Abstract
Aspergillus species are the most frequent cause of fungal infections of the lungs with a broad spectrum of clinical presentations including invasive pulmonary aspergillosis (IPA) and chronic pulmonary aspergillosis (CPA). IPA affects immunocompromised populations, which are increasing in number and diversity with the advent of novel anti-cancer therapies. Moreover, IPA has emerged as a complication of severe influenza and coronavirus disease 2019 in apparently immunocompetent hosts. CPA mainly affects patients with pre-existing lung lesions and is recognised increasingly frequently among patients with long-term survival following cure of tuberculosis or lung cancer. The diagnosis of pulmonary aspergillosis is complex as it relies on the presence of clinical, radiological and microbiological criteria, which differ according to the type of pulmonary aspergillosis (IPA or CPA) and the type of patient population. The management of pulmonary aspergillosis is complicated by the limited number of treatment options, drug interactions, adverse events and the emergence of antifungal resistance.
Short abstract
The clinical spectrum of pulmonary aspergillosis has broadened with the recognition of novel patient populations at risk and the emergence of resistance, which poses important diagnostic and therapeutic challenges for clinicians https://bit.ly/3R6Cf6Z
Introduction
Aspergillosis, caused predominantly by Aspergillus fumigatus, is the most frequent mould infection of the lungs. The spectrum of the disease is broad and depends on the immune status of the host. A. fumigatus can cause allergic reactions in the lungs of patients with asthma or cystic fibrosis known as allergic bronchopulmonary aspergillosis (ABPA) [1]. Chronic pulmonary aspergillosis (CPA) affects individuals who are immunocompetent or mildly immunocompromised and have underlying lung disease, such as chronic obstructive pulmonary disease, sequelae of tuberculosis, nontuberculous mycobacterial infections or lung cancer [2]. There are distinct patterns of CPA with overlapping clinical presentations ranging from simple aspergilloma (a fungus ball within an existing cavity) to chronic cavitary, fibrosing and microinvasive forms of pulmonary aspergillosis [2]. Subacute invasive aspergillosis, also known as semi-invasive or chronic necrotizing aspergillosis, refers to a chronic pulmonary form of the disease evolving towards invasion and necrosis of adjacent lung tissues in mildly immunocompromised patients [2]. Acute invasive pulmonary aspergillosis (IPA) affects patients who present with various degrees of immune suppression in the context of haematologic malignancies, chemotherapy-induced neutropenia or immunosuppressive therapies for autoimmune disorders or following bone marrow or solid organ transplantation [3]. IPA has also emerged among intensive care unit (ICU) patients under mechanical ventilation for severe influenza or coronavirus disease 2019 (COVID-19) and who are apparently immunocompetent [4–6].
Aspergillus fumigatus represents by far the most common cause of aspergillosis, followed by Aspergillus flavus (more predominant in some regions of Africa or Asia), Aspergillus terreus and Aspergillus niger [7, 8]. Other pathogenic species account for less than 3% of cases and include Aspergillus nidulans, Aspergillus calidoustus, Aspergillus glaucus, Aspergillus versicolor and some cryptic species (e.g. Aspergillus lentulus, Aspergillus udagawae).
Pulmonary aspergillosis poses a diagnostic and therapeutic challenge because of the modest sensitivity and specificity of diagnostic tests resulting in frequent diagnostic and therapeutic delays, limited therapeutic options, significant drug interactions (especially for triazoles), adverse events, and the emergence of resistance. The purpose of this review is to discuss current diagnostic and therapeutic approaches, recent advances and future perspectives in the management of IPA and CPA. Allergic Aspergillus diseases (i.e. ABPA) will not be discussed here.
Diagnosis
IPA
Because of the paucity of clinical signs and the limited sensitivity and/or specificity of radiology and mycological tests, the diagnosis of IPA is graded according to a scale of probability (possible, probable or proven) of disease. The European Organization for Research and Treatment of Cancer and Mycoses Study Group Education and Research Consortium (EORTC-MSGERC) has established definitions for the diagnosis of possible, probable and proven IPA in immunocompromised patients [9]. These definitions rely on host criteria (immunosuppressive conditions), clinical criteria (clinical and radiological signs of IPA) and mycological criteria (results of direct or indirect microbiological testing for Aspergillus species) (figure 1) [9].
FIGURE 1.
Schematic representation of the diagnostic classification of invasive pulmonary aspergillosis (IPA) according to the European Organization for Research and Treatment of Cancer and Mycoses Study Group Education and Research Consortium. Possible IPA must include at least one host criterion and one clinical criterion. Probable IPA must include at least one host criterion, one clinical criterion and one mycological criterion. Proven IPA is defined independently from the presence or absence of host/clinical/mycological criteria. For details, see reference [9]. BAL: bronchoalveolar lavage; CT: computed tomography; PCR: specific polymerase chain reaction for Aspergillus species.
Because initial clinical symptoms of IPA are often absent or not specific (e.g. fever), chest computed tomography (CT) scan represents a cornerstone of the diagnostic approach and should be performed whenever IPA is suspected in an immunocompromised patient [10]. On the contrary, standard chest radiography has poor sensitivity and is not considered appropriate for screening [10].
The available mycological tests for IPA diagnosis include histological examination of biopsy or surgical specimens, culture and nonculture methods, such as fungal biomarkers (galactomannan, 1,3-β-d-glucan (BDG)) and PCR [11, 12]. The different commercial tests and their characteristics are presented in table 1. Galactomannan (GM) testing can be performed in serum and bronchoalveolar lavage (BAL) fluid while the BDG test is only validated for use in serum. Whereas GM is a relatively specific marker of IPA, BDG can detect a broad range of pathogenic fungi including Aspergillus and Candida species with some exceptions (e.g. Mucorales) [11]. Multiple in-house PCRs have been developed for the detection of A. fumigatus or Aspergillus species. Recently, the European Aspergillus PCR Initiative has established laboratory procedures to improve the standardisation of these assays [13]. Moreover, some kits for the direct detection of Aspergillus species in clinical samples are now commercially available (table 1). Some of these assays also provide detection of the most important mutations associated with azole resistance.
TABLE 1.
Characteristics of nonculture commercialised diagnostic tests for invasive pulmonary aspergillosis
| Target | Type of test (manufacturer) | Technique | Spectrum of detection | Type of sample | Cut-off |
| Galactomannan | PlateliaTM Aspergillus EIA (Bio-Rad) | Immunoenzymatic sandwich assay | All Aspergillus species (specific)# | Serum, BAL | 0.5–1.0 ODI¶ |
| Soña Aspergillus galactomannan LFA (IMMY) | Immunochromatographic assay (LFA) | Visual reading or cube reader: 0.5–1.0¶ (index values) | |||
| Aspergillus galactomannan VirCliaTM (Vircell) | Chemoluminescent assay | 1.0 (index value) | |||
| (1→3)-β-d-Glucan | FungitellTM (Associates of Cape Cod) | Colorimetric assay (microplate) | All Aspergillus species (not specific)+ | Serum | 60–80 pg·mL−1§ |
| Fungitell STATTM (Associates of Cape Cod) | Colorimetric assay (single tube) | 0.75–1.2 (index values)§ | |||
| Wako β-glucan test (Fujifilm Wako Chemicals) | Turbidimetric assay (single tube) | 7.0 pg·mL−1 | |||
| Dynamiker Fungus (1–3)- β-d-glucan (Dynamiker Biotechnology) | Colorimetric assay (microplate) | 70–95 pg·mL−1§ | |||
| Aspergillus DNA | MycAssay AspergillusTM (Myconostica Ltd., now Microgen Bioproducts Ltd.) | Real-time PCR (18S rDNA) | Most relevant Aspergillus species | BAL, other respiratory samples, serum | NA |
| AsperGeniusTM (PathoNostics) | Multiplex real-time PCR (28S rDNA and Cyp51A) | Most relevant Aspergillus species, Cyp51A mutations (L98H, TR34, T289A, Y121F) | NA | ||
| MycoGenieTM (AdemTech) | Real-time PCR (28S rDNA and Cyp51A) | Aspergillus fumigatus, Cyp51A mutations (L98H, TR34) | NA | ||
| Fungiplex Aspergillus azole-RTM (Bruker Daltonics GmbH) | Multiplex real-time PCR | Aspergillus species, Cyp51A (TR34, TR46) | NA |
Note: the table is limited to the most relevant currently available test methods. BAL: bronchoalveolar lavage; EIA: enzyme immunoassay; LFA: lateral flow assay; NA: not applicable; ODI: optical density index. #Cross-reaction with some other fungal pathogens, e.g. Fusarium, Histoplasma. ¶ODI 0.5 is recommended by the manufacturer. Higher cut-offs (e.g. 1.0) are recommended for better specificity, notably in non-serum samples (BAL, cerebrospinal fluid). +Detection of most other fungal pathogens with some exception (e.g. Mucorales). §Values below, within and above this range are considered as negative, indeterminate and positive, respectively.
