Abstract
Scleredema of Buschke is a rare connective tissue disease with a poorly understood pathogenesis. Three types of scleredema have been distinguished according to its association with preceding or underlying conditions. Type 1 is usually secondary to a febrile infection, type 2 is mostly associated with paraproteinemia and type 3, usually named scleredema diabeticorum, has a strict association with Diabetes mellitus. A diffuse, non-pitting swelling and induration of the skin define this disease. The skin histology is characterized by a normal or slightly thinned epidermis, and the dermis containing a decreased number of elastic fibers and thick large swollen collagen bundles separated by mucopolysaccharide deposits in the deep reticular dermis. In this report we present a 58-year-old man with scleredema diabeticorum controlled with a topical steroid cream and an optimization of glycemic control. We reviewed clinical, histopathological characteristics and the various possible treatments.
Key words: Scleredema, Diabetes, Treatment
Introduction
Scleredema of Buschke is a rare, scleromucinous, connective tissue disorder characterized by symmetrical, diffuse induration of the skin due to accumulation of collagen and aminoglycans in the dermis of unknown aetiology.1 Severe cases of scleredema may present restrictive defect in pulmonary and cardiac function with a pathogenesis that remains unknown.2
Three types of scleredema have been distinguished according to its association with preceding or underlying conditions. Type 1 (55%) is usually secondary to a febrile infection and affects mainly children. Type 2 (25%) is mostly associated with paraproteinemia and type 3 (20%), usually named scleredema diabeticorum or scleredema adultorum of Buschke, has a strict association with Diabetes mellitus.1,3,4
Scleredema diabeticorum is characterized by thickening and tightening of the skin, which typically starts at the neck and progresses downward and laterally.4 Its natural history is variable, and some patients can experience spontaneous remission.5 For most the clinical course is chronic and treatment options are limited.6
Case Report
A 58-year-old male presented to the Dermatology Department with longstanding (duration otherwise undisclosed) pruritus on the nape of the neck and upper back. His past medical history included: 1) a diagnosis of Diabetes mellitus, 20 years ago, on metformin and linagliptin, with suboptimal control (HgbA1c 8,2%); 2) several periods of depression for the last 10 years; and 3) cigarette smoking, namely a pack of cigarettes a day, for the past 40 years. Physical examination was remarkable for a diffuse hardening and papulation of the skin on his neck and upper back, erythema especially on the neck (Figure 1) and also on the face (rubeosis faciei diabeticorum). There was no involvement of upper and lower limbs, hands or feet. He denied any additional symptoms, including tightness or pain. He denied any previous treatments.
Histology revealed a normal epidermis, with widening of the gaps between thickened collagen fibers on the reticular dermis, separated by the deposition of a bluish amorphous substance, highlighted with Alcian blue staining (Figure 2). These findings were consistent with the clinical diagnosis of scleredema adultorum.
The patient was prescribed a potent topical steroid cream and a close follow-up strategy was recommend in order to optimize glycemic control.
