muscular-ideal internalization in a targeted manner. For example, the terminology being changed to “ideal appearances” and insufficient examples for male participants may have led to an inadequate understanding of concerns related to muscular-ideal internalization, thus watering down the intervention effects for male participants. Second, male participants may be less engaged in the body image program than female participants, because of the lack of masculine points of reference [85]. Although app engagement ratings did not differ between sexes, there may be socially desirable or careless responses on the self-report questionnaires. This is also supported by research which highlighted that male participants are less likely to engage in body image interventions and digital mental health apps than female participants [86,87]. Moreover, as participants’ responses on the app program were not accessible by researchers to protect users’ confidentiality, the quality and length of the counterattitudinal written responses could not be objectively ascertained. Thus, there is a possibility that the men’s lower app engagement may have weakened the intervention effects.
Finally, the lack of group differences on media pressure for male participants was unexpected, as media literacy was previously found to be effective in reducing pressures from media influences [88]. A possible explanation may be that our media literacy content was inclined toward female appearance ideals and risk factors and thus the lack of specificity and relevance to male appearance ideals and risk factors may have reduced its effectiveness for male participants.
Strengths and Limitations
First, some causal conclusions can be drawn [89]. The use of an active waitlist control group as an attention waitlist control allowed us to disentangle the effects of attention and other nonspecific factors from the intervention effects, thus strengthening the RCT’s effects [90]. Another strength was the low attrition rate. Although some participants withdrew or could not continue because of technical glitches, the overall attrition rate was <10%, with no attrition-related biases. This conferred greater strength to the overall validity of our study. Separate analyses conducted for female and male participants in light of sex differences in body image allowed us to identify that our mixed-sex program was less effective for male participants than for female participants and thus identify ways to enhance intervention effects for male participants. Finally, the 4-week follow-up period gives some confidence that effects for female participants can be maintained over a short-term period.
This study has some limitations. First, student participants may limit the generalizability of findings, as university students and the public may differ in factors such as level of education [91]. Hence, the university sample may not be representative of the general young adult population. Secondly, self-report measures are prone to social desirability bias, expectancies, and demand characteristics, which all may have contributed to the observed effects. Third, incentivizing participants with course credits or money may have motivated their participation and retention.
The sample size for male participants in our study was small despite additional recruitment efforts and thus was likely underpowered. Moreover, in view of sex differences in body image, more research is required to better understand ways to increase the effectiveness of mobile-based body image programs for male participants in a mixed-sex format and address muscularity concerns. To capture male participants’ body image concerns more accurately, male-specific measures such as Male Body Attitudes Scale [92] can be used in future studies.
Finally, in light of increasing studies which found self-compassion to mediate the effects of body image interventions, future studies can examine self-compassion as a mechanism of change. It would also be beneficial to obtain qualitative feedback from participants on elements of the body image program, such as their perception of the tone or number of intervention messages, to evaluate the effectiveness of the program.
Conclusions
Overall, this RCT provides preliminary but encouraging support for the effectiveness of a self-guided mHealth body image app using cognitive dissonance and self-compassion approaches for university students. Mobile-based well-being programs are cost-effective and accessible and can thus be widely disseminated to benefit the masses. Future research should seek to further enhance the program’s effectiveness with the wider young adult population.
Acknowledgments
The authors would like to thank Intellect Pte Ltd for providing the mobile phone app for the programs in this study, Mr Lee Sze Chi for his advice on statistical analysis, and Ms Rachel Low for her assistance in data collection. The authors would also like to thank all participants for the time and effort that they put into our study.
Abbreviations
- AES
App Engagement Scale
- ANCOVA
analysis of covariance
- BIQ
Body Image Ideals Questionnaire
- CONSORT
Consolidated Standards of Reporting Trials
- mHealth
mobile health
- RCT
randomized controlled trial
CONSORT-eHEALTH checklist (V 1.6.1).
Footnotes
Authors' Contributions: The main author (WYO) and coauthor (OS) were responsible for the study conceptualization and methodology, designing of the body image mobile phone app program, data curation and formal analysis, and the writing and editing of the protocol and manuscript. The coauthor (OS) also provided supervision of the overall study and procured funding for the study.
