Abstract
We report the case of a 23-year-old woman with an erythematous, crusted patch of the scalp, lacking pustular lesions, with partial hair loss, developed after mechanical scalp trauma. Histopathological examination showed a dermal infiltrate, predominantly peri-adnexal and peri-vascular, rich in plasma cells and lymphocytes, but lacking neutrophils, possibly as a consequence of the time elapsed since the onset of the skin disease. Reduction of functional hair follicles was evidenced. Stains for bacterial or fungal infections were negative. Direct immunofluorescence was negative. Erosive pustular dermatosis of the scalp was diagnosed on the basis of clinical-anamnestic findings, supported by histology. Topical clobetasol propionate led to clinical improvement after a couple of weeks. Erosive pustular dermatosis of the scalp was diagnosed and soon after the patient developed also multiple sclerosis. Up to date, the pathogenesis of erosive pustular dermatosis of the scalp remains unknown, though a possible role of immunosenescence and autoimmunity has been suggested. Indeed, high levels of neutrophil-stimulating cytokines and chemokines have been found in erosive pustular dermatosis patients, possibly causing activation of an aberrant systemic neutrophilic reaction. Furthermore, the role of neutrophils has been recently highlighted also in the pathogenesis of multiple sclerosis. Herein we hypothesize a possible common immunological etiology of multiple sclerosis and erosive pustular dermatosis of the scalp, conceivably involving a hyperactivation of neutrophils.
Key words: hair loss, multiple sclerosis, pustules scalp, scalp, scarring alopecia
Introduction
Erosive pustular dermatosis of the scalp (EPDS) is a chronic inflammation of the scalp, with typical confluent sterile pustules, evolving into brownish crusts and occasional erosions, possibly leading to subsequent scarring alopecia.1
Usually, it is induced by local trauma, especially mechanic injuries and burns, but also, skin grafts, infections and topical treatments have been advocated in its etiology. 2-4
Associations of EPDS with autoimmune diseases such as Hashimoto’s thyroiditis, autoimmune hepatitis Takayasu’s arteritis, rheumatoid arthritis, and myasthenia gravis, have been reported, as well as with systemic conditions such as herpes zoster infection, myelodysplastic syndrome, Kindler syndrome and Klippel-Feil syndrome. 5
Case Report
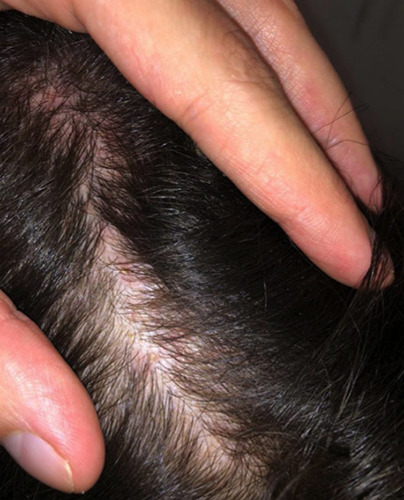
We report the case of a 23-year-old woman presenting with an erythematous, crusted patch of the scalp, lacking pustular lesions, with partial hair loss, developed two weeks after a severe mechanical scalp trauma, as shown in Figure 1.
Histopathological examination was aspecific, showing epidermal orthohyperkeratosis, spongiosis, and a dermal infiltrate, predominantly peri-adnexal and peri-vascular, rich in plasma cells and lymphocytes, but lacking neutrophils, possibly as a consequence of the time elapsed since the onset of the skin disease. Reduction of functional hair follicles was evidenced. Stains for bacterial or fungal infections were negative. Direct immunofluorescence was negative.
Topical clobetasol propionate led to clinical improvement after a couple of weeks as shown in Figure 2.
One month after, the patient developed optic neuritis. Nervous system MRI, showing multiple plaques, and subsequent lumbar puncture, showing antibodies abnormalities, permitted to diagnose multiple sclerosis (MS).
Corticosteroid boluses were administered with benefit of both diseases.
Erosive pustular dermatosis of the scalp (EPDS) was diagnosed on the basis of characteristic cutaneous clinical-anamnestic findings, such as the poorly healing lesions with non-follicular confluent crusts, and ex juvantibus with the excellent response to topical steroids. The diagnosis was supported by aspecific histology, negativity of immunofluorescence and microbial studies, excluding differential diagnoses.