Discussion
Scleredema of Buschke is a rare connective tissue disease with a poorly understood pathogenesis. First described by Curizo in 1752, the disease was better defined in 1902 and classified in 1968 into three main groups according to the age of onset and associated or preceding illnesses.3,7 The classic form, or type 1, is self-limited, lasts from several months to two years, and is associated with febrile disease. The most common infection associated with type 1 is streptococcal or viral respiratory tract infection. Type 2, which is often more durable, is associated with paraproteinemias or other malignancies, such as insulinoma and carcinoma of the gallbladder. 1 The third type may be referred to as scleredema diabeticorum. It affects 2.5% to 14% of all diabetic patients, with a male preponderance of 10:1. Individuals often have a long history of poor metabolic control, obesity, as well as other diabetic complications as severe diabetic vascular complications. 2 However, cases of scleredema diabeticorum in diabetics with controlled glucose have been reported. It has not been reported in children.3,8
In diabetes associated scleredema, an irreversible glycosylation of collagen leads to an excessive accumulation of collagen and mucin, which synthesis is stimulated by microvascular damage and hypoxia.7
The condition is characterized by firm, non-pitting edema typically beginning at the neck and spreading to the face, scalp, shoulders and trunk, characteristically sparing the hands and feet.7 Erythema and a peau d’orange appearance may be present, with indistinct demarcation between normal and abnormal skin.8
Diagnosis of scleredema is made clinically, with a definite diagnosis confirmed by histopathology.1 This usually shows a normal or slightly thinned epidermis, and the dermis containing a decreased number of elastic fibers and thick large swollen collagen bundles, particularly type 1 collagen, separated by mucopolysaccharide deposits in the deep reticular dermis.1,8 Mucin deposits represent non-sulphated acid mucopolysacharides, mainly hyaluronic acid (stable with Alcian blue dye, colloidal iron or toluidine blue). Fibroblasts are usually normal in number and morphology. The subcutaneous fat is replaced by coarse collagen fibres and the skin adnexae pushed upwards.1
Identification and treatment of the underlying cause is required. In scleredema type 1, antibiotics are indicated in the case of streptococcal infection. Patients of type 2 require management by a hematologist. Tight control of diabetes and weight is urged for type 3 patients.3,9 Two series that studied these patients, one with 4 type 1 diabetics, showed that a decrease in HgbA1c from 9.3 to 7.9% produced a significant improvement of the scleredema, similiarly to 5 other patients (from 11) that partially improved their scleredema.2 However other reports did not find any skin improvement after optimizing glucose control.2
Direct skin treatments that have shown to be effective include Ultraviolet A-1 (UVA-1) phototherapy and psoralen with ultraviolet A (PUVA).2 Out of all treatments reported, UVA-1 and PUVA light phototherapy have apparently the most successful results.2 The addition of colchicine to PUVA revealed to be a positive combination. 10 Allopurinol has been shown to have some antioxidant effects.11
Other treatments classically used are immunomodulators like corticosteroids, cyclosporine and methotrexate, despite inconsistent results.2,12,13 Due to concerns over adverse effects, these options should be reserved for patients with persistent, debilitating disease in whom phototherapy failed or for patients with scleredema-associated multiple myeloma.9
There are some cases describing intravenous immunoglobulin use.5,6 Some case reports also describe treatment with radiotherapy and prostaglandin E1, 4, 5.8 Other novel therapies have recently been suggested, such as tranilast.12
No treatment has nevertheless been shown to be consistently effective in large numbers of patients.6 The lack of randomized controlled trials about scleredema maintains some uncertainty over the best treatment regimens, optimum dose and long-term efficacy.6 Therefore, each treatment decision should be made individually, accounting for patient’s concomitant diseases, scleredema extent (size and localization), and possible trigger factors. Combination therapy should be tried. Adjuvant local therapy with corticosteroids or with physical therapy in patients’ musculoskeletal limitations or with motion or respiratory disability may be worthwhile.5,9,14 Patients should be informed that most of the treatment modalities are off-label use and that they may fail to fulfil the patient’s hopes and expectations.
Figure 1.
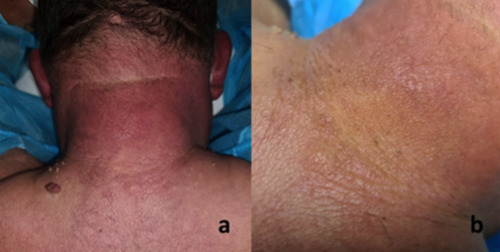
a) Erythematous induration of the posterior neck and upper back with scant excoriations; b) highlight with skin surface papulation and peau d’orange appearance.
Figure 2.
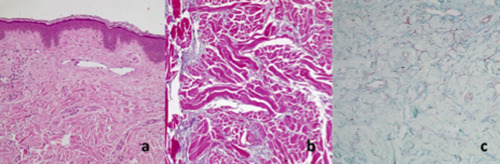
a) normal epidermis (H&E×10); b) widening between thickened reticular dermis collagen fibers interspersed by mucin deposition (H&E×40); c) mucin deposition (Alcian blue×40).
