Abstract
Background
Diabetes was commonly seen in chronic total occlusion (CTO) patients but data regarding the impact of successful percutaneous coronary intervention (PCI) on clinical outcome of CTO patients with diabetes was controversial. And importantly, no studies have compared quality of life (QOL) after CTO-PCI in patients with and without diabetes.
Methods
Consecutive patients undergoing elective CTO-PCI were prospectively enrolled from Apr. 2018 to May 2021. Patients were subdivided into 2 groups: Diabetes and No Diabetes. Detailed baseline characteristics, assessment of symptoms and QOL, angiographic and procedural details, in-hospital complications, and 1 month and 1 year follow-up data were collected. These data were analyzed accordingly for risk predictors of clinical outcome in patients who have diabetes and received successful CTO-PCI.
Results
A total of 1076 patients underwent CTO-PCI attempts. Diabetes was present in 374 (34.76%) patients, who had more hypertension, previous PCI and stroke. Regarding the coronary lesions, diabetic patients suffered more LCX lesion, multivessel disease, number of lesions per patient, blunt stump, calcification and higher J-CTO score (p < 0.05). In-hospital major adverse cardiac event (MACE) (4.13% vs. 5.35%; p = 0.362) was similar in the two groups. At 1 month and 1 year follow-up after successful CTO-PCI, the incidence of MACE and all-cause mortality were also similar in the two groups (p > 0.05). Number of lesions per patient was an independent risk factor of MACE and all-cause mortality (p < 0.001) 1 year after successful CTO-PCI. Symptom and QOL were markedly improved regardless of diabetes both at 1 month and 1 year follow-up, and importantly, patients with diabetes showed similar degrees of improvement to those without diabetes (P > 0.05).
Conclusions
Successful CTO-PCI could represent an effective strategy improving clinical outcome, symptoms and QOL in CTO patients with diabetes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-022-01708-0.
Keywords: Chronic total occlusion, Diabetes, Clinical outcomes, Symptoms, Quality of life
Introduction
Chronic total occlusion (CTO) accounted for approximately 13–41% of coronary artery disease (CAD) patients undergoing coronary angiography (CAG) [1, 2]. It has been reported that successful percutaneous coronary intervention (PCI) of CTO (CTO-PCI) could prolong long-term survival, relieve angina and dyspnea, and improve the ventricular function compared to failed revascularization [3–6]. Diabetes was a well-known CAD risk factor, and associated with a greater atherosclerotic burden, including diffused CAD, multivessel disease, and heavy coronary artery calcifications [7, 8]. Among the CTO patients, diabetes is relatively common, taking up approximately 30–40% [9, 10]. For CTO patients with diabetes, data regarding the clinical outcome after successful revascularization were controversial. Some reported that the incidence of long-term major adverse cardiac event (MACE) was higher in patients with diabetes [11, 12] while some found no obvious difference of long-term MACE in patients with or without diabetes [13–15]. Furthermore, as an important indicator for medical decision-making and a predictor for treatment success, quality of life (QOL) is therefore of prognostic importance. Especially for diabetic patients, QOL has been recognized as the ultimate goal [16, 17], while hitherto, there is no data regarding whether successful CTO-PCI improves QOL of CTO patients with diabetes. Therefore, in the present study, we aimed to comprehensively investigate the effect of successful CTO-PCI on clinical outcomes, symptoms and QOL, and to identify the variables associated with the incidence of the MACE and all-cause mortality in CTO patients with diabetes.
Methods
Patient population
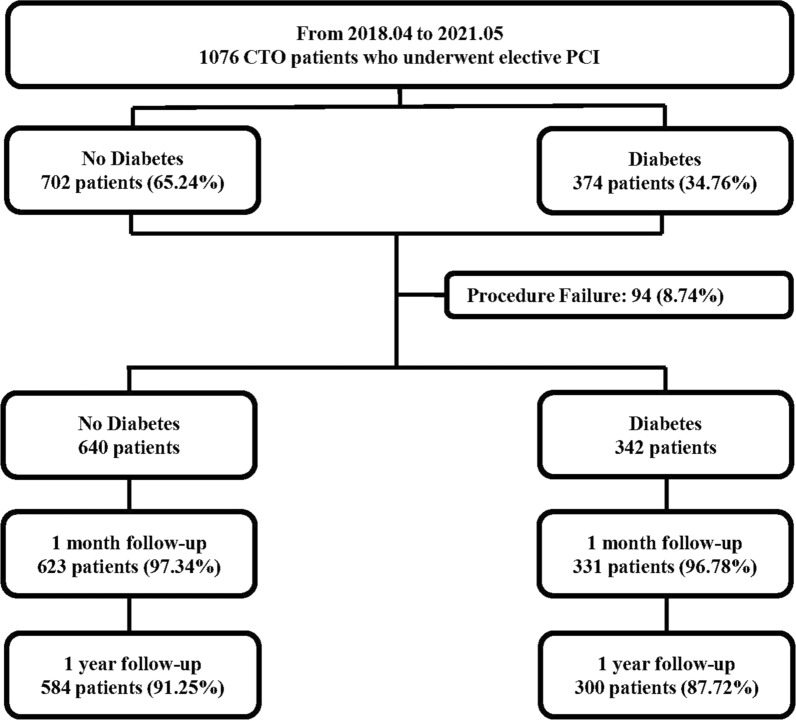
A total of 1076 patients who underwent elective PCI for at least 1 CTO lesion from Apr. 2018 to May 2021 at Xijing Hospital were prospectively and consecutively enrolled in this analysis (Fig. 1). All the procedures were performed by one CTO team of Xijing Hospital which was led by Dr. Chengxiang Li. Importantly, all the procedures were completed by Dr. Li or under his guidance. Patients with acute myocardial infarctions (ST elevation or non-ST elevation), cardiogenic shock, and unstable hemodynamics were excluded. Indications for coronary revascularization were based on angina symptoms or on noninvasive imaging (coronary artery CT). The decision to the revascularization strategy (PCI or CABG, and lesions to be revascularized) for each patient rested with the cardiac surgeon and internationalists in our center. In case of surgical indication rejected by the patients, PCI was proposed if considered to be feasible by the international operator. Study population was divided into two groups based on whether or not the diabetes was present: diabetes (374, 34.76%) and no diabetes (702, 65.24%). The study was approved by the Ethics Committee of Xijing Hospital, the Fourth Military Medical University, and each subject was provided with informed consent before recruitment (KY20172019-1).
Fig. 1.
