Abstract
Objective
The recent increasing incidence of human monkeypox cases highlights the necessity of early detection, prompt response and preventive management to stop it in its tracks, and healthcare workers play the most crucial role here. This study aims at assessing the preparedness of Bangladeshi medical doctors by assessing their knowledge and attitude regarding monkeypox.
Methodology
This cross-sectional study was conducted among the practicing medical doctors all over Bangladesh. The data was collected from 26th May to 4th June of 2022 using a semi-structured and self-administered questionnaire which was distributed through the internet, and a total of 389 data was collected. The cut-off points for defining good knowledge and positive attitude towards human monkeypox were considered as 70% and 80% of total values, respectively. Multivariable logistic regression analyses were carried out to identify the factors associated with good knowledge and a positive attitude. Statistical software R version 4.2.0 was used for data analysis.
Result
Of all, 330 (84.83%) doctors displayed a positive attitude towards preventive practices, but only 119 (30.59%) participants had good knowledge regarding monkeypox. In multivariable logistic regression analysis, getting any information about monkeypox in the medical curriculum and learning about monkeypox within the last one month had a significant association with good knowledge. Apart from the participant's age, no other variables revealed any significant association with a positive attitude toward preventive practices. Good knowledge showed a significant association with positive attitude (p < 0.05).
Conclusion
Knowledge regarding human monkeypox among medical doctors in Bangladesh was comparatively lower than the attitude towards its preventive measures. Developing and implementing practical sessions regarding the virus to enhance the knowledge and capacity of the medical doctors could be an effective strategy to get prepared for the monkeypox outbreak in Bangladesh.
Keywords: Monkeypox, Medical doctors, Bangladesh, Viral outbreak, Pandemic
Introduction
A zoonotic infection with smallpox-like signs and symptoms, human monkeypox (HMPX) is caused by the monkeypox virus (MPXV), which is a member of the genus orthopoxvirus. It is found predominantly in Central and Western Africa [34], [35], [36]. Timing of illness onset, rash distribution, and timing of rash occurrence are comparable to smallpox [28], [33], [34], [35], [36]. The first case of HMPX was recorded in the Democratic Republic of the Congo in 1970, and since then, multiple outbreaks and sporadic cases have been documented throughout the Central as well as the Western African nations [5]. The first human monkeypox cases reported outside of Africa occurred in 2003 in the United States of America [17]. The number of HMPX cases has increased dramatically over the past two decades [10], [28], and as a result, it is currently regarded as the most relevant orthopoxvirus from a public health view [37]. Republic of Congo, Democratic Republic of Congo, Central African Republic, Liberia, Nigeria, and Cameroon have reported recent HMPX outbreaks [24], [37], [5]. Although the case fatality rate (CFR) for the 2017–2018 outbreak in Nigeria was 6%, recent reports mention of a CFR of 2.6% in African Union member countries and globally 0.04% in 2022 which is much lower compared to the historical data [1], [19], [6], [7], [8], [37].
Recently the virus was reported to spread outside African continent and the United States [17], [34], [35], [36], the United Kingdom [32], and Israel [11], encountered HMPX transferred from other countries. In May of 2019, Singapore reported the first verified HMPX case in Asia; the patient was a Nigerian citizen who attended a training in Singapore [22]. About 100 countries have reported cases of monkeypox since May 2022, with over 62,000 confirmed cases [17]. As of yet, no confirmed case has been found in Bangladesh (The Daily Star 2022). In May of 2022, however, Bangladesh issued a health warning due to an outbreak of monkeypox worldwide [3].
The Democratic Republic of the Congo (DRC) performs routine surveillance for the monkeypox as it is endemic in this region [25], [4]. In DRC guidelines mandate for biweekly notification and incidence reporting and case investigations for suspected cases include specimen diagnosis and case report submission ([4]). WHO recommends reporting suspicious cases to public health authorities immediately, and case investigation should include a clinical assessment, possible sources identification and laboratory examination. Once a case is suspected, contact identification, contact tracing should be conducted immediately[34], [35], [36].
