Abstract
Background
To compile key strategies from the international experiences to improve access to primary healthcare (PHC) services in rural communities. Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities.
Methods
All published and unpublished qualitative and/or mixed method studies conducted to improvement access to PHC services were searched from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar. Articles published other than English language, citations with no abstracts and/or full texts, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We assessed the methodological quality of the included studies using mixed methods appraisal tool (MMAT) version 2018 to minimize the risk of bias. Data were extracted using JBI mixed methods data extraction form. Data were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes.
Results
Our analysis of 110 full-text articles resulted in ten key strategies to improve access to PHC services. Community health programs or community-directed interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, working with traditional healers, working with non-profit private sectors and non-governmental organizations including faith-based organizations are the key strategies identified from international experiences.
Conclusion
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies can play roles in achieving universal health coverage and reducing disparities in health outcomes among rural communities and enabling them to get healthcare when and where they want.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-022-01919-0.
Keywords: Primary healthcare, Access to PHC services, Rural communities, Key strategies to improve access to PHC services
Introduction
Universal health coverage (UHC) is used to provide expanding services to eliminate access barriers. Universal health coverage is defined by the world health organization (WHO) as access to key promotional, preventive, curative and rehabilitative health services for all at an affordable rate and ensuring equity in access. The term universal has been described as the State's legal obligation to provide healthcare to all its citizens, with particular attention to ensuring that all poor and excluded groups are included [1–3].
Strengthening primary healthcare (PHC) is the most comprehensive, reliable and productive approach to improving people's physical and mental wellbeing and social well-being, and that PHC is a pillar of a sustainable health system for UHC and health-related sustainable development goals [4, 5]. Despite tremendous progress over the last decades, there are still unaddressed health needs of people in all parts of the world [6, 7]. Many people, particularly the poor and people living in rural areas and those who are in vulnerable circumstances, face challenges to remain healthy [8].
Geographical and financial inaccessibility, inadequate funding, inconsistent medication supply and equipment and personnel shortages have left the reach, availability and effect of PHC services in many countries disappointingly limited [9, 10]. A recent Astana Declaration recognized those aspects of PHC need to be changed to adapt adequately to current and emerging threats to the healthcare system. This declaration discussed that implementation of a need-based, comprehensive, cost-effective, accessible, efficient and sustainable healthcare system is needed for disadvantaged and rural populations in more local and convenient settings to provide care when and where they want it [8].
Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities. The findings of this systematic literature review can be used by healthcare professionals, researchers and policy makers to improve healthcare service delivery in rural communities.
Methodology
Research question
What improves access to PHC services in rural communities? We used the PICO (population, issue/intervention, comparison/contrast, and outcome) construct to develop the search question [11]. The population is rural communities or remote communities in developing countries who have limited access to healthcare services. Moreover, we extended the population to developed countries to capture experiences of both developing and developed countries. The issue/intervention is implementation of different community-based health interventions to access to essential healthcare services. In this systematic review, we focused on PHC health services, mainly essential or basic healthcare services, community or public health services, and health promotion or health education. Primary healthcare is “a health care system that addressed social, economic, and political causes of poor health promotes health though health services at the primary care level enhances health of the community” [12]. Comparison/contrast is not appropriate for this review. The outcome is improved access to essential healthcare services.
Outcome measures
The outcome of this review is access to PHC services, such as preventive, promotive, curative, rehabilitative, and palliative health services which are affordable, convenient or acceptable, and available to all who need care.
Criteria for considering studies for this review
All published and unpublished qualitative and/or mixed method studies conducted to improve access to PHC services were included. Government and international or national organizations reports were also included. Different organizations whose primary mission is health or promotion of community health were selected. We included articles based on these eligibility criteria: context or scope of studies (access to PHC services), article type (primary studies), and publication language (English). Articles published other than English language, citations with no abstracts and/or full texts, reviews, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We didn’t use time of publication for screening.
Information sources and search strategy
We searched relevant articles from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar to access all forms of evidence. An initial search of MEDLINE was undertaken followed by analysis of the text words contained in the title and abstract, and of the index terms used to describe articles. We used the aforementioned performance indicators of PHC delivery and the PICO as we described above to choose keywords. A second search using all identified keywords and index terms was undertaken across all included databases. Thirdly, references of all identified articles were searched to get additional studies. The full electronic search strategy for MEDLINE, a major database we used for this review is included as a supplementary file (Additional file 1: Appendix 1).
Study selection and assessment of methodological quality
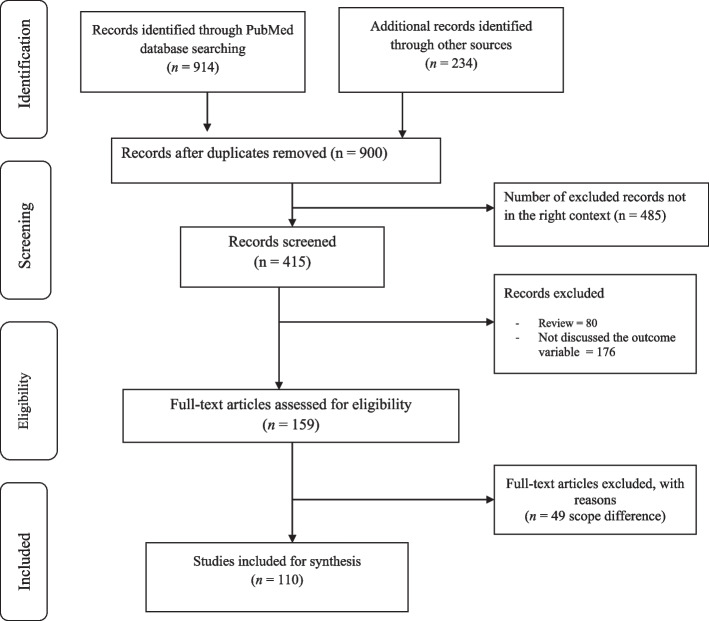
Search results from different electronic databases were exported to Endnote reference manager version 7 to remove duplication. Two independent reviewers (ZG and BA) screened out records. An initial screening of titles and abstracts was done based on the PICO criteria and language of publication. Secondary screening of full-text papers was done for studies we included at the initial screening phase. We further investigated and assessed records included in the full-text articles against the inclusion and exclusion criteria. We sat together and discussed the eligibility assessment. The interrater agreement was 90%. We resolved disagreements by consensus for points we had different rating. We used the PRISMA flow diagram to summarize the study selection processes.
Methodological quality of the included studies was assessed using mixed methods appraisal tool (MMAT) version 2018 [13]. As it is clearly indicated in the user guide of the MMAT tool, it is discouraged to calculate an overall score from the ratings of each criterion. Instead, it is advised to provide a more detailed presentation of the ratings of each criterion to better inform quality of the included studies. The rating of each criterion was, therefore, done as per the detail explanations included in the guideline. Almost all the included full text articles fulfilled the criteria and all the included full text articles were found to be better quality.
Data extraction
We independently extracted data from papers included in the review using JBI mixed methods data extraction form. This form is only used for reviews that follow a convergent integrated approach, i.e. integration of qualitative data and qualitative data [14]. The data extraction form was piloted on randomly selected papers and modified accordingly. One reviewer extracted the data from the included studies and the second reviewer checked the extracted data. Disagreements were resolved by discussion between the two reviewers. Information was extracted from each included study on: list of authors, year of publication, study area, population of interest, study type, methods, focus of the studies, main findings, authors’ conclusion, and limitations of the study.
Synthesis of findings
The included full-text articles were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes. Themes are strategies mentioned or discussed in the included records to improve access to PHC services. Themes were identified manually by reading the included records again and again. We then synthesized each theme by comparing the discussion and conclusion of the included articles.
Systematic review registration number
The protocol of this review is registered in PROSPERO (the registration number is: CRD42019132592) to avoid unplanned duplication and to enable comparison of reported review methods with what was planned in the protocol. It is available at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019132592.
Schematic of the systematic review and reporting of the search
We used PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 checklist [15] for reporting of this systematic review.
Results
Study selection
The search strategy identified 1148 titles and abstracts [914 from PubMed (Table 1) and 234 from other sources] as of 10 March 2022. We obtained 900 after we removed duplicated articles. Following assessment by title and abstract, 485 records were excluded because these records did not meet the criteria as mentioned in the method section. Additional 256 records were discarded because the records did not discuss the outcome of interest well and some records were systematic reviews. The full text of the remaining 159 records was examined in more detail. It appeared that 49 studies did not meet the inclusion criteria as described in the method section. One hundred ten records met the inclusion criteria and were included in the systematic review or synthesis (Fig. 1).
Table 1.
Search terms and number of articles found in PubMed Advanced search as of 10 March 2022
| Searches | Search term | Items found |
|---|---|---|
| 01 | “Rural communities”[All Fields] | 8,220 |
| 02 | “Remote population”[All Fields] | 84 |
| 03 | “Hard to reach areas”[All Fields] | 203 |
| 04 | “Medically underserved population”[All Fields] | 8,394 |
| 05 | 1 or 2 or 3 or 4 | 16,648 |
| 06 | “Healthcare service”[All Fields] | 2,435 |
| 07 | “Primary healthcare”[All Fields] | 8,556 |
| 08 | “Essential health services”[All Fields] | 307 |
| 09 | “Basic health services”[All Fields] | 382 |
| 10 | “Health extension program”[All Fields] | 101 |
| 11 | “Community health program”[All Fields] | 225 |
| 12 | “Health post”[All Fields] | 582 |
| 13 | “Community health worker” [All Fields] | 1,576 |
| 14 | “Strategies to improve healthcare” [All Fields] | 24 |
| 15 | “Access to essential healthcare services” [All Fields] | 12 |
| 16 | “Access to basic healthcare services” [All Fields] | 7 |
| 17 | “Equity to healthcare services” [All Fields] | 30 |
| 18 | “Health financing” [All Fields] | 43 |
| 19 | “Primary healthcare service delivery” [All Fields] | 6 |
| 20 | “Population health management” [All Fields] | 51 |
| 21 | “Availability of effective PHC services” [All Fields] | 130 |
| 22 | “Effective service coverage” [All Fields] | 65 |
| 23 | “Strategies to tackle healthcare barriers” [All Fields] | 147 |
| 24 | “Strategies to improve healthcare system” [All Fields] | 36,735 |
| 25 | 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 | 66,124 |
| 26 | 5 and 25 | 914 |
Fig. 1.