Conflicts of Interest: The study was partly funded by Intellect Pte Ltd. The study design, data management, interpretation, analysis, and reporting and the decision to publish the study are entirely independent of Intellect Pte Ltd. OS had a research collaboration with Intellect Pte Ltd at the time of the data collection and has since joined Intellect Pte Ltd as their clinical director.
References
- 1.Dakanalis A, Clerici M, Bartoli F, Caslini M, Crocamo C, Riva G, Carrà G. Risk and maintenance factors for young women's DSM-5 eating disorders. Arch Womens Ment Health. 2017 Dec;20(6):721–31. doi: 10.1007/s00737-017-0761-6.10.1007/s00737-017-0761-6 [DOI] [PubMed] [Google Scholar]
- 2.Howard LM, Romano KA, Heron KE. Prospective changes in disordered eating and body dissatisfaction across women's first year of college: the relative contributions of sociocultural and college adjustment risk factors. Eat Behav. 2020 Jan;36:101357. doi: 10.1016/j.eatbeh.2019.101357.S1471-0153(19)30081-9 [DOI] [PubMed] [Google Scholar]
- 3.Collison J, Harrison L. Prevalence of body dysmorphic disorder and predictors of body image disturbance in adolescence. Adolesc Psychiatr. 2020 Dec 21;10(3):206–18. doi: 10.2174/2210676610999200420112129. [DOI] [Google Scholar]
- 4.Tremblay L, Limbos M. Body image disturbance and psychopathology in children: research evidence and implications for prevention and treatment. Curr Psychiatr Rev. 2009 Feb 01;5(1):62–72. doi: 10.2174/157340009787315307. [DOI] [Google Scholar]
- 5.Bucchianeri MM, Arikian AJ, Hannan PJ, Eisenberg ME, Neumark-Sztainer D. Body dissatisfaction from adolescence to young adulthood: findings from a 10-year longitudinal study. Body Image. 2013 Jan;10(1):1–7. doi: 10.1016/j.bodyim.2012.09.001. https://europepmc.org/abstract/MED/23084464 .S1740-1445(12)00122-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones DC, Crawford JK. Adolescent boys and body image: weight and muscularity concerns as dual pathways to body dissatisfaction. J Youth Adolescence. 2005 Dec;34(6):629–36. doi: 10.1007/s10964-005-8951-3.S1740-1445(07)00123-4 [DOI] [Google Scholar]
- 7.Grossbard JR, Lee CM, Neighbors C, Larimer ME. Body image concerns and contingent self-esteem in male and female college students. Sex Roles. 2009 Feb;60(3-4):198–207. doi: 10.1007/s11199-008-9535-y. https://europepmc.org/abstract/MED/28959088 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson JK, Heinberg LJ, Altabe M, Tantleff-Dunn S. Exacting Beauty: Theory, Assessment, and Treatment of Body Image Disturbance. Washington, DC, USA: American Psychological Association; 1999. [Google Scholar]
- 9.van den Berg P, Thompson JK, Obremski-Brandon K, Coovert M. The Tripartite Influence model of body image and eating disturbance: a covariance structure modeling investigation testing the mediational role of appearance comparison. J Psychosom Res. 2002 Nov;53(5):1007–20. doi: 10.1016/s0022-3999(02)00499-3.S0022399902004993 [DOI] [PubMed] [Google Scholar]
- 10.Neumark-Sztainer D, Eisenberg ME. Body image concerns, muscle-enhancing behaviors, and eating disorders in males. JAMA. 2014 Nov 26;312(20):2156–7. doi: 10.1001/jama.2014.5138.1938543 [DOI] [PubMed] [Google Scholar]
- 11.Lawler M, Nixon E. Body dissatisfaction among adolescent boys and girls: the effects of body mass, peer appearance culture and internalization of appearance ideals. J Youth Adolesc. 2011 Jan;40(1):59–71. doi: 10.1007/s10964-009-9500-2. [DOI] [PubMed] [Google Scholar]