Monkeypox virus has been found to spread through direct contact with infectious rash, scabs or fluid from sores. Transmission through respiratory secretions and saliva during prolonged intimate physical contact including sex has been reported [6], [7], [8]. The secondary attack rate among unvaccinated contacts could be as high as 11% [5]. Healthcare-associated transmissions of MPXV were reported from central and west African countries (Yinka-Ogunleye et al., 2003; [21]; Lakhani et al., 2019; [37]). Enhancing the ability of healthcare professionals to identify cases and improve patient management is one of the most essential features of the surveillance system [4]. Healthcare professionals, especially medical doctors, should be familiar with the clinical symptoms of monkeypox in order to promptly detect, report, and treat new cases to prevent their spread.
A prior study in Indonesia, indicated that the understanding of HMPX among general practitioners (GPs) was quite low and approximately only 10% of them had a decent knowledge [13], [14]. Identified causative factors were: (a) no HMPX instances have been documented in Indonesia; and (b) the disease is not required to be taught in medical schools in the country according to the Indonesian Standard of Medical Doctor Competency [SKDI]. Due to these reasons the healthcare workers might not be able to handle an outbreak of HMPX [22], [13], [14]. Another report showed that a lack of knowledge about monkeypox, especially among healthcare workers, was one of the things that made it hard to stop the disease from coming back [33]. The recent growing incidence of human monkeypox cases necessitates prevention, early detection, prompt response and management by healthcare providers. Therefore, it is crucial for healthcare workers to be knowledgeable and prepared for monkeypox cases. No study so far has been conducted to assess the status of knowledge and attitude regarding monkeypox among Bangladeshi medical doctors. Hence, the present study was designed and undertaken to assess the knowledge regarding monkeypox and attitude towards its prevention among Bangladeshi medical doctors.
Methodology
Study design
This was a cross-sectional study among practicing medical doctors all over Bangladesh. Data was collected between 26th May 2022–4 th June. The researchers developed a semi-structured questionnaire. The questionnaire was circulated via the internet in the professional forum of Bangladeshi doctors. Those who gave consent participated in this study and submitted the questionnaire in Google form. The questionnaire was developed in English. Before circulating the questionnaire to the target population, it was pre-tested among 10 medical doctors. Based on their feedback, the final version was created and data collection was done.
Measures
One of the main purposes of the study was to assess the knowledge and attitude toward Human Monkeypox among Bangladeshi physicians. Based on the goal and to collect potential explanatory variables, it was divided into two sections, a) knowledge, and b) attitude. Knowledge is the understanding of facts and processes, which is acquired though information and experiences. And attitude is the feeling towards someone or something, which results readiness to act or behave in a certain way [26]. The explanatory variables were (a) Sociodemographic items; (b) Workplace characteristics; (c) Characteristics of the medical professional; and (d) Exposure to monkeypox-related information. There were 24 questions in the knowledge section and 6 questions in the attitude section. Questions were adapted from previous studies [13], [14]. The correct answers were determined based on guidelines and factsheets for monkeypox [34], [35], [36], [6], [7], [8]. For the knowledge domain, correct answer received a score of 1 and incorrect answers received a score of zero. The scores were added together to give a total knowledge score that ranges from 0 to 24, where a higher score indicates better knowledge. Regarding attitude, the questions were scored on a 3-point Likert scale (disagree, neither agree nor disagree, agree). The responses are given as 1 for ‘disagree’, 2 for ‘neither disagree or agree’ and 3 for ‘agree’. Scores were added to give an overall score of 6–18 for attitudes, where a higher score indicates a more positive attitude towards the monkeypox preventive measures.
Statistical analysis
Respectively, 70% and 80% of total values were considered as the cut-off point for defining good knowledge and positive attitude. Categorical and continuous variables were presented as frequency (percentage) and mean± standard deviation (SD), respectively. Univariate followed by multivariable logistic regression analyses were performed to identify factors associated with good knowledge and positive attitude. The outcomes were presented as odds ratios (ORs) with corresponding 95% confidence intervals (CIs). P-values< 0.05 were considered statistically significant, and statistical software R version 4.2.0 was used for data analysis.