Study selection flow diagram
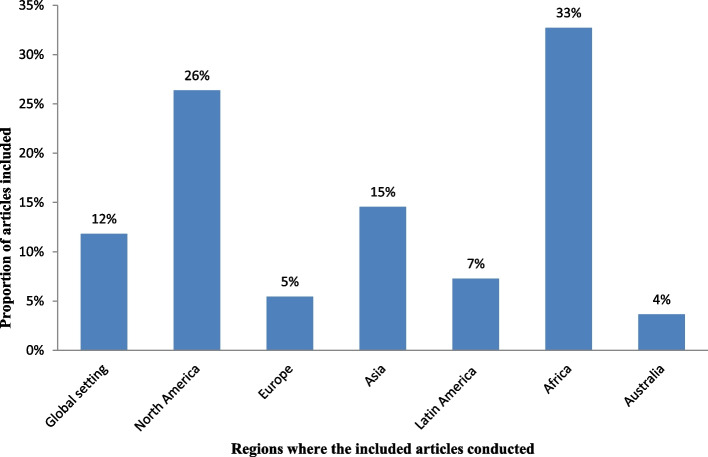
Of 900 articles resulting from the search term, 110 (12.2%) met the inclusion criteria. The included full-text articles were published between 1993 and 2021. Ninety-two (83.6%) of the included full-text articles were research articles, 5(4.5%) were technical reports, 3 (2.7%) were perspective, 4 (3.6%) was discussion paper, 3(2.7%) were dissertation or thesis, 2 (1.8%) were commentary, and 1 (0.9) was a book. Thirty-six (33%) and 29 (26%) of the included full-text articles were conducted in Africa and North America, respectively (Fig. 2).
Fig. 2.
Regions where the included full-test articles conducted
Key strategies identified
The analysis of 110 full-text articles resulted in 10 themes. The themes are key strategies to improve access to PHC services in rural communities. The key strategies identified are community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, promoting the role of traditional medicine, working with non-profit private sectors and non-governmental organizations (NGOs) including faith-based organizations (Table 2).
Table 2.
Key strategies identified to improve access to PHC services in rural communities
| Key strategies | References |
|---|---|
| Community health programs or community-directed healthcare interventions | [16–39] |
| School-based primary healthcare | [40–48] |
| Student-led healthcare services | [49–53] |
| Outreach services or mobile clinics | [54–71] |
| Family health program | [72–75] |
| Empanelment | [76–79] |
| Community health funding schemes | [80–90] |
| Telemedicine | [91–103] |
| Integrative medicine | [104–110] |
| Working with non-profit private sectors and non-governmental organizations | [111–125] |
Description of strategies
a. Community health programs or community-directed healthcare interventions
Twenty-four (21.8%) of the full-text articles included in this review discussed that community health programs (CHPs) or community-directed healthcare interventions are best strategies to provide basic health and medical care close to the community to increase access and coverage of essential health services. Community health programs are locally based health promotion, disease prevention, and treatment programs available typically to communities in need and community-directed intervention strategy is an approach in which communities themselves direct the planning and implementation of intervention delivery. Rural communities, especially, in developing countries have no access to healthcare facilities in the near distance and have less chance to receive healthcare from doctors, health officers, nurses or midwives. In response to this critical problems, many countries have been investing heavily in community based primary health care to bring services to rural and remote areas where most of the population lives. Community health programs include construction of health posts or community health centers close to the community and deployment of community health workers (CHWs), such as health extension workers, to reach-out every village, who play a prominent role as the gatekeepers of healthcare in rural communities. Community-directed healthcare intervention is an approach in which communities themselves direct the planning and implementation of healthcare interventions. Community participation remains crucial in the identification of health problems, planning or designing of health interventions and implementation of the interventions, which enhances need-based and demand-driven provision of health services while promoting sustainability and ownership (Additional file 2: Appendix 2, Table A1).
b. School-based primary healthcare
In this review, 9 of 110 (8.2%) of the included full-text articles pointed out that school-based healthcare services can be effective to improve access to PHC services. School-based health services are health programs that offer health care to children and youth either in a school or on school grounds and usually staffed according to school community needs and resources. School-based health services provide a variety of healthcare services to underserved children, youth and vulnerable populations in a convenient and accessible environment. Access to comprehensive health services via schools leads to improved access to healthcare (Additional file 3: Appendix 3, Table A2).
c. Student-led healthcare services
In this review, 5 of 110 (4.5%) of the full-text articles discussed that the use of medical and health science students as healthcare service providers can minimize problems related with shortage of health professionals in rural healthcare system and can play appreciable roles to minimize healthcare service access problems in rural communities. Student-led healthcare services are developed through consultation between universities and local health providers and are purposefully designed clinical placements with a focus on clinical educational activities for pre-registration students. Student-led clinics link students, healthcare professionals, community-based organizations, universities, and communities. In this approach, students can gain practical experience in an interdisciplinary setting and through exposure to a community with unique and severe needs (Additional file 4: Appendix 4, Table A3).
d. Outreach services or mobile clinics
In this systematic literature review, 18 of 110 (16.4%) of the included studies discussed that outreach services or mobile clinics in primary care and rural hospital settings can improve access to PHC services in rural communities. Mobile outreach service is defined as healthcare services provided by a mobile team of trained providers, from a higher-level health facility to a lower-level health facilities or locally available community facilities that are not used for clinical services, such as schools, health posts, or other community structures. Outreach services improve access to specialists and hospital-based services, strengthen connections between specialists and PHC providers, and give the benefits of consultations in primary care settings. Specialist outreach services have the potential to overcome access barriers faced by disadvantaged rural and remote communities. Furthermore, a community-based mobile clinics can be effective in uncovering illness and in directing patients to a healthcare home (Additional file 5: Appendix 5, Table A4).
e. Family health program
Four (3.6%) of the included full-text articles discussed that family health program (FHP) is highly cost-effective tool for improving access to healthcare services for deprived areas (such as rural communities). Family health program means the program is a program designed to provide primary care as well as the prevention and early treatment of communicable and non-communicable diseases in defined populations by deploying interdisciplinary healthcare teams include physicians, nurses, nurse assistants, and full-time community health agents. It has evolved into a robust approach to providing primary care for defined populations by deploying interdisciplinary healthcare teams. The nucleus of each team includes a physician, a nurse, a nurse assistant, and full-time community health agents. This approach is effective on improving access to healthcare and eliminating health disparities (Additional file 6: Appendix 6, Table A5).
f. Empanelment
This systematic review of literature identified that empanelment (also known as rostering) is a best strategy to proactively provide coordinated primary healthcare towards achieving universal health coverage. Empanelment is a continuous, iterative set of processes that identify and assign populations to facilities, care teams, or primary care providers who have a responsibility to know their assigned population. It enables health systems to improve health outcomes and to reduce costs. Empanelment establishes a point of care for individuals and simultaneously holds primary healthcare providers and care teams accountable for actively managing care for a specific group of individuals (Additional file 7: Appendix 7, Table A6).
g. Community health funding schemes
In this systematic review of literature, 11 (10%) of the included articles discussed that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare services in low-income rural communities. Community-based health insurance schemes are usually voluntary and characterized by community members pooling funds to offset the cost of healthcare. Moreover, this approach is effective to mobilize domestic resources for health at low income levels. For low-income countries, community health financing has modest ability to increase the total amount of funds for healthcare. Properly structured community health financing system can significantly improve efficiency, reduce the cost of healthcare, improve quality and health outcomes, and pool risks. Community-financing schemes could improve preventive services and reduce the incidence of diseases. It could also improve people’s access to healthcare and the quality of services, thus improving their health status. Community health financing could also improve risk pooling and reduce health-induced impoverishment. Community health insurance has potential positive impacts on health and social security (Additional file 8: Appendix 8, Table A7).
h. Telemedicine
In this review, 13 of 110 (11.8%) articles discussed that telemedicine is one of the solutions for rural subspecialty healthcare delivery. Telemedicine can be defined as the use of technology (computers, video, phone, messaging) by a medical professional to diagnose and treat patients in a remote location. The provision of subspecialty services using telemedicine to a remote and medically underserved population provides improved access to subspecialty care. Telemedicine brings sustainable healthcare to rural populations. Use of information and communication technologies in support of health and health-related fields, including healthcare services, health surveillance, health education, and health research has the potential to greatly improve health service efficiency, expand or scale up treatment delivery to thousands of patients in the rural populations (Additional file 9: Appendix 9, Table A8).
i. Promoting the role of traditional medicine
Seven (6.4%) of the included articles showed that incorporating traditional healers into public health system addresses healthcare needs of people with limited access to allopathic medicine. Traditional medicine is the sum total of the knowledge, skill, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness. Knowledge about traditional medicine has a catalyzing effect in meeting health sector development objectives. Integrating traditional medicine into national health systems in combination with national policy and regulation for products, practices and providers can enhance access to PHC services in remote populations (Additional file 10: Appendix 10, Table A9).
j. Working with non-profit private sectors and non-governmental organizations
In this systematic review, 15 of 110 (13.6%) of the included articles revealed that working with non-profit private sectors and NGOs strengthens the healthcare system. Involving the non-profit private sectors, faith-based organizations (FBOs), and NGOs for health system strengthening eventually contributes to create a healthcare system reflecting an increased efficiency, more equity and good governance in health. International and local NGOs have endeavored to fill the gaps in access to healthcare services, research and advocacy. Non-profit private sectors and NGOs have a key role in improving health in low- and middle-income countries. With networks that reach even the most remote communities, many FBOs are well positioned to promote demand and access for healthcare services. Partnership among FBOs is critical in increasing access to healthcare services, and ensuring sustainability by influencing behaviors at the community, family and individual level. Faith-based organizations play an integral role in the healthcare system by increasing health seeking behaviors and delivering supportive services that address common access and cultural barriers (Additional file 11: Appendix 11, Table A10).