Flowchart of the Study Population. CTO chronic total occlusion, PCI percutaneous coronary intervention
Definition and endpoints
Coronary CTOs were defined as angiographic evidence of total occlusions with thrombolysis in myocardial infarction flow grade 0 within a major epicardial coronary artery of at least 2.5 mm, and estimated duration of at least 3 months. Non-CTO was defined as diameter stenosis 50% for left main (LM) and 70% for non-LM CAD within a vessel diameter ≥ 2.5 mm [18]. Diabetes was defined as a fasting plasma glucose level ≥ 7.0 mmol/L, or a plasma glucose level ≥ 11.1 mmol/L at 2 h after an oral glucose tolerance test, or glycated hemoglobin ≥ 6.5% on more than two occasions, or random plasma glucose value ≥ 11.1 mmol/L in presence of classic symptoms of hyperglycemia, or the current use of hypoglycemic agents or insulin [19]. Revascularization was considered for angiographically significant stenosis (≥ 70% diameter reduction by visual assessment) and functionally significant stenosis (fractional flow reserve measurement < 0.80). The complete revascularization was defined as revascularization in all major significantly diseased epicardial vessels during the same hospitalization. The J-CTO (Multicenter CTO Registry in Japan) [20]. Procedural success was defined as successful CTO revascularization with achievement of < 30% residual diameter stenosis within the treated segment and restoration of TIMI flow grade 3 antegrade, and without any in-hospital MACE. In-hospital MACE included any of the following adverse events prior to hospital discharge: all-cause mortality, nonfatal myocardial infarction (MI), and clinically driven revascularization. Major bleeding was defined as Bleeding Academic Research Consortium (BARC) type bleeding of least 3 [21].
Follow-up
Patients were followed up by clinical visits or telephone interviews at 1 month and 1 year after CTO-PCI. The primary outcomes of interest for this study were the occurrence of MACE. MACE was defined as the composite of all-cause mortality, nonfatal MI and clinically driven revascularization by either PCI or CABG. The diagnosis of nonfatal MI was based on ECG findings (new Q waves in ≥ 2 contiguous leads) and cardiac biomarker elevations (more than 3 times the upper limit of creatine kinase or creatine kinase myocardial band in 2 plasma samples) [22]. Secondary endpoints were the change of symptoms and QOL across the three groups. In addition, details regarding MACE occurrence and health status assessment were obtained from hospital re-admission records, telephone contact with the referring physician, or outpatient visits.
Symptoms assessment
Dyspnea was assessed at baseline, 1 month, and 1 year after CTO-PCI according to New York Heart Association (NYHA) functional class and Rose Dyspnea Scale (RDS), respectively. The RDS is a 4-item questionnaire to assesses patients’ level of dyspnea with common activities [23]. Each activity associated with dyspnea is assigned 1 point, where RDS scores range from 0 to 4, with a score of 0 indicating no dyspnea and increased scores indicating greater dyspnea.
The angina status of the patient was assessed according to the Seattle Angina Questionnaire (SAQ) [24] at baseline, 1 month, and 1 year after CTO-PCI. SAQ consists of 19 items that measure 5 dimensions: angina frequency (AF); angina stability (AS); disease perception (DP); physical limitation (PL) and treatment satisfaction (TS). All items use 5-point descriptive scales and scores are calculated by totalling all the single scores within each group and transforming them to a scale of 0 to 100, where 0 is the worst and 100 is the best.
QOL assessment
Quality of life was assessed by means of the European Quality of Life-5 Dimensions (EQ-5D) and SF-12 questionnaire at baseline, 1 month, and 1 year after CTO-PCI. The EQ-5D assesses 5 dimensions of general health (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) with a 3-level scale. These scores can then be converted to utilities with an algorithm developed for Japan population. Utilities are preference-weighted health status assessments with scores that range from − 0.11 to 1.00, with 1.00 representing the perfectest health and − 0.11 representing the poorest health [25, 26].
The SF-12 is a shortened version of the SF-36, including 12 questions, with three to five answer categories each (Likert scale). The instrument covers eight dimensions: general health, physical functioning, role physical, bodily pain, vitality, social functioning, role emotional and mental health. Both a physical functioning component score (PCS) and a mental functioning component score (MCS), ranging between 0 and 100, can be calculated by using a scoring algorithm. Lower scores represent worse and higher scores represent better self-perceived HRQOL outcomes [27].
Statistical analysis
The continuous variables are presented as mean ± SD or as medians and interquartile ranges. The categorical variables are presented as percentages. The continuous variables were compared using the t test or Mann–Whitney U test where appropriate, and categorical variables were compared using the chi-square or fisher’s exact test. The all-cause mortality was analyzed using the Kaplan Meier method. Logistic regression analysis was used for univariate and multivariate analysis. A 2-sided p-value of < 0.05 was considered significant. The IBM SPSS Statistics 25 and STATA MP 14.0 software were used for calculations.
Results
A total of 1076 patients underwent CTO-PCI were prospectively and consecutively enrolled in the study, who were subdivided into 2 groups: diabetes (374, 34.76%), and no diabetes (702, 65.24%, Fig. 1). Compared to patients without diabetes, those with diabetes had more hypertension (58.83% vs. 67.11%; p = 0.008), previous PCI (48.15% vs. 55.61%; p = 0.020) and stroke (10.40% vs. 15.24%; p = 0.020), lower diastolic blood pressure, hemoglobin, CrCL, CK, and CK-MB level and higher FPG, NT-proBNP level (p < 0.05, Table 1). Additionally, the proportion of LCX lesion (68.80% vs. 81.02%; p < 0.001), multivessel disease (83.62% vs. 91.98%; p < 0.001), number of lesions per patient (2.40 ± 0.98 vs. 2.61 ± 0.93; p = 0.001), blunt stump (66.00% vs. 72.19%; p = 0.037), calcification (30.20% vs. 38.50%; p = 0.006) and J-CTO score (2.11 ± 1.13 vs. 2.31 ± 1.15; p = 0.005) were significantly higher in patients with diabetes than those without diabetes (Table 2). The incidence of in-hospital MACE was similar in patients with diabetes or not (p > 0.05, Table 3).
Table 1.
