Human monkeypox is a viral disease caused by an orthopoxvirus that is endemic in some African countries, including the Democratic Republic of the Congo and Nigeria. However, a sudden increase in the number of cases worldwide has been reported since May 2022, and over 80,000 people have been diagnosed with monkeypox during the current outbreak. Studies have shown that most cases of disease have occurred predominantly among men who have sex with men (MSM) with a high prevalence of lesions in the anogenital region [1,2]. Furthermore, there is growing evidence that close skin-to-skin contact is the primary route of monkeypox transmission [3].
Although Brazil accounts for approximately 12% of cases worldwide, epidemiological studies on monkeypox in the country are lacking. This study aimed to (1) report the incidence and geographic distribution of monkeypox in Brazil at the state level; (2) describe the clinical characteristics of patients with the disease; and (3) examine the relationship between incidence rates and socioeconomic and demographic determinants.
This nationwide population-based ecological study was carried out using open data from state health department bulletins in Brazil, a country with approximately 8.5 million km2, an estimated population of ∼213 million people, and a population density of ∼25 inhabitants per km2. In addition, Brazil is geopolitically divided into five regions (Northeast, North, Central-West, Southeast and South), has 26 states and one federal administrative district, 5570 municipalities, and a human development index (HDI) of 0.765.
To estimate monkeypox incidence rates in Brazil at the regional and state levels, we extracted data on confirmed cases from official bulletins from June 9 (first case report) to November 23, 2022. Furthermore, the following clinical variables were extracted: sex, age, race/ethnicity, sexual orientation, potential transmission route, and signs and symptoms. Other variables of interest included HDI and population density for each Brazilian state.
The monkeypox incidence rates per 100,000 inhabitants were calculated using the population estimate provided by the Brazilian Institute of Geography and Statistics (IBGE, acronym in Portuguese) (https://www.ibge.gov.br). The geographic distribution of monkeypox incidence was modelled using the Jenks natural breaks classification method in the ArcGis 10.3 software. Descriptive statistics were provided for the distribution of cases by sex, gender, race/ethnicity, sexual orientation, potential transmission route, and the presence of signs and symptoms. The relationship between monkeypox incidence rates and socioeconomic (HDI) and demographic (population density) determinants in a state-level analysis was carried out using a linear regression model with a backward selection process in the JASP software version 0.13 (JASP Team, Amsterdam, Netherlands). The significance level in the final model was set at 5%. Because all data were obtained from a public domain database and were deidentified, no institutional review board approval or informed consent were required.
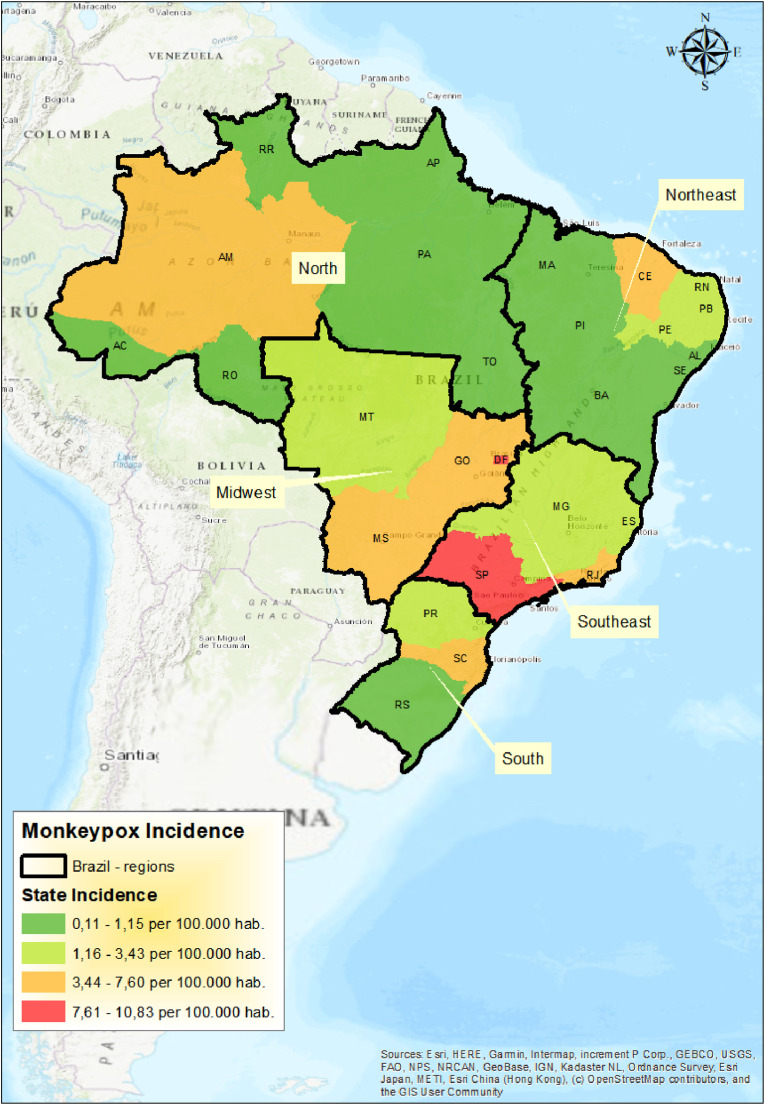
A total of 9729 cases and 12 deaths associated with monkeypox were confirmed until November 23, 2022. The overall incidence rate was 4.6 cases per 100,000 inhabitants, with the higher rates found in the central-west (7.0 cases per 100,000) and southwest (6.8 cases per 100,000) regions. At the state-level, the higher incidence rates were found in Distrito Federal (DF) (10.8 cases per 100,000), São Paulo (SP) (8.9 cases per 100,000), Goiás (GO) (7.6 cases per 100,000), and Rio de Janeiro (RJ) (7.3 cases per 100,000) (Fig. 1 ). The states with the highest HDI (β = 31.42, standard error [SE] = 9.30; p = 0.002) and population density (β = 0.01, SE = 0.01; p = 0.035) registered the highest incidence rates of the disease (model fit: R2 = 0.606; Durbin-Watson statistics = 1.901).