- 12.Tiggemann M. Media exposure, body dissatisfaction and disordered eating: television and magazines are not the same! Eur Eat Disorders Rev. 2003 Sep;11(5):418–30. doi: 10.1002/erv.502. [DOI] [Google Scholar]
- 13.Myers TA, Ridolfi DR, Crowther JH, Ciesla JA. The impact of appearance-focused social comparisons on body image disturbance in the naturalistic environment: the roles of thin-ideal internalization and feminist beliefs. Body Image. 2012 Jun;9(3):342–51. doi: 10.1016/j.bodyim.2012.03.005.S1740-1445(12)00039-3 [DOI] [PubMed] [Google Scholar]
- 14.Sheldon P. Pressure to be perfect: influences on college students' body esteem. South Commun J. 2010 Jun 29;75(3):277–98. doi: 10.1080/10417940903026543. [DOI] [Google Scholar]
- 15.Grabe S, Ward LM, Hyde JS. The role of the media in body image concerns among women: a meta-analysis of experimental and correlational studies. Psychol Bull. 2008 May;134(3):460–76. doi: 10.1037/0033-2909.134.3.460.2008-04614-005 [DOI] [PubMed] [Google Scholar]
- 16.Zhao S, Grasmuck S, Martin J. Identity construction on Facebook: digital empowerment in anchored relationships. Comput Human Behav. 2008 Sep;24(5):1816–36. doi: 10.1016/j.chb.2008.02.012. [DOI] [Google Scholar]
- 17.Brown JD. Mass media influences on sexuality. J Sex Res. 2002 Feb;39(1):42–5. doi: 10.1080/00224490209552118. [DOI] [PubMed] [Google Scholar]
- 18.Perloff RM. Social media effects on young women’s body image concerns: theoretical perspectives and an agenda for research. Sex Roles. 2014 May 29;71(11-12):363–77. doi: 10.1007/s11199-014-0384-6. [DOI] [Google Scholar]
- 19.Webb HJ, Zimmer-Gembeck MJ. The role of friends and peers in adolescent body dissatisfaction: a review and critique of 15 years of research. J Res Adolesc. 2014 Dec;24(4):564–90. doi: 10.1111/jora.12084. [DOI] [Google Scholar]
- 20.Etu SF, Gray JJ. A preliminary investigation of the relationship between induced rumination and state body image dissatisfaction and anxiety. Body Image. 2010 Jan;7(1):82–5. doi: 10.1016/j.bodyim.2009.09.004.S1740-1445(09)00096-5 [DOI] [PubMed] [Google Scholar]
- 21.Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspect Psychol Sci. 2008 Sep;3(5):400–24. doi: 10.1111/j.1745-6924.2008.00088.x.3/5/400 [DOI] [PubMed] [Google Scholar]
- 22.Avalos L, Tylka TL, Wood-Barcalow N. The Body Appreciation Scale: development and psychometric evaluation. Body Image. 2005 Sep;2(3):285–97. doi: 10.1016/j.bodyim.2005.06.002.S1740-1445(05)00054-9 [DOI] [PubMed] [Google Scholar]
- 23.Tylka TL, Wood-Barcalow NL. What is and what is not positive body image? Conceptual foundations and construct definition. Body Image. 2015 Jun;14:118–129. doi: 10.1016/j.bodyim.2015.04.001.S1740-1445(15)00038-8 [DOI] [PubMed] [Google Scholar]
- 24.Holmqvist K, Frisén A. "I bet they aren't that perfect in reality:" appearance ideals viewed from the perspective of adolescents with a positive body image. Body Image. 2012 Jun;9(3):388–95. doi: 10.1016/j.bodyim.2012.03.007.S1740-1445(12)00041-1 [DOI] [PubMed] [Google Scholar]
- 25.Wood-Barcalow NL, Tylka TL, Augustus-Horvath CL. "But I Like My Body": positive body image characteristics and a holistic model for young-adult women. Body Image. 2010 Mar;7(2):106–16. doi: 10.1016/j.bodyim.2010.01.001.S1740-1445(10)00002-1 [DOI] [PubMed] [Google Scholar]