Baseline Characteristics
| No Diabetes | Diabetes | p Value | |
|---|---|---|---|
| (n = 702) | (n = 374) | ||
| Age, yrs | 60.23 ± 10.78 | 61.35 ± 10.55 | 0.101 |
| Males, n% | 609(86.75) | 333(89.04) | 0.280 |
| BMI, kg/m2 | 25.25 ± 3.25 | 25.11 ± 3.03 | 0.474 |
| SBP, mmHg | 127.70 ± 20.23 | 126.96 ± 19.25 | 0.560 |
| DBP, mmHg | 72.87 ± 12.19 | 71.19 ± 11.99 | 0.031 |
| Smoking, n% | 275(39.17) | 125(33.42) | 0.063 |
| Hypertension, n% | 413(58.83) | 251(67.11) | 0.008 |
| Previous MI, n% | 298(42.45) | 145(38.77) | 0.243 |
| Previous PCI, % | 338(48.15) | 208(55.61) | 0.020 |
| Previous CABG, % | 20(2.85) | 15(4.01) | 0.306 |
| Previous stroke, n% | 73(10.40) | 57(15.24) | 0.020 |
| Chronic pulmonary disease, n% | 13(1.85) | 9(2.41) | 0.540 |
| Peripheral artery disease, n% | 14(1.99) | 13(3.48) | 0.139 |
| Family history of CHD, n% | 23(3.28) | 21(5.61) | 0.065 |
| WBC, *109/L | 6.98 ± 2.09 | 6.94 ± 1.97 | 0.783 |
| Platelet, *109/L | 208.63 ± 64.78 | 206.42 ± 65.43 | 0.596 |
| Hemoglobin, g/L | 141.24 ± 19.35 | 136.64 ± 18.96 | < 0.001 |
| FPG, mmol/ L | 5.55 ± 1.82 | 8.09 ± 3.53 | < 0.001 |
| TC, mmol/ L | 3.44 ± 1.06 | 3.28 ± 0.91 | 0.008 |
| TG, mmol/ L | 1.67 ± 1.02 | 1.66 ± 1.23 | 0.917 |
| LDL-C, mmol/ L | 1.96 ± 0.93 | 1.78 ± 0.77 | 0.001 |
| HDL-C, mmol/ L | 1.03 ± 0.42 | 0.98 ± 0.34 | 0.087 |
| ALT, U/L | 33.56 ± 47.35 | 28.73 ± 25.79 | 0.068 |
| AST, U/L | 29.35 ± 43.62 | 23.80 ± 19.81 | 0.004 |
| Scr, μmol/ L | 89.24 ± 64.23 | 94.90 ± 55.80 | 0.151 |
| eGFR, mL/min per 1.73 m2 | 83.34 ± 23.22 | 80.40 ± 27.85 | 0.081 |
| CrCL, ml/min | 88.17 ± 30.37 | 84.03 ± 32.68 | 0.040 |
| Uric acid, μmol/ L | 355.90 ± 95.27 | 337.98 ± 105.21 | 0.005 |
| Hyperuricemia, n% | 145(20.66) | 63(16.84) | 0.132 |
| cTnI, ng/mL | 1.01 ± 9.32 | 0.62 ± 3.93 | 0.433 |
| NT-proBNP, pg/ml | 294.80(115.00,956.93) | 368.60(127.90,1264.00) | 0.040 |
| CK, IU/L | 146.16 ± 343.72 | 106.19 ± 123.31 | 0.010 |
| CK-MB, IU/L | 18.58 ± 34.10 | 14.76 ± 14.60 | 0.019 |
| LVEF, % | 50.53 ± 9.47 | 49.46 ± 10.25 | 0.096 |
| Dyspnea(NYHA functional class), n% | 0.273 | ||
| I | 194(27.64) | 96(25.67) | |
| II | 340(45.58) | 180(48.13) | |
| III | 145(20.66) | 75(20.05) | |
| IV | 23(3.28) | 23(6.15) | |
| NYHA functional class III/ IV | 168(23.93) | 98(26.20) | 0.411 |
BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, MI myocardial infarction, PCI percutaneous coronary intervention, CABG coronary artery bypass grafting, CHD coronary atherosclerotic heart disease, WBC white blood cell, FPG fasting plasma glucose, TC total cholesterol, TG triglyceride, LDL-C low density lipoprotein cholesterol, HDL-C high density lipoprotein cholesterol, ALT alanine aminotransaminase, AST aspartate aminotransferase, Scr serum creatinine, eGFR estimated glomerular filtration rate, CrCL creatinine clearance, cTnI cardiac troponin I, NT-proBNP N-terminal pro-B type natriuretic peptide, CK creatine kinase, CK-MB creatine kinase MB, LVEF left ventricular ejection fraction, NYHA New York Heart Association
Table 2.
Angiographic Characteristics and Procedural Details
| No Diabetes | Diabetes | p Value | |
|---|---|---|---|
| (n = 702) | (n = 374) | ||
| Vascular lesion, n% | |||
| LM lesion | 129(18.38) | 82(21.93) | 0.163 |
| LAD lesion | 578(82.34) | 323(86.36) | 0.088 |
| LCX lesion | 483(68.80) | 303(81.02) | < 0.001 |
| RCA lesion | 552(78.63) | 301(80.48) | 0.476 |
| Multivessel disease, n% | 587(83.62) | 344(91.98) | < 0.001 |
| Number of lesions per patient | 2.40 ± 0.98 | 2.61 ± 0.93 | 0.001 |
| Location of the CTO, n% | |||
| LM-CTO | 7(1.00) | 3(0.80) | 0.751 |
| LAD-CTO | 327(46.58) | 169(45.19) | 0.662 |
| LCX-CTO | 202(28.77) | 120(32.09) | 0.259 |
| RCA-CTO | 403(57.41) | 232(62.03) | 0.142 |
| Multi-CTO lesion, n% | 205(29.20) | 126(33.69) | 0.129 |
| Number of CTO per patient | 1.34 ± 0.56 | 1.40 ± 0.61 | 0.087 |
| CTO target vessel, n% | |||
| LM-CTO | 5(0.71) | 3(0.80) | 0.870 |
| LAD-CTO | 272(38.75) | 141(37.70) | 0.737 |
| LCX-CTO | 107(15.24) | 52(13.90) | 0.556 |
| RCA-CTO | 347(49.43) | 192(51.34) | 0.551 |
| Ostial location, n% | 68(9.69) | 39(10.43) | 0.699 |
| In-stent occlusion, n% | 50(7.12) | 39(10.43) | 0.061 |
| Lesion length, mm | 27.85 ± 20.57 | 28.39 ± 16.96 | 0.672 |
| Lesion length ≥ 20 mm, n% | 450(64.10) | 255(68.18) | 0.180 |
| Blunt stump, n% | 463(66.00) | 270(72.19) | 0.037 |
| Tortuosity ≥ 45°, n% | 194(27.64) | 112(29.95) | 0.424 |
| Calcification, n% | 212(30.20) | 144(38.50) | 0.006 |
| Reattempt, n% | 104(14.81) | 66(17.65) | 0.225 |
| J-CTO score | 2.11 ± 1.13 | 2.31 ± 1.15 | 0.005 |
| Proximal cap side-branch, n% | 526(74.93) | 287(76.74) | 0.511 |
| “Interventional” collaterals, n% | 496(70.66) | 266(71.12) | 0.809 |
| Diseased distal landing zone, n% | 335(47.72) | 200(53.48) | 0.072 |
| Contrast volume, ml | 363.64 ± 203.53 | 362.99 ± 245.91 | 0.963 |
| Procedural time, min | 119.14 ± 69.29 | 117.21 ± 69.97 | 0.667 |
| Procedural success, n% | 640(91.17) | 342(91.44) | 0.879 |
LM left main coronary artery, LAD left anterior descending coronary artery, LCX left circumtrunnion coronary artery, RCA right coronary artery, CTO chronic total occlusion, J-CTO multicenter CTO registry in Japan
Table 3.
