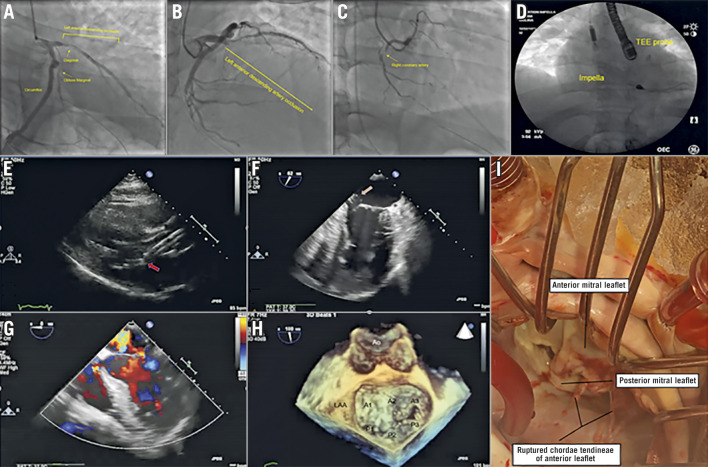
A 47-year-old man presented with witnessed out-of-hospital cardiac arrest at his wedding and anterior ST-elevation myocardial infarction. Initial blood pressure was 90/60 mmHg with pulse of 115 beats/minute. Coronary angiography showed 100% thrombotic occlusion of the proximal left anterior descending artery with Thrombolysis In Myocardial Infarction (TIMI) 0 flow, 90% disease in the proximal first diagonal, 80% disease in the small-calibre obtuse marginal-1, and 90% disease in the non-dominant mid right coronary artery (Figure 1A-Figure 1C). Aspiration thrombectomy was performed with the Pronto™ LP Extraction Catheter (Teleflex, Inc., Wayne, PA, USA), restoring sluggish flow. A 3.0×38 mm XIENCE (Abbott Vascular, Santa Clara, CA, USA) drug-eluting stent was deployed, establishing TIMI 3 flow. Haemodynamic support was provided with intra-aortic balloon counterpulsation and dopamine infusion. The patient developed significant hypoxaemia and pulmonary oedema requiring intubation, mechanical ventilation, and intravenous furosemide. Because of refractory cardiogenic shock, the patient was transferred to our hospital for advanced mechanical support. Workup showed lactate of 5.5 mmol/L and peak troponin-I of 90 ng/mL. After Heart Team discussion, the patient underwent transaxillary Impella™ 5.0 (Abiomed Inc., Danvers, MA, USA) implantation (Figure 1D). Within 48 hours, the patient’s haemodynamics improved; he was extubated and remained neurologically intact. The Impella P level was reduced as tolerated by haemodynamics; however, the patient continued to report significant orthopnoea. Chest X-ray demonstrated persistent pulmonary congestion. Transthoracic echocardiography (TTE) showed Impella inlet entrapment in the mitral subvalvular apparatus (Figure 1E, Moving image 1) and moderate mitral regurgitation (MR). The patient underwent explantation of the Impella device after 96 hours; however, the degree of MR remained unchanged. Console data review did not show any alarms or malfunction. To define the aetiology (ischaemic versus iatrogenic) and degree of MR better, transoesophageal echocardiography (TEE) was performed, which showed severe eccentric MR (Figure 1F, Figure 1G, Moving image 2, Moving image 3), while three-dimensional TEE showed flail A3, P3 scallops (Figure 1H, Moving image 4). Because of extensive damage noted intraoperatively (ruptured chordae tendineae) (Figure 1I), mitral valve repair was not feasible, and the patient underwent bioprosthetic mitral valve replacement. Left internal mammary to diagonal and saphenous vein to left posterolateral branch bypass grafting was also performed. Though rare, our case highlights an important complication of Impella-related chordal rupture and severe MR. Echocardiography is valuable to verify proper placement initially and on follow-up. Optimal placement of the Impella device is accomplished by positioning the inlet approximately 3.5 cm from the aortic valve annulus and avoiding posterior placement of the device towards the mitral valve leaflets. Accurate device positioning is critical to prevent mechanical valve injury.
Figure 1.
Impella entrapment in the mitral subvalvular apparatus in a patient with acute myocardial infarction and cardiogenic shock. A) - C) Coronary angiography. D) Cinefluoroscopy of the Impella in situ. E) TTE (parasternal long-axis view) - Impella abutting mitral valve (arrow). F) TEE showing flail P3 scallop (arrow). G) Colour TEE showing severe eccentric MR. H) 3D-TEE showing flail A3/P3 scallops. I) Ruptured chordae tendineae.
Supplementary data
Transthoracic echocardiogram (parasternal long-axis view) showing an Impella device abutting the mitral valve (red arrow).
Transoesophageal echocardiogram showing a flail P3 scallop (red arrow).
Colour transoesophageal echocardiogram showing severe eccentric mitral regurgitation.
Three-dimensional transoesophageal echo-cardio-gram showing flail A3 and P3 scallops.
Acknowledgments
Conflict of interest statement
R. Waksman reports being on the advisory board of Amgen, Boston Scientific, Cardioset, Cardiovascular Systems Inc., Medtronic, Philips, and Pi-Cardia Ltd., being a consultant to Amgen, Biotronik, Boston Scientific, Cardioset, Cardiovascular Systems Inc., Medtronic, Philips, and Pi-Cardia Ltd., receiving grant support from AstraZeneca, Biotronik, Boston Scientific, and Chiesi, being on the speakers bureau of AstraZeneca and Chiesi, and being an investor in MedAlliance. The other authors have no conflicts of interest to declare.
Contributor Information
Nauman Khalid, Section of Interventional Cardiology, MedStar Washington Hospital Center, Washington, DC, USA.
Evan Shlofmitz, Section of Interventional Cardiology, MedStar Washington Hospital Center, Washington, DC, USA.
Brian C. Case, Section of Interventional Cardiology, MedStar Washington Hospital Center, Washington, DC, USA.
Ron Waksman, Section of Interventional Cardiology, MedStar Washington Hospital Center, Washington, DC, USA.
References
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiogram (parasternal long-axis view) showing an Impella device abutting the mitral valve (red arrow).
Transoesophageal echocardiogram showing a flail P3 scallop (red arrow).
Colour transoesophageal echocardiogram showing severe eccentric mitral regurgitation.
Three-dimensional transoesophageal echo-cardio-gram showing flail A3 and P3 scallops.