- 26.Wasylkiw L, MacKinnon AL, MacLellan AM. Exploring the link between self-compassion and body image in university women. Body Image. 2012 Mar;9(2):236–45. doi: 10.1016/j.bodyim.2012.01.007.S1740-1445(12)00011-3 [DOI] [PubMed] [Google Scholar]
- 27.Albertson ER, Neff KD, Dill-Shackleford KE. Self-compassion and body dissatisfaction in women: a randomized controlled trial of a brief meditation intervention. Mindfulness (N Y) 2015;6(3):444–54. doi: 10.1007/s12671-014-0277-3. [DOI] [Google Scholar]
- 28.Toole AM, Craighead LW. Brief self-compassion meditation training for body image distress in young adult women. Body Image. 2016 Dec;19:104–12. doi: 10.1016/j.bodyim.2016.09.001.S1740-1445(15)30075-9 [DOI] [PubMed] [Google Scholar]
- 29.Homan KJ, Tylka TL. Self-compassion moderates body comparison and appearance self-worth's inverse relationships with body appreciation. Body Image. 2015 Sep;15:1–7. doi: 10.1016/j.bodyim.2015.04.007.S1740-1445(15)00044-3 [DOI] [PubMed] [Google Scholar]
- 30.Lewis-Smith H, Diedrichs PC, Halliwell E. Cognitive-behavioral roots of body image therapy and prevention. Body Image. 2019 Dec;31:309–20. doi: 10.1016/j.bodyim.2019.08.009.S1740-1445(19)30360-2 [DOI] [PubMed] [Google Scholar]
- 31.Stice E, Orjada K, Tristan J. Trial of a psychoeducational eating disturbance intervention for college women: a replication and extension. Int J Eat Disord. 2006 Apr;39(3):233–9. doi: 10.1002/eat.20252. [DOI] [PubMed] [Google Scholar]
- 32.Freijy T, Kothe EJ. Dissonance-based interventions for health behaviour change: a systematic review. Br J Health Psychol. 2013 May;18(2):310–37. doi: 10.1111/bjhp.12035. [DOI] [PubMed] [Google Scholar]
- 33.Stice E, Mazotti L, Weibel D, Agras WS. Dissonance prevention program decreases thin-ideal internalization, body dissatisfaction, dieting, negative affect, and bulimic symptoms: a preliminary experiment. Int J Eat Disord. 2000 Mar;27(2):206–17. doi: 10.1002/(sici)1098-108x(200003)27:2<206::aid-eat9>3.0.co;2-d.10.1002/(SICI)1098-108X(200003)27:2<206::AID-EAT9>3.0.CO;2-D [DOI] [PubMed] [Google Scholar]
- 34.Becker CB, Smith LM, Ciao AC. Reducing eating disorder risk factors in sorority members: a randomized trial. Behav Ther. 2005;36(3):245–53. doi: 10.1016/s0005-7894(05)80073-5. [DOI] [Google Scholar]
- 35.Stice E, Marti C, Shaw H, Rohde P. Meta-analytic review of dissonance-based eating disorder prevention programs: Intervention, participant, and facilitator features that predict larger effects. Clinical Psychology Review. 2019 Jun;79:91–107. doi: 10.1016/j.cpr.2019.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jankowski GS, Diedrichs PC, Atkinson MJ, Fawkner H, Gough B, Halliwell E. A pilot controlled trial of a cognitive dissonance-based body dissatisfaction intervention with young British men. Body Image. 2017 Dec;23:93–102. doi: 10.1016/j.bodyim.2017.08.006.S1740-1445(16)30171-1 [DOI] [PubMed] [Google Scholar]