In-hospital MACE
| No Diabetes | Diabetes | p Value | |
|---|---|---|---|
| (n = 702) | (n = 374) | ||
| MACE, n% | 29(4.13) | 20(5.35) | 0.362 |
| All-cause mortality, n% | 4(0.57) | 3(0.80) | 0.652 |
| Cardiac mortality, n% | 4(0.57) | 3(0.80) | 0.652 |
| Nonfatal MI, n% | 12(1.71) | 5(1.34) | 0.641 |
| Clinically driven revascularization, n% | 14(1.99) | 13(3.48) | 0.139 |
| Emergency PCI | 14(1.99) | 13(3.48) | 0.139 |
| Emergency CABG | 0 | 0 | − |
MACE major adverse cardiac event, MI myocardial infarction, PCI percutaneous coronary intervention, CABG coronary artery bypass grafting
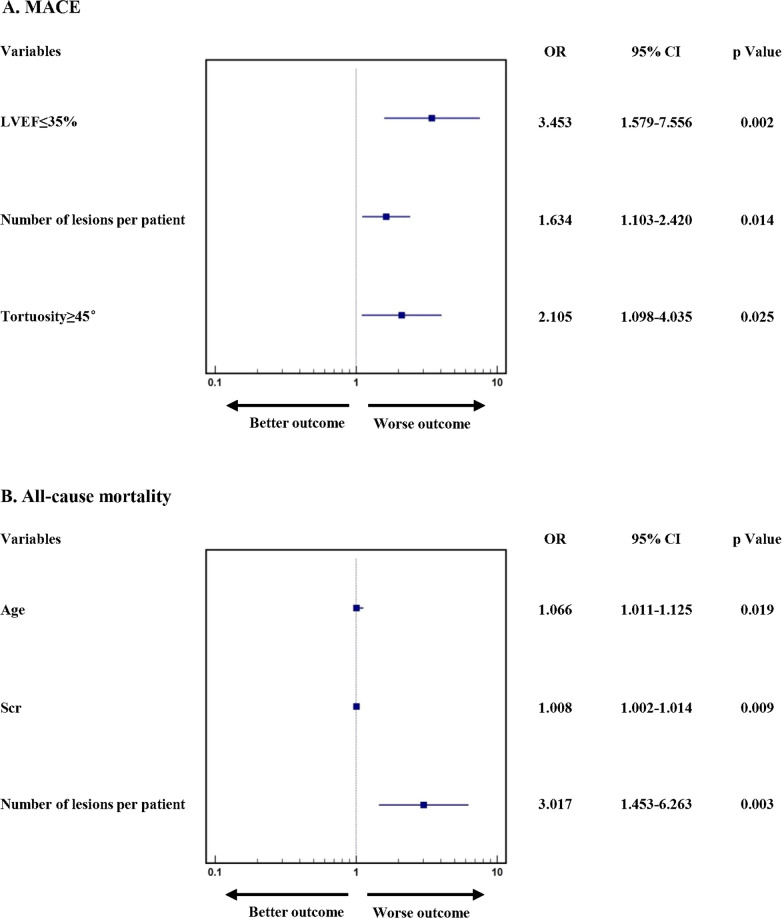
After successful CTO-PCI, follow-up visits were carried out at 1 month, completed for 623 (97.34%) and 331 (96.78%), and 1 year, completed for 584 (91.25%) and 300 (87.72%). The occurrence of MACE, including its three sub-items, was similar in the two groups both at 1 month (8.67% vs. 11.48%; p = 0.161) and 1 year (13.36% vs. 17.76%; p = 0.088, Table 4, Fig. 2). Moreover, the univariable and multivariable analysis of the CTO patients with diabetes receiving successful CTO-PCI showed that LVEF ≤ 35% (OR: 3.453, 95% CI 1.579–7.556, p = 0.002), number of lesions per patient (OR: 1.634, 95% CI 1.103–2.420, p = 0.014) and tortuosity ≥ 45° (OR: 2.105, 95% CI 1.098–4.035, p = 0.025) independently increased the risk of 1 year MACE (Table S4A, Fig. 3A). And, Age (OR: 1.066, 95% CI 1.011–1.125, p = 0.019), higher Scr (OR: 1.008, 95% CI 1.002–1.014, p = 0.009) and number of lesions per patient (OR: 3.017, 95% CI 1.453–6.263, p = 0.003) were independent risk factors of 1-year all-cause mortality (Table S4B, Fig. 3B).
Table 4.
Clinical Outcomes of Patients with Successful CTO-PCI
| No Diabetes | Diabetes | p Value | |
|---|---|---|---|
| 1 month follow-up | 623 | 331 | |
| MACE, n% | 54(8.67) | 38(11.48) | 0.161 |
| All-cause mortality, n% | 13(2.09) | 9(2.72) | 0.536 |
| Nonfatal MI, n% | 6(0.96) | 3(0.91) | 0.931 |
| Clinically driven revascularization, n% | 39(6.26) | 29(8.76) | 0.153 |
| 1 year follow-up | 584 | 300 | |
| MACE, n% | 78(13.36) | 53(17.76) | 0.088 |
| All-cause mortality, n% | 27(4.62) | 20(6.67) | 0.200 |
| Nonfatal MI, n% | 13(2.23) | 6(2.00) | 0.826 |
| Clinically driven revascularization, n% | 50(8.56) | 36(12.00) | 0.102 |
CTO chronic total occlusion, PCI percutaneous coronary intervention, MACE major cardiac event, MI myocardial infarction
Fig. 2.

Kaplan–Meier analysis of all-cause mortality in Patients with Successful CTO-PCI. CTO chronic total occlusion, PCI percutaneous coronary intervention
Fig. 3.
Multivariable Logistic Regression for 1-year Clinical Outcomes in Diabetic Patients with Successful CTO-PCI. CTO chronic total occlusion, PCI percutaneous coronary intervention, LVEF left ventricular ejection fraction, Scr serum creatinine, OR odds ratio, CI confidential interval
In regard to symptoms, significant improvement of dyspnea and angina were observed in all the CTO patients with successful CTO-PCI at 1 month and 1 year follow-up (Fig. 4 and Table 5). Compared with baseline, the proportion of NYHA functional class III/ IV and their RDS scores of the two groups was obviously decreased at 1 month and 1 year after CTO-PCI (p < 0.001, Fig. 4, Table 5); notably, RDS score in patients with diabetes decreased at a similar degree to those without diabetes (p > 0.05, Table 5), suggesting that successful CTO-PCI significantly alleviated dyspnea of all patients. Additionally, for patients with angina, successful CTO-PCI markedly increased the SAQ-AS and SAQ-AF scores of the two groups both at 1 month and 1 year follow-up (p < 0.001), and the SAQ-AS and SAQ-AF scores increased at the similar degree in the two groups (p > 0.05, Table 6), indicating that successful CTO-PCI also greatly relieved the angina of patients with diabetes or not.
Fig. 4.
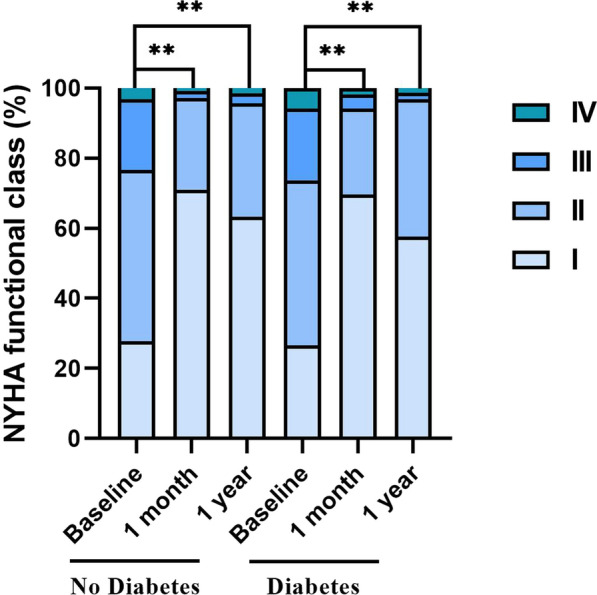
Changes of NYHA Functional Class in Patients with Successful CTO-PCI. ** p Value < 0.001. NYHA New York Heart Association, CTO chronic total occlusion, PCI percutaneous coronary intervention
Table 5.