Fig. 1.
Geographic distribution of monkeypox incidence at state level in Brazil.
Most cases were diagnosed among men (92.2%), aged 20–39 years (73.6%), whites (44.9%), and self-identified homo- or bisexual (67.5%). Approximately 5% of cases were reported in children and adolescents. The most common systemic features included fever (57.9%), lymphadenopathy (41.1%), headache (39.6%), and myalgia (36.9%). Cutaneous lesions were reported in 92.4% of cases, particularly in the anogenital region (61.5%). Oral lesions were reported in about 9% of patients, and proctitis in 2.1%. A limited number of patients have described the potential transmission route of the disease, and sexual exposure before the onset of signs and symptoms has been reported in 40% of cases (Table 1 ).
Table 1.
Geographic distribution and clinical characteristics of monkeypox cases in Brazil.
| Geographic distribution | Cases | Incidence rate (per 100,000 inhabitants) |
|---|---|---|
| Brazil | 9729 | 4.6 |
| Geographic regions | ||
| Central-West | 1161 | 7.0 |
| Southwest | 6106 | 6.8 |
| South | 927 | 3.1 |
| North | 403 | 2.1 |
| Northeast | 1132 | 2.0 |
| Clinical characteristics | Cases | Percentage (%) |
|---|---|---|
| Sex (n = 9100) | ||
| Male | 8386 | 92.2 |
| Female | 714 | 7.8 |
| Age (years) (n = 8546) | ||
| 0–19 | 411 | 4.8 |
| 20–39 | 6287 | 73.6 |
| ≥40 | 1835 | 21.5 |
| Missing data | 13 | 0.1 |
| Race/ethnicity (n = 6124) | ||
| White (“branco”) | 2748 | 44.9 |
| Brown (“pardo”) | 1649 | 26.9 |
| Black (“preto”) | 667 | 10.9 |
| Yellow (“amarelo” or of Asian ancestry) | 78 | 1.3 |
| Indigenous (“indígena”) | 7 | 0.1 |
| Missing data | 975 | 15.9 |
| Sexual orientation (n = 1753) | ||
| Homosexuality | 1012 | 57.7 |
| Heterosexuality | 324 | 18.5 |
| Bisexuality | 172 | 9.8 |
| Other | 21 | 1.2 |
| Missing data | 224 | 12.8 |
| Sexual exposure (n = 1457) | 579 | 40.0 |
| Signs and symptoms (n = 7518) | ||
| Cutaneous lesions | 6944 | 92.4 |
| Genital and/or anal lesions | 4622 | 61.5 |
| Fever | 4353 | 57.9 |
| Lymphadenopathy | 3088 | 41.1 |
| Headache | 2980 | 39.6 |
| Myalgia | 2773 | 36.9 |
| Asthenia | 2511 | 33.4 |
| Sore throat | 807 | 10.7 |
| Oral lesions | 662 | 8.8 |
| Arthralgia | 227 | 3.0 |
| Proctitis | 158 | 2.1 |
| Photosensitivity | 73 | 1.0 |
| Conjunctivitis | 36 | 0.5 |
This is the first study to describe the incidence rates, geographic distribution, and clinical characteristics of monkeypox in Brazil. During the first months of the current outbreak, Brazil experienced high transmission rates and a significant increase in confirmed monkeypox cases [4]. We estimated an accumulated incidence similar to the found in Germany (4.4 cases per 100,000) and United Kingdom (5.5 cases per 100,000), but lower than that reported in Spain (15.6 cases per 100,000) and United States (8.6 cases per 100,000), and higher than that registered in Italy (1.6 cases per 100,000) (https://ourworldindata.org/monkeypox). Differences in disease burden between countries can be explained by a variety of factors, including geographic, socioeconomic, educational, cultural, infrastructure, and public health policy aspects.