Ethical consideration
Ethical approval was obtained from the Institutional Review Board (IRB)/Ethical Review Committee (ERC) of North South University (2022/0R-NSU/IRB/0501). The purpose of the study was elaborately explained in the online questionnaire form and a consent script was included. Those who consented participated in this study. Participants’ privacy and data safety were strictly maintained according to the IRB instruction and ethical standards of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards were followed wherever applicable.
Result
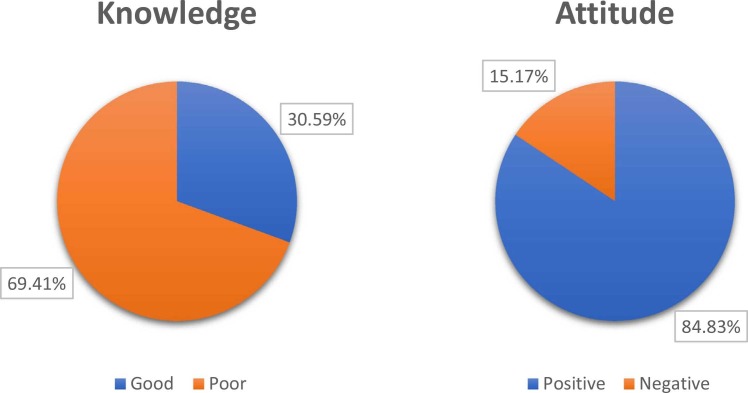
A total of 389 respondents who met the inclusion criteria voluntarily took part in this survey and were included in the final statistical analysis. The majority of our participants were female medical doctors (52.7%), aged less than 30 years (52,7%), graduated from government institutes (50.13%), worked in private hospitals (57.58%), with no post-graduate degree (83.55%) and practicing for less than 5 years (51.41%). Only 29.05% of doctors admitted learning information on monkeypox in their medical curriculum, and 82.26% learned about monkeypox within the last month prior to the survey. Among all, 119 (30.59%) doctors had good knowledge of monkeypox disease, its causation, symptoms, transmissions, and treatment. However, over four fifths (n = 330, 84.83%) of the participants displayed a positive attitude ( Fig. 1 & Table 1). All the responses to knowledge and attitude questions with their responses are provided in the supplementary file (Table S1, Table S2).
Fig. 1.
Distribution of knowledge and attitude level regarding monkeypox (Good knowledge was defined as having>70% score and good attitude was defined as having>80% score).
Table 1.
Knowledge and attitude of participants in terms of sociodemographic and professional characteristics.
| Variable | Frequency n (%) | Knowledge |
Attitude |
||
|---|---|---|---|---|---|
| Poor | Good | Negative | Positive | ||
| Age | |||||
| < 30 | 205 (52.7) | 146 (71.22) | 59 (28.78) | 41 (20) | 164 (80) |
| ≥ 30 | 184 (47.3) | 124 (67.39) | 60 (32.61) | 18 (9.78) | 166 (90.22) |
| Gender | |||||
| Female | 205 (52.7) | 144 (70.24) | 61 (29.76) | 30 (14.63) | 175 (85.37) |
| Male | 184 (47.3) | 126 (68.48) | 58 (31.52) | 29 (15.76) | 155 (84.24) |
| Institute | |||||
| Govt. Institute | 195 (50.13) | 136 (69.74) | 59 (30.26) | 28 (14.36) | 167 (85.64) |
| Private Institute | 194 (49.87) | 134 (69.07) | 60 (30.93) | 31 (15.98) | 163 (84.02) |
| Workplace | |||||
| Govt. Hospital | 140 (35.99) | 94 (67.14) | 46 (32.86) | 18 (12.86) | 122 (87.14) |
| Only Private Chamber/GP | 25 (6.43) | 19 (76) | 6 (24) | 6 (24) | 19 (76) |
| Private Hospital | 224 (57.58) | 157 (70.09) | 67 (29.91) | 35 (15.63) | 189 (84.37) |
| Education | |||||
| Graduate (MBBS) | 325 (83.55) | 233 (71.69) | 92 (28.31) | 54 (16.62) | 271 (83.38) |
| Postgraduate (Completed) | 64 (16.45) | 37 (57.81) | 27 (42.19) | 5 (7.81) | 59 (92.19) |
| Got information about monkeypox | |||||
| No | 276 (70.95) | 207 (75) | 69 (25) | 41 (14.86) | 235 (85.14) |
| Yes | 113 (29.05) | 63 (55.75) | 50 (44.25) | 18 (15.93) | 95 (84.07) |
| Learned about monkeypox | |||||
| Before last 1 month | 69 (17.74) | 33 (47.83) | 36 (52.17) | 11 (15.94) | 58 (84.06) |
| Within last 1 month | 320 (82.26) | 237 (74.06) | 83 (25.94) | 48 (15) | 272 (85) |
| Duration of medical practice | |||||
| < 5 years | 200 (51.41) | 132 (66) | 68 (34) | 35 (17.5) | 165 (82.5) |
| ≥ 5 years | 189 (48.59) | 138 (73.02) | 51 (26.98) | 24 (12.7) | 165 (87.3) |