- 37.Brown TA, Forney KJ, Pinner D, Keel PK. A randomized controlled trial of The Body Project: more than muscles for men with body dissatisfaction. Int J Eat Disord. 2017 Aug;50(8):873–83. doi: 10.1002/eat.22724. https://europepmc.org/abstract/MED/28481431 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kilpela LS, Blomquist K, Verzijl C, Wilfred S, Beyl R, Becker CB. The body project 4 all: a pilot randomized controlled trial of a mixed-gender dissonance-based body image program. Int J Eat Disord. 2016 Jun;49(6):591–602. doi: 10.1002/eat.22562. https://europepmc.org/abstract/MED/27188688 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yager Z, O'Dea JA. Prevention programs for body image and eating disorders on university campuses: a review of large, controlled interventions. Health Promot Int. 2008 Jun;23(2):173–189. doi: 10.1093/heapro/dan004.dan004 [DOI] [PubMed] [Google Scholar]
- 40.Watson HJ, Joyce T, French E, Willan V, Kane RT, Tanner-Smith EE, McCormack J, Dawkins H, Hoiles KJ, Egan SJ. Prevention of eating disorders: A systematic review of randomized, controlled trials. Int J Eat Disord. 2016 Sep;49(9):833–862. doi: 10.1002/eat.22577. [DOI] [PubMed] [Google Scholar]
- 41.Seekis V, Bradley G, Duffy A. The effectiveness of self-compassion and self-esteem writing tasks in reducing body image concerns. Body Image. 2017 Dec;23:206–213. doi: 10.1016/j.bodyim.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 42.Toole AM, LoParo D, Craighead LW. Self-compassion and dissonance-based interventions for body image distress in young adult women. Body Image. 2021 Sep;38:191–200. doi: 10.1016/j.bodyim.2021.04.001.S1740-1445(21)00054-1 [DOI] [PubMed] [Google Scholar]
- 43.Cerea S, Ghisi M, Bottesi G, Manoli T, Carraro E, Doron G. Cognitive behavioral training using a mobile application reduces body image-related symptoms in high-risk female university students: a randomized controlled study. Behav Ther. 2021 Jan;52(1):170–82. doi: 10.1016/j.beth.2020.04.002.S0005-7894(20)30052-6 [DOI] [PubMed] [Google Scholar]
- 44.Kosinski T. A brief mobile evaluative conditioning app to reduce body dissatisfaction? A pilot study in university women. Front Psychol. 2019 Nov 21;10:2594. doi: 10.3389/fpsyg.2019.02594. doi: 10.3389/fpsyg.2019.02594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodgers RF, Donovan E, Cousineau T, Yates K, McGowan K, Cook E, Lowy AS, Franko DL. BodiMojo: efficacy of a mobile-based intervention in improving body image and self-compassion among adolescents. J Youth Adolesc. 2018 Jul;47(7):1363–72. doi: 10.1007/s10964-017-0804-3.10.1007/s10964-017-0804-3 [DOI] [PubMed] [Google Scholar]
- 46.Ebert DD, Cuijpers P, Muñoz RF, Baumeister H. Prevention of mental health disorders using Internet- and mobile-based interventions: a narrative review and recommendations for future research. Front Psychiatry. 2017 Aug 10;8:116. doi: 10.3389/fpsyt.2017.00116. doi: 10.3389/fpsyt.2017.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Diedrichs PC, Atkinson MJ, Steer RJ, Garbett KM, Rumsey N, Halliwell E. Effectiveness of a brief school-based body image intervention 'Dove Confident Me: Single Session' when delivered by teachers and researchers: Results from a cluster randomised controlled trial. Behav Res Ther. 2015 Nov;74:94–104. doi: 10.1016/j.brat.2015.09.004. https://linkinghub.elsevier.com/retrieve/pii/S0005-7967(15)30039-5 .S0005-7967(15)30039-5 [DOI] [PubMed] [Google Scholar]
- 48.Gilbert P. Training our minds in, with and for compassion: an introduction to concepts and compassion-focused exercises. Get Self Help. 2010. [2022-11-03]. https://www.getselfhelp.co.uk/docs/GILBERT-COMPASSION-HANDOUT.pdf .