Changes of Symptoms in Patients with Successful CTO-PCI Comparison of changes in RDS from baseline to follow-up
| RDS | |
|---|---|
| No Diabetes | |
| Baseline | 1.03 ± 1.10 |
| 1 month follow-up | 0.21 ± 0.47 |
| 1 year follow-up | 0.46 ± 0.65 |
| mΔ | 0.81 ± 1.17 |
| yΔ | 0.57 ± 1.21 |
| mp Value | < 0.001 |
| yp Value | < 0.001 |
| Diabetes | |
| Baseline | 1.06 ± 1.08 |
| 1 month follow-up | 0.25 ± 0.63 |
| 1 year follow-up | 0.53 ± 0.71 |
| mΔ | 0.80 ± 1.22 |
| yΔ | 0.52 ± 1.29 |
| mp Value | < 0.001 |
| yp Value | < 0.001 |
| ap Value | 0.855 |
| bp Value | 0.654 |
CTO chronic total occlusion, PCI percutaneous coronary intervention, RDS Rose Dyspnea Scale
mΔ change between baseline and 1 month follow-up
yΔ change between baseline and 1 year follow-up
mp Value: baseline versus 1 month follow-up
yp Value: baseline versus 1 year follow-up
ap Value: comparison of mΔ in the two groups
bp Value: comparison of yΔ in the two groups
Table 6.
Comparison of changes in SAQ subscales from baseline to follow-up
| SAQ-PL | SAQ-AS | SAQ-AF | SAQ-TS | SAQ-DP | |
|---|---|---|---|---|---|
| No Diabetes | |||||
| Baseline | 63.49 ± 14.59 | 50.23 ± 17.19 | 78.86 ± 24.38 | 79.93 ± 14.78 | 69.58 ± 18.74 |
| 1 month follow-up | 69.12 ± 12.98 | 70.78 ± 23.97 | 97.93 ± 7.86 | 83.47 ± 11.56 | 72.31 ± 13.83 |
| 1 year follow-up | 67.78 ± 11.95 | 71.95 ± 27.15 | 94.15 ± 11.21 | 86.65 ± 10.54 | 78.73 ± 15.62 |
| mΔ | 5.46 ± 19.02 | 20.74 ± 30.16 | 19.56 ± 24.99 | 3.34 ± 16.45 | 2.90 ± 21.52 |
| yΔ | 4.69 ± 17.89 | 20.00 ± 32.68 | 16.48 ± 25.91 | 6.26 ± 18.37 | 9.47 ± 25.16 |
| mp Value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.005 |
| yp Value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Diabetes | |||||
| Baseline | 61.72 ± 16.10 | 50.00 ± 15.08 | 76.67 ± 26.07 | 80.25 ± 15.47 | 70.54 ± 19.01 |
| 1 month follow-up | 67.33 ± 14.45 | 72.90 ± 23.87 | 98.26 ± 7.07 | 84.16 ± 11.09 | 71.22 ± 14.18 |
| 1 year follow-up | 66.68 ± 14.04 | 70.09 ± 29.03 | 94.61 ± 11.88 | 87.08 ± 9.31 | 78.51 ± 16.04 |
| mΔ | 5.31 ± 20.37 | 22.98 ± 27.69 | 22.02 ± 26.32 | 3.76 ± 17.82 | 0.98 ± 22.74 |
| yΔ | 5.46 ± 18.78 | 20.00 ± 32.68 | 20.04 ± 29.83 | 6.53 ± 19.31 | 8.30 ± 26.45 |
| mp Value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | 0.617 |
| yp Value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| ap Value | 0.911 | 0.267 | 0.161 | 0.715 | 0.206 |
| bp Value | 0.562 | 0.389 | 0.076 | 0.843 | 0.534 |
SAQ seattle angina questionnaire, SAQ-PL seattle angina questionnaire-physical limitation, SAQ-AS seattle angina questionnaire-anginal stability, SAQ-AF seattle angina questionnaire-anginal frequency, SAQ-TS seattle angina questionnaire-treatment satisfaction, SAQ-DP seattle angina questionnaire-disease perception
mΔ change between baseline and 1 month follow-up
yΔ change between baseline and 1 year follow-up
mp Value: baseline versus 1 month follow-up
yp Value: baseline versus 1 year follow-up
ap Value: comparison of mΔ in the two groups
bp Value: comparison of yΔ in the two groups
Most importantly, EQ-5D and SF-12 were firstly used to assess QOL of CTO patients with diabetes in the present study. Compared with baseline, PCS score of the two groups was greatly elevated at 1 month and 1 year follow-up (p < 0.001, Table 7) and the two groups showed similar improvement of PCS score (p > 0.05, Table 7). Likewise, EQ-5D score also exhibited a significant increase at 1 month and 1 year after successful CTO-PCI both in the patients with diabetes or without (p < 0.001, Table 8). These data suggested successful CTO-PCI remarkably improved QOL and the degree of improvement in patients with diabetes was similar to those without diabetes.
Table 7.
Changes of Quality of Life in Patients with Successful CTO-PCI SF-12 during follow-up in each group
| PCS | MCS | |
|---|---|---|
| No Diabetes | ||
| Baseline | 44.73 ± 8.11 | 53.96 ± 6.95 |
| 1 month follow-up | 50.42 ± 6.13 | 56.24 ± 4.69 |
| 1 year follow-up | 51.07 ± 6.54 | 54.75 ± 6.80 |
| mΔ | 5.53 ± 9.99 | 2.28 ± 7.93 |
| yΔ | 6.34 ± 10.22 | 0.64 ± 9.47 |
| mp Value | < 0.001 | < 0.001 |
| yp Value | < 0.001 | 0.081 |
| Diabetes | ||
| Baseline | 44.00 ± 8.44 | 54.50 ± 7.29 |
| 1 month follow-up | 50.16 ± 7.06 | 55.51 ± 1.52 |
| 1 year follow-up | 51.07 ± 6.54 | 54.16 ± 6.78 |
| mΔ | 5.92 ± 10.15 | 1.13 ± 8.19 |
| yΔ | 7.19 ± 10.28 | -0.29 ± 10.54 |
| mp Value | < 0.001 | 0.015 |
| yp Value | < 0.001 | 0.722 |
| ap Value | 0.576 | 0.038 |
| bp Value | 0.257 | 0.197 |
CTO chronic total occlusion, PCI percutaneous coronary intervention, PCS physical functioning component score, MCS mental functioning component score
mΔ change between baseline and 1 month follow-up
yΔ change between baseline and 1 year follow-up
mp Value: baseline versus 1 month follow-up
yp Value: baseline versus 1 year follow-up
ap Value: comparison of mΔ in the two groups
bp Value: comparison of yΔ in the two groups
Table 8.