Conclusions
In this case our initial approach was directed at controlling pruritus, diabetes and weight due to essentially a localized form of disease. We’ll keep this strategy along with follow-up and if necessary, add other treatment options.
There are different approaches for the treatment of scleredema diabeticorum. Tight glycemic control is recommended irrespective of its lack of proven effectiveness on established skin lesions. Several direct skin treatment modalities are available. UVA-1 phototherapy and PUVA seem to be the most effective treatments for this condition. Combination therapy seems to be the break-even point.
Acknowledgements
The authors thank the patient who participated in this case report
Funding Statement
Funding: None.
References
- 1.Knobler R, Moinzadeh P, Hunzelmann N, et al. European dermatology forum S1-guideline on the diagnosis and treatment of sclerosing diseases of the skin, Part 2: Scleromyxedema, scleredema and nephrogenic systemic fibrosis. J Eur Acad Dermatol Venereol 2017;31:1581-94. [DOI] [PubMed] [Google Scholar]
- 2.Martín C, Requena L, Manrique K, et al. Scleredema diabeticorum in a patient with type 2 diabetes mellitus. Case Rep Endocrinol 2011;2011:560273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raboudi A, Litaiem N. Scleredema. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. [Google Scholar]
- 4.Namas R, Ashraf A. Scleredema of Buschke. Eur J Rheumatol 2016;3:191-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miguel D, Schliemann S, Elsner P. Treatment of Scleroedema Adultorum Buschke: A Systematic Review. Acta Derm Venereol 2018;98:305-9. [DOI] [PubMed] [Google Scholar]
- 6.Kennemer C, Pavlidakey P, Sami N. Successful treatment with IVIg therapy of diabetes-associated scleredema severe progressive case and review of the literature. Dermatol Ther 2017;30:10. [DOI] [PubMed] [Google Scholar]
- 7.Muhaidat J, Al-Qarqaz F, Alshiyab D. Unilateral Linear Induration of the Skin: A Case Report of an Unusual Presentation of Scleredema. J Clin Aesthet Dermatol 2020;13:E53-5. [PMC free article] [PubMed] [Google Scholar]
- 8.Shazzad MN, Azad AK, Abdal SJ, et al. Scleredema Diabeticorum - A Case Report. Mymensingh Med J. 2015;24:606-9. [PubMed] [Google Scholar]
- 9.Rongioletti F, Kaiser F, Cinotti E, et al. Scleredema. A multicentre study of characteristics, comorbidities, course and therapy in 44 patients. J Eur Acad Dermatol Venereol 2015;29:2399-404. [DOI] [PubMed] [Google Scholar]
- 10.Kokpol C, Rajatanavin N, Rattanakemakorn P. Successful Treatment of Scleredema Diabeticorum by Combining Local PUVA and Colchicine: A Case Report. Case Rep Dermatol 2012;4:265-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee FY, Chiu HY, Chiu HC. Treatment of acquired reactive perforating collagenosis with allopurinol incidentally improves scleredema diabeticorum. J Am Acad Dermatol 2011;65:e115-7. [DOI] [PubMed] [Google Scholar]
- 12.Simó-Guerrero O, Recasens-Gracia A, Giménez-Pérez G. Scleredema diabeticorum: Description of 11 cases. Escleredema diabeticorum: descripción de 11 casos. Med Clin (Barc) 2020;154:371-2. [DOI] [PubMed] [Google Scholar]
- 13.Doğramacı AÇ, Inan MU, Atik E, Gökçe C. Scleredema diabeticorum partially treated with low-dose methotrexate: a report of five cases. Balkan Med J 2012;29:218-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mickel M, Jalili A, Gesslbauer C, Crevenna R. Implementation and evaluation of a rehabilitation concept in a patient suffering from Scleredema Adultorum Buschke: a case report. Disabil Rehabil 2018;40:2833-5. [DOI] [PubMed] [Google Scholar]