As the clinical presentation, diagnostic work-up and performance of diagnostic tests of IPA can vary considerably according to the type of disease and patient population, we will review the characteristics of diagnostic approaches in different settings.
IPA in haematologic cancer patients
Allogeneic haematopoietic stem cell transplant (HSCT) recipients with graft-versus-host disease (GVHD) and patients with acute leukaemia and prolonged chemotherapy-induced neutropenia (i.e. >10 days) represent the groups of patients at highest risk of IPA with an incidence of 2–8% [14–18]. However, IPA is now diagnosed with increasing frequency among other onco-haematologic populations formerly considered at “low risk”, such as patients with lymphoma, multiple myeloma or chronic leukaemia [8, 19–21]. Moreover, novel anti-cancer therapies, such as the Bruton tyrosine kinase inhibitors (e.g. ibrutinib) have been associated with an increased risk of IPA [22].
Neutropenic haematologic cancer patients usually have pathognomonic radiological findings on chest CT, such as well-circumscribed dense lesions (nodules or masses) with or without a surrounding area of ground-glass opacity due to haemorrhage known as the halo sign [10]. The halo sign usually represents an early stage of the disease, while the air crescent sign (partial cavitation) and the presence of a cavity are later-stage radiological manifestations with poorer prognosis [10, 23].
In haematologic cancer patients, the yield of direct exam and cultures for Aspergillus detection is notoriously low (around 20% and 50%, respectively) [24–26]. Nonculture methods, in particular GM or PCR in serum or BAL, are the cornerstone of IPA diagnosis and are in more than 50% of cases the only mycological markers of IPA [8, 12, 25, 27]. Their sensitivity and specificity are presented in table 2. Overall, GM and PCR exhibit comparable diagnostic performances and their combined use in serum or BAL samples results in the highest sensitivity and specificity [28–30]. BDG testing in serum is not specific for Aspergillus species and is associated with some false-positive results in this population, notably among patients who have received intravenous immunoglobulins [11, 31, 32].
TABLE 2.
Performance of galactomannan (GM) and Aspergillus PCR in serum and bronchoalveolar lavage fluid (BAL) for the diagnosis of invasive pulmonary aspergillosis (IPA) in haematologic cancer patients: results of the most relevant meta-analyses
| Fungal biomarker | Study | Sensitivity (%) (95% CI) | Specificity (%) (95% CI) |
| Serum | |||
| GM | Pfeiffer et al. [38] | 58 (52–64) | 95 (94–96) |
| Leeflang et al. [98]¶ | 78 (70–85) | 85 (78–91) | |
| Arvanitis et al. [28] | 92 (83–96) | 90 (81–95) | |
| PCR | Mengoli et al. [99] | 88 (75–94) | 75 (63–84) |
| Arvanitis et al. [28] | 84 (71–92) | 76 (64–85) | |
| GM and PCR# | Arvanitis et al. [28] | 99 (96–100) | 98 (94–100) |
| BAL | |||
| GM | Guo et al. [100]¶ | 85 (72–93) | 94 (89–97) |
| Avni et al. [29]¶ | 85 (62–95) | 100 (97–100) | |
| Zou et al. [101]¶ | 86 (76–92) | 95 (91–97) | |
| Heng et al. [30] | 75 (55–88) | 95 (87–98) | |
| De Heer et al. [102]¶ | 78 (61–95) | 93 (87–98) | |
| PCR | Sun et al. [103]¶ | 91 (79–96) | 92 (87–96) |
| Avni et al. [29]¶ | 93 (70–98) | 98 (93–99) | |
| Zou et al. [101]¶ | 82 (61–93) | 98 (85–100) | |
| Heng et al. [30] | 57 (31–80) | 99 (60–100) | |
| GM and PCR# | Avni et al. [29]¶ | 97 (83–99) | 97 (93–99) |
| Heng et al. [30] | 84 (79–88) | 94 (91–97) |
Results are displayed for the diagnosis of proven and probable IPA. For GM, results are displayed for the cut-off of optical density index 0.5 for serum and 1.0 for BAL. #Where a positive result is considered as either GM or PCR positive and a negative result as both GM and PCR negative. ¶Mixed populations, but with a predominance of haematologic cancer patients.
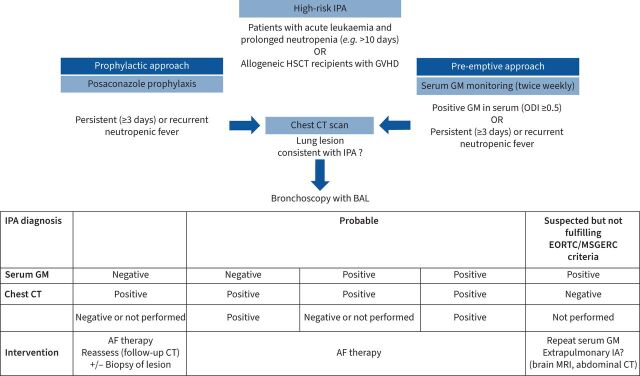
The epidemiology and diagnostic approach of IPA has changed with the increasing use of posaconazole prophylaxis in high-risk patients [33, 34]. Therefore, serial screening of GM in serum is not recommended in patients under posaconazole prophylaxis because of the low incidence of IPA, which results in low positive predictive value of the test [34, 35]. However, a pre-emptive approach with serial serum GM screening (e.g. twice per week) represents an alternative to systemic antifungal (AF) prophylaxis in these high-risk patients [34]. Chest CT scan should be performed in case of persistent or recurrent febrile neutropenia despite broad-spectrum antibiotics or in case of a positive serum GM. Bronchoscopy with BAL should be considered in the presence of a lung lesion consistent with IPA at CT scan. Indeed, BAL samplings are associated with the highest sensitivity and specificity to detect IPA (table 2) [12]. An algorithm for the diagnostic work-up of IPA in high-risk haematologic cancer patients is presented in figure 2. Patients with a positive serum GM have a worse prognosis, because of more advanced disease, which suggests that clinicians should have low threshold to perform chest CT for early detection of IPA [24].
FIGURE 2.
Diagnostic approach of invasive pulmonary aspergillosis (IPA) in high-risk haematologic cancer patients. AF: antifungal; BAL: bronchoalveolar lavage; CT: computed tomography; EORTC/MSGERC: European Organization for Research and Treatment of Cancer and Mycoses Study Group Education and Research Consortium; GM: galactomannan; GVHD: graft versus host disease; HSCT: haematopoietic stem cell transplantation; IA: invasive aspergillosis; MRI: magnetic resonance imaging; ODI: optical density index; PCR: specific polymerase chain reaction for Aspergillus species.
For other haematologic cancer patients at lower risk of IPA (e.g. chronic leukaemia, lymphoma, autologous HSCT recipients), anti-mould prophylaxis or serial GM screening are not recommended, but the threshold of clinical suspicion should be low to trigger chest CT and further investigations as IPA diagnosis is often missed in this population [19].
IPA in solid organ transplant recipients
The incidence of IPA among solid organ transplant (SOT) recipients is estimated to be 1–3% [36, 37]. It is higher among heart and lung than in other organ transplant recipients. The diagnosis of IPA in this population is difficult because of the lower specificity of radiological findings and lower sensitivity of mycological tests compared to those observed in haematologic cancer patients. Chest CT findings of IPA in SOT are not limited to well-circumscribed lung lesions (e.g. nodules or masses), but include a wide range of nonspecific abnormalities that cannot be distinguished from bacterial or viral pneumonias, such as tree-in-bud patterns, lobar infiltrates or ground-glass opacities [10].
The sensitivity of GM in serum is lower (around 40%) in SOT than in haematologic cancer patients [38]. BDG has poor sensitivity and specificity in this population [31, 39]. However, overall performance of GM and PCR in BAL is comparable to that reported in haematologic cancer patients with notably a similar high performance for their combined use [40, 41].
There is no recommendation for serial monitoring of serum fungal biomarkers in SOT patients because of their limited sensitivity and specificity [34]. In case of clinical suspicion (e.g. suggestive chest CT lesion), bronchoscopy should be performed and combined use of mycological tests (culture, GM, PCR) in BAL is the cornerstone for IPA diagnosis.
IPA in other immunocompromised hosts
Data about the performance of culture and nonculture diagnostic tests of IPA among patients with other immunosuppressive conditions (e.g. auto-immune diseases, corticosteroid therapy, treatment with Bruton tyrosine kinase inhibitors) are lacking. However, it is expected to be comparable to that observed in other nonneutropenic populations, such as SOT recipients.