EQ-5D during follow-up in each group
| EQ-5D | |
|---|---|
| No Diabetes | |
| Baseline | 0.89 ± 0.16 |
| 1 month follow-up | 0.97 ± 0.09 |
| 1 year follow-up | 0.97 ± 0.09 |
| mΔ | 0.08 ± 0.18 |
| yΔ | 0.07 ± 0.18 |
| mp Value | < 0.001 |
| yp Value | < 0.001 |
| Diabetes | |
| Baseline | 0.88 ± 0.18 |
| 1 month follow-up | 0.95 ± 0.12 |
| 1 year follow-up | 0.95 ± 0.13 |
| mΔ | 0.07 ± 0.20 |
| yΔ | 0.06 ± 0.22 |
| mp Value | < 0.001 |
| yp Value | < 0.001 |
| ap Value | 0.602 |
| bp Value | 0.378 |
CTO chronic total occlusion, PCI percutaneous coronary intervention, EQ-5D European Quality of Life-5 Dimensions
mΔ change between baseline and 1 month follow-up
yΔ change between baseline and 1 year follow-up
mp Value: baseline versus 1 month follow-up
yp Value: baseline versus 1 year follow-up
ap Value: comparison of mΔ in the two groups
bp Value: comparison of yΔ in the two groups
Discussion
This is the first prospective study to comprehensively evaluate the effect of successful revascularization on clinical outcomes, symptoms and QOL for CTO patients with diabetes. The main findings of the present study were as follows: (1) The CTO patients combined with diabetes had more hypertension, previous PCI and stroke, multivessel disease, number of lesions per patient and higher J-CTO score; (2) the occurrence of in-hospital MACE was similar in CTO patients with or without diabetes; (3) the incidence of MACE and all-cause mortality were similar in CTO patients with or without diabetes after successful CTO-PCI both at 1 month and 1 year follow-up; (4) LVEF ≤ 35%, number of lesions per patient and tortuosity ≥ 45° independently increased the risk of 1 year MACE and age, higher Scr level and number of lesions per patient were independent risk factors of 1-year all-cause mortality for diabetic patients underwent successful CTO-PCI; (5) successful CTO-PCI significantly alleviated symptoms and improved QOL regardless of diabetes, at similar rate across the two groups. This study demonstrated the benefits of successful CTO-PCI in patients with diabetes in a real-world setting (See Additional file 1: Table S1–S4).
China has the highest number of diabetic patients and annual number of deaths from diabetes, at approximately 140.9 and 1.4 million respectively [28]. In our study, diabetes was found with an overall prevalence of 34.76% in CTO patients, consistent with the epidemiology in the North America [9, 10]. Previous studies reported that diabetes was associated with greater burden of comorbidity, longer lesions, and more complex anatomy in CTO patients [7, 8, 29]. In the present study, we found CTO patients with diabetes suffered more hypertension, previous PCI and stroke, multivessel disease, number of lesions per patient, blunt stump, calcification and higher J-CTO score.
The benefits of clinical outcome of CTO patients combined with diabetes after successful CTO-PCI was still controversial. Guo L et al. found that the incidence of MACE was significantly higher in patients with diabetes after successful CTO-PCI at a 2.6-year follow-up [11]. Sanguineti F et al. also reported that CTO patients with diabetes suffered more MACE at the median follow-up 4.2 years [12]. However, there also existed some studies found that the MACE in patients with or without diabetes was not of obvious difference at the 1.7–5-year follow-up [13–15], importantly, all of which were from the Asia and consistent with our findings. In our study, the occurrence of MACE, including all-cause mortality, nonfatal MI and clinically driven revascularization, was similar in the CTO patients no matter whether combined with diabetes or not both at 1 month and 1 year after successful CTO-PCI. These findings demonstrate the necessity to achieve revascularization in these diabetic patients to achieve better clinical outcome.
For CHD patients, especially those suffered from CTO lesion, severe adverse symptoms, such as angina and dyspnea, have been the most troubling problems, hence symptoms improvement has been proposed as the primary indication for CTO-PCI by Global Expert Consensus [30]. Many RCT, registry and observational studies have demonstrated that successful CTO-CPI could improve symptoms, including angina and dyspnea [31–34]. However, to date, only one study by Salisbury AC et al. reported that successful CTO-PCI relieved angina and dyspnea and of a similar magnitude regardless of diabetes status at 1 year follow-up [29]. Similarly, our study also found that successful CTO-PCI could greatly alleviate symptoms of patients with diabetes at a comparable degree to those without diabetes.
QOL has been defined by WHO as people’ “perceptions of their position in life in the context of culture and value systems in which they live, and in relation to their goals, expectations, standards, and concerns”; it involves many important domains of human dynamics such as the physical, psychological, social, environmental, and spiritual factors [35]. Therefore, QOL is receiving increasing attention recently due to its critical status in assessing patients’ well-being. Additionally, diabetic patients require life-long self-care, including the improvement of both long-term health and QOL, indicating QOL is the ultimate goal [16, 17]. However, hitherto, no study has evaluated the impact of successful revascularization on QOL for CTO patients with diabetes. In the present study, we firstly assessed QOL of these patients using well-recognized QOL questionnaire SF-12 and EQ-5D, and found that successful CTO-PCI could greatly improve QOL of diabetic patients at a similar degree between patients with and without diabetes.
Study limitations
This study undoubtedly has some limitations. First, the single-team nature of our study is a potential weakness, which may be not suitable for other centers or team. Second, no angiographic and echocardiography follow-up data were collected. Third, our study did not include those who were either not provided PCI or referred for surgical revascularization. Fourth, we have no accessible information on residual ischemia. Fifth, objective measurements of physical capacities, such as those from exercise stress testing were not systematically available in follow-up. Finally, noninvasive testing such as cardiac magnetic resonance imaging should be performed in patients to assess the myocardial viability, which will be carried out in the future work.
Conclusions
The present study demonstrates that timely successful CTO-PCI was necessary for patients with diabetes to bring reduced long-term MACE, substantial symptom alleviation and improved QOL.
Supplementary Information
Additional file 1: Table S1 Non-CTO lesion characteristics. Table S2 Intraprocedural and In-hospital Complications. Table S3 Univariable Logistic Regression for 1-month Clinical Outcomes in Diabetic Patients with Successful CTO-PCI. Table S4 Univariable Logistic Regression for 1-year Clinical Outcomes in Diabetic Patients with Successful CTO-PCI
Acknowledgements
We thank all the patients for participating in this project.