In Brazil, a country with continental dimensions, regional differences are also noticeable. As a result, it is to be expected that the spread of monkeypox is not geographically uniform. In this study, we found higher disease incidence rates in states with better socioeconomic indicators and higher population density. Similar findings have also been demonstrated in relation to COVID-19 [5,6] and may reflect better access to healthcare in more developed urban communities. In addition, it was shown that human population density is an important variable in monkeypox distribution in endemic countries, which may be caused by increased human-environment interaction [7].
Individuals with monkeypox in Brazil appear to have clinical features similar to those reported in other non-endemic countries [1] and most of them are gay/bisexual male young adults. However, a significant number of cases have been described in women and the pediatric population, which may indicate an incipient change in the distribution pattern of the disease [8]. Although the route of transmission is poorly reported by official bulletins in Brazil, there is evidence of a high risk of infection from close contact with skin lesions [3]. Furthermore, the high prevalence of lesions in the anogenital region suggests high-risk sexual behavior among these individuals and the need to implement sex education policies and programs. Importantly, a recent global case series study showed that approximately 75% of women with monkeypox have anogenital lesions and 25% have oral lesions, with sexual contact being the most likely route of transmission [9]. These findings add to the growing body of evidence linking sexual practices to clinical lesions also present in women. Unfortunately, knowledge about disease transmission chains among children and adolescents in the current outbreak is limited.
Despite the potential for underreporting, state-level findings are the best publicly available data in the country for investigating regional differences in monkeypox estimates. Our study showed that most cases of monkeypox in Brazil have been registered in states with better socioeconomic indicators and higher population density. In addition, monkeypox in Brazil has been characterized by a high incidence of the disease in the anogenital region among young MSM. Strategies for improving diagnosis in vulnerable socioeconomic populations, including people from racial and ethnic minority groups, must be implemented.
Authors contributions
All authors contributed equally to this manuscript.
Financial source
There is no funding source.
Declaration of competing interest
The authors declare they have no conflicts of interest.
References
- 1.Martins-Filho P.R., Tanajura D.M., Vecina-Neto G. Multi-country monkeypox outbreak: a quantitative evidence synthesis on clinical characteristics, potential transmission routes, and risk factors. Eur J Intern Med. 2022 doi: 10.1016/j.ejim.2022.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thornhill J.P., Barkati S., Walmsley S., Rockstroh J., Antinori A., Harrison L.B., et al. Monkeypox virus infection in humans across 16 countries — april–june 2022. N Engl J Med. 2022;387:679–691. doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 3.Martins-Filho P.R., Tanajura D.M., Alves dos Santos C. Polymerase chain reaction positivity and cycle threshold values in biological samples from patients with monkeypox: a meta-analysis. Trav Med Infect Dis. 2022;50 doi: 10.1016/j.tmaid.2022.102448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schrarstzhaupt I.N., Fontes-Dutra M., Diaz-Quijano F.A. Early estimates of the incidence trend and the reproductive number of the monkeypox epidemic in Brazil. Trav Med Infect Dis. 2022;50 doi: 10.1016/j.tmaid.2022.102484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martins-Filho P.R., de Souza Araújo A.A., Quintans-Júnior L.J., Santos V.S. COVID-19 fatality rates related to social inequality in Northeast Brazil: a neighbourhood-level analysis. J Trav Med. 2020;27 doi: 10.1093/jtm/taaa128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martins-Filho P.R. Relationship between population density and COVID-19 incidence and mortality estimates: a county-level analysis. J Infect Public Health. 2021;14:1087–1088. doi: 10.1016/j.jiph.2021.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arotolu T.E., Afe A.E., Wang H., Lv J., Shi K., Huang L., et al. Spatial modeling and ecological suitability of monkeypox disease in Southern Nigeria. PLoS One. 2022;17 doi: 10.1371/journal.pone.0274325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martins-Filho P.R., de Souza M.F., Oliveira Góis M.A., Bezerra G.V.B., Gonçalves C.C.A., dos Santos Nascimento É.R., et al. Unusual epidemiological presentation of the first reports of monkeypox in a low-income region of Brazil. Trav Med Infect Dis. 2022;50 doi: 10.1016/j.tmaid.2022.102466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thornhill J.P., Palich R., Ghosn J., Walmsley S., Moschese D., Cortes C.P., et al. Human monkeypox virus infection in women and non-binary individuals during the 2022 outbreaks: a global case series. Lancet. 2022 doi: 10.1016/S0140-6736(22)02187-0. [DOI] [PMC free article] [PubMed] [Google Scholar]