Univariate regression analysis identified level of education, getting information about monkey pox in medical curriculum and the time of learning about monkeypox to be significantly associated with good knowledge about monkey pox. Those that completed post-graduation degree, got information about monkey pox in medical curriculum had higher odds of having good knowledge regarding monkey pox (OR=1.85 and OR=2.38, respectively). And those that learned about monkeypox within the last month had lower odds ratio of 0.32 (95% CI= 0.19, 0.55) ( Table 2: Univariate logistic regression analysis exploring factors associated with good knowledge and attitude about monkeypox among medical doctors). In case of attitude, older participants displayed higher odds of having positive attitude (OR=2.31, 95% CI=1.29, 4.27).
Table 2.
Univariate logistic regression analysis exploring factors associated with good knowledge and attitude about monkeypox among medical doctors.
| Model for | Knowledge |
Attitude |
||||||
|---|---|---|---|---|---|---|---|---|
| Variables | OR | 95% Confidence Interval |
p-value | OR | 95% Confidence Interval |
p-value | ||
| Lower | Upper | Lower | Upper | |||||
| Age | ||||||||
| < 30 years | Ref. | Ref. | ||||||
| ≥ 30 years | 1.20 | 0.78 | 1.85 | 0.414 | 2.31 | 1.29 | 4.27 | 0.006 |
| Gender | ||||||||
| Female | Ref. | Ref. | ||||||
| Male | 1.09 | 0.71 | 1.67 | 0.706 | 0.92 | 0.53 | 1.60 | 0.757 |
| Institute | ||||||||
| Govt. Institute | Ref. | Ref. | ||||||
| Private Institute | 1.03 | 0.67 | 1.60 | 0.886 | 0.88 | 0.50 | 1.54 | 0.656 |
| Workplace | ||||||||
| Govt. Hospital | Ref. | Ref. | ||||||
| Only Private chamber/GP | 0.65 | 0.22 | 1.64 | 0.383 | 0.47 | 0.17 | 1.42 | 0.153 |
| Private Hospital | 0.87 | 0.55 | 1.38 | 0.555 | 0.80 | 0.42 | 1.45 | 0.467 |
| Education | ||||||||
| Graduate (MBBS) | Ref. | Ref. | ||||||
| Post-graduate (Completed) | 1.85 | 1.06 | 3.2 | 0.029 | 2.35 | 0.99 | 6.97 | 0.080 |
| Got information about monkeypox | ||||||||
| No | Ref. | Ref. | ||||||
| Yes | 2.38 | 1.50 | 3.78 | < 0.001 | 0.92 | 0.51 | 1.72 | 0.789 |
| Learned about monkeypox | ||||||||
| Before last 1 month | Ref. | Ref. | ||||||
| Within last 1 month | 0.32 | 0.19 | 0.55 | < 0.001 | 1.07 | 0.50 | 2.13 | 0.843 |
| Duration of medical practice | ||||||||
| < 5 years | Ref. | Ref. | ||||||
| ≥ 5 years | 0.72 | 0.46 | 1.11 | 0.134 | 1.46 | 0.84 | 2.58 | 0.189 |
Note: Reference category for both knowledge and attitude is Poor and p value< 0.05 indicates significant
Multivariate logistic regression analysis revealed a statistically significant association of whether they got any information about monkeypox in the medical curriculum or not and the time of learning about monkeypox with good knowledge regarding monkeypox ( Table 3) when adjusted for other covariates. Getting information about monkeypox at any point in their medical academic curriculum were associated with a significant aOR value of 1.83 (95% CI=1.11, 3.01). However, learning about monkeypox within the last month showed lower odds ratio (aOR=0.43) of possessing good knowledge compared to those who learned about it before one month. Although in the univariate model education of the participant showed significant association, in multivariate model it was observed to be not significant (aOR=1.67, 95% CI=0.94, 2.96) when adjusted for other covariates. Only age of a participant showed a significant statistical association with positive attitude in the logistics regression model (aOR=2.31, 95% CI=1.29, 4.27) (Table 3).