Abbreviations
- ALT
Alanine aminotransaminase
- AST
Aspartate aminotransferase
- BMI
Body mass index
- CABG
Coronary artery bypass graft
- CHD
Coronary atherosclerotic heart disease
- CI
Confidence interval
- cTnI
Cardiac troponin I
- CTO
Chronic total occlusion
- CTO-PCI
Chronic total occlusion treated with percutaneous coronary intervention
- DBP
Diastolic blood pressure
- eGFR
estimated glomerular filtration rate
- EQ-5D
European quality of life-5 dimensions
- FPG
Fasting plasma glucose
- HDL-C
High density lipoprotein cholesterol
- HF
Heart failure
- J-CTO
Multicenter CTO registry in Japan
- LAD
Left anterior descending coronary artery
- LCX
Left circumtrunnion coronary artery
- LDL-C
Low density lipoprotein cholesterol
- LM
Left main coronary artery
- LVEF
Left ventricular ejection fraction
- MACE
Major adverse cardiac event
- MCS
Mental functioning component score
- MI
Myocardial infarction
- NT-proBNP
N-terminal pro-B type natriuretic peptide
- NYHA
New York Heart Association
- OR
Odds ratio
- PCI
Percutaneous coronary intervention
- PCS
Physical functioning component score
- QOL
Quality of life
- RCA
Right coronary artery
- RCT
Randomized controlled trial
- RDS
Rose dyspnea scale
- SAQ
Seattle Angina Questionnaire
- SAQ-PL
Seattle Angina Questionnaire-physical limitation
- SAQ-AS
Seattle Angina Questionnaire-anginal stability
- SAQ-DP
Seattle Angina Questionnaire-disease perception
- SAQ-AF
Seattle Angina Questionnaire-anginal frequency
- SAQ-TS
Seattle Angina Questionnaire-treatment satisfaction
- SBP
Systolic blood pressure
- Scr
Serum creatinine
- TC
Total cholesterol
- TG
Triglyceride
- WBC
white blood cell
Author contributions
The conception and design of the study and manuscript drafting were performed by SZ, YC, QYW, KL, CXL and HKG. The generation and data collection and follow-up were performed by BDZ, TTY, PH, LY, HW, CHX, and WW. The assembly and analysis and/or interpretation of the data were performed by ZHW, ZWW, JYW, YMZ, WTH, CL and QLL. All authors read and approved the final manuscript.
Funding
This work was supported by New Clinical Technology and New Business of Xijing Hospital (XJGX15Y39), the Program for the National Natural Science Foundation of China (Grant No. 81670229, 81570210), Bethune-Merck Diabetes Research Foundation (G2017044), Advanced Foundation of Xinxin Cardiovascular Health Foundation in Suzhou Industrial Park (2019-CCAACCESS065), Xi’an Science and Technology Project (20YXYJ0003(4)).
Availability of data and materials
The datasets generated and analyzed for this current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Xijing Hospital, the Fourth Military Medical University, and each subject was provided with informed consent before recruitment (KY20172019-1).
Consent for publication
All authors consent this manuscript for publication.
Competing interests
The authors have no conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shuai Zhao, Yan Chen and Qingyi Wang contributed equally to this work
Contributor Information
Haokao Gao, Email: hk_gao@163.com.
Chengxiang Li, Email: lichx1@163.com.
Kun Lian, Email: liank1122@163.com.
References
- 1.Tajstra M, Pyka L, Gorol J, Pres D, Gierlotka M, Gadula-Gacek E, Kurek A, Wasiak M, Hawranek M, Zembala MO, et al. Impact of chronic total occlusion of the coronary artery on long-term prognosis in patients with ischemic systolic heart failure: insights From the COMMIT-HF registry. JACC Cardiovasc Interv. 2016;9(17):1790–1797. doi: 10.1016/j.jcin.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Tomasello SD, Boukhris M, Giubilato S, Marzà F, Garbo R, Contegiacomo G, Marzocchi A, Niccoli G, Gagnor A, Varbella F, et al. Management strategies in patients affected by chronic total occlusions: results from the Italian registry of chronic total occlusions. Eur Heart J. 2015;36(45):3189–3198. doi: 10.1093/eurheartj/ehv450. [DOI] [PubMed] [Google Scholar]
- 3.Sirnes PA, Myreng Y, Mølstad P, Bonarjee V, Golf S. Improvement in left ventricular ejection fraction and wall motion after successful recanalization of chronic coronary occlusions. Eur Heart J. 1998;19(2):273–281. doi: 10.1053/euhj.1997.0617. [DOI] [PubMed] [Google Scholar]
- 4.George S, Cockburn J, Clayton TC, Ludman P, Cotton J, Spratt J, Redwood S, de Belder M, de Belder A, Hill J, et al. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central Cardiac Audit Database. J Am Coll Cardiol. 2014;64(3):235–243. doi: 10.1016/j.jacc.2014.04.040. [DOI] [PubMed] [Google Scholar]
- 5.Guo L, Wu J, Zhong L, Ding H, Xu J, Zhou X, Huang R. Two-year clinical outcomes of medical therapy vs. revascularization for patients with coronary chronic total occlusion. Hellenic J Cardiol. 2020;61(4):264–271. doi: 10.1016/j.hjc.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Yan Y, Zhang M, Yuan F, Liu H, Wu D, Fan Y, Guo X, Xu F, Zhang M, Zhao Q, et al. Successful revascularization versus medical therapy in diabetic patients with stable right coronary artery chronic total occlusion: a retrospective cohort study. Cardiovasc Diabetol. 2019;18(1):108. doi: 10.1186/s12933-019-0911-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iglesias JF, Degrauwe S, Rigamonti F, Noble S, Roffi M. Percutaneous coronary intervention of chronic total occlusions in patients with diabetes mellitus: a treatment-risk paradox. Curr Cardiol Rep. 2019;21(2):9. doi: 10.1007/s11886-019-1091-2. [DOI] [PubMed] [Google Scholar]
- 8.Nicholls SJ, Tuzcu EM, Kalidindi S, Wolski K, Moon KW, Sipahi I, Schoenhagen P, Nissen SE. Effect of diabetes on progression of coronary atherosclerosis and arterial remodeling: a pooled analysis of 5 intravascular ultrasound trials. J Am Coll Cardiol. 2008;52(4):255–262. doi: 10.1016/j.jacc.2008.03.051. [DOI] [PubMed] [Google Scholar]
- 9.Michael TT, Karmpaliotis D, Brilakis ES, Fuh E, Patel VG, Mogabgab O, Alomar M, Kirkland BL, Lembo N, Kalynych A, et al. Procedural outcomes of revascularization of chronic total occlusion of native coronary arteries (from a multicenter United States registry) Am J Cardiol. 2013;112(4):488–492. doi: 10.1016/j.amjcard.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Brilakis ES, Banerjee S, Karmpaliotis D, Lombardi WL, Tsai TT, Shunk KA, Kennedy KF, Spertus JA, Holmes DR, Jr, Grantham JA. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National Cardiovascular Data Registry) JACC Cardiovasc Interv. 2015;8(2):245–253. doi: 10.1016/j.jcin.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 11.Guo L, Wang J, Ding H, Meng S, Zhang X, Lv H, Zhong L, Wu J, Xu J, Zhou X, et al. Long-term outcomes of medical therapy versus successful recanalisation for coronary chronic total occlusions in patients with and without type 2 diabetes mellitus. Cardiovasc Diabetol. 2020;19(1):100. doi: 10.1186/s12933-020-01087-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanguineti F, Garot P, O'Connor S, Watanabe Y, Spaziano M, Lefèvre T, Hovasse T, Benamer H, Unterseeh T, Chevalier B, et al. Chronic total coronary occlusion treated by percutaneous coronary intervention: long-term outcome in patients with and without diabetes. EuroIntervention. 2017;12(15):e1889–e1897. doi: 10.4244/EIJ-D-15-00278. [DOI] [PubMed] [Google Scholar]