Discussion
This systematic literature review found that community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telehealth, integrative medicine, and working with non-profit private sectors and NGOs are key strategies to improve access to PHC services in rural communities. The identified strategies address the four major pillars of primary healthcare (i.e., community participation, inter-sectoral coordination, appropriate technology, and support mechanism made available) [126]. Moreover, the identified strategies are effective to improve access to healthcare services to rural communities. Moreover, the identified strategies are effective to solve shortage of manpower and to build knowledge and skill of the local health workforces in rural healthcare system. The ability of a healthcare system to meet health needs of the population depends largely on the knowledge, skills, motivation and deployment of the people responsible for organizing and delivering health services. The results of this review can strengthen the health information system, which are core elements of the healthcare system that ensure community engagement through dissemination and use of timely and reliable health information to rural populations. This review also suggests strategies to narrow down the health disparities among rural populations, which is wide in most Least and Middle Income Countries (LMICs). Healthcare services are usually disproportionately concentrated in major urban areas. As a result, rural communities face growing health disparities, largely attributed to weak policies, inefficiencies, poor leadership, and governance in healthcare system.
This review identified that community health programs or community-directed healthcare interventions address health disparities by ensuring equitable access to health resources in communities where health equity is limited by socioeconomic and geographical factors. Community health programs include identifying and prioritizing public health problems in a specific geographic area; designing and implementing public health interventions (such as establishing community health centers, mobile clinics, and outreach programs); providing services (such as health education, screenings, social support, and counseling), and deploying community health workers to promote healthy behaviors; advocating for improved care for populations at risk; and working with stakeholders to address community healthcare needs [16–18, 127–130]. The community-oriented PHC model which is socially responsive medicine makes a healthcare system more rational, accountable, appropriate, and socially relevant to the public. Consequently, this model serves as a paradigm for reforming healthcare systems. Community-directed interventions can be considered as a realistic means to increase accessibility of interventions at community-level in rural areas [32–38]. This approach is best in situations where there are cultural barriers to implement interventions because this strategy is effective to develop ownership in the community. In-service and on-the-job training for community health workers, close supervision and government support, and program evaluation is very important to strengthen the community health program [131–133].
This review identified that school-based PHC services are effective strategies to improve access to PHC services. School-based health services provide a variety of healthcare services to children, youth and vulnerable populations in a convenient and accessible environment which indirectly improve leadership and governance. Science teachers and home room teachers play important roles to implement this strategy. It impacts on delivering preventive care such as immunizations, managing chronic illnesses and providing reproductive health services for adolescents. Comprehensive health services via schools improve access to healthcare information [40–47]. Access to school around the world increased drastically in the last century [134]. This high schooling rate is a good opportunity to provide healthcare services to school learners in accessible places and to disseminate health messages to families. Prior researches suggest that school-based healthcare services increase access to healthcare by increasing utilization of primary care, prevention services, and health maintenance visits [135, 136]. Including science teachers, home room teachers, school principals, students, communities, community health workers, and other interested parties in the school-based healthcare system as main actors or promoters must be considered to sustain the impact. Health and education sectors should work in collaboration with the above-mentioned actors to plan, implement and monitor the progress. School-based healthcare services are preferable in situations when there is high schooling rate and limited access to healthcare institutions. This strategy is also an alternative way in areas where the health seeking behavior of the community is low.
The use of medical and health science students in rural healthcare system was identified as a key strategy to minimize health inequalities in rural communities due to shortages in health workforce and distribution of healthcare resources [49–53]. Student-led health intervention is an alternative approach to provide essential healthcare services to the community where there is shortage of healthcare workers [137, 138]. Students will have opportunities to learn professional skills and competencies while they are providing healthcare services to the community. Moreover, benefits for student learning include increased communication, collaboration, and leadership skills [53, 139]. Student-led health intervention also enables increased access to services, more time for assessments and treatments, increased depth of health teaching, holistic and integrated healthcare, and free health supports [140–143]. However, the use of medical and health science students in the rural healthcare system may have ethical and competency issues. Supporting strategies such as close supervision, preparing clear protocols, and including senior experts in the team should be considered.
This systematic review of literature found that outreach services or mobile clinics can improve access to PHC service delivery in rural populations [54–69]. In developing countries, the highest proportion of people lives in rural areas where doctor services are not available. Rural communities travel to major cities to get specialist services. This reflects a desire for closer integration between primary and secondary care. Specialist outreach services or mobile clinics have become one of the effective solution to solve health disparities, to improve access to healthcare services, and to build capacity of local healthcare workforces. This strategy is preferable in situations when there are high loads in tertiary or referral level hospitals and when there is high patient leakage in the referral system [63–69]. However, the implementation may not be easy. It needs well established healthcare system and budget. Moreover, the efficiency of care may be lower compared with hospital-based cares and the effect on patients’ health outcomes might be small [56, 57, 61]. Irregular specialist visits in rural areas may not have real impacts unless the services are sustainable with a strong commitment at national and local levels. Outreach activities should be included in health policies with strong leadership, healthcare financing, and private initiatives must be encouraged to maintain the activities over time.
This review revealed that FHP is highly effective tool for improving health for rural communities. The FHP has provided a new, more robust model of primary healthcare services designed to provide accessible, first contact, comprehensive, and whole person care that is coordinated with other healthcare services. It has positive results to improved availability, access to, and use of health services, and improved health indicators, such as reduced infant mortality, improved detection of cases of neglected diseases, and reduced health disparities [73, 144–146]. The FHP deploys interdisciplinary healthcare teams. The team includes a physician, a nurse, a nurse assistant, and full-time community health agents. Family health teams are organized geographically. The teams are responsible for delivering public health interventions [72, 74]. Family health program is an alternative strategy in rural healthcare system in situations when there are inequities in access to care; when there is high hospitalization rate; when there is low health seeking behavior in the community; and when there is poor case detecting and reporting system. Despite these remarkable achievements, the FHP has some challenges include difficulties in the recruitment and retention of doctors trained appropriately to deliver primary healthcare, large variations in quality of local care, patchy integration of primary care services with existing secondary and tertiary care, and slow adoption of FHP in large population [147].
In this review, empanelment has been identified as a best strategy to deliver coordinated primary healthcare towards achieving universal health coverage [76–79]. The goal of empanelment is provide people-centered healthcare services based on their needs to ensure that every established patient receives optimal care, whether he/she regularly visits healthcare centers. Major activities in this approach include assignment of all patients to a healthcare provider panel; update panel assignments on a regular basis; and use panel data to educate, and track patients [79]. Empanelment enables healthcare systems to improve patient experiences, reduce costs, and improve health outcomes. Empanelment is an effective strategy to deliver four key functions: first-contact accessibility, continuity, comprehensiveness, and coordination [148]. Effective empanelment requires responsibility for the health of a target population, including providing healthcare services based on their health status, which is an important step in moving towards people-centered integrated healthcare [79].
This review identified that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare in low-income rural communities. Moreover, this approach is effective to mobilize domestic resources for health at low income levels [80–90]. Community-based health insurance is an emerging strategy to provide financial protection against the cost of illness. It is an effective strategy to improve access to quality health services for low-income rural households [149]. Existence of social capital in the community is a determinant factor for the effectiveness of CBHI as social capital has a positive effect on the community's demand for insurance [150, 151]. Moreover, solidarity and trust between the members are the key principles for the good functioning of a CBHI. Solidarity and trust stir-up members who are susceptible to risk to put together their resources for common use [149, 152, 153]. Affordability of premiums or contributions, technical arrangements made by the scheme management, timing of collecting the contributions, trust in the integrity and competence of the managers of the CBHI, The quality of care offered through the CBHI, accessible across different population groups are some of the determinant factors to be considered to increase people’s decision to join the CBHI schemes [154, 155].
In this review, telemedicine has been identified as one of the many possible solutions for rural subspecialty healthcare delivery. Telemedicine is a vital technological tool to increase healthcare access, improve care delivery systems, engage in culturally competent outreach, health workforce development, and health information system [91–100]. Telemedicine can be a great alternative to the traditional healthcare system in situations like diagnoses of common medical problems; inquiries about various medical issues for home treatments; post-treatment check-ins or follow-up for chronic care; holidays, weekends, late night or any other situation when regular medical care is not possible; patient inability to leave the house; patients who lack regular access to relevant medical expertise in their geographic area; and etc. However, technological issues are challenges when dealing with telemedicine, especially in developing countries. General problems of Internet connectivity and access to infrastructure can minimize benefits of this strategy. Costs associated with technology can also be a barrier. Furthermore, health technology requires human capacity to use it. Therefore, strengthening the information communication technologies (ICT) and human capacity building on ICT are important to address the health needs of the rural communities.
This systematic review of literature identified that promoting the role of TM solves problems of access to allopathic medicine. Integration of TM in health system will result in increased coverage and access to healthcare services. The role of complementary and alternative medicine for health is undisputed particularly in light of its role in health promotion and well-being. It also supports local health workforces [104–109]. Incorporating traditional healers into the public health system addresses healthcare needs [156, 157]. However, integrating TM to the public healthcare system is challenging. It is a general belief that TM defies scientific procedures in terms of objectivity, measurement, codification and classification [157]. If integrated, who provides training to medical doctors on the ontology, epistemology and the efficacies of TM in modern medicine [157]. Due to these, some scholars suggest that both TM and modern medicine be allowed to operate and develop independent of one another [158, 159]. Another fundamental challenge to TM is the widespread reported cases of fake healers and healings [157]. Generally, this strategy is more of feasible in areas where formal trainings on integrative medicine are available. Even though the integration is challenging, the health sector can use traditional healers as health educators or health promoters by providing training and continuous support. It can be also possible to use traditional healers as facilitators in the community-directed approaches. In general TM can be used in the primary healthcare system where no access to allopathic medicine and when conventional medicine is ineffective in treatment of disease [160].