IPA in ICU patients
The incidence of IPA in ICU is highly variable. Patients with severe influenza or COVID-19 are at the highest risk with reported incidences ranging from 5 to 30% [42]. There is more evidence supporting the association of IPA and influenza with one control study demonstrating a significantly higher incidence of IPA among ICU patients with severe influenza compared to those with other community-acquired pneumonia [6]. Moreover, evidence of angio-invasion, based on a positive GM in serum or histopathology, is more frequent in influenza than in COVID-19 [42–44]. In the latter, the distinction between Aspergillus colonisation and true IPA is difficult [45, 46]. However, recovery of Aspergillus in a respiratory sample by direct or indirect diagnostic tests seems to be a marker of poor prognosis in both influenza and COVID-19 patients [4, 6]. Other conditions that may predispose to IPA among ICU patients include liver cirrhosis, extracorporeal membrane oxygenation and short courses of corticosteroids [5, 47, 48].
IPA should be suspected in intubated patients with deteriorating respiratory conditions despite broad-spectrum antibiotic therapy. Chest CT findings are usually not distinguishable from viral or bacterial pneumonias [5, 42, 49, 50].
The EORTC-MSGERC criteria for IPA do not apply in ICU patients who do not have host criteria of immunosuppression in most cases. Customised definitions have been proposed for IPA in ICU, and specifically for IPA in patients with influenza or COVID-19 [49–51]. While the distinction between Aspergillus colonisation of the airways and true IPA is difficult to assess in this setting, the diagnostic criteria usually rely on a positive test for Aspergillus (direct exam, culture, GM or PCR) in a BAL sample. The significance of positive results in nonbronchoscopic respiratory samples (e.g. bronchial aspirates) is more difficult to interpret. GM in serum has a sensitivity around 50–60% for IPA detection in influenza [6, 44], but of less than 15% in COVID-19 [42].
CPA
CPA mainly affects patients with underlying lung diseases (sequelae of tuberculosis, nontuberculous mycobacterial infections, lung cancer, bronchiectasis) and no or mild immunosuppression [2]. A suggestive chest CT imaging is the key element for diagnosis [2]. Presence of a fungus ball (aspergilloma) in a pre-existing lung cavity is the most typical hallmark of CPA. Other radiological patterns include expansion or wall thickening of a pre-existing cavity, parenchymal destruction or fibrosis developing around a pre-existing cavity, pleural thickening or effusion, enlargement or pseudo-aneurysm of a bronchial artery [2]. Aspergillus nodules are a distinct feature, which is often misdiagnosed for a lung cancer because of its irregular or spiculated borders [2].
Microbiological documentation can be obtained by cultures on respiratory samples obtained by noninvasive (sputum) or invasive procedures (bronchoscopy with BAL) [2]. Aspergillus PCR is a very sensitive tool, but could be less specific than culture for the distinction between colonisation and infection [2, 52]. Among patients under AF therapy for CPA, PCR can be useful for the detection of azole resistance as a positive result was shown to be a good predictor [53].
GM testing can be performed in BAL with acceptable sensitivity (75–85%) and specificity (75–80%) [2, 54, 55]. GM testing in serum has poor sensitivity and is not recommended [2, 56]. Detection of anti-Aspergillus immunoglobulin G or precipitins has good positive predictive value for the diagnosis CPA and acceptable sensitivity (75–80%) for aspergilloma but not for chronic cavitary pulmonary aspergillosis [2, 57]. It is recommended for diagnosis and is also useful for the monitoring of response to therapy [2].
Treatment
AF drugs
Three AF drug classes are currently licensed for the treatment of aspergillosis (table 3): the polyenes (amphotericin B formulations), the triazoles (voriconazole, posaconazole, isavuconazole, itraconazole) and the echinocandins (anidulafungin, caspofungin, micafungin) [33, 34]. Some novel AF drugs with potent anti-Aspergillus activity (e.g. olorofim, fosmanogepix) are currently under clinical investigation and are available for compassionate use [58]. These drugs are expected to become key players for the treatment of azole-resistant IPA.
TABLE 3.
Antifungal agents for the treatment of pulmonary aspergillosis
| Antifungal class | Drugs | Dosage | Therapeutic use | Comments |
| Polyenes | Deoxycholate amphotericin B | 1–1.5 mg·kg−1 once daily (intravenous only) | Should be avoided (privilege lipid formulations of amphotericin B if available) | Monitor kidney function and electrolytes (K+) Consider co-administration of paracetamol if fever and/or rigors Consider alternative therapy for Aspergillus terreus |
| Liposomal amphotericin B | 3–5 mg·kg−1 once daily (intravenous only) | Treatment of IPA (second choice after triazoles; first choice in areas with high prevalence of azole-resistant Aspergillus fumigatus isolates if no culture/fungigram available) | ||
| Amphotericin B lipid complex | 5 mg·kg−1 once daily (intravenous only) | Treatment of IPA (privilege liposomal amphotericin B if available) | ||
| Amphotericin B colloidal dispersion | 6 mg·kg−1 once daily (intravenous only) | Treatment of IPA (privilege liposomal amphotericin B if available) | ||
| Triazoles | Itraconazole | 200 mg once daily or twice daily (intravenous or oral) TDM recommended (target: Ctrough: 1–4 mg·L−1) |
Treatment of CPA | Monitor hepatic tests (ALT, AST, ALP, GGT, bilirubin) Monitor ECG (QT interval, in particular voriconazole) DDIs (in particular voriconazole) Consider alternative therapy for Aspergillus calidoustus or cryptic species of section Fumigati (e.g. Aspergillus lentulus) |
| Voriconazole | Intravenous: 6 mg·kg−1 twice daily (D1), then 4 mg·kg−1 twice daily Oral: 400 mg twice daily (D1), then 200–300 mg twice daily TDM recommended (target: Ctrough: 1–5 mg·L−1) |
Treatment of IPA (first choice) Treatment of CPA |
||
| Posaconazole | Intravenous or oral tablets: 300 mg twice daily (D1), then 300 mg once daily Oral suspension: 200 mg three times daily TDM recommended (target: Ctrough: >1 mg·L−1 for therapy and >0.7 mg·L−1 for prophylaxis) |
Prophylaxis or treatment of IPA Treatment of CPA (privilege itraconazole or voriconazole) Oral suspension should be avoided or limited to prophylaxis (privilege intravenous formulation or oral tablets) |
||
| Isavuconazole | 200 mg three times daily (D1–2), then 200 mg once daily TDM not routinely recommended (may be considered) |
Treatment of IPA Treatment of CPA (privilege itraconazole or voriconazole) |
||
| Echinocandins | Caspofungin | 70 mg (D1), then 50 mg once daily (intravenous only) | Treatment of IPA as monotherapy (third choice after triazoles and lipid formulations of amphotericin B) Treatment of IPA in combination with triazoles (severe cases and/or positive GM; azole-resistant Aspergillus fumigatus isolates) |
|
| Anidulafungin | 200 mg (D1), then 100 mg once daily (intravenous only) | |||
| Micafungin | 100 mg once daily (intravenous only) |
ALP: alkaline phosphatase; ALT: alanine aminotransferase; AST: aspartate aminotransferase; CPA: chronic pulmonary aspergillosis; D1: day 1; DDI: drug–drug interaction; GGT: gamma glutamyltranspeptidase; GM: galactomannan; IPA: invasive pulmonary aspergillosis; TDM: therapeutic drug monitoring, W1: week 1.