Table 3.
Multivariate logistic regression analysis exploring factors associated with good knowledge and attitude about monkeypox among medical doctors.
| Model for | Variables | aOR | 95% Confidence Interval |
p-value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Knowledge | Education | ||||
| Graduate (MBBS) | Ref. | ||||
| Post-graduate (Completed) | 1.67 | 0.94 | 2.96 | 0.078 | |
| Got information about monkeypox | |||||
| No | Ref. | ||||
| Yes | 1.83 | 1.11 | 3.01 | 0.017 | |
| Learned about monkeypox | |||||
| Before last 1 month | Ref. | ||||
| Within last 1 month | 0.43 | 0.24 | 0.76 | 0.004 | |
| Attitude | Age | ||||
| < 30 years | Ref. | ||||
| ≥ 30 years | 2.31 | 1.29 | 4.27 | 0.006 | |
Note: Reference category for both knowledge and attitude is Poor and p value< 0.05 indicates significant
Statistically significant association was found between knowledge and attitude of a participant; out of 119 doctors scored good in knowledge, 110 (92.44%) scored 80% or more in the attitude domain ( Table 4).
Table 4.
Association between knowledge and attitude related to monkeypox among medical doctors.
| Knowledge | Attitude |
p-value | |
|---|---|---|---|
| Positive | Negative | ||
| Good | 110 | 9 | 0.009 |
| Poor | 220 | 50 | |
Note: p-value< 0.05 indicates significant.
Overall, participants had a better attitude despite the overwhelming poor knowledge of monkeypox.
Discussion
After overcoming the COVID-19 pandemic for two years, new zoonotic monkeypox virus transmission has recently been reported in many non-endemic nations. Although it is an unusual, self-limiting infection that is generally milder than smallpox and is not a cause for alarm at this time, early discovery and prompt action are crucial for disease control [31]. To effectively combat this epidemic, all governments and their respective public health departments should be on high alert and work together closely. People must be informed about the disease's treatment options and preventative and risk factors via massive awareness initiatives. The frontline medical professionals need to be educated on handling confirmed or suspected cases and protecting themselves while doing so. It is essential for medical professionals and physicians, in particular, to have a sufficient grasp of this condition to completely detect, diagnose, and treat instances of it. Only then can the disease be managed effectively.
According to our study's findings, the knowledge level about monkeypox among doctors in Bangladesh is inadequate. Approximately 31% were capable of providing accurate responses to 70% or more of the 24 questions. In a similar study, general practitioners in Indonesia knew relatively little about the emerging infection known as monkeypox [13], [14]. In contrast, regarding endemic diseases in Bangladesh, the level of knowledge is rather high; most doctors are well-versed in diseases such as "dengue," which are transmitted by Aedes aegypti [18]. It should not come as a surprise that participants in general lack awareness about monkeypox since it is a re-emerging infectious disease, and instances of it have never been documented in Bangladesh. Another possible reason behind this fact is that, due to time constraints, medical students in Bangladesh may be mainly focused on common diseases. Because of this, medical graduates are not expected to be able to treat or manage this condition altogether.