Working with non-profit private sectors and NGOs has been identified as effective strategies to strengthen the healthcare system in developing countries [111–118]. Since governments in developing countries are challenged to meet the health needs of their populations because of financial constraints, limited human resources, and weak health infrastructure; the private sector (especially the non-profit private sectors) and non-governmental organizations can help expand access to healthcare services through its resources, expertise, and infrastructure. However, the presence of an NGO in the operation, may contribute to unrealistic expectations of health services, affecting perceptions of the latter negatively [113]. Moreover, reports have it that besides other issues in many instances NGOs allocated funds only to disease specific projects (vertical programming) rather than to broad based investments (horizontal programming) [161]. There are also concerns that donor expenditures in developing countries are not only unsustainable but may be considered as inadequate considering the enormous healthcare burden [161–164]. To avoid unrealistic expectations and dissatisfaction, and to increase and sustain the population’s trust in the organization, NGOs should operate in a manner that is as integrated as possible within the existing structure and should work close to the population it serves, with services anchored in the community. Moreover, faith-based organizations contribute in health such as disease prevention, health education or promotion, and community health development beyond psychological and spiritual care [119–124]. Religious organizations can reach all segments of rural populations. Therefore, integrating PHC services, especially health education and promotion, diseases prevention and community health development with religious organizations intensifies delivery of healthcare services. Working with FBOs is a best way in situations where cultural and faith-based barriers are common and in areas, where access problems are often related to lack of providers. However, religious organizations need intensive training on health promotion and health system to enable them to respond to local contexts within the framework of national policies. Moreover, there should be strong partnership with government agenesis to sustain the effort [165–168].
Contribution of this review
Various studies reported one or more strategies to improve access to primary healthcare services. However, the strategies reported by individual studies are not compiled together and there is lack of pooled evidence on effective strategies to improve access to healthcare system. This systematic literature review was, therefore, conducted to compile effective strategies to improve access to healthcare services in rural communities. The review suggests key strategies to improve access to PHC services in rural communities. These suggested strategies are implementable in countries that suffer from shortage of health workers and healthcare financing because all the strategies used locally available opportunities. The local healthcare system needs, therefore, scan the available opportunities in the locality for implementing the suggested strategies and needs to integrate the strategies in the healthcare system to sustain the impacts. Healthcare providers, researchers and policy makers could use the results of this systematic literature review to increase access to healthcare services in hard-to-reach areas. As the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional, and geographical challenges to adopt the identified strategies. Moreover, some of the experiences only come from one or two countries. Therefore, strategy developers and implementers need to consider these contextual challenges or variation during adopting and implementing different strategies.
Strengths and limitations of the study
As a strength, this systematic review explores international (both developed and developing countries) best experiences on primary healthcare service delivery and identified ten key approaches to improve access to PHC services in rural communities. We also searched relevant published or unpublished articles, dissertations or theses, discussion papers, and perspectives from a wide range of sources, such as MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar.
As a limitation, we entirely relied on electronic databases to search relevant articles. We didn’t include locally available printed out records. We also applied limits for language. We excluded articles published other than English language. We believed we could get more relevant articles if we had access to records available in prints and if we include articles published other than English language. Furthermore, since the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional and geographical challenges to adopt the identified strategies. There was also limited evidence for some articles, especially reports to rate their methodological quality. Readers should also note that our review might missed some important work in improving access to PHC services and the identified strategies are not the only strategies to improve access to PHC services. There might be other effective strategies which are not included in this review. In addition generalizability might be affected since some of the experiences only come from one or two countries. Moreover, this review focuses on access not quality of care delivered.
Conclusion
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies are effective to improve access to healthcare services in rural or remote communities. They can also play roles in achieving UHC and reducing disparities in health outcomes and increase access to rural communities to get healthcare when and where they want. Therefore, incorporating these key strategies suggested by this review in to the healthcare system is useful to enhance PHC services and to minimize impacts of health disparity in rural communities. However, the identified strategies may not be easy to implement. Increasing number and capacity of human resource for health; strengthening the healthcare financing system; improving medicine and supplies; working in different partners and communities; establishing monitoring and evaluation system; strong and committed leadership; and encouraging private initiatives must be considered to implement and maintain these strategies over time. Moreover, policy makers, program planners and implementers who want to utilize findings of this review should be aware that these are not the only effective strategies to improve access to primary healthcare services.
Supplementary Information
Additional file 1: Searchstrategy. MEDLINE (PubMed).
Additional file 2: Appendix 2: Table A1.Description of full-text articles which discussed community health programs or community-directed interventions as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 3: Appendix 3: Table A2.Description of full-text articles which discussed school-based healthcareservices as a strategy to improve PHCservice delivery in rural communities.
Additional file 4: Appendix 4: Table A3. Description of full-text articles which discussed student-led healthcareservices as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 5: Appendix 5: Table A4. Descriptionof full-text articles which discussed outreach services or mobile clinics as astrategy to improve PHC service delivery in ruralcommunities.
Additional file 6: Appendix 6: Table A5.Description of full-text articles which discussed family health program as astrategy to improve PHC service delivery in rural,communities.
Additional file 7: Appendix 7: Table A6. Description of full-text articles whichdiscussed empanelment as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 8: Appendix 9: Table A8.Description of full-text articles which discussed telemedicine or mobile healthas a strategy to improve PHC service delivery in ruralcommunities.
Additional file 9: Appendix 8: Table A7.Description of full-text articles which discussed community health funding schemes as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 10: Appendix 10: Table A9.Description of full-text articles which discussed promoting the role of workingwith traditional healers as a strategy toimprove PHC service delivery in rural communities.
Additional file 11: Appendix 11: Table A10.Description of full-text articles which discussed working with non-profitprivate sectors and non-governmental organizations as a strategy to improve PHC service delivery in rural communities.
Acknowledgements
The author would like to thank IPHC- E for funding this review.
Abbreviations
- CBHI
Community-based health insurance
- FBOs
Faith-based organizations
- FHP
Family health program
- ICT
Information communication technologies
- MMAT
Mixed methods appraisal tool
- NGOs
Non-governmental organizations
- PHC
Primary healthcare
- PHCPI
Primary Health Care Performance Initiative
- PICo
Population, phenomena of interest and context)
- TM
Traditional medicine
- UHC
Universal health coverage
Authors’ contributions
ZG prepared the manuscript. TA and GMK critically reviewed the protocol and manuscript. All the authors read and approved the final manuscript.
Funding
This review was funded by International Institute for Primary Health Care- Ethiopia (IPHC- E).
Availability of data and materials
All the extracted data are included in the manuscript.
Declarations
Ethics approval and consent to participate
Systematic review does not required ethics approval.
Consent for publication
This manuscript does not contain any individual person’s data.
Competing interests
The authors declared that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zemichael Gizaw, Email: zemichael12@gmail.com.
Tigist Astale, Email: tigist.astale@iifphc.org.
Getnet Mitike Kassie, Email: getnet.mitike@iifphc.org.
References
- 1.Hampton MB, Kettle AJ, Winterbourn CC. Inside the neutrophil phagosome: oxidants, myeloperoxidase, and bacterial killing. Blood. 1998;92(9):3007–3017. [PubMed] [Google Scholar]
- 2.Kirby M. The right to health fifty years on: Still skeptical? Health Hum Rights. 1999;4(1):6–25. [PubMed] [Google Scholar]
- 3.O’Connell T, Rasanathan K, Chopra M. What does universal health coverage mean? The Lancet. 2014;383(9913):277–9. [DOI] [PubMed]
- 4.White F. Primary health care and public health: foundations of universal health systems. Med Princ Pract. 2015;24(2):103–116. doi: 10.1159/000370197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanders D, Nandi S, Labonté R, Vance C, Van Damme W. From primary health care to universal health coverage—one step forward and two steps back. The Lancet. 2019;394(10199):619–621. doi: 10.1016/S0140-6736(19)31831-8. [DOI] [PubMed] [Google Scholar]
- 6.Brezzi M, Luongo P. Regional Disparities In Access To Health Care. 2016. [Google Scholar]
- 7.Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94(10):1675–1678. doi: 10.2105/ajph.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walraven G. The 2018 Astana declaration on primary health care, is it useful? J Glob Health. 2019;9(1). [DOI] [PMC free article] [PubMed]
- 9.Gillam S. Is the declaration of Alma Ata still relevant to primary health care? BMJ (Clinical research ed) 2008;336(7643):536–538. doi: 10.1136/bmj.39469.432118.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tollman S, Doherty J, Mulligan JA. General Primary Care. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, editors. Disease Control Priorities in Developing Countries. Washington: World Bank The International Bank for Reconstruction and Development/The World Bank Group; 2006. Available at https://www.ncbi.nlm.nih.gov/books/NBK11789/pdf/Bookshelf_NBK11789.pdf. [PubMed]
- 11.Stern C, Jordan Z, McArthur A. Developing the review question and inclusion criteria. AJN The Am J Nurs. 2014;114(4):53–56. doi: 10.1097/01.NAJ.0000445689.67800.86. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. losing the gap in a generation. Commission on Social Determinants of Health FINAL REPORT. 2008. Available at https://www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf. Accessed on 22 March 2022.
- 13.Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, GagnonM-P GF, Nicolau B, O’Cathain A. Mixed methods appraisal tool (MMAT), version 2018. Canada: IC Canadian Intellectual Property Office, Industry; 2018. Available at https://mixedmethodsappraisaltoolpublicpbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf.
- 14.JBI Manual for Evidence Synthesis. Appendix 8.1 JBI Mixed Methods Data Extraction Form following a Convergent Integrated Approach. Available at https://jbi-global-wiki.refined.site/space/MANUAL/3318284375/Appendix+8.1+JBI+Mixed+Methods+Data+Extraction+Form+following+a+Convergent+Integrated+Approach. Accessed on 12 August 2021.