Triazoles
Mould-active triazoles include itraconazole, voriconazole, posaconazole and isavuconazole. These AF agents inhibit the biosynthesis of ergosterol and are fungicidal against most Aspergillus species with some rare exceptions such as cryptic species of section Fumigati (e.g. A. lentulus, A. udagawae) and all species of section Usti (e.g. A. calidoustus), which account for a very low proportion of IPA (<3%) [59, 60]. Triazoles have the advantage to be available as intravenous and oral formulations. Their main side-effect is hepatotoxicity, which is more frequent in patients treated with voriconazole and posaconazole (10–15%) than in those treated with isavuconazole (<10%) [25, 61]. Hepatotoxicity may require treatment interruption but is usually reversible. Triazoles are substrates and inhibitors of cytochrome P450 isoenzymes, which results in multiple drug–drug interactions [62]. These interactions are a particular concern for voriconazole and may require dosage adaptations of other drugs, but they rarely prevent the use of triazoles. With the exception of isavuconazole, triazoles may prolong the QT interval and require electrocardiographic monitoring. Significant QT prolongation has been observed in about 15% of onco–haematological patients and is associated with other medications affecting the QT interval and/or electrolytic disorders in most cases [63]. Life-threatening complications (torsades de pointes) are very rare events. Therapeutic drug monitoring (TDM) is recommended for itraconazole, voriconazole and posaconazole because of inter- and intra-individual variability of serum concentrations [34]. For voriconazole, trough concentrations of 1 to 5.5 mg·L−1 have been proposed based on pharmacodynamic studies correlating low and high concentrations with failure of therapy and toxicity (visual or neurological disturbances), respectively [34, 64, 65]. Genetic polymorphisms in the CYP2C19, the cytochrome P450 isoenzyme involved in the primary metabolism of voriconazole, can explain inter-individual variations between rapid and poor metabolisers [66]. For posaconazole, important variations of serum concentrations have been observed with the oral suspension formulation and have been related to high gastric pH (e.g. co-administration of proton pump inhibitors, type of food) [67]. More stable pharmacokinetic profiles are observed with the new oral formulation (tablets) and the intravenous formulation [68]. However, TDM is still recommended with targeted trough concentrations of 0.7 mg·L−1 and 1.0 mg·L−1 for prophylaxis and treatment, respectively [34]. For isavuconazole, TDM is not routinely recommended because of more stable pharmacokinetic profiles and lack of correlation between trough concentrations and outcomes [34, 69].
Triazoles represents the mainstay for the treatment of aspergillosis [2, 33, 34]. While voriconazole is recommended as the first-line therapy of IPA [33, 34], new azoles (posaconazole, isavuconazole) have demonstrated similar efficacy in randomised clinical trials [25, 61]. Isavuconazole is of particular interest as it is associated with less hepatotoxicity, fewer drug interactions and more stable pharmacokinetic profiles (i.e. no need for TDM) than voriconazole [25, 70]. The global emergence of azole resistance in A. fumigatus, thought to be associated with the widespread use of fungicides in the environment, is of particular concern [71]. Various mutations have been described in the azole target gene (cyp51A), the most frequent ones being the TR34/L98H and the TR46/Y121F/T289A mutations, which are associated with pan-azole resistance [72]. Patients receiving first-line voriconazole therapy for IPA due to an azole-resistant A. fumigatus have significantly higher mortality rates compared to those infected with an azole-susceptible isolate [73].
Amphotericin B
This AF agent binds to ergosterol, which results in altered integrity of the cell membrane with loss of protons and monovalent cations [74]. The AF activity of amphotericin B may also result from production of reactive oxygen species and oxidative damage [75]. It has a broad spectrum of AF activity and is fungicidal against most Aspergillus species with the exception of A. terreus [74, 76]. Acquired resistance among other Aspergillus species, such as A. fumigatus, is rare and mechanisms are poorly elucidated [77].
Over the last two decades, conventional amphotericin B deoxycholate has been substituted by safer lipid formulations of amphotericin B, such as liposomal amphotericin B, amphotericin B lipid complex or amphotericin B colloidal dispersion.
The use of amphotericin B is limited by its adverse events and its availability as an intravenous formulation only. Nephrotoxicity is the main adverse effect, which was observed in one third of patients treated with amphotericin B deoxycholate [78]. However, novel amphotericin B lipid formulations are associated with reduced nephrotoxicity (10–15%) [78]. Other side effects, such as infusion-related reactions (fever, rigors) and hypokalaemia are also significantly less frequent with the lipid formulations, notably liposomal amphotericin B [78, 79].
One randomised study showed that amphotericin B deoxycholate was associated with lower rate of therapeutic success and more drug-related adverse events compared to voriconazole [80]. Although data from randomised controlled trials are lacking for liposomal amphotericin B, this drug has been associated with success rates similar to those observed with voriconazole for IPA treatment [81].
Liposomal amphotericin B is a second-line therapy of IPA and the first-line therapy for azole-resistant IPA [34]. It is also recommended as initial empirical therapy for suspected or possible invasive mould infection because of its broader spectrum of activity against pathogenic moulds including the Mucorales and azole-resistant Aspergillus species [34]. The local epidemiology regarding the prevalence of these more resistant pathogens should be taken into consideration in the choice of initial empirical AF therapy.
Echinocandins
Echinocandins inhibit the beta-glucan synthase, which results in loss of the fungal cell wall integrity [82]. Currently licensed echinocandins are caspofungin, anidulafungin and micafungin, which are available only as intravenous formulations. Rezafungin is a novel molecule of this class with prolonged half-life that can be administered once weekly [83]. Echinocandins have limited in vitro activity against Aspergillus species with a fungistatic effect resulting in blunted hyphae and growth inhibition [82]. In vitro and in animal models, caspofungin displays a paradoxical effect (i.e. decreased efficacy at increased concentrations), of uncertain clinical relevance [82]. Acquired echinocandin resistance may occur in A. fumigatus via mutations in the beta-glucan synthase gene but this has been very rarely observed in clinical isolates [82, 84].
In clinical practice, variable success rates have been reported with echinocandin monotherapy and there is no randomised trials comparing the efficacy and safety of echinocandins versus amphotericin B or triazoles [82, 85]. Currently, echinocandins are not routinely recommended for IPA treatment, except in particular situations when underlying conditions or toxicity prevents the use of triazoles or amphotericin B formulations [33, 34]. Echinocandins may be used in combination therapy with voriconazole in severe IPA [34]. While this combination demonstrated some synergism in vitro and in animal models [82, 86, 87], its superiority over voriconazole monotherapy could not be clearly demonstrated in a randomised trial showing only a trend towards better survival with the combination and a significant effect limited to the subgroup of patients with a positive GM [26]. This combination also represents a therapeutic option for the treatment of azole-resistant IPA (as an alternative to liposomal amphotericin B), but clinical efficacy in this setting is not demonstrated [88]. Some pre-clinical (in vitro and murine model) and clinical data (single pilot study) also suggest a synergistic interaction between echinocandins and amphotericin B [82, 89].
Novel AF agents
Because of the limited therapeutic options against azole-resistant IPA, novel AF drugs with potent and broad anti-Aspergillus activity are warranted. Olorofim is an inhibitor of the fungal dihydroorotate dehydrogenase, an enzyme involved in pyrimidine biosynthesis, which has a potent activity with a time-dependent fungicidal effect against all Aspergillus species including those with intrinsic or acquired azole resistance [58]. The prodrug fosmanogepix, which is converted to its active moiety manogepix by systemic phosphatases, is an inhibitor of an enzyme in the glycosylphosphatidylinositol anchor biosynthetic pathway (Gwt1) [58]. It has potent fungistatic activity against all Aspergillus species including those with intrinsic or acquired azole resistance. Both compounds have the advantage to be available as intravenous and oral formulations. They are currently in phase II clinical trials for the treatment of IPA [58]. Ibrexafungerp is a beta-glucan synthase inhibitor with a structure distinct from echinocandins that can be administered by oral route [58]. Its spectrum of activity against Aspergillus species is comparable to that of echinocandins [58]. A phase II trial comparing ibrexafungerp given in combination with voriconazole versus voriconazole monotherapy for the treatment of IPA is ongoing [58].
Within existing drug classes, other drugs with improved pharmacologic properties (e.g. tetrazoles, encochleated amphotericin B) are in clinical phases of investigation [58].
Therapeutic approaches
IPA
AF therapy should be initiated promptly when IPA is suspected. When a bronchoscopy is planned, AF therapy should be started after the procedure whenever possible, but should not be delayed by more than 24 h. The therapeutic approach of IPA in the different subsets of immunocompromised patients (e.g. haematologic cancer patients, SOT, ICU patients) does not substantially differ. Triazoles (voriconazole, isavuconazole or posaconazole) should be privileged for proven or probable IPA and liposomal amphotericin B for possible IPA to ensure broad coverage including the Mucorales and azole-resistant Aspergillus species. Other parameters, such as the baseline liver and kidney functions and the co-medications with potential drug–drug interactions may also influence the choice of initial AF therapy as described above. Combination therapies of triazoles and echinocandins should be limited to patients with severe or refractory IPA. Surgical interventions are rarely necessary for IPA unless there is a need for source control because of involvement of adjacent structures (e.g. pleura, mediastinum), extrapulmonary foci (e.g. cerebral aspergillosis), life-threatening haemoptysis or nonresponsive disease. Bone-marrow recovery or reduction of immunosuppression are important outcome determinants. Tapering of immunosuppressive therapies should be considered very carefully in a multidisciplinary approach to avoid graft rejection, GVHD or worsening of underlying immune diseases.