- 13.Fu D, Li H, Gao T, Liu M, Feng L, Li C, Xiao X, Jiang H, Yang P, Li X. Comparison of long-term clinical outcomes of percutaneous coronary intervention for chronic total occlusion between patients with and without diabetes mellitus: a single-center retrospective observational study. Ann Palliat Med. 2021;10(9):9993–10004. doi: 10.21037/apm-21-2354. [DOI] [PubMed] [Google Scholar]
- 14.Tsai CT, Huang WC, Teng HI, Tsai YL, Lu TM. Long term clinical impact of successful recanalization of chronic total occlusion in patients with and without type 2 diabetes mellitus. Cardiovasc Diabetol. 2020;19(1):119. doi: 10.1186/s12933-020-01093-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mashaly A, Rha SW, Choi BG, Baek MJ, Ryu YG, Choi SY, Byun JK, Li H, Shim MS, Jang WY, et al. Impact of diabetes mellitus on 5-year clinical outcomes in patients with chronic total occlusion lesions. Coron Artery Dis. 2018;29(2):119–126. doi: 10.1097/MCA.0000000000000562. [DOI] [PubMed] [Google Scholar]
- 16.Speight J, Holmes-Truscott E, Hendrieckx C, Skovlund S, Cooke D. Assessing the impact of diabetes on quality of life: what have the past 25 years taught us? Diabet Med. 2020;37(3):483–492. doi: 10.1111/dme.14196. [DOI] [PubMed] [Google Scholar]
- 17.Rodríguez-Almagro J, García-Manzanares Á, Lucendo AJ, Hernández-Martínez A. Health-related quality of life in diabetes mellitus and its social, demographic and clinical determinants: a nationwide cross-sectional survey. J Clin Nurs. 2018;27(21–22):4212–4223. doi: 10.1111/jocn.14624. [DOI] [PubMed] [Google Scholar]
- 18.Lee SW, Lee PH, Ahn JM, Park DW, Yun SC, Han S, Kang H, Kang SJ, Kim YH, Lee CW, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion. Circulation. 2019;139(14):1674–1683. doi: 10.1161/CIRCULATIONAHA.118.031313. [DOI] [PubMed] [Google Scholar]
- 19.Classification and diagnosis of diabetes Standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17–s38. doi: 10.2337/dc22-S002. [DOI] [PubMed] [Google Scholar]
- 20.Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, Ochiai M, Noguchi Y, Kato K, Shibata Y, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4(2):213–221. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 21.Koo BK, Kang J, Park KW, Rhee TM, Yang HM, Won KB, Rha SW, Bae JW, Lee NH, Hur SH, et al. Aspirin versus clopidogrel for chronic maintenance monotherapy after percutaneous coronary intervention (HOST-EXAM): an investigator-initiated, prospective, randomised, open-label, multicentre trial. Lancet. 2021;397(10293):2487–2496. doi: 10.1016/S0140-6736(21)01063-1. [DOI] [PubMed] [Google Scholar]
- 22.Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, van den Brand M, Van Dyck N, Russell ME, Mohr FW, et al. The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1(2):219–227. [PubMed] [Google Scholar]
- 23.Rose GA, Blackburn H. Cardiovascular survey methods. Monogr Ser World Health Organ. 1968;56:1–188. [PubMed] [Google Scholar]
- 24.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonnell M, Fihn SD. Development and evaluation of the Seattle Angina questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 25.Tsuchiya A, Ikeda S, Ikegami N, Nishimura S, Sakai I, Fukuda T, Hamashima C, Hisashige A, Tamura M. Estimating an EQ-5D population value set: the case of Japan. Health Econ. 2002;11(4):341–353. doi: 10.1002/hec.673. [DOI] [PubMed] [Google Scholar]
- 26.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol group. Ann Med. 2001;33(5):337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 27.Ware J, Jr, Kosinski M, Keller SD. A 12-Item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Sun H, Saeedi P, Karuranga S, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. 10.1016/j.diabres.2021.109119. [DOI] [PMC free article] [PubMed]
- 29.Salisbury AC, Sapontis J, Grantham JA, Qintar M, Gosch KL, Lombardi W, Karmpaliotis D, Moses J, Cohen DJ, Spertus JA, et al. Outcomes of chronic total occlusion percutaneous coronary intervention in patients with diabetes: insights from the OPEN CTO registry. JACC Cardiovasc Interv. 2017;10(21):2174–2181. doi: 10.1016/j.jcin.2017.08.043. [DOI] [PubMed] [Google Scholar]
- 30.Brilakis ES, Mashayekhi K, Tsuchikane E, Abi Rafeh N, Alaswad K, Araya M, Avran A, Azzalini L, Babunashvili AM, Bayani B, et al. Guiding principles for chronic total occlusion percutaneous coronary intervention. Circulation. 2019;140(5):420–433. doi: 10.1161/CIRCULATIONAHA.119.039797. [DOI] [PubMed] [Google Scholar]
- 31.Werner GS, Martin-Yuste V, Hildick-Smith D, Boudou N, Sianos G, Gelev V, Rumoroso JR, Erglis A, Christiansen EH, Escaned J, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39(26):2484–2493. doi: 10.1093/eurheartj/ehy220. [DOI] [PubMed] [Google Scholar]
- 32.Obedinskiy AA, Kretov EI, Boukhris M, Kurbatov VP, Osiev AG, Ibn Elhadj Z, Obedinskaya NR, Kasbaoui S, Grazhdankin IO, Prokhorikhin AA, et al. The IMPACTOR-CTO trial. JACC Cardiovasc Interv. 2018;11(13):1309–1311. doi: 10.1016/j.jcin.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 33.Sapontis J, Salisbury AC, Yeh RW, Cohen DJ, Hirai T, Lombardi W, McCabe JM, Karmpaliotis D, Moses J, Nicholson WJ, et al. Early procedural and health status outcomes after chronic total occlusion angioplasty: a report from the OPEN-CTO registry. JACC Cardiovasc Interv. 2017;10(15):1523–1534. doi: 10.1016/j.jcin.2017.05.065. [DOI] [PubMed] [Google Scholar]
- 34.Walsh SJ, Hanratty CG, McEntegart M, Strange JW, Rigger J, Henriksen PA, Smith EJ, Wilson SJ, Hill JM, Mehmedbegovic Z, et al. Intravascular healing is not affected by approaches in contemporary CTO PCI: the consistent CTO study. JACC Cardiovasc Interv. 2020;13(12):1448–1457. doi: 10.1016/j.jcin.2020.03.032. [DOI] [PubMed] [Google Scholar]
- 35.WHOQOL The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41(10):1403–1409. doi: 10.1016/0277-9536(95)00112-K. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1 Non-CTO lesion characteristics. Table S2 Intraprocedural and In-hospital Complications. Table S3 Univariable Logistic Regression for 1-month Clinical Outcomes in Diabetic Patients with Successful CTO-PCI. Table S4 Univariable Logistic Regression for 1-year Clinical Outcomes in Diabetic Patients with Successful CTO-PCI
Data Availability Statement
The datasets generated and analyzed for this current study are available from the corresponding author upon reasonable request.