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Glob Health. 2019;15(1):1–11. doi: 10.1186/s12992-019-0470-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Admassie A, Abebaw D, Woldemichael AD. Impact evaluation of the Ethiopian health services extension programme. J Dev Eff. 2009;1(4):430–449. [Google Scholar]
- 18.Yitayal M, Berhane Y, Worku A, Kebede Y. The community-based Health extension Program significantly improved contraceptive utilization in West gojjam Zone, ethiopia. J Multidiscip Healthc. 2014;7:201. doi: 10.2147/JMDH.S62294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Croke K, Mengistu AT, O’Connell SD, Tafere K. The impact of a health facility construction campaign on health service utilisation and outcomes: analysis of spatially linked survey and facility location data in Ethiopia. BMJ Glob Health. 2020;5(8):e002430. [DOI] [PMC free article] [PubMed]
- 20.Arwal S. Health Posts in Afghanistan. J Gen Practice. 2015;3(213):2. [Google Scholar]
- 21.Negussie A, Girma G. Is the role of Health Extension Workers in the delivery of maternal and child health care services a significant attribute? The case of Dale district, southern Ethiopia. BMC Health Serv Res. 2017;17(1):1–8. doi: 10.1186/s12913-017-2590-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Than KK, Mohamed Y, Oliver V, Myint T, La T, Beeson JG, Luchters S. Prevention of postpartum haemorrhage by community-based auxiliary midwives in hard-to-reach areas of Myanmar: a qualitative inquiry into acceptability and feasibility of task shifting. BMC Pregnancy Childbirth. 2017;17(1):1–10. doi: 10.1186/s12884-017-1324-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Medhanyie A, Spigt M, Kifle Y, Schaay N, Sanders D, Blanco R, GeertJan D, Berhane Y. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res. 2012;12(1):1–9. doi: 10.1186/1472-6963-12-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sakeah E, McCloskey L, Bernstein J, Yeboah-Antwi K, Mills S, Doctor HV. Can community health officer-midwives effectively integrate skilled birth attendance in the community-based health planning and services program in rural Ghana? Reprod Health. 2014;11(1):1–13. doi: 10.1186/1742-4755-11-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sarmento DR. Traditional birth attendance (TBA) in a health system: what are the roles, benefits and challenges: a case study of incorporated TBA in Timor-Leste. Asia Pac Fam Med. 2014;13(1):1–9. doi: 10.1186/s12930-014-0012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rahmawati R, Bajorek B. Peer Reviewed: A Community Health Worker-Based Program for Elderly People with Hypertension in Indonesia: A Qualitative Study, 2013. Prev Chronic Dis. 2015;12:E175. doi: 10.5888/pcd12.140530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feltner FJ, Ely GE, Whitler ET, Gross D, Dignan M. Effectiveness of community health workers in providing outreach and education for colorectal cancer screening in Appalachian Kentucky. Soc Work Health Care. 2012;51(5):430–440. doi: 10.1080/00981389.2012.657296. [DOI] [PubMed] [Google Scholar]
- 28.Hughes MM, Yang E, Ramanathan D, Benjamins MR. Community-based diabetes community health worker intervention in an underserved Chicago population. J Community Health. 2016;41(6):1249–1256. doi: 10.1007/s10900-016-0212-8. [DOI] [PubMed] [Google Scholar]
- 29.Panday S, Bissell P, Van Teijlingen E, Simkhada P. The contribution of female community health volunteers (FCHVs) to maternity care in Nepal: a qualitative study. BMC Health Serv Res. 2017;17(1):1–11. doi: 10.1186/s12913-017-2567-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Datiko DG, Lindtjørn B. Health extension workers improve tuberculosis case detection and treatment success in southern Ethiopia: a community randomized trial. PLoS ONE. 2009;4(5):e5443. doi: 10.1371/journal.pone.0005443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.le Roux KW, Almirol E, Rezvan PH, Le Roux IM, Mbewu N, Dippenaar E, Stansert-Katzen L, Baker V, Tomlinson M, Rotheram-Borus M. Community health workers impact on maternal and child health outcomes in rural South Africa–a non-randomized two-group comparison study. BMC Public Health. 2020;20(1):1–14. doi: 10.1186/s12889-020-09468-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Witmer A, Seifer SD, Finocchio L, Leslie J, O’Neil EH. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85(8 Pt 1):1055–8. [DOI] [PMC free article] [PubMed]
- 33.Wright RA. Community-oriented primary care. The cornerstone of health care reform. Jama. 1993;269(19):2544–2547. [PubMed] [Google Scholar]
- 34.Makaula P, Bloch P, Banda HT, Mbera GB, Mangani C, de Sousa A, Nkhono E, Jemu S, Muula AS. Primary Health Care in rural Malawi - a qualitative assessment exploring the relevance of the community-directed interventions approach. BMC Health Serv Res. 2012;12:328. doi: 10.1186/1472-6963-12-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Katabarwa MN, Habomugisha P, Richards FO Jr, Hopkins D. Community-directed interventions strategy enhances efficient and effective integration of health care delivery and development activities in rural disadvantaged communities of Uganda. Trop Med Int Health : TM & IH. 2005;10(4):312–21. [DOI] [PubMed]
- 36.Madon S, Malecela MN, Mashoto K, Donohue R, Mubyazi G, Michael E. The role of community participation for sustainable integrated neglected tropical diseases and water, sanitation and hygiene intervention programs: A pilot project in Tanzania. Soc Sci Med. 1982;2018(202):28–37. doi: 10.1016/j.socscimed.2018.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Okeibunor JC, Orji BC, Brieger W, Ishola G, Otolorin E, Rawlins B, Ndekhedehe EU, Onyeneho N, Fink G. Preventing malaria in pregnancy through community-directed interventions: evidence from Akwa Ibom State, Nigeria. Malaria J. 2011;10:227. doi: 10.1186/1475-2875-10-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brieger WR, Sommerfeld JU, Amazigo UV. The Potential for Community-Directed Interventions: Reaching Underserved Populations in Africa. Int Q Community Health Educ. 2015;35(4):295–316. doi: 10.1177/0272684X15592757. [DOI] [PubMed] [Google Scholar]
- 39.Braimah JA, Sano Y, Atuoye KN, Luginaah I. Access to primary health care among women: the role of Ghana’s community-based health planning and services policy. Prim Health Care Res Dev. 2019;20:e82. doi: 10.1017/S1463423619000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaplan DW, Brindis CD, Phibbs SL, Melinkovich P, Naylor K, Ahlstrand K. A comparison study of an elementary school–based health center: effects on health care access and use. Arch Pediatr Adolesc Med. 1999;153(3):235–243. doi: 10.1001/archpedi.153.3.235. [DOI] [PubMed] [Google Scholar]
- 41.Allison MA, Crane LA, Beaty BL, Davidson AJ, Melinkovich P, Kempe A. School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics. 2007;120(4):e887–e894. doi: 10.1542/peds.2006-2314. [DOI] [PubMed] [Google Scholar]
- 42.Keeton V, Soleimanpour S, Brindis CD. School-based health centers in an era of health care reform: Building on history. Curr Probl Pediatr Adolesc Health Care. 2012;42(6):132–156. doi: 10.1016/j.cppeds.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brindis CD, Klein J, Schlitt J, Santelli J, Juszczak L, Nystrom RJ. School-based health centers: Accessibility and accountability. J Adolesc Health. 2003;32(6):98–107. doi: 10.1016/s1054-139x(03)00069-7. [DOI] [PubMed] [Google Scholar]
- 44.Hutchinson P, Carton TW, Broussard M, Brown L, Chrestman S. Improving adolescent health through school-based health centers in post-Katrina New Orleans. Child Youth Serv Rev. 2012;34(2):360–368. [Google Scholar]
- 45.Paschall MJ, Bersamin M. School-based health centers, depression, and suicide risk among adolescents. Am J Prev Med. 2018;54(1):44–50. doi: 10.1016/j.amepre.2017.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Minguez M, Santelli JS, Gibson E, Orr M, Samant S. Reproductive health impact of a school health center. J Adolesc Health. 2015;56(3):338–344. doi: 10.1016/j.jadohealth.2014.10.269. [DOI] [PubMed] [Google Scholar]
- 47.Gibson EJ, Santelli JS, Minguez M, Lord A, Schuyler AC. Measuring school health center impact on access to and quality of primary care. J Adolesc Health. 2013;53(6):699–705. doi: 10.1016/j.jadohealth.2013.06.021. [DOI] [PubMed] [Google Scholar]
- 48.Bozigar M. A Cross-Sectional Survey to Evaluate Potential for Partnering With School Nurses to Promote Human Papillomavirus Vaccination. Prev Chronic Dis. 2020;17:E111. doi: 10.5888/pcd17.190451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suen J, Attrill S, Thomas JM, Smale M, Delaney CL, Miller MD. Effect of student-led health interventions on patient outcomes for those with cardiovascular disease or cardiovascular disease risk factors: a systematic review. BMC Cardiovasc Disord. 2020;20(1):1–10. doi: 10.1186/s12872-020-01602-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Atuyambe LM, Baingana RK, Kibira SP, Katahoire A, Okello E, Mafigiri DK, Ayebare F, Oboke H, Acio C, Muggaga K. Undergraduate students’ contributions to health service delivery through communitybased education. BMC Med Educ. 2016;16:123. doi: 10.1186/s12909-016-0626-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stuhlmiller CM, Tolchard B. Developing a student-led health and wellbeing clinic in an underserved community: collaborative learning, health outcomes and cost savings. BMC Nurs. 2015;14(1):1–8. doi: 10.1186/s12912-015-0083-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Campbell DJ, Gibson K, O’Neill BG, Thurston WE. The role of a student-run clinic in providing primary care for Calgary’s homeless populations: a qualitative study. BMC Health Serv Res. 2013;13(1):1–6. doi: 10.1186/1472-6963-13-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Simpson SA, Long JA. Medical student-run health clinics: important contributors to patient care and medical education. J Gen Intern Med. 2007;22(3):352–356. doi: 10.1007/s11606-006-0073-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gruen RL, O’Rourke IC, Bailie RS, d’Abbs PH, O’Brien MM, Verma N. Improving access to specialist care for remote Aboriginal communities: evaluation of a specialist outreach service. Med J Aust. 2001;174(10):507–11. [DOI] [PubMed]
- 55.Gruen RL, Weeramanthri T, Bailie R. Outreach and improved access to specialist services for indigenous people in remote Australia: the requirements for sustainability. J Epidemiol Community Health. 2002;56(7):517–521. doi: 10.1136/jech.56.7.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gruen RL, Bailie RS, Wang Z, Heard S, O’Rourke IC. Specialist outreach to isolated and disadvantaged communities: a population-based study. The Lancet. 2006;368(9530):130–8. [DOI] [PubMed]