The study also reveals a positive attitude towards monkeypox and its prevention among doctors as more than 84% had a good score in the attitude domain. A similar finding was observed in a study conducted in Conakry, Guinea, during the Ebola virus outbreak [2]. The reason behind this positive attitude is that the physicians are already worn down by their experiences with COVID-19 and are aware of the repercussions of a pandemic. Because of this, they exhibited a positive attitude toward learning about this virus, and they are highly willing to take the necessary steps to avoid the virus's spread and to follow the treatment protocol. According to the findings of this research, education was not found to be significantly associated with good knowledge or positive attitude. However, older age was found to be associated with positive attitude. This is because as one gets older, they can amass more experience, increase their depth of knowledge and increase positivity in their attitude. However, the results of this research demonstrated that a longer period of medical practice was associated with a decreased likelihood of having good knowledge. Similarly, a systematic review of 12 research published between 1966 and 2004 indicated that more years of experience in medical practice were associated with lower knowledge levels [9]. In this case, it can be said that, because of long-term clinical practice, medical professionals gain expertise in diagnosing and treating prevalent illnesses, but they become less aware of new diseases or infections.
We found that individuals who got information about monkeypox in curriculum of medical school and individuals who learned about monkeypox in the last one month became more knowledgeable about the disease. However, this is contrary to the findings in Indonesia, where there was no significant difference found in knowledge between physicians who received information on monkeypox as part of their medical education and those who did not [13], [14].
A statistically significant relationship was observed in our investigation between the individuals' knowledge levels and attitudes. These findings are consistent with the results reported studies carried out in Pakistan and Indonesia [12], [15], [16]. The conclusion that can be drawn from this is that one's level of knowledge can always influence one's attitude and that having a better comprehension of anything may lead to having a more positive attitude.
The study will be the first research of its kind to come out of Bangladesh, and it will help us gauge the scope of the status of knowledge and attitude regarding monkeypox in Bangladesh, and guide us to take necessary strategies to enhance KAP on further aspects of the issue. Survey results will inform an intervention approach reflective of local conditions and cultural influences; this will allow us to tailor our efforts to the target group's needs. However, it is crucial to acknowledge some of our study's limitations and the approaches we took to address them. Due to our study’s cross-sectional nature, we cannot infer causality for the associations we presented in this paper. Furthermore, in non-random studies, selection bias is always a possible drawback. Also, the fact that the questionnaire was self-administered is another constraint: our research findings are not generalizable since we used a convenience sample.
Conclusion
The attitude towards human monkeypox prevention among medical doctors in Bangladesh was quite good. However, the knowledge level regarding the virus was low. The study identified that presence of information regarding monkeypox in the medical curriculum and when a participant learned about monkeypox had a significant association with knowledge level. On the other hand, the participants’ attitude towards human monkeypox was satisfactory and only age of a participant had a significant association with attitude. Developing and implementing practical knowledge-sharing sessions to enhance the capacity of doctors regarding human monkeypox could be an effective strategy towards improving the current condition and preparing for any future outbreak.
CRediT authorship contribution statement
MH and MEH did the literature search. DHH, HTN and MASK conceived and designed the study. DHH, IJ and PD oversaw its implementation, analysis, and write-up. MASK planned the statistical analyses. MAH, MH and MEH outlined the data collection procedure. SC, MFR, MAH, MEH and IJ contributed to the field implementation of the study and did data entry. MASK, HTN and MAH verified the underlying data. PD did the statistical analyses. IJ, MFR, MEH, SC wrote the first draft of the manuscript. All authors read and approved the manuscript.
Conflict of interest
We have no conflict of interest to declare.
Acknowledgment
The authors in this study express their heartfelt gratitude for the those that participated in this study.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jiph.2022.11.032.
Appendix A. Supplementary material
Supplementary material
.
References
- 1.Africa CDC. Outbreak brief 11: Monkeypox in Africa union member states. [accessed 2022, October 08]. AFRICA CDC. 〈https://africacdc.org/disease-outbreak/outbreak-brief-11-monkeypox-in-africa-union-member-states/〉.