The duration of therapy is not well defined, but it should be at least 6–12 weeks depending on the recovery of immunosuppression and the evolution of CT lesions that should be carefully monitored [33, 34]. Some case series have addressed the role of positron emission tomography/CT in monitoring response to therapy of invasive fungal infections with interesting results, which should be confirmed in larger datasets [10, 90]. Secondary prophylaxis should be considered in patients with prolonged immunosuppression [34]. Shorter treatment duration (e.g. 4–6 weeks) may be considered in immunocompetent ICU patients (e.g. influenza and COVID-19) once they are discharged from ICU [46].
Chronic pulmonary aspergillosis (CPA)
The management of CPA is complex and requires a multidisciplinary approach involving pulmonologists, thoracic surgeons, radiologists and infectious diseases specialists. As CPA may present with very heterogeneous radiological patterns and degree of extension, indications for surgery should be carefully assessed on an individual basis considering the number and size of the lesions and the patient's underlying structural lung disease and/or degree of lung function impairment [2]. In case of surgery, pre-operative AF therapy may be warranted for complex surgical procedures to prevent spillage of the fungus (e.g. within pleural cavity) [2]. Post-operative AF therapy should be considered in case of partial resection of the lesion(s), complex procedures with risk of spillage or when histopathology or cultures show presence of fungal elements invading the adjacent lung parenchyma [2].
In the absence of surgery, AF therapy may prevent progression of the lesions (e.g. fibrosis) and life-threatening complications, such as haemoptysis, and improve respiratory conditions, quality of life and outcomes [2, 91]. Long-term suppressive AF therapy is usually required as therapeutic response is very slow and only partial in most cases. Regular chest CT (every 3 or 6 months) is indicated to assess therapeutic response [2]. Oral triazoles are the cornerstone of CPA treatment. Itraconazole may be used as first-line therapy because of its low cost and good safety profile [2, 91]. Voriconazole (or posaconazole) can be administered for more severe disease [2, 92, 93]. Isavuconazole can be used in case of toxicity or drug–drug interactions. Patients with long-term triazole therapy should have regular dermatologic control (every 6 months) for the early detection of skin cancer [94]. Echinocandin therapy may be considered in case of intolerance or resistance to triazoles [2, 95]. Rezafungin (administered only once a week) or the novel oral beta-glucan synthase inhibitor ibrexafungerp may represent interesting alternative treatments although data supporting their efficacy in CPA are currently lacking.
For patients who are not eligible for surgery and experience failure of AF therapy with recurrent haemoptysis, direct instillation of amphotericin B or a triazole (itraconazole, miconazole) in the aspergilloma cavity has shown some efficacy [2, 96].
Haemoptysis is the most feared complication and may require administration of tranexamic acid or arterial embolisation in the most severe cases [2]. Surgery should be considered in case of severe or recurrent haemoptysis [2].
Because of the paucity of clinical trials, management of CPA mainly relies on experts’ opinions [2]. A multicentre collaboration has been recently initiated to establish an international registry (CPAnet), which is expected to improve our understanding of the disease and to standardise therapeutic approaches [97].
Conclusions
With the advent of novel anti-cancer and immune modulation therapies and the recent H1N1 influenza and COVID-19 pandemics, the incidence and clinical spectrum of pulmonary aspergillosis has increased significantly. The heterogeneity of clinical and radiological patterns and limited sensitivity and specificity of microbiological tests poses a diagnostic challenge. Clinicians should be educated to suspect and recognise pulmonary aspergillosis among these new or atypical categories of patients where it is often missed. Emergence of azole resistance among A. fumigatus is a major concern as current alternative therapeutic options are limited. However, the development of novel AF drug classes are opening up promising perspectives for the management of such cases.
Points for clinical practice
The incidence and clinical spectrum of pulmonary aspergillosis are increasing because of the expanding population at risk of developing the disease.
Notably, pulmonary aspergillosis is increasingly recognised among patients with mild immunosuppressive conditions or in apparently immunocompetent patients, such as those with severe influenza or COVID-19.
The diagnosis of pulmonary aspergillosis is challenging because of the limited sensitivity and specificity of diagnostic tests and the need to combine these tests for improved diagnostic accuracy.
The treatment of pulmonary aspergillosis is challenging because of the limited number of available AF drug classes and the emergence of resistance.
Footnotes
Number 7 in the Series “Respiratory infections” Edited by Antoni Torres and Michael S. Niederman
Provenance: Commissioned article, peer reviewed.
Previous articles in this series: No. 1: Kumar K, Daley CL, Griffith DE, et al. Management of Mycobacterium avium complex and Mycobacterium abscessus pulmonary disease: therapeutic advances and emerging treatments. Eur Respir Rev 2022; 31: 210212. No. 2: Cilloniz C, Luna CM, Hurtado JC, et al. Respiratory viruses: their importance and lessons learned from COVID-19. Eur Respir Rev 2022; 31: 220051. No. 3: Cavallazzi R, Ramirez JA. How and when to manage respiratory infections out of hospital. Eur Respir Rev 2022; 31: 220092. No. 4: Reynolds D, Burnham JP, Vazquez Guillamet C, et al. The threat of multidrug-resistant/extensively drug-resistant Gram-negative respiratory infections: another pandemic. Eur Respir Rev 2022; 31: 220068. No. 5: Puerta-Alcalde P, Garcia-Vidal C. Non-Aspergillus mould lung infections. Eur Respir Rev 2022; 31: 220104. No. 6: Al-Tawfiq JA, Kim H, Memish ZA. Parasitic lung diseases. Eur Respir Rev 2022; 31: 220093.
Conflict of interest: F. Lamoth has research funding from Gilead, MSD, Pfizer and Novartis, and has participated in Advisory boards for Gilead, MSD and Pfizer. All contracts were made with and fees paid to his institution (CHUV).
Conflict of interest: T. Calandra has participated in advisory boards or consulted for Menarini, Shinogi, Cytosorbent, ThermoFisher and GE Healthcare for projects unrelated to the submitted work and on data safety monitoring boards for Cidara and Novartis. All contracts were made with and fees paid to his institution (CHUV).
This article has an editorial commentary: https://doi.org/10.1183/16000617.0150-2022
References
- 1.Tracy MC, Okorie CUA, Foley EA, et al. Allergic bronchopulmonary aspergillosis. J Fungi 2016; 2: 17. doi: 10.3390/jof2020017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Denning DW, Cadranel J, Beigelman-Aubry C, et al. Chronic pulmonary aspergillosis: rationale and clinical guidelines for diagnosis and management. Eur Respir J 2016; 47: 45–68. doi: 10.1183/13993003.00583-2015 [DOI] [PubMed] [Google Scholar]
- 3.Cadena J, Thompson GR III, Patterson TF. Aspergillosis: epidemiology, diagnosis, and treatment. Infect Dis Clin North Am 2021; 35: 415–434. doi: 10.1016/j.idc.2021.03.008 [DOI] [PubMed] [Google Scholar]
- 4.Bartoletti M, Pascale R, Cricca M, et al. Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: a prospective study. Clin Infect Dis 2020; 73: e3606–e3614. doi: 10.1093/cid/ciaa1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meersseman W, Vandecasteele SJ, Wilmer A, et al. Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med 2004; 170: 621–625. doi: 10.1164/rccm.200401-093OC [DOI] [PubMed] [Google Scholar]
- 6.Schauwvlieghe A, Rijnders BJA, Philips N, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med 2018; 6: 782–792. doi: 10.1016/S2213-2600(18)30274-1 [DOI] [PubMed] [Google Scholar]