- 57.Bond M, Bowling A, Abery A, McClay M, Dickinson E. Evaluation of outreach clinics held by specialists in general practice in England. J Epidemiol Community Health. 2000;54(2):149–156. doi: 10.1136/jech.54.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Irani M, Dixon M, Dean JD. Care closer to home: past mistakes, future opportunities. J R Soc Med. 2007;100(2):75–77. doi: 10.1258/jrsm.100.2.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bailey JJ, Black ME, Wilkin D. Specialist outreach clinics in general practice. BMJ (Clinical research ed) 1994;308(6936):1083–1086. doi: 10.1136/bmj.308.6936.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.De Roodenbeke E, Lucas S, Rouzaut A, Bana F. Outreach services as a strategy to increase access to health workers in remote and rural areas. Geneva: WHO; 2011. [PubMed] [Google Scholar]
- 61.Bowling A, Stramer K, Dickinson E, Windsor J, Bond M. Evaluation of specialists’ outreach clinics in general practice in England: process and acceptability to patients, specialists, and general practitioners. J Epidemiol Community Health. 1997;51(1):52–61. [DOI] [PMC free article] [PubMed]
- 62.Spencer N. Consultant paediatric outreach clinics–a practical step in integration. Arch Dis Child. 1993;68(4):496–500. doi: 10.1136/adc.68.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Aljasir B, Alghamdi MS. Patient satisfaction with mobile clinic services in a remote rural area of Saudi Arabia. East Mediterr Health J. 2010;16(10):1085–1090. [PubMed] [Google Scholar]
- 64.Lee EJ, O’Neal S. A mobile clinic experience: nurse practitioners providing care to a rural population. J Pediatr Health Care. 1994;8(1):12–7. [DOI] [PubMed]
- 65.Cone PH, Haley JM. Mobile clinics in Haiti, part 1: Preparing for service-learning. Nurse Educ Pract. 2016;21:1–8. doi: 10.1016/j.nepr.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 66.Diaz-Perez Mde J, Farley T, Cabanis CM. A program to improve access to health care among Mexican immigrants in rural Colorado. J Rural Health. 2004;20(3):258–264. doi: 10.1111/j.1748-0361.2004.tb00037.x. [DOI] [PubMed] [Google Scholar]
- 67.Hill C, Zurakowski D, Bennet J, Walker-White R, Osman JL, Quarles A, Oriol N. Knowledgeable Neighbors: a mobile clinic model for disease prevention and screening in underserved communities. Am J Public Health. 2012;102(3):406–410. doi: 10.2105/AJPH.2011.300472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Edgerley LP, El-Sayed YY, Druzin ML, Kiernan M, Daniels KI. Use of a community mobile health van to increase early access to prenatal care. Matern Child Health J. 2007;11(3):235–239. doi: 10.1007/s10995-006-0174-z. [DOI] [PubMed] [Google Scholar]
- 69.Peters G, Doctor H, Afenyadu G, Findley S, Ager A. Mobile clinic services to serve rural populations in Katsina State, Nigeria: perceptions of services and patterns of utilization. Health Policy Plan. 2014;29(5):642–649. doi: 10.1093/heapol/czt052. [DOI] [PubMed] [Google Scholar]
- 70.Neke NM, Gadau G, Wasem J. Policy makers’ perspective on the provision of maternal health services via mobile health clinics in Tanzania—Findings from key informant interviews. PLoS ONE. 2018;13(9):e0203588. doi: 10.1371/journal.pone.0203588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Padmadas SS, Johnson FA, Leone T, Dahal GP. Do mobile family planning clinics facilitate vasectomy use in Nepal? Contraception. 2014;89(6):557–563. doi: 10.1016/j.contraception.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 72.Macinko J, Harris MJ. Brazil’s family health strategy—delivering community-based primary care in a universal health system. N Engl J Med. 2015;372(23):2177–81. [DOI] [PubMed]
- 73.Macinko J, Lima Costa MF. Access to, use of and satisfaction with health services among adults enrolled in Brazil’s Family Health Strategy: evidence from the 2008 National Household Survey. Tropical Med Int Health. 2012;17(1):36–42. doi: 10.1111/j.1365-3156.2011.02866.x. [DOI] [PubMed] [Google Scholar]
- 74.Dourado I, Oliveira VB, Aquino R, Bonolo P, Lima-Costa MF, Medina MG, Mota E, Turci MA, Macinko J. Trends in primary health care-sensitive conditions in Brazil: the role of the Family Health Program (Project ICSAP-Brazil) Medical care. 2011;49:577–584. doi: 10.1097/MLR.0b013e31820fc39f. [DOI] [PubMed] [Google Scholar]
- 75.Aquino R, De Oliveira NF, Barreto ML. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health. 2009;99(1):87–93. doi: 10.2105/AJPH.2007.127480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chong P-N, Tang WE. Transforming primary care—the way forward with the TEAMS2 approach. Fam Pract. 2019;36(3):369–370. doi: 10.1093/fampra/cmy074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Primary Health Care Performance Initiatives (phcpi). Improvement strategies model: Population health management: Empanelment. Available at https://improvingphc.org/sites/default/files/Empanelment%20-%20v1.2%20-%20last%20updated%2012.13.2019.pdf. Accessed on 18 March 2022.
- 78.McGough P, Chaudhari V, El-Attar S, Yung P. A health system’s journey toward better population health through empanelment and panel management. Healthcare. 2018;6(66):1–9. [DOI] [PMC free article] [PubMed]
- 79.Bearden T, Ratcliffe HL, Sugarman JR, Bitton A, Anaman LA, Buckle G, Cham M, Quan DCW, Ismail F, Jargalsaikhan B. Empanelment: A foundational component of primary health care. Gates Open Res. 2019;3:1654. doi: 10.12688/gatesopenres.13059.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hsiao WC. Unmet health needs of two billion: is community financing a solution? 2001. [Google Scholar]
- 81.Wang W, Temsah G, Mallick L. The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health Policy Plan. 2017;32(3):366–375. doi: 10.1093/heapol/czw135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Atnafu DD, Tilahun H, Alemu YM. Community-based health insurance and healthcare service utilisation, North-West, Ethiopia: a comparative, cross-sectional study. BMJ Open. 2018;8(8):e019613. doi: 10.1136/bmjopen-2017-019613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.USAID. Ethiopia’s Community-based Health Insurance: A Step on the Road to Universal Health Coverage. Available at https://www.hfgproject.org/ethiopias-community-based-health-insurance-step-road-universal-health-coverage/. Accessed on 18 March 2022.
- 84.Blanchet NJ, Fink G, Osei-Akoto I. The effect of Ghana’s National Health Insurance Scheme on health care utilisation. Ghana Med J. 2012;46(2):76–84. [PMC free article] [PubMed] [Google Scholar]
- 85.Nshakira-Rukundo E, Mussa EC, Nshakira N, Gerber N, von Braun J. Impact of community-based health insurance on utilisation of preventive health services in rural Uganda: a propensity score matching approach. Int J Health Econ Manag. 2021;21(2):203–227. doi: 10.1007/s10754-021-09294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mwaura JW, Pongpanich S. Access to health care: the role of a community based health insurance in Kenya. Pan Afr Med J. 2012;12(1):35. [PMC free article] [PubMed] [Google Scholar]
- 87.Jutting JP. The Impact Of Health Insurance On The Access To Health Care And Financial Protection In Rural Developing Countries: The Example of Senegal. HNP discussion paper series;. World Bank, Washington, DC. © World Bank. 2011. https://openknowledge.worldbank.org/handle/10986/13774. License: CC BY 3.0 IGO.
- 88.Balamiento NC. The impact of social health insurance on healthcare utilization outcomes: evidence from the indigent program of the Philippine National Health Insurance. International Institute of Social Studies. 2018. Available at https://thesis.eur.nl/pub/46445/Balamiento,%20Neeanne_MA_2017_18%20_ECD.pdf. Accessed 30 Nov 2022.
- 89.Farrell CM, Gottlieb A. The effect of health insurance on health care utilization in the justice-involved population: United States, 2014–2016. Am J Public Health. 2020;110(S1):S78–S84. doi: 10.2105/AJPH.2019.305399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Thuong NTT. Impact of health insurance on healthcare utilisation patterns in Vietnam: a survey-based analysis with propensity score matching method. BMJ Open. 2020;10(10):e040062. doi: 10.1136/bmjopen-2020-040062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Custodio R, Gard AM, Graham G. Health information technology: addressing health disparity by improving quality, increasing access, and developing workforce. J Health Care Poor Underserved. 2009;20(2):301–307. doi: 10.1353/hpu.0.0142. [DOI] [PubMed] [Google Scholar]
- 92.Meier CA, Fitzgerald MC, Smith JM. eHealth: extending, enhancing, and evolving health care. Annu Rev Biomed Eng. 2013;15:359–382. doi: 10.1146/annurev-bioeng-071812-152350. [DOI] [PubMed] [Google Scholar]
- 93.Anstey Watkins JOT, Goudge J, Gomez-Olive FX, Griffiths F. Mobile phone use among patients and health workers to enhance primary healthcare: A qualitative study in rural South Africa. Soc Sci Med. 1982;2018(198):139–147. doi: 10.1016/j.socscimed.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 94.Kuntalp M, Akar O. A simple and low-cost Internet-based teleconsultation system that could effectively solve the health care access problems in underserved areas of developing countries. Comput Methods Programs Biomed. 2004;75(2):117–126. doi: 10.1016/j.cmpb.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 95.Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, Ruggiero KJ. mHealth: a mechanism to deliver more accessible, more effective mental health care. Clin Psychol Psychother. 2014;21(5):427–436. doi: 10.1002/cpp.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bashshur RL, Shannon GW, Krupinski EA, Grigsby J, Kvedar JC, Weinstein RS, Sanders JH, Rheuban KS, Nesbitt TS, Alverson DC, et al. National telemedicine initiatives: essential to healthcare reform. Telemed J E Health. 2009;15(6):600–610. doi: 10.1089/tmj.2009.9960. [DOI] [PubMed] [Google Scholar]
- 97.Norton SA, Burdick AE, Phillips CM, Berman B. Teledermatology and underserved populations. Arch Dermatol. 1997;133(2):197–200. [PubMed] [Google Scholar]
- 98.Raza T, Joshi M, Schapira RM, Agha Z. Pulmonary telemedicine–a model to access the subspecialist services in underserved rural areas. Int J Med Informatics. 2009;78(1):53–59. doi: 10.1016/j.ijmedinf.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 99.Shouneez YH. Smartphone hearing screening in mHealth assisted community-based primary care. UPSpace Institutional Repository, Department of Liberary Service. Dissertation (MCommPath)--University of Pretoria. 2016. Available at http://hdl.handle.net/2263/53477. Accessed 17 Mar 2022.