- 2.Alioune C. Knowledge, attitudes and practices of health care workers on Ebola in hospital towards Ebola virus disease, Conakry, guinea, 2016. Cent Afr J Publ Health. 2018;4(1):1. doi: 10.11648/j.cajph.20180401.11. [DOI] [Google Scholar]
- 3.Bangladesh declares health alert amid monkeypox outbreak. 2022. ANI News [Internet]. [accessed 2022 Jul 3]. 〈https://www.aninews.in/news/world/asia/bangladesh-declares-health-alert-amid-monkeypox-outbreak20220522183345/〉.
- 4.Bass J., Tack D.M., McCollum A.M., Kabamba J., Pakuta E., Malekani J., et al. Enhancing health care worker ability to detect and care for patients with monkeypox in the Democratic Republic of the Congo. Int Health. 2013;5(4):237–243. doi: 10.1093/inthealth/iht029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beer E.M., Rao V.B. A systematic review of the epidemiology of human monkeypox outbreaks and implications for outbreak strategy. PLoS Negl Trop Dis. 2019;13(10) doi: 10.1371/journal.pntd.0007791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC. 2022a. Monkeypox. Centers for Disease Control and Prevention [Internet]. [accessed 2022 Jul 3]. 〈https://www.cdc.gov/poxvirus/monkeypox/index.html〉.
- 7.CDC. (2022b, September 1). 2022 Monkeypox outbreak global map. Centers for Disease Control and Prevention. 〈https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html〉.
- 8.CDC. (2022c, September 16). How it spreads. Centers for Disease Control and Prevention. 〈https://www.cdc.gov/poxvirus/monkeypox/if-sick/transmission.html〉.
- 9.Choudhry N.K., Fletcher R.H., Soumerai S.B. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142(4):260–273. doi: 10.7326/0003-4819-142-4-200502150-00008. [DOI] [PubMed] [Google Scholar]
- 10.Durski K.N., McCollum A.M., Nakazawa Y., Petersen B.W., Reynolds M.G., Briand S., et al. Emergence of Monkeypox - west and central Africa, 1970-2017. MMWR Morb Mortal Wkly Rep. 2018;67(10):306–310. doi: 10.15585/mmwr.mm6710a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Erez N., Achdout H., Milrot E., Schwartz Y., Wiener-Well Y., Paran N., et al. Diagnosis of imported Monkeypox, Israel, 2018. Emerg Infect Dis. 2019;25(5):980–983. doi: 10.3201/eid2505.190076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ul Haq N., Hassali M.A., Shafie A.A., Saleem F., Farooqui M., Aljadhey H. A cross sectional assessment of knowledge, attitude and practice towards Hepatitis B among healthy population of Quetta, Pakistan. BMC Public Health. 2012;12(1):692. doi: 10.1186/1471-2458-12-692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harapan H., Setiawan A.M., Yufika A., Anwar S., Wahyuni S., Asrizal F.W., et al. Knowledge of human monkeypox viral infection among general practitioners: a cross-sectional study in Indonesia. Pathog Glob Health. 2020;114(2):68–75. doi: 10.1080/20477724.2020.1743037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harapan H., Setiawan A.M., Yufika A., Anwar S., Wahyuni S., Asrizal F.W., et al. Confidence in managing human monkeypox cases in Asia: A cross-sectional survey among general practitioners in Indonesia. Acta Trop. 2020;206(105450) doi: 10.1016/j.actatropica.2020.105450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harapan H., Rajamoorthy Y., Anwar S., Bustamam A., Radiansyah A., Angraini P., et al. Knowledge, attitude, and practice regarding dengue virus infection among inhabitants of Aceh, Indonesia: a cross-sectional study. BMC Infect Dis. 2018;18(1) doi: 10.1186/s12879-018-3006-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harapan H., Rajamoorthy Y., Utomo P.S., Anwar S., Setiawan A.M., Alleta A., et al. Knowledge and attitude towards pregnancy-related issues of Zika virus infection among general practitioners in Indonesia. BMC Infect Dis. 2019;19(1):693. doi: 10.1186/s12879-019-4297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ilic I., Zivanovic Macuzic I., Ilic M. Global outbreak of human Monkeypox in 2022: Update of epidemiology. Trop Med Infect Dis. 2022;7(10):264. doi: 10.3390/tropicalmed7100264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koonisetty K.S., Aghamohammadi N., Urmi T., Yavaşoglu S.