- 7.Pagano L, Caira M, Candoni A, et al. Invasive aspergillosis in patients with acute myeloid leukemia: a SEIFEM-2008 registry study. Haematologica 2010; 95: 644–650. doi: 10.3324/haematol.2009.012054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steinbach WJ, Marr KA, Anaissie EJ, et al. Clinical epidemiology of 960 patients with invasive aspergillosis from the PATH Alliance registry. J Infect 2012; 65: 453–464. doi: 10.1016/j.jinf.2012.08.003 [DOI] [PubMed] [Google Scholar]
- 9.Donnelly JP, Chen SC, Kauffman CA, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis 2020; 71: 1367–1376. doi: 10.1093/cid/ciz1008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexander BD, Lamoth F, Heussel CP, et al. Guidance on imaging for invasive pulmonary aspergillosis and mucormycosis: from the imaging working group for the revision and update of the consensus definitions of fungal disease from the EORTC/MSGERC. Clin Infect Dis 2021; 72: S79–S88. doi: 10.1093/cid/ciaa1855 [DOI] [PubMed] [Google Scholar]
- 11.Lamoth F, Alexander BD. Nonmolecular methods for the diagnosis of respiratory fungal infections. Clin Lab Med 2014; 34: 315–336. doi: 10.1016/j.cll.2014.02.006 [DOI] [PubMed] [Google Scholar]
- 12.Lamoth F, Calandra T. Early diagnosis of invasive mould infections and disease. J Antimicrob Chemother 2017; 72: i19–i28. doi: 10.1093/jac/dkx030 [DOI] [PubMed] [Google Scholar]
- 13.White PL, Mengoli C, Bretagne S, et al. Evaluation of Aspergillus PCR protocols for testing serum specimens. J Clin Microbiol 2011; 49: 3842–3848. doi: 10.1128/JCM.05316-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kontoyiannis DP, Marr KA, Park BJ, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001–2006: overview of the Transplant-Associated Infection Surveillance Network (TRANSNET) Database. Clin Infect Dis 2010; 50: 1091–1100. doi: 10.1086/651263 [DOI] [PubMed] [Google Scholar]
- 15.Kuster S, Stampf S, Gerber B, et al. Incidence and outcome of invasive fungal diseases after allogeneic hematopoietic stem cell transplantation: a Swiss transplant cohort study. Transpl Infect Dis 2018; 20: e12981. doi: 10.1111/tid.12981 [DOI] [PubMed] [Google Scholar]
- 16.Mariette C, Tavernier E, Hocquet D, et al. Epidemiology of invasive fungal infections during induction therapy in adults with acute lymphoblastic leukemia: a GRAALL-2005 study. Leuk Lymphoma 2017; 58: 586–593. doi: 10.1080/10428194.2016.1204652 [DOI] [PubMed] [Google Scholar]
- 17.Pagano L, Caira M, Candoni A, et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica 2006; 91: 1068–1075. [PubMed] [Google Scholar]
- 18.Pagano L, Caira M, Nosari A, et al. Fungal infections in recipients of hematopoietic stem cell transplants: results of the SEIFEM B-2004 study–Sorveglianza Epidemiologica Infezioni Fungine Nelle Emopatie Maligne. Clin Infect Dis 2007; 45: 1161–1170. doi: 10.1086/522189 [DOI] [PubMed] [Google Scholar]
- 19.Caudron de Coquereaumont G, Couchepin J, Perentes JY, et al. Limited index of clinical suspicion and underdiagnosis of histopathologically documented invasive mold infections. Open Forum Infect Dis 2021; 8: ofab174. doi: 10.1093/ofid/ofab174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gil L, Kozlowska-Skrzypczak M, Mol A, et al. Increased risk for invasive aspergillosis in patients with lymphoproliferative diseases after autologous hematopoietic SCT. Bone Marrow Transplant 2009; 43: 121–126. doi: 10.1038/bmt.2008.303 [DOI] [PubMed] [Google Scholar]
- 21.Guery R, Suarez F, Lanternier F, et al. Poor outcome and high prevalence of invasive fungal infections in patients with adult T-cell leukemia/lymphoma exposed to zidovudine and interferon alfa. Ann Hematol 2021; 100: 2813–2824. doi: 10.1007/s00277-021-04622-9 [DOI] [PubMed] [Google Scholar]
- 22.Chamilos G, Lionakis MS, Kontoyiannis DP. Call for action: invasive fungal infections associated with ibrutinib and other small molecule kinase inhibitors targeting immune signaling pathways. Clin Infect Dis 2018; 66: 140–148. doi: 10.1093/cid/cix687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caillot D, Couaillier JF, Bernard A, et al. Increasing volume and changing characteristics of invasive pulmonary aspergillosis on sequential thoracic computed tomography scans in patients with neutropenia. J Clin Oncol 2001; 19: 253–259. doi: 10.1200/JCO.2001.19.1.253 [DOI] [PubMed] [Google Scholar]
- 24.Couchepin J, Brunel AS, Jaton K, et al. Role of bi-weekly serum galactomannan screening for the diagnosis of invasive aspergillosis in haematological cancer patients. Mycoses 2018; 61: 350–354. doi: 10.1111/myc.12755 [DOI] [PubMed] [Google Scholar]
- 25.Maertens JA, Raad II, Marr KA, et al. Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi (SECURE): a phase 3, randomised-controlled, non-inferiority trial. Lancet 2016; 387: 760–769. doi: 10.1016/S0140-6736(15)01159-9 [DOI] [PubMed] [Google Scholar]
- 26.Marr KA, Schlamm HT, Herbrecht R, et al. Combination antifungal therapy for invasive aspergillosis: a randomized trial. Ann Intern Med 2015; 162: 81–89. doi: 10.7326/M13-2508 [DOI] [PubMed] [Google Scholar]
- 27.Neofytos D, Horn D, Anaissie E, et al. Epidemiology and outcome of invasive fungal infection in adult hematopoietic stem cell transplant recipients: analysis of Multicenter Prospective Antifungal Therapy (PATH) Alliance registry. Clin Infect Dis 2009; 48: 265–273. doi: 10.1086/595846 [DOI] [PubMed] [Google Scholar]
- 28.Arvanitis M, Anagnostou T, Mylonakis E. Galactomannan and polymerase chain reaction-based screening for invasive aspergillosis among high-risk hematology patients: a diagnostic meta-analysis. Clin Infect Dis 2015; 61: 1263–1272. doi: 10.1093/cid/civ555 [DOI] [PubMed] [Google Scholar]
- 29.Avni T, Levy I, Sprecher H, et al. Diagnostic accuracy of PCR alone compared to galactomannan in bronchoalveolar lavage fluid for diagnosis of invasive pulmonary aspergillosis: a systematic review. J Clin Microbiol 2012; 50: 3652–3658. doi: 10.1128/JCM.00942-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heng SC, Morrissey O, Chen SC, et al. Utility of bronchoalveolar lavage fluid galactomannan alone or in combination with PCR for the diagnosis of invasive aspergillosis in adult hematology patients: a systematic review and meta-analysis. Crit Rev Microbiol 2015; 41: 124–134. doi: 10.3109/1040841X.2013.804033 [DOI] [PubMed] [Google Scholar]
- 31.Lamoth F, Akan H, Andes D, et al. Assessment of the role of 1,3-beta-d-glucan testing for the diagnosis of invasive fungal infections in adults. Clin Infect Dis 2021; 72: S102–S108. doi: 10.1093/cid/ciaa1943 [DOI] [PubMed] [Google Scholar]
- 32.Tschopp J, Brunel AS, Spertini O, et al. High false-positive rate of (1,3)-beta-d-glucan in onco-hematological patients receiving immunoglobulins and therapeutic antibodies. Clin Infect Dis 2022; 75: 330–333. doi: 10.1093/cid/ciab1028 [DOI] [PubMed] [Google Scholar]
- 33.Patterson TF, Thompson GR III, Denning DW, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the infectious diseases Society of America. Clin Infect Dis 2016; 63: e1–e60. doi: 10.1093/cid/ciw326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ullmann AJ, Aguado JM, Arikan-Akdagli S, et al. Diagnosis and management of Aspergillus diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect 2018; 24: Suppl 1, e1–e38. doi: 10.1016/j.cmi.2018.01.002 [DOI] [PubMed] [Google Scholar]
- 35.Duarte RF, Sanchez-Ortega I, Cuesta I, et al. Serum galactomannan-based early detection of invasive aspergillosis in hematology patients receiving effective antimold prophylaxis. Clin Infect Dis 2014; 59: 1696–1702. doi: 10.1093/cid/ciu673 [DOI] [PubMed] [Google Scholar]
- 36.Neofytos D, Chatzis O, Nasioudis D, et al. Epidemiology, risk factors and outcomes of invasive aspergillosis in solid organ transplant recipients in the Swiss Transplant Cohort Study. Transpl Infect Dis 2018; 20: e12898. doi: 10.1111/tid.12898 [DOI] [PubMed] [Google Scholar]
- 37.Pappas PG, Alexander BD, Andes DR, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin Infect Dis 2010; 50: 1101–1111. doi: 10.1086/651262 [DOI] [PubMed] [Google Scholar]
- 38.Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis 2006; 42: 1417–1427. doi: 10.1086/503427 [DOI] [PubMed] [Google Scholar]