- 100.Marcin JP, Ellis J, Mawis R, Nagrampa E, Nesbitt TS, Dimand RJ. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics. 2004;113(1 Pt 1):1–6. doi: 10.1542/peds.113.1.1. [DOI] [PubMed] [Google Scholar]
- 101.Olu O, Muneene D, Bataringaya JE, Nahimana M-R, Ba H, Turgeon Y, Karamagi HC, Dovlo D. How can digital health technologies contribute to sustainable attainment of universal health coverage in Africa? A perspective. Front Public Health. 2019;7:341. doi: 10.3389/fpubh.2019.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ryan MH, Yoder J, Flores SK, Soh J, Vanderbilt AA. Using health information technology to reach patients in underserved communities: A pilot study to help close the gap with health disparities. Global J Health Sci. 2016;8(6):86. doi: 10.5539/gjhs.v8n6p86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Buckwalter KC, Davis LL, Wakefield BJ, Kienzle MG, Murray MA. Telehealth for elders and their caregivers in rural communities. Fam Community Health. 2002;25(3):31–40. doi: 10.1097/00003727-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 104.WHO Regional Committee for Africa. Promoting the role of traditional medicine in health systems: a strategy for the African Region. World Health Organization. Regional Office for Africa. Available at http://www.who.int/iris/handle/10665/95467..
- 105.Mishra SR, Neupane D, Kallestrup P. Integrating complementary and alternative medicine into conventional health care system in developing countries: an example of Amchi. J Evid-Based Complementary Altern Med. 2015;20(1):76–79. doi: 10.1177/2156587214547575. [DOI] [PubMed] [Google Scholar]
- 106.Mbwambo ZH, Mahunnah RL, Kayombo EJ. Traditional health practitioner and the scientist: bridging the gap in contemporary health research in Tanzania. Tanzan Health Res Bull. 2007;9(2):115–120. doi: 10.4314/thrb.v9i2.14313. [DOI] [PubMed] [Google Scholar]
- 107.Poudyal AK, Jimba M, Murakami I, Silwal RC, Wakai S, Kuratsuji T. A traditional healers’ training model in rural Nepal: strengthening their roles in community health. Trop Med Int Health : TM & IH. 2003;8(10):956–60. [DOI] [PubMed]
- 108.Payyappallimana U. Role of Traditional Medicine in Primary Health Care: An Overview of Perspectives and Challenges. Yokohama J Social Sciences. 2009;14(6):723–743. [Google Scholar]
- 109.Kange’ethe SM. Traditional healers as caregivers to HIV/AIDS clients and other terminally challenged persons in Kanye community home-based care programme (CHBC), Botswana. SAHARA J. 2009;6(2):83–91. [DOI] [PMC free article] [PubMed]
- 110.Habtom GK. Integrating traditional medical practice with primary healthcare system in Eritrea. J Complement Integr Med. 2015;12(1):71–87. doi: 10.1515/jcim-2014-0020. [DOI] [PubMed] [Google Scholar]
- 111.Ejaz I, Shaikh BT, Rizvi N. NGOs and government partnership for health systems strengthening: a qualitative study presenting viewpoints of government, NGOs and donors in Pakistan. BMC Health Serv Res. 2011;11(1):1–7. doi: 10.1186/1472-6963-11-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wu FS. International non-governmental actors in HIV/AIDS prevention in China. Cell Res. 2005;15(11):919–922. doi: 10.1038/sj.cr.7290369. [DOI] [PubMed] [Google Scholar]
- 113.Biermann O, Eckhardt M, Carlfjord S, Falk M, Forsberg BC. Collaboration between non-governmental organizations and public services in health–a qualitative case study from rural Ecuador. Glob Health Action. 2016;9(1):32237. doi: 10.3402/gha.v9.32237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mercer A, Khan MH, Daulatuzzaman M, Reid J. Effectiveness of an NGO primary health care programme in rural Bangladesh: evidence from the management information system. Health Policy Plan. 2004;19(4):187–198. doi: 10.1093/heapol/czh024. [DOI] [PubMed] [Google Scholar]
- 115.Baqui AH, Rosecrans AM, Williams EK, Agrawal PK, Ahmed S, Darmstadt GL, Kumar V, Kiran U, Panwar D, Ahuja RC. NGO facilitation of a government community-based maternal and neonatal health programme in rural India: improvements in equity. Health Policy Plan. 2008;23(4):234–243. doi: 10.1093/heapol/czn012. [DOI] [PubMed] [Google Scholar]
- 116.Ricca J, Kureshy N, LeBan K, Prosnitz D, Ryan L. Community-based intervention packages facilitated by NGOs demonstrate plausible evidence for child mortality impact. Health Policy Plan. 2014;29(2):204–216. doi: 10.1093/heapol/czt005. [DOI] [PubMed] [Google Scholar]
- 117.Ahmed N, DeRoeck D, Sadr-Azodi N. Private sector engagement and contributions to immunisation service delivery and coverage in Sudan. BMJ Glob Health. 2019;4(2):e001414. doi: 10.1136/bmjgh-2019-001414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Edimond BJ. The Contribution of Non-Governmental Organizations in Delivery of Basic Health Services in Partnership with Local Government. Doctoral Dissertation, Uganda Martyrs University. 2014. [Google Scholar]
- 119.Chand S, Patterson J: Faith-Based Models for Improving Maternal and Newborn Health. IMA World Health and ActionAid International USA, 2007 Available at https://imaworldhealthorg/wp-content/uploads/2014/06/faith_based_models_for_improving_maternal_and_newborn_health.pdf
- 120.Magezi V. Churchdriven primary health care: Models for an integrated church and community primary health care in Africa (a case study of the Salvation Army in East Africa). HTS Teologiese Studies/ Theological Studies. 2018;74(2):4365.
- 121.Villatoro AP, Dixon E, Mays VM. Faith-based organizations and the Affordable Care Act: Reducing Latino mental health care disparities. Psychol Serv. 2016;13(1):92–104. doi: 10.1037/a0038515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Levin J. Faith-based initiatives in health promotion: history, challenges, and current partnerships. American journal of health promotion : AJHP. 2014;28(3):139–41. [DOI] [PubMed]
- 123.Green A, Shaw J, Dimmock F, Conn C. A shared mission? Changing relationships between government and church health services in Africa. Int J Health Plann Manage. 2002;17(4):333–353. doi: 10.1002/hpm.685. [DOI] [PubMed] [Google Scholar]
- 124.Bandy G, Crouch A. Building from common foundations : the World Health Organization and faith-based organizations in primary healthcare. World Health Organization; 2008. Available at https://apps.who.int/iris/handle/10665/43884. Accessed 16 Mar 2022.
- 125.Zahnd WE, Jenkins WD, Shackelford J, Lobb R, Sanders J, Bailey A. Rural cancer screening and faith community nursing in the era of the Affordable Care Act. J Health Care Poor Underserved. 2018;29(1):71–80. doi: 10.1353/hpu.2018.0008. [DOI] [PubMed] [Google Scholar]
- 126.Wagle K. Primary Health Care (PHC): History, Principles, Pillars, Elements & Challenges. Global Health, 2020. Available at https://www.publichealthnotes.com/primary-health-care-phc-history-principles-pillars-elements-challenges/. Accessed 4 June 2022.
- 127.Bhatt J, Bathija P. Ensuring access to quality health care in vulnerable communities. Acad Med. 2018;93(9):1271. doi: 10.1097/ACM.0000000000002254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Arvey SR, Fernandez ME. Identifying the core elements of effective community health worker programs: a research agenda. Am J Public Health. 2012;102(9):1633–1637. doi: 10.2105/AJPH.2012.300649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. Community health needs assessment: potential for population health improvement. Popul Health Manag. 2016;19(3):178–186. doi: 10.1089/pop.2015.0075. [DOI] [PubMed] [Google Scholar]
- 130.Chudgar RB, Shirey LA, Sznycer-Taub M, Read R, Pearson RL, Erwin PC. Local health department and academic institution linkages for community health assessment and improvement processes: a national overview and local case study. J Public Health Manag Pract. 2014;20(3):349–355. doi: 10.1097/PHH.0b013e31829dc26b. [DOI] [PubMed] [Google Scholar]
- 131.Desta FA, Shifa GT, Dagoye DW, Carr C, Van Roosmalen J, Stekelenburg J, Nedi AB, Kols A, Kim YM. Identifying gaps in the practices of rural health extension workers in Ethiopia: a task analysis study. BMC Health Serv Res. 2017;17(1):1–9. doi: 10.1186/s12913-017-2804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lehmann U, Sanders D. Community health workers: what do we know about them. The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers Geneva: World Health Organization; 2007. Available at https://www.hrhresourcecenter.org/node/1587.html. Accessed 17 Mar 2022.