Discussion
The diagnosis of EPDS is essentially clinical, based on the history of recent trauma combined with characteristic clinical appearance of chronic, poorly healing lesions with non-follicular confluent pustules and crusts, and with the excellent response to topical steroids.2
Histology is aspecific and mainly excludes differential diagnoses, including non-melanoma skin cancer, folliculitis decalvans and psoriasis of the scalp. However, dermal infiltrates of plasma cells and peri-vascular lymphocytes have been recently identified as diagnostic clues of EPDS.1
Also, immunofluorescence and microbial studies are prevalently used to exclude other similar conditions as bacterial or mycotic infections as Kerium Celsi, pemphigus foliaceous, cicatricial pemphigoid of Brunsting-Perry.1,2
Treating EPDS may require long-term management with high-potency topical corticosteroids or topical calcineurin inhibitors, which are considered first-line therapy. Oral corticosteroids, acitretin, dapsone gel and topical calcipotriol may be used as second-line therapies.4
Up to date, the pathogenesis of EPDS remains unknown, though a possible role of immunological senescence and autoimmunity has been suggested.1-6
Interestingly, in a patient with EPDS and myasthenia gravis, Yu Sawada et al. found high levels of neutrophil-stimulating cytokines and chemokines, (G-CSF, IL-6, and IL-8), which might be involved in the activation of an aberrant systemic neutrophilic reaction, shedding a light on the possible involvement of neutrophilic hyperactivation in the pathogenesis of EPDS, which seems to be in common with MG.4
Furthermore, the role of neutrophils has been recently highlighted also in the pathogenesis of MS: spikes in plasma levels of CXCL5, have been associated with the development of new lesions in relapsing remitting MS.5 The presented case is noteworthy suggesting a possible common immunological etiology of MS and EPDS, conceivably involving the hyperactivation of neutrophils, though this thesis would need to be confirmed by further studies.
Figure 1.

Clinical presentation of erosive pustular dermatosis of the scalp with erythematous crusted patch of the scalp with initial hair loss, but lack of pustules.
Figure 2.
Resolution of crusts with almost complete restitutio ad integrum of the scalp after topical steroid therapy.
Conclusions
Though the association of EPDS and MS in the presented case is likely casual, the two diseases were almost concomitant, suggesting a possible connection. Therefore, we hypothesize a possible common immunological etiology of MS and EPDS, conceivably involving a systemic hyperactivation of neutrophils; this is however just a hypothesis which would need to be confirmed by further studies.
Funding Statement
Funding: None.
References
- 1.Parodi A, Ciaccio M, Rebora A. Erosive pustular dermatosis of the scalp. Int J Dermatol 1990;29:517-8. [DOI] [PubMed] [Google Scholar]
- 2.Reschke R, Grunewald S, Paasch U, et al. Erosive pustular dermatosis of the scalp: clinicopathological correlation leading to a definition of diagnostic criteria. Wounds 2021;33:143-6. [PubMed] [Google Scholar]
- 3.Michelerio A, Vassallo C, Fiandrino G, Tomasini CF. Erosive Pustular Dermatosis of the Scalp: A Clinicopathologic Study of Fifty Cases. Dermatopathology (Basel) 2021;8:450-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sawada Y, Bito T, Kawakami C, et al. Erosive pustular dermatosis of the scalp and leg associated with myasthenia gravis: A possible pathogenetic role for neutrophil-stimulating cytokines and chemokines. Acta Derm Venereol 2010;90:652-3. [DOI] [PubMed] [Google Scholar]
- 5.Karanfilian KM, Wassef C. Erosive pustular dermatosis of the scalp: causes and treatments. Int J Dermatol 2021;60: 25-32 [DOI] [PubMed] [Google Scholar]
- 6.Rumble JM, Huber AK, Krishnamoorthy G, et al. Neutrophilrelated factors as biomarkers in EAE and MS. J Exp Med 2015;212:23-35. [DOI] [PMC free article] [PubMed] [Google Scholar]