- 39.Alexander BD, Smith PB, Davis RD, et al. The (1,3)β-d-glucan test as an aid to early diagnosis of invasive fungal infections following lung transplantation. J Clin Microbiol 2010; 48: 4083–4088. doi: 10.1128/JCM.01183-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Imbert S, Meyer I, Palous M, et al. Aspergillus PCR in bronchoalveolar lavage fluid for the diagnosis and prognosis of aspergillosis in patients with hematological and non-hematological conditions. Front Microbiol 2018; 9: 1877. doi: 10.3389/fmicb.2018.01877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Luong ML, Clancy CJ, Vadnerkar A, et al. Comparison of an Aspergillus real-time polymerase chain reaction assay with galactomannan testing of bronchoalvelolar lavage fluid for the diagnosis of invasive pulmonary aspergillosis in lung transplant recipients. Clin Infect Dis 2011; 52: 1218–1226. doi: 10.1093/cid/cir185 [DOI] [PubMed] [Google Scholar]
- 42.Lamoth F, Lewis RE, Walsh TJ, et al. Navigating the uncertainties of COVID-19 associated aspergillosis (CAPA): a comparison with influenza associated aspergillosis (IAPA). J Infect Dis 2021; 224: 1631–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kula BE, Clancy CJ, Hong Nguyen M, et al. Invasive mould disease in fatal COVID-19: a systematic review of autopsies. Lancet Microbe 2021; 2: e405–e414. doi: 10.1016/S2666-5247(21)00091-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vanderbeke L, Spriet I, Breynaert C, et al. Invasive pulmonary aspergillosis complicating severe influenza: epidemiology, diagnosis and treatment. Curr Opin Infect Dis 2018; 31: 471–480. doi: 10.1097/QCO.0000000000000504 [DOI] [PubMed] [Google Scholar]
- 45.Fekkar A, Neofytos D, Nguyen MH, et al. COVID-19-associated pulmonary aspergillosis (CAPA): how big a problem is it? Clin Microbiol Infect 2021; 27: 1376–1378. doi: 10.1016/j.cmi.2021.06.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lamoth F. Invasive aspergillosis in coronavirus disease 2019: a practical approach for clinicians. Curr Opin Infect Dis 2022; 35: 163–169. doi: 10.1097/QCO.0000000000000812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aubron C, Pilcher D, Leong T, et al. Aspergillus sp. isolated in critically ill patients with extracorporeal membrane oxygenation support. Scand J Infect Dis 2013; 45: 715–721. doi: 10.3109/00365548.2013.797598 [DOI] [PubMed] [Google Scholar]
- 48.Kluge S, Strauss R, Kochanek M, et al. Aspergillosis: emerging risk groups in critically ill patients. Med Mycol 2021; 60: myab064. doi: 10.1093/mmy/myab064 [DOI] [PubMed] [Google Scholar]
- 49.Koehler P, Bassetti M, Chakrabarti A, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis 2021; 21: e149–e162. doi: 10.1016/S1473-3099(20)30847-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Verweij PE, Rijnders BJA, Bruggemann RJM, et al. Review of influenza-associated pulmonary aspergillosis in ICU patients and proposal for a case definition: an expert opinion. Intensive Care Med 2020; 46: 1524–1535. doi: 10.1007/s00134-020-06091-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Blot SI, Taccone FS, Van den Abeele AM, et al. A clinical algorithm to diagnose invasive pulmonary aspergillosis in critically ill patients. Am J Respir Crit Care Med 2012; 186: 56–64. doi: 10.1164/rccm.201111-1978OC [DOI] [PubMed] [Google Scholar]
- 52.Vergidis P, Moore CB, Novak-Frazer L, et al. High-volume culture and quantitative real-time PCR for the detection of Aspergillus in sputum. Clin Microbiol Infect 2020; 26: 935–940. doi: 10.1016/j.cmi.2019.11.019 [DOI] [PubMed] [Google Scholar]
- 53.Moazam S, Eades CP, Muldoon EG, et al. Positive Aspergillus PCR as a marker of azole resistance or sub-therapeutic antifungal therapy in patients with chronic pulmonary aspergillosis. Mycoses 2020; 63: 376–381. doi: 10.1111/myc.13052 [DOI] [PubMed] [Google Scholar]
- 54.Izumikawa K, Yamamoto Y, Mihara T, et al. Bronchoalveolar lavage galactomannan for the diagnosis of chronic pulmonary aspergillosis. Med Mycol 2012; 50: 811–817. doi: 10.3109/13693786.2012.682228 [DOI] [PubMed] [Google Scholar]
- 55.Kono Y, Tsushima K, Yamaguchi K, et al. The utility of galactomannan antigen in the bronchial washing and serum for diagnosing pulmonary aspergillosis. Respir Med 2013; 107: 1094–1100. doi: 10.1016/j.rmed.2013.04.007 [DOI] [PubMed] [Google Scholar]
- 56.Shin B, Koh WJ, Jeong BH, et al. Serum galactomannan antigen test for the diagnosis of chronic pulmonary aspergillosis. J Infect 2014; 68: 494–499. doi: 10.1016/j.jinf.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 57.Uffredi ML, Mangiapan G, Cadranel J, et al. Significance of Aspergillus fumigatus isolation from respiratory specimens of nongranulocytopenic patients. Eur J Clin Microbiol Infect Dis 2003; 22: 457–462. doi: 10.1007/s10096-003-0970-y [DOI] [PubMed] [Google Scholar]
- 58.Lamoth F, Lewis RE, Kontoyiannis DP. Investigational antifungal agents for invasive mycoses: a clinical perspective. Clin Infect Dis 2022; 75: 534–544. doi: 10.1093/cid/ciab1070 [DOI] [PubMed] [Google Scholar]
- 59.Glampedakis E, Erard V, Lamoth F. Clinical relevance and characteristics of Aspergillus calidoustus and other Aspergillus species of section Usti. J Fungi 2020; 6: 84. doi: 10.3390/jof6020084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lamoth F. Aspergillus fumigatus-related species in clinical practice. Front Microbiol 2016; 7: 683. doi: 10.3389/fmicb.2016.00683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maertens JA, Rahav G, Lee DG, et al. Posaconazole versus voriconazole for primary treatment of invasive aspergillosis: a phase 3, randomised, controlled, non-inferiority trial. Lancet 2021; 397: 499–509. doi: 10.1016/S0140-6736(21)00219-1 [DOI] [PubMed] [Google Scholar]
- 62.Amsden JR, Gubbins PO. Pharmacogenomics of triazole antifungal agents: implications for safety, tolerability and efficacy. Expert Opin Drug Metab Toxicol 2017; 13: 1135–1146. doi: 10.1080/17425255.2017.1391213 [DOI] [PubMed] [Google Scholar]
- 63.Barreto JN, Cullen MW, Mara KC, et al. QT prolongation in patients with acute leukemia or high-risk myelodysplastic syndrome prescribed antifungal prophylaxis during chemotherapy-induced neutropenia. Leuk Lymphoma 2019; 60: 3512–3520. doi: 10.1080/10428194.2019.1639165 [DOI] [PubMed] [Google Scholar]
- 64.Pascual A, Calandra T, Bolay S, et al. Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin Infect Dis 2008; 46: 201–211. doi: 10.1086/524669 [DOI] [PubMed] [Google Scholar]
- 65.Pascual A, Csajka C, Buclin T, et al. Challenging recommended oral and intravenous voriconazole doses for improved efficacy and safety: population pharmacokinetics-based analysis of adult patients with invasive fungal infections. Clin Infect Dis 2012; 55: 381–390. doi: 10.1093/cid/cis437 [DOI] [PubMed] [Google Scholar]
- 66.Zhang Y, Hou K, Liu F, et al. The influence of CYP2C19 polymorphisms on voriconazole trough concentrations: systematic review and meta-analysis. Mycoses 2021; 64: 860–873. doi: 10.1111/myc.13293 [DOI] [PubMed] [Google Scholar]
- 67.Krishna G, Moton A, Ma L, et al. Pharmacokinetics and absorption of posaconazole oral suspension under various gastric conditions in healthy volunteers. Antimicrob Agents Chemother 2009; 53: 958–966. doi: 10.1128/AAC.01034-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen L, Krekels EHJ, Verweij PE, et al. Pharmacokinetics and pharmacodynamics of posaconazole. Drugs 2020; 80: 671–695. doi: 10.1007/s40265-020-01306-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Andes D, Kovanda L, Desai A, et al. Isavuconazole concentration in real-world practice: consistency with results from clinical trials. Antimicrob Agents Chemother 2018; 62: e00585-18. doi: 10.1128/AAC.00585-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pagano L, Cattaneo C, Quattrone M, et al. Isavuconazole-animal data and clinical data. J Fungi 2020; 6: 209. doi: 10.3390/jof6040209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.van der Linden JW, Arendrup MC, Warris A, et al. Prospective multicenter international surveillance of azole resistance in Aspergillus fumigatus. Emerg Infect Dis 2015; 21: 1041–1044. doi: 10.3201/eid2106.140717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lestrade PPA, Buil JB, van der Beek MT, et al. Paradoxal trends in azole-resistant Aspergillus fumigatus in a national multicenter surveillance program, the Netherlands, 2013–2018. Emerg Infect Dis 2020; 26: 1447–1455. doi: 10.3201/eid2607.200088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lestrade PP, Bentvelsen RG, Schauwvlieghe A, et al. Voriconazole resistance and mortality in invasive aspergillosis: a multicenter retrospective cohort study. Clin Infect Dis 2019; 68: 1463–1471. doi: 10.1093/cid/ciy859 [DOI] [PubMed] [Google Scholar]