- 133.Chen N, Raghavan M, Albert J, McDaniel A, Otiso L, Kintu R, West M, Jacobstein D. The community health systems reform cycle: strengthening the integration of community health worker programs through an institutional reform perspective. Global Health: Sci Practice. 2021;9(Supplement 1):S32–S46. doi: 10.9745/GHSP-D-20-00429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Roser M, Ortiz-Ospina E: Global rise of education. Our World in Data 2017. Available at https://ourworldindata.org/global-rise-of-education. Accessed on 29 May 2019.
- 135.Santelli J, Morreale M, Wigton A, Grason H. School health centers and primary care for adolescents: a review of the literature. J Adolesc Health. 1996;18(5):357–366. doi: 10.1016/1054-139X(96)00025-0. [DOI] [PubMed] [Google Scholar]
- 136.Wade TJ, Mansour ME, Guo JJ, Huentelman T, Line K, Keller KN. Access and utilization patterns of school-based health centers at urban and rural elementary and middle schools. Public Health Reports. 2008;123(6):739–750. doi: 10.1177/003335490812300610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Johnson I, Hunter L, Chestnutt IG. Undergraduate students’ experiences of outreach placements in dental secondary care settings. Eur J Dent Educ. 2012;16(4):213–217. doi: 10.1111/j.1600-0579.2012.00744.x. [DOI] [PubMed] [Google Scholar]
- 138.Ndira S, Ssebadduka D, Niyonzima N, Sewankambo N, Royall J. Tackling malaria, village by village: a report on a concerted information intervention by medical students and the community in Mifumi Eastern Uganda. Afr Health Sci. 2014;14(4):882–888. doi: 10.4314/ahs.v14i4.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Frakes K-a, Brownie S, Davies L, Thomas JB, Miller M-E, Tyack Z. Capricornia Allied Health Partnership (CAHP): a case study of an innovative model of care addressing chronic disease through a regional student-assisted clinic. Aust Health Rev. 2014;38(5):483–486. doi: 10.1071/AH13177. [DOI] [PubMed] [Google Scholar]
- 140.Frakes KA, Brownie S, Davies L, Thomas J, Miller ME, Tyack Z. The sociodemographic and health-related characteristics of a regional population with chronic disease at an interprofessional student-assisted clinic in Q ueensland C apricornia A llied H ealth P artnership. Aust J Rural Health. 2013;21(2):97–104. doi: 10.1111/ajr.12017. [DOI] [PubMed] [Google Scholar]
- 141.Frakes K-A, Tyzack Z, Miller M, Davies L, Swanston A, Brownie S. The Capricornia Project: Developing and implementing an interprofessional student-assisted allied health clinic. 2011. [Google Scholar]
- 142.Frakes K-A, Brownie S, Davies L, Thomas J, Miller M-E, Tyack Z. Experiences from an interprofessional student-assisted chronic disease clinic. J Interprof Care. 2014;28(6):573–575. doi: 10.3109/13561820.2014.917404. [DOI] [PubMed] [Google Scholar]
- 143.Schutte T, Tichelaar J, Dekker RS, van Agtmael MA, de Vries TP, Richir MC. Learning in student-run clinics: A systematic review. Med Educ. 2015;49(3):249–263. doi: 10.1111/medu.12625. [DOI] [PubMed] [Google Scholar]
- 144.Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. The Lancet. 2011;377(9779):1778–1797. doi: 10.1016/S0140-6736(11)60054-8. [DOI] [PubMed] [Google Scholar]
- 145.Rocha R, Soares RR. Evaluating the impact of community-based health interventions: evidence from Brazil’s Family Health Program. Health Econ. 2010;19(S1):126–58. [DOI] [PubMed]
- 146.Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ (Clinical research ed) 2014;349:g4014. doi: 10.1136/bmj.g4014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Harris M. Brazil’s Family Health Programme: A cost effective success that higher income countries could learn from. BMJ: Br Med J. 2010;341(7784):1171–2.
- 148.Starfield B. Is primary care essential? The lancet. 1994;344(8930):1129–1133. doi: 10.1016/s0140-6736(94)90634-3. [DOI] [PubMed] [Google Scholar]
- 149.Donfouet HPP, Mahieu P-A. Community-based health insurance and social capital: a review. Heal Econ Rev. 2012;2(1):1–5. doi: 10.1186/2191-1991-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Zhang L, Wang H, Wang L, Hsiao W. Social capital and farmer’s willingness-to-join a newly established community-based health insurance in rural China. Health Policy. 2006;76(2):233–42. [DOI] [PubMed]
- 151.Donfouet HPP. Essombè J-RE, Mahieu P-A, Malin E: Social capital and willingness-to-pay for community-based health insurance in rural Cameroon. Global J Health Sci. 2011;3(1):142. doi: 10.1007/s10754-011-9097-3. [DOI] [PubMed] [Google Scholar]
- 152.Grunau J. Exploring people’s motivation to join or not to join the community-based health insurance’Sina Passenang’in Sotouboua, Togo. 2013.
- 153.Gitahi JW. Innovative Healthcare Financing and Equity through Community Based Health Insurance Schemes (CBHHIS) In Kenya. United States International University-Africa Digital Repository. Available at http://erepo.usiu.ac.ke/11732/3654. Accessed 18 May 2022.
- 154.Carrin G, Waelkens MP, Criel B. Community-based health insurance in developing countries: a study of its contribution to the performance of health financing systems. Tropical Med Int Health. 2005;10(8):799–811. doi: 10.1111/j.1365-3156.2005.01455.x. [DOI] [PubMed] [Google Scholar]
- 155.Umeh CA, Feeley FG. Inequitable access to health care by the poor in community-based health insurance programs: a review of studies from low-and middle-income countries. Global Health: Science And Practice. 2017;5(2):299–314. doi: 10.9745/GHSP-D-16-00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Odebiyi AI. Western trained nurses’ assessment of the different categories of traditional healers in southwestern Nigeria. Int J Nurs Stud. 1990;27(4):333–42. [DOI] [PubMed]
- 157.Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med : AJTCAM. 2011;8(5 Suppl):115–23. [DOI] [PMC free article] [PubMed]
- 158.Taye OR. Yoruba Traditional Medicine and the Challenge of Integration. The J Pan Afr Studies. 2009;3(3):73–90. [Google Scholar]
- 159.Konadu K. Medicine and Anthropology in Twentieth Century Africa: Akan Medicine and Encounters with (Medical) Anthropology. African Studies Quarterly. 2008;10(2 & 3).
- 160.Benzie IF, Wachtel-Galor S: Herbal medicine: biomolecular and clinical aspects. 2nd Ed. 2011. Available at https://www.crcpress.com/Herbal-Medicine-Biomolecular-and-Clinical-Aspects-Second-Edition/Benzie-Wachtel-Galor/p/book/9781439807132. Accessed 21 May 2022. [PubMed]
- 161.Ejughemre U. Donor support and the impacts on health system strengthening in sub-saharan africa: assessing the evidence through a review of the literature. Am J Public Health Res. 2013;1(7):146–151. [Google Scholar]
- 162.Seppey M, Ridde V, Touré L, Coulibaly A. Donor-funded project’s sustainability assessment: a qualitative case study of a results-based financing pilot in Koulikoro region. Mali Globalization and health. 2017;13(1):1–15. [DOI] [PMC free article] [PubMed]
- 163.Shaw RP, Wang H, Kress D, Hovig D. Donor and domestic financing of primary health care in low income countries. Health Systems & Reform. 2015;1(1):72–88. doi: 10.1080/23288604.2014.996413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gotsadze G, Chikovani I, Sulaberidze L, Gotsadze T, Goguadze K, Tavanxhi N. The challenges of transition from donor-funded programs: results from a theory-driven multi-country comparative case study of programs in Eastern Europe and Central Asia supported by the Global Fund. Global Health: Science and Practice. 2019;7(2):258–272. doi: 10.9745/GHSP-D-18-00425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ascroft J, Sweeney R, Samei M, Semos I, Morgan C. Strengthening church and government partnerships for primary health care delivery in Papua New Guinea: Lessons from the international experience. Health policy and health finance knowledge hub Working paper series. 2011(16).
- 166.Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- 167.Olivier J, Wodon Q. The role of faith-inspired health care providers in Sub-Saharan Africa and public private partnerships: Strengthening the Evidence for faith-inspired health engagement in Africa, Volume 1. Health, Nutrition and Population (HNP) Discussion Paper Series 76223v1. Available at https://documents1.worldbank.org/curated/en/851911468203673017. Accessed 20 May 2022.
- 168.Schumann C, Stroppa A, Moreira-Almeida A. The contribution of faith-based health organisations to public health. Int Psychiatry. 2011;8(3):62–64. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Searchstrategy. MEDLINE (PubMed).
Additional file 2: Appendix 2: Table A1.Description of full-text articles which discussed community health programs or community-directed interventions as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 3: Appendix 3: Table A2.Description of full-text articles which discussed school-based healthcareservices as a strategy to improve PHCservice delivery in rural communities.
Additional file 4: Appendix 4: Table A3. Description of full-text articles which discussed student-led healthcareservices as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 5: Appendix 5: Table A4. Descriptionof full-text articles which discussed outreach services or mobile clinics as astrategy to improve PHC service delivery in ruralcommunities.
Additional file 6: Appendix 6: Table A5.Description of full-text articles which discussed family health program as astrategy to improve PHC service delivery in rural,communities.
Additional file 7: Appendix 7: Table A6. Description of full-text articles whichdiscussed empanelment as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 8: Appendix 9: Table A8.Description of full-text articles which discussed telemedicine or mobile healthas a strategy to improve PHC service delivery in ruralcommunities.
Additional file 9: Appendix 8: Table A7.Description of full-text articles which discussed community health funding schemes as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 10: Appendix 10: Table A9.Description of full-text articles which discussed promoting the role of workingwith traditional healers as a strategy toimprove PHC service delivery in rural communities.
Additional file 11: Appendix 11: Table A10.Description of full-text articles which discussed working with non-profitprivate sectors and non-governmental organizations as a strategy to improve PHC service delivery in rural communities.
Data Availability Statement
All the extracted data are included in the manuscript.