- 49.Neff KD. The development and validation of a scale to measure self-compassion. Self Identity. 2003 Jul;2(3):223–50. doi: 10.1080/15298860309027. [DOI] [Google Scholar]
- 50.Stice E, Rohde P, Butryn ML, Shaw H, Marti CN. Effectiveness trial of a selective dissonance-based eating disorder prevention program with female college students: effects at 2- and 3-year follow-up. Behav Res Ther. 2015 Aug;71:20–6. doi: 10.1016/j.brat.2015.05.012. https://europepmc.org/abstract/MED/26056749 .S0005-7967(15)00095-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wade T, George WM, Atkinson M. A randomized controlled trial of brief interventions for body dissatisfaction. J Consult Clin Psychol. 2009 Oct;77(5):845–54. doi: 10.1037/a0016879.2009-17643-006 [DOI] [PubMed] [Google Scholar]
- 52.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007 May;39(2):175–91. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 53.Franko DL, Cousineau TM, Rodgers RF, Roehrig JP. BodiMojo: effective Internet-based promotion of positive body image in adolescent girls. Body Image. 2013 Sep;10(4):481–8. doi: 10.1016/j.bodyim.2013.04.008. https://europepmc.org/abstract/MED/23768797 .S1740-1445(13)00058-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stice E, Rohde P, Durant S, Shaw H. A preliminary trial of a prototype Internet dissonance-based eating disorder prevention program for young women with body image concerns. J Consult Clin Psychol. 2012 Oct;80(5):907–16. doi: 10.1037/a0028016. https://europepmc.org/abstract/MED/22506791 .2012-09463-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spokas ME, Rodebaugh TL, Heimberg RG. Treatment outcome research. In: McKay D, editor. Handbook of Research Methods in Abnormal and Clinical Psychology. Thousand Oaks, CA, USA: Sage Publications; 2008. pp. 513–30. [Google Scholar]
- 56.Schulz KF, Altman DG, Moher D, CONSORT Group CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010 Jun 01;152(11):726–32. doi: 10.7326/0003-4819-152-11-201006010-00232. https://www.acpjournals.org/doi/abs/10.7326/0003-4819-152-11-201006010-00232?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .0003-4819-152-11-201006010-00232 [DOI] [PubMed] [Google Scholar]
- 57.Cash TF, Szymanski ML. The development and validation of the Body-Image Ideals Questionnaire. J Pers Assess. 1995 Jun;64(3):466–77. doi: 10.1207/s15327752jpa6403_6. [DOI] [PubMed] [Google Scholar]
- 58.Tylka TL, Wood-Barcalow NL. The body appreciation scale-2: Item refinement and psychometric evaluation. Body Image. 2015 Jan;12:53–67. doi: 10.1016/j.bodyim.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 59.Schaefer LM, Harriger JA, Heinberg LJ, Soderberg T, Kevin Thompson J. Development and validation of the sociocultural attitudes towards appearance questionnaire-4-revised (SATAQ-4R) Int J Eat Disord. 2017 Feb;50(2):104–17. doi: 10.1002/eat.22590. [DOI] [PubMed] [Google Scholar]
- 60.Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin Psychol Psychother. 2011;18(3):250–5. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- 61.Bakker D, Rickard N. Engagement in mobile phone app for self-monitoring of emotional wellbeing predicts changes in mental health: MoodPrism. J Affect Disord. 2018 Feb;227:432–42. doi: 10.1016/j.jad.2017.11.016.S0165-0327(17)31678-6 [DOI] [PubMed] [Google Scholar]