- 74.Hamill RJ. Amphotericin B formulations: a comparative review of efficacy and toxicity. Drugs 2013; 73: 919–934. doi: 10.1007/s40265-013-0069-4 [DOI] [PubMed] [Google Scholar]
- 75.Shekhova E, Kniemeyer O, Brakhage AA. Induction of mitochondrial reactive oxygen species production by itraconazole, terbinafine, and amphotericin B as a mode of action against Aspergillus fumigatus. Antimicrob Agents Chemother 2017; 61: e00978-17. doi: 10.1128/AAC.00978-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vahedi-Shahandashti R, Dietl AM, Binder U, et al. Aspergillus terreus and the interplay with amphotericin B: from resistance to tolerance? Antimicrob Agents Chemother 2022; 66: e0227421. doi: 10.1128/aac.02274-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chamilos G, Kontoyiannis DP. Update on antifungal drug resistance mechanisms of Aspergillus fumigatus. Drug Resist Updat 2005; 8: 344–358. doi: 10.1016/j.drup.2006.01.001 [DOI] [PubMed] [Google Scholar]
- 78.Botero Aguirre JP, Restrepo Hamid AM. Amphotericin B deoxycholate versus liposomal amphotericin B: effects on kidney function. Cochrane Database Syst Rev 2015; 2015: CD010481. doi: 10.1002/14651858.CD010481.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Prentice HG, Hann IM, Herbrecht R, et al. A randomized comparison of liposomal versus conventional amphotericin B for the treatment of pyrexia of unknown origin in neutropenic patients. Br J Haematol 1997; 98: 711–718. doi: 10.1046/j.1365-2141.1997.2473063.x [DOI] [PubMed] [Google Scholar]
- 80.Herbrecht R, Denning DW, Patterson TF, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 2002; 347: 408–415. doi: 10.1056/NEJMoa020191 [DOI] [PubMed] [Google Scholar]
- 81.Cornely OA, Maertens J, Bresnik M, et al. Liposomal amphotericin B as initial therapy for invasive mold infection: a randomized trial comparing a high-loading dose regimen with standard dosing (AmBiLoad trial). Clin Infect Dis 2007; 44: 1289–1297. doi: 10.1086/514341 [DOI] [PubMed] [Google Scholar]
- 82.Aruanno M, Glampedakis E, Lamoth F. Echinocandins for the treatment of invasive aspergillosis: from laboratory to bedside. Antimicrob Agents Chemother 2019; 63: e00399-19. doi: 10.1128/AAC.00399-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhao Y, Perlin DS. Review of the novel echinocandin antifungal rezafungin: animal studies and clinical data. J Fungi 2020; 6: 192. 10.3390/jof6040192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jimenez-Ortigosa C, Moore C, Denning DW, et al. Emergence of echinocandin resistance due to a point mutation in the fks1 gene of Aspergillus fumigatus in a patient with chronic pulmonary aspergillosis. Antimicrob Agents Chemother 2017; 61: e01277-17. 10.1128/AAC.01277-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Heinz WJ, Buchheidt D, Ullmann AJ. Clinical evidence for caspofungin monotherapy in the first-line and salvage therapy of invasive Aspergillus infections. Mycoses 2016; 59: 480–493. doi: 10.1111/myc.12477 [DOI] [PubMed] [Google Scholar]
- 86.Kirkpatrick WR, Perea S, Coco BJ, et al. Efficacy of caspofungin alone and in combination with voriconazole in a guinea pig model of invasive aspergillosis. Antimicrob Agents Chemother 2002; 46: 2564–2568. doi: 10.1128/AAC.46.8.2564-2568.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Perea S, Gonzalez G, Fothergill AW, et al. In vitro interaction of caspofungin acetate with voriconazole against clinical isolates of Aspergillus spp. Antimicrob Agents Chemother 2002; 46: 3039–3041. doi: 10.1128/AAC.46.9.3039-3041.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Verweij PE, Ananda-Rajah M, Andes D, et al. International expert opinion on the management of infection caused by azole-resistant Aspergillus fumigatus. Drug Resist Updat 2015; 21–22: 30–40. doi: 10.1016/j.drup.2015.08.001 [DOI] [PubMed] [Google Scholar]
- 89.Caillot D, Thiebaut A, Herbrecht R, et al. Liposomal amphotericin B in combination with caspofungin for invasive aspergillosis in patients with hematologic malignancies: a randomized pilot study (Combistrat trial). Cancer 2007; 110: 2740–2746. doi: 10.1002/cncr.23109 [DOI] [PubMed] [Google Scholar]
- 90.Ankrah AO, Span LFR, Klein HC, et al. Role of FDG PET/CT in monitoring treatment response in patients with invasive fungal infections. Eur J Nucl Med Mol Imaging 2019; 46: 174–183. doi: 10.1007/s00259-018-4192-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Agarwal R, Vishwanath G, Aggarwal AN, et al. Itraconazole in chronic cavitary pulmonary aspergillosis: a randomised controlled trial and systematic review of literature. Mycoses 2013; 56: 559–570. doi: 10.1111/myc.12075 [DOI] [PubMed] [Google Scholar]
- 92.Jain LR, Denning DW. The efficacy and tolerability of voriconazole in the treatment of chronic cavitary pulmonary aspergillosis. J Infect 2006; 52: e133–e137. doi: 10.1016/j.jinf.2005.08.022 [DOI] [PubMed] [Google Scholar]
- 93.Saito T, Fujiuchi S, Tao Y, et al. Efficacy and safety of voriconazole in the treatment of chronic pulmonary aspergillosis: experience in Japan. Infection 2012; 40: 661–667. doi: 10.1007/s15010-012-0322-x [DOI] [PubMed] [Google Scholar]
- 94.Goyal RK. Voriconazole-associated phototoxic dermatoses and skin cancer. Expert Rev Anti Infect Ther 2015; 13: 1537–1546. doi: 10.1586/14787210.2015.1102053 [DOI] [PubMed] [Google Scholar]
- 95.Kohno S, Izumikawa K, Kakeya H, et al. Clinical efficacy and safety of micafungin in Japanese patients with chronic pulmonary aspergillosis: a prospective observational study. Med Mycol 2011; 49: 688–693. doi: 10.3109/13693786.2011.561369 [DOI] [PubMed] [Google Scholar]
- 96.Kravitz JN, Berry MW, Schabel SI, et al. A modern series of percutaneous intracavitary instillation of amphotericin B for the treatment of severe hemoptysis from pulmonary aspergilloma. Chest 2013; 143: 1414–1421. doi: 10.1378/chest.12-1784 [DOI] [PubMed] [Google Scholar]
- 97.Laursen CB, Davidsen JR, Van Acker L, et al. CPAnet registry–an international chronic pulmonary aspergillosis registry. J Fungi 2020; 6: 96. doi: 10.3390/jof6030096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Leeflang MM, Debets-Ossenkopp YJ, Wang J, et al. Galactomannan detection for invasive aspergillosis in immunocompromised patients. Cochrane Database Syst Rev 2015; 2015: CD007394 10.1002/14651858.CD007394.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mengoli C, Cruciani M, Barnes RA, et al. Use of PCR for diagnosis of invasive aspergillosis: systematic review and meta-analysis. Lancet Infect Dis 2009; 9: 89–96. doi: 10.1016/S1473-3099(09)70019-2 [DOI] [PubMed] [Google Scholar]
- 100.Guo YL, Chen YQ, Wang K, et al. Accuracy of BAL galactomannan in diagnosing invasive aspergillosis: a bivariate metaanalysis and systematic review. Chest 2010; 138: 817–824. doi: 10.1378/chest.10-0488 [DOI] [PubMed] [Google Scholar]
- 101.Zou M, Tang L, Zhao S, et al. Systematic review and meta-analysis of detecting galactomannan in bronchoalveolar lavage fluid for diagnosing invasive aspergillosis. PLoS One 2012; 7: e43347. doi: 10.1371/journal.pone.0043347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.de Heer K, Gerritsen MG, Visser CE, et al. Galactomannan detection in broncho-alveolar lavage fluid for invasive aspergillosis in immunocompromised patients. Cochrane Database Syst Rev 2019; 5: CD012399. 10.1002/14651858.CD012399.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sun W, Wang K, Gao W, et al. Evaluation of PCR on bronchoalveolar lavage fluid for diagnosis of invasive aspergillosis: a bivariate metaanalysis and systematic review. PLoS One 2011; 6: e28467. doi: 10.1371/journal.pone.0028467 [DOI] [PMC free article] [PubMed] [Google Scholar]