İ., Rahman M.S., Nandy R., et al. Assessment of knowledge, attitudes, and practices regarding dengue among physicians: a web-based cross-sectional survey. Behav Sci. 2021;11(8):105. doi: 10.3390/bs11080105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kozlov M. How deadly is monkeypox? What scientists know. Nature. 2022;609(7928):663. doi: 10.1038/d41586-022-02931-1. [DOI] [PubMed] [Google Scholar]
- 21.Nakoune E., Lampaert E., Ndjapou S.G., Janssens C., Zuniga I., Van Herp M., et al. A nosocomial outbreak of human Monkeypox in the Central African Republic. Open Forum Infect Dis. 2017;4(4) doi: 10.1093/ofid/ofx168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ng O.T., Lee V., Marimuthu K., Vasoo S., Chan G., Lin R.T.P., et al. A case of imported Monkeypox in Singapore. Lancet Infect Dis. 2019;19(11):1166. doi: 10.1016/S1473-3099(19)30537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ogoina D., Izibewule J.H., Ogunleye A., Ederiane E., Anebonam U., Neni A., et al. The 2017 human monkeypox outbreak in Nigeria-Report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. PLoS One. 2019;14(4) doi: 10.1371/journal.pone.0214229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osadebe L., Hughes C.M., Shongo Lushima R., Kabamba J., Nguete B., Malekani J., et al. Enhancing case definitions for surveillance of human monkeypox in the Democratic Republic of Congo. PLoS Negl Trop Dis. 2017;11(9) doi: 10.1371/journal.pntd.0005857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pradhan H.B. A Textbook of Health Education (Philosophy and Principles) 2nd ed.., Educational Publishing House; Kathmandu: 2017. [Google Scholar]
- 28.Petersen E., Kantele A., Koopmans M., Asogun D., Yinka-Ogunleye A., Ihekweazu C., et al. Human Monkeypox: Epidemiologic and clinical characteristics, diagnosis, and prevention. Infect Dis Clin North Am. 2019;33(4):1027–1043. doi: 10.1016/j.idc.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shanmugaraj B., Phoolcharoen W., Khorattanakulchai N. Emergence of monkeypox: Another concern amidst COVID-19 crisis. Asian Pac J Trop Med. 2022;15(5):193. doi: 10.4103/1995-7645.346081. [DOI] [Google Scholar]
- 32.Vaughan A., Aarons E., Astbury J., Balasegaram S., Beadsworth M., Beck C.R., et al. Two cases of monkeypox imported to the United Kingdom, September 2018. Eur Surveill. 2018;23(38) doi: 10.2807/1560-7917.ES.2018.23.38.1800509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. Informal Consultation on Monkeypox 2017 [Internet]. [accessed 2022 Jul 3]. 〈https://apps.who.int/iris/bitstream/handle/10665/272620/WHO-WHE-IHM-2018.3-eng.pdf〉.
- 34.World Health Organization. Monkeypox. Who.int [Internet]. [accessed 2022a Jul 3]. 〈https://www.who.int/news-room/questions-and-answers/item/monkeypox〉.
- 35.World Health Organization. Multi-country monkeypox outbreak: situation update. (n.d.). Who.int. [accessed October 8, 2022b] from 〈https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON396〉.
- 36.World Health Organization. Surveillance, case investigation and contact tracing for monkeypox: interim guidance, [accessed 25 August 2022c]. Who.int; 〈https://www.who.int/publications/i/item/WHO-MPX-Surveillance-2022.3〉.
- 37.Yinka-Ogunleye A., Aruna O., Dalhat M., Ogoina D., McCollum A., Disu Y., et al. Outbreak of human monkeypox in Nigeria in 2017-18: a clinical and epidemiological report. Lancet Infect Dis. 2019;19(8):872–879. doi: 10.1016/S1473-3099(19)30294-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material