- 62.Quittkat HL, Hartmann AS, Düsing R, Buhlmann U, Vocks S. Body dissatisfaction, importance of appearance, and body appreciation in men and women over the lifespan. Front Psychiatry. 2019 Dec 17;10:864. doi: 10.3389/fpsyt.2019.00864. doi: 10.3389/fpsyt.2019.00864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Golan M, Hagay N, Tamir S. Gender related differences in response to "in favor of myself" wellness program to enhance positive self and body image among adolescents. PLoS One. 2014 Mar 11;9(3):e91778. doi: 10.1371/journal.pone.0091778. https://dx.plos.org/10.1371/journal.pone.0091778 .PONE-D-13-46816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Parent MC. Handling item-level missing data: simpler is just as good. Couns Psychol. 2012 May 10;41(4):568–600. doi: 10.1177/0011000012445176. [DOI] [Google Scholar]
- 65.Stice E, Shaw H. Eating disorder prevention programs: a meta-analytic review. Psychol Bull. 2004 Mar;130(2):206–27. doi: 10.1037/0033-2909.130.2.206.2004-11156-002 [DOI] [PubMed] [Google Scholar]
- 66.Vickers AJ, Altman DG. Statistics notes: analysing controlled trials with baseline and follow up measurements. BMJ. 2001 Nov 10;323(7321):1123–4. doi: 10.1136/bmj.323.7321.1123. https://europepmc.org/abstract/MED/11701584 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nimon KF. Statistical assumptions of substantive analyses across the general linear model: a mini-review. Front Psychol. 2012 Aug 28;3:322. doi: 10.3389/fpsyg.2012.00322. doi: 10.3389/fpsyg.2012.00322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition. Mahwah, NJ, USA: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 69.Alleva JM. Body matters: interventions and change techniques designed to improve body image. Universitaire Pers Maastricht. 2015. [2022-11-03]. https://cris.maastrichtuniversity.nl/ws/files/1429541/guid-73c30008-0245-46fe-821c-f72ce60db8cc-ASSET1.0 .
- 70.Festinger L. A Theory of Cognitive Dissonance. Volume 2. Redwood City, CA, USA: Stanford University Press; 1957. [Google Scholar]
- 71.Stice E, Becker CB, Yokum S. Eating disorder prevention: current evidence-base and future directions. Int J Eat Disord. 2013 Jul;46(5):478–85. doi: 10.1002/eat.22105. https://europepmc.org/abstract/MED/23658095 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Khademian F, Aslani A, Bastani P. The effects of mobile apps on stress, anxiety, and depression: overview of systematic reviews. Int J Technol Assess Health Care. 2020 Dec 14;37:e4. doi: 10.1017/S0266462320002093.S0266462320002093 [DOI] [PubMed] [Google Scholar]
- 73.Maher AL, Lane BR, Mulgrew KE. Self-compassion and body dissatisfaction in men: extension of the tripartite influence model. Psychol Men Masculinities. 2021 Apr;22(2):345–53. doi: 10.1037/men0000271. [DOI] [Google Scholar]
- 74.Marta-Simões J, Ferreira C, Mendes AL. Exploring the effect of external shame on body appreciation among Portuguese young adults: the role of self-compassion. Eat Behav. 2016 Dec;23:174–9. doi: 10.1016/j.eatbeh.2016.10.006.S1471-0153(16)30138-6 [DOI] [PubMed] [Google Scholar]
- 75.Yarnell LM, Stafford RE, Neff KD, Reilly ED, Knox MC, Mullarkey M. Meta-analysis of gender differences in self-compassion. Self Identity. 2015 Apr 27;14(5):499–520. doi: 10.1080/15298868.2015.1029966. [DOI] [Google Scholar]
- 76.Levant RF. Research in the psychology of men and masculinity using the gender role strain paradigm as a framework. Am Psychol. 2011 Nov;66(8):765–76. doi: 10.1037/a0025034.2011-25622-036 [DOI] [PubMed] [Google Scholar]
- 77.Yarnell LM, Neff KD, Davidson OA, Mullarkey M. Gender differences in self-compassion: examining the role of gender role orientation. Mindfulness (N Y) 2018 Nov 27;10(6):1136–52. doi: 10.1007/s12671-018-1066-1. [DOI] [Google Scholar]
- 78.Reilly ED, Rochlen AB, Awad GH. Men’s self-compassion and self-esteem: the moderating roles of shame and masculine norm adherence. Psychol Men Masculinity. 2014 Jan;15(1):22–8. doi: 10.1037/a0031028. [DOI] [Google Scholar]
- 79.Matera C, Nerini A, Stefanile C. The role of peer influence on girls’ body dissatisfaction and dieting. Eur Rev Appl Psychol. 2013 Mar;63(2):67–74. doi: 10.1016/j.erap.2012.08.002. [DOI] [Google Scholar]
- 80.Wagner BM, Compas BE. Gender, instrumentality, and expressivity: moderators of the relation between stress and psychological symptoms during adolescence. Am J Community Psychol. 1990 Jun;18(3):383–406. doi: 10.1007/BF00938114. [DOI] [PubMed] [Google Scholar]
- 81.Stroud LR, Salovey P, Epel ES. Sex differences in stress responses: social rejection versus achievement stress. Biol Psychiatry. 2002 Aug 15;52(4):318–27. doi: 10.1016/s0006-3223(02)01333-1.S0006322302013331 [DOI] [PubMed] [Google Scholar]
- 82.Stroud LR, Tanofsky-Kraff M, Wilfley DE, Salovey P. The Yale Interpersonal Stressor (YIPS): affective, physiological, and behavioral responses to a novel interpersonal rejection paradigm. Ann Behav Med. 2000;22(3):204–13. doi: 10.1007/BF02895115. [DOI] [PubMed] [Google Scholar]
- 83.Holsen I, Carlson Jones D, Skogbrott Birkeland M. Body image satisfaction among Norwegian adolescents and young adults: a longitudinal study of the influence of interpersonal relationships and BMI. Body Image. 2012 Mar;9(2):201–8. doi: 10.1016/j.bodyim.2012.01.006.S1740-1445(12)00008-3 [DOI] [PubMed] [Google Scholar]
- 84.Murray K, Rieger E, Byrne D. The effect of peer stress on body dissatisfaction in female and male young adults. J Exp Psychopathol. 2016 May 16;7(2):261–76. doi: 10.5127/jep.046514. [DOI] [Google Scholar]
- 85.Seaton CL, Bottorff JL, Jones-Bricker M, Oliffe JL, DeLeenheer D, Medhurst K. Men's mental health promotion interventions: a scoping review. Am J Mens Health. 2017 Nov;11(6):1823–37. doi: 10.1177/1557988317728353. https://journals.sagepub.com/doi/10.1177/1557988317728353?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Garrido S, Millington C, Cheers D, Boydell K, Schubert E, Meade T, Nguyen QV. What works and what doesn't work? A systematic review of digital mental health interventions for depression and anxiety in young people. Front Psychiatry. 2019 Nov 13;10:759. doi: 10.3389/fpsyt.2019.00759. doi: 10.3389/fpsyt.2019.00759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: encouraging findings. Annu Rev Clin Psychol. 2007;3:207–31. doi: 10.1146/annurev.clinpsy.3.022806.091447. [DOI] [PubMed] [Google Scholar]
- 88.McLean SA, Paxton SJ, Wertheim EH. The role of media literacy in body dissatisfaction and disordered eating: a systematic review. Body Image. 2016 Dec;19:9–23. doi: 10.1016/j.bodyim.2016.08.002.S1740-1445(15)30076-0 [DOI] [PubMed] [Google Scholar]
- 89.Hariton E, Locascio JJ. Randomised controlled trials - the gold standard for effectiveness research: study design: randomised controlled trials. BJOG. 2018 Dec;125(13):1716. doi: 10.1111/1471-0528.15199. https://europepmc.org/abstract/MED/29916205 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Aycock DM, Hayat MJ, Helvig A, Dunbar SB, Clark PC. Essential considerations in developing attention control groups in behavioral research. Res Nurs Health. 2018 Jun;41(3):320–8. doi: 10.1002/nur.21870. [DOI] [PubMed] [Google Scholar]
- 91.Hanel PH, Vione KC. Do student samples provide an accurate estimate of the general public? PLoS One. 2016 Dec 21;11(12):e0168354. doi: 10.1371/journal.pone.0168354. https://dx.plos.org/10.1371/journal.pone.0168354 .PONE-D-16-18796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tylka TL, Bergeron D, Schwartz JP. Development and psychometric evaluation of the Male Body Attitudes Scale (MBAS) Body Image. 2005 Jun;2(2):161–75. doi: 10.1016/j.bodyim.2005.03.001.S1740-1445(05)00027-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CONSORT-eHEALTH checklist (V 1.6.1).


